Abstract
Background
Iterative reconstruction algorithms are often used to reduce image noise in low-dose coronary computed tomography angiography (CCTA) but encounter limitations. The newly introduced deep learning image reconstruction (DLIR) algorithm may provide new opportunities. We assessed the image quality and diagnostic performance of DLIR in low radiation dose and contrast medium dose CCTA of pediatric patients with 70 kVp and a shortened injection protocol.
Methods
This was a prospective study. A total of 27 consecutive arrhythmic pediatric patients were enrolled in the study group and underwent CCTA using a prospective ECG-triggered single-beat protocol: tube voltage 70 kVp, automatic tube current modulation for a noise index (NI) of 22, and contrast dose of 0.4–0.6 mL/kg. Images were reconstructed with DLIR. They were compared with 27 matched patients in the control group scanned with 80 kVp, a lower NI setting (NI =19), and a higher contrast dose (0.8–1.2 mL/kg). The images in the control group were reconstructed using the adaptive statistical iterative reconstruction (ASIR-V) algorithm. The image contrast, image quality, and diagnostic confidence were assessed by 2 experienced radiologists using a 5-point scale (1: nondiagnostic and 5: excellent). The CT value and standard deviation of the aorta and perivascular tissue were measured, and the contrast-to-noise ratio (CNR) for the aorta was calculated. The contrast medium and radiation doses were compared.
Results
The study and control groups had similar image contrast scores (4.75±0.57 vs. 4.78±0.42), image quality scores (3.67±0.47 vs. 3.44±0.51), and diagnostic confidence (4.74±0.44 vs. 4.74±0.45) (all P>0.05). There was an adequate enhancement in the aorta (614.74±127.73 vs. 705.89±111.20 HU) and similar CNR (20.34±4.64 vs. 20.99±4.14) in both groups. The image noise of the study group was lower in the aorta (30.61±3.88 vs. 34.77±3.49) and similar in perivascular tissue (27.66±6.24 vs. 27.55±3.33) compared with the control group. The study group reduced the total contrast medium dose by 53% to 15.07±3.68 mL and radiation dose by 36% to 0.57±0.31 mSv.
Conclusions
The DLIR algorithm in CCTA for children using 70 kVp tube voltage with a shortened contrast medium injection protocol maintains image quality and diagnostic confidence while significantly reducing contrast medium dose and radiation dose compared with the use of the conventional CCTA protocol.
Keywords: Tomography, X-ray computed, coronary angiography, child, deep learning, image reconstruction
Introduction
Coronary computed tomography angiography (CCTA) is the first-line diagnostic imaging method for children with coronary artery diseases (1-3), such as those of abnormal origin (4) and coronary aneurysm (5). Reducing radiation and contrast medium doses while providing acceptable image quality (6,7), eliminating motion artifacts (8,9), and maintaining fast and easy operation remains the research focuses. In recent years, through the application of faster gantry rotation and motion correction algorithms such as the Snapshot Freeze (SSF) and wide-detector coverage for the single-beat cardiac scan technique and other technologies, CCTA image quality has been significantly improved. Simultaneously, low voltage technology has been used to increase the iodine CT value, thereby reducing the amount of contrast medium. Additionally, various iterative reconstruction techniques have been used to reduce image noise so that the required radiation dose is further reduced. However, through literature review, we have found that reducing radiation dose and contrast medium dose in CCTA has reached a plateau. Conventional iterative reconstruction algorithms need to balance image noise, spatial resolution and image appearance. Literature review shows that most contrast medium injection protocols still require 8–12 s of injection time (7,10-13). To further reduce radiation dose and contrast medium dose while maintaining the contrast medium concentration and injection rate, we have designed a new protocol in pediatric CCTA. This protocol has a shortened contrast medium injection time to reduce contrast dose, a 70 kVp tube voltage to boost contrast enhancement in vessels, and a newly developed deep learning image reconstruction (DLIR, GE Healthcare, USA) to reduce image noise and maintain the image quality at a lower radiation dose. The purpose of this study was to evaluate the image quality of the reduced contrast medium dose and radiation dose CCTA using 70 kVp and DLIR for children.
Methods
Patient information
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was a prospective study, which the Ethical Committee approved of Beijing Children’s Hospital. The study protocols were performed following the approved guidelines and regulations of our hospital and informed consents were signed by the parents of pediatric patients. The scan data in the study group for children who suffered from arrhythmia were collected from 2020-03-17 to 2020-05-21. The scan data for the control group were retrospectively selected from the hospital database before June 01, 2018. The inclusion criteria were as follows: patients with a clinical diagnosis of arrhythmia; echocardiogram (Echo) showed no abnormal cardiac structure; under 18 years of age. The exclusion criteria were as follows: ejection fraction on Echo was lower than 50%; the arrhythmia was caused by a definite primary disease, such as Kawasaki disease or infective endocarditis.
CCTA scan parameters
All children were scanned on a 256-row detector CT scanner (Revolution CT, GE Healthcare, USA) with prospective electrocardiography triggering. The acquisition cardiac phase windows (R-R interval) for cardiac scans were automatically selected by the scanner and were dependent on the children’s heart rates (HR) just before CCTA: 75% for HR =30–60 bpm, 40–80% for HR =60–78 bpm, 35–55% for HR =78–120 bpm, and 0–100% for HR >120 bpm. The detector z-coverage was 8–16 cm depending on the children’s heart sizes between the aorta arch and diaphragm, the matrix size was 512×512 pixels, voxel size was 0.625 mm, gantry rotation time was 0.28 second/rotation, and the display field-of-view (DFOV) for the image reconstruction was 250 mm with an image slice thickness and interval of 0.625 mm. For the study group, tube voltage was 70 kVp, and tube current was given by the automatic tube current modulation technique with an mA range of 198–499 mA to obtain a noise index (NI) of 22. NI is a parameter in the scan protocol to control radiation dose: higher NI requires a lower radiation dose. The NI value in the study group was higher than that (NI =19, see below) of the control group to reduce radiation dose, and the adjustment referenced previous research by Benz et al. (13), which indicated that the use of DLIR could reduce about 26% of image noise compared with 70% ASIR-V. Data acquisition was triggered using a bolus-tracking technique, which started at the shortest delay time (about 1.5 s based on the current modulation) after the CT value in the descending aorta became higher than the triggering threshold of 190 HU. For the control group, tube voltage was 80 kVp, NI was 19 with an mA range of 203–499 mA, and data acquisition started 3.5 s after the CT value reached 220 HU. Some children were too young to cooperate, and sedation with oral chloral hydrate (10%, 0.4 mL/kg) was applied to these children before the CT scan. The contrast medium Iohexol (350 mgI/mL, GE healthcare, Ireland) was used, and contrast dose was adjusted according to the bodyweight of the children: 0.4–0.5 mL/kg (0.5 mL/kg for 20–30 kg, 0.4 mL/kg for heavier than 30 kg) in the study group, and 0.8–1.2 mL/kg (1.2 mL/kg for 20–35 kg, 1.0 mL/kg for 35–50 kg, 0.8 mL/kg for heavier than 50 kg) in the control group. The contrast medium was injected with a fixed injection time of 4 s in the study group, followed by 0.9% saline solution with a volume double the amount of contrast medium and injected in 8 s. For the control group, the contrast medium was injected with a fixed injection time of 8 s, followed by 0.9% saline solution with a volume half the amount of contrast medium and injected in 4 s. All injections were performed using a double head injector (EmpowerCTA+, Bracco Injeneering S.A., NJ, USA). Scan protocols for the study group and control group are listed in Table 1.
Table 1. Scan protocols for the study group and control group.
| Parameter | Study group | Control group |
|---|---|---|
| Scan voltage (kVp) | 70 | 80 |
| Tube current range (mA) | 198–499 | 203–499 |
| Noise index | 22 | 19 |
| Triggering threshold (HU) | 190 | 220 |
| Acquisition started after trigger (s) | 1.5 | 3.5 |
| Contrast medium (CM) dose (mL/kg) | 0.4–0.8 | 0.8–1.8 |
| Injection duration of CM (s) | 4 | 8 |
| 0.9% saline solution (NS) dose (mL/kg) | 0.8–1.6 | 0.4–0.9 |
| Injection duration of NS (s) | 8 | 4 |
| Image reconstruction (algorithm) | DL–H | 50% ASIR–V |
CM, contrast medium; NS, 0.9% saline solution; DL-H, deep learning image reconstruction with the high setting; 50% ASIR-V, adaptive statistical iterative reconstruction-V with 50% weighting percentage.
CCTA image reconstruction
The cardiac phase with the least motion artifacts was selected by an experienced radiologist (with 16 years of experience in pediatric CT and cardiovascular disease diagnosis). The images in the study group were reconstructed using the DLIR with a high setting (DL-H), and the images in the control group were reconstructed using the state-of-the-art ASIR-V algorithm with a weight of 50% (50% ASIR-V). The motion correction technique (SSF) was applied in image reconstructions in both groups.
Subjective evaluation
All images were transmitted to a GE AW4.7 CT workstation (GE Healthcare, USA) for analysis. The relevant information of children, scanning parameters, and reconstruction algorithms was shielded. Two cardiovascular radiologists (with 15 and 9 years of experience in pediatric CT imaging for cardiovascular disease) who were blinded to the reconstruction algorithms assessed the image quality of CCTA in random order. If the scores given by the 2 observers were not the same, a third senior doctor with 17 years of experience in reviewing CCTA images would evaluate the images and gave the final score. During the evaluation process, the 2 radiologists could adjust window width and level according to their habits, and multiplanar reconstruction (MPR) and volume rendering (VR) were also available for viewing. Accordingly, a 5-point grading system was used to evaluate the image quality, including artery contrast which represented enhancement degree in arteries, and image quality which included margin resolution, image noise, and diagnosis confidence separately. For artery contrast, the scores were: 5= strong; 4= good; 3= moderate and acceptable; 2= not adequate; and 1= not acceptable. For image quality, the scores were: 5= excellent; 4= good; 3= moderate and acceptable; 2= blurred margin and not acceptable; and 1= not detectable. For diagnosis confidence, the scores were: 5= very confident; 4= confident; 3= moderately confident and acceptable; 2= not confident; and 1= cannot make diagnosis. Scores greater than or equal to 3 were considered acceptable.
The objective image assessment was performed by the 2 same observers together. For every patient, the aortic (Ao) root was examined at the left main coronary artery level on an axial image. The mean attenuation (CT value) and its standard deviation (SD) in Hounsfield units (HU) of the aorta and adjacent perivascular tissue (PT) on the same slice were measured by placing a region of interest (ROI) on these areas (Figure 1). From these measurements, the signal-to-noise ratio (SNR) and the contrast-to-noise ratio (CNR) for the descending aorta were calculated using the following formula:
Figure 1.
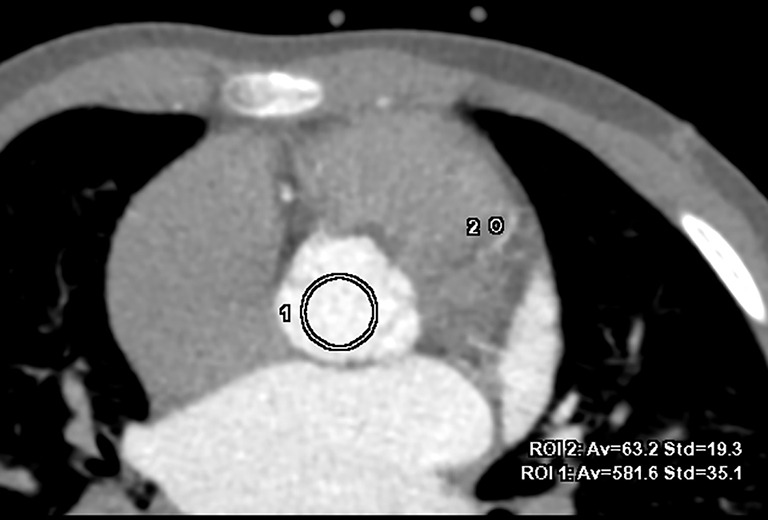
Quantitative image analysis with an axial image of deep learning image reconstruction with a high setting (DL-H) depicting the aortic root and the left main artery. CT value and standard deviation (SD), representing image noise, in the aortic root (circle 1) for the aorta (Ao) and the perivascular tissue (PT) of the ventricle (circle 2) were measured. Since children have less fat than adults, soft tissues, like ventricle muscles for PT, were selected to measure CT value and SD for the background.
| [1] |
| [2] |
Radiation dose and contrast medium dose
The radiation dose and contrast medium dose of the 2 groups were recorded. The radiation dose included the volumetric CT dose index (CTDIvol), dose-length product (DLP), and effective dose (ED). The ED was calculated using the following formula: ED = DLP × W. W is the patient age-dependent conversion factor for the chest area of pediatric patients based on the report of ICRP 103 for CT (14). The contrast dose included the total volume of the contrast medium and the amount of iodine used. The amount of iodine was calculated according to the concentration of the contrast medium.
Statistical analysis
Statistical analysis was performed using SPSS 22.0 software. All data were expressed as mean ± SD. For the 2 scan groups, continuous data were compared with the independent sample t-test, and nominal data were compared with the Chi-square test. The ordinal scales or continuous variables that failed to follow the normal distribution were analyzed using the Mann-Whitney U test. Interobserver agreement for the qualitative analysis of image quality was evaluated using Cohen’s kappa (k), where kappa values <0 were considered as indicating no agreement, 0.0< k ≤0.2 as poor, 0.2< k ≤0.4 as fair, 0.4< k ≤0.6 as moderate, 0.6< k ≤0.8 as substantial, and 0.8< k ≤1.0 as excellent agreement. P<0.05 was considered to indicate a statistically significant difference.
Results
In the present study, 27 cases were eventually enrolled in the study group, and the average age was 9.3±3.1 years. There were 5 cases with the abnormal origin of the coronary artery, 3 cases with slightly thinner coronary diameter, 1 case with coronary sinus dilatation, 1 case with myocardial bridge, and 17 cases were normal. For the 27 cases in the control group, the average age was 9.5±2.4 years. There were 5 cases with the abnormal origin of the coronary artery, 1 case with coronary sinus dilatation, and 21 cases were normal. The contrast medium dose was 15.07±3.58 mL, and the ED was 0.57±0.31 mSv in the study group, which were 53% and 36% lower than the contrast medium dose (32.15±7.84 mL) and ED (0.89±0.43 mSv) in the control group, respectively (P<0.05). The injection rate was 3.66±0.75 mL/s in the study group and 3.87±0.71 mL/s in the control group (P>0.05). Other information is listed in Table 2.
Table 2. Patient information of the study group and control group.
| Patient information | Study group | Control group | Statistical value | P value |
|---|---|---|---|---|
| Sex (male: female) | 13:14 | 12:15 | 0.07# | 0.79 |
| Age (years) | 9.3±3.1 (5 to 14) | 9.5±2.4 (5 to 13) | 0.26 | 0.79 |
| Weight (kg) | 35.7±12.6 (20 to 61) | 34.2±10.9 (20 to 59) | 0.50 | 0.62 |
| Heart rates (bpm) | 83.74±17.45 (59 to 121) | 81.59±16.25 (55 to 111) | 0.43 | 0.67 |
| CM dose (mL) | 15.07±3.75 (10 to 22) | 32.15±7.84 (24 to 48) | 10.41 | <0.001 |
| Injection rate (mL/s) | 3.66±0.75 (2.5 to 5.0) | 3.87±0.71 (2.8 to 5.5) | 1.04 | 0.31 |
| CTDIvol (mGy) | 1.40±0.57 (0.70 to 3.28) | 2.24±1.09 (0.95 to 5.74) | 3.35 | 0.01 |
| DLP (mGy.cm) | 18.56±8.46 (8.43 to 45.90) | 32.45±17.25 (12.89 to 91.84) | 3.61 | 0.01 |
| ED (mSv) | 0.57±0.31 (0.21 to 1.58)* | 0.89±0.43 (0.44 to 2.28) | 2.87 | 0.01 |
*, at present, there is no conversion factor for 70 kVp, so this paper used the corresponding 80 kVp conversion factors from the ICRP 103. #, statistical value of sex was compared with the Chi square test, other values were compared with the paired t-test. CM, contrast medium; CTDIvol, volume CT dose index; DLP, dose-length product; ED, effective dose.
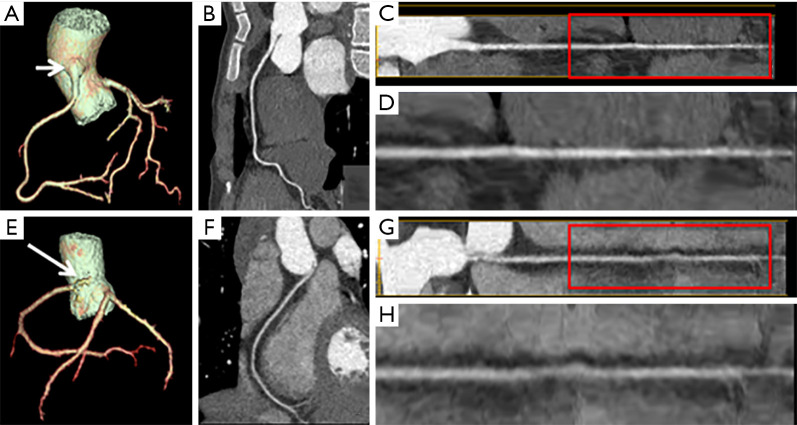
For the subjective evaluation, all images in both groups could display all coronary arteries clearly and had strong confidence for diagnosis (Figure 2). The image contrast score (4.56±0.57 vs. 4.78±0.42), overall image quality score (3.67±0.47 vs. 3.44±0.51), and diagnostic confidence (4.74±0.44 vs. 4.74±0.45) had no statistically significant differences (P>0.05) (Figure 3).
Figure 2.
(A,B,C,D) Images of the right coronary artery (RCA) of a 13-year-old girl in the study group. (A) 3D reconstruction; (B) curved image; (C) RCA analysis image and (D) an enlarged image of (C). (E,F,G,H) Images of the right coronary artery (RCA) of a 10-year-old girl in the control group. (E) 3D reconstruction; (F) curved image; (G) RCA analysis image and (H) an enlarged image of 2G. The girl in the study group weighed 49 kg and suffered from arrhythmia. The total contrast medium volume was 20 mL. Her RCA originated from the aorta, higher than the right coronary sinus (white arrow). The enhancement in the RCA was high, with a contrast score of 5, and the margin was clear and sharp. The perivascular tissue (PT) was clear enough and image noise was low, resulting in an image quality score of 4 and a very confident diagnosis with a score of 5. The girl in the control group weighed 38 kg and suffered from arrythmia. The total contrast medium volume was 38 mL. Her RCA arose from the middle of the left and right coronary sinus (long white arrow). The contrast in the RCA was high, with a contrast score of 5, and the margin was moderate and acceptable. The PT was a little blurry and image noise was high but accepted, resulting in an overall image quality score of 3, and a very confident diagnosis with a score of 5.
Figure 3.
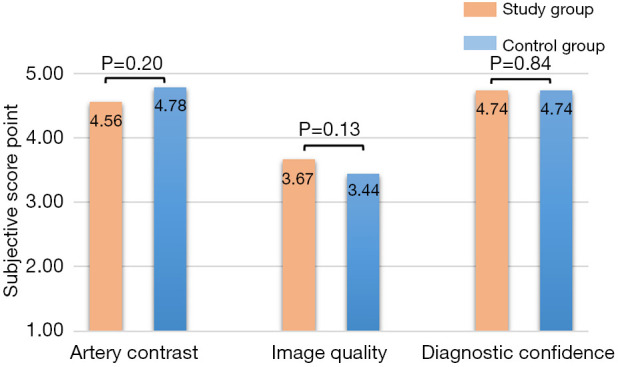
Subjective score comparison. There were no statistical differences in all aspects of subjective scores between the study group and control group.
The objective measurement results are listed in Table 3. Both groups had adequate contrast enhancement in vessels. The control group had a 14.8% higher CT value (705.89±111.20 vs. 614.74±127.73 HU) and a 13.6% higher SD value (34.77±3.49 vs. 30.61±3.88 HU) in the aorta than the study group (P<0.05). The study group had a 12.6% higher CT value in PT (63.78±9.37 vs. 56.63±12.55 HU, P<0.05), but a similar SD value (27.66±6.24 vs. 27.55±3.33, P=0.94) compared with the control group. SNR (20.34±4.72 vs. 20.47±3.61) and CNR (19.18±4.84 vs. 20.99±4.14) for the aorta had no statistically significant differences between the 2 groups (P>0.05). Interobserver agreement was substantial concerning the overall image quality (k =0.79, P<0.05).
Table 3. The results of objective evaluation.
| Objective result | Study group | Control group | t value | P value |
|---|---|---|---|---|
| Ao CT value (Hu) | 614.74±130.16 (339.3 to 876.8) | 705.89±111.2 (493.0 to 1,014.1) | 2.58 | 0.02 |
| Ao SD | 30.61±3.88 (22.2 to 39.1) | 34.77±3.49 (30.1 to 41.8) | 3.84 | <0.001 |
| PT CT value (Hu) | 63.78±9.37 (41.2 to 81.0) | 56.63±12.55 (35.0 to 83.8) | 2.44 | 0.02 |
| PT SD | 27.66±6.24 (16.5 to 37.3) | 27.55±3.33 (20.1 to 34.4) | 0.07 | 0.94 |
| Ao SNR | 20.34±4.72 (10.00 to 30.77) | 20.47±3.61 (13.58 to 28.40) | 0.10 | 0.92 |
| Ao CNR | 19.18±4.84 (9.58 to 30.02) | 20.99±4.14 (13.04 to 28.29) | 1.36 | 0.19 |
All statistical values were compared with the paired t-test. Ao, aortic root; PT, perivascular tissue; SD, standard deviation for noise; SNR, signal-to-noise ratio; CNR, contrast-to-noise ratio.
Discussion
This study evaluated the image quality of reduced contrast medium dose and radiation dose CCTA for children by using a shortened contrast medium injection time and 70 kVp tube voltage acquisition together with a newly developed commercially available DLIR algorithm. DLIR is less constrained by the limited parameters in traditional modeling methods such as iterative reconstruction algorithms. DLIR incorporates millions of parameters for reconstruction through a deep learning process with no need to simplify the complex models of the actual detection system into limited parameters as in the current iterative reconstruction algorithms. These millions of parameters can be directly formed through the training process using artificial intelligence and deep neural networks. By doing so, DLIR can overcome the usual tradeoffs between image noise and spatial resolution in the conventional IR algorithms. Therefore, DLIR can reduce image noise more effectively than IR algorithms and overcome the “blurred margins” often seen in high-strength IR images, restricting their ability to improve image quality (15). It has been pointed out that DLIR (16) or deep learning-based post-processing algorithms (17) can significantly reduce image noise in CCTA, improve the display of blood vessels, and improve the image quality compared with conventional IR algorithms under the same radiation dose condition. Greffier et al. (18) demonstrated the potential of DLIR in reducing radiation dose and image noise while maintaining the favorable image noise power spectrum and avoiding a blotchy or plastic-looking appearance in the images associated with the conventional high-strength iterative reconstruction algorithms in a phantom study. Lenfant et al. (19) and Bernard et al. (20) also demonstrated the ability of deep learning-based image reconstruction (DLR) by Canon Medical Systems to improve image quality in CT pulmonary angiography and CCTA with reduced radiation dose, respectively. Our study evaluated the performance of DLIR by GE Healthcare in maintaining image quality and diagnostic confidence with both reduced radiation dose and contrast medium dose. The radiation dose reduction was realized using a higher NI setting (from 19 to 22), and the contrast dose reduction was realized by using a shortened contrast injection time in the scan protocol for the study group. Our results demonstrated adequate enhancement in the vessels and 12% image noise reduction in the aorta with slightly higher image quality (3.67±0.47 vs. 3.44±0.51) and excellent diagnostic confidence, while further reducing contrast dose by 53% and radiation dose by 36% in the study group compared with the conventional low dose CCTA protocol. Perisinakis et al. (21) reported that tissues receive higher amounts of radiation dose if CT acquisition is performed after contrast medium administration. Given that tissue uptake in the control group was expected to be higher than the study group, the dose difference reported in our study might be slightly underestimated since the DLP to ED conversion factor does not take into account tissue contrast uptake. Namely, the use of a lower contrast amount for the examination in the study group might provide a bonus towards reducing the absorbed radiation dose burden of the patient.
CCTA is the first-line imaging modality to detect pediatric coronary artery abnormalities. Although CCTA has obvious advantages over other methods (22,23), we still strive to reduce the radiation dose and contrast medium dose according to the ALARA principle. At present, the more widely used method is to use low tube voltage scanning to improve contrast enhancement in blood vessels combined with iterative reconstruction (IR) algorithms or deep learning-based image reconstruction algorithms (16,17) to reduce image noise, to ensure adequate contrast-to-noise for blood vessels to meet the diagnostic requirements. For the contrast injection in CCTA, the guidelines suggest 1–2 mL/kg for the contrast medium dose and an injection time of 10s for children (24). The recommended 10s injection time is more relevant when the total scan time of CCTA requires a few seconds to cover the entire heart. With the use of a 16-cm wide detector coverage, the scan time for the whole heart is less than 1 second, and the injection time can be substantially shortened. Therefore, in this study, we proposed a new CCTA protocol with a commonly available contrast medium (Iohexol with a concentration of 350 mgI/mL) and the same contrast injection rate, but a much shorter injection time for contrast injection to reduce the total amount of contrast medium dose by more than 50%. However, to ensure the contrast medium completely entered the left ventricular system, the total injection time in this new contrast medium injection protocol remained unchanged. The injection time for contrast medium was shortened to 4 s, and the injection time for follow-up saline was extended to 8 s, for a total injection time of 12 s. By shortening the contrast medium injection to 4 s, we substantially reduced the contrast dose to patients. This also reduced the concentration of contrast medium in the bloodstream. To compensate for this decrease, we used a low tube voltage of 70 kVp to boost the contrast enhancement in the vessels. Our results indicated that even at the reduced contrast dose, we still obtained an average enhancement of approximately 600 HU in the aorta in the study group, which is adequate for diagnosis, and a high subjective rating for image contrast in the study group that was similar to the control group. Relevant guidelines have pointed out that a coronary CT value higher than 250 HU can meet the diagnostic requirements. Therefore, we believe there might be room for further contrast dose reduction in the future. The high CT attenuation value in the vessels also allowed us to further relax the image noise requirement to achieve a clinically acceptable CNR. The relaxed image noise requirement was directly translated into a lower radiation dose requirement in our study, with a higher NI setting (from the conventional 19 to 22 in the study group).
With the shortened contrast medium injection duration and short scan duration of less than 1s, the scan timing becomes very critical. There was only a short time window of less than 4s for scanning in the study group, and we needed to trigger the scan as soon as possible after the contrast medium entered the aorta. Therefore, in the study group, we reduced the trigger threshold value from the conventional 220 to 190 HU and applied the shortest scan delay time of the CT scanner after triggering, which was 1.50±0.11 s from the original scan delay time of 3.5 s. This change proved to be effective for capturing the peak enhancement for the short scan scenario with the wide-detector CT scanner.
There were some limitations in this study. First, because this was a pilot study, the number of cases included in the study group was limited. Furthermore, parameters such as scan and injection protocols between the 2 groups did not match precisely. Hence, this research was not a truly comparative study, which might introduce statistical bias. Even though the results could already demonstrate the validity of the study design, further study is required with larger sample size and a design with fewer variables. In our research, the weights of some children were higher than 50 kg, up to 61 kg, although this study was focused on pediatric CCTA. There is some space to use the same logic in slim adult patients. Second, the age distribution of cases was not uniformly distributed. All cases were over 5 years of age, and the suitability for the younger age group was not verified. Third, all cases were diagnosed with CCTA, and there was no further invasive coronary angiography or surgery for confirmation in terms of diagnostic accuracy. Fourth, there was still no literature reporting the conversion factor for 70 kVp, so we used the conversion factor for 80 kVp by Deak et al. to represent 70 kVp instead (14). In our study, we did not consider the potential differences in such conversion factors for males and females. However, in our research, the 2 groups had a similar boy/girl ratio (13:14 and 12:15, respectively), so the impact on the dose-comparison could be ignored.
Conclusions
We have proposed a method to reduce contrast medium dose and radiation dose in CCTA for children by using a shortened contrast injection time and 70 kVp tube voltage combined with DLIR. We demonstrated that a significant reduction in contrast medium dose and radiation dose could be achieved while maintaining similar image quality and diagnostic confidence by using DLIR in image reconstruction, compared with the conventional CCTA protocol using the state-of-the-art 50% ASIR-V algorithm.
Acknowledgments
The authors would like to thank Dr. Zhimin Liu, a senior cardiovascular radiologist, for helping us to produce the final subjective evaluation results in case of disagreement between the two observers. We also would like to thank Dr. Xuan Zhang, Dr. Min Yu for their help in generating DLIR images and Dr. Ying Zheng for her help in understanding the advanced cardiac CT scan techniques
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethical Committee of Beijing Children’s Hospital. The study protocols were performed in accordance with the approved guidelines and regulations of our hospital. Informed consents were signed by the parents of pediatric patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/qims-20-1159). Dr. JL reports that he is an employee of GE Healthcare, the manufacturer of the CT system used in this study. The other authors have no conflicts of interest to declare.
References
- 1.Moss AJ, Williams MC, Newby DE, Nicol ED. The Updated NICE Guidelines: Cardiac CT as the First-Line Test for Coronary Artery Disease. Curr Cardiovasc Imaging Rep 2017;10:15. 10.1007/s12410-017-9412-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koplay M, Kizilca O, Cimen D, Sivri M, Erdogan H, Guvenc O, Oc M, Oran B. Prospective ECG-gated High-Pitch Dual-Source Cardiac CT Angiography in the Diagnosis of Congenital Cardiovascular Abnormalities: Radiation Dose and Diagnostic Efficacy in a Pediatric Population. Diagn Interv Imaging 2016;97:1141-50. 10.1016/j.diii.2016.03.014 [DOI] [PubMed] [Google Scholar]
- 3.Yang FB, Guo WL, Sheng M, Sun L, Ding YY, Xu QQ, Xu MG, Lv HT. Diagnostic Accuracy of Coronary Angiography Using 64-slice Computed Tomography in Coronary Artery Disease. Saudi Med J 2015;36:1156-62. 10.15537/smj.2015.10.12415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia-Arribas D, Olmos C, Higueras J, Marcos-Alberca P, de la Pedraja I, Garcia-Bouza M. Anomalous Origin of Left Coronary Artery With Intramural Aortic Course Causing Symptoms in a Teenaged Athlete. Tex Heart Inst J 2020;47:165-7. 10.14503/THIJ-16-5771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goh YG, Ong CC, Tan G, Liang CR, Soomar SM, Lim CW, Quek SC, Teo LS. Coronary Manifestations of Kawasaki Disease in Computed Tomography Coronary Angiography. J Cardiovasc Comput Tomogr 2018;12:275-80. 10.1016/j.jcct.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 6.Tanabe Y, Kido T, Kimura F, Kobayashi Y, Matsunaga N, Yoshioka K, Yoshimura N, Mochizuki T. Japanese Survey of Radiation Dose Associated With Coronary Computed Tomography Angiography - 2013 Data From a Multicenter Registry in Daily Practice. Circ J 2020;84:601-8. 10.1253/circj.CJ-19-0843 [DOI] [PubMed] [Google Scholar]
- 7.Shirasaka T, Nagao M, Yamasaki Y, Kojima T, Kondo M, Hamasaki H, Kamitani T, Kato T, Asayama Y. Low Radiation Dose and High Image Quality of 320-Row Coronary Computed Tomography Angiography Using a Small Dose of Contrast Medium and Refined Scan Timing Prediction. J Comput Assist Tomogr 2020;44:7-12. 10.1097/RCT.0000000000000951 [DOI] [PubMed] [Google Scholar]
- 8.Liang J, Wang H, Xu L, Yang L, Dong L, Fan Z, Wang R, Sun Z. Diagnostic Performance of 256-row Detector Coronary CT Angiography in Patients With High Heart Rates Within a Single Cardiac Cycle: A Preliminary Study. Clin Radiol 2017;72:694.e7-14. 10.1016/j.crad.2017.03.004 [DOI] [PubMed] [Google Scholar]
- 9.Liang J, Sun Y, Ye Z, Sun Y, Xu L, Zhou Z, Thomsen B, Li J, Sun Z, Fan Z. Second-generation Motion Correction Algorithm Improves Diagnostic Accuracy of Single-Beat Coronary CT Angiography in Patients With Increased Heart Rate. Eur Radiol 2019;29:4215-27. 10.1007/s00330-018-5929-6 [DOI] [PubMed] [Google Scholar]
- 10.Zhang Q, Mi H, Shi X, Li W, Guo S, Wang P, Suo H, Wang Z, Jin S, Yan F, Niu Y, Xian J. Higher Iodine Concentration Enables Radiation Dose Reduction in Coronary CT Angiography. Acad Radiol 2020. doi: . [Epub ahead of print]. 10.1016/j.acra.2020.05.012 [DOI] [PubMed] [Google Scholar]
- 11.El Merhi F, Bou-Fakhredin R, El Ashkar B, Ghieh D, Ghosn Y, Saade C. State of the Art of Coronary Computed Tomography Angiography. Radiography (Lond) 2020;26:174-82. 10.1016/j.radi.2019.10.001 [DOI] [PubMed] [Google Scholar]
- 12.Chen Y, Liu Z, Li M, Yu Y, Jia Y, Ma G, Hu Z, Wei D, Li D, He T. Reducing Both Radiation and Contrast Doses in Coronary CT Angiography in Lean Patients on a 16-cm Wide-Detector CT Using 70 kVp and ASiR-V Algorithm, in Comparison with the Conventional 100-kVp Protocol. Eur Radiol 2019;29:3036-43. 10.1007/s00330-018-5837-9 [DOI] [PubMed] [Google Scholar]
- 13.Benz DC, Gräni C, Moch BH, Mikulicic F, Vontobel J, Fuchs TA, Stehli J, Clerc OF, Possner M, Pazhenkottil AP, Gaemperli O, Buechel RR, Kaufmann PA. A. Low-Dose and an Ultra-Low-Dose Contrast Agent Protocol for Coronary CT Angiography in a Clinical Setting: Quantitative and Qualitative Comparison to a Standard Dose Protocol. Br J Radiol 2017;90:20160933. 10.1259/bjr.20160933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deak PD, Smal Y, Kalender WA. Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 2010;257:158-66. 10.1148/radiol.10100047 [DOI] [PubMed] [Google Scholar]
- 15.Park C, Choo KS, Jung Y, Jeong HS, Hwang J, Yun MS. CT iterative vs deep learning reconstruction: comparison of noise and sharpness. Eur Radiol 2021;31:3156-64. 10.1007/s00330-020-07358-8 [DOI] [PubMed] [Google Scholar]
- 16.Benz DC, Benetos G, Rampidis G, von Felten E, Bakula A, Sustar A, Kudura K, Messerli M, Fuchs TA, Gebhard C, Pazhenkottil AP, Kaufmann PA, Buechel RR. Validation of Deep-Learning Image Reconstruction for Coronary Computed Tomography Angiography: Impact on Noise, Image Quality and Diagnostic Accuracy. J Cardiovasc Comput Tomogr 2020;14:444-51. 10.1016/j.jcct.2020.01.002 [DOI] [PubMed] [Google Scholar]
- 17.Liu P, Wang M, Wang Y, Yu M, Wang Y, Liu Z, Li Y, Jin Z. Impact of Deep Learning-based Optimization Algorithm on Image Quality of Low-dose Coronary CT Angiography With Noise Reduction: A Prospective Study. Acad Radiol 2020;27:1241-8. 10.1016/j.acra.2019.11.010 [DOI] [PubMed] [Google Scholar]
- 18.Greffier J, Hamard A, Pereira F, Barrau C, Pasquier H, Paul Beregi J, Frandon J. Image quality and dose reduction opportunity of deep learning image reconstruction algorithm for CT: a phantom study. Eur Radiol 2020;30: 3951-9. 10.1007/s00330-020-06724-w [DOI] [PubMed] [Google Scholar]
- 19.Lenfant M, Chevallier O, Comby P, Secco G, Haioun K, Ricolfi F, Lemogne B, Loffroy R. Deep Learning Versus Iterative Reconstruction for CT Pulmonary Angiography in the Emergency Setting: Improved Image Quality and Reduced Radiation Dose. Diagnostics (Basel) 2020;10:558. 10.3390/diagnostics10080558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bernard A, Comby P, Lemogne B, Haioun K, Ricolfi F, Chevallier O, Loffroy R. Deep learning reconstruction versus iterative reconstruction for cardiac CT angiography in a stroke imaging protocol: reduced radiation dose and improved image quality. Quant Imaging Med Surg 2021;11:392-401. 10.21037/qims-20-626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perisinakis K, Tzedakis A, Spanakis K, Papadakis AE, Hatzidakis A, Damilakis J. The effect of iodine uptake on radiation dose absorbed by patient tissues in contrast enhanced CT imaging: Implications for CT dosimetry. Eur Radiol 2018;28:151-8. 10.1007/s00330-017-4970-1 [DOI] [PubMed] [Google Scholar]
- 22.Tan SK, Ng KH, Yeong CH, Aman RRAR, Sani FM, Aziz YFA, Sun Z, Personalized administration of contrast medium with high delivery rate in low tube voltage coronary computed tomography angiography. Quant Imaging Med Surg 2019;9:552-64. 10.21037/qims.2019.03.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leipsic J, Abbara S, Achenbach S., Cury R, Earls JP, Mancini GJ, Nieman K, Pontone G, Raff GL. SCCT Guidelines for the Interpretation and Reporting of Coronary CT Angiography: A Report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2014;8:342-58. 10.1016/j.jcct.2014.07.003 [DOI] [PubMed] [Google Scholar]
- 24.Abbara S, Blanke P, Maroules CD, Cheezum M, Choi AD, Han BK, Marwan M, Naoum C, Norgaard BL, Rubinshtein R, Schoenhagen P, Villines T, Leipsic J. SCCT Guidelines for the Performance and Acquisition of Coronary Computed Tomographic Angiography: A Report of the Society of Cardiovascular Computed Tomography Guidelines Committee: Endorsed by the North American Society for Cardiovascular Imaging (NASCI). J Cardiovasc Comput Tomogr 2016;10:435-49. 10.1016/j.jcct.2016.10.002 [DOI] [PubMed] [Google Scholar]