Abstract
Subchondral insufficiency fracture (SIF) of the medial femoral condyle has been proposed to be a primary event in so-called ‘spontaneous osteonecrosis of the knee’. SIF is also known to be associated with bone marrow lesions (BML), but the detailed histopathology of the BML has not been fully clarified. We thus investigated the pathophysiology of BML based on MRI and histology in the 4 consecutive patients diagnosed with SIF, whose onset was within 4 months. In all cases, BMLs were enhanced on T1 Gd-enhanced MRI. Histologically, BMLs comprised serous exudate, fibrous tissue, and vascular-rich granulation tissue in the marrow space. In addition, a lower signal intensity line was observed within the BML in all cases on T1 MRI. Histologically, this line showed thickened bone trabeculae accompanied by fibrovascular tissue in two cases, while the other two cases showed formation of woven bone trabeculae around the original fractured bone trabeculae indicating the presence of another fracture in the bone marrow space. In summary, BML in SIF was considered to be a secondary phenomenon resulting from a subchondral fracture.
Keywords: Subchondral insufficiency fracture, histopathological evaluation, spontaneous osteonecrosis of the knee, magnetic resonance imaging evaluation
Introduction
Spontaneous osteonecrosis of the knee was first described in 1968, and had originally been considered to be osteonecrosis resulting from ischemia [1]. However, a histologic study suggested that the primary event in spontaneous osteonecrosis of the knee was not ischemia, but a subchondral insufficiency fracture (SIF) [2]. This concept has been confirmed by further histological studies [3-7] as well as the magnetic resonance imaging (MRI) studies [8-13].
The characteristic MRI appearance of SIF is the presence of a fracture line showing low signal intensity on T1 MRI [14]. SIF has also been known to be associated with a bone marrow edema pattern on MRI [2-15], which has been recognized as a bone marrow lesion (BML) [14-16]. However, the detailed histopathology of the BML has not been fully clarified, since previous histologic studies have mainly focused on the fractured lesion in terms of the presence of necrosis and osteopenia based on various conditions, including spontaneous osteonecrosis, postmenisectomy osteonecrosis, and bone bruising [2-4,6,7,17,18].
In addition, within BMLs, the presence of another lower signal intensity line has been reported based on T1 MRI, and was speculated to represent a fracture line within the BML [14]. However, the pathophysiology of this lower signal intensity line was not histologically evaluated.
The purpose of this study was to evaluate the histopathology of the BML as well as the lower signal intensity line on T1 MRI using Gd-MRI and a bone biopsy.
Material and methods
Subjects
The present study was approved by the institutional review board of our institution (IRB ID: 2017M076), and informed consent was obtained from all participants. The study included four consecutive patients with SIF (one male and three females; mean age 67 years, range 54-74 years). All patients underwent both radiologic and histologic examinations in our institution between December 2017 and May 2018. The assessed clinical characteristics included sex, age at presentation, and duration between the onset of pain and surgery (Table 1).
Table 1.
Clinical characteristics of four consecutive patients with spontaneous osteonecrosis of the knee
| Case number | Sex, age (years) | Affected side | Duration between onset of pain and surgery (months) |
|---|---|---|---|
| 1 | F, 74 | R | 2 |
| 2 | F, 68 | R | 2 |
| 3 | F, 72 | L | 3 |
| 4 | M, 54 | L | 4 |
The case numbers were assigned in ascending order of the time between the onset of pain and surgery.
The diagnosis of SIF was made based on previously reported criteria [1], namely, older patients with acute onset of pain localized in the medial condyle of the knee, absence of antecedent trauma, no history of excessive corticosteroid administration or alcohol intake, presence of collapse in the medial femoral condyle on plain radiography, and a subchondral fracture line on MRI.
Surgical indication and procedure
Our indication for the surgical treatment (opening wedge high tibial osteotomy) for SIF included persistent pain over two months as well as the appearance of a collapse of the medial femoral condyle on radiographs.
We routinely performed arthroscopy before opening wedge high tibial osteotomy to assess the cartilage surface and meniscal tear, and to obtain a biopsy for decompression. After the arthroscopic procedure, a conventional opening wedge high tibial osteotomy was performed in all cases [19].
Radiological and histological assessment
Patients routinely underwent radiography comprising anteroposterior, lateral, and Rosenberg views, and standing lower limb radiographs. Anteroposterior radiographic findings were used to divide the cases into four categories in accordance with the Koshino classification [20]. The femorotibial angle was measured on standing lower limb radiographs as an indicator of lower limb alignment [21].
The duration from the onset of pain to MRI evaluation was assessed. Both conventional and Gd-enhanced MRI were performed using an Ingenia 1.5-Tesla system (Philips Medical Systems) in case 1, an Achieva 1.5-Tesla system (Philips Medical Systems) in cases 3 and 4, and a Discovery 3.0-Tesla system (GE Medical Systems) in case 2. After conventional MRI, Gd-enhanced MRI was performed by injecting gadobutrol (Gadavist; Bayer Healthcare Pharmaceuticals, Wayne, NJ) at a dose of 0.1 mmol/kg bodyweight. The MRI sequences used with the 1.5-Tesla and 3.0-Tesla systems were T1-weighted spin-echo images (TR range/TE ranges: 400-515/8.8-15 and 719-835/9.5-10, respectively) in coronal and sagittal phases, as well as in Gd-enhanced MRI. The slice thickness was 4.0 mm for both the coronal and sagittal images.
An osteochondral pillar biopsy (bone cylinder) was obtained from the affected BML at the time of surgery. Each specimen was long enough to include the BML. All specimens were fixed in 10% formalin solution and decalcified in 5% nitric acid solution. Specimens were embedded in paraffin, sectioned, and sections were stained with hematoxylin and eosin. The biopsy specimens were histologically examined by a pathologist with more than 30 years’ experience.
Results
Radiological findings
Radiologic data are shown in Table 2. All cases showed a subchondral collapse in the medial femoral condyle.
Table 2.
Radiological findings
| Case | Radiographic Stage | Duration until contrast MRI (months) | Conventional T1-weighted MRI | Gadolinium-enhanced T1-weighted MRI | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Low intensity area | Lower intensity line | Low intensity area | Lower intensity line | |||
| 1 | 2 | 2 | + | + | Enhanced | Not enhanced |
| 2 | 2 | 2 | + | + | Enhanced | Enhanced |
| 3 | 2 | 3 | + | + | Enhanced | Partly enhanced |
| 4 | 2 | 4 | + | + | Enhanced | Partly enhanced |
MRI findings
The average duration from the onset of pain to the MRI was 2.75 months. All cases showed a diffuse low signal intensity on T1 MRI and high intensity on T2 MRI in the medial femoral condyle. In addition, a lower signal intensity line was observed on T1 MRI within the BML in all cases (Figures 1, 3).
Figure 1.
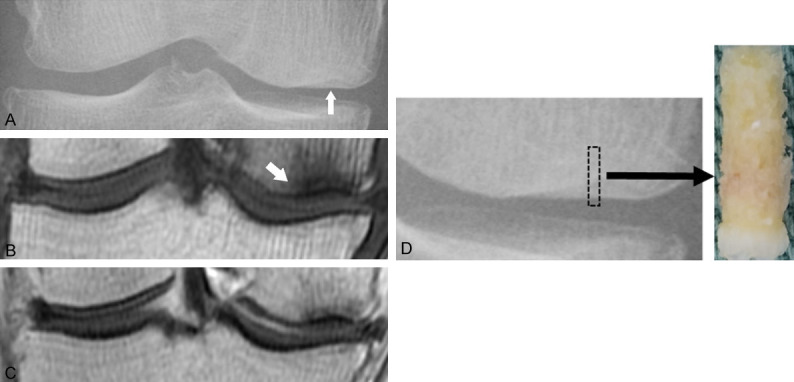
Images and histology of a 68-year-old female (case 2). A. Anteroposterior radiograph of the right knee shows flattening and slight sclerotic change (arrow) of the medial condyle. B. T1-weighted MRI coronal slice shows diffuse low intensity at the medial femoral condyle, with an associated lower intensity line at 5.0 mm from the articular surface (arrow). C. Gadolinium-enhanced T1-weighted MRI shows enhancement of the low intensity areas. D. An osteochondral pillar obtained from the affected area at the medial condyle. Biopsy diameter is 2.4 mm and depth is 13 mm.
Figure 3.
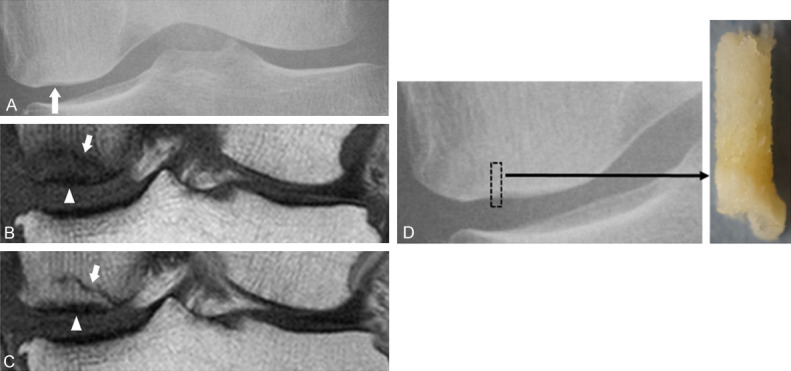
Images and histology of a 72-year-old female (case 3). A. Anteroposterior radiograph of the left knee shows flattening and slight sclerotic change (arrow) of the medial condyle. B. T1-weighted MRI shows diffuse low intensity at the medial femoral condyle, with an associated lower intensity line (arrow), and a lower intensity area around the articular cartilage (arrowhead). C. Gadolinium-DTPA-enhanced T1-weighted MRI. The low intensity area is enhanced, while the lower intensity line (arrow) is partly enhanced and the small area around the articular surface (arrowhead) is not enhanced. D. An osteochondral pillar obtained from the affected area at the medial condyle. Biopsy diameter is 2.4 mm and depth is 14 mm.
On Gd-enhanced MRI, BMLs were uniformly enhanced in all cases, but the small area around the subchondral fracture was not enhanced in cases 3 and 4 (Figure 3C). The lower signal intensity line was enhanced in one case, partly enhanced in two, and not enhanced in one (Table 2).
Histological findings
Histologic findings are shown in Table 3. All cases showed a fracture line associated with a fracture callus, reactive cartilage, and dense fibrous tissue in the subchondral area (Figures 2B, 4B). Fracture-related small foci of bone and bone marrow debris were observed in the focal area around the fracture (Figure 4B). The bone marrow space was filled by serous exudate, fibrous tissue, and vascular-rich granulation tissue, which corresponded to the BML on MRI.
Table 3.
Histological findings at the low intensity area and the lower intensity line on T1-weighted MRI
| Case | Low intensity area | Lower intensity line | |
|---|---|---|---|
|
| |||
| Subchondral area | Proximal bone marrow area | ||
| 1 | Fracture line associated with fracture callus and reactive cartilage | Serous exudate, fibrous tissue and vascular-rich granulation tissue | Thickened bone trabeculae surrounded by fibrovascular tissue |
| 2 | Fracture line associated with fracture callus and reactive cartilage | Serous exudate, fibrous tissue and vascular-rich granulation tissue | Thickened bone trabeculae surrounded by fibrovascular tissue |
| 3 | Fracture line associated with fracture callus, fracture-related bone debris | Serous exudate, fibrous tissue and vascular-rich granulation tissue | Formation of woven bone trabeculae |
| 4 | Fracture line associated with fracture callus, fracture-related bone debris | Serous exudate, fibrous tissue and vascular-rich granulation tissue | Formation of woven bone trabeculae |
Figure 2.
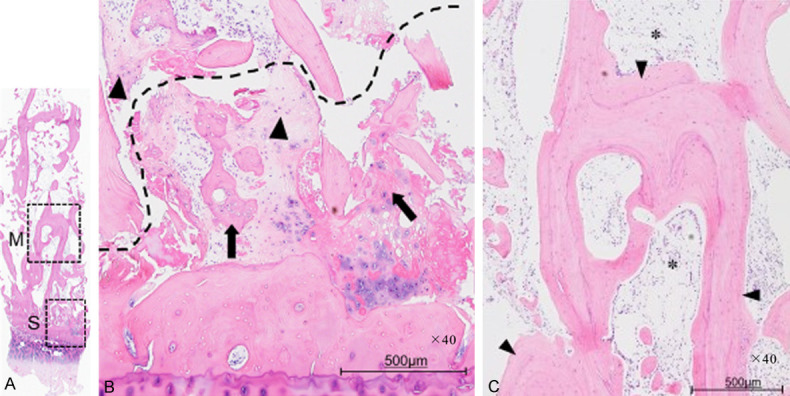
A. A LOUPE image of the whole specimen (hematoxylin and eosin, ×1.25 magnification). Area “S” corresponds to the low intensity area on T1-weighted MRI. Area “M” corresponds to the lower intensity line on T1-weighted MRI. B. Photomicrograph of area “S” (hematoxylin and eosin, ×40 magnification, articular cartilage at the bottom, and bone marrow at the top). There is a fracture line (broken line) associated with a fracture callus (arrow) and reactive cartilage (arrowheads). C. Photomicrograph of area “M” (hematoxylin and eosin, ×40 magnification, articular cartilage at the bottom, and bone marrow at the top). Several thickened trabecular bones (arrowheads) are observed, and fibrovascular tissue is observed in the marrow space (asterisk).
Figure 4.
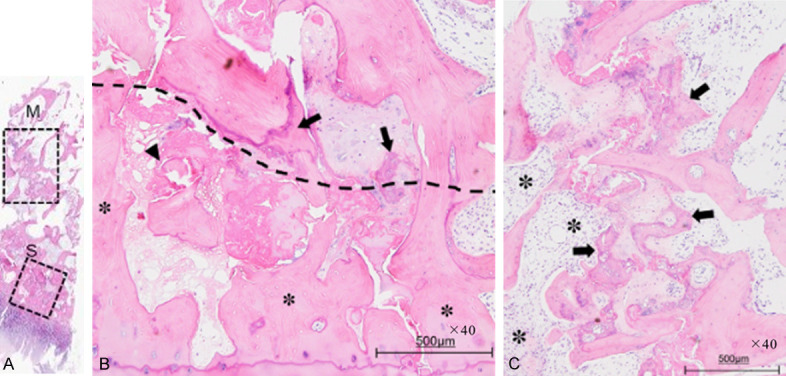
A. LOUPE image of the whole specimen (hematoxylin and eosin, ×1.25 magnification). Area “S” corresponds to the low intensity area on T1-weighted MRI. Area “M” corresponds to the lower intensity line on T1-weighted MRI. B. Photomicrograph of area “S” (hematoxylin and eosin, ×40 magnification). There is a fracture line (broken line) associated with a fracture callus (arrow) and bone marrow cell debris (arrowhead). Empty lacunae are observed distal to the fracture line (asterisk). C. Photomicrograph of area “M” (hematoxylin and eosin, ×40 magnification). Woven trabecular bone formation (arrow) is observed around the original fractured bone trabeculae at 5.0-7.0 mm from the articular cartilage. The bone marrow space is filled with fibrovascular tissue (asterisk).
The histology of the lower signal intensity line on T1 MRI indicated thickened bone trabeculae accompanied by fibrovascular tissue in the bone marrow space in two cases (Figure 2C), while the other two cases (cases 3 and 4) showed the formation of woven bone trabeculae around the original fractured bone trabeculae (Figure 4C).
Discussion
We investigated the pathophysiology of BMLs based on MRI and histology. Histologic examination of the BMLs showed edematous tissue associated with fibrosis and vascular tissue in the bone marrow. Such an edematous change in the marrow space is known to be caused by fracture [21]. Our findings indicate that the BML in SIF corresponded to bone marrow edema caused by a subchondral fracture.
A lower signal intensity line was recognized within the BML in all cases on T1 MRI. Histologically, two of four cases (cases 1, 2) showed thickened trabecular bone surrounded by fibrovascular tissues, indicating sclerotic changes in the process of halo formation. The mechanism of this phenomenon may be similar to that of sclerotic changes frequently seen in cyst formation in osteoarthritis [21,23]. In addition, the lower signal intensity line was enhanced on Gd-enhanced MRI in one case but not in the other three cases. This may be because of variations in the degree of osteosclerosis progression.
Two cases showed the formation of woven trabecular bone around the original fractured bone trabeculae, indicating the presence of another fracture in the marrow space. The presence of a subchondral fracture extending into the proximal bone marrow has been reported in a previous MRI study [10].
The present study also reconfirmed that SIF is the primary event in so-called ‘spontaneous osteonecrosis of the knee’. Several studies have described the outcome and natural history of spontaneous osteonecrosis of the knee. The outcome is affected by the size and width of the lesion, and small lesions heal under conservative treatment [24-27]. The healing mechanism of this disease is considered to result from reduced mechanical stress to the affected lesion without further collapse [19]. Our results showed that BMLs were viable, which may be useful information in the selection of SIF treatment strategy.
The present study has several limitations. First, the patient cohort was small. However, all four cases showed similar histopathologic features. Second, our histologic examination was performed using bone biopsies and thus the examined area in each case was relatively limited. However, both the affected BML and the lower signal intensity line were included in the biopsy specimens. Third, the mechanism of another fracture within the BML was not clarified. Further sequential imaging studies seem to be necessary.
In conclusion, BML observed in SIF comprised serous exudate, fibrous tissue, vascular-rich granulation tissue, thickened bone trabeculae, and formation of woven bone trabeculae around the fractured original bone trabeculae, suggesting that BML in SIF is a secondary phenomenon resulting from a subchondral fracture.
Acknowledgements
We thank Kelly Zammit, BVSc, from Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript.
Disclosure of conflict of interest
None.
References
- 1.Ahlbäck S, Bauer GC, Bohne WH. Spontaneous osteonecrosis of the knee. Arthritis Rheum. 1968;11:705–733. doi: 10.1002/art.1780110602. [DOI] [PubMed] [Google Scholar]
- 2.Yamamoto T, Bullough PG. Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J Bone Joint Surg Am. 2000;82:858–866. doi: 10.2106/00004623-200006000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Nakamura N, Horibe S, Nakamura S, Mitsuoka T. Subchondral microfracture of the knee without osteonecrosis after arthroscopic medial meniscectomy. Arthroscopy. 2002;18:538–541. doi: 10.1053/jars.2002.30058. [DOI] [PubMed] [Google Scholar]
- 4.Takeda M, Higuchi H, Kimura M, Kobayashi Y, Terauchi M, Takagishi K. Spontaneous osteonecrosis of the knee: histopathological differences between early and progressive cases. J Bone Joint Surg Br. 2008;90:324–329. doi: 10.1302/0301-620X.90B3.18629. [DOI] [PubMed] [Google Scholar]
- 5.Mears SC, McCarthy EF, Jones LC, Hungerford DS, Mont MA. Characterization and pathological characteristics of spontaneous osteonecrosis of the knee. Iowa Orthop J. 2009;29:38–42. [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka Y, Mima H, Yonetani Y, Shiozaki Y, Nakamura N, Horibe S. Histological evaluation of spontaneous osteonecrosis of the medial femoral condyle and short-term clinical results of osteochondral autografting: a case series. Knee. 2009;16:130–135. doi: 10.1016/j.knee.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Hatanaka H, Yamamoto T, Motomura G, Sonoda K, Iwamoto Y. Histopathologic findings of spontaneous osteonecrosis of the knee at an early stage: a case report. Skeletal Radiol. 2016;45:713–716. doi: 10.1007/s00256-016-2328-4. [DOI] [PubMed] [Google Scholar]
- 8.Roemer FW, Frobell R, Hunter DJ, Crema MD, Fischer W, Bohondorf K, Guermazi A. MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthr Cartil. 2009;17:1115–1131. doi: 10.1016/j.joca.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Kon E, Ronga M, Filardo G, Farr J, Madry H, Milano G, Andriolo L, Shabshin N. Bone marrow lesions and subchondral bone pathology of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:797–814. doi: 10.1007/s00167-016-4113-2. [DOI] [PubMed] [Google Scholar]
- 10.Gorbachova T, Melenevsky Y, Cohen M, Cerniglia BW. Osteochondral lesions of the knee: differentiating the most common entities at MRI. Radiographics. 2018;38:1478–1495. doi: 10.1148/rg.2018180044. [DOI] [PubMed] [Google Scholar]
- 11.Lee S, Saifuddin A. Magnetic resonance imaging of subchondral insufficiency fractures of the lower limb. Skeletal Radiol. 2019;48:1011–1021. doi: 10.1007/s00256-019-3160-4. [DOI] [PubMed] [Google Scholar]
- 12.Ramnath RR, Kattapuram SV. MR appearance of SONK-like subchondral abnormalities in the adult knee: SONK redefined. Skeletal Radiol. 2004;33:575–581. doi: 10.1007/s00256-004-0777-7. [DOI] [PubMed] [Google Scholar]
- 13.Kattapuram TM, Kattapuram SV. Spontaneous osteonecrosis of the knee. Eur J Radiol. 2008;67:42–48. doi: 10.1016/j.ejrad.2008.01.055. [DOI] [PubMed] [Google Scholar]
- 14.Bonadio MB, Filho AG, Helito CP, Stump XM, Demange MK. Bone marrow lesion: image, clinical presentation, and treatment. Magn Reson Insights. 2017;10:1–6. doi: 10.1177/1178623x17703382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lotke PA, Ecker ML. Osteonecrosis of the knee. J Bone Joint Surg Am. 1988;70:470–473. [PubMed] [Google Scholar]
- 16.Nairn LN, Subramaniam M, Ekhtiari S, Axelrod DE, Grant JA, Khan M. Safety and early results of subchondroplasty® for the treatment of bone marrow lesions in osteoarthritis: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-06294-w. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Higuchi H, Kobayashi Y, Kobayashi A, Hatayama K, Kimura M. Histologic analysis of postmeniscectomy osteonecrosis. Am J Orthop (Belle Mead NJ) 2013;42:220–222. [PubMed] [Google Scholar]
- 18.Rangger C, Kathrein A, Freund MC, Klestil T, Kreczy A. Bone bruise of the knee: histology and cryosections in 5 cases. Acta Orthop Scand. 1998;69:291–294. doi: 10.3109/17453679809000933. [DOI] [PubMed] [Google Scholar]
- 19.Takeuchi R, Aratake M, Bito H, Saito I, Kumagai K, Hayashi R, Sasaki Y, Akamatsu Y, Ishikawa H, Amakado E, Aota Y, Saito T. Clinical results and radiographical evaluation of opening wedge high tibial osteotomy for spontaneous osteonecrosis of the knee. Knee Surg Sports Traumatol Arthrosc. 2009;17:361–368. doi: 10.1007/s00167-008-0698-4. [DOI] [PubMed] [Google Scholar]
- 20.Koshino T. The treatment of spontaneous osteonecrosis of the knee by high tibial osteotomy with and without bone-grafting or drilling of the lesion. J Bone Joint Surg Am. 1982;64:47–58. [PubMed] [Google Scholar]
- 21.Odenbring S, Berggren AM, Peil L. Roentgenographic assessment of the hip-knee-ankle axis in medial gonarthrosis. A study of reproducibility. Clin Orthop Relat Res. 1993;289:195–196. [PubMed] [Google Scholar]
- 22.Pouders C, De Maeseneer M, Van Roy P, Gielen J, Goossens A, Shahabpour M. Prevalence and MRI-anatomic correlation of bone cysts in osteoarthritic knees. AJR Am J Roentgenol. 2008;190:17–21. doi: 10.2214/ajr.07.2098. [DOI] [PubMed] [Google Scholar]
- 23.Chen Y, Wang T, Guan M, Zhao W, Leung FKL, Pan H, Cao X, Guo XE, Lu WW. Bone turnover and articular cartilage differences localized to subchondral cysts in knees with advanced osteoarthritis. Osteoarthr Cartil. 2015;23:2174–2183. doi: 10.1016/j.joca.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 24.Lotke PA, Abend JA, Ecker ML. The treatment of osteonecrosis of the medial femoral condyle. Clin Orthop Relat Res. 1982;171:109–116. [PubMed] [Google Scholar]
- 25.Lecouvet FE, van de Berg BC, Maldague BE, Lebon CJ, Jamart J, Saleh M, Noël H, Malghem J. Early irreversible osteonecrosis versus transient lesions of the femoral condyles: prognostic value of subchondral bone and marrow changes on MR imaging. AJR Am J Roentgenol. 1998;170:71–77. doi: 10.2214/ajr.170.1.9423603. [DOI] [PubMed] [Google Scholar]
- 26.Yates PJ, Calder JD, Stranks GJ, Conn KS, Peppercorn D, Thomas NP. Early MRI diagnosis and non-surgical management of spontaneous osteonecrosis of the knee. Knee. 2007;14:112–116. doi: 10.1016/j.knee.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 27.Pareek A, Parkes CW, Bernard C, Camp CL, Saris DBF, Stuart MJ, Krych AJ. Spontaneous osteonecrosis/subchondral insufficiency fractures of the knee: high rates of conversion to surgical treatment and arthroplasty. J Bone Joint Surg Am. 2020;102:821–829. doi: 10.2106/JBJS.19.00381. [DOI] [PubMed] [Google Scholar]


