Abstract
With the growth of vertical integration among physician practices (i.e., hospital–physician integration), there have been many studies of its effects on health care treatments and spending. It is unknown if integration shapes provider configurations, especially against the backdrop of increasing employment of nurse practitioners (NPs) and physician assistants (PAs) across specialties. Using a longitudinal panel of 144,289 practices (2008–2015), we examined the association of vertical integration with NP and PA employment. We find positive associations between vertical integration and newly employing NPs and PAs within physician practices; however, the relationships differ by practice specialty type as well as timing of vertical integration. Supplementary analyses offer supporting evidence for coinciding enhancements to practice productivity, diversification, and provider task allocation. Our results suggest that vertical integration may promote interdisciplinary provider configurations, which has the potential to improve care delivery efficiency.
Keywords: vertical integration, health care consolidation, nurse practitioners, physician assistants, health care workforce
Introduction
The “doctor’s workshop” model of hospital–physician relationships has been on a long-running decline, but a variety of alternative arrangements, with varying degrees of economic and clinical success, have since surfaced (Burns & Muller, 2008; Robinson, 1998). On the far end of the spectrum, hospitals can simply bind the fortunes of physician practices to their own via direct ownership stakes. The 1990s witnessed a wave of this type of vertical integration (i.e., the purchasing of physician practices by hospitals/health systems), but it was quickly followed by extensive divestures (Ciliberto & Dranove, 2006; Kocher & Shani, 2011). However, vertical integration (i.e., hospital–physician integration) among physician practices is again on the rise (Capps et al., 2018; Kocher & Shani, 2011; Neprash et al., 2015; Nikpay et al., 2018; Richards et al., 2016), and this time may be different. Health care delivery and market dynamics have evolved, such as increased vertical integration across multiple health care sectors and practice specialties (Nikpay et al., 2018; Richards et al., 2016); thus, the current motivations for consolidating may be stronger and more long-lasting.
The justifications for vertical integration largely fall within two domains: efficiency-based or strategy-based arguments (Post et al., 2018). The former rests heavily on incomplete contracts and transaction cost considerations when trying to coordinate care and payments across multiple, distinct entities. The latter justification is concerned with negotiation leverage vis-à-vis insurers and other suppliers (e.g., medical device and inventory companies). A burgeoning empirical literature has, in turn, investigated integration behavior and a variety of subsequent outcomes.
Existing studies find vertical integration leads to strategic changes in physician referral patterns and care delivery settings (Baker et al., 2016; Carlin et al., 2016; Koch et al., 2017) as well as increases in health care prices, spending, and treatment intensity (Capps et al., 2018; Koch et al., 2017; Konetzka et al., 2018; Neprash et al., 2015; Post et al., 2018; Robinson & Miller, 2014).1 But there is scant evidence for efficiency gains or improved care quality following these formal tie-ups (Burns et al., 2013; Carlin et al., 2015; Scott et al., 2017). Other downstream implications from vertical integration are largely unexplored, however—with the adoption and use of health information technology being one exception (Everson et al., 2019; Lammers, 2013; McCullough & Snir, 2010).
One unstudied area of health care delivery and policy importance is the structure and performance of physician practices postintegration. There is longstanding interest in differences in productivity and allocative efficiency across various physician practice configurations. Much of the literature has specifically focused on the influences of practice size and specialty mix—economies of scale and scope, respectively (Burns et al., 2013; DeFelice & Bradford, 1997; Gaynor & Pauly, 1990). However, some prominent, though often dated, work has also explored the implications of physician and nonphysician input combinations on practices’ throughput and earnings. It is well-known that other high-skilled clinicians, such as nurse practitioners (NP) and physician assistants (PA), can substitute or complement physician labor within certain settings and/or specific service lines (Maier et al., 2016); yet, related research tends to find suboptimal use of these alternative input factors (Golladay et al., 1973; Reinhardt, 1972; Zeckhauser & Eliastam, 1974).
There is little empirical knowledge of how organizational structures shape physician practice composition. For example, Kaissi et al. (2003) show that group practice increases the likelihood of PA and NP employment, but this is a cross-sectional analysis of a small geographic area and dated by many years. Park and colleagues (Park et al., 2018) document greater use of NP and PA providers when community health centers transition to “medical home” models; however, this (safety-net) practice type and highly specific organizational evolution are uncommon within the broader market. Consequently, there is a nontrivial gap in the literature, with growing salience due to the known uptick in NP and PA provider reliance in recent years (Barnes et al., 2018; Martsolf et al., 2018) as well as the greater acceptance of NP- and PA-delivered care by consumers (Dill et al., 2013).
New Contributions
To shed needed light in this research area, we examine the association of physician practice vertical integration with NP and PA employment. We leverage a balanced panel of 144,289 physician practices (i.e., exact same practices across all years) spanning 2008–2015. The data offer granular detail on ownership structure, and crucially, the complete staffing picture for all NPs, PAs, and physicians working within a given practice. We employ practice-level regression analyses with two-way fixed effects to capture changes in NP and PA employment after a physician practice is newly integrated with a hospital or health system. In addition, we conduct event studies to assess the dynamics of the associations over time. Using extensive practice provider data and more rigorous analytic approaches, this study extends the available research and is the first to capture the relationship between changes in physician practice ownership structure and provider configuration over time, as well as across practice types (i.e., primary care, nonprimary care, and multispecialty practices).
Conceptual Basis for the Study
The reasons behind any underutilization of nonphysician clinical personnel are potentially manifold and not mutually exclusive (Reinhardt, 1972). For example, physicians may underestimate the productivity and financial gains from employing the additional staff, or relatedly, not appreciate how costly it is for them to perform some tasks that could be safely (and less expensively) allocated to other clinical professionals. More simply, physicians may have an aversion to assuming the role of a practice manager. Managerial skill takes development, and it is generally not emphasized within medical education.
Importantly, vertically integrating with a hospital or health system could overcome one or more of the barriers to greater NP and PA use. Vertical integration allows health systems to share (or impose) management strategies with the newly acquired physician practice. While profit sharing with physicians is common, health systems are ultimately the residual claimant on the practice’s earned income—i.e., the proverbial “buck stops there.” Thus, the locus of managerial control shifts (at least to some degree) to the larger entity that has now enveloped the physician practice. The health system can then exploit any opportunities to enhance productivity and/or profits by altering the labor composition within the practice, and relatedly, by improving task matching across provider types. Moreover, the presence of an overarching firm likely limits growth in physicians’ managerial responsibilities and subsumes the practice within the health system’s existing “brand.” These features can mitigate any inherent physician reticence toward employing more advanced practice clinical labor.
Method
Data
We benefit from a panel of physician practices over the 2008–2015 time period. The data are from SK&A (IQVIA, 2020), which aims to be a near-universe (i.e., census) of physician office-based practices across the United States. Practices are located in all 50 states plus the District of Columbia. SK&A does not sample practices in a manner that ensures national representativeness; however, what is the most salient and unique about the SK&A data, and that allows for our panel estimation, is the ability to follow the same practices over time (2008–2015) and observe within practice changes in ownership status and provider configurations (i.e., employment of NPs and PAs). Additionally, the data include rich practice-level detail, including specialty designations as well as ownership structure. The latter element in combination with our relatively long time series allows us to capture extensive integration behavior over time. Specifically, we consider a practice as vertically integrated when it reports ownership by a hospital or health system (i.e., hospital–physician integration) in a given year. The SK&A data have been the key source of integration information for recent studies in this area (e.g., Baker et al., 2016; Everson et al., 2019; Koch et al., 2017; Nikpay et al., 2018; Richards et al., 2016). These data have been found to be comprehensive and representative of greater than 90% of ambulatory practices in the United States (Rhodes et al., 2014). We ultimately rely on a balanced panel of physician practices over this 8-year analytic window, which translates to 144,289 individual practices that span the country as well as the gamut of practice size and specialty types.
A highly relevant and unique feature of our data is the ability to account for the number of providers working within a given practice across three separate provider domains: NP, PA, and physician. As previously stated, these are all high-skill clinical providers (i.e., graduate-level training), with high degrees of substitutability across a variety of patient care services. Many studies of physician practices (e.g., those focused on size differences and trends) typically do not include NP or PA inputs—making any inferences at least partially confounded by unobserved dimensions of the overall practice configuration. Our data avoid this shortcoming, and instead, let us observe evolutions in high-skilled labor composition within physician practices.
Of note, during the extensive health care integration literature review by Post et al. (2018), the authors remark that existing insights are somewhat incomplete due to many current studies’ heavy focus on the hospital sector (rather than other market participants) and/or reliance on data from just one or few states. We are fortunately not restrained by either limitation in our empirical setting.
Descriptive Motivation
The amount of vertical integration activity we observe in our analytic sample can be seen in Figure 1. Across all three specialty designations (i.e., primary care, nonprimary care, and multispecialty), health system ownership is largely flat from 2008 to 2010 but then accelerates in subsequent years. By 2015, the prevalence of vertical integration is 100% to 200% higher for each specialty group when compared with our baseline year (2008). The patterns also align with other studies using similar data (Nikpay et al., 2018; Richards et al., 2016).2
Figure 1.
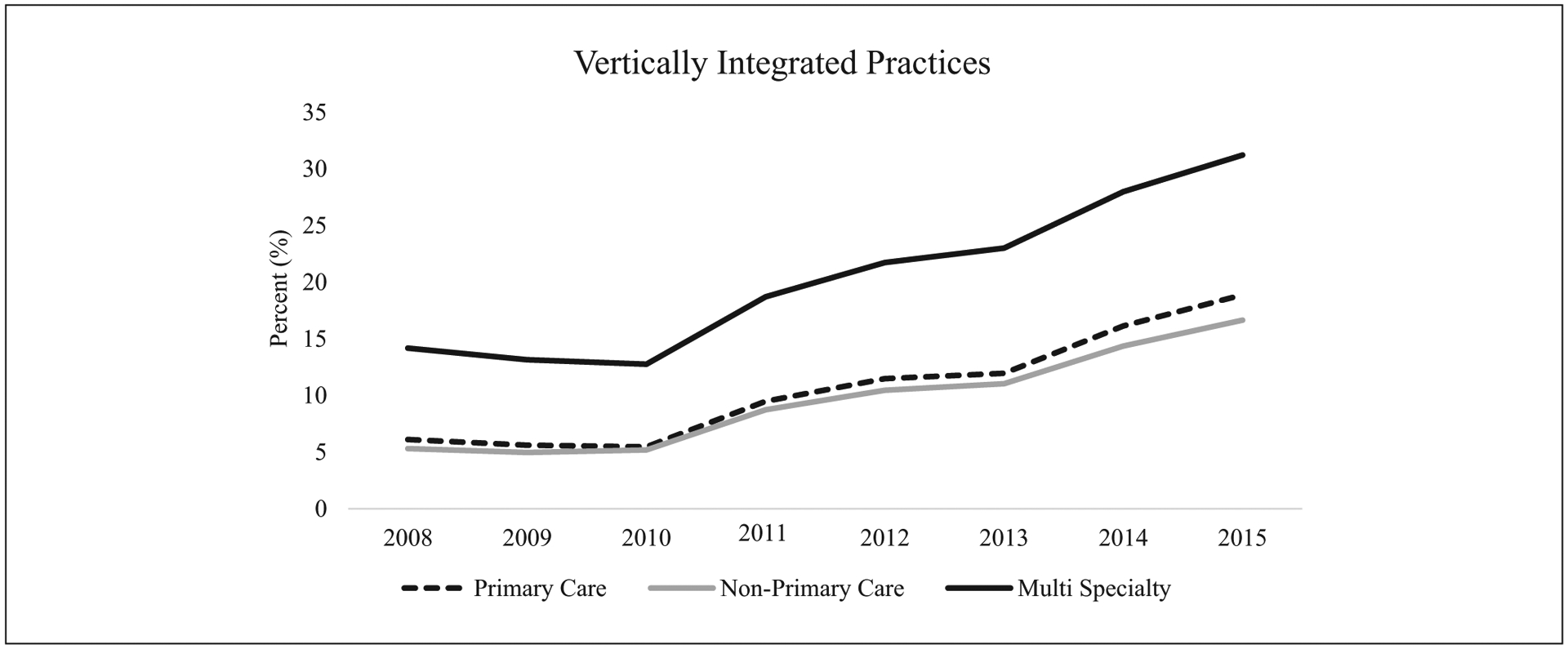
Trends in physician practice vertical integration 2008–2015.
Note. Balanced panel of 144,289 practices across eight years. Primary care = 50,635 practices. “Vertical” practices report hospital/health system ownership (i.e., hospital–physician integration). Nonprimary care = 76,773 practices. Multispecialty = 16,881 practices. Practice specialty designated by SK&A reported practice specialty in the baseline year (2008). Primary care includes family practice, general practice, geriatric medicine, internal medicine, and pediatrics. Nonprimary care includes single medical and surgical specialty fields.
Figure 2 offers an annual snapshot of NP and PA employment prevalence for our analytic sample that has been stratified by practice ownership type (i.e., independent, horizontal, and vertical). Using common, standard definitions, independent practices are defined as a physician-owned practices, and horizontally integrated practices are those reporting physician group ownership (Burns et al., 2013). It is clear from Figure 2 that independently owned practices are the least likely to incorporate high-skill, NP or PA labor. Only 10% to 15% of independent practices employ NP or PA providers in any given year. Vertically integrated practices are the most likely to rely on NPs as part of their clinical staffing, however, with roughly one third of these practices having at least one NP within the practice over our study period. Interestingly, vertically integrated practices do not have a similarly disproportionate tilt toward PA labor (bottom panel of Figure 2). Only about 20% of vertically integrated practices staff a PA in a given year, which is higher than independent practices but typically below that of horizontally integrated (i.e., physician group ownership) practices. Figure 2 therefore displays some prima facie evidence suggesting relatively stronger NP labor demand within these vertically structured firms.3
Figure 2.
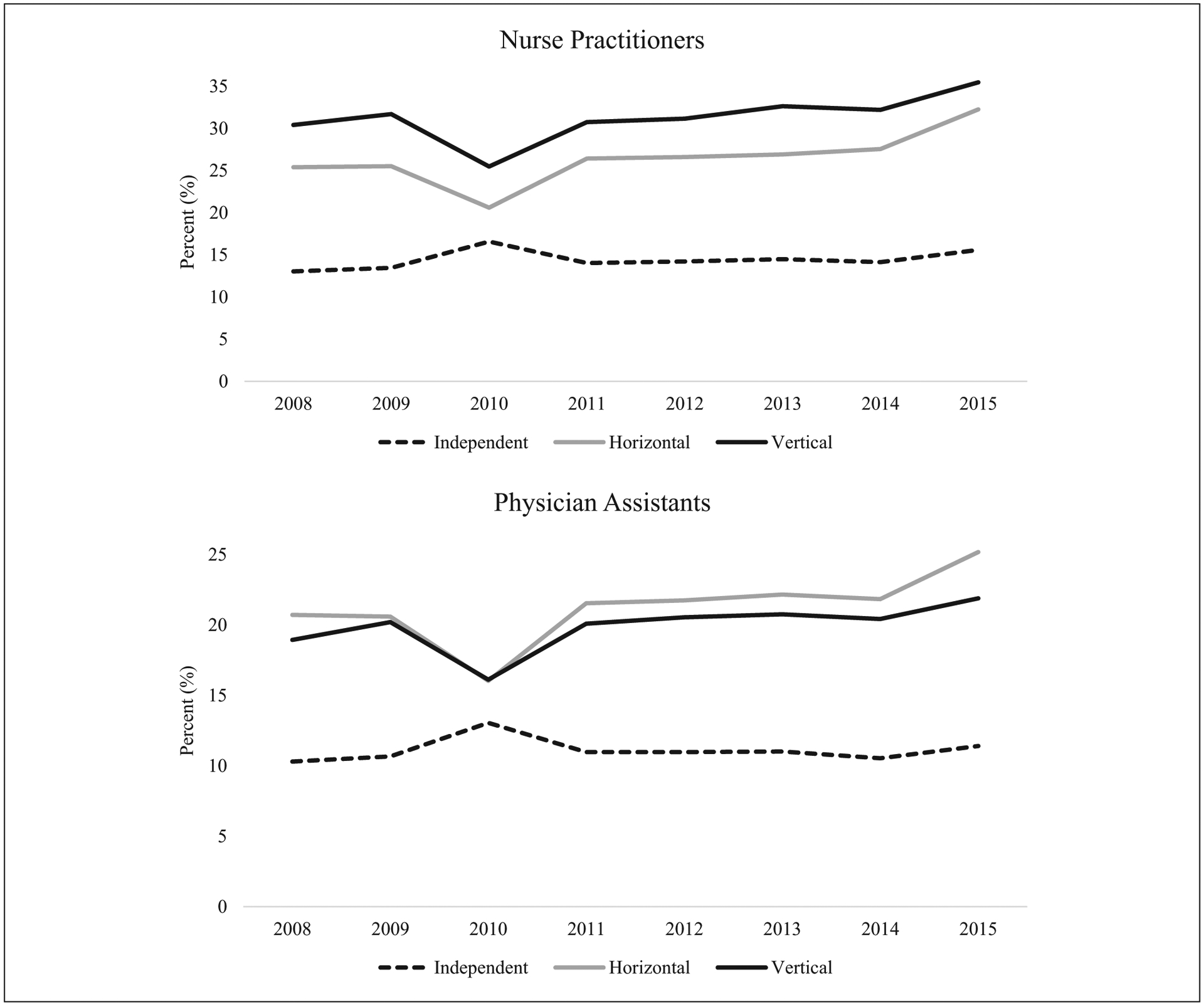
The percentage of physician practices that employ nurse practitioners and physician assistants by ownership type: 2008–2015.
Note. Balanced panel of 144,289 practices across 8 years. “Vertical” practices report hospital/health system ownership (i.e., hospital–physician integration), while “Horizontal” practices report physician group ownership.
Regression Analyses
Using a linear probability model, our simplest specification is akin to a generalized difference-in-differences model with two-way fixed effects, which we then complement with an event study model. The unit of observation is at the practice (p)-year (t) level.
| (1) |
Our outcomes of interest (Y) in Equation 1 are two separate binary indicators for the presence of an NP (PA) in the physician practice.4 Vertical is a time-varying indicator for whether a given practice is owned by a health system in a given year. We also have practice (λ) and year (η) fixed effects—making the delta coefficient our focal parameter that informs the existence and strength of any association between vertical integration activity and practice staffing decisions. We additionally incorporate a set of time-varying practice-level characteristics (X). These covariates include the number of physicians within the practice, a policy indicator for full NP practice authority at the state-level and county-level demographic information (annual population estimates, rural location, percentage of non-White population, percentage of adults older than 65 years, percentage of uninsured, percentage of living in poverty, and unemployment rate). For full NP practice authority, we created a time-varying dummy variable based on state requirements that NPs maintain collaborative agreements with physicians to practice and/or prescribe medication. Following the method used by Kuo et al. (2013) and including data from Phillips (2014, 2015, 2016), we considered a state as having full NP practice authority if no collaborative agreements were required and a state as having restricted practice if any collaborative agreements were required (Supplemental Appendix Table A2, available online). County-level demographics were obtained from the Area Health Resource File. We also estimate Equation 1 with and without these covariates as a sensitivity check. Standard errors were clustered at the practice level.
Following full sample estimation, we reapply the analytic specification to three separate specialty group classifications: primary care (family practice, general practice, geriatric medicine, internal medicine, and pediatrics), nonprimary care (single medical and surgical specialties), and multispecialty practices. Stratifying by specialty type is motivated by several empirical facts. First, other work has documented meaningful differences in the prevalence of vertically integrated practices across physician specialties (Nikpay et al., 2018), and we observe absolute and relative differences within our analytic data as well (Figure 3). Previous research also finds primary care practices to disproportionately rely on NP and PA labor (Kaissi et al., 2003). The descriptive data in Figure 3 largely conform to this pattern. Cross-sectionally, and among vertically integrated practices, NP and PA utilization favors primary care over nonprimary care settings in nearly all years. Additionally, it is clear from Figure 3 that vertically integrated multispecialty practices are the most likely to employ NPs and PAs in any given year. Approximately 40% of these practices rely on NP labor and about 30% of them rely on PA labor; these prevalence rates are also fairly stable over the 2008–2015 period. However, the association between changes in integration status and changes in provider configurations can diverge from these cross-sectional patterns, which further motivates our subsequent analyses that isolate specific practice specialty types.5
Figure 3.
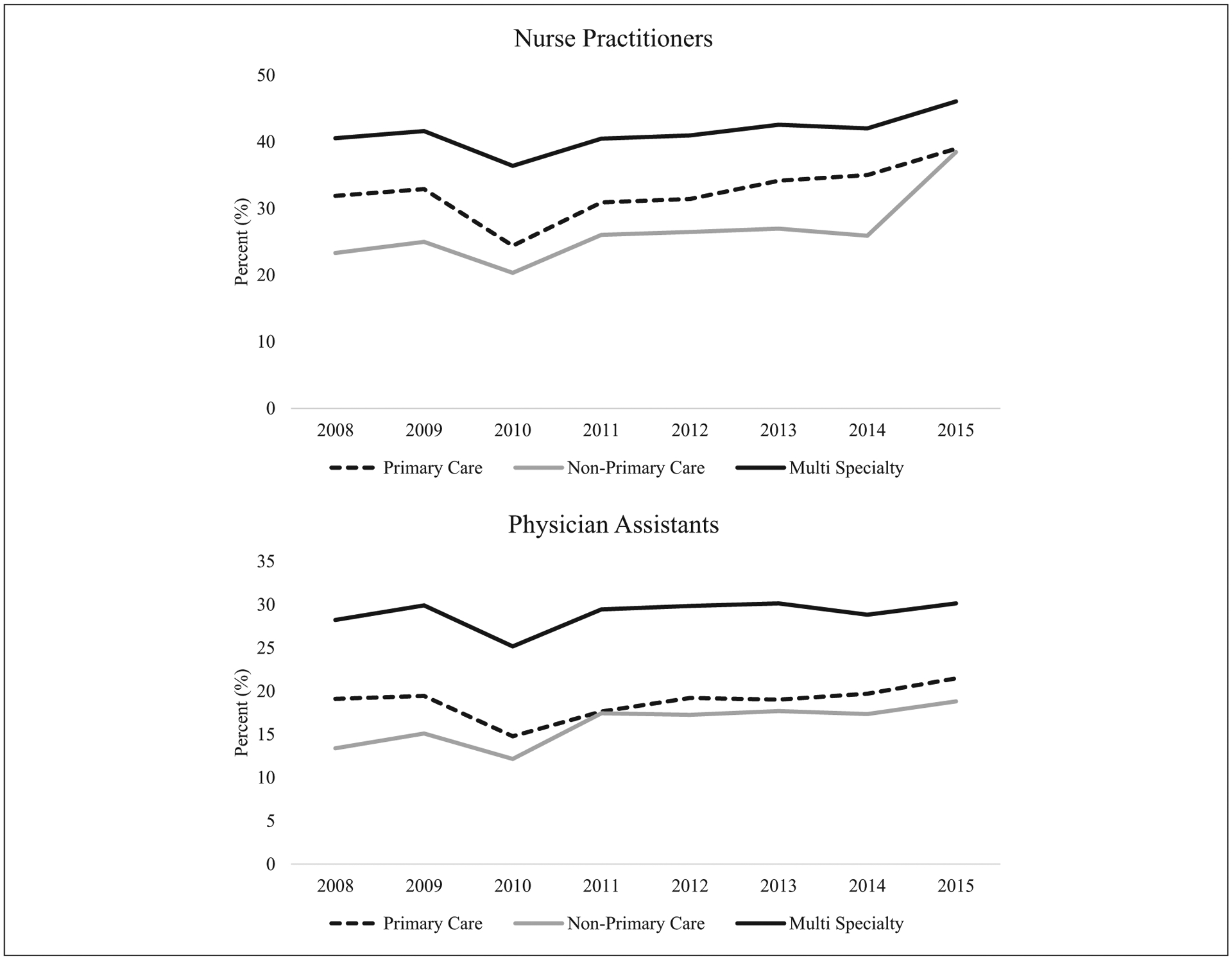
The percentage of vertically integrated physician practices that employ nurse practitioners and physician assistants by practice specialty type: 2008–2015.
Note. Data are from SK&A and restricted to vertically integrated practices within a given year (i.e., those that report hospital/health system ownership in that year).
To further assess the strength of and dynamics in any associations and related interpretations from Equation 1, we apply an event study regression model to our longitudinal data. The specification subsequently takes the form:
| (2) |
Equation 2 generates a set of differential parameters (β) for specific individual years: three or more years prior to vertically integrating (t − 3+), two years prior to vertically integrating (t − 2), the year of integration (t + 0), 1 year following vertical integration (t + 1), 2 years following vertical integration (t + 2), and 3 or more years following vertical integration (t + 3+). The reference category omitted from the event study is 1 year prior to vertically integrating (t − 1). As argued within Capps et al. (2018) and Baker et al. (2016), exploiting the granular nature of the panel data around the observed timing of integration helps support clearer and more compelling interpretations of the downstream consequences of hospital–physician vertical integration. That said, a given practice’s contribution to the set of beta coefficients is determined by the timing of its vertical integration event belonging to the practice. For example, practices integrating in 2010, will not contribute to the −3+ event dummy just as practices integrating in 2014 will not contribute to the 3+ dummy since the corresponding years are outside our analytic data range (2008–2015).
Results
Main Findings for Vertical Integration Association
Table 1 reports the simpler two-way fixed effects estimates across all physician practice types using a linear probability model. Nineteen percentage of these practices employ at least one NP over our analytic period, while 14% employ at least one PA. There is a precisely estimated 1.2 percentage point increase in the likelihood of staffing NPs following vertical integration. Relative to the sample mean, this is a 6% increase when the practice is newly under health system ownership, and the association is unaffected by the inclusion of time-varying covariates (column 2). Conversely, there is no obvious relationship between vertical integration and the use of PA clinicians across all practice types. The point estimate in columns 3 and 4 is small (1% to 2% of the sample mean) and lacks precision.6
Table 1.
Association of a Change in Vertical Integration Status on Advanced Practice Provider Employment Using a Linear Probability Model: 2008–2015.
| Pr(Employ NP) | Pr(Employ PA) | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Vertical | 0.012*** (0.002) | 0.012*** (0.002) | 0.003 (0.001) | 0.002 (0.001) |
| Year FEs | Yes | Yes | Yes | Yes |
| Practice FEs | Yes | Yes | Yes | Yes |
| Covariates | No | Yes | No | Yes |
| Observations | 1,154,312 | 1,154,292 | 1,154,312 | 1,154,292 |
| Unique practices | 144,289 | 144,289 | 144,289 | 144,289 |
| Sample mean | 0.19 | 0.19 | 0.14 | 0.14 |
Note. Data are from SK&A and include 144,289 practices present for all 8 years. “Vertical” practices report hospital/health system ownership (i.e., hospital–physician integration). Outcomes are binary indicators for employing at least one of the specified advanced practice provider (i.e., NP and PA). Covariates include the following: number of physicians in the practice, a dummy for full independence for NP scope of practice, and county-level demographics. Standard errors clustered at the practice level. NP = nurse practitioner; PA = physician assistant; FEs = fixed effects.
p < .05.
p < .01.
p < .001.
Table 2 introduces heterogeneity in NP staffing changes across our three practice specialty groupings and provides the corresponding results from our event study models for this employment outcome. The two-way fixed effect estimates in columns 1 and 3 imply a 1.3 percentage point positive correlation between the probability of utilizing NPs and newly integrating with a hospital/health system for both primary care and nonprimary care practices, respectively (6% and 9% increases relative to their analytic sample means). The event study models in column 2 (primary care) and column 4 (nonprimary care) show marked differences in the dynamics of these employment behavior changes, however. For primary care, a statistically significant, positive association does not materialize until at least 3 years postintegration, which is necessarily driven by practices integrating earlier in our study period. Among nonprimary care practices, a statistically significant and positive association materializes in the first year of vertical integration (t + 0), with the magnitude increasing over time. However, both practice specialty types show a below average likelihood in employing any NPs 3 or more years prior to integration. This preperiod differential adds some caution to the interpretations from the simpler two-way fixed effects models, but it also could reflect a “catching up” phenomenon whereby new hospital/health system ownership allows these practices to overcome some previous staffing gaps when compared with their practice peers. As our results in Figure 3 show, primary care and nonprimary care practices are the least likely to employ NPs or PAs among these three practice classifications. Our dynamic findings could therefore be evidence of already-evolving provider configurations; a process that, along with new organizational goals for clinical practice and productivity, vertical integration may be a part of. Additionally, the negative and statistically significant coefficient for the 3 or more years prior to integration could alternatively reflect that when it comes to baseline staffing makeup and postintegration staffing decisions, practices acquired “late” in our sample period are different than those acquired “early” since the latter does not contribute to that particular time dummy coefficient. Columns 5 and 6 in Table 2 show no differential behavior before or after vertical integration among multispecialty practices.
Table 2.
Association of a Change in Vertical Integration Status on Nurse Practitioner (NP) Employment by Practice Specialty Type Using Linear Probability Models and Event Studies: 2008–2015.
| Primary care | Nonprimary care | Multispecialty | ||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Vertical | 0.013** (0.003) | — | 0.013*** (0.002) | — | 0.0003 (0.004) | — |
| Vertical (t – 3+) | −0.011** (0.004) | −0.013*** (0.003) | −0.010 (0.006) | |||
| Vertical (t – 2) | — | −0.005 (0.003) | — | −0.004 (0.002) | — | −0.004 (0.004) |
| Vertical (t + 0) | — | 0.004 (0.003) | — | 0.005* (0.002) | — | 0.001 (0.005) |
| Vertical (t + 1) | — | 0.007 (0.004) | — | 0.012*** (0.003) | — | 0.001 (0.006) |
| Vertical (t + 2) | — | 0.008 (0.005) | — | 0.009* (0.004) | — | −0.007 (0.007) |
| Vertical (t + 3+) | — | 0.027*** (0.006) | — | 0.021*** (0.005) | — | −0.005 (0.009) |
| Year FEs | Yes | Yes | Yes | Yes | Yes | Yes |
| Practice FEs | Yes | Yes | Yes | Yes | Yes | Yes |
| Covariates | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 405,060 | 405,060 | 614,184 | 614,176 | 135,048 | 135,048 |
| Unique practices | 50,635 | 50,635 | 76,773 | 76,772 | 16,881 | 16,881 |
| Sample mean | 0.22 | 0.22 | 0.14 | 0.14 | 0.31 | 031 |
Note. Data are from SK&A and include practices present for all eight years. “Vertical” practices report hospital/health system ownership (i.e., hospital–physician integration). Outcome is binary indicator for employing at least one NP. Event study reference category is the year prior to vertical integration (i.e., t − 1). Covariates include the following: number of physicians in the practice, a dummy for full independence for NP scope of practice, and county-level demographics. Standard errors clustered at the practice level. FEs = fixed effects.
p < .05.
p < .01.
p < .001.
Table 3 shows the results of the event study for the outcome of PA employment. Compared with NP employment, only the coefficient for nonprimary care practices is statistically significant (column 3, Table 3), and the relative change is 4% when compared with the analytic sample’s mean. In the event study for nonprimary care practices (column 4, Table 3), the coefficients for the time periods leading up to vertical integration (t − 3+, t − 2) are negatively signed, and nonsignificant. In the year the practice is vertically integrated (t + 0), the coefficient is positive, but remains nonsignificant. It is not until the following year (t + 1) that there is a statistically significant increase in the likelihood of employing PAs, which then grows in subsequent years (t + 2 and t + 3+). In the final time period, there is a 1.3 percentage point increase in the likelihood that a nonprimary care practice employs a PA (11% increase relative to the sample mean). Among multispecialty practices, the two-way fixed effects and event study coefficients show no relationship between being taken over by a health system and the propensity to use PA labor within the practice (columns 5 and 6 in Table 3). Despite vertically integrated multispecialty practices relying on NPs and PAs more than any other practice type (see Figure 3), the organizational change itself does not appear to induce an altered high-skill provider configuration—suggesting that multispecialty practices may already have a strong bent toward a mix of provider types, irrespective of financial ownership structure.
Table 3.
Association of a Change in Vertical Integration Status on Physician Assistant (PA) Employment by Practice Specialty Type Using Linear Probability Models and Event Studies: 2008–2015.
| Primary care | Nonprimary care | Multispecialty | ||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Vertical | 0.001 (0.003) | — | 0.005** (0.002) | — | −0.007 (0.004) | — |
| Vertical (t – 3+) | −0.004 (0.003) | −0.004 (0.003) | 0.005 (0.005) | |||
| Vertical (t – 2) | — | −0.002 (0.002) | — | −0.002 (0.002) | — | −0.001 (0.004) |
| Vertical (t + 0) | — | −0.003 (0.002) | — | 0.003 (0.002) | — | −0.0004 (0.0039) |
| Vertical (t + 1) | — | −0.002 (0.003) | — | 0.007** (0.003) | — | −0.003 (0.005) |
| Vertical (t + 2) | — | −0.004 (0.004) | — | 0.008* (0.003) | — | 0.001 (0.006) |
| Vertical (t + 3+) | — | 0.010 (0.005) | — | 0.13** (0.004) | — | 0.004 (0.007) |
| Year FEs | Yes | Yes | Yes | Yes | Yes | Yes |
| Practice FEs | Yes | Yes | Yes | Yes | Yes | Yes |
| Covariates | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 405,060 | 405,060 | 614,184 | 614,176 | 135,048 | 135,048 |
| Unique practices | 50,635 | 50,635 | 76,773 | 76,772 | 16,881 | 16,881 |
| Sample mean | 0.14 | 0.14 | 0.12 | 0.12 | 0.26 | 0.26 |
Note. Data are from SK&A and include practices present for all 8 years. “Vertical” practices report hospital/health system ownership (i.e., hospital–physician integration). Outcome is binary indicator for employing at least one PA. Event study reference category is the year prior to vertical integration (i.e., t − 1). Covariates include the following: number of physicians in the practice, a dummy for full independence for nurse practitioner scope of practice, and county-level demographics. Standard errors clustered at the practice level. FEs = fixed effects.
p < .05.
p < .01.
p < .001.
Supplementary Analyses
To add context to and complement our main results, we explore some potential motivations that may underlie the propensity toward greater NP and PA staffing following vertical integration.
Additional Outcomes From Primary Data Source.
We first reestimate Equation 1 for two complementary outcomes from the SK&A data: practice daily patient volume and multispecialty practice status. We do so separately for our primary care and nonprimary care practices. Supplemental Appendix Table A4 (available online) contains a description of the patient volume measure and corresponding results.
Columns 1 and 2 show a positive association between integration and daily practice volume for both specialization types. Vertical integration correlates with a 4-patient-per-day increase among primary care practices (10% relative increase) and with a 2.5-patient-per-day increase among nonprimary care practices (6% relative increase). Assuming the typical practice is open 5 days per week and 50 weeks per year, the annual increase in patient visits postintegration translates to 1,000 and 625 for primary care and nonprimary care single-specialty practices, respectively. The findings in column 1 and 2 therefore suggest that health system acquisition is associated with greater throughput (in terms of patients seen) for a given practice. The coefficients in columns 3 and 4 further imply that vertical integration is strongly associated with an increased probability of transforming into a multispecialty practice postintegration. The increase is 2.9 percentage points for primary care practices and 2.4 percentage points for nonprimary care practices. Given that only 4% to 5% of primary care and nonprimary care practices make a multispecialty practice transition over our entire study period, the relative increases associated with being vertically integrated are a striking 50% to 60%. As previously seen in Figure 3, multispecialty practices owned by a hospital/health system are highly likely to rely on NPs and PAs during our study period. Thus, the move to diversify the revenue stream and/or benefit from economies of scope may co-occur with the introduction of one or more of these clinicians within a practice—especially among nonprimary care single-specialty practices at baseline.
Procedure Output Changes From Secondary Data Source.
To introduce additional supporting evidence, we combine our vertical integration information from SK&A with physician-level procedure output from the state of Florida. The Florida data are from the Agency for Health Care Administration, which capture the universe of quarterly discharge records from inpatient providers and outpatient (ambulatory procedure) providers over time. Importantly, each discharge record has individual provider identification information for the clinician primarily responsible for the patient’s procedure performed during a given episode of care. Specifically, we use the physician National Provider Identification numbers to link the two data sets. The full data description and corresponding results are presented in the appendix (available online).
Specifically, Supplemental Appendix Table A5 (available online) shows that vertical integration is positively correlated with total procedure output at the physician level. On average, a physician produces 18 more procedures per year after the ownership change, which is a 7% increase relative to the analytic sample mean. Yet the greater number of procedures appears to come almost entirely from outpatient (ambulatory) procedures (column 1, Supplemental Appendix Table A5, available online). Vertical integration is associated with more than 15 additional ambulatory procedures per year or an 8% increase relative to the sample mean. The absolute and relative impact on inpatient procedure activity is much smaller and not precisely estimated (column 2, Supplemental Appendix Table A5, available online). Given that ambulatory procedures are more likely to be elective and tend to be highly profitable, it is unsurprising that output changes seem to localize to this delivery setting. Coupled with the supplementary results in Appendix Table A4 (available online), the associations in Appendix Table A5 (available online) are at least consistent with vertical integration leading to greater attention paid to physician productivity and efficient clinical labor allocations (e.g., shifting more nonprocedural care duties to NPs and PAs) after the health system purchases the physician practice.
Discussion
It is common to characterize hospital and health systems’ purchases of physician practices as an aggregation exercise where solo and small groups are combined into a larger entity owned by the overarching system (Burns & Muller, 2008). However, this process can also affect how clinical labor is configured within the practice, and subsequently, how various tasks are allocated to different provider types. Benefiting from a balanced panel of physician practices with detailed information on practice labor composition and ownership structure, we find that vertical integration is associated with an increased likelihood of employing high-skill provider labor within a practice. The positive correlations with NP and PA clinician staffing appear largely confined to the extensive margin (i.e., having any NP or PAs present in the practice), though there are observed differences across practice specialties as well as vertical integration timing.
Our supplementary analyses offer support for productivity changes, economies of scope, and allocative efficiency interpretations for the potential motivations for employing NPs and PAs after being vertically integrated. Interestingly, while multispecialty physician practices show no change in provider blending after being acquired by a health system, single-specialty practices are much more likely (50%−60%) to be transformed into multispecialty practices postintegration. Thus, expanding the remit of the practice may be a key driver for the observed greater NP and PA reliance—given that nearly half and about a third of vertically integrated multispecialty practices employ NPs and PAs, respectively (see Figure 3).
Returning to the possible explanations for any underutilization of nonphysician high-skilled labor (Reinhardt, 1972), our findings are more consistent with the first two propositions (i.e., underappreciation of potential productivity gains and/or mispricing of physicians’ own time). Our results suggest that health systems may be able to correct these issues after purchasing a practice (perhaps by importing their own managers and/or management styles). Relatedly, when reviewing the literature, Burns et al. (2013) argue that production functions and efficiency opportunities likely vary across practice specialty types—making managerial skills perhaps more important for optimal performance than achieving some presupposed ideal size. Our data seem to favor the authors’ conjecture. The responses among nonprimary care practices is also inconsistent with a fear of eventual physician skill erosion and/or substandard care delivery. NPs and PAs are unlikely to substitute for these physicians’ procedural tasks, and our complementary data (Supplemental Appendix Table A5, available online) indicates that physicians are perhaps devoting more time to performing procedures postacquisition, rather than less. A more plausible scenario is that the introduction of advanced practice provider labor is helping free up physician time as the NP or PA take on more of the outpatient clinic management roles (e.g., preprocedure visits and postprocedure follow-up care)—an industry-wide trend that has been noted elsewhere (Karash, 2018). Additionally, McCullough and Snir (2010) find greater investments in provider monitoring health IT after hospitals purchase physician practices. Doing so can help resolve incomplete incentive contract problems (as the authors argue), but it also signals a more sophisticated approach to personnel management, which aligns with our findings.
The emphasis on and ability to expand NP and PA employment, specifically, within vertically integrated systems may stem from several factors. First, it has been previously noted that prevailing regulations can blunt some provider substitution possibilities within physician practices (Zeckhauser & Eliastam, 1974). Restrictive scope of practice regulations can prohibit advanced practice providers from performing some clinical duties and/or mandate costly joint production to some degree during care delivery (i.e., dual involvement of physicians and NPs/PAs). However, these laws may be less influential within a vertically integrated environment since legal compliance with any oversight requirements might be more easily satisfied.7 The integrated firm already employs both provider types, and the different sources of clinical labor are likely to work within close proximity and share common clinical and billing infrastructure (e.g., electronic health records, e-prescribing software, and medical billing resources). Such regulations may, in turn, only weakly bind for these more complex firms—and perhaps not at all. Second, expanding provider supply via NP and PA labor can help restrain the broader health system’s labor cost growth. This strategy can then facilitate lower cost service provision, which might be most important for care supplied to publicly insured (and hence lower reimbursing) patients. For example, Richards et al. (2016) find increases in Medicaid acceptance following physician practice takeovers by health systems. Conversely, more efficient care delivery could leave service prices unaltered and instead improve profit margins across services. Although NP-delivered primary care has been associated with lower Medicare spending and intensity of care (Perloff et al., 2016), an industry-focused study reports that physician practices relying more on advanced practice providers actually generate higher net income, especially among hospital-owned entities (Kacik, 2018). For these reasons, it cannot be assumed that greater use of advanced practice clinicians will necessarily translate to less expensive care supplied to the market. Any enhanced supply and efficiency of care delivery can be socially beneficial outcomes from vertical integration, but other downsides from greater industry consolidation (e.g., higher service prices) remain. In fact, these organizational adjustments may be co-occurring strategic behaviors on the part of integrated health systems (i.e., delivery care more cheaply while raising prices for payers).
Limitations
Our study is not without limitations. First, the SK&A data do not provide information on the employment status (full-time or part-time) of NPs and PAs or how these clinicians are being utilized within practices. Thus, we do not know if NPs and PAs carry their own panel of patients; provide services in only certain types of patient visits; or if clinical work within the practice is delegated to the NP or PA or delivered within a team-based model of care. Our longitudinal design and wider geographic scope improve on the available research, but we cannot claim causality of the impact of vertical integration on the decision of the practice or health system to employ NPs and PAs. This decision may be driven by other care delivery needs and cost factors not represented in the data. However, our results provide new empirical evidence of greater use of NPs and PAs after physician practice vertical integration with corresponding improvements in practice and physician productivity.
Conclusion
The regulatory tensions between incentivizing tighter care coordination and inadvertently driving health care industry consolidation are salient tradeoffs facing policymakers (Baicker & Levy, 2013; Berenson et al., 2010; Burns & Muller, 2008). For example, other work has shown broad trends toward greater physician consolidation (Fulton, 2017; Muhlestein & Smith, 2016), which likely corresponds to higher service prices in the presence of weakened competition (Baker et al., 2014; Dunn & Shapiro, 2014). Moreover, in a recent trade press report, only 3% of surveyed health systems say that hiring more physicians has been financially harmful—with far more claiming direct financial benefits from these transactions (Bannow, 2018).
Notwithstanding these potential downsides from increased hospital ownership of physician practices, we show that vertical integration is associated with increased blending of high-skill provider types within practices and that these changes appear to coincide with enhanced productivity, practice diversification (in terms of specialty—and hence patient—mix), and task allocation. These observed changes suggest opportunities for improved efficiency in care delivery and are broadly appealing to clinicians and administrators, especially since “team-based” care remains challenging and perhaps aspirational for the plurality of health care providers (Castellucci, 2017). Yet, from a social welfare perspective, the anticompetitive effects from aggressive M&A activity across the health care sector can proceed in parallel and ultimately overwhelm any physician practice management benefits from vertical integration. For these reasons, the encouraging organizational behavior changes we document do not lessen the need for careful and ongoing antitrust scrutiny of current and future hospital–physician firm combinations.
Supplementary Material
Acknowledgments
We thank the organizers and participants of the 2019 American Society of Health Economists (ASHEcon) conference in Washington, DC, for the opportunity to present this work. Additionally, we wish to thank the Leonard Davis Institute of Health Economics and the Center for Health Outcomes and Policy Research (both part of the University of Pennsylvania) for providing financial support and excellent data resources. We also thank the Florida Agency for Health Care Administration (AHCA) for providing additional data resources. AHCA did not contribute to any analyses or interpretations of the data. All expressed views and any errors belong solely to the authors.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the AcademyHealth 2016 New Investigator Small Grant Program (Barnes, PI) and the National Institute of Nursing Research (T32NR007104, Aiken, PI).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
Ciliberto and Dranove (2006) are an important exception; the authors do not find price changes for hospitals integrating (and disintegrating) in the 1990s.
In contrast, Supplemental Appendix Figure A1 (available online) shows the trends in horizontal (i.e., physician group ownership) integration over time among our analytic sample. There is virtually no meaningful variation along this ownership structure margin, so we do not include it in our main empirical work. Regressions such as those we use for vertical integration changes, show no pattern of a relationship between horizontal integration and staffing patterns (results available by request from the corresponding author).
We also examined the average number of physicians employed in practices by ownership type. Supplemental Appendix Table A1 (available online) shows that the practices are not really growing in size in terms of physician count over time.
We have also explored the intensive margin (i.e., number of NPs or PAs within a practice), but it seems that all vertical integration effects localize to the extensive margin. For example, Supplemental Appendix Figure A2 (available online) shows trends in the number of NPs and PAs among vertically integrated practices that employed at least one of these providers at baseline. Integrated practices are not strongly titrating up the number of advanced practice clinicians over time.
Practice specialty categories were determined by the specialization reported in the 2008 (i.e., baseline) wave of our analytic data.
We also estimated our simple, two-way specification using a logistic regression model (with full vectors of practice and time fixed effects) and display the average marginal effect for the vertical integration indicator variable (Supplemental Appendix Table A3, available online). Overall, the results share the same qualitative patterns of the results of our main model. With the nonlinear model relying on within-practice variation over time, we lose practices where there is no within-practice variation of the dependent variables (i.e., NP or PA employment is always 1 or always 0 across all study years). Thus, there is a substantial loss of information in the logistic fixed effect regression model compared with the LPM in our two-way fixed effect analytic setting.
We also ran a version of Equation 1 that interacted the time-varying vertical integration variable with practices’ state-level scope of practice laws (i.e., a dummy variable indicated the practice is located in a state granting full scope of practice for NPs in that year). The resulting coefficient for the probability of NP employment was 0.008 (p = .049), suggesting that the positive association was slightly (roughly 1 percentage point) larger within regulatory environments more accommodating to NPs. However, the additional interaction was never statistically significant when stratifying by practice specialty nor when examining the PA employment outcome (results available by request).
References
- Baicker K, & Levy H (2013). Coordination versus competition in health care reform. New England Journal of Medicine, 369(9), 789–791. 10.1056/NEJMp1306268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker LC, Bundorf MK, & Kessler DP (2016). The effect of hospital/physician integration on hospital choice. Journal of Health Economics, 50(December), 1–8. 10.1016/j.jhealeco.2016.08.006 [DOI] [PubMed] [Google Scholar]
- Baker LC, Bundorf MK, Royalty AB, & Levin Z (2014). Physician practice competition and prices paid by private insurers for office visits. Journal of the American Medical Association, 312(16), 1653–1662. 10.1001/jama.2014.10921 [DOI] [PubMed] [Google Scholar]
- Bannow T (2018, July 14). Docs don’t drain hospital finances, systems say. Modern Healthcare. https://www.modernhealthcare.com/article/20180714/NEWS/180719978/docs-don-t-drain-hospital-finances-systems-say [Google Scholar]
- Barnes H, Richards MR, McHugh MD, & Martsolf G (2018). Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Affairs (Millwood), 37(6), 908–914. 10.1377/hlthaff.2017.1158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson RA, Ginsburg PB, & Kemper N (2010). Unchecked provider clout in California foreshadows challenges to health reform. Health Affairs (Millwood), 29(4), 699–705. 10.1377/hlthaff.2009.0715 [DOI] [PubMed] [Google Scholar]
- Burns LR, Goldsmith JC, & Sen A (2013). Horizontal and vertical integration of physicians: A tale of two tails. Annual Review of Health Care Management, 15, 39–119. 10.1108/s1474-8231(2013)0000015009 [DOI] [PubMed] [Google Scholar]
- Burns LR, & Muller RW (2008). Hospital-physician collaboration: Landscape of economic integration and impact on clinical integration. Milbank Quarterly, 86(3), 375–434. 10.1111/j.1468-0009.2008.00527.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capps C, Dranove D, & Ody C (2018). The effect of hospital acquisitions of physician practices on prices and spending. Journal of Health Economics, 59(May), 139–152. 10.1016/j.jhealeco.2018.04.001 [DOI] [PubMed] [Google Scholar]
- Carlin CS, Dowd B, & Feldman R (2015). Changes in quality of health care delivery after vertical integration. Health Services Research, 50(4), 1043–1068. 10.1111/1475-6773.12274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlin CS, Feldman R, & Dowd B (2016). The impact of hospital acquisition of physician practices on referral patterns. Health Economics, 25(4), 439–454. 10.1002/hec.3160 [DOI] [PubMed] [Google Scholar]
- Castellucci M (2017, June 14). Advanced practitioners called on to ease cancer care shortage, but challenges remain. Modern Healthcare. http://www.modernhealthcare.com/article/20170614/NEWS/170619950 [Google Scholar]
- Ciliberto F, & Dranove D (2006). The effect of physician–hospital affiliations on hospital prices in California. Journal of Health Economics, 625(1), 29–38. 10.1016/j.jhealeco.2005.04.008 [DOI] [PubMed] [Google Scholar]
- DeFelice LC, & Bradford WD (1997). Relative inefficiencies in production between solo and group practice physicians. Health Economics, 6(5), 455–465. [DOI] [PubMed] [Google Scholar]
- Dill MJ, Pankow S, Erikson C, & Shipman S (2013). Survey shows consumers open to a greater role for physician assistants and nurse practitioners. Health Affairs (Millwood), 32(6), 1135–1142. 10.1377/hlthaff.2012.1150 [DOI] [PubMed] [Google Scholar]
- Dunn A, & Shapiro AH (2014). Do physicians possess market power? Journal of Law & Economics, 57(1), 159–193. 10.1086/674407 [DOI] [Google Scholar]
- Everson J, Richards MR, & Buntin MB (2019). Horizontal and vertical integration’s role in meaningful use attestation over time. Health Services Research, 54(5), 1075–1083. 10.1111/1475-6773.13193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulton BD (2017). Health care market concentration trends in the United States: Evidence and policy responses. Health Affairs (Millwood), 36(9), 1530–1538. 10.1377/hlthaff.2017.0556 [DOI] [PubMed] [Google Scholar]
- Gaynor M, & Pauly MV (1990). Compensation and productive efficiency in partnerships: Evidence from medical groups practice. Journal of Political Economy, 98(3), 544–573. 10.1086/261694 [DOI] [Google Scholar]
- Golladay FL, Miller M, & Smith KR (1973). Allied health manpower strategies: Estimates of the potential gains from efficient task delegation. Medical Care, 11(6), 457–469. 10.1097/00005650-197311000-00001 [DOI] [PubMed] [Google Scholar]
- IQVIA. (2020). OneKey by IQVIA. www.skainfo.com
- Kacik A (2018, July 20). Advanced practice and nurse practitioners bring more profit, productivity, to medical practices. Modern Healthcare. https://www.modernhealthcare.com/article/20180720/NEWS/180729986/advanced-practice-and-nurse-practitioners-bring-more-profit-productivity-to-medical-practices [Google Scholar]
- Kaissi A, Kralewski J, & Dowd B (2003). Financial and organizational factors affecting the employment of nurse practitioners and physician assistants in medical group practices. Journal of Ambulatory Care Management, 26(3), 209–216. 10.1097/00004479-200307000-00004 [DOI] [PubMed] [Google Scholar]
- Karash JA (2018, July 28). Value-based healthcare models require a better-educated, patient-centered workforce. Modern Healthcare. https://www.modernhealthcare.com/article/20180728/NEWS/180729930/value-based-health-care-models-require-a-better-educated-patient-centered-workforce [Google Scholar]
- Koch TG, Wendling BW, & Wilson NE (2017). How vertical integration affects the quantity and cost of care for Medicare beneficiaries. Journal of Health Economics, 52(March), 19–32. 10.1016/j.jhealeco.2016.12.007 [DOI] [PubMed] [Google Scholar]
- Kocher R, & Shani NR (2011). Hospitals’ race to employ physicians: The logic behind a money-losing proposition. New England Journal of Medicine, 364(19), 1790–1793. 10.1056/NEJMp1101959 [DOI] [PubMed] [Google Scholar]
- Konetzka RT, Stuart EA, & Werner RM (2018). The effect of integration of hospitals and post-acute care providers on Medicare payment and patient outcomes. Journal of Health Economics, 61(September), 244–258. 10.1016/j.jhealeco.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo YF, Loresto FL Jr., Rounds LR, & Goodwin JS (2013). States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Affairs, 32(7), 1236–1243. 10.1377/hlthaff.2013.0072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lammers E (2013). The effect of hospital-physician integration on health information technology adoption. Health Economics, 22(10), 1215–1229. 10.1002/hec.2878 [DOI] [PubMed] [Google Scholar]
- Maier CB, Barnes H, Aiken LH, & Busse R (2016). Descriptive, cross-country analysis of the nurse practitioner workforce in six countries: Size, growth, physician substitution potential. BMJ Open, 6(9), 1–11. 10.1136/bmjopen-2016-011901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martsolf GR, Barnes H, Richards MR, Ray KN, Brom HM, & McHugh MD (2018). Employment of advanced practice clinicians in physician practices. JAMA Internal Medicine, 178(7), 988–990. 10.1001/jamainternmed.2018.1515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough JS, & Snir EM (2010). Monitoring technology and firm boundaries: Physician-hospital integration and technology utilization. Journal of Health Economics, 29(3), 457–467. 10.1016/j.jhealeco.2010.03.003 [DOI] [PubMed] [Google Scholar]
- Muhlestein DB, & Smith NJ (2016). Physician consolidation: Rapid movement from small to large group practices, 2013–2015. Health Affairs (Millwood), 35(9), 1638–1642. 10.1377/hlthaff.2016.0130 [DOI] [PubMed] [Google Scholar]
- Neprash HT, Chernew ME, Hicks AL, Gibson T, & McWilliams JM (2015). Association of financial integration between physicians and hospitals with commercial health care prices. JAMA Internal Medicine, 175(12), 1932–1939. 10.1001/jamainternmed.2015.4610 [DOI] [PubMed] [Google Scholar]
- Nikpay SS, Richards MR, & Penson D (2018). Hospital-physician consolidation accelerated in the past decade in cardiology, oncology. Health Affairs (Millwood), 37(7), 1123–1127. 10.1377/hlthaff.2017.1520 [DOI] [PubMed] [Google Scholar]
- Park J, Wu X, Frogner BK, & Pittman P (2018). Does the patient-centered medical home model change staffing and utilization in the community health centers? Medical Care, 56(9), 784–790. 10.1097/MLR.0000000000000965 [DOI] [PubMed] [Google Scholar]
- Perloff J, DesRoches CM, & Buerhaus P (2016). Comparing the cost of care provided to Medicare beneficiaries assigned to primary care nurse practitioners and physicians. Health Services Research, 51(4), 1407–1423. 10.1111/1475-6773.12425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips SJ (2014). 26th Annual legislative update: Progress for APRN authority to practice. Nurse Practitioner, 39(1), 29–52. 10.1097/01.NPR.0000440642.09390.fa [DOI] [PubMed] [Google Scholar]
- Phillips SJ (2015). 27th Annual APRN legislative update: Advancements continue for APRN practice. Nurse Practitioner, 40(1), 16–42. 10.1097/01.NPR.0000457433.04789.ec [DOI] [PubMed] [Google Scholar]
- Phillips SJ (2016). 28th Annual APRN legislative update: Advancements continue for APRN practice. Nurse Practitioner, 41(1), 21–48. 10.1097/01.NPR.0000475369.78429.54 [DOI] [PubMed] [Google Scholar]
- Post B, Buchmueller T, & Ryan AM (2018). Vertical integration of hospitals and physicians: Economic theory and empirical evidence on spending and quality. Medical Care Research and Review, 75(4), 399–433. 10.1177/1077558717727834 [DOI] [PubMed] [Google Scholar]
- Reinhardt U (1972). A production function for physician services. Review of Economics and Statistics, 54(1), 55–66. 10.2307/1927495 [DOI] [Google Scholar]
- Rhodes KV, Kenney GM, Friedman AB, Saloner B, Lawson CC, Chearo D, Wissoker D, & Polsky D (2014). Primary care access for new patients on the eve of health care reform. JAMA Internal Medicine, 174(6), 861–869. 10.1001/jamainternmed.2014.20 [DOI] [PubMed] [Google Scholar]
- Richards MR, Nikpay SS, & Graves JA (2016). The growing integration of physician practices: With a Medicaid side effect. Medical Care, 54(7), 714–718. 10.1097/MLR.0000000000000546 [DOI] [PubMed] [Google Scholar]
- Robinson JC (1998). Physician-hospital integration and the economic theory of the firm. Medical Care Research and Review, 54(1), 3–24. 10.1177/107755879705400101 [DOI] [PubMed] [Google Scholar]
- Robinson JC, & Miller K (2014). Total expenditures per patient in hospital-owned and physician-owned physician organizations in California. Journal of the American Medical Association, 312(16), 1663–1669. 10.1001/jama.2014.14072 [DOI] [PubMed] [Google Scholar]
- Scott KW, Orav EJ, Cutler DM, & Jha AK (2017). Changes in hospital–physician affiliations in U.S. hospitals and their effect on quality of care. Annals of Internal Medicine, 166(1), 1–8. 10.7326/M16-0125 [DOI] [PubMed] [Google Scholar]
- Zeckhauser R, & Eliastam M (1974). The productivity potential of the physician assistant. Journal of Human Resources, 9(1), 95–116. 10.2307/145047 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


