Abstract
Objective: To innvestigate the application of etomidate and propofol mixture in the evacuation of hematoma in patients with epidural hematoma. Methods: 98 patients with epidural hematoma were randomly divided into two groups: the joint group (n=49, anesthesia induction with etomidate and propofol) and the etomidate group (n=49, anesthesia induction with etomidate) using a random number table. Hemodynamics, stress response and cerebral oxygen metabolism were compared between the two groups at T0 (pre-anesthesia induction), T1 (after endotracheal intubation), T2 (10 min after the beginning of the operation) and T3 (the end of the operation). Adverse reactions were also analyzed. Results: Compared with T0, the mean arterial pressure (MAP) at T1, T2 and T3 in the joint group decreased first and then increased, and the MAP at T1 was significantly lower than that in the etomidate group (P<0.05). Compared with T0, blood oxygen saturation of internal jugular vein bulb (SjvO2) increased in T1-T3 groups, and SjvO2 in the joint group was higher than that in the etomidate group (all P<0.05). Compared with T0, cerebral oxygen uptake rate (CERO2) in the T1-T3 groups decreased significantly, and CERO2 at T3 in the joint group was higher than that in the etomidate group (all P<0.05). Compared with T0, the levels of cortisol and superoxide dismutase (SOD) at T3 in the two groups were significantly lower, but those in the etomidate group were higher than those in the combination group (all P<0.05). There was no significant difference in the incidence of postoperative anesthesia-related adverse reactions between the two groups (P>0.05). Conclusion: Etomidate has less effect on hemodynamics and stress reaction during intravenous anesthesia, but its combination with propofol can improve cerebral oxygen metabolism to a certain extent with fewer adverse reactions.
Keywords: Etomidate, propofol, hematoma removal, hemodynamics, cerebral oxygen metabolism, stress response
Introduction
Epidural hematoma refers to the vascular brain edema caused by the rupture and hemorrhage of bridging vein between venous sinus and cortex, which can lead to pathological changes such as cerebral ischemia and hypoxia, abnormal brain metabolism, a rapid increase of intracranial pressure, and the mortality rate is as high as 60%-90% [1,2]. Some studies have pointed out that if the hematoma is removed within 4 hours after the onset of the disease, patients’ survival rate can be increased to about 70%, but some patients still die due to irreversible damage of brain function [3-5].
Evacuation of intracranial hematoma is an essential operation for the treatment of epidural hematoma. However, the use of anesthetics during the operation will impact on the outcome of the patients’ hemodynamics and cerebral oxygen metabolism, which is not conducive to patients’ postoperative recovery [6,7]. Therefore, choosing a safe and effective anesthesia method has crucial clinical significance, such as reducing hemodynamics’ fluctuation during the operation, reducing cerebral oxygen metabolism injury, and promoting patients’ postoperative recovery.
Etomidate and propofol are commonly used intravenous anesthetics. Studies showed that intravenous anesthesia with etomidate has little effect on hemodynamics but a relatively significant impact on cerebral oxygen metabolism [8,9]. However, whether the combination with propofol can significantly improve cerebral oxygen metabolism in surgical patients has not been reported. Therefore, this study aims to compare etomidate’s effect and its combination with propofol on the hemodynamics, stress response and cerebral oxygen metabolism.
Materials and methods
General data
In this prospective study, 98 patients with epidural hematoma who underwent hematoma removal in our hospital from October 2018 to January 2020 were divided into the joint group (n=49) and the etomidate group (n=49) according to the random number table method.
Inclusive criteria: 1) patients aged 25-65 years old; 2) patients with a clear history of trauma and diagnosed by brain CT or MRI; 3) patients with hematoma volume <200 mL; 4) patients with midline displacement <10 mm; 5) patients with elective hematoma removal; 6) patients with ASA classification of II-III [10].
Exclusion criteria: 1) patients with coagulation system dysfunction; 2) patients with complex systemic injury; 3) patients with other cerebrovascular diseases, such as cerebral infarction; 4) patients with malignant tumor; 5) pregnant or breast-feeding women; 6) patients who are allergic to drugs in this study; 7) patients who participated in other researches at the same time; 8) patients with mental diseases and unable to cooperate. All patients in this study signed informed consent and the medical ethics committee of our hospital approved this study.
Method
The patients in both groups were given an intramuscular injection of 0.5 mg atropine (Jiangsu Yuexing Pharmaceutical Co., Ltd., batch number: 180427) 30 min before the operation. After entering the room, venous access was established and regular oxygen inhalation was performed. In the etomidate group, 0.3 mg/kg etomidate (Jiangsu Enhua Pharmaceutical Co., Ltd., batch number: 181112), 3 μg/kg fentanyl (Jiangsu Enhua Pharmaceutical Co., Ltd., batch No.: 180805), 0.15 mg/kg vecuronium (Chongqing Yaoyou Pharmaceutical Co., Ltd., batch No.: 181120) were injected intravenously in turn for induction of anesthesia. Endotracheal intubation was performed after the muscle relaxation was satisfied, and the anesthesia was maintained by continuous infusion of etomidate 0.4-0.7 mg/(kg·h) with micropump during the operation. Anesthesia induction in the joint group was the same as that in the etomidate group. Propofol and etomidate were continuously pumped with a micropump to maintain anesthesia at 4-6 mg/(kg·h) and 0.2-0.4 mg/(kg·h), respectively during the operation. Vecuronium was injected intermittently according to the specific situation of patients during the operation.
Outcome measures
Primary outcome measures
(1) The hemodynamics including mean arterial pressure (MAP, normal range 70-105 mmHg) and heart rate (HR, normal range 60-100 beats/min) at T0, T1, T2 and T3 were compared between the two groups. T0, T1, T2 and T3 represented pre-anesthesia induction, after the endotracheal intubation, 10 min after the beginning of the operation and at the end of the operation, respectively. (2) The levels of cerebral oxygen metabolism indexes, including CERO2 and SjvO2 were compared between the two groups. (3) The stress indexes, including cortisol and superoxide dismutase (SOD) at T0 and T3 were compared between the two groups.
Secondary outcome measures
The incidence of adverse reactions (such as nausea, vomiting, dizziness, etc.) was calculated. Anesthesia-related postoperative adverse reactions such as nausea, vomiting and dizziness were compared between the two groups. The total incidence of adverse reactions = cases of adverse reactions/total cases * 100%.
Statistical analysis
SPSS 20.0 was used for data statistics. The counting data was expressed as (n/%). A Chi-square test was used for comparison. The measurement data was expressed as (x̅ ± s). The paired t-test was used for comparison before and after the treatment in the same group. The independent t-test was used for comparison between the two groups. The difference was statistically significant when P<0.05.
Results
General information
There was no significant difference in the general information between the two groups (all P>0.05). The two groups were comparable. See Table 1.
Table 1.
Comparison of general data between the two groups (n, x̅ ± s)
| Joint group (n=49) | Etomidate group (n=49) | χ2/t | P | |
|---|---|---|---|---|
| Gender (n) | 0.653 | 0.419 | ||
| Male | 26 | 22 | ||
| Female | 23 | 27 | ||
| Age (year) | 46.6±5.9 | 47.2±6.4 | 0.483 | 0.631 |
| BMI (kg/m2) | 23.33±2.10 | 23.18±1.75 | 0.384 | 0.702 |
| Time from injury to admission (h) | 2.02±0.88 | 2.13±0.79 | 0.651 | 0.517 |
| Hematoma volume (mL) | 143.28±20.93 | 145.04±22.28 | 0.403 | 0.688 |
| Midline shift (mm) | 6.68±1.89 | 6.43±1.77 | 0.676 | 0.501 |
| Causes of injury (n) | 1.646 | 0.649 | ||
| Fall from a height | 13 | 10 | ||
| Violent injuries | 10 | 12 | ||
| Traffic accident | 18 | 15 | ||
| Others | 8 | 12 | ||
| ASA classification (n) | 2.003 | 0.157 | ||
| Grade ll | 29 | 22 | ||
| Grade lll | 20 | 27 |
Note: BMI: body mass index; ASA: American Society of anesthesiologists.
Hemodynamics
There were no significant MAP and HR changes at T0-T3 in the etomidate group and HR at T0-T3 in the joint group (all P>0.05). The MAP at T1, T2 and T3 in the joint group decreased first and then increased compared with that at T0 and the difference was statistically significant. MAP at T1 was significantly lower than that in the etomidate group (P<0.05). See Table 2.
Table 2.
Hemodynamic changes during anesthesia in two groups (x̅ ± s)
| Groups | Time | MAP (mmHg) | HR (times/min) |
|---|---|---|---|
| Joint group (n=49) | T0 | 98.89±10.88 | 73.30±5.44 |
| T1 | 94.48±9.66*,# | 73.98±5.93 | |
| T2 | 104.40±10.80* | 74.03±6.49 | |
| T3 | 103.22±8.64* | 73.39±5.93 | |
| Etomidate group (n=49) | T0 | 99.57±11.95 | 73.86±6.11 |
| T1 | 102.08±10.76 | 73.77±6.44 | |
| T2 | 101.94±11.48 | 74.20±5.49 | |
| T3 | 100.77±11.45 | 74.08±5.89 |
Note: MAP: mean arterial pressure; HR: heart rate. Compared with T0;
P<0.05.
Compared with etomidate group at the same time;
P<0.05.
Cerebral oxygen metabolism index
Compared with T0, the SjvO2 of the two groups increased significantly at T1-T3, and the SjvO2 of the joint group was higher than that of the etomidate group at the same time (all P<0.05). Compared with T0, CERO2 of both groups decreased significantly at T1-T3, and CERO2 of the joint group at T3 was higher than that of the etomidate group (all P<0.05). See Table 3.
Table 3.
Changes of cerebral oxygen metabolism during anesthesia in two groups (x̅ ± s)
| Groups | Time | CERO2 | SjvO2 |
|---|---|---|---|
| Joint group (n=49) | T0 | 39.98±2.99 | 63.98±3.77 |
| T1 | 34.60±3.02* | 84.49±4.88*,# | |
| T2 | 36.10±2.85* | 77.79±4.30*,# | |
| T3 | 38.09±3.04*,# | 74.46±3.84*,# | |
| Etomidate group (n=49) | T0 | 40.04±3.20 | 64.40±3.02 |
| T1 | 35.49±3.33* | 78.88±4.97* | |
| T2 | 35.48±3.20* | 70.05±3.38* | |
| T3 | 34.44±3.82* | 67.74±3.08* |
Note: CERO2: cerebral oxygen uptake rate; SjvO2: blood oxygen saturation of internal jugular bulb. Compared with T0;
P<0.05.
Compared with etomidate group at the same time;
P<0.05.
Stress indexes
Compared with T0, the levels of cortisol and SOD in the two groups at T3 were significantly lower, but the cortisol and SOD levels in the etomidate group were higher than those in the joint group (all P<0.05). See Table 4.
Table 4.
Changes of stress response indexes during anesthesia in two groups (x̅ ± s)
| Group | Index | T0 | T3 |
|---|---|---|---|
| Joint group (n=49) | Cortisol (mmol/L) | 355.37±20.98 | 238.90±19.83*,# |
| SOD (U/L) | 104.40±9.93 | 89.48±8.77*,# | |
| Etomidate group (n=49) | Cortisol (mmol/L) | 356.55±18.70 | 273.30±17.47* |
| SOD (U/L) | 103.96±10.04 | 97.78±7.46* |
Note: SOD: superoxide dismutase. Compared with T0 time in the same group;
P<0.05.
Compared with the Etomidate group at the same time;
P<0.05.
Adverse reactions
There was no significant difference in the incidence of postoperative anesthesia-related adverse reactions between the two groups (P>0.05). See Table 5 and Figure 1.
Table 5.
Comparison of the incidence of adverse reactions between the two groups
| Group | Nausea | Vomiting | Dizzy | Blurred vision | Total incidence |
|---|---|---|---|---|---|
| Joint group (n=49) | 5 (10.20) | 2 (4.08) | 1 (2.04) | 1 (2.04) | 9 (18.37) |
| Etomidate group (n=49) | 4 (8.16) | 1 (2.04) | 0 (0.00) | 1 (2.04) | 6 (12.24) |
Figure 1.
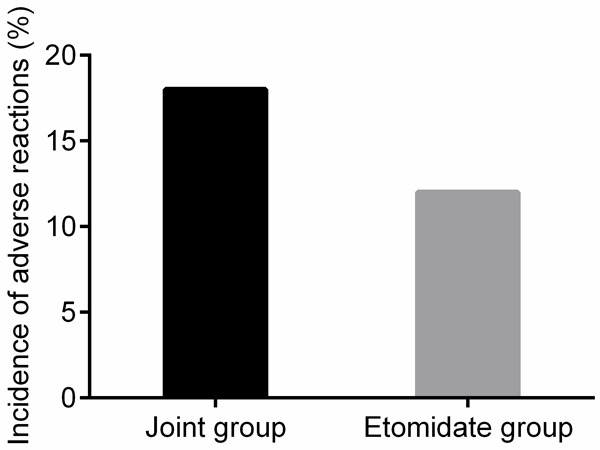
Comparison of the incidence of adverse reactions between the two groups.
Discussion
Evacuation of intracranial hematoma is the primary operation method of epidural hematoma, but anesthetics will inevitably affect the body’s hemodynamics and cerebral oxygen metabolism [11,12]. So it is vital to find safe and effective drugs to reduce the adverse impact of surgery on patients.
Etomidate and propofol are commonly used clinical intravenous anesthesia induction drugs, which have fast onset, fast recovery after an operation, and fewer adverse reactions caused by anesthesia. However, a single induction of etomidate has a more significant impact on the hemodynamics of patients. Propofol can directly inhibit the systolic cardiac function, affect the circulatory system, and reduce cardiac output [13,14]. There were no significant changes in MAP and HR at T0-T3 in the etomidate group and HR at T0-T3 in the joint group in this study. The MAP at T1, T2 and T3 in the joint group decreased first and then increased compared with that at T0, and the difference was statistically significant. This phenomenon suggested that etomidate had less effect on hemodynamics during intravenous anesthesia than propofol. It was speculated that etomidate did not affect the tension discharge of the sympathetic nerve. It does not affect atrial function and conduction and does not inhibit the reflex of vascular baroreceptors, leading to less impact on fluctuation in heart rate and blood pressure [15]. The hemodynamics fluctuated more after the combination with propofol. This study is consistent with the results of Meyancı et al., which also pointed out that general anesthesia with etomidate can make patients’ hemodynamics more stable during the operation [16].
The imbalance of cerebral oxygen supply and demand is the leading cause of secondary brain injury in patients with intracranial epidural hematoma. Some studies [17] showed that reducing or restoring the imbalance of cerebral oxygen supply and demand as soon as possible can improve patients’ prognosis after the removal of intracranial hematoma. The traditional detection of intracranial pressure and cerebral blood flow is not enough to reflect patients’ cerebral oxygen metabolism because the detection of intracranial pressure ignores the influence of cerebrovascular resistance and the detection of cerebral blood flow can only reflect the body’s hemodynamics. However, CERO2 and SjvO2 can directly affect the balance of cerebral oxygen supply and patients’ demand [18]. SjvO2 >75% indicates that brain tissue’ oxygen supply increases and the cerebral blood flow is sufficient. The decrease of SjvO2 indicates that the oxygen supply of brain tissue is decreased and the cerebral blood flow is decreased. The other characteristic of SjvO2 is that SjvO2 will decline abnormally before the brain tissue of patients shows symptoms of hypoxia, so it can be used as an early evaluation index of cerebral oxygen supply and demand imbalance [19,20]. The results showed that compared with T0, the SjvO2 of the two groups increased significantly at T1-T3, and the SjvO2 of the joint group was higher than that of the etomidate group at the same time. Compared with T0, CERO2 of both groups decreased significantly at T1-T3, and CERO2 of the joint group at T3 was higher than that of the etomidate group, suggesting that compared with etomidate, propofol combined with etomidate can effectively improve cerebral oxygen metabolism of patients undergoing intracranial hematoma removal. It is speculated that propofol has a good blocking effect on non-selective calcium channels, which can inhibit the release and inflow of calcium ions, expand the arteries and veins, and improve cerebral oxygen balance supply and demand of patients [21]. This study’s results are similar to that of Lee et al., which also pointed out that etomidate combined with propofol has less effect on oxygen metabolism in brain tissue [22].
Surgery and anesthetics are stressors for surgical patients, which will lead to different degrees of stress reaction. In this study, the cortisol and SOD levels of the two groups at T3 were significantly lower than those at T0. However, the cortisol and SOD levels of the etomidate group were higher than those of the joint group, suggesting that etomidate caused less stress response during intravenous anesthesia with etomidate and propofol. The reason may be that etomidate can inhibit the release of adrenocortical function and cortisol secretion [23].
Similar studies by Kaushal et al. also showed that etomidate has less stress response than propofol [24]. In terms of adverse reactions, no severe adverse reactions occurred in the two groups, and there was no significant difference in the incidence of anesthesia-related adverse reactions, suggesting that etomidate and propofol are safe for intravenous anesthesia. However, this study is a single-center study with limited sample size. Further studies are needed to confirm the effect of the combination of the two drugs on anesthesia patients.
In conclusion, compared with propofol, etomidate has less effect on hemodynamics and less stress reaction during intravenous anesthesia. However, etomidate combined with propofol can improve cerebral oxygen metabolism and with fewer adverse reactions.
Disclosure of conflict of interest
None.
References
- 1.Raffee L, Abuzayed B, Al Qawasmeh M, Alawneh K, Abdalla K, Aleshawi A. Isolated retrodental epidural hematoma without dens fracture. J Emerg Med. 2020;58:67–71. doi: 10.1016/j.jemermed.2019.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Eto F, Tatsumura M, Iwabuchi S, Ogawa T, Mammoto T, Hirano A. Clinical features of spontaneous spinal epidural hematoma. J Rural Med. 2019;14:206–210. doi: 10.2185/jrm.3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee LO, Bateman BT, Kheterpal S, Klumpner TT, Housey M, Aziz MF, Hand KW, MacEachern M, Goodier CG, Bernstein J, Bauer ME Multicenter Perioperative Outcomes Group Investigators. Risk of epidural hematoma after neuraxial techniques in thrombocytopenic parturients: a report from the Multicenter Perioperative Outcomes Group. Anesthesiology. 2017;126:1053–1063. doi: 10.1097/ALN.0000000000001630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuriyama M. Clinical manifestations of spinal epidural hematoma-stroke mimic and pitfalls in diagnosis. Brain Nerve. 2017;69:119–128. doi: 10.11477/mf.1416200652. [DOI] [PubMed] [Google Scholar]
- 5.Salehpour F, Mirzaei F, Kazemzadeh M, Alavi SAN. Spontaneous epidural hematoma of cervical spine. Int J Spine Surg. 2018;12:26–29. doi: 10.14444/5005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mercier FJ, Soued M, Morau E, Ngan Kee WD. Noradrenaline for haemodynamic control in obstetric anaesthesia: is it now a suitable alternative to phenylephrine? Anaesth Crit Care Pain Med. 2019;38:591–593. doi: 10.1016/j.accpm.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Hannam JA, Mitchell SJ, Cumin D, Frampton C, Merry AF, Moore MR, Kruger CJ. Haemodynamic profiles of etomidate vs propofol for induction of anaesthesia: a randomised controlled trial in patients undergoing cardiac surgery. Br J Anaesth. 2019;122:198–205. doi: 10.1016/j.bja.2018.09.027. [DOI] [PubMed] [Google Scholar]
- 8.Wang B, Yang J, Chen J, Kang Y, Yang LH, Liu J, Zhang WS. An etomidate analogue with less adrenocortical suppression, stable hemodynamics, and improved behavioral recovery in rats. Anesth Analg. 2017;125:442–450. doi: 10.1213/ANE.0000000000002063. [DOI] [PubMed] [Google Scholar]
- 9.Hadjihambi A, Karagiannis A, Theparambil SM, Ackland GL, Gourine AV. The effect of general anaesthetics on brain lactate release. Eur J Pharmacol. 2020;881:173–178. doi: 10.1016/j.ejphar.2020.173188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Apfelbaum JL, Connis RT. The American Society of Anesthesiologists practice parameter methodology. Anesthesiology. 2019;130:367–384. doi: 10.1097/ALN.0000000000002551. [DOI] [PubMed] [Google Scholar]
- 11.Al-Mufti F, Mayer SA. Neurocritical care of acute subdural hemorrhage. Neurosurg Clin N Am. 2017;28:267–278. doi: 10.1016/j.nec.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Khan AI, Fischer M, Pedoto AC, Seier K, Tan KS, Dalbagni G, Donat SM, Arslan-Carlon V. The impact of fluid optimisation before induction of anaesthesia on hypotension after induction. Anaesthesia. 2020;75:634–641. doi: 10.1111/anae.14984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Panagiotis F, Vanarvas V, Dewals W, Carvalho HN, Asmundis CD. Electrocardiographic effects of propofol versus etomidate in patients with brugada syndrome. Anesthesiology. 2020;132:440–451. doi: 10.1097/ALN.0000000000003030. [DOI] [PubMed] [Google Scholar]
- 14.Smischney NJ, Nicholson WT, Brown DR, Gallo De Moraes A, Hoskote SS, Pickering B, Oeckler RA, Iyer VN, Gajic O, Schroeder DR, Bauer PR. Ketamine/propofol admixture vs etomidate for intubation in the critically ill: KEEP PACE Randomized clinical trial. J Trauma Acute Care Surg. 2019;87:883–891. doi: 10.1097/TA.0000000000002448. [DOI] [PubMed] [Google Scholar]
- 15.Keating SC, Sage AM, Ambrisko TD, Somrak A, Carroll MQ, Oba PM, Martins B, Swanson KS. The effect of midazolam or lidocaine administration prior to etomidate induction of anesthesia on heart rate, arterial pressure, intraocular pressure and serum cortisol concentration in healthy dogs. Vet Anaesth Analg. 2020;47:160–167. doi: 10.1016/j.vaa.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 16.Meyancı Köksal G, Erbabacan E, Tunalı Y, Karaören G, Vehid S, Öz H. The effect of single dose etomidate during emergency intubation on hemodynamics and adrenal cortex. Ulus Travma Acil Cerrahi Derg. 2015;21:358–365. doi: 10.5505/tjtes.2015.06325. [DOI] [PubMed] [Google Scholar]
- 17.Jang KM, Choi HH, Mun HY, Nam TK, Park YS, Kwon JT. Critical depressed brain volume influences the recurrence of chronic subdural hematoma after surgical evacuation. Sci Rep. 2020;10:1145. doi: 10.1038/s41598-020-58250-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X, Hu Q, Liu Z, Huang H, Zhang Q, Dai H. Comparison between nitroglycerin and remifentanil in acute hypervolemic hemodilution combined with controlled hypotension during intracranial aneurysm surgery. Int J Clin Exp Med. 2015;8:19353–19359. [PMC free article] [PubMed] [Google Scholar]
- 19.Catchlove SJ, Macpherson H, Hughes ME, Chen Y, Parrish TB, Pipingas A. An investigation of cerebral oxygen utilization, blood flow and cognition in healthy aging. PLoS One. 2018;13:e0197055. doi: 10.1371/journal.pone.0197055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vestergaard MB, Larsson HB. Cerebral metabolism and vascular reactivity during breath-hold and hypoxic challenge in freedivers and healthy controls. J Cereb Blood Flow Metab. 2019;39:834–848. doi: 10.1177/0271678X17737909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wan HJ, Wang Y, Si JQ, Li L. Propofol-induced vasodilation of mesenteric arterioles via BKCa channel and gap junction. Exp Ther Med. 2018;16:2960–2968. doi: 10.3892/etm.2018.6527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee JM, Min G, Keum B, Lee JM, Kim SH, Choi HS, Kim ES, Seo YS, Jeen YT, Chun HJ, Lee HS, Um SH, Kim CD. Using etomidate and midazolam for screening colonoscopies results in more stable hemodynamic responses in patients of all ages. Gut Liver. 2019;13:649–657. doi: 10.5009/gnl18514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang J, Kang Y, Wang B, Yang L, Liu J, Zhang W. Metabolite-inactive etomidate analogues alleviating suppression on adrenal function in Beagle dogs. Eur J Pharm Sci. 2017;99:343–349. doi: 10.1016/j.ejps.2016.12.041. [DOI] [PubMed] [Google Scholar]
- 24.Kaushal RP, Vatal A, Pathak R. Effect of etomidate and propofol induction on hemodynamic and endocrine response in patients undergoing coronary artery bypass grafting/mitral valve and aortic valve replacement surgery on cardiopulmonary bypass. Ann Card Anaesth. 2015;18:172–178. doi: 10.4103/0971-9784.154470. [DOI] [PMC free article] [PubMed] [Google Scholar]


