Abstract
Objective: This study was designed to explore the occurrence of post-traumatic stress disorder (PTSD) symptoms, job burnout and its influencing factors among nurses in intensive care units (ICU). Methods: A total of 150 ICU nurses were selected for questionnaire survey by systematic sampling and 143 questionnaires were returned. The questionnaires included a PTSD Checklist-Civilian Version (PCL-C), Maslach Burnout Inventory (MBI), Connor-Davidson Resilience Scale (CD-RISC) and the Social Support Rating Scale (SSRS). ICU nurses were divided into positive and negative groups according to PCL-C scores, the differences between the groups were compared, and the influencing factors for the occurrence of PTSD were analyzed. Results: ICU nurses had PCL-C scores ranging from 11 to 55 and were divided into the positive group (PCL-C ≥ 38, N=32) and the negative group (PCL-C < 38, N=111) according to the presence of PTSD, with a positive rate of 22.38%. The total MBI scores and scores in emotional exhaustion, depersonalization, and personal accomplishment in the positive group were significantly higher than those in the negative group, (P < 0.05). Health status, years of experience, age, CD-RISC scores, and SSRS scores showed significant difference between the two groups (P < 0.05). Multivariate logistic regression showed that MBI score was an independent risk factor for the development of PTSD symptoms among ICU nurses (OR > 1, P < 0.05), while CD-RISC score was a protective factor (OR < 1, P < 0.05). Conclusion: The incidence rate of PTSD among ICU nurses was 22.38%, and MBI score and CD-RISC score were independent influencing factors for the occurrence of PTSD symptoms.
Keywords: Post-traumatic stress disorder, job burnout, influencing factors, intensive care unit nurses
Introduction
Intensive care units (ICUs) are areas of the hospital where seriously ill patients receive specialized care with specialized equipment and resources [1]. Due to the nature of the ICU, critical care nursing requires an advanced technical skill set and the ability to cope with an increased workload. The ICU is also a frequent area of cardiopulmonary resuscitation, end-of-life issues and medical malpractice disputes. ICU nurses are exposed to stressors for a long time and bear mental stress [2]. It has been reported that the prevalence of PTSD is about 29% among ICU nurses [3]. PTSD is harmful, which limits patients’ functional ability and is detrimental to the ICU’s role in end-of-life care. Normally, PTSD lasts for a long time and can lead to disability in severe cases. Therefore, timely diagnosis of PTSD in ICU nurses and clarification of the influencing factors for occurrence of PTSD in ICU nurses are of great significance to improve PTSD symptoms and physical and mental health of ICU nurses, so as to improve their work efficiency. Clinical reports show that the occurrence of PTSD is related to job burnout, and PTSD is more likely to occur when job burnout is at a high level [4]. The high morbidity and mortality of their patients has great demands on their daily work. They need to also show care and patience to patients and work on day and night shifts, where they are more likely to experience PTSD. Therefore, this study analyzed the occurrence of PTSD symptoms, job burnout and the influencing factors for occurrence of PTSD among ICU nurses, so as to provide a reference for reducing the incidence of PTSD among ICU nurses.
Materials and methods
Baseline data
A systematic sampling method was used to select 150 ICU nurses for questionnaire survey. This study was approved by the Ethics Committee of Guangzhou Red Cross Hospital, Jinan University.
Inclusion criteria
(1) ICU nurses who voluntarily participated in the study and signed the informed consent; (2) registered ICU nurses with more than 6 months of work experience.
Exclusion criteria
(1) those with severe physical illness; (2) those with a history of mental illness; (3) women during pregnancy or lactation. A total of 150 questionnaires were distributed in this study, and 143 questionnaires were returned, with a return rate of 95.33%.
Methods
Questionnaires
PTSD was assessed using a 17-item PTSD Checklist-Civilian Version (PCL-C) [5], which showed good temporal stability, internal consistency, test-retest reliability, sensitivity, specificity and convergent validity. It covered three main syndromes of re-experiencing, avoidance and hypervigilance in 17 items on a 1 to 5 Likert scale, ranging from 17 to 85. Positive PTSD is indicated when the PCL-C is ≥ 38.
The Maslach Burnout Inventory (MBI) [6] is a psychological assessment instrument comprising 22 symptom items on a 0 to 6 Likert scale (6 being every day, 5 being several times a week, 4 being once a week, 3 being several times a month, 2 being once a month, 1 being several times a year, and 0 being none). It covers emotional exhaustion (9 items), depersonalization (5 items), and personal fulfillment (8 items), with the total score as the sum of the three dimensions. A higher score indicates greater emotional exhaustion, depersonalization, with a lower sense of personal accomplishment, and a greater degree of job burnout.
Connor-Davidson Resilience Scale (CD-RISC) consists of 25 items, which are evaluated on a five-point Likert scale ranging from 0-4 in terms of resilience, self-improvement, and optimism. A higher score indicates better resilience [7].
The Social Support Rating Scale (SSRS) consists of 10 items in terms of objective support, subjective support, and social support utilization. A higher score indicates higher social support [8].
Outcome measurements
Nurses’ gender, age, education, marital status, years of experience, job title, monthly income, PCL-C, MBI, CD-RISC, and SSRS scores were collected.
Statistical methods
The statistical software SPSS 22.0 was used to process the data. The count data of nurses such as gender, age, education, marital status, years of experience, job title, and monthly income were expressed as rates, and were examined by one-way χ2 test. Measurement data of age, PCL-C, MBI, CD-RISC, and SSRS scores were recorded as (x̅ ± s), and one-way ANOVAs were performed. Those with significant differences in one-way tests were included in multivariate logistic regression analysis. GraphPad Prism 8 was used to illustrate the figures. Differences were considered statistically significant when P < 0.05.
Results
Prevalence of PTSD symptoms among ICU nurses
ICU nurses scored 11 to 55 on the PCL-C, (9.52±3.87) on re-experiencing, (12.25±3.76) on avoidance, and (9.92±3.34) on hypervigilance, with a total score of (31.70±9.21). There were 32 nurses in the positive group (PCL-C ≥ 38) and 111 nurses in the negative group (PCL-C < 38), with a positive rate of 22.38% (Figure 1A).
Figure 1.
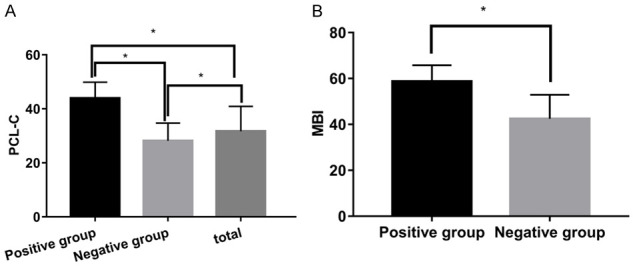
Comparison of PCL-C scores and MBI between positive and negative groups. A. Shows that PCL-C scores in the positive group were significantly higher than those in the negative group (t=12.191, P < 0.05). B. Shows that MBI in the positive group was significantly higher than that in the negative group (t=8.249, P < 0.05). *denotes a comparison between the two groups, P < 0.05.
Burnout in ICU nurses
In the positive group, the MBI scores and scores of emotional exhaustion, depersonalization, and personal accomplishment were (58.69±7.10) points, (24.44±3.66) points, (8.59±2.37) points, and (25.66±3.41) points, respectively, which were significantly higher than those of the negative group, i.e. (42.45±10.45), (20.11±6.57), (5.69±2.47), and (16.40±4.52) (P < 0.05) (Figure 1B).
Influencing factors for the occurrence of PTSD among ICU nurses
The differences were not significant in gender, education, marital status, title, and monthly income between the two groups of nurses (P > 0.05); while the differences were statistically significant in health status, years of work, age, CD-RISC score, and SSRS scores between the two groups (P < 0.05) (Table 1).
Table 1.
Analysis of influencing factors for the occurrence of PTSD symptoms among ICU nurses [n (%)]/(x̅ ± s)
| Influencing factors | Classification | Positive group (n=32) | Negative group (n=111) | χ2/t | P |
|---|---|---|---|---|---|
| Gender | Male | 2 (6.25) | 17 (15.32) | 1.772 | 0.183 |
| Female | 30 (93.75) | 94 (84.68) | |||
| Health status | Poor | 11 (34.38) | 19 (17.12) | 4.463 | 0.035 |
| Good | 21 (65.63) | 92 (82.88) | |||
| Education level | Secondary school | 2 (6.25) | 3 (2.70) | 1.076 | 0.300 |
| Tertiary | 12 (37.50) | 39 (35.14) | |||
| Bachelor’s degree and above | 18 (56.25) | 70 (63.06) | |||
| Marital status | Married | 18 (56.25) | 71 (63.96) | 1.257 | 0.262 |
| Unmarried | 12 (37.50) | 37 (33.33) | |||
| Divorce or separation | 2 (6.25) | 3 (2.70) | |||
| Years of working experience | < 3 years | 14 (43.75) | 39 (35.14) | 6.571 | 0.010 |
| 3~5 years | 10 (31.25) | 18 (16.22) | |||
| 6~10 years | 6 (18.75) | 40 (36.04) | |||
| > 10 years | 2 (6.25) | 14 (12.61) | |||
| Title | Nurse | 19 (59.38) | 68 (61.26) | 0.181 | 0.670 |
| Nurse practitioner | 8 (25.00) | 27 (24.32) | |||
| Chief Nurse | 3 (9.38) | 11 (9.91) | |||
| Associate Chief Nurse | 2 (6.25) | 5 (4.50) | |||
| Monthly income | < 1000 Yuan | 1 (3.13) | 3 (2.70) | 0.544 | 0.461 |
| 1000~3000 Yuan | 20 (62.50) | 62 (55.86) | |||
| 3001~5000 Yuan | 7 (21.88) | 28 (25.23) | |||
| > 5,000 Yuan | 4 (12.50) | 18 (16.22) | |||
| Age (years) | - | 34.31±3.71 | 29.10±3.20 | 7.824 | < 0.001 |
| CD-RISC score | - | 52.34±11.41 | 63.49±13.56 | 4.236 | < 0.001 |
| Toughness | 26.41±8.17 | 32.61±9.42 | 3.373 | 0.001 | |
| Strength | 17.31±4.56 | 21.04±6.29 | 3.123 | 0.002 | |
| Optimistic | 8.63±1.98 | 9.84±2.73 | 2.334 | 0.021 | |
| SSRS score | 24.25±5.52 | 27.95±5.59 | 3.308 | 0.001 | |
| Objective support | 7.16±2.05 | 8.11±2.12 | 2.249 | 0.026 | |
| Subjective support | 10.50±2.22 | 11.85±2.72 | 2.570 | 0.011 | |
| Social support utilization | 6.59±2.21 | 8.00±1.98 | 3.457 | 0.001 |
Multivariate analysis of influencing factors for the occurrence of PTSD among ICU nurses
PTSD was taken as the dependent variable (PTSD positive was assigned “1”, and PTSD negative was assigned “0”), and the single factor analysis result P < 0.05 was taken as the independent variable (poor health and working years of < 3 years were assigned “1”, good health and working years of 3-5 years were assigned “2”, working years of 6-10 years were assigned “3”, and working years of > 10 years were assigned “4”). MBI score was an independent risk factor for occurrence of PTSD among ICU nurses (OR > 1, P < 0.05), while CD-RISC score was a protective factor (OR < 1, P < 0.05) (Table 2).
Table 2.
Influencing Factors for the occurrence of PTSD symptoms among ICU nurses
| Variable | B | S.E. | Wald | P | OR | 95% confidence interval | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower limit | Upper limit | ||||||
| MBI scores | 0.687 | 0.240 | 8.203 | 0.004 | 1.988 | 1.242 | 3.181 |
| Health status | 1.025 | 1.933 | 0.281 | 0.596 | 2.787 | 0.063 | 123.074 |
| Years of experience | -0.001 | 0.788 | < 0.001 | 0.999 | 0.999 | 0.213 | 4.682 |
| Age | 0.485 | 0.291 | 2.784 | 0.095 | 1.624 | 0.919 | 2.872 |
| CD-RISC scores | -0.345 | 0.129 | 7.107 | 0.008 | 0.709 | 0.550 | 0.913 |
| SSRS scores | -0.278 | 0.176 | 2.478 | 0.115 | 0.758 | 0.536 | 1.070 |
| Constant | -28.644 | 16.347 | 3.070 | 0.080 | < 0.001 | ||
Discussion
PTSD is a psychological trauma caused by catastrophic and extraordinary traumatic events. It was originally used to reflect the mental health disorders caused by war. Later, people gradually discovered that violent attacks, natural disasters, deaths of relatives, occupational stress and other events can lead to PTSD [9]. It has been found that PTSD is more common among ICU nurses because they are prone to mental trauma due to the heavy workload of ICU nurses, traumatic events such as sudden emergencies or changes in conditions, and occasional bullying from colleagues [10,11]. This study found that ICU nurses scored 11 to 55 on the PCL-C, (9.52±3.87) for re-experiencing, (12.25±3.76) for avoidance, and (9.92±3.34) for high vigilance, with a total score of (31.70±9.21) and a positive rate of 22.38%, indicating a high prevalence of PTSD among ICU nurses and the need for targeted intervention.
Reports in recent years have also shown a high incidence of job burnout among medical staff [12,13]. Burnout is a psychological and physical fatigue syndrome caused by prolonged occupational stress, which can lead to emotional, attitudinal, and behavioral exhaustion in individuals, and it severely affects the quality and productivity of workers [14]. In this study, total MBI scores and scores on three dimensions in the positive group were significantly higher than those in the negative group, and MBI score was an independent risk factor for PTSD occurrence in ICU nurses, suggesting that the occurrence of PTSD is closely related to all dimensions of burnout. The reason may be that when ICU nurses have severe emotional exhaustion, depersonalization, low personal fulfillment, and low stress tolerance, their brain may experience a dissociative state to avoid the pain caused by the work [15].
A study has found that the occurrence of PTSD is related to family and psychosocial factors [16]. The present study showed that the difference between the two groups of nurses in terms of gender, education level, marital status, job title, and monthly income was not significant, slightly different from results of previous studies. Due to the physical differences between females and males, females are more flexible and tend to reveal inner feelings better and have a higher incidence of PTSD than males [17]. However, no difference was observed in this study, possibly due to fewer male nurses. It has been suggested that those with higher levels of literacy cope more calmly in the face of stressful events and have a lower incidence of PTSD, but some studies have shown no relationship between the level of literacy and the occurrence of PTSD [17,18], possibly due to the high professional requirements of ICU nurses and the relatively high level of literacy of all practitioners. It was found [19] that the incidence of PTSD is higher in divorced or separated individuals than in those in a harmonious family. However, the present study found that marital status did not affect the occurrence of PTSD, which may be due to a small sample size. Moreover, the effect of title and monthly income on the occurrence of PTSD in this study was not significant, which is consistent with the results of other studies.
In addition, this study showed significant differences in health status, years of experience, age, CD-RISC score, SSRS score between the positive and negative groups, and that CD-RISC score was a protective factor for the occurrence of PTSD symptoms among ICU nurses. Generally, a poorer health status, indicated nurses were more likely to be fatigued at work, and as ICU nurses experience urgent and heavy workloads consuming a lot of energy and mental effort, those with a poor health status are more stressed, so the risk of PTSD is higher. In this study, it was shown that the incidence of PTSD was higher in those with < 3 and 3-5 years of work experience, presumably because new nurses are inexperienced in coping with stress, while nurses with 3-5 years of work experience are the backbone of the ICU, with more tasks, responsibilities and more stress, leading to a higher risk of PTSD [20]. Some studies have shown that older people have a higher risk of developing PTSD [21,22]. Although age is associated with the occurrence of PTSD in this study, it is not an independent influencing factor, probably because although age can lead to reduced tolerance and increased risk of PTSD, ICU nurses are mostly young and there are fewer older workers [23]. Good social support can reduce and improve the symptoms of PTSD, and the provision of medical treatment and supplies by the state for earthquakes or other severe disasters can effectively reduce the occurrence of PTSD [24,25]. However, social support was not an independent protective factor in this study. The reason may be that social support is already high. This study shows that CD-RISC score is a protective factor for the occurrence of PTSD in ICU nurses. The reason may be that the higher CD-RISC scores, the higher psychological resilience and the better overall resilience, and the less likely to choose avoidance in the face of stress or stressful events [26,27].
In conclusion, the incidence rate of PTSD was 22.38% among ICU nurses, and the occurrence of PTSD was associated with health status, years of work, age, CD-RISC score, and SSRS score, where MBI score was an independent risk factor and CD-RISC score was an independent protective factor for the occurrence of PTSD. The limitations are that the small sample size included may have an impact on the study results, and in-depth studies with larger samples are still needed in the future.
Disclosure of conflict of interest
None.
References
- 1.Caricato A, Melchionda I, Antonelli M. Continuous electroencephalography monitoring in adults in the intensive care unit. Crit Care. 2018;22:75. doi: 10.1186/s13054-018-1997-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartog CS, Hoffmann F, Mikolajetz A, Schröder S, Michalsen A, Dey K, Riessen R, Jaschinski U, Weiss M, Ragaller M, Bercker S, Briegel J, Spies C, Schwarzkopf D. Non-beneficial therapy and emotional exhaustion in end-of-life care: results of a survey among intensive care unit personnel. Anaesthesist. 2018;67:850–858. doi: 10.1007/s00101-018-0485-7. [DOI] [PubMed] [Google Scholar]
- 3.Mealer ML, Shelton A, Berg B, Rothbaum B, Moss M. Increased prevalence of post-traumatic stress disorder symptoms in critical care nurses. Am J Respir Crit Care Med. 2007;175:693–697. doi: 10.1164/rccm.200606-735OC. [DOI] [PubMed] [Google Scholar]
- 4.Waegemakers Schiff J, Lane AM. PTSD Symptoms, vicarious traumatization, and burnout in front line workers in the homeless sector. Community Ment Health J. 2019;55:454–462. doi: 10.1007/s10597-018-00364-7. [DOI] [PubMed] [Google Scholar]
- 5.Stanley IH, Hom MA, Chu C, Dougherty SP, Gallyer AJ, Spencer-Thomas S, Shelef L, Fruchter E, Comtois KA, Gutierrez PM, Sachs-Ericsson NJ, Joiner TE. Perceptions of belongingness and social support attenuate PTSD symptom severity among firefighters: a multistudy investigation. Psychol Serv. 2019;16:543–555. doi: 10.1037/ser0000240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calderón-de la Cruz GA, Merino-Soto C, Juárez-García A, Dominguez-Lara S, Fernández-Arata M. Is the factorial structure of the Maslach Burnout Inventory Human Service Survey (MBI-HSS) replicable in the nursing profession in Peru? A national study. Enferm Clin. 2020;30:340–348. doi: 10.1016/j.enfcli.2019.12.013. [DOI] [PubMed] [Google Scholar]
- 7.Tsigkaropoulou E, Douzenis A, Tsitas N, Ferentinos P, Liappas I, Michopoulos I. Greek Version of the Connor-Davidson resilience scale: psychometric properties in a sample of 546 subjects. In Vivo. 2018;32:1629–1634. doi: 10.21873/invivo.11424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang C, Zhao H, Zhu R, Lu J, Hou L, Yang XY, Yin M, Yang T. Improvement of social support in empty-nest elderly: results from an intervention study based on the Self-Mutual-Group model. J Public Health (Oxf) 2019;41:830–839. doi: 10.1093/pubmed/fdy185. [DOI] [PubMed] [Google Scholar]
- 9.Duncan LE, Ratanatharathorn A, Aiello AE, Almli LM, Amstadter AB, Ashley-Koch AE, Baker DG, Beckham JC, Bierut LJ, Bisson J, Bradley B, Chen CY, Dalvie S, Farrer LA, Galea S, Garrett ME, Gelernter JE, Guffanti G, Hauser MA, Johnson EO, Kessler RC, Kimbrel NA, King A, Koen N, Kranzler HR, Logue MW, Maihofer AX, Martin AR, Miller MW, Morey RA, Nugent NR, Rice JP, Ripke S, Roberts AL, Saccone NL, Smoller JW, Stein DJ, Stein MB, Sumner JA, Uddin M, Ursano RJ, Wildman DE, Yehuda R, Zhao H, Daly MJ, Liberzon I, Ressler KJ, Nievergelt CM, Koenen KC. Largest GWAS of PTSD (N=20070) yields genetic overlap with schizophrenia and sex differences in heritability. Mol Psychiatry. 2018;23:666–673. doi: 10.1038/mp.2017.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanchez M, Simon A, Ford D. PTSD in Tx ICU nurses. J Heart Lung Transplant. 2019;38:S93–S94. [Google Scholar]
- 11.Schuster M, Dwyer PA. Post-traumatic stress disorder in nurses: an integrative review. J Clin Nurs. 2020;29:2769–2787. doi: 10.1111/jocn.15288. [DOI] [PubMed] [Google Scholar]
- 12.Mealer M, Jones J, Moss M. A qualitative study of resilience and posttraumatic stress disorder in United States ICU nurses. Intensive Care Med. 2012;38:1445–1451. doi: 10.1007/s00134-012-2600-6. [DOI] [PubMed] [Google Scholar]
- 13.Mukherjee S, Tennant A, Beresford B. Measuring burnout in pediatric oncology staff: should we be using the maslach burnout inventory? J Pediatr Oncol Nurs. 2020;37:55–64. doi: 10.1177/1043454219873638. [DOI] [PubMed] [Google Scholar]
- 14.Guenette JP, Smith SE. Burnout: job resources and job demands associated with low personal accomplishment in United States radiology residents. Acad Radiol. 2018;25:739–743. doi: 10.1016/j.acra.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 15.Mealer M, Jones J, Newman J, McFann KK, Rothbaum B, Moss M. The presence of resilience is associated with a healthier psychological profile in intensive care unit (ICU) nurses: results of a national survey. Int J Nurs Stud. 2012;49:292–299. doi: 10.1016/j.ijnurstu.2011.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCabe CT, Mohr CD, Hammer LB, Carlson KF. PTSD symptomology and motivated alcohol use among military service members: testing a conditional indirect effect model of social support. Subst Use Misuse. 2019;54:257–270. doi: 10.1080/10826084.2018.1517176. [DOI] [PubMed] [Google Scholar]
- 17.Duagani Masika Y, Leys C, Matonda-Ma-Nzuzi T, Blanchette I, Mampunza Ma Miezi S, Kornreich C. Peritraumatic dissociation and post-traumatic stress disorder in individuals exposed to armed conflict in the Democratic Republic of Congo. J Trauma Dissociation. 2019;20:582–593. doi: 10.1080/15299732.2019.1597814. [DOI] [PubMed] [Google Scholar]
- 18.Goenjian AK, Khachadourian V, Armenian H, Demirchyan A, Steinberg AM. Posttraumatic stress disorder 23 years after the 1988 spitak earthquake in Armenia. J Trauma Stress. 2018;31:47–56. doi: 10.1002/jts.22260. [DOI] [PubMed] [Google Scholar]
- 19.O’Donnell J, Logan J, Bossarte R. Ten-year trend and correlates of reported posttraumatic stress disorder among young male veteran suicide decedents-results from the national violent death reporting system, 16 U.S. States, 2005-2014. Suicide Life Threat Behav. 2019;49:1473–1487. doi: 10.1111/sltb.12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hosseininejad SM, Jahanian F, Elyasi F, Mokhtari H, Koulaei ME, Pashaei SM. The prevalence of post-traumatic stress disorder among emergency nurses: a cross sectional study in Northern Iran. Biomedicine (Taipei) 2019;9:19. doi: 10.1051/bmdcn/2019090319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carmassi C, Gesi C, Corsi M, Cremone IM, Bertelloni CA, Massimetti E, Olivieri MC, Conversano C, Santini M, Dell’Osso L. Exploring PTSD in emergency operators of a major University Hospital in Italy: a preliminary report on the role of gender, age, and education. Ann Gen Psychiatry. 2018;17:17. doi: 10.1186/s12991-018-0184-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jung SJ, Winning A, Roberts AL, Nishimi K, Chen Q, Gilsanz P, Sumner JA, Fernandez CA, Rimm EB, Kubzansky LD, Koenen KC. Posttraumatic stress disorder symptoms and television viewing patterns in the Nurses’ Health Study II: a longitudinal analysis. PLoS One. 2019;14:e0213441. doi: 10.1371/journal.pone.0213441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim SJ, Yeo JH. Factors affecting posttraumatic stress disorder in South Korean trauma nurses. J Trauma Nurs. 2020;27:50–57. doi: 10.1097/JTN.0000000000000482. [DOI] [PubMed] [Google Scholar]
- 24.Okech D, Hansen N, Howard W, Anarfi JK, Burns AC. Social support, dysfunctional coping, and community reintegration as predictors of ptsd among human trafficking survivors. Behav Med. 2018;44:209–218. doi: 10.1080/08964289.2018.1432553. [DOI] [PubMed] [Google Scholar]
- 25.Braš M, Brajković L, Đorđević V, Pjevač N, Braš B. The role of PTSD in perception of health-related quality of life and social support among croatian war veterans. Psychiatr Danub. 2019;31:761–768. [PubMed] [Google Scholar]
- 26.Trip H, Tabakakis K, Maskill V, Richardson S, Dolan B, Josland H, McKay L, Richardson A, Cowan L, Hickmott B, Houston G. Psychological health and resilience: the impact of significant earthquake events on tertiary level professional students. A cross-sectional study. Contemp Nurse. 2018;54:319–332. doi: 10.1080/10376178.2018.1503549. [DOI] [PubMed] [Google Scholar]
- 27.Wolf EJ, Miller MW, Sullivan DR, Amstadter AB, Mitchell KS, Goldberg J, Magruder KM. A classical twin study of PTSD symptoms and resilience: evidence for a single spectrum of vulnerability to traumatic stress. Depress Anxiety. 2018;35:132–139. doi: 10.1002/da.22712. [DOI] [PMC free article] [PubMed] [Google Scholar]


