Abstract
Objective: To evaluate the effects of heat-sensitive moxibustion (HSM) combined with naprapathy and warming needle moxibustion (WNM) combined with naprapathy on shoulder function and serum levels of calcitonin gene-related peptide (CGRP), substance P (SP), tumor necrosis factor-α (TNF-α) and interleukin-2 (IL-2) in patients with periarthritis of shoulder (POS). Methods: From July 2017 to July 2020, sixty patients with POS admitted to our hospital were selected as the study subjects, and divided into HSM group (n=29) receiving HSM combined with naprapathy and WNM group receiving WNM combined with naprapathy (n=31). The changes in shoulder function, degrees of pain and serum levels of CGRP, SP, TNF-α and IL-2 were compared between the two groups. Results: After treatment, the scores of myodynamia, pain, range of motion (ROM) of shoulder joint and activities of daily living (ADLs) were improved in both groups (P<0.05), and the scores in HSM group were remarkably higher than those in WNM group (P<0.05). Visual analogue scale (VAS) scores after 3 courses of treatment were lower than those after 1 and 2 courses of treatment respectively (P<0.05), and the VAS scores in HSM group were markedly lower than those in WNM group after 1, 2, and 3 courses of treatment (P<0.05). After treatment, the serum levels of CGRP, SP, TNF-α and IL-2 were decreased in both groups (P<0.05), and the levels in HSM group were noticeably lower than those in WNM group (P<0.05). Conclusion: HSM combined with naprapathy is superior to WNM combined with naprapathy in inhibition of inflammatory factors of pain and serum inflammatory factors, alleviating the pain and promoting the restoration of shoulder function in patients with POS.
Keywords: Heat-sensitive moxibustion, warming needle moxibustion, naprapathy, periarthritis of shoulder, shoulder function, inflammatory factor
Introduction
Periarthritis of shoulder (POS) is a common disorder that causes reduced mobility and pain in the shoulder as a result of chronic inflammation of shoulder joint and its peripheral soft tissues induced by degenerative changes and acute and chronic strain in soft tissues around shoulder joint. The shoulder pain progressively worsens, and is obviously worse at night. In addition, protraction of shoulder pain occurs as it progresses, which may lead to dysfunction in daily activities, muscular atrophy, and even self-care incapability [1,2]. POS is highly prevalent in population aged 40-70 years, and is more common in young population [3].
Clinically, Western medicine treats POS with medication, surgeries and local block. Although the clinical symptoms can be improved, the expected efficacy cannot be achieved because of aggravated pain of patients induced by the long course of disease. Traditional Chinese medicine (TCM) believes that POS, also known as “frozen shoulder” and “omalgia”, belongs to “arthromyodynia”, and is induced by blockage of meridian and unsmooth circulation of Qi and blood as a result of strain, trauma or invasion of wind-cold damp pathogen. Multiple options for treatment of POS are available in TCM. Among them, acupuncture has been extensively implemented, showing a satisfactory efficacy. According to Prescriptions Worth a Thousand in Gold, “every disease ... blockage of Qi and blood ... should be treated with acupuncture”. According to Regulation of the Channels, “For regulation of blood and Qi ... temperature will dissipate it”. These suggest the importance of acupuncture in treatment of POS.
Acupuncture can be performed starting from freezing period to expand the range of motion (ROM) of shoulder joint, to relieve adhesion, and to restore joint motion function. Warming needle moxibustion (WNM) combined with naprapathy can transmit the heat generated by moxibustion to the body through the needle body, and give full play to the effects of moxibustion and acupuncture, thus treating POS [4]. Heat-sensitive moxibustion (HSM) is a novel option for the treatment of POS. During the acupuncture treatment, special moxibustion sensations (e.g., diathermancy, heat diffusion and transmission) occur, and the sensory transmission of acupuncture effects is noticeable, so as to achieve the clinical efficacy [5]. However, the comparative studies on the efficacies of HSM combined with naprapathy and WNM combined with naprapathy in the treatment of POS are rarely reported. In view of this, this study compared the effects of HSM combined with naprapathy and WNM combined with naprapathy on shoulder function, serum levels of calcitonin gene-related peptide (CGRP), substance P (SP), tumor necrosis factor-α (TNF-α) and interleukin-2 (IL-2) in patients with POS.
Materials and methods
General data
A total of 60 patients with POS admitted to our hospital from July 2017 to July 2020 were selected as the study subjects and divided into HSM group (n=29) and WNM group (n=31) according to the different therapeutic methods. Inclusion criteria: ① patients diagnosed as POS and in line with the diagnostic criteria for POS; ② those with excellent compliance, and ability to cooperate with the acupuncturist. Exclusion criteria: ① shoulder pain induced by traumatic fracture, pyoarthrosis, rheumatic arthritis, cervical spondylosis, and acute shoulder dislocation; ② those with cardiovascular and cerebrovascular disease and severe hepatic and renal dysfunction; ③ those with respiratory system diseases, hematological system diseases or malignant tumors; ④ those with allergic physique and acupuncture syncope; ⑤ recently treated with other options; ⑥ halfway withdrawal. This study has been approved by the Ethics Committee of Yichun People’s Hospital. All study participants provided written informed consent before participating in the study.
Methods
HSM group was treated with HSM combined with naprapathy. ① HSM: the scapular region and neck were selected as the heat-sensitive points, and meridian acupoints around the induration site, pressure pain points, and lesion sites were selected as the warming moxibustion center. The warming moxibustion with a diameter of 6 cm was performed for 2 min at a distance of 4 cm from the skin, followed by circling moxibustion for 2 min. Subsequently, birdpecking moxibustion was carried out to enhance the sensitization for 1 min. Next, round-trip meridian moxibustion was performed to stimulate pneuma, and warming moxibustion was conducted to stimulate sensory transmission. The characteristics of heat-sensitive acupoints were that local heat was lower than distant heat, surface heat was lower than the deep heat, and the sensations (numbness, swelling, aching and pain) occurred at the moxibustion (or non-moxibustion) sites. A total of 2 or 3 heat-sensitive acupoints were selected for suspended moxibustion at the specific acupoints. ② Naprapathy: a. Gentle manipulation for relaxation: the patients were required in the sitting position, and the physician gently manipulated the shoulder with the palm for 3-5 times, manipulated the shoulder using the rolling manipulation for 5-10 min, and then kneaded the upper arm and shoulder using multiple fingers for several minutes. b. Plucking and acupressure: the physician stood behind the patient, sought the pain spots through kneading and pushing the muscle groups in the neck and shoulder using the two thumbs, and plucked away the adhesions at the cord-like adhesion using the thumb plucking technique. After a few minutes, acupressure was applied on acupoints (e.g., t’ien tsung, supraclavicular fossa, shoulder well, watching wind, wind pond and upright shoulder). c. Motion of the shoulder joint: the adduction was recommended, and the affected arm was anteflexed. The patients were told to place their palms down and put their hands on the contralateral shoulder. The physician held the affected elbow with one hand, pushed and pressed the healthy shoulder with the other hand, and pulled the affected elbow toward the healthy shoulder. After rotation, the shoulder was kneaded, the affected arm was extended backward, and the elbow was bent, with the center of the palm towards the physician. The physician pulled the shoulder upward while kneading and pressing the shoulder with one hand, and pulled the wrist with the other hand. The shoulder joint was rotated. The physician held the elbow joint with one hand, rotated it clockwise and counterclockwise for 5 times respectively, with the other hand on the affected shoulder. The ROM of shoulder joint was increased gradually with patients’ tolerability. d. Patting, pulling and shaking: the physician conducted patting from the shoulder to anterior wall using an empty fist or two-handed staff, rubbed and shook the shoulder several times, and kneaded the shoulder with multiple fingers.
WNM group was treated with WNM combined with naprapathy. WNM: the acupoints (e.g., shoulder crevice, shoulder blade, Jianqian, upright shoulder, shoulder well, huge bone, and medial side of upper arm) were selected as principal acupoints, and the matching acupoints (e.g., narrow mouth, yang ming meridians and connected valleys, zhongping, outer pass, quchi, tai yang meridian and back stream) were selected according to the channel and the sites of pain spots. The acupuncture needle (0.30 mm × 50 mm) was applied in the principal and matching acupoints, the needles was retained for 30 min after the desired sensation was brought about, and moxa stick (1 cm) was used at the needle end for moxibustion. Naprapathy was the same as that in HSM group.
Three times were a course of treatment, and the two groups received three courses of treatment.
Observational indices
① Shoulder function was evaluated by Constant-Murley score [6]. Constant-Murley includes myodynamia (25 points), pain (15 points), ROM of shoulder joint (40 points) and activities of daily living (ADLs) (20 points). A higher score indicated a better restoration of shoulder function.
② Degree of pain was evaluated by visual analogue scale (VAS) [7]. VAS scoring criteria: 0 point indicates painless and 10 points indicate the most severe pain.
③ A total of 5 mL of fasting venous blood was collected at admission (before treatment) and after three courses of treatment, and centrifuged at 3500 rpm/min for 5 min, and the supernatant blood was taken for testing. The serum levels of CGRP, SP, TNF-α, and IL-2 were detected by the enzyme-linked immunosorbent assay (ELISA).
Statistical method
All data were processed by SPSS22.0. The enumeration data were represented by (n, %), and detected using χ2 test. The measurement data were represented by (x̅ ± s). The comparison between groups was detected using the independent sample t test, and the comparison within groups was detected using the paired t test. The comparisons at different time points were performed using analysis of variance (ANOVA) of repeatedly measured data, so as to analyze the differences between groups and the time differences of values measured at the time points. Subsequently, the least significant difference (LSD) t-test was performed. Graphpad prism 8 was adopted for statistical charts. P<0.05 indicated a statistically significant difference.
Results
Baseline data
HSM group had 29 patients, including 16 males and 13 females in, with a mean age of (55.54±8.56) years, while WNM group had 31 patients, including 18 males and 13 females, with a mean age of (54.43±9.66) years. There was no marked difference in baseline data [e.g., age, body mass index (BMI), gender, course of disease, and lesion sites] between the two groups (P<0.05) (Table 1).
Table 1.
Comparison of baseline treatment between the two groups (x̅ ± s; n, %)
| Groups | Number of cases | Age | BMI (kg/m2) | Gender | Course of disease (weeks) | Lesion site | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Male | Female | Left shoulder | Right shoulder | Shoulders | |||||
| HSM group | 29 | 55.54±8.56 | 22.45±1.04 | 16 (55.17) | 13 (44.83) | 33.26±7.95 | 13 (44.83) | 14 (48.28) | 2 (6.9) |
| WNM group | 31 | 54.43±9.66 | 22.72±1.54 | 18 (58.06) | 13 (41.94) | 32.56±8.62 | 14 (45.16) | 16 (51.61) | 1 (3.23) |
| t value | 0.838 | 1.416 | 0.051 | 0.582 | 0.033 | ||||
| P value | 0.403 | 0.158 | 0.821 | 0.561 | 0.855 | ||||
Restoration of shoulder function
Before treatment, there was no remarkable difference in scores of myodynamia, pain, ROM of shoulder joint and ADLs between the two groups (P>0.05). After treatment, the scores of myodynamia, pain, ROM of shoulder joint and ADLs were elevated in both groups (P<0.05), and the scores in HSM group [(22.34±1.18), (12.32±1.38), (35.84±1.62), and (17.46±1.67)] were noticeably higher than those in WNM group [(18.39±2.14), (9.46±1.53), (30.15±3.65), and (15.43±2.21)] (P<0.05) (Table 2).
Table 2.
Comparison of Constant-Murley scores between the two groups before and after treatment (x̅ ± s)
| Groups | Time points | Myodynamia | Pain | ROM of shoulder joint | ADLs |
|---|---|---|---|---|---|
| HSM group (n=29) | Before treatment | 15.97±2.35 | 7.38±2.09 | 24.61±4.64 | 12.32±2.45 |
| After treatment | 22.34±1.18 | 12.32±1.38 | 35.84±1.62 | 17.46±1.67 | |
| t a value | 13.045 | 10.622 | 12.305 | 9.335 | |
| P a value | <0.001 | <0.001 | <0.001 | <0.001 | |
| WNM group (n=31) | Before treatment | 15.93±2.39 | 7.35±2.11 | 23.89±4.56 | 12.37±2.49 |
| After treatment | 18.39±2.14 | 9.46±1.53 | 30.15±3.65 | 15.43±2.21 | |
| t a value | 4.269 | 4.507 | 5.967 | 5.117 | |
| P a value | <0.001 | <0.001 | <0.001 | <0.001 | |
| t b value | 0.065 | 0.055 | 0.606 | 0.078 | |
| P b value | 0.948 | 0.956 | 0.547 | 0.938 | |
| t c value | 8.768 | 7.585 | 7.711 | 3.993 | |
| P c value | <0.001 | <0.001 | <0.001 | <0.001 | |
Note: t a and P a indicate the comparison within groups, t b and P b indicate the comparison before treatment, and t c and P c indicate the comparison after treatment.
Degrees of pain
The repeated measurements showed that there were marked differences in VAS scores between groups at different time points, and the interactions of time points and between groups were significantly different (P<0.05). The LSD-t test suggested that there were significant differences in VAS scores between the two groups before treatment (P>0.05). The comparison of VAS scores between groups revealed that VAS scores after 3 courses of treatment were lower than those after 2 courses of treatment and those after 1 course of treatment (P<0.05), and the VAS scores in HSM group were notably lower than those in WNM group after 1, 2, and 3 courses of treatment (P<0.05) (Table 3 and Figure 1).
Table 3.
Comparison of VAS scores between the two groups at different time points (x̅ ± s)
| Groups | Number of cases | Before treatment | 1 course of treatment | 2 courses of treatment | 3 courses of treatment | Ftime points | Fbetween groups | Finteraction |
|---|---|---|---|---|---|---|---|---|
| HSM group | 29 | 6.45±0.74 | 3.21±0.62a | 1.55±0.51a,b | 0.93±0.26a,b,c | 1002.7413 | 186.851 | 108.331 |
| WNM group | 31 | 6.45±0.81 | 5.65±0.71a | 4.23±0.56a,b | 2.23±0.43a,b,c | |||
| t value | 0.015 | 14.174 | 19.377 | 14.076 | ||||
| P value | 0.987 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.608 |
Note: compared with before treatment;
P<0.05.
Compared with one course of treatment;
P<0.05.
Compared with two courses of treatment;
P<0.05.
Figure 1.
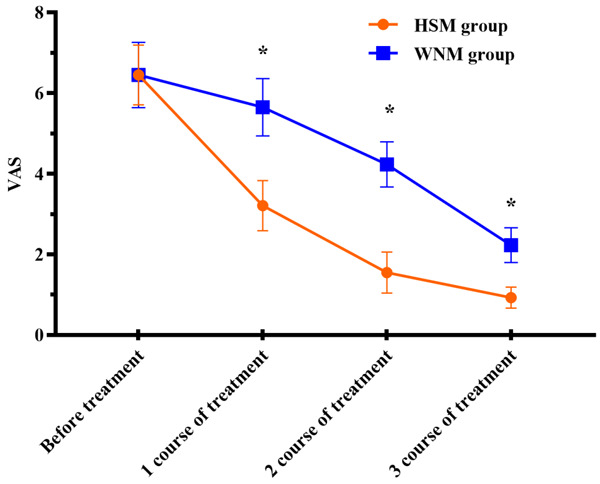
Comparison of VAS scores between the two groups at different time points. There was no remarkable difference in VAS scores between the two groups before treatment (P>0.05). The VAS scores in HSM group were notably lower than those in WNM group after 1, 2, and 3 courses of treatment (P<0.05). *indicates the comparison between the two groups at the same time points (P<0.05).
The serum levels of CGRP, SP, TNF-α and IL-2
There was no significant difference in the serum levels of CGRP, SP, TNF-α, and IL-2 between the two groups before treatment (P<0.05). After treatment, the serum levels of CGRP, SP, TNF-α and IL-2 were reduced in the two groups (P<0.05), and the levels in HSM group [(78.68±10.49) ng/L, (68.42±8.83) ng/mL, (26.11±5.67) pg/mL, and (107.52±15.65) pg/mL] were noticeably lower than those in WNM group [(137.61±18.95) ng/L, (159.85±13.58) ng/mL, (32.62±6.68) pg/mL, and (155.43±22.17) pg/mL] (P<0.05) (Table 4, Figures 2, 3, 4 and 5).
Table 4.
Comparison of the serum levels of CGRP, SP, TNF-α and IL-2 between the two groups before and after treatment (x̅ ± s)
| Groups | Time points | CGRP (ng/L) | SP (ng/mL) | TNF-α (pg/mL) | IL-2 (pg/mL) |
|---|---|---|---|---|---|
| HSM group (n=29) | Before treatment | 285.47±23.23 | 312.61±20.38 | 42.51±8.02 | 641.36±144.43 |
| After treatment | 78.68±10.49 | 68.42±8.83 | 26.11±5.67 | 107.52±15.65 | |
| t a value | 43.69 | 59.206 | 8.992 | 19.789 | |
| P a value | <0.001 | <0.001 | <0.001 | <0.001 | |
| WNM group (n=31) | Before treatment | 284.32±23.11 | 313.41±20.09 | 43.21±7.96 | 642.31±140.43 |
| After treatment | 137.61±18.95 | 159.85±13.58 | 32.62±6.68 | 155.43±22.17 | |
| t a value | 27.332 | 35.258 | 5.674 | 19.068 | |
| P a value | <0.001 | <0.001 | <0.001 | <0.001 | |
| t b value | 0.192 | 0.153 | 0.339 | 0.026 | |
| P b value | 0.848 | 0.879 | 0.736 | 0.979 | |
| t c value | 14.759 | 30.685 | 4.056 | 9.609 | |
| P c value | <0.001 | <0.001 | <0.001 | <0.001 | |
Note: compared with before treatment;
P<0.05.
Compared with one course of treatment;
P<0.05.
Compared with two courses of treatment;
P<0.05.
Figure 2.
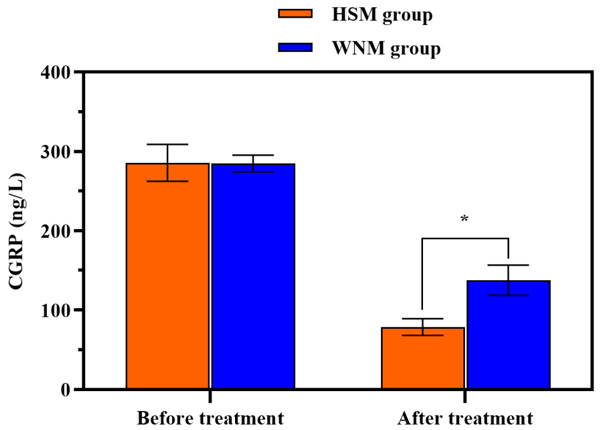
Comparison of CGRP levels between the two groups before and after treatment. There was no marked difference in the CGRP levels between the two groups before treatment (P>0.05), and the CGRP levels in HSM group were notably lower than those in WNM group after treatment (P<0.05). *indicates the comparison between the two groups (P<0.05).
Figure 3.
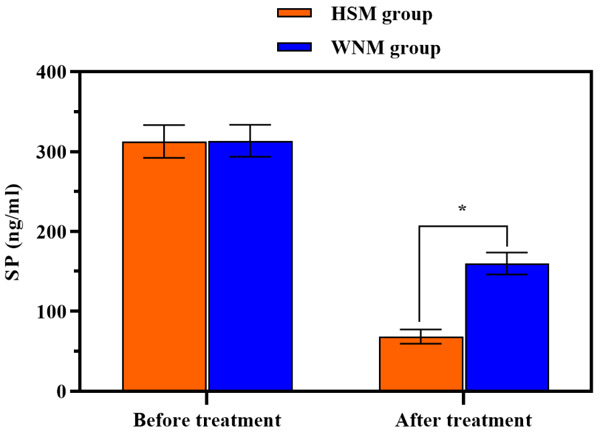
Comparison of SP levels between the two groups before and after treatment. There was no noticeable difference in the SP levels between the two groups before treatment (P>0.05), and the SP levels in HSM group were significantly lower than those in WNM group after treatment (P<0.05). *indicates the comparison between the two groups (P<0.05).
Figure 4.
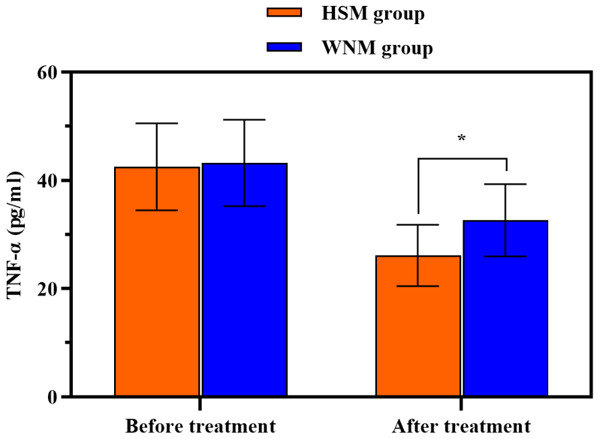
Comparison of TNF-α levels between the two groups before and after treatment. There was no remarkable difference in the TNF-α levels between the two groups before treatment (P>0.05), and the TNF levels in HSM group were notably lower than those in WNM group after treatment (P<0.05). *indicates the comparison between the two groups (P<0.05).
Figure 5.
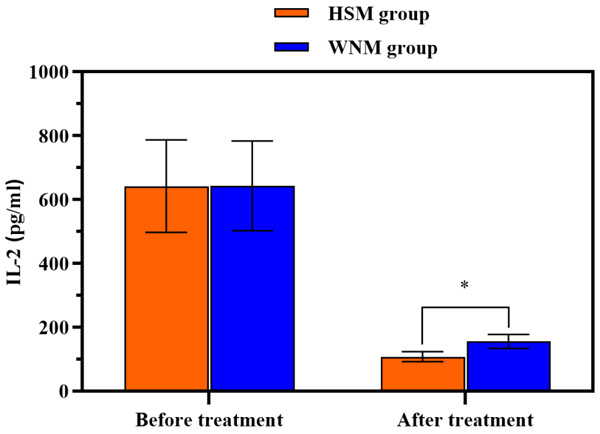
Comparison of IL-2 levels between the two groups before and after treatment. There was no noticeable difference in the IL-2 levels between the two groups before treatment (P>0.05), and the IL-2 levels in HSM group were markedly lower than those in WNM group after treatment (P<0.05). *indicates the comparison between the two groups (P<0.05).
Discussion
According to TCM, the occurrence of POS is due to insufficient nourishment of blood and Qi-stagnancy and blood stasis in tendon and vessel induced by meridians invaded by wind cold caused by exogenous pathogenic factor in the shoulder. Therefore, it is necessary to dredge the meridians, activate blood circulation, and dispel cold and remove dampness. Acupuncture can stimulate meridians to improve local blood circulation, thus promoting Qi to activate blood and dredge meridians and collaterals. Naprapathy is a TCM option used to treat diseases by clicking, pinching, kneading, patting, pushing, and pressing, and can dredge meridians, promote the circulation of Qi and blood, regulate Yin and Yang, heal the wounded and relieve pain, and eliminate pathogen to support vital qi [8]. WNM can transfer the heat generated by moxa stick and moxibustion through the needle body to muscle for exudation, and has the function of warming Yang and dispelling cold, dispersing blood stasis and dredging collaterals, thus strengthening blood circulation, promoting tissue metabolism and alleviate patients’ pain [9,10]. HSM can promote the conduction and circulation of meridian Qi through stimulating the sensory transmission of meridian Qi, so that sensitized acupoints can have “a big response” to a small exogenous stimulus, thereby warming meridians and dispelling cold, dispersing blood stasis and eliminating stagnation, and tonifying healthy Qi. This study compared the efficacies of HSM combined with naprapathy and WNM combined with naprapathy in the treatment of POS, and the results suggested that HSM combined with naprapathy demonstrated a more satisfactory efficacy [11].
In this study, the scores of myodynamia, pain, ROM of shoulder joint and ADLs were improved in the two groups after treatment, and the aforementioned scores in HSM group were remarkably higher than those in WNM group, suggesting that HSM combined with naprapathy was superior to WNM combined with naprapathy in improving shoulder function. This can be attributed to the reason that HSM can induce six special moxibustion sensations: a. diathermancy, namely, patients can feel a continuous stream of heat flow penetrating into the body and reaching the internal organs; b. heat transmission, namely, patients can feel that heat is primarily transmitted along the meridians to other places at the moxibustion site; c. heat diffusion, namely, patients feels that the heat is diffused around the moxibustion site; d. patients do not feel local heat at the moxibustion site, but feel heat at the distant site; e. patients do not feel heat on the skin surface at the moxibustion site, but feel heat at the deep site; f. patients have sensations (e.g., numbness, swelling, and aching). During the HSM, patients have the aforementioned moxibustion sensations (i.e., heat sensitivity), which can improve the efficacy and remarkably restore shoulder function.
Studies suggest that patients with POS experience abnormal local inflammatory responses and an unbalanced expression of inflammatory factors [12,13]. CGRP, an endogenous vasodilator material, has the strongest effect and is related to pain reaction [14]. A study reveals that healthy people have a low content of CGRP, the release of a large amount of CGRP leads to the transmission of pain information, and CGRP is related to neuropathologic pain [15]. In addition, CGRP can promote the release of SP and enhance the activity of SP, while SP can induce and transmit pain, and the release of SP is closely related to local neurogenic inflammation [16,17]. TNF-α, secreted by monocytes, can aggravate local inflammatory reactions [18]. IL-2, a pro-inflammatory T cell mainly generated in Th1 cells, can enhance the immune response of cells and activate macrophages. Studies demonstrate that IL-2 is related to inflammation [19,20]. In this study, the serum levels of CGRP, SP, TNF-α, and IL-2 were decreased in the two groups after treatment, and the aforementioned levels in HSM group were noticeably lower than those in WNM group. The results exhibited that HSM combined with naprapathy was superior to WNM combined with naprapathy in improving inflammatory factors of pain and serum inflammatory factors. The VAS scores were decreased with time in the two groups, and the VAS scores in HSM group were significantly lower than those in WNM group after different courses of treatment. Moreover, HSM combined with naprapathy could more effectively alleviate the pain of patients with POS through inhibition inflammatory factors of pain.
In summary, HSM combined with naprapathy is superior to WNM combined with naprapathy in improving the serum levels of CGRP, SP, TNF-α, and IL-2, inhibiting inflammatory factors of pain and serum inflammatory factors, alleviating the pain, and promoting the restoration of shoulder function in patients with POS. However, due to the small sample size, the observation duration of only three courses of treatment, and the short-term follow-ups, no long-term efficacy was obtained. Therefore, the future studies with a larger sample size and a longer duration for follow-ups should be performed, so as to further investigate the long-term efficacy.
Disclosure of conflict of interest
None.
References
- 1.Schiefer M, Teixeira PFS, Fontenelle C, Carminatti T, Santos DA, Righi LD, Conceição FL. Prevalence of hypothyroidism in patients with frozen shoulder. J Shoulder Elbow Surg. 2017;26:49–55. doi: 10.1016/j.jse.2016.04.026. [DOI] [PubMed] [Google Scholar]
- 2.Stütz T, Emsenhuber G, Huber D, Domhardt M, Tiefengrabner M, Oostingh GJ, Fötschl U, Matis N, Ginzinger S. Mobile phone-supported physiotherapy for frozen shoulder: feasibility assessment based on a usability study. JMIR Rehabil Assist Technol. 2017;4:e6. doi: 10.2196/rehab.7085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu WT, Chang KV, Han DS, Chang CH, Yang FS, Lin CP. Effectiveness of glenohumeral joint dilatation for treatment of frozen shoulder: a systematic review and meta-analysis of randomized controlled trials. Sci Rep. 2017;7:10507. doi: 10.1038/s41598-017-10895-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woo HL, Ji HR, Pak YK, Lee H, Heo SJ, Lee JM, Park KS. The efficacy and safety of acupuncture in women with primary dysmenorrhea: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e11007. doi: 10.1097/MD.0000000000011007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang H, Xie F, Gong H, Huang H, Chen S, Kang M, Fu Y. Effects of heat-sensitive moxibustion on HPA axis in rats with irritable bowel syndrome. Zhongguo Zhen Jiu. 2017;37:1315–1321. doi: 10.13703/j.0255-2930.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 6.Merolla G, Parel I, Cutti AG, Filippi MV, Paladini P, Porcellini G. Assessment of anatomical and reverse total shoulder arthroplasty with the scapula-weighted Constant-Murley score. Int Orthop. 2019;43:659–667. doi: 10.1007/s00264-018-4088-3. [DOI] [PubMed] [Google Scholar]
- 7.Nemade SV, Shinde KJ. Clinical efficacy of tinnitus retraining therapy based on tinnitus questionnaire score and visual analogue scale score in patients with subjective tinnitus. Turk Arch Otorhinolaryngol. 2019;57:34–38. doi: 10.5152/tao.2019.3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stein DJ. Massage acupuncture, moxibustion, and other forms of complementary and alternative medicine in inflammatory bowel disease. Gastroenterol Clin North Am. 2017;46:875–880. doi: 10.1016/j.gtc.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Chen B, Zhang G, Liu C, Chen Q, Zhang M, Li J, Zhou P, Fu W, Zhu M. Effectiveness and safety of warm needle acupuncture on insomnia: protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e13598. doi: 10.1097/MD.0000000000013598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen LA, Liu HT, Huang C, Zhang L, Zeng F, Xie B. Effectiveness and safety of warm needle acupuncture on children with cerebral palsy: protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e14959. doi: 10.1097/MD.0000000000014959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiao L, Chi ZH, Chen RX. Discussion on the enlightenment of heat-sensitive moxibustion technology to acupuncture clinic: dynamically grasping the state of acupoints, on-demand treatment are the key to achieving clinical efficacy. Zhongguo Zhen Jiu. 2019;39:54–58. doi: 10.13703/j.0255-2930.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Cho CH, Lho YM, Hwang I, Kim DH. Role of matrix metalloproteinases 2 and 9 in the development of frozen shoulder: human data and experimental analysis in a rat contracture model. J Shoulder Elbow Surg. 2019;28:1265–1272. doi: 10.1016/j.jse.2018.11.072. [DOI] [PubMed] [Google Scholar]
- 13.Whelton C, Peach CA. Review of diabetic frozen shoulder. Eur J Orthop Surg Traumatol. 2018;28:363–371. doi: 10.1007/s00590-017-2068-8. [DOI] [PubMed] [Google Scholar]
- 14.Lu CX, Qiu T, Liu ZF, Su L, Cheng B. Calcitonin gene-related peptide has protective effect on brain injury induced by heat stroke in rats. Exp Ther Med. 2017;14:4935–4941. doi: 10.3892/etm.2017.5126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh Y, Gupta G, Shrivastava B, Dahiya R, Tiwari J, Ashwathanarayana M, Sharma RK, Agrawal M, Mishra A, Dua K. Calcitonin gene-related peptide (CGRP): a novel target for Alzheimer’s disease. CNS Neurosci Ther. 2017;23:457–461. doi: 10.1111/cns.12696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.N’Diaye A, Gannesen A, Borrel V, Maillot O, Enault J, Racine PJ, Plakunov V, Chevalier S, Lesouhaitier O, Feuilloley MG. Substance P and calcitonin gene-related peptide: key regulators of cutaneous microbiota homeostasis. Front Endocrinol (Lausanne) 2017;8:15. doi: 10.3389/fendo.2017.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yan D, Liu X, Guo SW. Neuropeptides substance P and calcitonin gene related peptide accelerate the development and fibrogenesis of endometriosis. Sci Rep. 2019;9:2698. doi: 10.1038/s41598-019-39170-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alawieyah Syed Mortadza S, Sim JA, Neubrand VE, Jiang LH. A critical role of TRPM2 channel in Aβ(42) -induced microglial activation and generation of tumor necrosis factor-α. Glia. 2018;66:562–575. doi: 10.1002/glia.23265. [DOI] [PubMed] [Google Scholar]
- 19.Kanagalingam T, Solomon L, Vijeyakumaran M, Palikhe NS, Vliagoftis H, Cameron L. IL-2 modulates Th2 cell responses to glucocorticosteroid: a cause of persistent type 2 inflammation? Immun Inflamm Dis. 2019;7:112–124. doi: 10.1002/iid3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roy U. Structure and function of an inflammatory cytokine, interleukin-2, analyzed using the bioinformatic approach. Protein J. 2019;38:525–536. doi: 10.1007/s10930-019-09833-8. [DOI] [PubMed] [Google Scholar]


