Abstract
Objective: To study effect of joint distraction osteogenesis combined with platelet-rich plasma injections on traumatic ankle arthritis (TAA). Methods: 106 patients with TAA admitted to our hospital (from January 2018 to January 2020) were recruited as the study cohort and randomly divided into a surgical group and a combined group. The surgical group was treated with simple joint retraction surgery, and the combined group was treated with platelet-rich plasma injections in addition to the surgery administered to the operation group. After 6 months of treatment, the clinical efficacy of the two groups was evaluated, and the changes in the ankle joint function, the serum related factors, and the quality of life before and at six months after the treatment were observed. The incidences of adverse reactions (ARS) in the two groups were counted to evaluate the treatment safety. Results: The total effective rate was 98.11% in the combined group and 77.36% in the operation group. The overall curative effect of the combined group was better than it was in the operation group (P<0.05). After the treatment, the ankle joint movement angles, the joint function, the serum factor levels, and the quality of life of the patients in combined group were better than they were in the operation group (P<0.05). No significant difference was found in the incidence of ARs (P>0.05). Conclusion: Arthroplasty with platelet-rich plasma injections can improve joint function recovery, inhibit the inflammatory factor expression levels, and enhance TAA patients’ quality of life.
Keywords: Traumatic arthritis, ankle joint, arthroplasty of joint retraction, platelet rich plasma injections
Introduction
The ankle joint is composed of the joint surfaces of the tibia, fibula, and talus trochlea, and it is an important weightbearing joint in the human body [1,2]. Traumatic ankle arthritis (TAA) is a degenerative disease of the ankle cartilage induced by trauma, and it can progress to cartilage hyperplasia and ossification [3,4]. Conservative treatment is ineffective for TAA. At present, TAA is mainly treated surgically, and ankle arthroplasty is a common clinical operation [5,6]. Over of clinical practice, it has been proved that TAA can cause some problems such as partial loss of function and the early degeneration of the adjacent joints. The post-surgical clinical effectiveness among females is lower than it is among males, and ankle arthritis may progress over the long term after the operation. Therefore, to a certain extent, it limits the curative effect of simple ankle arthroplasty. In recent years, platelet-rich plasma (PRP) injections have achieved good clinical effectiveness in knee osteoarthritis [7,8]. Therefore, ankle arthroplasty combined with platelet-rich plasma (PRP) injections has been gradually popularized in TAA in clinical practice. PRP injections refer to a treatment scheme in which autologous whole blood is centrifuged to obtain a platelet-rich concentrate, and it is administered through injections. PRP injections can promote cartilage formation and repair cartilage damage and can make up for the deficiency of the surgical treatment when it is used in the auxiliary treatment of ankle arthroplasty. In order to objectively evaluate the specific efficacy and safety of PRP injections, this study was carried out in our hospital.
Materials and methods
General information
106 patients with TAA admitted in our hospital were recruited as the study cohort. The patients were randomly divided into a surgical group and a combined group, with 53 patients in each group. Inclusion criteria: (1) Patients who meet the diagnostic criteria for TAA [9]. (2) Patients with a range of motion in the ankle joint of less than 20°. (3) Patients whose treatment was ineffective after conservative treatment for more than six months and who met the adaptation scope and requirements for ankle arthroplasty. (4) Patients who met the requirements for PRP injection. (5) Patients who voluntarily joined the group and who signed informed consent. This study was approved by the ethics committee of our hospital. Exclusion criteria: (1) Patients with an allergic constitution. (2) Patients with blood system diseases, anemia, and a hypercoagulable state. (3) Patients with acute ankle arthritis. (4) Patients with immune dysfunction. (5) Patients with a history of cardiovascular or cerebrovascular diseases. (6) Patients with an original physical disability. (7) Patients with cognitive dysfunction, psychiatric diseases, or communication disorders. (8) Patients with malignant bone tumors or severe osteoporosis.
Methods
Surgical group
The patients were treated with simple ankle arthroplasty. Each patient was placed in a supine position and operated on under general anesthesia. 10 ml of sodium chloride was injected into the medial tibialis anterior tendon and the ankle joint of the third fibula muscle. An incision of about 5 mm was made, and the subcutaneous tissue was incised, then an arthroscope was inserted, and the hyperplastic tissue and osteophyte of the affected ankle joint were removed under the arthroscopic display system. Following that, the foot ring, ankle hinge, and tibial reference ring were installed step by step. The medical staff then confirmed that the ankle joint moved normally without joint subluxation, took out the arthroscope, and sealed the wound. After the operation, the ankle joint was stretched at a speed of 0.5 mm/d until the joint space reached 5 mm. After three months’ treatment, the patient could walk with full weight.
Combination group
Arthroplasty combined with PRP injection was administered. The operation method was completely consistent with the operation group. For the PRP injections, 5 ml of PRP preparation solution (produced by Shanghai Xinfan Biotechnology Co., Ltd.) was used. Before the arthroplasty of the joint retraction, 45 ml of venous blood was taken, and the venous blood was centrifuged at 2000 r/min for 10 min and repeated once. After the operation, the prepared PRP was injected into the affected ankle. The PRP injections were repeated at four weeks and 12 weeks after the operations.
Observation indexes
After six months of treatment, the clinical efficacy of the two groups was evaluated. The changes in ankle joint function, the serum factors, and the quality of life before and at 6 months after the treatment were observed, and the incidence of ARs was counted to evaluate the treatment safety.
The ankle joint function evaluation indexes include: range of motion, dorsiflexion angle, foot and ankle scale (AAOS), the Berg balance scale (BBS) scores, and the short-form Mai-Ji pain questionnaire (SF-MPQ) scores [10]. The AAOS scale includes three aspects: lower limb core score, full ankle score, and shoe comfort. The scale covers 34 items, and each item ranges from 1-7 points. The higher the score, the better the function is improved. The BBS scores ranged from 0 to 56, and the higher the score, the better the balance function. The SF-MPQ questionnaire includes 14 items, and each item is scored from 0 to 3 points. The higher the score, the more serious the pain.
Serum related factors: PGE2, TNF-α, and IL-6. Before and after the treatment, 3 ml fasting venous blood samples were collected from all the patients, and the serum was obtained by centrifugation at a speed of 3000 r/min for 10 min. The serum was measured using ELISA, and the operational steps were performed according to the kit instructions.
The quality of life was evaluated using the SF-36 Quality of Life Scale [11]. The SF-36 scale includes four aspects: physical activity, psychological function, social function, and material life.
The clinical efficacy was evaluated according to the standards established in the medical literature [12]. Specific criteria: the ankle joint function is completely or basically normal, and one is clearly able to walk with full weight. The ankle joint function has been improved, and it is basically effective to walk with full weight. The ankle joint symptoms have not improved or have progressed, and the patient is unable to walk. The total effectiveness is the sum of effectiveness and effectiveness.
Statistical analysis
SPSS 21.0 was used. Rank sum tests were done for the grade data, Chi-square tests were used for the count data and were expressed as [n (%)]. The measurement data were tested using t-tests and expressed as (x̅±s).
Results
General data
31 males and 22 females were included in the operation group (21-39 years old), with an average age of 30.46±5.63 years old. Affected side: the left side in 21 cases and the right side in 32 cases. There were 32 males and 21 females in the combined group (21-42 years old), with an average age of 31.02±6.11 years old. Affected side: 20 cases on the left and 33 cases on the right side. See Table 1.
Table 1.
The general data of the two groups
| Group | n | Sex (Male/Female) | Age (years) | Affected side (Left/Right) |
|---|---|---|---|---|
| Surgical group | 53 | 31/22 | 30.46±5.63 | 21/32 |
| Combination group | 53 | 32/21 | 31.02±6.11 | 20/33 |
| χ2/t | 0.039 | 0.491 | 0.040 | |
| P | 0.843 | 0.625 | 0.842 |
Clinical efficacy
The total effective rate was 98.11% in the combined group and 77.36% in the surgical group. The total effective rate in the combination group was higher than it was in the operation group (P<0.05), and the overall clinical effectiveness was better than it was in the operation group (P<0.05). See Table 2.
Table 2.
Comparison of the clinical efficacy between the two groups n (%)
| Group | n | Significantly effective | Effective | Invalid | Total effective rate |
|---|---|---|---|---|---|
| Surgical group | 53 | 22 (41.51) | 19 (35.85) | 12 (22.64) | 41 (77.36) |
| Combination group | 53 | 35 (66.04) | 17 (32.08) | 1 (1.89) | 52 (98.11) |
| Z/x2 | -3.080 | 10.609 | |||
| P | 0.002 | 0.001 |
Movement angle of the ankle joint
After the treatment, the dorsiflexion and plantarflexion angles of the ankle joint in the combined group were larger than they were in the operation group (P<0.05). See Figure 1.
Figure 1.
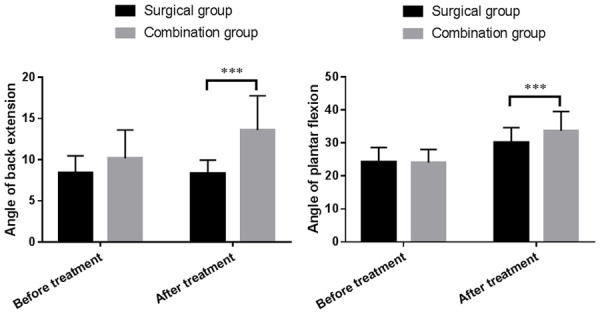
Comparison of the ankle joint movement angles between the two groups before and after treatment. The dorsiflexion angle (left) and plantarflexion angle. *** indicates P<0.001.
Ankle joint function
After the treatment, the BBS and AAOS scores in the combined group were higher than they were in the operation group, and the SF-MPQ scores were lower than they were in the operation group (P<0.05). See Table 3.
Table 3.
Comparison of the ankle function evaluations between the two groups before and after treatment (x̅ ± s)
| Group | Time | BBS | AAOS | SF-MPQ |
|---|---|---|---|---|
| Surgical group | Before treatment | 29.37±2.93 | 54.12±7.28 | 30.85±5.40 |
| n=53 | After treatment | 41.09±4.28 | 182.76±14.13 | 15.27±3.06 |
| Combination group | Before treatment | 29.31±2.49 | 53.22±5.98 | 31.52±5.67 |
| n=53 | After treatment | 50.38±5.51 | 198.06±16.23 | 10.07±1.72 |
| Before treatment | t | 0.099 | 0.695 | 0.623 |
| p | 0.922 | 0.488 | 0.534 | |
| After treatment | t | 9.688 | 5.175 | 10.777 |
| p | <0.001 | <0.001 | <0.001 |
Serum factor levels
After the treatment, the serum PGE2, TNF-α, and IL-6 levels in the combined group were lower than they were in the surgical group (P<0.05). See Table 4.
Table 4.
Comparison of the ankle function evaluation between the two groups before and after treatment (x̅ ± s)
| Group | Time | PGE2 (pg/ml) | TNF-α (ng/ml) | IL-6 (μg/ml) |
|---|---|---|---|---|
| Surgical group | Before treatment | 456.85±22.49 | 554.38±13.64 | 65.14±9.45 |
| n=53 | After treatment | 187.01±17.47 | 452.35±14.36 | 51.17±6.62 |
| Combination group | Before treatment | 457.57±28.00 | 555.49±13.87 | 65.91±8.86 |
| n=53 | After treatment | 142.12±15.49 | 407.75±12.70 | 45.53±5.71 |
| Before treatment | t | 0.148 | 0.414 | 0.433 |
| p | 0.883 | 0.680 | 0.666 | |
| After treatment | t | 13.996 | 16.940 | 4.693 |
| p | <0.001 | <0.001 | <0.001 |
Quality of life
After the treatment, the physical activity, psychological function, and social function scores in the combined group were higher than they were in the operation group (P<0.05), but there were no significant differences in the material life scores between the two groups (P>0.05). See Table 5.
Table 5.
Comparison of the SF-36 scores between the two groups before and after treatment (x̅ ± s)
| Group | Time | Physical activity | Psychological function | Social function | Material life |
|---|---|---|---|---|---|
| Surgical group | Before treatment | 45.62±4.55 | 60.34±3.89 | 60.09±4.31 | 73.62±6.14 |
| n=53 | After treatment | 73.51±4.60 | 74.71±5.25 | 75.15±4.32 | 72.46±5.66 |
| Combination group | Before treatment | 45.42±3.48 | 59.97±3.61 | 59.43±4.02 | 73.14±6.08 |
| n=53 | After treatment | 84.83±6.66 | 86.58±4.99 | 82.44±4.00 | 73.26±6.03 |
| Before treatment | t | 0.254 | 0.506 | 0.818 | 0.410 |
| p | 0.800 | 0.614 | 0.415 | 0.683 | |
| After treatment | t | 10.181 | 11.924 | 9.014 | 0.702 |
| P | <0.001 | <0.001 | <0.001 | 0.484 |
Adverse reaction
No serious adverse reactions were found in the two groups, with 2 cases (3.77%) of wound swelling in the operation group and 2 cases (3.77%) in the combined group, and they were relieved after routine disinfection.
Discussion
The ankle joint is one of the main weight-bearing joints of the human body, and it has a complex biological structure and many active functions such as flexion and extension, abduction, and adduction and eversion [13,14]. The stability of the ankle joint is relatively low in a horizontal position, and it is vulnerable to injury under external forces. Inflammatory lesions of the ankle joint induced by trauma in daily activities are called TAA. TAA is a common disease of the ankle joint, and it can cause serious adverse effects on patients’ lives. In recent years, the incidence of TAA in China has been on the rise, and TAA occurs at all ages due to trauma, so it is widely concerning. Patients with TAA often have ankle pain with redness, swelling, fever, and limited movement, and severe cases can be seen as a joint deformity. For patients with TAA, ankle arthroplasty is traditionally used clinically, but there is a certain failure rate and the clinical effectiveness is not satisfactory. Arthroplasty with ankle joint retraction has become an important operation for treating TAA in recent years, as it has the advantages of minimal invasiveness and an easy post-surgical recovery. However, its clinical effectiveness is easily affected by many factors such as the patient’s own health level, and there is a risk of joint space shrinking in the long term after the operation.
PRP injections are widely used in multiple joint diseases [15,16]. In order to make up for the deficiencies of ankle arthroplasty, surgery combined with PRP injections has been widely used in TAA in recent years, and it has achieved ideal results. Simple ankle arthroplasty mainly relieves the mechanical stress on the ankle cartilage, promotes cartilage repair, and restores the walking ability of the ankle joint under load. Although the curative effect is definite, the trauma caused by the surgical treatment and the recovery level of the soft tissue and the patients’ muscle strength cannot be improved promptly, so the joint gradually declines, which leads to a progression of the disease. It is necessary to make up for the curative effect through other operations such as ankle fusion. Combined with PRP injections after the operation, the treatment can supplement a variety of growth factors locally to the affected area, which have many physiological functions such as antagonistic and inflammatory factors, stimulating the proliferation and repair of the chondrocytes, and it can enhance local muscle nutrition, and because there is no other rejection reaction from the autologous blood, it can effectively improve the clinical and prognostic effects [17,18]. The combination with PRP injections can effectively prevent long-term joint dysfunction and the disease progression induced by it, thus assisting in improving the surgical effectiveness.
Measuring the dorsiflexion and plantarflexion angles of the ankle joint can quantitatively evaluate the recovery of the range of motion of the affected joint. This study showed that the angles of ankle dorsiflexion and plantar flexion were larger in the operation group. This indicates that combined PRP injection therapy can improve the movement angle of the affected ankle joint and provide a better foundation for functional recovery. The AAOS score is an important tool for evaluating ankle function, and it can objectively evaluate the degree of ankle injury and correctly judge the prognosis. The results of this study showed that the BBS and AAOS scores in the combined group were higher than they were in the surgical group after the treatment. This also indicates that combined PRP injection therapy can improve the physiological function recovery level of the affected ankle joint and the lower limb function on the affected side, and then improves patients’ balance function. The SF-MPQ scale is a tool to evaluate patients’ pain. The results of this study show that the SF-MPQ scores of the patients in the combined group were lower than the corresponding scores in the operation group. This indicates that combined PRP injection treatment can effectively reduce patients’ pain levels. PGE2 has regulatory function in the human body, and it mainly participates in many physiological and pathological processes such as fever, inflammatory reactions, pain perception, cell growth and differentiation, etc. TNF-α is an important pro-inflammatory factor in the human body, and its expression level has a clear correlation with fever reactions. IL-6 is an important member of the interleukin family, and it can promote the occurrence of inflammatory reactions and aggravate the degree of inflammatory reactions. The results of this study showed that the serum PGE2, TNF-α, and IL-6 levels in the combined group were lower than they were in the operation group after the treatment. This indicates that combined PRP injection therapy can effectively antagonize the postoperative inflammatory reactions and the ankle inflammation and has an important role in promoting postoperative recovery. The evaluation showed that the quality of life of the patients in the combined group was better than it was in the operation group at six months after the operations. This is mainly due to the better recovery of ankle joint function and the effective pain relief. After the comparison, there were no serious adverse reactions and no differences in the incidence of slight adverse reactions between the two groups, which indicated that combined PRP injections are safe and feasible.
At present, there are many papers on the application of PRP in joint diseases, but there are few studies on the application of PRP in ankle joint diseases, and it remains controversial. The majority believes that PRP in treatment of traumatic ankle arthritis, both anti-inflammatory and repair, is of great significance for the long-term functional recovery of patients and for the improvement of chronic pain. However, there is no uniform standard for platelet concentration and dosage in PRP, and whether the inflammatory factors contained in it affect the efficacy remains to be verified. The results of this study confirm that ankle joint distraction combined with the intra-articular injection of platelet-rich plasma has an excellent effect in traumatic ankle arthritis. It can significantly improve patients’ joint function and improve their quality of life [19,20]. Still, this study had several shortcomings. This study was a single-center study with a small cohort and a short follow-up time. In addition, this study did not discuss the optimal concentration, so it has a limited guiding significance for clinical practice.
To sum up, joint distraction osteogenesis combined with platelet-rich plasma injections can improve the clinical efficacy of traumatic ankle arthritis, promote the recovery of joint function, antagonize the anti-inflammatory reactions, and comprehensively improve patients’ quality of life.
Disclosure of conflict of interest
None.
References
- 1.O’Connell B, Wragg NM, Wilson SL. The use of PRP injections in the management of knee osteoarthritis. Cell Tissue Res. 2019;376:143–152. doi: 10.1007/s00441-019-02996-x. [DOI] [PubMed] [Google Scholar]
- 2.Pan W, Dai C, Li Y, Yin Y, Gong L, Machuki JO, Yang Y, Qiu S, Guo K, Gao F. PRP-chitosan thermoresponsive hydrogel combined with black phosphorus nanosheets as injectable biomaterial for biotherapy and phototherapy treatment of rheumatoid arthritis. Biomaterials. 2020;239:119851. doi: 10.1016/j.biomaterials.2020.119851. [DOI] [PubMed] [Google Scholar]
- 3.Southworth TM, Naveen NB, Tauro TM, Leong NL, Cole BJ. The use of platelet-rich plasma in symptomatic knee osteoarthritis. J Knee Surg. 2019;32:37–45. doi: 10.1055/s-0038-1675170. [DOI] [PubMed] [Google Scholar]
- 4.Dowty ME, Lin TH, Jesson MI, Hegen M, Martin DA, Katkade V, Menon S, Telliez JB. Janus kinase inhibitors for the treatment of rheumatoid arthritis demonstrate similar profiles of in vitro cytokine receptor inhibition. Pharmacol Res Perspect. 2019;7:e00537. doi: 10.1002/prp2.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao J, Huang H, Liang G, Zeng LF, Yang W, Liu J. Effects and safety of the combination of platelet-rich plasma (PRP) and hyaluronic acid (HA) in the treatment of knee osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2020;21:224. doi: 10.1186/s12891-020-03262-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meheux CJ, McCulloch PC, Lintner DM, Varner KE, Harris JD. Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: a systematic review. Arthroscopy. 2016;32:495–505. doi: 10.1016/j.arthro.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Bennell KL, Hunter DJ, Paterson KL. Platelet-rich plasma for the management of hip and knee osteoarthritis. Curr Rheumatol Rep. 2017;19:24. doi: 10.1007/s11926-017-0652-x. [DOI] [PubMed] [Google Scholar]
- 8.O’Donnell C, Migliore E, Grandi FC, Koltsov J, Lingampalli N, Cisar C, Indelli PF, Sebastiano V, Robinson WH, Bhutani N, Chu CR. Platelet-rich plasma (PRP) from older males with knee osteoarthritis depresses chondrocyte metabolism and upregulates inflammation. J Orthop Res. 2019;37:1760–1770. doi: 10.1002/jor.24322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Su K, Bai Y, Wang J, Zhang H, Liu H, Ma S. Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis. Clin Rheumatol. 2018;37:1341–1350. doi: 10.1007/s10067-018-3985-6. [DOI] [PubMed] [Google Scholar]
- 10.Shen L, Yuan T, Chen S, Xie X, Zhang C. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12:16. doi: 10.1186/s13018-017-0521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laver L, Marom N, Dnyanesh L, Mei-Dan O, Espregueira-Mendes J, Gobbi A. PRP for degenerative cartilage disease: a systematic review of clinical studies. Cartilage. 2017;8:341–364. doi: 10.1177/1947603516670709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen P, Huang L, Ma Y, Zhang D, Zhang X, Zhou J, Ruan A, Wang Q. Intra-articular platelet-rich plasma injection for knee osteoarthritis: a summary of meta-analyses. J Orthop Surg Res. 2019;14:385. doi: 10.1186/s13018-019-1363-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moussa M, Lajeunesse D, Hilal G, El Atat O, Haykal G, Serhal R, Chalhoub A, Khalil C, Alaaeddine N. Platelet rich plasma (PRP) induces chondroprotection via increasing autophagy, anti-inflammatory markers, and decreasing apoptosis inhuman osteoarthritic cartilage. Exp Cell Res. 2017;352:146–156. doi: 10.1016/j.yexcr.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Mehranfar S, Abdi Rad I, Mostafav E, Akbarzadeh A. The use of stromal vascular fraction (SVF), platelet-rich plasma (PRP) and stem cells in the treatment of osteoarthritis: an overview of clinical trials. Artif Cells Nanomed Biotechnol. 2019;47:882–890. doi: 10.1080/21691401.2019.1576710. [DOI] [PubMed] [Google Scholar]
- 15.Taniguchi Y, Yoshioka T, Kanamori A, Aoto K, Sugaya H, Yamazaki M. Intra-articular platelet-rich plasma (PRP) injections for treating knee pain associated with osteoarthritis of the knee in the Japanese population: a phase I and IIa clinical trial. Nagoya J Med Sci. 2018;80:39–51. doi: 10.18999/nagjms.80.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dai WL, Zhou AG, Zhang H, Zhang J. Efficacy of platelet-rich plasma in the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Arthroscopy. 2017;33:659–670. e1. doi: 10.1016/j.arthro.2016.09.024. [DOI] [PubMed] [Google Scholar]
- 17.Richards MM, Maxwell JS, Weng L, Angelos MG, Golzarian J. Intra-articulartreatment of knee osteoarthritis: from anti-inflammatories to products of regenerative medicine. Phys Sportsmed. 2016;44:101–108. doi: 10.1080/00913847.2016.1168272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Görmeli G, Görmeli CA, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25:958–965. doi: 10.1007/s00167-015-3705-6. [DOI] [PubMed] [Google Scholar]
- 19.Raeissadat SA, Rayegani SM, Hassanabadi H, Fathi M, Ghorbani E, Babaee M, Azma K. Knee osteoarthritis injection choices: platelet- rich plasma (PRP)versus hyaluronic acid (a one-year randomized clinical trial) Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. doi: 10.4137/CMAMD.S17894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jadah NA, Shamkhi IA. A comparative study of low-level laser efficacy on autologous activity of PRP injected in knee arthritis, in vivo study. Lasers Med Sci. 2021;36:357–363. doi: 10.1007/s10103-020-03039-6. [DOI] [PubMed] [Google Scholar]


