Abstract
BACKGROUND:
Social determinants of health are known to contribute to disparities in health outcomes. Routine screening for basic social needs is not a part of standard care; however, the association of those needs with increased healthcare utilization and poor compliance with guideline-directed care is well established.
OBJECTIVE:
In this study, we aimed to assess the prevalence of basic social resource needs identified through a quality improvement initiative in a gynecologic oncology outpatient clinic. In addition, we aimed to identify clinical and demographic factors associated with having basic social resource needs.
STUDY DESIGN:
We performed a prospective cohort study of women presenting to a gynecologic oncology clinic at an urban academic institution who were screened for basic social resource needs as part of a quality improvement initiative from July 2017 to May 2018. The following 8 domains of resource needs were assessed: food insecurity, housing insecurity, utility needs, financial strain, transportation, childcare, household items, and difficulty reading hospital materials. Women with needs were referred to resources to address those needs. Demographic and clinical information were collected for each patient. The prevalence of needs and successful follow-up interventions were calculated. Patient factors independently associated with having at least 1 basic social resource need were identified using multivariable Poisson regression.
RESULTS:
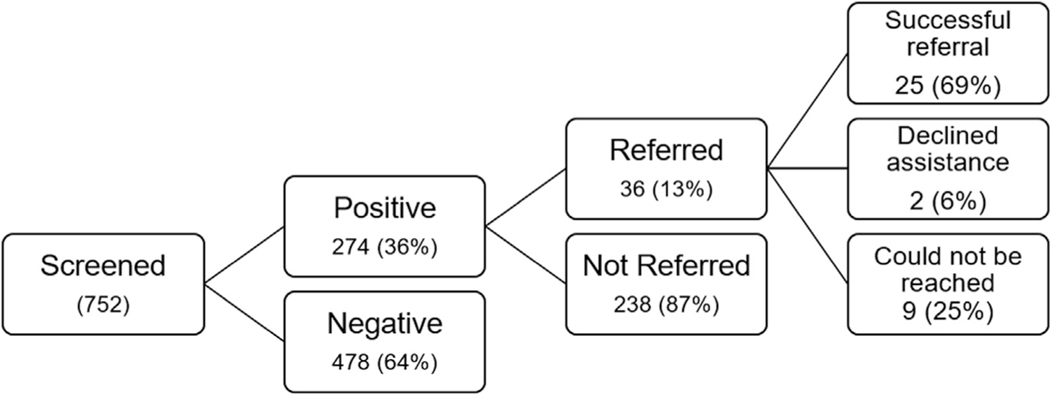
A total of 752 women were screened in the study period, of whom 274 (36%) reported 1 or more basic social resource need, with a median of 1 (range, 1e7) need. Financial strain was the most commonly reported need (171 of 752, 23%), followed by transportation (119 of 752, 16%), difficulty reading hospital materials (54 of 752, 7%), housing insecurity (31 of 752, 4%), food insecurity (28 of 752, 4%), household items (22 of 752, 3%), childcare (15 of 752, 2%), and utility needs (13 of 752, 2%). On multivariable analysis, independent factors associated with having at least 1 basic social resource need were being single, divorced or widowed, nonwhite race, current smoker, nonprivate insurance, and a history of anxiety or depression. A total of 36 of 274 (13%) women who screened positive requested assistance and were referred to resources to address those needs. Of the 36 women, 25 (69%) successfully accessed a resource or felt equipped to address their needs, 9 (25%) could not be reached despite repeated attempts, and 2 (6%) declined assistance.
CONCLUSION:
Basic social resource needs are prevalent in women presenting to an urban academic gynecologic oncology clinic and can be identified and addressed through routine screening. To help mitigate ongoing disparities in this population, screening for and addressing basic social resource needs should be incorporated into routine comprehensive care in gynecologic oncology clinics.
Keywords: basic resources, cervical cancer, gynecologic cancer, healthcare disparities, Health Leads, routine screening, ovarian cancer, social determinants of health, supportive care, uterine cancer
Unmet basic social resource needs have recently been recognized at the national level for their negative effect on overall health outcomes and their contribution to health disparities.1 More than 70% of health outcomes are attributable to social and environmental factors experienced by the patient outside of the hospital or ambulatory setting.2 A basic social resource need is the lack of an essential resource that is required for day-to-day living, such as food and housing, transportation, finances, or other nonessential resources such as childcare. These needs represent key components of the following 5 primary social determinants of health: economic stability, neighborhood and the built environment, social and community context, health and healthcare, and education.3
The most vulnerable patient populations, such as those in minority groups and individuals with lower levels of education and socioeconomic status, are more likely to present with basic social resource needs,4 which exacerbate existing health disparities.5,6 In gynecologic cancer care, multimodality treatments are common, requiring the patient to access the healthcare system in multiple ways. As a result, social factors such as lack of access to transportation are linked to diagnosis of a disease at later stage and worse survival outcomes, particularly in women with cervical cancer.7,8 Basic social resource needs are also linked to higher costs and unnecessary healthcare utilization.9 Although financial toxicity and the effect of financial strain have been extensively explored in the gynecologic oncology patient population,10–12 other basic social resource needs have not been well studied. A way to include screening for basic social resource needs in the comprehensive care of patients with cancer is notably absent in oncology practice guidelines.
Health Leads is a national nonprofit organization that has been partnering with communities and health systems since 1996 to address systemic causes of inequity and disease. The organization works to remove barriers that keep patients from identifying, accessing, and choosing the basic resources every person needs to be healthy.13 Health Leads published a Social Needs Screening Toolkit that provides a blueprint for hospital systems to screen for and address patients’ social determinants of health. The toolkit is publicly available and updated annually based on the latest research in the field.14 We recognized the potential of this toolkit to identify and address the basic needs of patients at our institution, where social factors have been previously shown to affect the patients’ ability to receive recommended, guideline-based gynecologic care.15 We conducted a quality improvement initiative to screen for basic social resource needs in a diverse gynecologic oncology outpatient cohort at an urban academic center as a way to begin to address disparities in access to and completion of gynecologic cancer care.
Methods
We performed a prospective cohort study of a 2-phase quality improvement initiative aimed at reducing barriers to address the basic social resource needs of patients presenting to a gynecologic oncology outpatient clinic. The first phase consisted of the development of a screening tool. In the second phase, the resultant written screening tool was given to all women presenting to the gynecologic oncology clinic at The Johns Hopkins Hospital, Baltimore, MD. The final screening tool and a detailed description of development are described in Supplemental Material. This study was part of a quality improvement initiative conducted from July 2017 to May 2018 and was determined by the Johns Hopkins Medicine Institutional Review Board (IRB) to be IRB exempt.
Adaptation of the Health Leads screening toolkit
Clinically validated questions written at the 4th to 10th grade reading level were identified from the Health Leads Social Needs Screening Toolkit and used to develop a basic social resource screening tool.14 Initially, 7 resource domains, including the 5 essential domains of food insecurity, housing insecurity, utility needs, transportation needs, and financial needs, and 2 nonessential domains, including education and childcare, were included. In addition women were asked whether they felt comfortable answering questions about these topics if their healthcare provider inquired and whether they had ever discussed these topics with a physician or a social worker. From July 2017 to December 2017, a Health Leads advocate administered the tool in person. After reviewing the first 50 responses from participants, additional questions about financial need (the most prevalent need) and need for household items were added. Furthermore, for times when the tool could not be administered in person, the following questions were added: “Would you like to receive assistance with any of these needs?” and “Are any of your needs urgent?” The latter question allowed for identification of patients who warranted urgent referral to social work and Health Leads.
Implementation of the screening tool
The written questionnaire was given to patients by the front desk check-in staff of the Johns Hopkins Gynecologic Oncology outpatient clinic from January 2018 to May 2018. Physicians reviewed the form to identify any urgent needs, warranting social work follow-up. All women who received positive screening results and indicated they would like assistance were referred to the Health Leads program. Health Leads is a nonprofit institution that trains undergraduate volunteers to connect individuals with needs to community-based resources and provides ongoing follow-up as needed.16,17 In this study, a Health Leads advocate contacted the patient (most often through telephone), assessed their needs, and provided resources. The Health Leads program enrolled women and remained in contact weekly until the women felt equipped to independently address their needs. Women were classified as having a successful referral, declining assistance, or being unable to be reached. A successful referral was defined as confirmation that the woman had (1) accessed or received the recommended resources, (2) reported that they felt equipped to access a needed resource on their own, or (3) received a rapid referral from Health Leads for a resource that did not require follow-up, such as a list of food pantries or locations to obtain free winter clothing. Health Leads would attempt to establish contact for 30 days through weekly phone calls, after which attempts were terminated.
Statistical analyses
Patient demographics, clinical characteristics, and responses to the screening tool were extracted from the electronic medical record (EMR). Data on success of referrals were abstracted from the Health Leads database. Because of the lack of income data in the EMR, United States Census Bureau median income estimation for the zip code of their primary residence was used.18 Data were collected and managed using REDCap (research electronic data capture) tools hosted by Johns Hopkins University.19 The primary outcome of this study was the presence of “at least 1 basic social resource need,” as measured by a series of binary yes or no questions. Transportation and financial strain were assessed on a 5-point Likert scale and responses of sometimes, often, or always were considered a positive screen.
We used descriptive statistics to report the clinical and demographic characteristics, the prevalence of needs, and the response rate of each question in all women screened. Prevalence of needs was compared by race (white vs black or other) using Fisher’s exact tests based on the a priori hypothesis that basic social resource needs differ by race. We calculated the proportion of eligible women presenting to the clinic who completed the screening. We used univariate Poisson regression to evaluate the relationship between having “at least 1 basic social resource need” and patient demographic, clinical, and screening tool (ie, in person with the advocate or written) characteristics; variables that were significantly associated with univariate analysis (P<.05) were included in multivariable regression to identify independent factors associated with having needs.
Results
A total of 752 women completed screening between July 2017 and May 2018, representing 47% of eligible women. The reason for not completing screening was not monitored. The majority of women were white (453 of 752, 60%) and had a history of gynecologic cancer (461 of 752, 61%). Furthermore, 165 of the 752 women (22%) were actively undergoing cancer treatment (Table 1).
TABLE 1.
Demographics and clinical characteristics of the women assessed for basic social resource needs via the Health Leads Screening Tool
| Overall (N=752) | |
|---|---|
| Patient demographics | |
| Age at assessment | 56 (43.00–65.00) |
| BMI | 27.99 (23.56–34.32) |
| Race | |
| White | 453 (60.2%) |
| Black | 201 (26.7%) |
| Other race | 98 (13.0%) |
| Zip code income tertile | |
| First: <$63,533 | 245 (33.0%) |
| Second: $63,533-$93,557 | 252 (34.0%) |
| Third: >$93,557 | 245 (33.0%) |
| Unemployed or retired | |
| Yes | 363 (49.1%) |
| English as their primary language | |
| Yes | 725 (96.4%) |
| Smoking status | |
| Never smoked | 510 (67.8%) |
| Former smoker | 188 (25.0%) |
| Current smoker | 54 (7.2%) |
| Insurance type | |
| Private | 506 (67.3%) |
| Public (Medicare, Medicaid) or none | 246 (32.7%) |
| Clinical characteristics | |
| Diagnosis of gynecologic cancer | |
| None | 291 (38.7%) |
| Uterine | 185 (24.6%) |
| Ovarian | 173 (23.0%) |
| Cervix | 61 (8.1%) |
| Vulvar or other | 42 (5.6%) |
| Comorbidities | |
| HIV positive | |
| Yes | 14(1.9%) |
| Hepatitis C positive | |
| Yes | 14(1.9%) |
| Diabetes mellitus | |
| Yes | 113 (15%) |
| Overall (N=752) | |
| Psychiatric illness | |
| None | 576 (76.6%) |
| Anxiety | 56 (7.4%) |
| Depression | 56 (7.4%) |
| Anxiety and depression | 47 (6.3%) |
| Bipolar disorder or other | 17(2.4%) |
| Visit or treatment information | |
| Actively undergoing cancer treatment | 165 (21.9%) |
| In surveillance for cancer | 277 (36.8%) |
| Being worked up for cancer | 65 (8.6%) |
| Visit type | |
| New | 194 (25.8%) |
| Return | 558 (74.2%) |
| Screening type | |
| Paper | 702 (93.4%) |
| In person | 48 (6.4%) |
| Phone call | 2 (0.3%) |
| Number of basic social resource needs | |
| 0 | 573 (76.2%) |
| 1 | 123 (16.4%) |
| 2 | 31 (4.1%) |
| 3 | 11 (1.5%) |
| 4 | 9 (1.2%) |
| >5 | 5 (0.7%) |
Beavis et al. Basic social resource needs screening in the gynecologic oncology clinic: a quality improvement initiative. Am J Obstet Gynecol 2020.
Data are presented as median (IQR) or n (%).
BMI, body mass index; HIV, human immunodeficiencyvims; IQR, interquartile range.
Screening response rates and prevalence of basic social resource needs
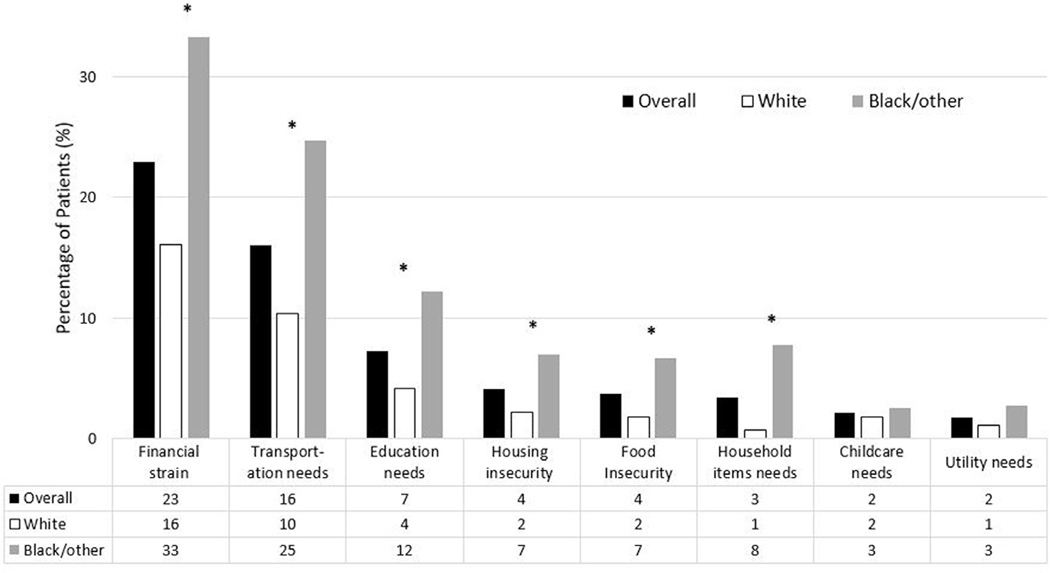
Response rates to binary questions assessing the 8 basic social resource domains were 97% or greater, with the exception of childcare (95.3%). Likert scale questions about transportation and financial strain were left blank by 46 of 752 (6.1%) and 37 of 752 (4.9%) women, respectively (Table 2). Overall, 274 of 752 (36%) women had at least 1 basic social resource need. Of those women, the median number of needs reported was 1 (range, 1–7). Only 3 of 752 (0.4%) women reported urgent needs. The most commonly reported needs were financial strain (23%), transportation (16%), difficulty reading hospital materials (7%), food insecurity (4%), housing insecurity (4%), utility needs (2%), and childcare barriers (2%). When comparing women of white race with women of black or other race, women of a minority group were more likely to report all needs except childcare and utility needs (Figure 1). Furthermore, women of minority groups were more likely to have 2 or more needs compared with women of white race (20% black or other race vs 7% white race; P<.001).
TABLE 2.
Question-specific response rates for screening questions on basic social resource needs
| Social resource domain assessed | Question asked | Number with no response | Response rate |
|---|---|---|---|
| Food insecurity | In the last 12 months, did you ever eat less than you felt you should because there wasnť enough money for food? | 2 | 99.7% |
| Housing insecurity | Are you worried that in the next 2 months, you may not have stable housing? | 4 | 99.5% |
| Utility needs | In the past year, has the utility company shut off your service for not paying your bills? | 7 | 99.1% |
| Financial strain | Please indicate how often this describes you: I donť have enough money to pay my bills. (5-point Likert scale) | 46 | 93.9% |
| In the last 12 months, have you needed to see a doctor but could not because of cost?a | 6 | 99.2% | |
| Transportation | Are you regularly able to get a friend or relative to take you to your doctors' appointments? | 8 | 98.9% |
| How often do you miss or need to delay appointments due to lack of transportation? (5-point Likert scale) | 37 | 95.1% | |
| Childcare | Do problems getting childcare make it difficult for you to get to appointments? | 35 | 95.3% |
| Education | Do you need help reading hospital materials? | 16 | 97.9% |
| Commodities | Do you need help finding household items such as furniture or clothing?a | 16 | 97.9% |
Binaryyes or no questions had significantly higher response rates than Likert scale questions (P<.01).
Asked on the written screening tool during the second phase only (n=672).
Beavis et al. Basic social resource needs screening in the gynecologic oncology clinic: a quality improvement initiative. Am J Obstet Gynecol 2020.
FIGURE 1. Prevalence of social needs by race.
Black bars indicate overall prevalence of social needs, the white bar indicates prevalence of social needs in white women, and the gray bar indicates prevalence of social needs in women who are black or of other races. Women of a minority group had a significantly higher prevalence of all needs except childcare and utility compared with white women. Need categories with statistically significant differences between white women and women who are black or of other races are marked with an asterisk (P<.05).Beavis et al. Basic social resource needs screening in the gynecologic oncology clinic: a quality improvement initiative. Am J Obstet Gynecol 2020.
Factors associated with basic social resource needs
In the multivariable model, many demographic factors remained independently associated with having any basic social resource need (Table 3). Being single, divorced, or widowed increased the prevalence of any need by 59% (relative risk [RR], 1.59; 95% confidence interval [CI], 1.28–1.99) and 46% (RR, 1.46; 95% CI, 1.16–1.84), respectively. Women of nonwhite race had 68% higher prevalence than women of white race (RR, 1.68; 95% CI, 1.37–2.06). Current smokers had almost double the risk (RR, 1.81; 95% CI, 1.40–2.35) of people who never smoked. Women with nonprivate insurance had 36% higher risk of having any need (RR, 1.36; 95% CI, 1.10–1.69), similar to the increased risk seen in women with anxiety or depression (RR, 1.30; 95% CI, 1.05–1.60). Employment status, income, body mass index, medical comorbidities, and screening type (in person with the advocate vs written) were not independently associated with having any basic social resource need.
TABLE 3.
Univariate and multivariable analysis of factors associated with having any social resource need
| Univariate | Multivariable | |||||
|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | |||
| Factor | RR | 95% CI | RR | 95% CI | ||
| Marital status | ||||||
| Married | Ref | — | — | — | — | — |
| Single | 1.81 | 1.46 | 2.26 | 1.59 | 1.28 | 1.99 |
| Divorced or widowed | 1.81 | 1.43 | 2.28 | 1.46 | 1.16 | 1.84 |
| Age | ||||||
| Age | 1.00 | 0.99 | 1.00 | — | — | — |
| Visit type | ||||||
| New | Ref | — | — | — | — | — |
| Return | 0.94 | 0.76 | 1.16 | — | — | — |
| BMI | ||||||
| Normal, 18.5–24.9 | Ref | — | — | — | — | — |
| Underweight, <18.5 | 0.63 | 0.23 | 1.77 | 0.58 | 0.22 | 1.52 |
| Overweight, 25–30 | 1.06 | 0.81 | 1.40 | 0.98 | 0.75 | 1.29 |
| Obese, >30 | 1.34 | 1.07 | 1.68 | 1.10 | 0.87 | 1.38 |
| Race | ||||||
| White | Ref | — | — | — | — | — |
| Black and/or other | 1.48 | 1.24 | 1.77 | 1.68 | 1.37 | 2.06 |
| Employment status | ||||||
| Employed | Ref | — | — | — | — | — |
| Unemployed | 1.45 | 1.19 | 1.76 | 1.08 | 0.87 | 1.35 |
| Religion | ||||||
| No | Ref | — | — | — | — | — |
| Yes | 0.91 | 0.75 | 1.11 | — | — | — |
| Smoking status | ||||||
| Never smoked | Ref | — | — | — | — | — |
| Former smoker | 1.03 | 0.81 | 1.29 | 0.93 | 0.74 | 1.18 |
| Current smoker | 2.03 | 1.63 | 2.53 | 1.82 | 1.40 | 2.35 |
| Median zip income tertile | ||||||
| <$63,533 | Ref | — | — | — | — | — |
| $63,533–$93,557 | 0.82 | 0.66 | 1.01 | 0.93 | 0.75 | 1.14 |
| >$93,557 | 0.59 | 0.46 | 0.75 | 0.87 | 0.68 | 1.11 |
| Insurance | ||||||
| Private | Ref | — | — | — | — | — |
| Public and/or none | 1.53 | 1.27 | 1.84 | 1.36 | 1.10 | 1.69 |
| Attending | ||||||
| 1 | Ref | — | — | — | — | — |
| 2 | 1.21 | 0.96 | 1.53 | — | — | — |
| 3 | 1.12 | 0.86 | 1.46 | — | — | — |
| 4 | 0.76 | 0.53 | 1.09 | — | — | — |
| 5 | 0.73 | 0.41 | 1.32 | — | — | — |
| 6 | 0.95 | 0.19 | 4.75 | — | — | — |
| Invasive cancer | ||||||
| No | Ref | — | — | — | — | — |
| Yes | 0.96 | 0.79 | 1.16 | — | — | — |
| Cancer type | ||||||
| None | Ref | — | — | — | — | — |
| Uterine | 0.93 | 0.73 | 1.18 | 0.90 | 0.70 | 1.15 |
| Ovarian | 0.69 | 0.52 | 0.92 | 0.74 | 0.56 | 0.98 |
| Cervix | 1.28 | 0.95 | 1.71 | 1.15 | 0.84 | 1.57 |
| Vulvar and/or other | 1.24 | 0.87 | 1.75 | 1.21 | 0.84 | 1.72 |
| Stage of treatment | ||||||
| No cancer | Ref | — | — | — | — | — |
| Undergoing treatment | 0.92 | 0.71 | 1.18 | — | — | — |
| In surveillance | 0.87 | 0.69 | 1.08 | — | — | — |
| Working up for cancer | 0.85 | 0.59 | 1.24 | — | — | — |
| Diabetes | ||||||
| No | Ref | — | — | — | — | — |
| Yes | 1.42 | 1.14 | 1.77 | 1.22 | 0.98 | 1.53 |
| Hypertension | ||||||
| No | Ref | — | — | — | — | — |
| Yes | 1.24 | 1.03 | 1.50 | — | — | — |
| Hepatitis C | ||||||
| No | Ref | — | — | 0.92 | 0.54 | 1.57 |
| Yes | 2.00 | 1.41 | 2.82 | — | — | — |
| HIV | ||||||
| No | Ref | — | — | — | — | — |
| Yes | 2.20 | 1.65 | 2.95 | 1.05 | 0.64 | 1.71 |
| Psychiatric history | ||||||
| None | Ref | — | — | — | — | — |
| Anxiety±Depression | 1.18 | 0.95 | 1.47 | 1.30 | 1.05 | 1.60 |
| Other | 1.70 | 1.13 | 2.57 | 1.47 | 1.00 | 2.16 |
| Cancer stage | ||||||
| 1 | Ref | — | — | — | — | — |
| 2 | 1.37 | 0.91 | 2.05 | — | — | — |
| 3 | 1.01 | 0.74 | 1.38 | — | — | — |
| 4 | 1.17 | 0.80 | 1.70 | — | — | — |
| Not applicable | 1.10 | 0.86 | 1.40 | — | — | — |
| Unknown | 0.82 | 0.48 | 1.40 | — | — | — |
| Screen type | ||||||
| Paper | Ref | — | — | — | — | — |
| In person | 1.47 | 1.11 | 1.96 | 0.97 | 0.71 | 1.32 |
Bold text indicates significance on univariate and multivariable analyses.
BMI, body mass index; CI, confidence interval; RR relative risk.
Beavis et al. Basic social resource needs screening in the gynecologic oncology clinic: a quality improvement initiative. Am J Obstet Gynecol 2020.
Having a history of cancer was not associated with an increased risk, but women with ovarian cancer had 26% lower risk of having any basic social resource need than women without cancer (RR, 0.74; 95% CI, 0.56–0.98).
Enrollment in Health Leads and follow-up
Of 274 women with any needs, 36 (13%) stated that they would like assistance and were referred to Health Leads. Of the 36 women, 25 (69%) were successfully referred, 9 (25%) could not be reached, and 2 (6%) ultimately declined assistance (Figure 2). Of those 25 women successfully referred, 14 (56%) had their needs resolved through Health Leads, and 3 (12%) received a rapid resource referral. After Health Leads conducted a more in-depth assessment, the median number of basic social resource needs was 3. Other needs that were identified and addressed by Health Leads included mental health medical equipment prescription assistance other miscellaneous such as legal aid, holiday gifts, and benefits denials; and insurance-related. Notably, 100 of 274 (36.5%) women with needs were not referred because they did not answer whether they would like assistance.
FIGURE 2. Health Leads referral outcomes.
Participants were referred to Health Leads if they screened positive and requested assistance.Beavis et al. Basic social resource needs screening in the gynecologic oncology clinic: a quality improvement initiative. Am J Obstet Gynecol 2020.
Comment
Principal findings
This study found that in an urban, tertiary gynecologic oncology outpatient clinic, basic social resource needs were prevalent in more than one-third of the population. Moreover, the participants exist across socioeconomic boundaries. We found that using publicly available tools and partnering with community-based organizations can be a catalyst for successful implementation of a program to screen for and address basic social resource needs. This study identified women who were at very high risk of basic social resource needs, including women of minority groups, who are not married, who smoke, with public health insurance, and with mental illness. Moreover, we identified transportation, financial strain, and difficulty reading hospital materials as the most common needs in this population. The results support the expansion of the best supportive care in gynecologic oncology to include basic social resource needs.
Results
Addressing the social determinants of health is particularly important for women with gynecologic cancers who undergo complex, multimodal therapy and numerous interactions with the healthcare system. Vulnerable populations with basic social resource needs may not receive optimal care even when recommended by their healthcare provider.7,8 For example, because of transportation needs, women of minority groups undergoing chemoradiation for cervical cancer are less likely to complete treatment, worsening health outcomes and exacerbating survival disparities.6 Social and economic factors, such as public or no insurance, low SES, and being black, are associated with poor compliance with guideline-directed treatment plans and increased cancer-specific mortality.5 Consistent with the literature, we found that being part of a minority group and having public or no insurance were associated with an increased risk of having basic social resource needs. Although our study indicates that these basic needs can be detected and addressed through screening, further studies are required to optimize interventions to improve patient outcomes. Screening for needs at treatment initiation has the potential to mitigate disparities in treatment adherence related to social needs; as such, we reported that the Health Leads Social Needs Screening Toolkit can be effectively implemented for this purpose. In both pediatric and primary care settings, similar screening tools have been found to result in successful resource referrals in 50% to 70% of cases, similar to this study.20–22 In addition, integration of the screening tool into the EMR may increase compliance with screening and referrals to resources.23 Our screening tool was physically handed to the patient, which could have contributed to half of the women not completing the questionnaire. Similar to other studies, we planned to integrate the screening tool into the EMR and evaluate the effect on successful referrals and proportion of women screened.
Clinical implications
It is imperative to have mechanisms and resources immediately available to address basic social resource needs when implementing a screening program.24 Surveys of healthcare providers show that the providers recognize the importance of addressing social needs but do not feel equipped to address them.20,25,26 Our study is unique in that using an existing Health Leads program already integrated into the Johns Hopkins pediatric clinic allowed us to build a partnership and referral plan for the gynecologic oncology patients without placing additional burden on hospital social work resources. The first phase of the study ensured that adequate follow-up could be achieved before initiating widespread implementation. Other healthcare providers could use this same screening tool by collaborating with social workers or financial counselors within their institution or by engaging local organizations. Institutions without community partnerships can use online resources such as www.auntbertha.com, an online portal with free access to a nationwide database of community-based organizations addressing the social determinants of health, to identify potential partners and find local resources.27 Additional resources are listed in Supplemental Material.
Addressing social needs should be recognized as an important part of cancer care. There are validated instruments to assess supportive care domains such as symptom distress and mental health, but none that addresses basic social resource needs.28,29 Noncancer life stressors can impair quality of life in cancer patients,30 and the National Comprehensive Cancer Network’s Best Supportive Care Checklist does not provide guidance regarding screening for and addressing basic social resource needs.31 To our knowledge, this is the first published study to identify and address basic resource needs in the gynecologic oncology population. Because many cancer centers already have structured screening tools in place, including basic social resource needs screening is feasible and should be considered a priority to address disparities.
Research implications
We plan to continue our research addressing basic resource needs in the gynecologic oncology population by examining the effect of screening and interventions on quality and timeliness of cancer care delivery in addition to cancer care outcomes. Although the focus of this study was on patients with cancer, use of this screening tool is equally appropriate and feasible on patients presenting to nonspecialty obstetrics and gynecology clinics. The needs identified in this study, including financial barriers to care, housing, and food insecurity, are commonly reported in both pediatric and primary care populations, suggesting that these same screening questions can be used in a variety of settings.22 Although a majority of Americans report at least 1 social determinant of health challenge, most have not discussed these issues with their healthcare providers, similar to the results of this study.32 The Centers for Medicare and Medicaid Services’ Accountable Health Communities Model is currently used to evaluate the effect of a variety of interventions that address social needs on patient outcomes, demonstrating the national recognition of the importance of identifying and addressing basic social resource needs in healthcare.1 The results will clarify whether social needs screening and intervention affect outcomes such as cost and healthcare utilization. Importantly, the effect of screening on outcomes in gynecologic cancer remains an unmet research need.
Strengths and limitations
This study’s strengths include its large sample size and high-risk, diverse population. We used a validated instrument written at a low reading grade level, based on the most up-to-date data on social needs screening. The diversity of our population allowed for examination of racial differences in social needs. The intervention, however, is not universally implementable—we had access to unique resources with the Health Leads program. Other limitations include the lack of tracking of the number of women who were given the questionnaire and who declined to complete it and the lack of person-level income data that may have affected our ability to see differences in needs by SES. In addition, we identified difficulty reading hospital materials as a common need, which could have contributed to the lack of responses on the written questionnaire for some women. Continued follow-up of this program is ongoing, including strategies to increase screening and decrease the number of participants lost during follow-up. For example, reporting the success of the program to key stakeholders such as the front desk staff in this study may improve compliance with universal administration to all eligible patients.33 Future research will be performed to determine why women decline to complete screening and the characteristics of those women for whom a different screening modality may be appropriate.
Conclusions
Closing the gap in healthcare quality for vulnerable populations is imperative. This study provided evidence that successful screening tools used in pediatric and primary care populations also can be used effectively in an urban gynecologic oncology population. We will continue to refine the process, with feedback from stakeholders and EMR integration with reflex referrals for positive screens as part of standard-of-care treatment. As we strive to decrease disparities in the social determinants of health for women with gynecologic malignancies, we ultimately aim to improve cancer-related outcomes and quality of life. This study demonstrates a framework to initiate that work through the detection and addressing of basic social resource needs.
Supplementary Material
AJOG at a Glance.
Why was this study conducted?
Basic social resource needs are associated with health disparities. However, there is limited guidance on how to screen for and address these needs in patients presenting to a gynecologic oncology clinic.
Key findings
Of patients presenting to a gynecologic oncology clinic, 36% reported 1 or more basic social resource needs. The most common were financial strain (23%), transportation (16%), and needing help reading hospital materials (7%). Being single, divorced or widowed, nonwhite, or a smoker and having nonprivate insurance or a history of anxiety or depression were associated with an increased risk of reporting a need.
What does this add to what is known?
Basic social resource needs are common in patients presenting to a gynecologic oncology clinic and can be successfully identified and addressed through routine screening.
Acknowledgments
We thank the members of the Health Leads organization for their support, resources, and dedication to this quality improvement initiative.
The findings of this study were presented at the 50th annual meeting of the Society of Gynecologic Oncology, Honolulu, HI, March 16–19, 2019.
Footnotes
Ms Kristin Topel is employed as a program manager at Health Leads. All other authors report no conflict of interest.
Contributor Information
Anna Louise Beavis, From the Kelly Gynecologic Oncology Service, Department of Gynecology and Obstetrics, Johns Hopkins School of Medicine, Baltimore, MD.
Awa Sanneh, Johns Hopkins University School of Medicine, Baltimore, MD.
Rebecca L. Stone, From the Kelly Gynecologic Oncology Service, Department of Gynecology and Obstetrics, Johns Hopkins School of Medicine, Baltimore, MD.
Margaret Vitale, Johns Hopkins University, Baltimore, MD.
Kimberly Levinson, From the Kelly Gynecologic Oncology Service, Department of Gynecology and Obstetrics, Johns Hopkins School of Medicine, Baltimore, MD.
Anne F. Rositch, Department of Cancer Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD.
Amanda Nickles Fader, From the Kelly Gynecologic Oncology Service, Department of Gynecology and Obstetrics, Johns Hopkins School of Medicine, Baltimore, MD.
Kristin Topel, Department of General Pediatrics and Adolescent Medicine, Johns Hopkins University, Baltimore, MD.
Ashley Abing, Johns Hopkins University, Baltimore, MD.
Stephanie L. Wethington, From the Kelly Gynecologic Oncology Service, Department of Gynecology and Obstetrics, Johns Hopkins School of Medicine, Baltimore, MD.
References
- 1.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities: addressing social needs through Medicare and Medicaid. N Engl J Med 2016;374:8–11. [DOI] [PubMed] [Google Scholar]
- 2.Hood CM, Gennuso KP, Swain GR, Catlin BB. County health rankings: relationships between determinant factors and health outcomes. Am J Prev Med 2016;50:129–35. [DOI] [PubMed] [Google Scholar]
- 3.Magnan S. Social determinants of Health 101 for health care: five plus five. NAM Perspectives; 2017;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boucher NA, Kuchibhatla M, Johnson KS. Meeting basic needs: social supports and services provided by hospice. J Palliat Med 2017;20:642–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chatterjee S, Gupta D, Caputo TA, Holcomb K. Disparities in gynecological malignancies. Front Oncol 2016;6:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uppal S, Chapman C, Spencer RJ, et al. Association of hospital volume with racial and ethnic disparities in locally advanced cervical cancer treatment. Obstet Gynecol 2017;129: 295–304. [DOI] [PubMed] [Google Scholar]
- 7.Ramondetta LM, Sun C, Hollier L, et al. Advanced cervical cancer treatment in Harris County: pilot evaluation of factors that prevent optimal therapy. Gynecol Oncol 2006;103: 547–53. [DOI] [PubMed] [Google Scholar]
- 8.Ramondetta LM, Meyer LA, Schmeler KM, et al. Avoidable tragedies: disparities in healthcare access among medically underserved women diagnosed with cervical cancer. Gynecol Oncol 2015;139:500–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med 2017;53: 719–29. [DOI] [PubMed] [Google Scholar]
- 10.Stokes ME, Ishak J, Proskorovsky I, Black LK, Huang Y. Lifetime economic burden of prostate cancer. BMC Health Serv Res 2011;11:349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Svynarenko R, Zhang Q, Kim H. The financial burden of cancer: financial ratio analysis. J Fam Econ Issues 2018;40:165–79. [Google Scholar]
- 12.Bouberhan S, Shea M, Kennedy A, et al. Financial toxicity in gynecologic oncology. Gynecol Oncol 2019;154:8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Our history. Health Leads. Available at: https://healthleadsusa.org/about-us/our-history/. Accessed January 20, 2020.
- 14.Health Leads. Social Needs Screen Toolkit 2017. Available at: https://healthleadsusa.org/resources/the-health-leads-screening-toolkit/. Accessed July 28, 2020.
- 15.Levinson KL, Bristow RE, Donohue PK, Kanarek NF, Trimble CL. Impact of payer status on treatment of cervical cancer at a tertiary referral center. Gynecol Oncol 2011;122:324–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Health Leads. Available at: https://healthleadsusa.org/. Accessed April 25, 2020.
- 17.Garg A, Marino M, Vikani AR, Solomon BS. Addressing families’ unmet social needs within pediatric primary care: the health leads model. Clin Pediatr (Phila) 2012;51:1191–3. [DOI] [PubMed] [Google Scholar]
- 18.United States Census Bureau. American FactFinder—community facts. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/community_facts.xhtml?src=bkmk. Accessed March 4, 2020.
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garg A, Cull W, Olson L, et al. Screening and referral for low-income families’ social determinants of health by US pediatricians. Acad Pediatr 2019;19:875–83. [DOI] [PubMed] [Google Scholar]
- 21.Garg A, Sarkar S, Marino M, Onie R, Solomon BS. Linking urban families to community resources in the context of pediatric primary care. Patient Educ Couns 2010;79: 251–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med 2017;177:244–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gottlieb LM, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med 2015;48: 215–8. [DOI] [PubMed] [Google Scholar]
- 24.Hamity C, Jackson A, Peralta L, Bellows J. Perceptions and experience of patients, staff, and clinicians with social needs assessment. Perm 2018;22:18–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schickedanz A, Hamity C, Rogers A, Sharp AL, Jackson A. Clinician experiences and attitudes regarding screening for social determinants of health in a large integrated health system. Med Care 2019;57(Suppl 6 Suppl 2): S197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naz A, Rosenberg E, Andersson N, Labonté R, Andermann A; CLEAR Collaboration. Health workers who ask about social determinants of health are more likely to report helping patients: mixed-methods study. Can Fam Phys 2016;62: e684–93. [PMC free article] [PubMed] [Google Scholar]
- 27.Aunt Bertha—the Social Care Network. Available at: https://www.auntbertha.com/?gclid=CjwKCAjwv4_1BRAhEiwAtMDLsmo1i_tj1afZvosC6U-MXIeIAfVPU9BDdPpxjPjblaK1K9uoExW0aBoCpbEQAvD_BwE. Accessed April 25, 2020.
- 28.von Gruenigen VE, Huang HQ, Cella D, et al. Quality of life, symptoms and care needs in patients with persistent or recurrent platinum-resistant ovarian cancer: an NRG Oncology/Gynecologic Oncology Group study. Gynecol Oncol 2018;150:119–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Olesen ML, Hansson H, Ottesen B, Thranov IR, Thisted LB, Zoffmann V. The psychosocial needs of gynaecological cancer survivors: a framework for the development of a complex intervention. Eur J Oncol Nurs 2015;19:349–58. [DOI] [PubMed] [Google Scholar]
- 30.Lutgendorf SK, Slavich GM, Degeest K, et al. Non-cancer life stressors contribute to impaired quality of life in ovarian cancer patients. Gynecol Oncol 2013;131:667–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boucher NA, Nicolla J, Ogunseitan A, Kessler ER, Ritchie CS, Zafar YY. Feasibility and acceptability of a best supportive care checklist among clinicians. J Palliat Med 2018;21: 1074–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosenberg J. Survey highlights high prevalence of social determinant challenges, need to better address them. Am J Manag Care. 2018. Available at: https://www.ajmc.com/focus-of-the-week/survey-highlights-high-prevalence-of-social-determinant-challenges-need-to-better-address-them. Accessed July 13, 2020. [Google Scholar]
- 33.Draayer A. Integrating social health data to improve care delivery and address social needs. 2018. Available at: http://www.archildrens.org/media/file/82089. Accessed February 23, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.