Abstract
Background
Intraoperative neuromonitoring (IONM) reduces the risk of recurrent laryngeal nerve (RLN) injury during thyroid surgery. However, the use of neuromuscular blocking agents (NMBAs), which are essential to improve intubation conditions, may hinder the electromyographic response during IONM. The aim of this prospective, double-blind, randomized controlled trial was to explore the optimal dosage of cisatracurium to produce adequate muscle relaxation for tracheal intubation without significantly affecting evoked potentials of IONM during thyroidectomy.
Methods
Patients undergoing thyroidectomy with IONM in our institution, with an American Society of Anesthesiologists grade of I–II, aged 18–75 years, and with a body mass index below 32 kg/m2 were enrolled and randomly assigned (by random numbers) to receive 1× (group C1) or 2× (group C2) the effective dose (ED95) of cisatracurium for tracheal intubation. The patients, surgeons, and anesthesiologists in charge were blinded to group assignment. Anesthesia was induced with sufentanil, propofol, and cisatracurium (0.05 mg/kgin group C1, 0.1 mg/kg in group C2). Ease of intubation was evaluated with the intubation condition score (Cooper score) and the intubation difficulty scale (IDS). Amplitudes of evoked potentials during intermittent IONM were compared between groups. The primary outcomes were the Cooper score, the IDS score, and the evoked potentials of IONM.
Results
Fifty-three patients were randomized from October 2019 to November 2020, and 52 were analyzed (with 26 patients in each group). The Cooper score was significantly lower in group C1 [median, 8.0 (interquartile range, 7.0–8.3)] than in group C2 [9.0 (9.0–9.0), P<0.001]. The rate of difficult laryngoscopy without external laryngeal pressure was significantly higher in group C1 than in group C2 (61.5% vs. 11.5%, P<0.001). More patients in group C1 required assistance to complete tracheal intubation (16 vs. 4, P=0.001). The IDS score was significantly higher in group C1 [3.0 (0.0–4.0) vs. 1.0 (0.0–1.0), P=0.045]. There were no significant differences between groups in amplitudes of evoked potentials. No serious adverse events were observed.
Conclusions
A dose of 2× ED95 of cisatracurium provided better intubation conditions and easier tracheal intubation than 1× ED95, without disturbing IONM.
Trial Protocol
Chinese Clinical Trial Registry (No. ChiCTR1900022884).
Keywords: Intraoperative neuromonitoring (IONM), cisatracurium, tracheal intubation, total intravenous anesthesia (TIVA), thyroidectomy
Introduction
Recurrent laryngeal nerve (RLN) injury is a complication of great concern during thyroid surgery. Intraoperative neuromonitoring (IONM) has become a powerful risk minimization tool for prevention of RLN injury in thyroid surgery (1-5). IONM is particularly recommended for use in bilateral operations and surgeries for malignancy (6,7). Standard application of IONM have been developed; however, there remain unresolved issues concerning anesthesia. Neuromuscular blocking agents (NMBAs) are indispensable during tracheal intubation to optimize intubation conditions and to reduce laryngeal morbidity (8-10). However, insufficient neuromuscular blockade recovery may hinder IONM by diminishing the electromyographic (EMG) response (2,11). A negative stimulation during surgery may cause anxiety for surgeons and may prolong operation time.
A small dose of non-depolarizing NMBA is recommended for anesthesia induction, without repeat NMBA administration after intubation, to allow for successful IONM (2). However, insufficient muscle relaxation during intubation may result in a higher incidence of difficult airway and intubation-related complications. Cisatracurium is one of the most commonly used non-depolarizing NMBAs. It has excellent hemodynamic stability because it does not cause histamine release. Furthermore, cisatracurium is largely unaffected by hepatic or renal dysfunction because it is metabolized via Hoffman elimination, which is independent of organ function. These characteristics make cisatracurium favorable for old and critical patients (12,13). Moreover, the recovery index of cisatracurium is slightly shorter than that of rocuronium and other non-depolarizing NMBAs, a quality that may be advantageous during thyroid surgery with IONM (14). Cisatracurium has long been used by clinicians to facilitate intubation for thyroid surgery. However, the dosage of cisatracurium for intubation of patients undergoing thyroid surgery with IONM has generally been determined according to the individual clinician’s preference. Previous literatures have studied the dosage effect of rocuronium (15,16). However, studies on the application of cisatracurium during thyroid surgery with IONM remain limited. The optimal dosage of cisatracurium that both provides adequate muscle relaxation during intubation and allows for reliable timely neuromonitoring interpretations has not been investigated.
This prospective, double-blind, randomized controlled trial aimed to investigate the optimal intubation dosage of the commonly used non-depolarizing NMBA cisatracurium to simultaneously produce optimized intubation conditions and allow successful early IONM detection during thyroidectomy. For all we know, this is the first study investigating on the dosage effect of cisatracurium on IONM in patients undergoing thyroidectomy.
We present the following article in accordance with the CONSORT reporting checklist (available at https://dx.doi.org/10.21037/gs-21-109).
Methods
Participants
This is a prospective, double-blind, randomized controlled trial. The study took place in a tertiary teaching hospital in China. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Peking University Cancer Hospital (No. 2019YJZ53), and all participants provided written informed consent. The study was registered in the Chinese Clinical Trial Registry (No. ChiCTR1900022884). Patients diagnosed with thyroid cancer, scheduled for elective thyroidectomy (with/without central neck dissection) with IONM, with an American Society of Anesthesiologists grade of I–II, aged 18–75 years, and with a body mass index below 32 kg/m2 were enrolled. A research member used statistical software (SPSS, version 19.0; IBM, Chicago, Illinois) to generate numbers for simple randomization. Patients were randomly assigned in a 1:1 ratio to receive 1× (group C1) or 2× (group C2) the effective dose (ED95) of cisatracurium. The patients, surgeons, and anesthesiologists in charge were blinded to group assignment. Random numbers were placed in sealed envelopes by a resident. After all baseline assessments had been completed, each patient’s envelope was opened by a research member who was independent of the recruitment process. Patients with one or more of the following conditions were excluded from the study: (I) severe hypertension, cardiovascular disease, or cerebrovascular disease; (II) pregnancy or lactation; (III) existing laryngeal nerve injury or preoperative vocal fold dysfunction on laryngoscopy; (IV) neuromuscular disorders; (V) treated with medication that interferes with neuromuscular transmission; (VI) risk of difficult face mask ventilation; (VII) any contraindication to the anesthetics used in the study; and (VIII) refusal to participate.
Anesthesia
Anesthesia was induced with intravenous sufentanil (0.3 μg/kg) and propofol (2–3 mg/kg). Cisatracurium (0.05 mg/kg in group C1 and 0.1 mg/kg in group C2) was used for muscle relaxation. Cisatracurium was provided in accordance with group assignment (prepared in a 10-mL syringe with an equal volume of normal saline) by a research nurse not involved in the perioperative anesthesia management or postoperative follow-up. Modified Cormack-Lehane classification was determined, and tracheal intubation was performed in the sniffing position with a Macintosh laryngoscope by an attending anesthesiologist with more than 10 years of clinical experience who was not involved in the detailed preoperative evaluation and who was blinded to group assignment. An endotracheal tube (Nerve Integrity Monitor, NIM; Medtronic, Jacksonville, Florida) was placed (size 6.0 for women and size 7.0 for men) after adequate muscle relaxation, which was evaluated on the basis of the clinician’s experience. Difficult airway was defined as the clinical situation in which a conventionally trained anesthesiologist experienced difficulty with facemask ventilation of the upper airway, difficulty with tracheal intubation, or both (17). If difficult airway occurred due to insufficient muscle relaxation, additional NMBA was allowed to improve intubation conditions, patients were excluded from the study after documentation, and intubation was completed according to the guidelines of the American Society of Anesthesiologists (17). After intubation, the patient’s head and neck were placed in a hyperextended position, the endotracheal tube was connected to a NIM-Response monitor, and the monitor was tested. The stimulator probe was set at 1–2 mA, and an activated evoked potential greater than 100 μV was considered a positive signal. General anesthesia was maintained with target-controlled infusion of propofol (plasma concentration, 2.5–5.0 μg/mL) and remifentanil (plasma concentration, 3.0–5.0 ng/mL) in both groups. Propofol concentration was adjusted to maintain an adequate depth of anesthesia, which was monitored with the bispectral index (spectral entropy value, 40–60). Remifentanil concentration was adjusted according to hemodynamic changes. Intermittent sufentanil was administered according to the anesthesiologist’s preference. No repeat muscle relaxant was allowed after tracheal intubation. If patient bucking or movement occurred during the operation, an extra bolus of propofol (30–50 mg) was administered. Surgeries were performed by the same surgeons. After surgery, patients were transferred to the postoperative anesthetic care unit for further observation. Patients were extubated after fulfilling extubation criteria (responding to verbal commands, achieving adequate spontaneous ventilation and full recovery from muscle relaxation with a train-of-four ratio greater than 0.9 on neuromuscular transmission monitoring).
Measurements
Preoperative evaluation of difficult airway was documented. Difficult laryngoscopy was defined as grade III/IV modified Cormack-Lehane classification (inability to visualize any portion of the vocal cords at conventional laryngoscopy) (17). Difficult tracheal intubation was defined as intubation requiring multiple attempts, in the presence or absence of tracheal pathology (17). All assistance during intubation were documented. If difficult intubation occurred because of insufficient muscle relaxation, additional NMBA was allowed, and intubation was completed according to the guidelines of the American Society of Anesthesiologists (17). These patients were documented and then excluded from the study. Intubation conditions and ease of intubation were evaluated with the Cooper score (Table 1) and intubation difficulty scale (IDS) (Table 2) (18,19). Intubation time was defined as time from insertion of the laryngoscope to the successful recording of capnography. Immediate complications after intubation (e.g., dental trauma, visible lacerations in the oropharynx, laryngospasm, bronchospasm, and blood on the intubation device) were noted. Blood-tinged sputum during extubation was recorded. Post-intubation symptoms (e.g., severe sore throat, odynophagia, and hoarseness) were assessed 30 min after extubation by a nurse from the postoperative anesthetic care unit who was blinded to group assignment. The anesthetic consumption was recorded.
Table 1. Scoring of intubating condition (18).
| Score | Jaw relaxation (laryngoscopy) | Vocal cords | Response to intubation |
|---|---|---|---|
| 0 | Poor (impossible) | Closed | Severe coughing or bucking |
| 1 | Minimal (difficult) | Closing | Mild coughing |
| 2 | Moderate (fair) | Moving | Slight diaphragmatic movement |
| 3 | Good (easy) | Open | None |
Total score of 8–9= excellent; 6–7= good; 3–5= fair; 0–2= poor. Reproduced from [Cooper R, Mirakhur RK, Clarke RS, et al. Comparison of intubating conditions after administration of Org 9426(rocuronium) and suxamethonium. Br J Anaesth 1992;69:269-73.], with permission from Elsevier.
Table 2. Intubation difficulty scale (19).
| Parameter | Score |
|---|---|
| Number of attempts >1 | 1 point each |
| Number of operators >1 | 1 point each |
| Number of alternative techniques | 1 point each |
| Cormack-Lehane grade - 1 | 0 to 3 points |
| Lifting force required | |
| Normal | 0 point |
| Increased | 1 point |
| External laryngeal pressure applied | |
| Not applied | 0 point |
| Applied | 1 point |
| Vocal cord mobility | |
| Abduction | 0 point |
| Adduction | 1 point |
IDS score = sum of points. Adapted from [Adnet F, Borron SW, Racine SX, et al. The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology 1997;87:1290-7.],Copyright (1997), with permission from Wolters Kluwer Health, Inc.
IONM was performed intermittently following a standardized sequence of steps: confirmation of vagus nerve (V1) and RLN (R1) functional integrity before dissection; confirmation of RLN (R2) and vagus nerve (V2) functional integrity after dissection (4). Repeated stimulation was performed every 5 min until a positive EMG signal occurred. Evoked potentials of V1, R1, R2, and V2 were recorded. If the EMG signals were lost during surgery, patients were documented and excluded from the study.
Movement or bucking of the patient during surgery was documented. All adverse events during the study were recorded.
Outcomes
The primary outcomes were the Cooper score, the IDS score, and the evoked potentials of IONM. The secondary outcomes were comparison of intubation-related complications, bucking or movement during surgery, and anesthetic consumption.
Sample size
A preliminary trial conducted by the authors found that the Cooper score was 7.67±1.23 (mean ± SD) in group C1 and 8.56±0.88 in group C2. According to Power Analysis and Sample Size software (version 11.0; NCSS, LLC, Kaysville, Utah), a sample size of 24 patients per group was estimated to have at least 80.0% power at a significance level of 5%.
Statistical analysis
Statistical software (SPSS, version 19.0; IBM, Chicago, Illinois) was used for statistical analysis. Categorical variables were reported as number (percentage) and were analyzed with the Pearson chi-squared test or Fisher’s exact test. Continuous variables were reported as mean ± SD or median (interquartile range). Normally distributed data were analyzed with independent-samples t-test, and non-normally distributed data were analyzed with the Mann-Whitney U test. A value of P<0.05 was considered statistically significant.
Results
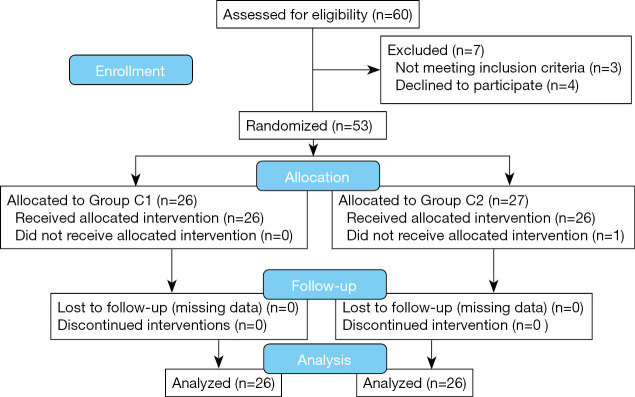
Fifty-three patients were enrolled and randomized from October 2019 to November 2020 (Figure 1). One patient was excluded from the study because the EMG signals were lost during surgery. During surgery, this patient was found to have RLN invasion that required unilateral RLN resection to achieve complete tumor resection. Fifty-two patients were analyzed, with 26 patients in each group. There were no significant differences between the two groups in demographic characteristics or intraoperative data (Table 3). Anesthetic consumption of propofol [group C1: 767.6 mg (578.2, 1,040.9), group C2: 807.6 mg (597.5, 1,097.1); P=0.971], remifentanil [group C1: 699.4 μg (497.9, 1,069.2), group C2: 824.8 μg (535.4, 1,197.0); P=0.288], and sufentanil [group C1: 20.0 μg (19.5, 24.3), group C2: 24.0 μg (20.0, 25.0); P=0.253] were comparable between the two groups.
Figure 1.
Flow diagram.
Table 3. Demographic characteristics and intraoperative data.
| Variable | Group C1 (n=26) | Group C2 (n=26) | Statistics | P | 95% CI |
|---|---|---|---|---|---|
| Age (years) | 42.4±9.9 | 42.4±11.5 | 0.013† | 0.990 | −5.9 to 6.0 |
| Sex (M/F) | 9/17 | 5/21 | 1.564‡ | 0.211 | – |
| Height (cm) | 165.5 (159.5–171.0) | 165.0 (158.0–168.5) | 0.661§ | 0.509 | – |
| Weight (kg) | 68.5±13.6 | 68.3±9.3 | 0.048† | 0.962 | −6.3 to 6.6 |
| BMI (kg/m2) | 24.6±3.0 | 25.3±2.6 | 0.920† | 0.362 | −2.3 to 0.9 |
| Type of thyroidectomy | 1.926‡ | 0.165 | – | ||
| Unilateral lobectomy | 16 (61.5) | 11 (42.3) | |||
| Total thyroidectomy | 10 (38.5) | 15 (57.7) | |||
| Central neck dissection | 24 (92.3) | 21 (80.8) | 0.419 | – | |
| Duration of surgery (min) | 67.0 (51.8–84.5) | 79.5 (50.8–111.5) | 0.979§ | 0.327 | – |
| Bucking | 3 (11.5) | 1 (3.8) | 0.610 | – | |
| Movement | 1 (3.8) | 0 (0.0) | 1.000 | – |
Data are presented as mean ± SD, n (%), or median (interquartile range). Group C1, patients intubated with 1× ED95 (0.05 mg/kg) of cisatracurium; Group C2, patients intubated with 2× ED95 (0.1 mg/kg) of cisatracurium. †, t value; ‡, chi-square value; §, Z value. BMI, body mass index; CI, confidence interval.
The time from injection of cisatracurium during anesthesia induction until initial monitoring with IONM (time to initial monitoring) and the evoked potentials are presented in Table 4. A positive evoked potential at initial monitoring were obtained from all patients in both groups. The amplitudes of the evoked potentials were not significantly different between the two groups.
Table 4. IONM monitoring during surgery.
| Variable | Group C1 (n=26) | Group C2 (n=26) | Statistics | P | 95% CI |
|---|---|---|---|---|---|
| Time to initial monitoring (min) | 39.7±7.8 | 38.2±7.5 | 0.710† | 0.481 | −2.7 to 5.7 |
| V1 (μV) | 561.0 (290.8–1,111.5) | 448.0 (184.0–747.3) | 0.842‡ | 0.400 | – |
| R1 (μV) | 738.0 (482.8–1,332.5) | 580.0 (307.3–1,008.8) | 1.556‡ | 0.120 | – |
| R2 (μV) | 882.0 (396.0–1,377.8) | 777.0 (394.0–1,255.3) | 0.320‡ | 0.749 | – |
| V2 (μV) | 782.0 (342.0–1,005.0) | 471.5 (281.0–1,001.0) | 0.824‡ | 0.410 | – |
Data are presented as mean ± SD or median (interquartile range). Group C1, patients intubated with 1× ED95 (0.05 mg/kg) of cisatracurium; Group C2, patients intubated with 2× ED95 (0.1 mg/kg) of cisatracurium. †, t value; ‡, Z value. CI, confidence interval.
Data regarding the intubation process are presented in Table 5. There were no significant differences between group C1 and group C2 regarding preoperative airway evaluation [mouth opening, group C1: 4.5 cm (4.0, 5.0), group C2: 4.5 cm (4.0, 5.0), P=0.241; thyromental distance, group C1: 8.3 cm (7.5, 8.5), group C2: 8.0 cm (7.9, 8.6), P=0.993; Mallampati classification III/IV, group C1: 9 (34.6%), group C2: 15 (57.7%), P=0.095]. All patients in both groups were successfully intubated. The first-attempt success rate was 96.2% in both groups. Two patients (one in each group) had two intubation attempts and were finally intubated with a Shikani optical stylet due to difficult laryngoscopy despite the assistance of external laryngeal pressure.
Table 5. Data regarding difficulty of intubation.
| Variable | Group C1 (n=26) | Group C2 (n=26) | Statistics | P |
|---|---|---|---|---|
| Cooper score | 8.0 (7.0–8.3) | 9.0 (9.0–9.0) | 4.799† | <0.001*** |
| Cormack-Lehane grade III/IV | 16 (61.5) | 3 (11.5) | 14.016‡ | <0.001*** |
| Required assistance | 16 (61.5) | 4 (15.4) | 11.700‡ | 0.001** |
| IDS score | 3.0 (0.0–4.0) | 1.0 (0.0–1.0) | 2.001† | 0.045* |
| Intubation time (s) | 42.5 (33.0–50.0) | 35.0 (29.8–40.0) | 2.090† | 0.037* |
Data are presented as median (interquartile range) or n (%). Group C1, patients intubated with 1× ED95 (0.05 mg/kg) of cisatracurium; Group C2, patients intubated with 2× ED95 (0.1 mg/kg) of cisatracurium. †, Z value; ‡, chi-square value; *, P<0.05; **, P<0.01; ***, P<0.001. IDS, intubation difficulty scale.
There were no immediate complications after intubation in either group. Intubation-related postoperative complications are presented in Table 6. No serious adverse events were observed.
Table 6. Intubation-related complications.
| Variable | Group C1 (n=26) | Group C2 (n=26) | χ2 | P |
|---|---|---|---|---|
| Blood-tinged sputum during extubation | 5 (19.2) | 3 (11.5) | – | 0.703 |
| Sore throat | 6 (23.1) | 6 (23.1) | 0.000 | 1.000 |
| Odynophagia | 8 (30.8) | 7 (26.9) | 0.094 | 0.760 |
| Hoarseness | 2 (7.7) | 0 (0.0) | – | 0.490 |
Data are presented as n (%). Group C1, patients intubated with 1× ED95 (0.05 mg/kg) of cisatracurium; Group C2, patients intubated with 2× ED95 (0.1 mg/kg) of cisatracurium.
Discussion
The practical implementation of IONM is affected by the use of muscle relaxants. However, the use of muscle relaxants is essential during tracheal intubation. NMBAs improve intubation conditions, abolish upper airway muscle tone (including laryngospasm), reduce the number of intubation attempts, and reduce intubation-related complications (20). Avoidance of NMBAs is associated with increased intubation difficulty (10). Studies have investigated the optimal dosage of rocuronium for anesthesia induction during thyroid surgery with IONM (15,16). However, despite its many advantages, evidence of the dosage effect of cisatracurium in this setting is clearly lacking. The present study investigated the dosage effect of 1× versus 2× ED95 of cisatracurium on intubation conditions and IONM under total intravenous anesthesia (TIVA) in patients undergoing radical thyroidectomy.
Intubation conditions were evaluated with the Cooper score. In the present study, the Cooper score was significantly higher in group C2 than in group C1, indicating that better intubation conditions were obtained with 2× the ED95 of cisatracurium. The rate of difficult laryngoscopy without assistance was significantly higher in group C1 than in group C2. More patients in group C1 required external laryngeal pressure to improve laryngoscopy exposure to complete tracheal intubation. The difficulty of intubation according to IDS score was significantly greater and intubation time was significantly longer in group C1, compared with group C2. These results suggest that tracheal intubation was significantly more difficult in patients who received 1× the ED95 of cisatracurium for anesthesia induction. In contrast, 2× ED95 of cisatracurium provided improved intubation conditions and allowed easier airway management. Despite the differences in intubation conditions and difficulty of intubation, all patients in both groups were successfully intubated. Patients with difficult intubation were successfully managed with external laryngeal pressure, or by using an additional intubation device, such as a Shikani optical stylet. Intubation-related complications were not significantly different between the two groups. The comparable rates of intubation-related complications may be attributed to the fact that intubation in both groups was completed by attending anesthesiologists with more than 10 years of clinical experience.
A positive evoked potential at initial monitoring was obtained from all patients in both groups. The amplitudes of V1, R1, R2, and V2 did not significantly differ between the two groups. These results indicate that spontaneous recovery of cisatracurium-induced neuromuscular paralysis was sufficient to achieve successful IONM in both 1× ED95 and 2× ED95 groups under TIVA. IONM was not affected by dosage (1× ED95 versus 2× ED95) of cisatracurium in the early stage of the operation. In previous studies of rocuronium, 1× the ED95 of rocuronium was recommended to guarantee sufficient recovery of neuromuscular transmission for IONM (15,16,21,22). However, a lower degree of neuromuscular blockade resulted in less favorable intubation conditions (22). Although 2× the ED95 of rocuronium provided better intubation conditions in one study, positive EMG signals were not obtained for all patients until 55 minutes after administration of this dose of rocuronium (15). In the present study, initial monitoring started at 39.7±7.8 and 38.2±7.5 min after administration of cisatracurium in groups C1 and C2, respectively. All patients had a positive signal. We believe one of the reasons for this difference between studies is that cisatracurium has a slightly shorter recovery index than rocuronium and other non-depolarizing NMBAs, which makes it preferable (14,23). The second reason for the difference is the application of TIVA rather than sevoflurane for maintenance of anesthesia in the present study. The enhancement and prolongation of the effect of NMBAs that occurs with inhaled agents were consequently avoided (24-26). Therefore, we recommend cisatracurium at an optimal dosage of 2× ED95 (0.1 mg/kg) for intubation of patients undergoing thyroidectomy with IONM.
The present study had some limitations. First, evaluation of intubation conditions is essentially subjective. Although the anesthesiologists were blinded to group allocation, the group assignment could sometimes be obvious to an experienced anesthesiologist because of differences in the degree of muscle relaxation and intubation response between groups. However, this limitation was inevitable, and the intubation conditions and difficulty of intubation were evaluated with objective scoring systems, which allow some standardization of assessments. Second, a dosage of 3× the ED95 of cisatracurium (standard dose for tracheal intubation) was not studied because of its distinct disadvantage in prolonging neuromuscular blockade, which was observed when IONM was initially applied in our institution. Finally, a high initial EMG amplitude (V1) is recommended for correct interpretation and verification of intact RLN function (3,21). Although all patients in the present study had a positive signal of >100 μV at initial monitoring and the amplitude of V1 was comparable between the two groups, the median amplitude of V1 in group C2 was slightly lower than the recommended high initial EMG amplitude of >500 μV. This is a drawback that must be evaluated individually in this specific clinical setting. Better EMG signals are achieved with a smaller dosage of NMBAs at the expense of less favorable intubation conditions; the opposite is also true.
Conclusions
In conclusion, 2× the ED95 of cisatracurium provided better intubation conditions and easier tracheal intubation, compared with 1× the ED95. Both 1× and 2× the ED95 of cisatracurium at intubation allowed successful detection of IONM with similar amplitude of evoked potentials under TIVA. Therefore, 2× the ED95 of cisatracurium (0.1 mg/kg) can be used as an optimal dose for tracheal intubation in patients undergoing radical thyroidectomy with IONM.
Acknowledgments
We thank Tianxiao Wang, Hao Yu and Yabing Zhang for assisting in the surgical procedures.
Funding: This research was funded by the National Natural Science Foundation of China (No. 81972719).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Peking University Cancer Hospital (No. 2019YJZ53) and all individual participants provided informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://dx.doi.org/10.21037/gs-21-109
Study Protocol: Available at https://dx.doi.org/10.21037/gs-21-109
Data Sharing Statement: Available at https://dx.doi.org/10.21037/gs-21-109
Peer Review File: Available at https://dx.doi.org/10.21037/gs-21-109
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/gs-21-109). The authors have no conflicts of interest to declare.
References
- 1.Fundakowski CE, Hales NW, Agrawal N, et al. Surgical management of the recurrent laryngeal nerve in thyroidectomy: American Head and Neck Society Consensus Statement. Head Neck 2018;40:663-75. 10.1002/hed.24928 [DOI] [PubMed] [Google Scholar]
- 2.Randolph GW, Dralle H, Abdullah H, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 2011;121 Suppl 1:S1-16. 10.1002/lary.21119 [DOI] [PubMed] [Google Scholar]
- 3.Schneider R, Randolph GW, Dionigi G, et al. International neural monitoring study group guideline 2018 part I: Staging bilateral thyroid surgery with monitoring loss of signal. Laryngoscope 2018;128 Suppol 3:S1-S17. [DOI] [PubMed]
- 4.Schneider R, Machens A, Randolph GW, et al. Opportunities and challenges of intermittent and continuous intraoperative neural monitoring in thyroid surgery. Gland Surg 2017;6:537-45. 10.21037/gs.2017.06.08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang S, Zhou L, Lu Z, et al. Systematic review with meta-analysis of intraoperative neuromonitoring during thyroidectomy. Int J Surg 2017;39:104-13. 10.1016/j.ijsu.2017.01.086 [DOI] [PubMed] [Google Scholar]
- 6.Bai B, Chen W. Protective effects of intraoperative nerve monitoring (IONM) for recurrent laryngeal nerve injury in thyroidectomy: meta-analysis. Sci Rep 2018;8:7761. 10.1038/s41598-018-26219-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barczyński M, Konturek A, Pragacz K, et al. Intraoperative nerve monitoring can reduce prevalence of recurrent laryngeal nerve injury in thyroid reoperations: results of a retrospective cohort study. World J Surg 2014;38:599-606. 10.1007/s00268-013-2260-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality of tracheal intubation: a randomized controlled trial. Anesthesiology 2003;98:1049-56. 10.1097/00000542-200305000-00005 [DOI] [PubMed] [Google Scholar]
- 9.Lundstrøm LH, Møller AM, Rosenstock C, et al. Avoidance of neuromuscular blocking agents may increase the risk of difficult tracheal intubation: a cohort study of 103,812 consecutive adult patients recorded in the Danish Anaesthesia Database. Br J Anaesth 2009;103:283-90. 10.1093/bja/aep124 [DOI] [PubMed] [Google Scholar]
- 10.Combes X, Andriamifidy L, Dufresne E, et al. Comparison of two induction regimens using or not using muscle relaxant: impact on postoperative upper airway discomfort. Br J Anaesth 2007;99:276-81. 10.1093/bja/aem147 [DOI] [PubMed] [Google Scholar]
- 11.Marusch F, Hussock J, Haring G, et al. Influence of muscle relaxation on neuromonitoring of the recurrent laryngeal nerve during thyroid surgery. Br J Anaesth 2005;94:596-600. 10.1093/bja/aei110 [DOI] [PubMed] [Google Scholar]
- 12.Lee LA, Athanassoglou V, Pandit JJ. Neuromuscular blockade in the elderly patient. J Pain Res 2016;9:437-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Szakmany T, Woodhouse T. Use of cisatracurium in critical care: a review of the literature. Minerva Anestesiol 2015;81:450-60. [PubMed] [Google Scholar]
- 14.Hemmerling TM, Russo G, Bracco D. Neuromuscular blockade in cardiac surgery: an update for clinicians. Ann Card Anaesth 2008;11:80-90. 10.4103/0971-9784.41575 [DOI] [PubMed] [Google Scholar]
- 15.Lu IC, Tsai CJ, Wu CW, et al. A comparative study between 1 and 2 effective doses of rocuronium for intraoperative neuromonitoring during thyroid surgery. Surgery 2011;149:543-8. 10.1016/j.surg.2010.11.006 [DOI] [PubMed] [Google Scholar]
- 16.Han YD, Liang F, Chen P. Dosage effect of rocuronium on intraoperative neuromonitoring in patients undergoing thyroid surgery. Cell Biochem Biophys 2015;71:143-6. 10.1007/s12013-014-0176-1 [DOI] [PubMed] [Google Scholar]
- 17.Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013;118:251-70. 10.1097/ALN.0b013e31827773b2 [DOI] [PubMed] [Google Scholar]
- 18.Cooper R, Mirakhur RK, Clarke RS, et al. Comparison of intubating conditions after administration of Org 9426 (rocuronium) and suxamethonium. Br J Anaesth 1992;69:269-73. 10.1093/bja/69.3.269 [DOI] [PubMed] [Google Scholar]
- 19.Adnet F, Borron SW, Racine SX, et al. The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology 1997;87:1290-7. 10.1097/00000542-199712000-00005 [DOI] [PubMed] [Google Scholar]
- 20.Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth 2018;120:323-52. 10.1016/j.bja.2017.10.021 [DOI] [PubMed] [Google Scholar]
- 21.Chiang FY, Wu CW, Chang PY, et al. Trans-thyroid cartilage recording for neural monitoring of the recurrent laryngeal nerve in thyroid surgery. Laryngoscope 2020;130:E280-E283. 10.1002/lary.28049 [DOI] [PubMed] [Google Scholar]
- 22.Lu IC, Wu SH, Wu CW. Neuromuscular blockade management for intraoperative neural monitoring. Kaohsiung J Med Sci 2020;36:230-5. 10.1002/kjm2.12153 [DOI] [PubMed] [Google Scholar]
- 23.Keleş GT, Yentür A, Cavuş Z, et al. Assessment of neuromuscular and haemodynamic effects of cisatracurium and vecuronium under sevoflurane-remifentanil anaesthesia in elderly patients. Eur J Anaesthesiol 2004;21:877-81. [DOI] [PubMed] [Google Scholar]
- 24.Amin AM, Mohammad MY, Ibrahim MF. Comparative study of neuromuscular blocking and hemodynamic effects of rocuronium and cisatracurium under sevoflurane or total intravenous anesthesia. Middle East J Anaesthesiol 2009;20:39-51. [PubMed] [Google Scholar]
- 25.Turan G, Dincer E, Ozgültekm A, et al. Recovery from neuromuscular block following infusion of cisatracurium using either sevoflurane or propofol for anaesthesia. Eur J Anaesthesiol 2004;21:751-3. 10.1097/00003643-200409000-00017 [DOI] [PubMed] [Google Scholar]
- 26.Li X, Zhang B, Yu L, et al. Influence of sevoflurane-based anesthesia versus total intravenous anesthesia on intraoperative neuromonitoring during thyroidectomy. Otolaryngol Head Neck Surg 2020;162:853-9. 10.1177/0194599820912030 [DOI] [PubMed] [Google Scholar]