Abstract
Background:
Analyzing health risk factors among current workers by industry and occupation (IO) provides information on disparities between worker groups, especially when comparing workers within manual labor occupations. Mining and oil and gas extraction (OGE) are unique industries with different work environments that could affect health risk factors. The study objective was to compare the prevalence of health risk factors of miners, OGE, other manual labor, and non-manual labor workers.
Methods:
The Behavioral Risk Factor Surveillance System’s IO module was analyzed for years 2013–2017 to compare prevalences of excessive alcohol use, smoking, smokeless tobacco use, seat belt use, inadequate sleep, and obesity among four worker groups. National Health Interview Survey IO codes were used to categorize miners, OGE, other manual labor, and non-manual labor workers.
Findings:
Miners and OGE workers had higher prevalence estimates than both non-manual and manual labor workers for all health risk factors except current smoking. Both miners and OGE workers were significantly more likely than other manual labor workers to report smokeless tobacco use and not always wearing seatbelts. Compared with other manual labor workers, OGE workers were significantly more likely to report obesity, and miners were significantly more likely to report inadequate sleep.
Conclusions/Application to Practice:
Prevalence of most health risk factors differed among miners, OGE, other manual labor, and non-manual labor workers. These differences could lead to disparities in health outcomes. Occupational health professionals in mining and OGE can use this information to inform and target integrated wellness and health and safety programs.
Keywords: miners, oil and gas industry, risk factors
Background
The National Institute for Occupational Safety and Health (NIOSH) has distinct health and safety research programs focused on mining and oil and gas extraction (OGE), both of which have demonstrated disparities in health outcomes (Yeoman et al., 2016; NIOSH, 2015). Providing health information specific to each industry is an important step to allow NIOSH’s Mining and Oil and Gas Programs to individually prioritize further research as well as develop interventions to mitigate health risks. One important focus of NIOSH is respiratory health among coal miners. NIOSH has demonstrated that the prevalence of coal workers’ pneumoconiosis (CWP) has been increasing since 2000, with one in ten long-tenured miners showing evidence of CWP (Blackley, Halldin, & Laney, 2018). Miners other than coal workers also have disparities in health outcomes, with some studies demonstrating that metal and nonmetal miners have excess mortality from cardiovascular disease, as well as elevated risk of lung cancer, nonmalignant respiratory disease, and persistent respiratory symptoms (Yeoman et al., 2016). Excess mortality from cancers of the prostate has been identified among some groups of U.S. oil and gas workers, although no upward trend has been found with increased length of employment (Wong & Raabe, 2000). Data from NIOSH’s National Occupational Mortality Surveillance program have demonstrated that U.S. OGE workers have excess mortality from heart disease and several cancer types (i.e. larynx, prostate, oral cavity, pharynx, bladder, kidney, and mesothelioma) (NIOSH, 2015).
These health outcomes have multifactorial causes. Although most research has focused on the association of these health outcomes with environmental and workplace exposures, other relevant risk factors to consider include genetics, sociodemographic variables (i.e., age, sex, race/ethnicity, and education level), comorbidities, and health risk factors such as smoking, excessive alcohol use, and obesity. Most mining and OGE studies focus on health outcomes, without controlling for underlying health risk factors. Health risk factors have not been well studied in either mining or OGE workers, but the possible contribution of risk factors to disparities in these workers’ health outcomes needs to be evaluated. To improve miner and OGE worker health, focused attention on these workers is necessary to better identify and understand worker health risk factors, their connections to work demands and work conditions, and their potential health outcomes.
Any disparities in health risk factors among miners, OGE workers, and other workers might initially be attributed to the higher prevalence of risk factors that have been noted among general manual labor workers like miners and OGE workers. Studies have demonstrated substantial differences in the prevalence of health risk factors between manual (i.e. farming, construction, maintenance/repair, manufacturing, and transportation) and non-manual (i.e. professional, administrative, management) labor workers. For example, a higher prevalence of cigarette smoking among manual labor occupations has been demonstrated (Cho, Kim, Myong, & Kim, 2013; Bang & Kim, 2001), and differences in smoking prevalence between manual and non-manual labor workers have persisted or widened despite an overall decrease in smoking rates among the general working population (Nelson et al., 1994; Lee et al., 2007). Studies have also found disparities in alcohol use, with manual labor workers having higher average daily alcohol consumption than non-manual labor workers (Harford, Parker, Grant, & Dawson, 1992; Parker & Harford, 1992) and a higher prevalence of excessive alcohol use (Berry, Pidd, Roche, & Harrison, 2007). Disparities in health risk factors among workers in manual and non-manual labor occupations, and within different industries and occupations, can lead to disparities in health outcomes. To improve worker health, we need to reduce these disparities in health risk factors.
To evaluate disparities in health risk factors, researchers use industry and occupation (IO) data from national health surveys such as the Behavioral Risk Factor Surveillance System (BRFSS). IO data can be classified into manual and non-manual labor or into individual industries and occupations. However, the major (highest-level) industry groups combine multiple industries together, and the major occupation groups combine multiple occupations together, which limits the ability to understand risks in specific work groups. For example, the highest male suicide rate in 17 states during 2012 and 2015 was in the Standard Occupation Classification (BLS, 2018) construction and extraction major occupation group (Peterson et al., 2018). The construction and extraction major occupation group was also found to have the highest proportional mortality ratios for opioid overdoses (Morano, Steege, & Luckhaupt, 2018). However, the construction and extraction classification includes construction workers, miners, and OGE workers, making it difficult to determine whether these health outcomes are present across the entire group of workers or are restricted to a particular industry. Mining, except oil and gas,and oil and gas extraction are subsections of the Mining Sector (two-digit code 21) in the North American Industry Classification System (U.S. Census Bureau, 2017), but they are distinct industries that are regulated separately, by the Mine Safety and Health Administration and the Occupational Safety and Health Administration, respectively.
The purpose of this study was to compare the prevalence of health risk factors (i.e., smoking, smokeless tobacco use, inadequate sleep, obesity, excessive alcohol use, and seat belt use) of miners and OGE workers with other workers. We separately compared miners and OGE workers with other manual labor workers and with non-manual labor workers. To our knowledge, this is the first study to compare the prevalence of health risk factors among miners and OGE workers relative to other manual labor workers.
Methods
We used BRFSS data from 32 states that included the optional CDC Industry and Occupation (IO) module in at least one year during 2013–2017. BRFSS is an annual, state-based, random-digit-dialed telephone survey of U.S. non-institutionalized adults aged ≥18 years that is coordinated by the Centers for Disease Control and Prevention (CDC, 2017a). The purpose of the survey was to gather data on health behaviors, chronic health conditions, and use of health services. The survey was comprised of a core questionnaire administered by all states and optional modules or state-added questions that were chosen according to state priorities. NIOSH sponsored the optional Industry and Occupation (IO) module beginning in 2013. In the IO module, respondents reporting current or recent (unemployed for <1 year) employment were asked, “What kind of business or industry do you work in (for example, hospital, elementary school, clothing manufacturing, restaurant)?” and “What kind of work do you do (for example, registered nurse, janitor, cashier, auto mechanic)?” The dataset also included data from functionally equivalent state-added IO questions by Wyoming and Washington BRFSS in 2013 (Washington State Department of Health, 2011–2013; Wyoming Department of Health, 2011–2013). Open-ended responses to the IO module were recorded in text form, and NIOSH subsequently coded these responses using the 2002 and 2010 U.S. Census Bureau industry and occupation codes. The Census Bureau codes are then grouped into broader categories using the National Health Interview Survey (NHIS) simple and detailed recodes (CDC, 2017b).
Study population
The BRFSS population of interest for this study was adults reporting that they were employed for wages, self-employed, or out of work for less than one year. Workers out of work for less than one year were included in our employed definition because the mining and OGE industries workers often are unemployed for periods under one year because of high turnover resulting from changes in commodity prices.
Inclusion and exclusion criteria
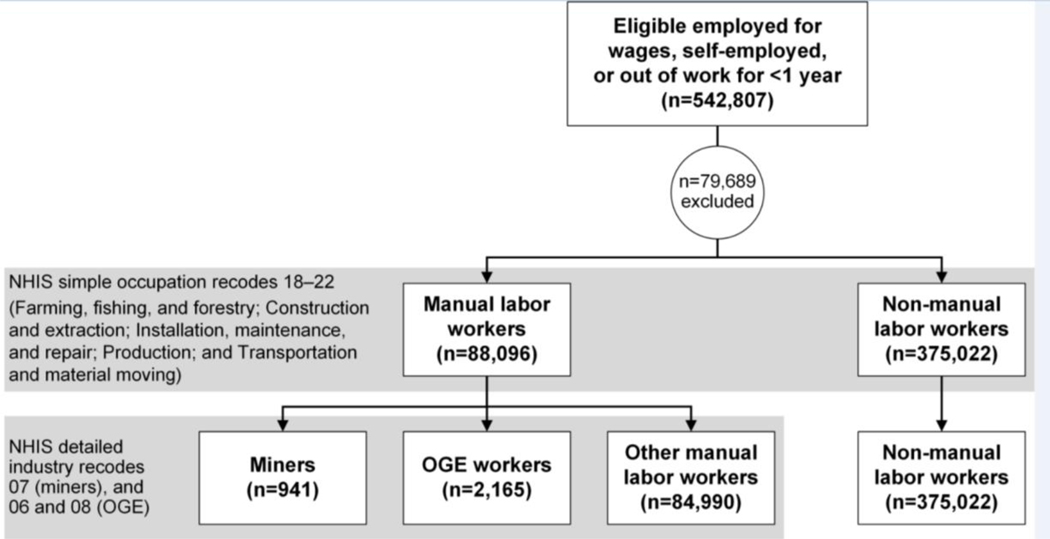
Of 542,807 employed respondents eligible for inclusion, 79,689 (14.7%) were excluded because of ineligible, missing, or insufficient industry or occupation codes, resulting in a final sample size of 463,118 (Figure 1). Persons reporting that they worked in an Armed Forces IO group (n= 1,296) were excluded from analyses because BRFSS does not include a representative sample of the military. The remaining excluded respondents were retirees and students (n=888) and participants with missing or insufficient (i.e. unable to be coded) industry or occupation data (n=77,505).
Figure 1: Eligibility and categorization of miners, oil and gas workers, other manual labor workers, and non-manual labor workers.
Categorization into worker groups
Simple and detailed NHIS occupation and industry codes were used to categorize employed respondents into one of four groups as follows: miners, OGE workers, other manual labor workers, and non-manual labor workers. First, NHIS simple occupation recodes of 18–22 were categorized as manual labor occupations, which comprised the following occupation groups: farming, fishing, and forestry; construction and extraction; installation, maintenance, and repair; production; and transportation and material moving (Krieger, Barbeau, & Soobader, 2005; McCollister et al., 2010). All other occupation codes were considered to be non-manual labor occupations. Next, miners were separated from OGE workers within the manual labor category by using detailed NHIS industry recodes. OGE workers were identified by the detailed groups of oil and gas extraction (recode 06) and support activities for mining (recode 08), and miners were identified by the detailed group of mining except oil and gas (recode 07). Although the detailed recode 08 comprises both mining and OGE support workers, all records coded into this group were placed in the OGE category, because a categorization based on OGE-keyword searching of the free text IO responses demonstrated that 97% of workers with detailed recodes 06 and 08 were OGE workers. Non-manual labor occupations within the mining and OGE industries, including engineering, geology, accounting, and administrative occupations, were placed in the non-manual labor category. In this analysis, miners and OGE workers refer only to those workers who reported working in manual labor occupations within the mining and OGE industries.
Outcome variables
The health risk factors analyzed included the following: current smoking, smokeless tobacco use, excessive alcohol use, obesity, reporting that seat belts were not always used, and inadequate sleep. Current smoking was defined as having smoked at least 100 cigarettes during the lifetime and currently smoking some days or every day. Smokeless tobacco use entailed currently using chewing tobacco or similar smokeless tobacco products some days or every day. Excessive alcohol use was classified as either self-reported binge drinking or heavy alcohol use. Binge drinking was defined as drinking ≥5 alcoholic beverages for men (≥4 for women) on an occasion within the past 30 days. Heavy alcohol use was defined as self-reported drinking >14 drinks per week for men (>7 for women). Obesity status was categorized into three groups based on calculated body mass index (BMI) from self-reported height and weight as follows: <25 kg/m2 representing normal weight or underweight, 25 to <30 kg/m2 representing overweight, and ≥30 kg/m2 representing obesity. Reporting seat belt use nearly always, sometimes, seldom, or never was classified as not always wearing seat belts. Self-reported average number of hours of sleep each day was used to categorize inadequate sleep as averaging <7 hours of sleep per day. The proportion of respondents within each worker category with missing data on the health risk factors ranged from 4.4 to 8.0% for excessive alcohol use; 2.6–4.8% for current smoking; 2.4–5.1% for smokeless tobacco use; 4.9–8.4% for seat belt use; 0.03–0.5% for inadequate sleep; and 2.5–14.1% for obesity.
Statistical analysis
To account for the complex sampling design and differential participation rates among sociodemographic groups, all analyses were conducted using sample weights and survey procedures in SAS 9.4 (SAS Institute, Cary, NC) and SUDAAN 11.0.1 (RTI International, Research Triangle Park, NC). Weighted prevalence and adjusted prevalence ratios were calculated for each health risk factor among the four IO groups of interest. Prevalence ratios were calculated using multiple logistic regression and were adjusted for age category, education level, race/ethnicity, and sex. Because of the skewed distribution of sociodemographic characteristics and small sample size of the mining and OGE groups, the original BRFSS categories were collapsed for age group, education, and race/ethnicity covariates, which resulted in age groups of 18–34 years, 35–54 years, and ≥55 years; education levels of less than high school, completion of high school, and attending or completion of some college or technical school; and race/ethnicity of non-Hispanic white and non-white. The proportion of respondents with missing data for a demographic variable by worker category (i.e. miners, OGE workers, manual and non-manual labor workers) was low, ranging from 0% to 1.7%. For calculation of the prevalence ratios, non-manual labor workers served as the reference group for comparison with miners, OGE workers, and other manual labor workers. The other manual labor workers served as the reference group for comparison with miners and OGE workers. Because the question on number of hours of sleep per day was asked in only three of the five study years, a separate dataset containing data from years 2013, 2014, and 2016 was created and weighted by dividing the final weight for each state by the number of years that the state contributed data, and this outcome was analyzed separately. Statistical significance level was set at α = 0.05. BRFSS data collection received human subjects review and approval. The work was reviewed and approved by the Centers for Disease Control and Prevention under the CDC IRB protocol number 2988.
Results
Among the study sample of 463,118 workers, 88,096 (19.0%) were categorized as manual labor workers, of whom 941 (1.1%) were miners, 2,165 (2.5%) were OGE workers, and 84,990 (96.5%) were other manual labor workers. Of all workers in the mining and OGE industries, 69.5% and 65.6% were categorized as miners and OGE workers (i.e. working within manual labor occupations), respectively. A total of 375,022 (69.1%) workers were categorized as non-manual labor workers, including 413 and 1,135 within the mining and OGE industries, respectively.
The four groups differed in sociodemographic composition. Men accounted for 44.8% of non-manual labor workers but accounted for over 95% of miners and OGE workers and over 85% of other manual labor workers (Table 1). Compared with non-manual labor workers, lower proportions of miners, OGE workers, and other manual labor workers attended or completed college or technical school. Miners had the highest proportion (84.0%) of non-Hispanic white workers, whereas other manual labor workers had the lowest proportion (56.3%). OGE workers had the highest proportion of young workers ≤34 years of age (39.8%), whereas miners had the highest proportion of workers aged ≥55 years (30.2%).
Table 1:
Demographics of non-manual labor workers, miners, oil and gas (OGE) workers, and other manual labor workers, 2013–2017 BRFSS, 32 statesa,b
| Characteristic | Non-manual labor workers | Miners | OGE workers | Other manual labor workers | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unweighted frequency | Weighted percentage of sample population (%) | 95% CI | Unweighted frequency | Weighted percentage of sample population (%) | 95% CI | Unweighted frequency | Weighted percentage of sample population (%) | 95% CI | Unweighted frequency | Weighted percentage of sample population (%) | 95% CI | |
| SEX | ||||||||||||
| Male | 150,246 | 44.8 | 44.3, 45.2 | 902 | 97.6 | 96.1, 99.0 | 2,097 | 97.8 | 96.9, 98.7 | 71,480 | 85.9 | 85.3, 86.5 |
| Female | 224,745 | 55.2 | 54.8, 55.7 | 39 | c | 1.0, 3.9 | 68 | 2.2 | 1.3, 3.1 | 13,503 | 14.1 | 13.5, 14.7 |
| EDUCATION | ||||||||||||
| < High school (H.S.) | 11,624 | 7.0 | 6.7, 7.2 | 57 | 12.6 | 7.4, 17.8 | 267 | 19.6 | 15.9, 23.3 | 9,773 | 22.0 | 21.2, 22.8 |
| Graduated H.S. | 72,470 | 21.3 | 20.9, 21.6 | 487 | 58.6 | 47.7, 69.5 | 1,031 | 45.0 | 41.0, 48.9 | 36,748 | 39.8 | 39.0, 40.7 |
| Attended or graduated college or technical school | 290,370 | 71.6 | 71.2, 72.0 | 394 | 28.8 | 20.6, 36.9 | 865 | 35.4 | 31.6, 39.3 | 38,285 | 38.0 | 37.1, 38.8 |
| AGE (years) | ||||||||||||
| 18–34 | 72,957 | 31.9 | 31.5, 32.3 | 202 | 29.1 | 20.6, 37.6 | 657 | 39.8 | 35.8, 43.7 | 19,279 | 33.4 | 32.5, 34.3 |
| 35–54 | 158,097 | 44.3 | 43.9, 44.8 | 408 | 40.7 | 30.0, 51.4 | 933 | 44.0 | 40.0, 48.1 | 37,027 | 45.9 | 45.1, 46.8 |
| ≥55 | 143,968 | 23.7 | 23.4, 24.1 | 331 | 30.2 | 13.6, 46.8 | 575 | 16.3 | 13.9, 18.6 | 28,684 | 20.7 | 20.1, 21.3 |
| RACE/ETHNICITY | ||||||||||||
| Non-Hispanic white | 295,720 | 64.2 | 63.7, 64.6 | 781 | 84.0 | 78.5, 89.4 | 1,646 | 73.1 | 69.6, 76.7 | 61,860 | 56.3 | 55.4, 57.2 |
| Non-white or Hispanic | 74,757 | 34.6 | 34.1, 35.1 | 141 | 14.3 | 9.2, 19.4 | 494 | 25.7 | 22.2, 29.2 | 21,985 | 42.5 | 42.5, 41.6 |
Participating states: AK, CA, CO, CT, FL, GA, HI, ID, IL, IA, LA, MD, MA, MI, MN, MS, MT, NE, NH, NJ, NM, NY, NC, ND, OR, TN, UT, VT, WA (state-added 2013), WV, WI, WY (state-added 2013)
Estimates do not always round to 100% because of rounding errors and missing responses
Estimate does not meet BRFSS precision guidelines for reporting
The estimated prevalence of excessive alcohol use was over 30% among OGE workers and miners, over 25% among other manual laborers, and was approximately 20% among non-manual labor workers (Table 2). Estimated prevalence of smokeless tobacco was greater than 20% among miners and OGE workers, compared with much lower prevalence of 7.7% and 2.6% among other manual labor and non-manual labor workers, respectively. Estimated prevalence of not always wearing seat belts among miners was approximately 38%. Estimated prevalence of sleeping less than seven hours per night among miners and OGE workers was 57% and 38.5%, respectively. Compared with non-manual labor workers, OGE and other manual labor workers were significantly more likely to smoke or drink alcohol excessively (Table 3). Miners and OGE workers were approximately four times more likely to use smokeless tobacco, and other manual labor workers were almost two times more likely to use smokeless tobacco, compared with non-manual labor workers. Miners were almost three times more likely to report not always wearing seat belts, whereas OGE workers and other manual labor workers were respectively 70% and 30% more likely to report not always wearing seat belts than non-manual labor workers. Miners were 70% more likely to report sleeping less than seven hours per night compared with non-manual labor workers. Obesity was significantly more prevalent among each of the manual labor groups, with miners, OGE, and other manual labor workers having approximately 30%, 50%, and 10% higher prevalence of obesity than non-manual labor workers, respectively.
Table 2:
Unweighted frequency and weighted unadjusted prevalence of health risk factors for non-manual labor workers, miners, oil and gas (OGE) workers, and other manual labor workers, 2013–2017 BRFSS, 32 statesa
| Health risk factor | Non-manual labor workers | Miners | OGE workers | Other manual labor workers | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unweighted frequency | Weighted prevalence | 95% CI | Unweighted frequency | Weighted prevalence | 95% CI | Unweighted frequency | Weighted prevalence | 95% CI | Unweighted frequency | Weighted prevalence | 95% CI | |
| Excessive alcohol | 67,323 | 20.1 | 19.7, 20.4 | 279 | 36.8 | 21.5, 52.1 | 685 | 31.3 | 27.7, 34.8 | 21,043 | 25.4 | 24.7, 26.2 |
| Current smoker | 47,556 | 13.8 | 13.6, 14.1 | 207 | 23 | 15.8, 30.2 | 580 | 26.8 | 23.5, 30.1 | 20,127 | 24.4 | 23.7, 25.2 |
| Current smokeless tobacco | 10,041 | 2.6 | 2.4, 2.7 | 220 | 23.3 | 16.3, 30.4 | 499 | 21.6 | 18.4, 24.8 | 7,571 | 7.7 | 7.2, 8.2 |
| Does not always wear seat belt | 46,657 | 10.1 | 9.8, 10.3 | 282 | 37.6 | 22.4, 52.8 | 640 | 23.7 | 20.3, 27.1 | 18,393 | 16.3 | 15.6, 16.9 |
| Sleep <7 hours per night | 75,415 | 35.4 | 34.8, 35.9 | 309 | 57.1 | 39.2, 74.9 | 585 | 38.5 | 33.7, 43.3 | 19,490 | 38.1 | 37.1, 39.2 |
| Obesity | 99,413 | 25.6 | 25.2, 26.0 | 344 | 31.3 | 22.6, 40.0 | 859 | 39.4 | 35.4, 43.4 | 26,492 | 30.4 | 29.7, 31.2 |
Participating states: AK, CA, CO, CT, FL, GA, HI, ID, IL, IA, LA, MD, MA, MI, MN, MS, MT, NE, NH, NJ, NM, NY, NC, ND, OR, TN, UT, VT, WA (state-added 2013), WV, WI, WY (state-added 2013)
Table 3:
Adjusteda prevalence ratios (aPR) with 95% confidence intervals (CI) of health risk factors comparing miners, oil and gas (OGE) workers, and other manual labor workers with non-manual labor workers, 2013–2017 BRFSS, 32 statesb
| Health risk factor | Non-manual labor workers | Miners | OGE workers | Other manual labor workers | |||
|---|---|---|---|---|---|---|---|
| aPR | aPR | 95% CI | aPR | 95% CI | aPR | 95% CI | |
| Excessive alcohol | 1.0 (ref) | 1.6 | 0.9, 2.6 | 1.3 | 1.1, 1.4 | 1.1 | 1.1, 1.2 |
| Current smoker | 1.0 (ref) | 1.2 | 0.9, 1.7 | 1.4 | 1.2, 1.6 | 1.4 | 1.4, 1.5 |
| Current smokeless tobacco | 1.0 (ref) | 4.1 | 3.1, 5.4 | 3.9 | 3.3, 4.7 | 1.7 | 1.6, 1.9 |
| Does not always wear seat belt | 1.0 (ref) | 2.7 | 1.7, 4.3 | 1.7 | 1.4, 1.9 | 1.3 | 1.2, 1.3 |
| Sleep <7 hours per night | 1.0 (ref) | 1.7 | 1.2, 2.3 | 1.1 | 0.96, 1.2 | 1.1 | 1.02, 1.1 |
| Obesity | 1.0 (ref) | 1.3 | 1.1, 1.5 | 1.5 | 1.3, 1.6 | 1.1 | 1.1, 1.2 |
Note: bold values represent statistically significant differences
Adjusted for sex, age, race/ethnicity, education level
Participating states: AK, CA, CO, CT, FL, GA, HI, ID, IL, IA, LA, MD, MA, MI, MN, MS, MT, NE, NH, NJ, NM, NY, NC, ND, OR, TN, UT, VT, WA (state-added 2013), WV, WI, WY (state-added 2013)
Miners were approximately twice as likely as other manual labor workers to use smokeless tobacco, almost twice as likely to not always wear seat belts, and 50% more likely to sleep less than seven hours per night (Table 4). OGE workers were also more than twice as likely to use smokeless tobacco, 20% more likely to not always wear seat belts, and 30% more likely to be obese compared with other manual labor workers.
Table 4:
Adjusteda prevalence ratios (aPR) with 95% confidence intervals (CI) of health risk factors comparing miners and oil and gas (OGE) workers with other manual labor workers, 2013–2017 BRFSS, 32 statesb
| Health risk factor | Other manual labor workers | Miners | OGE workers | |||
|---|---|---|---|---|---|---|
| aPR | aPR | 95% CI | aPR | 95% CI | ||
| Excessive alcohol | 1.0 (ref) | 1.3 | 0.8, 2.2 | 1.1 | 0.99, 1.3 | |
| Current smoker | 1.0 (ref) | 0.8 | 0.6, 1.1 | 1 | 0.9, 1.1 | |
| Current smokeless tobacco | 1.0 (ref) | 2.3 | 1.7, 2.9 | 2.2 | 1.9, 2.6 | |
| Does not always wear seat belt | 1.0 (ref) | 1.9 | 1.3, 3.0 | 1.2 | 1.1, 1.4 | |
| Sleep <7 hours per night | 1.0 (ref) | 1.5 | 1.1, 2.1 | 1 | 0.9, 1.1 | |
| Obesity | 1.0 (ref) | 1.1 | 0.97, 1.3 | 1.3 | 1.2, 1.4 | |
Note: bold values represent statistically significant differences
Adjusted for sex, age, race/ethnicity, education level
Participating states: AK, CA, CO, CT, FL, GA, HI, ID, IL, IA, LA, MD, MA, MI, MN, MS, MT, NE, NH, NJ, NM, NY, NC, ND, OR, TN, UT, VT, WA (state-added 2013), WV, WI, WY (state-added 2013)
Discussion
This study revealed that miners and OGE workers had higher prevalence estimates than both non-manual and manual labor workers for all health risk factors except current smoking. More importantly, miners and OGE workers combined had significantly higher adjusted prevalence ratios than manual labor workers for four of the six health risk factors. Compared with other manual labor workers, miners had significantly higher prevalence of smokeless tobacco use, not always wearing seat belts, and inadequate sleep, and OGE workers had significantly higher prevalence of smokeless tobacco use, not always wearing seat belts, and obesity. The finding of disparities among miners, OGE workers, and non-manual labor workers is not unexpected, given previous research demonstrating a higher prevalence of health risk factors (including smoking, excessive alcohol use, and obesity) among manual labor workers compared with non-manual labor workers (Bang & Kim, 2001; Berry, Pidd, Roche, & Harrison, 2007; Krieger, Barbeau, & Soobader, 2005; Lee et al., 2007; Lynch, Kaplan, & Salonen, 1997). Our results largely support these studies comparing manual and non-manual labor workers. However, our study also compared workers within the manual labor category, and we would expect the prevalence of health risk factors among miners, OGE workers, and other manual labor workers to be similar. The striking disparities seen between these populations in our analysis indicate the need for further evaluation, including possible work-related contributions to these disparities and whether these disparities place them at higher risk for illnesses or injuries on the job.
In our analysis, the most prominent disparity for workers within general manual labor occupations was the prevalence of smokeless tobacco use. Both miners and OGE workers had significantly higher prevalence of smokeless tobacco use than other manual labor workers. In 2005 and 2010, the estimated prevalence of smokeless tobacco use for construction and extraction workers, which includes mining and OGE workers, was 7.7% and 10.8%, respectively (Mazurek, Syamlal, King, and Castellan, 2014). In contrast, our analysis found miners and OGE workers had prevalence estimates greater than 20%, whereas other manual labor workers had a lower prevalence of 7.7%. Previous analyses likely underestimated smokeless tobacco use for miners and OGE workers because they included miners and OGE workers with the much larger population of construction workers. Higher proportions of blue-collar workers use smokeless tobacco than white-collar workers (Dietz et al., 2011; Marcus, Crane, Shopland, & Lynn, 1989), and persons with no more than a high school education and white males have higher prevalence of use (Mazurek, Syamlal, King, and Castellan, 2014). While these factors likely play a role, miners and OGE workers both had a higher prevalence of use even when compared with other manual labor workers, who have similar education levels and a high proportion of male workers. Many mining and OGE worksites do not permit smoking for safety reasons, which could encourage workers at these sites to switch to smokeless tobacco. However, a previous study demonstrated that workers at sites with smoking restrictions had lower rates of smokeless tobacco use compared with workers at sites without smoking restrictions (Dietz et al., 2011). Although the mechanism behind this finding is unknown, Dietz et al. (2011) postulated that if persons are in smoking-restricted environments where they do not participate in or see others engaging in tobacco use, they are more likely to refrain from use of tobacco products. However, this hypothesis does not seem to apply to miners and OGE workers, many of whom work in smoking-restricted workplaces but still have elevated prevalence of smokeless tobacco use. A better understanding of factors contributing to the disparity in smokeless tobacco use is needed.
The second largest disparity among manual labor workers was seat belt use. Both miners and OGE workers had significantly higher prevalence of not always wearing seat belts than other manual labor workers. Lack of seat belt use is an important risk behavior when considering that motor vehicle crashes (MVCs) are the leading cause of work-related deaths in the United States (BLS, 2004–2018; CDC, 2019). During 2003–2009, MVC fatalities among OGE workers and miners were respectively 8.5 and 2.6 times that of private wage and salary workers (Retzer, Hill, & Pratt, 2013). Loomis (1991) calculated that the age-adjusted odds of MVC-related fatalities for workers in the extractive occupations (i.e. mining and OGE) was 1.8 times that of the control group, which comprised all other occupations. Further study is needed to understand the reasons for lower seat belt use among miners and OGE workers. In focus groups, Canadian OGE workers described multiple risks impacting their commutes to and from work, including fatigue and numerous consecutive shifts (Rothe, 2008). Workers reported a perception that accepting safety risks were expected aspects of their work lives (Rothe, 2008).
The third highest disparity was inadequate sleep, but the difference in prevalence was only significant between miners and other manual labor workers. Miners had significantly higher prevalence of inadequate sleep compared with other manual labor workers. Short sleep duration among miners may increase fatigue-related injuries. Barnes and Wagner (2009) evaluated the effect of shorter sleep duration on underground miners on the Monday after Daylight Savings Time and found that a 40-minute average sleep deficit was associated with 3.6 more injuries and 2,600 more days lost from injuries when compared with other days of the year. The higher prevalence of inadequate sleep among miners could be partly explained by work organization. Workers in the extractive industries (i.e. mining and OGE) work a higher average number of hours each week compared with workers in most other industries (Alterman, Luckhaupt, Dahlhamer, Ward, & Calvert, 2013; BLS, 2017). Shift length could also play a role. Over 50% of active mines employing more than 20 workers use shifts greater than eight hours, and approximately 18% use shifts greater than 10 hours (Mine Safety and Health Administration, 2016). An additional factor is commute time. Miners have the longest commutes of almost all industries due to the remoteness of work locations (Kopf, 2016).
The fourth largest disparity was obesity, but unlike inadequate sleep, the difference in prevalence was only significant for OGE workers. OGE workers and miners had higher prevalence of obesity than other manual labor workers, but only OGE workers significantly so. A 2010 analysis of obesity rates by industry demonstrated an obesity prevalence of 27.9% in the extractive industries, compared with a prevalence of 27.7% among all workers (Luckhaupt, Cohen, Li, & Calvert, 2014). However, in our analysis the estimated prevalence of obesity was 40% and 30% among OGE workers and miners, respectively. Reasons for higher prevalence of obesity among this population warrant further investigation. Working over 40 hours per week is significantly associated with obesity (Luckhaupt, Cohen, Li, & Calvert, 2014), and workers in the extractive industries have the highest average number of hours worked per week of all industries (BLS, 2017). Additionally, miners and OGE workers generally work long (10–12 hour) shifts for multiple days in a row.
As these results show, miners and OGE workers have similarities and differences in prevalence of health risk factors when compared with other manual labor workers. Understanding the reasons for these similarities and differences is an important step in examining disparities in health. Focused investigations of these disparities can lead to the development of relevant and industry-appropriate interventions to decrease health risk factors and improve overall health status among miners and OGE workers. Workplace interventions to improve health risk factors should focus on multiple levels, including individual factors (e.g. task monotony, isolation, coping mechanisms), organizational factors (e.g. job control, job stress, and hazardous exposures), and community factors (e.g., exposure to advertising, availability of resources) (Sorensen, Barbeau, Hunt, & Emmons, 2004). The work environments within mining and OGE could affect health risk factors in a myriad of ways, and further research is needed to understand the interplay between these work environments and health risk factors. For example, many miners work alone, performing monotonous tasks in secluded worksites within mines. Coping mechanisms could include snacking and drinking sugar-sweetened beverages, leading to weight gain. Both miners and OGE workers are exposed to shiftwork, lack of job control, and various environmental hazards, and they might worry less about personal health behaviors as a result. In addition, mining communities and OGE temporary lodging sites tend to be remote and small, and thus workers are likely exposed to similar community factors. Research is needed on the contributions of these various factors to disparities in health risk factors for both mining and OGE workers, and interventions accounting for these factors should be developed.
Implications for Occupational Health Practice
This research indicates that disparities in health risk factors exist between different worker populations within manual labor occupations. Awareness of disparities in health risk factors by occupational health professionals working in mining, OGE, and other manual labor occupations is an important step in decreasing these disparities. Total Worker Health® (TWH) is defined as “policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness prevention efforts to advance worker well-being” (CDC 2018). This approach recognizes that work conditions can affect health problems that were traditionally thought to be unrelated to work (CDC 2018). Occupational health practitioners can use this approach to integrate these findings on health risk factor disparities with traditional occupational health and safety practices to develop more effective programs and policies to improve worker health and well-being. Additionally, these findings indicate that occupational health practitioners need to collaborate with public health providers to address health disparities among their workers.
Strengths and Limitations
Future research should confirm and explain our findings, especially given the limitations to this study. The analysis was exploratory in nature, and similar studies in other manual labor occupations would be beneficial. The small sample size for miners led to wider confidence intervals than the other groups and limited statistical power to detect differences. Coding workers’ free text responses to the BRFSS industry and occupation questions, and using NHIS industry and occupation codes to distinguish miners from OGE workers, and manual from non-manual labor workers, could have resulted in some misclassification of industry or occupation. To check for possible misclassification, we conducted keyword searches of industry and occupation free text responses to identify miners and OGE workers. Comparing keyword search with NHIS code results, we determined that misclassification was minimal (<4%). The dataset included 32 states that adopted the IO Module during at least one study year, and thus these findings might not be representative of the entire U.S. In particular, some states with prominent mining or OGE activities, such as Texas, Nevada, Arizona, Pennsylvania, and Kentucky did not adopt the IO module. Additionally, the BRFSS data are cross-sectional and no conclusions can be drawn regarding causality. Furthermore, missing data within BRFSS can introduce bias. In our analysis, missing data were largely minimal for all risk factors but obesity, in which approximately 14% of miners had missing data. Finally, no information on workplace exposures is available in BRFSS.
Conclusions
Despite limitations, to our knowledge this is the first study using the BRFSS data to separate mining from OGE worker respondents and to evaluate these groups independently for prevalence of several health risk factors. This study provides information on similarities and differences in health risk factors among mining, OGE, other manual labor workers, and non-manual labor workers. Although differences in prevalence of health risk factors between manual and non-manual labor have been demonstrated previously (Lee et al., 2007; Sorensen, Barbeau, Hunt, & Emmons, 2004), comparisons between various manual labor workers are less common. Given disparities in prevalence between miners, OGE workers, and other manual labor workers, investigations of smokeless tobacco use, seat belt use, obesity, and inadequate sleep are needed to evaluate reasons why miners or OGE workers have higher prevalence of these risk factors than workers in similar manual labor occupations. These investigations should also evaluate whether these risk factors increase workers’ risk for illness or injury at work. These studies will be an essential step in understanding commonalities and differences in the interaction of work experiences and health risk factors among workers. Improved understanding of this interaction could lead to strategies to decrease health disparities between various worker populations.
Applying Research to Practice.
The findings of this study demonstrate that miners and oil and gas extraction (OGE) workers have higher prevalence estimates than both non-manual and manual labor workers for smokeless tobacco use, excessive alcohol, not always wearing seat belts, inadequate sleep, and obesity. Additionally, miners and OGE workers combined had significantly higher adjusted prevalence ratios than manual laborers for smokeless tobacco use, not always wearing seat belts, inadequate sleep, and obesity. A better understanding is needed of the underlying reasons for differences in health risk factors between various manual labor worker groups. Awareness of these disparities by occupational health professionals within mining, OGE, and other manual labor occupations can be used to inform integrated wellness and health and safety programs by assessing for these risk factors and targeting interventions to improve overall health.
Acknowledgements:
We wish to thank staff, coders, and data managers of the NIOSH Division of Field Studies and Engineering; and BRFSS state coordinators, interviewers, and managers from all states that provided industry and occupation data.
Funding: The authors report that there was no funding source for the work that resulted in the article or the preparation of the article.
Footnotes
Institution and Ethics approval and informed consent: Work reviewed and approved by Centers for Disease Control and Prevention. CDC IRB protocol number 2988, OMB control number 0230–1061 was used.
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention. Mention of any company or product does not constitute endorsement by NIOSH.
Conflict of Interest: Authors declare no conflicts of interest.
References
- Alterman T, Luckhaupt SE, Dahlhamer JM, Ward BW, & Calvert GM (2013). Prevalence rates of work organization characteristics among workers in the U.S.: Data from the 2010 National Health Interview Survey. American Journal of Industrial Medicine, 56, 647–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bang KM, & Kim JM (2001). Prevalence of cigarette smoking by occupation and industry in the United States. American Journal of Industrial Medicine, 40, 233–239. [DOI] [PubMed] [Google Scholar]
- Barnes CM, & Wagner DT (2009). Changing to daylight saving time cuts into sleep and increases workplace injuries. Journal of Applied Psychology, 94(5), 1305–1317. [DOI] [PubMed] [Google Scholar]
- Berry JG, Pidd K, Roche AM, & Harrison JE (2007). Prevalence and patterns of alcohol use in the Australian workforce: findings from the 2001 National Drug Strategy Household Survey. Addiction, 102(9), 1399–1410. [DOI] [PubMed] [Google Scholar]
- Blackley DJ, Halldin CN, & Laney AS (2018). Continued increase in prevalence of coal workers’ pneumoconiosis in the United States, 1970–2017. American Journal of Public Health, 108,1220–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics (BLS, 2004–2018). Fatal occupational injuries resulting from transportation incidents and homicides, all United States, 2003–2017. Retrieved from https://www.bls.gov/iif/oshcfoi1.htm.
- Bureau of Labor Statistics (BLS, 2017). Average weekly hours and overtime of production and nonsupervisory employees on private nonfarm payrolls by industry sector, seasonally adjusted (Economic News Release, Table B7). Retrieved from https://www.bls.gov/news.release/empsit.t23.htm.
- Bureau of Labor Statistics (BLS, 2018). Standard Occupational Classification 2018. Retrieved from https://www.bls.gov/soc/.
- Centers for Disease Control and Prevention (CDC, 2017a). Behavioral Risk Factor Surveillance System Survey Data 2017. Retrieved from https://www.cdc.gov/brfss/data_documentation/index.htm.
- Centers for Disease Control and Prevention (CDC, 2017b). National Health Interview Survey sample adult layout 2017. Retrieved from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2017/samadult_layout.pdf.
- Centers for Disease Control and Prevention (CDC, 2018). Total Worker Health. Retrieved from https://www.cdc.gov/niosh/twh/totalhealth.html.
- Centers for Disease Control and Prevention (CDC, 2019). Motor vehicle safety at work. Retrieved from https://www.cdc.gov/niosh/motorvehicle/resources/crashdata/facts.html.
- Cho Y-S. Kim H-R, Myong J-P, Kim HW (2013). Association between work conditions and smoking in South Korea. Safety and Health at Work, 4, 197–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz NA, Lee DJ, Fleming LE, LeBlanc WG, McCollister KE, Arheart KL, et al. (2011). Trends in smokeless tobacco use in the U.S. workforce: 1987–2005. Tobacco Induced Diseases, 9, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford TC, Parker DA, Grant BF, & Dawson DA (1992). Alcohol use and dependence among employed men and women in the United States in 1988. Alcoholism, Clinical and Experimental Research, 16(2), 146–148. [DOI] [PubMed] [Google Scholar]
- Kopf D. (2016, February 23). Which professions have the longest commutes? Priceonomics. Retrieved from https://priceonomics.com/which-professions-have-the-longest-commutes/. [Google Scholar]
- Krieger N, Barbeau E, & Soobader MJ (2005). Class matters: U.S. versus U.K. measures of occupational disparities in access to health services and health status in the 2000 U.S. National Health Interview Survey. International Journal of Health Services, 35(2), 213–236. [DOI] [PubMed] [Google Scholar]
- Lee DJ, Fleming LE, Arheart KL, LeBlanc WG, Caban AJ, Chung-Bridges K, et al. (2007). Smoking rate trends in U.S. occupational groups: the 1987 to 2004 National Health Interview Survey. Journal of Occupational and Environmental Medicine, 49(1), 75–81. [DOI] [PubMed] [Google Scholar]
- Loomis DP (1991). Occupation, industry, and fatal motor vehicle crashes in 20 states, 1986–1987. American Journal of Public Health, 81, 733–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luckhaupt SE, Cohen MA, Li J, & Calvert GM (2014). Prevalence of obesity among U.S. workers and associations with occupational factors. American Journal of Preventive Medicine, 46(3), 237–248. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA, & Salonen JT (1997). Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Social Science and Medicine,, 44(6), 809–819. [DOI] [PubMed] [Google Scholar]
- Marcus AC, Crane LA, Shopland DR, & Lynn WR (1989). Use of smokeless tobacco in the United States: recent estimates from the current population survey. National Cancer Institute Monographs, 8, 17–23. [PubMed] [Google Scholar]
- Mazurek JM, Syamlal G, King BA, & Castellan RM (2014). Smokeless tobacco use among working adults – United States, 2005 and 2010. MMWR Morbidity and Mortality Weekly Report,, 63(22), 477–482. [PMC free article] [PubMed] [Google Scholar]
- McCollister KE, Arheart KL, Lee DJ, Fleming LE, Davila EP, LeBlanc WG, et al. (2010). Declining health insurance access among U.S. Hispanic workers: Not all jobs are created equal. American Journal of Industrial Medicine, 53, 163–170. [DOI] [PubMed] [Google Scholar]
- Mine Safety and Health Administration (MSHA, 2016). Mines dataset. Retrieved from https://arlweb.msha.gov/OpenGovernmentData/OGIMSHA.asp.
- Morano LH, Steege AL, & Luckhaupt SE (2018). Occupational patterns in unintentional and undetermined drug-involved and opioid-involved overdose deaths – United States, 2007–2012. MMWR Morbidity and Mortality Weekly Report, 67(33), 925–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health (NIOSH, 2015). National Occupational Mortality Surveillance (NOMS) 2015. Retrieved from https://www.cdc.gov/niosh/topics/noms/noms2charts/oil_gas_extraction/ind-nc-48.html.
- Nelson DE, Emont SL, Brackbill RM, Cameron LL, Peddicord J, & Fiore MC (1994). Cigarette smoking prevalence by occupation in the United States. A comparison between 1978 to 1980 and 1987 to 1990. Journal of Occupational Medicine, 36(5), 516–525. [PubMed] [Google Scholar]
- Parker DA, & Harford TC (1992). The epidemiology of alcohol consumption and dependence across occupations in the United States. Alcohol Health and Research World, 16(2):97–105. [Google Scholar]
- Peterson C, Stone DM, Marsh SM, Schumacher PK, Tiesman HM, McIntosh WL, et al. (2018). Suicide rates by major occupational group – 17 states, 2012 and 2015. MMWR Morbidity and Mortality Weekly Report, 67, 1253–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retzer KD, Hill RD, & Pratt SG (2013). Motor vehicle fatalities among oil and gas extraction workers. Accident Analysis and Prevention, 51, 168–174. [DOI] [PubMed] [Google Scholar]
- Rothe JP (2008). Oil workers and seat-belt wearing behavior: the northern Alberta context. International Journal of Circumpolar Health, 67(2–3), 226–234. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Hunt MK, & Emmons K. (2004). Reducing social disparities in tobacco use: a social-contextual model for reducing tobacco use among blue-collar workers. American Journal of Public Health, 94(2), 230–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2017). North American Industry Classification System. Retrieved from https://www.census.gov/eos/www/naics/.
- Washington State Department of Health (WSDOH), Center for Health Statistics, Behavioral Risk Factor Surveillance System, supported in part by Centers for Disease Control and Prevention, Cooperative Agreement, U58/SO000047–1 through 3. (2011–2013). [Google Scholar]
- Wyoming Department of Health (WDH), Public Health Division, Behavioral Risk Factor Surveillance System, supported in part by Centers for Disease Control and Prevention, Cooperative Agreement, U58/SO000016–1 through 3. (2011–2013). [Google Scholar]
- Wong O, & Raabe GK (2000). A critical review of cancer epidemiology in the petroleum industry, with a meta-analysis of a combined database of more than 350,000 workers. Regulatory Toxicology and Pharmacology, 32, 78–98. [DOI] [PubMed] [Google Scholar]
- Yeoman KM, Halldin CN, Wood J, Storey E, Johns D, & Laney AS (2016). Current knowledge of US metal and nonmetal miner health: Current and potential data sources for analysis of miner health status. Archives of Environmental and Occupational Health. Retrieved from https://www.tandfonline.com/doi/full/10.1080/19338244.2014.998330. [DOI] [PMC free article] [PubMed] [Google Scholar]