Abstract
Background:
The manner in which posttraumatic stress disorder (PTSD) develops remains largely unknown. PTSD is comprised of 20 symptoms across 4 clusters. These clusters were hypothesized to reflect a failure of recovery model in which intrusive symptoms appear first. Intrusive symptoms led to avoidance of trauma-related stimuli, which resulted in sustained arousal. The sustained arousal ultimately led to dysphoria.
Methods
This hypothesized symptoms progression was evaluated during the acute post trauma period (the first 30 days post event). Participants (N = 80) reported their PTSD symptoms for 30 days via mobile devices. Using a short-term dynamic modeling framework, a temporal and contemporaneous model of PTSD symptoms were obtained.
Results:
In the temporal network, a fear-conditioning component was identified that supported the hypothesized set of relations among symptom clusters. The contemporaneous network was classified by two subnetworks. The first corresponded to a fear conditioning model that included symptoms of intrusions and avoidance. The second included symptoms of dysphoria and arousal.
Conclusions:
These findings suggest that, following a trauma, there may be a fear-conditioning process that involves intrusive, avoidance, and arousal symptoms. Dysphoric symptoms were also present, but developed as a partially distinct component.
Keywords: PTSD, Trauma, Stress
Exposure to traumatic events markedly increases risk for a range of mental health conditions including posttraumatic stress disorder (PTSD) (Bryant et al., 2010; Zatzick et al., 2007). PTSD is conceptualized as a failure of the natural recovery process (Yehuda & LeDoux, 2007) given that the majority (77%) of those exposed to a traumatic event will recover (Zatzick et al., 2007). However, the process by which PTSD develops is complex and largely unknown (Galatzer-Levy & Bryant, 2013). Such complexity has prevented the development of methods to accurately predict and prevent PTSD (Kearns, Ressler, Zatzick, & Rothbaum, 2012). An improved understanding of how PTSD symptoms develop in the month after a trauma, referred to as the acute post trauma period, is necessary to develop these clinical tools.
The PTSD diagnosis, according to the DSM 5, is comprised of 20 symptoms across 4 clusters [Intrusions, Avoidance, Negative alterations to cognition and mood (NACM), and Alterations to arousal and reactivity (AAR)]. These clusters are posited to reflect the process by which recovery after a trauma is incomplete (McNally, 2012). Trauma cues and intrusive memories result in strong emotional and physiological reactions. Such reactions lead to avoidance of thoughts and cues about the event (Ehlers & Clark, 2000). Intrusions and avoidance result in an increased sensitivity to threat (Bryant et al., 2017; Price, Legrand, Brier, & Hébert-Dufresne, 2019). This portion of the process most closely resembles a fear conditioning model (Bryant et al., 2017; Hoge et al., 2016; Zoellner, Rothbaum, & Feeny, 2011). The sensitization to threats ultimately results in a dysphoric mood (Ehlers & Clark, 2000). The theorized linear progression of symptoms suggests each cluster does not contribute to the diagnosis equally during the acute post trauma period. It also simplifies what is likely a complex and nonlinear process (Bryant et al., 2017; Price et al., 2019; Stockert, Fried, Armour, & Pietrzak, 2018). Empirical investigations that model the complexity of these hypothesized relations are needed.
Longitudinal studies provide partial support for the theorized progression of symptoms within a failure of recovery model. In a study of traumatic injury survivors assessed from the time of the trauma through the following year, AAR and intrusions symptoms were elevated relative to avoidance symptoms in the week after the trauma (O’Donnell, Elliott, Lau, & Creamer, 2007). A similarly designed study that assessed symptoms over 12 months also reported that AAR and intrusions symptoms were initially elevated shortly after the trauma whereas negative mood symptoms were relatively lower (Schell, Marshall, & Jaycox, 2004). Importantly, this study also examined interactions between the symptom clusters. Elevated AAR and intrusions were the only clusters to influence other symptom clusters. Taken together, these results indicate that PTSD development is a dynamic process in which symptoms interact over time (Gelkopf et al., 2017). As hypothesized, intrusions and AAR symptoms may be more important early on and lead to other symptoms in the disorder. Further examination of these relations within the acute post trauma period are needed. Examining the associations between specific symptoms may be beneficial because each symptom cluster contains several constructs. For example, AAR includes hyperarousal and poor sleep and these symptoms may contribute to PTSD in a different manner.
Network models conceptualize psychopathology as an organized set of relations between symptoms (Borsboom & Cramer, 2013). Networks have been applied to the PTSD diagnosis in cross-sectional studies among individuals with established trauma histories (Armour, Fried, Deserno, Tsai, & Pietrzak, 2017; McNally et al., 2015; Price et al., 2019). Only one study has examined the network structure of PTSD in the acute post trauma period (Bryant et al., 2017). Symptoms of intrusions such as thought intrusions and reactivity to trauma cues were highly central. Centrality refers to how important a symptom is to the network structure (Borgatti, 2005). In a network of the same sample assessed 12-months post-trauma, reactivity to trauma cues remained central, but the centrality of arousal symptoms increased. Furthermore, overall network density was stronger at 12-months than during the acute post trauma period. These results are consistent with the findings of other work in which intrusion symptoms were prominent immediately following a trauma and arousal symptoms became more pronounced in the following months (Shalev et al., 2000; Stam, 2007). Cross-sectional networks, however, are unable to examine symptom dynamics – how the symptoms interacted longitudinally.
The interactions among PTSD symptoms can be conceptualized as a short-term dynamic system (Bringmann et al., 2013). Short-term dynamics refers to determining how variables affect one another over brief time intervals. This modeling approach determines how a symptom at a given time point (t) is affected by other symptoms and itself at the previous time point (t-1). These relations create a directed temporal network. Of interest are the in strength and out strength of symptoms. In strength refers to the sum of edge weights that a symptom has going to it, which determines the extent it is affected by other symptoms at the previous time point. Out strength refers to the sum of edge weights that a symptom has going from it, which determines the extent that it affects other symptoms at the next time point.
Only one study to date has used a short-term dynamic model to examine PTSD symptoms (Greene, Gelkopf, Epskamp, & Fried, 2018). In a large sample of civilians exposed to an ongoing military conflict, PTSD symptoms were measured for 30 days. Within the temporal network, exaggerated startle had the strongest out strength. Avoidance of trauma-related thoughts also had a modest out strength. Intrusions symptoms had a modest in strength, but a relatively low out strength. These relations differed from those that were theorized to explain the development of PTSD. The authors attributed these results to the ongoing nature of the trauma. Continuous threat exposure may have increased the importance of arousal. It remains unclear how symptoms interact with one another during the acute post trauma period when the trauma has ended. Such interactions may help determine if the failure of recovery model is helpful in understanding how PTSD develops after a traumatic event.
The present study was an exploratory investigation of the short-term dynamics of PTSD symptoms after a traumatic injury. The overarching hypothesis was that the dynamic network would support a failure of recovery model in which intrusions led to avoidance, which led to arousal, which led to dysphoria. Specifically, it was hypothesized that that intrusion symptoms would have high out strength and low in strength. AAR symptoms were hypothesized to have the highest in strength. NACM and avoidance symptoms were hypothesized to have low out strength and a high in strength. These relations were consistent with prior work that proposed trauma-related intrusions results in avoidance, sustained arousal, and dysphoric mood (Bryant et al., 2017; Ehlers & Clark, 2000). Furthermore, a contemporaneous network that modeled the relations of symptoms occurring within the same time period (t) was estimated. Such a network allows for comparisons of symptom relations within a time period to those across a time period. It was hypothesized that intrusion symptoms were at the center of the contemporaneous network and dysphoric symptoms were at the periphery.
Methods
Participants
Participants (N = 80) were recruited from a Level 1 Acute and Critical Care Service in the Northeastern US. The mean age was M = 34.59, SD = 10.23 and the majority of the sample was male (n = 48, 60.0%).
Measures
Standardized Trauma Interview (STI; Foa & Rothbaum, 2001).
The STI is a 41-item interview assessing relevant aspects of the trauma. The STI was only used to determine if the most recent traumatic event met criterion A for a diagnosis of PTSD.
PTSD Checklist-5 (PCL; Blevins, Weathers, Davis, Witte, & Domino, 2015):
The PCL-5 is a 20-item self-report measure that assesses PTSD symptoms experienced over the last month according to DSM 5 criteria. Items assess symptoms on a 0–4 point Likert scale. Total scores range from 0–80.
Mobile Assessment:
Each mobile assessment consisted of 9 items. These included the eight items of the abbreviated PCL-5 (Table S1: Price, Szafranski, van Stolk-Cooke, & Gros, 2016) and an additional item from the PCL-5 assessing sleep (Item 20). The abbreviated scale includes 2 items from each cluster of PTSD. The PCL assessment was linked to the trauma for which the participant presented at the hospital and anchored to the past day. The abbreviated PCL was used to improve the feasibility of data collection and reduce participant burden (Price, van Stolk-Cooke, Brier, & Legrand, 2018; Price et al., 2014)
Procedure
The procedures that were used in this study are described in detail in the supplemental materials and elsewhere (Price et al., 2018). Participants were met bedside M = 4.88, SD = 5.22 days after their traumatic event. The most common type of trauma exposure was motor vehicle accident (48.7%). The variability in days in which participants were approached was due to ongoing clinical care. Participants downloaded a mobile application [Metricwire (Waterloo, ON)] to their device that administered the surveys on a fixed schedule for 30 days after the initial assessment. All study procedures were approved by the Institutional Review Board at the location in which the study was conducted.
Data Analytic Plan
All analyses were conducted in R (version 3.5.1). Mobile responses obtained between 5 and 34 days post trauma using a lag of 1 day were used to estimate the networks. The response rate across 30 days was M = 59.4% (SD = 26.0%, range = 4–30), which is comparable to other samples (Bunnell et al., 2019; Davidson, Bunnell, & Ruggiero, 2017; Greene et al., 2018). A total of 1439 time points were used with less than 1% missing data within each time point. Mutlilevel vector autoregressive (mlVAR) models were estimated using the mlVAR package (version 0.4.2, Eskamp et al., 2018). Networks were estimated using the two-step multilevel VAR method (for a detailed overview of this approach see: Eskamp et al., 2018; Bringmann et al., 2013). A network is created by first fitting a set of multilevel models in which each variable in the analysis at time t is predicted by itself and all other variables in the model at time t-1. The multilevel models included fixed effects and random effects. Due to the number of variables in the current model, random effects were not correlated (Eskamp et al., 2018). The fixed effects from this step comprised the edges of a directed network in which edges were interpreted as the extent that the origin variable at t-1 predicted the endpoint variable at t. The second step conducted another set of multilevel models with the residuals from the first step as the outcome and all other variables measured at the same time point as predictors. The fixed effects from this step constructed a contemporaneous network in which edges represented the association between variables within a given time point. This network was estimated using the “or” rule, in which an edge was retained if one of the edges between two variables in the contemporaneous network was significant. There were only two edges in which only one path had p > 0.05. These paths were p < .06, however. The threshold for retaining an edge was held at a significant relation at p < .05 due to the exploratory nature of the current study (Wasserstein, Schirm, & Lazar, 2019).
Networks were plotted using the qgraph (version 1.5) and igraph (version 1.2.2) packages according to the Fruchterman and Reingold algorithm (1991). The strength of the connectivity between nodes is represented by the thickness of the edge. For the temporal model, self-loops were allowed and represented visually by a circular arrow on the node. A self-loop indicates that a given symptom predicts itself at the following time point.
Centrality metrics were calculated for the temporal and contemporaneous networks. Centrality is a method of describing how nodes fit into a network’s structure. Of interest were four metrics of centrality: Strength, Triangles, Betweenness, and K-Core Decomposition. Strength refers to the sum of the edge weights associated with a node. For the temporal network, in strength and out strength were calculated separately. For the contemporaneous network, total strength was used in which each edge was counted once. Triangles refer to the number of node triples that are completely connected. The number of triangles that a node is part of determines the extent that a node is influential in the network (Borgatti, 2005). In mlVAR, the edges are defined by regression coefficients and so a triangle suggests that one node has both a direct effect and an indirect effect on a second node via a third node. Betweenness refers to the inverse of the number of shortest paths between all pairs of nodes that include a given node. Finally, a K-Core decomposition was conducted using the onion approach (Hébert-Dufresne, Grochow, & Allard, 2016). This method classifies nodes according to layers that are based on how well connected a node is to other high degree nodes (degree referring to a count of the edges to a node). At the lowest layers are nodes with low degree with edges to other low degree nodes. As the algorithm decomposes the network, nodes with a high degree that are connected to other nodes with a high degree are placed at higher layers. Nodes at the highest layers form the core of the network. The K-Core decomposition was conducted on the contemporaneous network. A detailed script that outlines these analyses is provided in the supplemental materials (S2).
Results
Descriptive information is presented in Table 1. Figure 1 depicts the temporal network of the 9 included PTSD symptoms. The network included a 6-node component and three independent nodes. The network had a low density (16.0% of possible edges). The large component consisted of six symptoms. Emotional reactivity (I4) had an out strength of 0.23 and a 0 in strength. It was the only symptom to predict other symptoms but not be predicted by other symptoms or itself and thus reflected a starting point (Table 2). Exaggerated Startle (AAR4) had the highest in strength and a 0 out strength, suggesting that it was a terminal point. Low Interest (NACM5) had the highest out strength, predicting 4 symptoms including itself. This symptom also had a modest in strength, suggesting it was an important node on the network. Indeed, Low Interest (NACM5) had the highest betweenness score. As further evidence of the importance of Low Interest (NACM5) in this network, it was part of 3 triangles, suggesting that it had direct and indirect effects on three other symptoms [Avoidance: Internal (AR1), Avoidance: External (AR2), and Exaggerated Startle (AAR4)]. The majority of the symptoms in the larger component were part of at least 1 triangle.
Table 1.
Descriptive statistics for PCL items over time.
| Day 10 | Day 20 | Day 30 | |
|---|---|---|---|
| I1: Thought Intrusions | 0.78 (0.98) | 0.71 (0.93) | 0.62 (0.75) |
| I4: Emotional Reactivity to Cues | 0.93 (1.15) | 0.84 (1.02) | 0.85 (0.93) |
| A1: Avoidance: External | 0.57 (0.83) | 0.54 (0.83) | 0.48 (0.71) |
| A2: Avoidance: Internal | 0.62 (0.86) | 0.62 (0.87) | 0.60 (0.79) |
| NACM2: Neg Thoughts about Self, Others, World | 0.77 (0.91) | 0.77 (1.05) | 0.97 (1.22) |
| NACM5: Low Interest | 0.82 (1.08) | 0.67 (0.89) | 0.76 (1.08) |
| AAR4: Startle | 0.63 (0.90) | 0.46 (0.90) | 0.53 (0.90) |
| AAR5: Concentration Difficulties | 1.04 (1.12) | 0.89 (0.96) | 0.80 (1.1) |
| AAR6: Sleep Difficulties | 1.29 (1.17) | 1.49 (1.08) | 1.22 (1.18) |
| Baseline Total PCL-5 | 24.60 (15.06) | - | - |
Note: I = Intrusions. A = Avoidance. NACM = Negative Alterations to Cognition and Mood. AAR = Alterations to Arousal and Reactivity. Values in parentheses are SDs.
Figure 1.
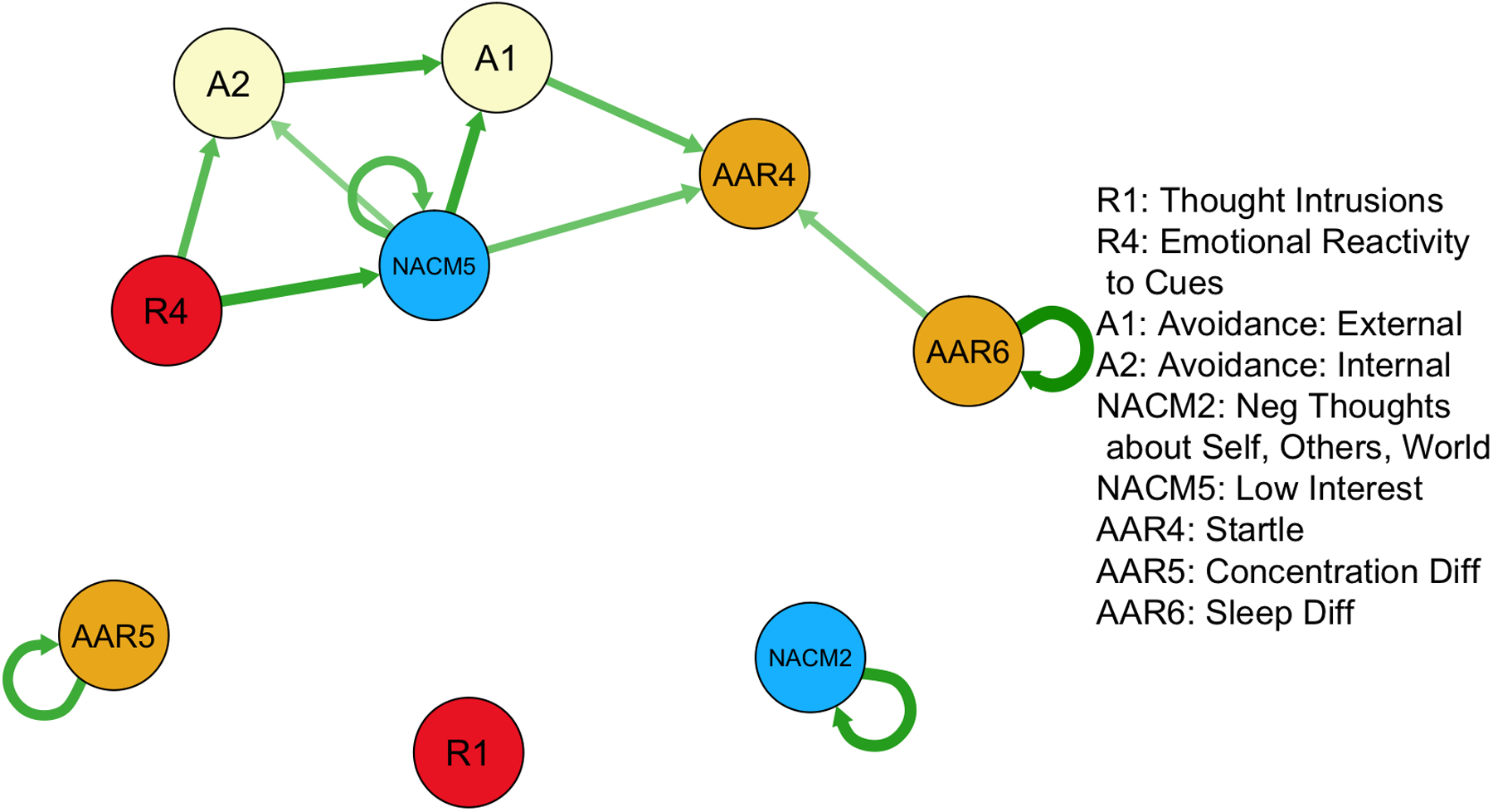
Temporal network of PTSD symptoms. Edges correspond to change across one day to the next. All edges included are significant at p < .05. Edge thickness corresponds to magnitude of association.
Table 2.
Descriptive statistics of the temporal and contemporaneous networks.
| Temporal Network | Contemporaneous Network | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| In-Strength | Out-Strength | Triangle | Betweenness | Strength | Triangle | Betweenness | K-core Layer | ||
| I1: Thought Intrusions | 0.00 | 0.00 | 0 | 0 | 0.60 | 2 | 3.65 | 3 | |
| I4: Emotional Reactivity to Cues | 0.00 | 0.23 | 1 | 0 | 0.80 | 5 | 3.40 | 5 | |
| A1: Avoidance: External | 0.25 | 0.09 | 2 | 2 | 0.28 | 0 | 0.33 | 2 | |
| A2: Avoidance: Internal | 0.17 | 0.12 | 2 | 2 | 0.52 | 2 | 3.68 | 4 | |
| NACM2: Neg Thoughts about Self, Others, World | 0.14 | 0.14 | 0 | 0 | 0.73 | 5 | 9.32 | 4 | |
| NACM5: Low Interest | 0.23 | 0.38 | 3 | 0 | 0.37 | 1 | 0 | 2 | |
| AAR4: Startle | 0.25 | 0.00 | 1 | 0 | 0.36 | 2 | 0.53 | 4 | |
| AAR5: Concentration Diff | 0.12 | 0.12 | 0 | 0 | 0.45 | 3 | 2.08 | 4 | |
| AAR6: Sleep Diff | 0.17 | 0.24 | 0 | 0 | 0.18 | 1 | 0.00 | 2 | |
Note: I = Intrusions. A = Avoidance. NACM = Negative Alterations to Cognition and Mood. AAR = Alterations to Arousal and Reactivity.
The independent nodes [Thought Intrusions (I1), Negative Thoughts(NACM2), and Concentration Difficulties [AAR5]) suggested that levels of these symptoms over time were independent from the larger component. Four symptoms [Concentration Difficulties (AAR5), Low Interest in Activities (NACM2), Sleep Difficulties (AAR6), and Negative Thoughts (NACM2)] had self-loops, which suggested that these symptoms were self-perpetuating. Interestingly, only one symptom with a self-loop (NACM5) had other edges.
The contemporaneous network, displaying the association between symptoms within the same day, is presented in Figure 2. This network had a higher network density than the temporal network (44.4% of possible edges) and included a single component. Within this network, emotional reactivity (I4) and Negative Thoughts (NACM2) had the highest strength and had the highest number of triangles of any nodes (n = 5) (Table 2). Negative Thoughts (NACM2) had the highest betweenness as well. Finally, the K-core decomposition identified emotional reactivity (I4) at the highest layer of the network. This result suggests that in addition to emotional reactivity (I4) having the highest strength, it had edges to other nodes of a high strength and thus was the core of the network.
Figure 2.
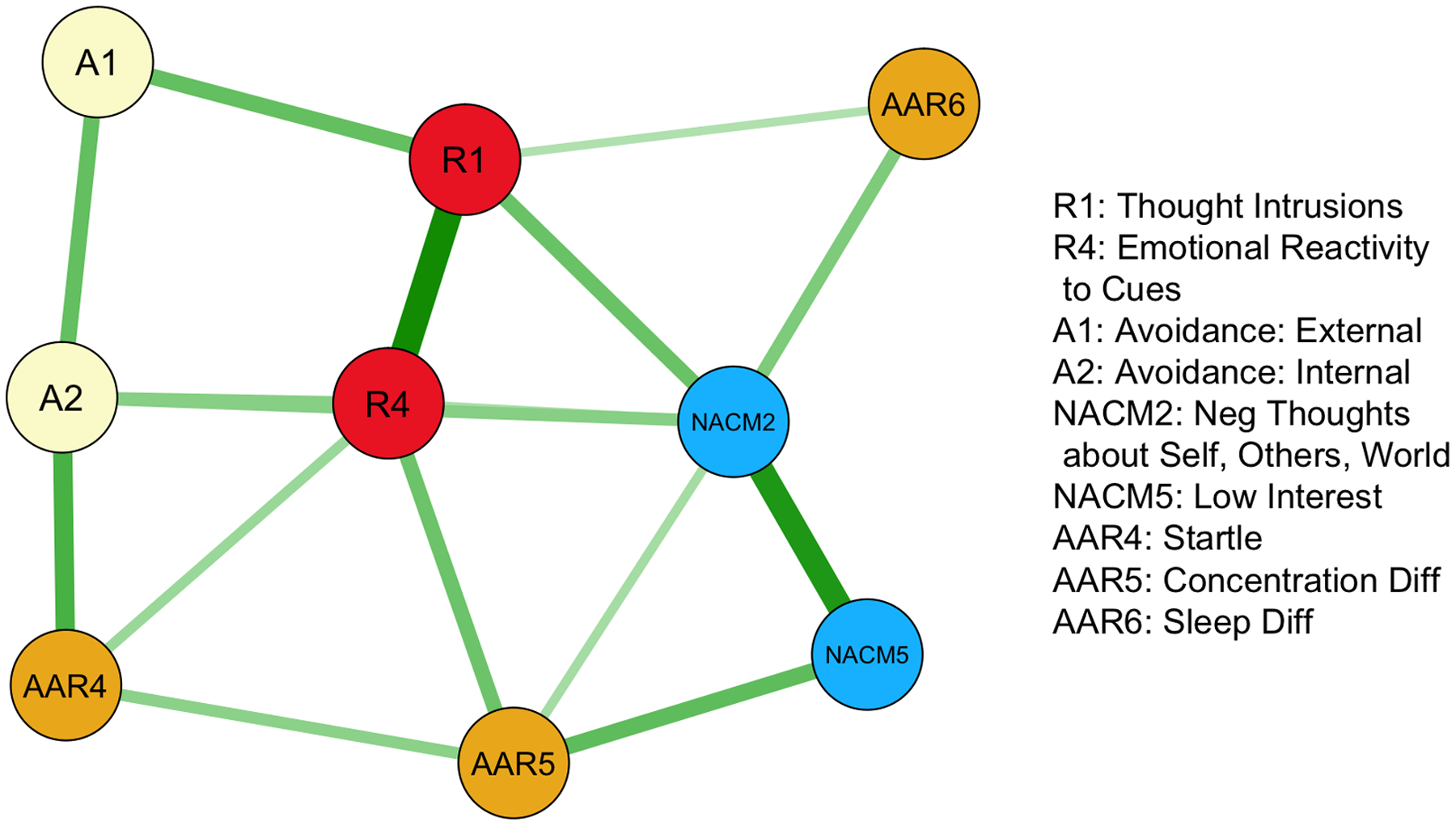
Contemporaneous network of PTSD symptoms. Edges correspond to change across one day to the next. All edges included are significant at p < .05. Edge thickness corresponds to magnitude of association.
Discussion
The present study was the first to examine the short-term dynamics of PTSD symptoms during the acute post trauma period. As hypothesized, symptoms associated with fear conditioning were a key part of the network of PTSD symptoms. This finding was consistent with the ‘failure of recovery model’ conceptualization of PTSD development (Bryant, O’Donnell, Creamer, McFarlane, & Silove, 2013; Ehlers & Clark, 2000; Weston, 2014). The temporal network contained paths that began with emotional reactivity to trauma cues (I4) and led to avoidance (NACM5, A1, A2), which resulted in elevated startle (AA4). The NACM symptom of diminished interest in activities represented an avoidance symptom in this network given its relation to the other avoidance symptom and the manner in which the question was phrased. The lack of ingoing paths to emotional reactivity to trauma cues (I4) and the lack of outgoing paths from startle (AAR4) indicated these symptoms served as starting and end points of this reactivity to sensitization process.
Results highlighted the important role that reactivity to trauma cues (I4) had in the initial propagation of PTSD symptoms. Within the temporal network, this symptom served as the starting point of a large component of the network, similar to a fear conditioning model (Milad, Rauch, Pitman, & Quirk, 2006). Within the contemporaneous network, reactivity to trauma cues had the highest number of triangles, the highest strength and was at the highest layer in the network. Its highly centralized position suggested that it affected and was affected by most of the other symptoms. By contrast, thought intrusions that were not triggered by a trauma cue (I1) had a substantially less central role in the contemporaneous network and was disconnected from the large component in the temporal network. This result was consistent with the other network study of PTSD symptoms in which cue reactivity was more important during the acute phase relative to other intrusion symptoms (Bryant et al., 2017). Taken together, these findings emphasized the importance of reactivity to cues and the utility of using fear conditioning models to understand, predict, and potentially treat PTSD in this early period (Hoge et al., 2016; Zoellner et al., 2011).
The contemporaneous network suggested there was also a subnetwork characterized by dysphoria symptoms. The symptoms associated with fear conditioning [thought intrusions (I1), emotional reactivity (I4), internal avoidance (A1), external avoidance (A2), and hyperarousal (AAR4)] had a high edge density (6/10, 60%). The remaining symptoms [Negative cognitions (NACM2), Low interest (NACM5), Concentration difficulties (AAR5), Difficulty sleeping (AAR6)] also had a similar high edge density (4/6, 66%). The edge density across the symptoms of these two sets, was markedly lower (5/20, 25%). Furthermore, the majority of these cross-set edges (3/5) were with Negative thoughts (NACM2), suggesting that this symptom may be a hub. Factor analytic work has suggested that dysphoric symptoms are part of an independent factor that is distinct from intrusions and avoidance (Elhai & Palmieri, 2011; Pietrzak et al., 2015). Further, dysphoria is more weakly related to intrusions and avoidance than it is to depression symptoms (Elhai et al., 2015; Price et al., 2019; Price & van Stolk-Cooke, 2015). In the temporal network, negative thoughts had a strong self-loop, suggesting that it influenced itself over time. Taken together, these data suggest that the early period after a traumatic event is characterized by dysphoria and fear symptoms, but that the extent that they sustain each other over this period is unclear and requires further investigation.
The present study had several limitation. First, it did not asses all 20 symptoms of PTSD, which limited the conclusions that could be drawn. The included 9 symptoms were most strongly related to each cluster of PTSD and to overall PTSD severity (Price et al., 2016). The abbreviated scale was chosen to reduce the burden on participants. Although this approach increased the feasibility of the study, it limited the number of symptoms available to analyze. Given that networks rely on item-level data (McNally et al., 2015), the findings of the present study should be considered preliminary. The limited number of symptoms also prevented the examination of clustering within this network, which may have further supported the proposed associations between intrusions and avoidance symptoms.
A second limitation was the focus on traumatic injury relative to other trauma types. A traumatic injury sample is relatively homogenous in that the majority of participants in the current study experienced car accidents. It is unclear if these same networks would have been obtained had additional trauma types, such as interpersonal violence or sexual assault, been included as these traumas are thought to evoke more dysphoric symptoms (Aakvaag et al., 2016).
A third limitation was the inability to compare the networks of those who developed PTSD and those who recovered. Given the rates of PTSD after trauma exposure (Bryant et al., 2010; Zatzick et al., 2007), large cohorts of trauma victims are needed to have sufficient power to examine the networks of those who develop clinically significant symptoms as opposed to recovered. Nevertheless, the present study provided useful information for understanding the overall progress of symptoms in the acute aftermath of a traumatic event.
Finally, the temporal network reflected the directional relation between symptoms from one day to the next. The contemporaneous network reflects the associations between symptoms within a given day of the acute post trauma period. However, the speed with which these symptoms affect one another is likely faster than a single day. A recent study demonstrated that the relation between the clusters of PTSD varies depending on the frequency with which they were assessed (Gelkopf, Pickman, Carlson, & Greene, 2019). Future work should consider assessing symptoms multiple times per day.
The results of the present study supported the theorized process by which PTSD develops after a traumatic event. This process includes a fear conditioning component in which reactivity to trauma cues leads to avoidance which results in elevated arousal. These findings suggested that fear conditioning models and associated treatments, such as exposure, may prove useful in assessment and early intervention (Rothbaum et al., 2012). Furthermore, dysphoric symptoms appear to represent a distinct process that is hypothesized to become gradually more integrated with other symptoms over time. Through continued investigations of PTSD symptom interactions during the acute post trauma period, new assessment and early intervention strategies will be developed to identify and treat those at greatest risk.
Supplementary Material
Footnotes
None of the authors have any have conflicts or disclosures related to this work.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Aakvaag HF, Thoresen S, Wentzel-Larsen T, Dyb G, Røysamb E, & Olff M (2016). Broken and guilty since it happened: A population study of trauma-related shame and guilt after violence and sexual abuse. Journal of Affective Disorders, 204, 16–23. 10.1016/j.jad.2016.06.004 [DOI] [PubMed] [Google Scholar]
- Armour C, Fried EI, Deserno MK, Tsai J, & Pietrzak RH (2017). A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in U.S. military veterans. Journal of Anxiety Disorders, 45, 49–59. 10.1016/j.janxdis.2016.11.008 [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Borgatti SP (2005). Centrality and network flow. Social Networks, 27(1), 55–71. 10.1016/j.socnet.2004.11.008 [DOI] [Google Scholar]
- Borsboom D, & Cramer AOJ (2013). Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annual Review of Clinical Psychology, 9(1), 91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Vissers N, Wichers M, Geschwind N, Kuppens P, Peeters F, … Tuerlinckx F (2013). A Network Approach to Psychopathology: New Insights into Clinical Longitudinal Data. PLOS ONE, 8(4), e60188. 10.1371/journal.pone.0060188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA, Creamer M, O’Donnell M, Forbes D, McFarlane AC, Silove D, & Hadzi-Pavlovic D (2017). Acute and Chronic Posttraumatic Stress Symptoms in the Emergence of Posttraumatic Stress Disorder: A Network Analysis. JAMA Psychiatry, 74(2), 135–142. 10.1001/jamapsychiatry.2016.3470 [DOI] [PubMed] [Google Scholar]
- Bryant RA, O’Donnell ML, Creamer M, McFarlane AC, Clark CR, & Silove D (2010). The psychiatric sequelae of traumatic injury. American Journal of Psychiatry, 167(3), 312–320. 10.1176/appi.ajp.2009.09050617 [DOI] [PubMed] [Google Scholar]
- Bryant RA, O’Donnell ML, Creamer M, McFarlane AC, & Silove D (2013). A Multisite Analysis of the Fluctuating Course of Posttraumatic Stress Disorder. JAMA Psychiatry, 70(8), 839–846. 10.1001/jamapsychiatry.2013.1137 [DOI] [PubMed] [Google Scholar]
- Bunnell BE, Davidson TM, Winkelmann JR, Maples-Keller JL, Ridings LE, Dahne J, … Ruggiero KJ (2019). Implementation and Utility of an Automated Text Messaging System to Facilitate Symptom Self-Monitoring and Identify Risk for Post-traumatic Stress Disorder and Depression in Trauma Center Patients. Telemedicine and E-Health. 10.1089/tmj.2018.0170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson TM, Bunnell BE, & Ruggiero KJ (2017). An Automated Text-Messaging System to Monitor Emotional Recovery After Pediatric Injury: Pilot Feasibility Study. Psychiatric Services, 68(8), 859–860. 10.1176/appi.ps.201600515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Elhai JD, Contractor AA, Tamburrino M, Fine TH, Cohen G, Shirley E, … Galea S (2015). Structural relations between DSM-5 PTSD and major depression symptoms in military soldiers. Journal of Affective Disorders, 175, 373–378. 10.1016/j.jad.2015.01.034 [DOI] [PubMed] [Google Scholar]
- Elhai JD, & Palmieri PA (2011). The factor structure of posttraumatic stress disorder: A literature update, critique of methodology, and agenda for future research. Journal of Anxiety Disorders, 25(6), 849–854. 10.1016/j.janxdis.2011.04.007 [DOI] [PubMed] [Google Scholar]
- Foa EB, & Rothbaum BO (2001). Treating the Trauma of Rape: Cognitive-Behavioral Therapy for PTSD. Guilford Press. [Google Scholar]
- Galatzer-Levy IR, & Bryant RA (2013). 636,120 ways to have posttraumatic stress disorder. Perspectives on Psychological Science, 8(6), 651–662. 10.1177/1745691613504115 [DOI] [PubMed] [Google Scholar]
- Gelkopf M, Pickman LL, Carlson EB, & Greene T (2019). The Dynamic Relations Among Peritraumatic Posttraumatic Stress Symptoms: An Experience Sampling Study During Wartime. Journal of Traumatic Stress, 32(1), 119–129. 10.1002/jts.22374 [DOI] [PubMed] [Google Scholar]
- Gelkopf M, Pickman LL, Grinapol S, Werbeloff N, Carlson EB, & Greene T (2017). Peritraumatic Reaction Courses During War: Gender, Serious Mental Illness, and Exposure. Psychiatry, 80(4), 382–398. 10.1080/00332747.2017.1286893 [DOI] [PubMed] [Google Scholar]
- Greene T, Gelkopf M, Epskamp S, & Fried E (2018). Dynamic networks of PTSD symptoms during conflict. Psychological Medicine, 48(14), 2409–2417. 10.1017/S0033291718000351 [DOI] [PubMed] [Google Scholar]
- Hébert-Dufresne L, Grochow JA, & Allard A (2016). Multi-scale structure and topological anomaly detection via a new network statistic: The onion decomposition. Scientific Reports, 6, 31708. 10.1038/srep31708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Yehuda R, Castro CA, McFarlane AC, Vermetten E, Jetly R, … Rothbaum BO (2016). Unintended Consequences of Changing the Definition of Posttraumatic Stress Disorder in DSM-5: Critique and Call for Action. JAMA Psychiatry, 73(7), 750–752. 10.1001/jamapsychiatry.2016.0647 [DOI] [PubMed] [Google Scholar]
- Kearns MC, Ressler KJ, Zatzick D, & Rothbaum BO (2012). Early interventions for PTSD: A review. Depression and Anxiety, 29(10), 833–842. 10.1002/da.21997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ (2012). The Ontology of Posttraumatic Stress Disorder: Natural Kind, Social Construction, or Causal System? Clinical Psychology: Science and Practice, 19(3), 220–228. 10.1111/cpsp.12001 [DOI] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK, & Borsboom D (2015). Mental Disorders as Causal Systems: A Network Approach to Posttraumatic Stress Disorder. Clinical Psychological Science, 3(6), 836–849. 10.1177/2167702614553230 [DOI] [Google Scholar]
- Milad MR, Rauch SL, Pitman RK, & Quirk GJ (2006). Fear extinction in rats: Implications for human brain imaging and anxiety disorders. Biological Psychology, 73(1), 61–71. 10.1016/j.biopsycho.2006.01.008 [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Elliott P, Lau W, & Creamer M (2007). PTSD symptom trajectories: From early to chronic response. Behaviour Research and Therapy, 45(3), 601–606. 10.1016/j.brat.2006.03.015 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Tsai J, Armour C, Mota N, Harpaz-Rotem I, & Southwick SM (2015). Functional significance of a novel 7-factor model of DSM-5 PTSD symptoms: Results from the National Health and Resilience in Veterans Study. Journal of Affective Disorders, 174, 522–526. 10.1016/j.jad.2014.12.007 [DOI] [PubMed] [Google Scholar]
- Price M, Legrand AC, Brier ZMF, & Hébert-Dufresne L (2019). The symptoms at the center: Examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. Journal of Psychiatric Research, 109, 52–58. 10.1016/j.jpsychires.2018.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M, Szafranski DD, van Stolk-Cooke K, & Gros DF (2016). Investigation of abbreviated 4 and 8 item versions of the PTSD Checklist 5. Psychiatry Research, 239, 124–130. 10.1016/j.psychres.2016.03.014 [DOI] [PubMed] [Google Scholar]
- Price M, & van Stolk-Cooke K (2015). Examination of the interrelations between the factors of PTSD, major depression, and generalized anxiety disorder in a heterogeneous trauma-exposed sample using DSM 5 criteria. Journal of Affective Disorders, 186, 149–155. 10.1016/j.jad.2015.06.012 [DOI] [PubMed] [Google Scholar]
- Price M, van Stolk-Cooke K, Brier ZMF, & Legrand AC (2018). mHealth solutions for early interventions after trauma: Improvements and considerations for assessment and intervention throughout the acute post-trauma period. MHealth, 4. 10.21037/mhealth.2018.06.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, & Ruggiero KJ (2014). mHealth: A Mechanism to Deliver More Accessible, More Effective Mental Health Care. Clinical Psychology & Psychotherapy, 21(5), 427–436. 10.1002/cpp.1855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Kearns MC, Price M, Malcoun E, Davis M, Ressler KJ, … Houry D (2012). Early Intervention May Prevent the Development of Posttraumatic Stress Disorder: A Randomized Pilot Civilian Study with Modified Prolonged Exposure. Biological Psychiatry, 72(11), 957–963. 10.1016/j.biopsych.2012.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schell TL, Marshall GN, & Jaycox LH (2004). All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology, 113(2), 189–197. 10.1037/0021-843X.113.2.189 [DOI] [PubMed] [Google Scholar]
- Shalev AY, Peri T, Brandes D, Freedman S, Orr SP, & Pitman RK (2000). Auditory Startle Response in Trauma Survivors With Posttraumatic Stress Disorder: A Prospective Study. American Journal of Psychiatry, 157(2), 255–261. 10.1176/appi.ajp.157.2.255 [DOI] [PubMed] [Google Scholar]
- Stam R (2007). PTSD and stress sensitisation: A tale of brain and body: Part 1: Human studies. Neuroscience & Biobehavioral Reviews, 31(4), 530–557. 10.1016/j.neubiorev.2006.11.010 [DOI] [PubMed] [Google Scholar]
- Stockert S. H. H. von, Fried EI, Armour C, & Pietrzak RH (2018). Evaluating the stability of DSM-5 PTSD symptom network structure in a national sample of U.S. military veterans. Journal of Affective Disorders, 229, 63–68. 10.1016/j.jad.2017.12.043 [DOI] [PubMed] [Google Scholar]
- Wasserstein RL, Schirm AL, & Lazar NA (2019). Moving to a World Beyond “p < 0.05.” The American Statistician, 73(sup1), 1–19. 10.1080/00031305.2019.1583913 [DOI] [Google Scholar]
- Weston CS (2014). Posttraumatic Stress Disorder: A Theoretical Model of the Hyperarousal Subtype. Frontiers in Psychiatry, 5. 10.3389/fpsyt.2014.00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R, & LeDoux J (2007). Response Variation following Trauma: A Translational Neuroscience Approach to Understanding PTSD. Neuron, 56(1), 19–32. 10.1016/j.neuron.2007.09.006 [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Rivara FP, Nathens AB, Jurkovich GJ, Wang J, Fan M-Y, … Mackenzie EJ (2007). A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychological Medicine, 37(10), 1469–1480. 10.1017/S0033291707000943 [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Rothbaum BO, & Feeny NC (2011). PTSD not an anxiety disorder? DSM committee proposal turns back the hands of time. Depression and Anxiety, 28(10), 853–856. 10.1002/da.20899 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


