Abstract
Purpose:
To develop and evaluate psychometrically a self-reported instrument assessing physical fatigability (PF) and mental fatigability (MF) in adults with spinal cord injury (SCI).
Design:
Cross-sectional.
Setting:
Peer-support groups at rehabilitation centers, on-line support groups.
Participants:
Adults with SCI (N=464) in the US.
Interventions:
Not applicable.
Main Outcome Measures:
The dimensional structure was assessed by confirmatory factor analysis. The relationship between item responses and fatigability was measured with item response theory (graded response model). Reliability was measured with test information functions. Differential item functioning was evaluated with Wald chi-square tests and the weighted area between the curves (wABC). Construct validity was assessed using the known groups method.
Results:
An 82-item pool was developed from prior qualitative research and consultations with rehabilitation experts. A non-probability sample (N=464) was used to evaluate the psychometric properties of the PF and MF scales. The item pool was reduced to 75 based on factor loadings and R2. Both scales are primarily unidimensional, despite moderate multidimensionality. There is good discrimination overall: 18 PF items and 26 MF items have high or very high discrimination power (slopes > 1.35). The measurement precision in the theta range −2.0 to 2.5 is the equivalent of 0.94 reliability for PF and 0.91 for MF. For both measures, F-statistics p-values were significant at p < .01, and means were higher for those with paraplegia vs quadriplegia, and for those with incomplete paraplegia.
Conclusions:
The Fatigability Index is the first instrument designed to assess physical and mental fatigability in adults with SCI. It highlights causes of fatigue and areas requiring immediate intervention. Development of short-forms and further research on representative samples are necessary.
Keywords: fatigability, physical fatigue, mental fatigue, spinal cord injury, health-related quality of life
Introduction
Spinal cord injury (SCI) affects approximately 300,000 individuals in the US.1 A prevalent symptom associated with SCI is fatigue: “a subjective lack of physical and/or mental energy that is perceived by the individual or caregiver to interfere with usual or desired activities.”2 About 25% of individuals with SCI report fatigue that is severe enough to impact upon daily functioning and well-being.3,4 Adults with SCI may experience fatigue associated with their age, their full-time use of a wheelchair, daily activities, co-morbidities, and other consequences of SCI (e.g., poor posture, pressure management).4-11 Just like non-SCI adults, persons with SCI may try to avoid fatigue and exhaustion by decreasing or completely eliminating certain activities (cooking) or wheelchair maneuvers (wheelchair-to-car transfers).
Fatigability is “a characteristic describing an individual’s susceptibility to experiencing fatigue for a given quantifiable demand.”2 There are two forms of fatigability. The first is performance-related fatigability, which is observed and could be measured by a clinician, and refers to erosion in force, power, speed or stamina related to performance of a given activity.2 The second type of fatigability is perceived (self-reported) fatigability, which is the focus of this study: it refers to feelings of tiredness and wear related to duration and intensity of an activity.2 Self-reported fatigability has been measured in contexts other than SCI, with instruments such as the Physical Energy Scale from the Motivation and Energy Inventory, the Dutch Exertion Fatigue Scale, the Situational Fatigue Scale, and the Pittsburgh Fatigability Scale.12-17 To date, no self-reported fatigability instrument specifically for SCI individuals has been developed and assessed psychometrically.
Development of such targeted instruments aligns with patient-centered care goals of being “respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions.”18 In this study we aimed to develop and evaluate a SCI fatigability measure that could complement clinical processes like rehabilitation, seating, pressure/posture management, or other interventions to ameliorate the symptoms.
Methods
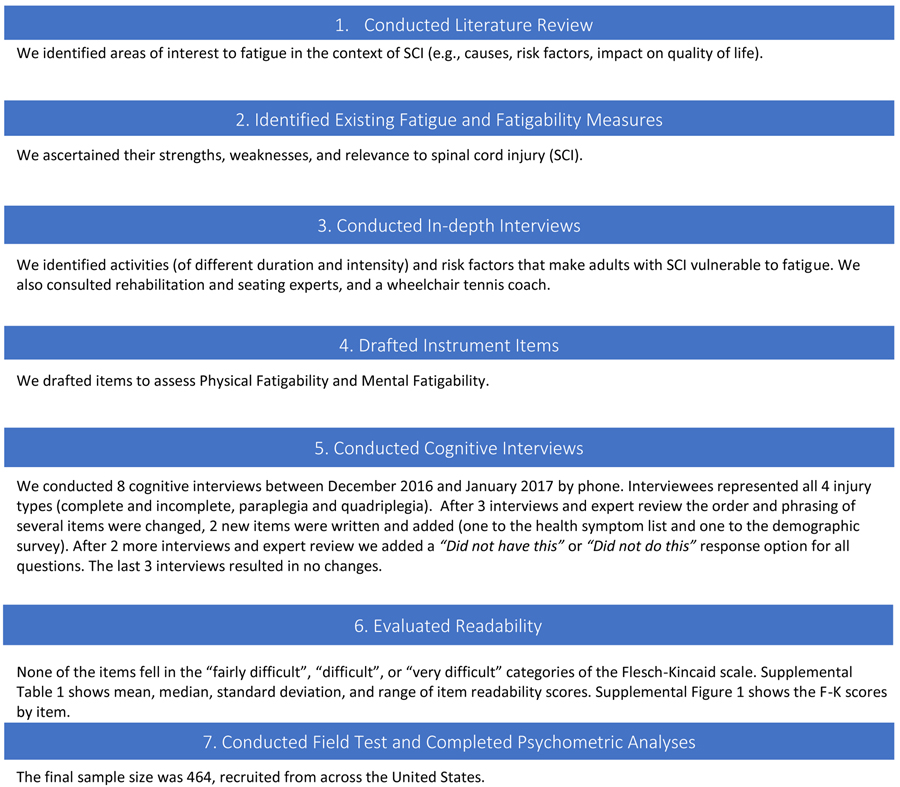
We developed the measures following the International Society for Quality of Life Research (ISOQOL) minimum standards and recommendations for patient-reported outcome measures (Figure 1).19
Figure 1.
Overview of survey development and testing approach.
Initial Fatigability 82-Item Pool
First, we conducted a literature review to identify areas of interest relating to fatigue, that is, causes of fatigue in adults with SCI, and the relationship between fatigue and health-related quality of life in this subgroup of the population.3-17 We also identified existing fatigue instruments that were evaluated psychometrically among persons with SCI. 3-17 We conducted 20 in-depth interviews with adults with SCI who are full-time wheelchair users, exploring quality of life in the context of SCI, and preferences for different health outcome measures, with findings reported elsewhere.20 The need for two separate scales emerged from these in-depth interviews. Physical fatigue was defined as reduced physical function due to wear or disease (tiredness and weakness are symptoms of fatigue). Physical fatigue was also described as progressive, increasing in severity over time. Interviewees defined mental fatigue as reduced mental function due to perceived high level of stress, worries about the future, perceived need for extensive logistical planning, and perceived bureaucratic burden (such as filling out forms for health or welfare benefits). Participants discussed that for many activities, physical and mental fatigue can compete and conspire to frustrate and reduce what a disabled person can do in their life. With input from experts in wheelchair and seating assessment, rehabilitation, wheelchair sports coaching, survey development and psychometric evaluation, we drafted a large pool of Physical Fatigability (PF) and Mental Fatigability (MF) items (Table 1). The items represent four areas of fatigability: health problems, problems in the home environment, activities in the home, and activities away from home (which may be more demanding, with varying degrees of logistical challenges and physical exertion). For example, going to a doctor’s appointment differs from taking an overnight trip away from home.
Table 1.
Physical and Mental Fatigue (PF/MF) Item Pool
| ItemID | Item Stem and Item Content | |
|---|---|---|
| Health | During the past 4 weeks did you experience each of the following? If so, how much physical & mental fatigue did each cause you? | |
| PF&MF | Hlth1 | Sleep problems |
| PF&MF | Hlth2 | Pain |
| PF&MF | Hlth3 | Indigestion problems |
| PF&MF | Hlth4 | Dehydration problems |
| PF&MF | Hlth5 | Poor posture |
| PF&MF | Hlth6 | Spasticity |
| PF&MF | Hlth7 | Stress |
| PF&MF | Hlth8 | Medication side-effects |
| Home environment | During the past 4 weeks did you experience each of the following? If so, how much physical & mental fatigue did each cause you? | |
| PF&MF | Envr1 | Lack of peace and quiet |
| PF&MF | Envr2 | Inadequately adapted home |
| PF&MF | Envr3 | Inadequate medical care when at home |
| PF&MF | Envr4 | Inadequate non-medical care when at home |
| Activities at home | During the past 4 weeks did you experience each of the following? If so, how much physical & mental fatigue did each cause you? | |
| PF&MF | Home1 | Wheelchair transfer to and from bed |
| PF&MF | Home2 | Sitting in a wheelchair for an hour or more |
| PF&MF | Home3 | Concentrating for an hour or more (such as reading, writing, or holding a conversation) |
| PF&MF | Home4 | Using a computer for an hour or more |
| PF&MF | Home5 | Wheelchair use around the home |
| PF&MF | Home6 | Spending all day in your wheelchair |
| PF&MF | Home7 | Pressure management (preventing pressure sores) |
| PF&MF | Home8 | Posture management |
| PF&MF | Home9 | Household chores, such as cleaning and tidying |
| PF&MF | Home10 | Preparing and clearing away a meal |
| PF&MF | Home11 | Eating a meal |
| PF&MF | Home12 | Letter-writing, form filling or paying bills |
| Activities away from home | During the past 4 weeks did you experience each of the following? If so, how much physical & mental fatigue did each cause you? | |
| PF&MF | Away1 | Wheelchair use over a smooth surface |
| PF&MF | Away2 | Wheelchair use over an uneven surface |
| PF&MF | Away3 | Wheelchair transfer to and from car |
| PF&MF | Away4 | Traveling in your vehicle for an hour or more |
| PF&MF | Away5 | Using an adapted taxi |
| PF&MF | Away6 | Using a bus |
| PF&MF | Away7 | Using a train |
| PF&MF | Away8 | Receiving a session of physiotherapy |
| PF&MF | Away9 | Going to a doctor's appointment |
| PF&MF | Away10 | Shopping, such as having access and reaching merchandise |
| PF&MF | Away11 | Going out to a restaurant |
| PF&MF | Away12 | Attending an event, such as cinema, theater, or a show |
| PF&MF | Away13 | Visiting friends |
| PF&MF | Away14 | Attending a sporting event |
| PF&MF | Away15 | Taking a day trip away from home |
| PF&MF | Away16 | Taking an overnight trip away from home |
| PF&MF | Away17 | Taking a vacation away from home |
Abbreviations: Physical Fatigue (PF); Mental Fatigue (MF). These 41 items were presented separately for the physical fatigue and the mental fatigue scales, hence 82 total item count. The answer range was: No Fatigue (0), Mild Fatigue (1); Moderate Fatigue (2), Extreme Fatigue (3); Did not have or Did not do this (99). However, due to sparse distributions, the “Did not have or Did not do this” category was collapsed into “Mild fatigue” (based on Duncan Multiple Range Test results) in order to have no cell with <5% of the data (23 participants). For all these items, higher scores mean higher vulnerability to physical and mental fatigue respectively.
We asked, separately, about the level of physical and mental fatigue associated with 41 activities using the following response scale: 0 (no fatigue), 1 (Mild fatigue), 2 (Moderate fatigue) and 3 (Extreme fatigue), and Did not have this/Did not do this. In addition, we assessed the importance of each item to the respondent. For health, they were asked “How important is it that each of the following is treated?”; regarding activities they were asked “How important is it that you can perform each of these activities?” The importance questions were not used in the analyses reported here.
Field Test Data Collection and Sampling
Eligibility included being 18 years or older, U.S. residents, with a self-reported diagnosis of SCI, at least 1-year post hospital discharge, full-time wheelchair users, and could read and write in English. Excluded were individuals unable to provide informed consent (including cognitive impairments such as dementia or Alzheimer’s disease), and those who were part-time wheelchair users.
This was a non-probability (convenience) sample recruited nationally through (1) print advertisements distributed through peer support groups in the United States (US), and veterans’ support groups (local chapters of Paralyzed Veterans of America); (2) online advertisements distributed through organizations such as The Dana and Christopher Reeve Foundation (Members’ Board: http://www.spinalcordinjury-paralysis.org/) and the United Spinal Association (http://www.spinalcord.org/resource-center/askus/index.php). In addition, 4 separate paid ad campaigns were conducted via Facebook Ads at 2-week intervals, with target specifications including US as a location, “SCI” and “wheelchairs” as user interests, and a population target of 12,000 for each campaign. Upon expressing interest in being interviewed, participants were sent an email with information about the study, and were given the option to take the survey online or via the phone. All respondents in this study, including several with high neck injuries who were on ventilators, chose to take the survey online between January and May 2017. No remuneration was provided for survey participation. A total of 491 individuals expressed interest in the study; 478 completed the survey. Fourteen respondents were eliminated because they resided in Australia, New Zealand, Canada, England and Scotland. The final sample was 464. This study was approved (Certified Exempt) by the Institutional Review Board of the University of California Los Angeles (IRB#16-000231).
Missing Data
Inappropriately missing data was 6% and was similar across all diagnosis levels. This degree of missing data is considered small in magnitude, and acceptable by traditional standards.21 In contrast, appropriately missing data due to items not being applicable was 21%. The number of “did not have” or “did not do this” responses per item varied from 2% to 85%.
The high proportion of the not-applicable answers resulted in some response options rarely being chosen – that is, a data sparsity problem. We further investigated the position of the not applicable responses in relation to the other response options. Average PF and MF scores were used as dependent variables in one-way ANOVAs with response options for each item as the independent variables. Duncan multiple range tests were used to compare mean scores by each response option. 22 Means for both PF and MF for those picking the not applicable response to items were closer to the Mild Fatigue score than any other answer option. Therefore, we collapsed the not applicable response with the “Mild fatigue” responses so that no cell had less than 5% of data (23 participants). We retained items with the high levels of not applicable responses because the majority of them were considered by at least half of the respondents to be “Vital” or “Important” for them to be able to do. For example, the high not applicable rate for an item such as “Taking a vacation away from home” may reflect inadequate transport and leisure infrastructure for people in wheelchairs, but it is possible that such services will improve in future.
Categorical Confirmatory Factor Analysis (CFA)
We investigated the factor structure of the 41 PF items and the 41 MF items using Mplus v.7.4.23 The hypothesized structure was based on theories proposed by previous studies.20,24 For the PF scale, we hypothesized five multi-item domains: “Health challenges,” “Daily living challenges,” “Mental tasks,” “Access challenges,” and “Seating challenges.” The hypothesized structure for the MF scale included four multi-item domains: “Daily living challenges,” “Access challenges,” “Concentration challenges,” and “Health challenges.”
A five-factor categorical confirmatory analysis model, a modified four-factor model, and a bifactor model were fit for the PF items. For the MF scale, a four-factor categorical confirmatory analysis model, a modified four-factor model, and a bifactor model were fit. All models used weighted least squares means and variances adjusted (WLSMV) estimation.25 The multi-factor models specified correlations among the domains (factors), but not among item error variances. We also estimated item means, standard deviations, item-total correlation (corrected for overlap), and coefficient alpha for each multi-item scale using Stata 15.26
The following commonly used model fit indices and thresholds were used: Root Mean Square Error of Approximation (RMSEA) < 0.08; Comparative Fit Index (CFI) > 0.95; and the Tucker-Lewis Index (TLI) > 0.95.27-31 Factor loadings (i.e. the relation of an item to the hypothesized scale) were also inspected, looking for standardized loadings lower than 0.30, and R2 lower than 10% as indicators of potential problematic items. For the bi-factor model, an instrument is considered primarily unidimensional if the percent uncontaminated correlations (PUC) < 0.80 (this is the percentage of covariance that reflects only variance from the general dimension), the explained common variance on the general dimension (ECVGEN) > 60%, and omega hierarchical, the variance in raw total scores that can be attributed to individual differences on the general factor (Omega H) > 0.70.32,33
Item Response Theory (IRT) - Graded Response Model Analysis
Unidimenional IRT has several underlying assumptions. Unidimensionality was evaluated using CFA. Local independence means that after accounting for the underlying factor, items are uncorrelated.34 To assess this we evaluated the residual correlation matrix for any values higher than 0.20. Monotonicity was evaluated by graphing item characteristic curves depicting the relationships between IRT estimated fatigability scores and responses to each item.19,35 Reliability (analogous to IRT information) of at least 0.70 was considered adequate for group comparisons.36
Differential Item Functioning (DIF) analyses evaluated whether the items were free of measurement bias—that is, conditional on estimated fatigability, the probability of selecting each response option was not associated with other factors such as age, time since injury, level of injury (paraplegia or quadriplegia) or gender.34,37,38 For this study we used the Wald chi-square procedure which evaluates the equality of parameter estimates across groups. The approach obviates the need to identify DIF-free anchor items, and estimates the mean difference between the groups based on all the items in the scale.37 To avoid false positives due to multiple hypotheses testing we applied the Benjamini-Hochberg adjustment (P < 0.01).31,35,37-39 The magnitude of DIF was assessed using the weighted area between the curves (wABC) method, which measures the DIF effect size whilst accounting for the underlying distribution: for measurement items with four response categories, a wABC of 0.24 is considered non-negligible.35,37
Construct Validity
We assessed construct validity for the PF/MF scales, with F statistics evaluating the significance of difference between means among the four diagnosis groups.40 We hypothesized that means would be higher for those with paraplegia and for those with incomplete paraplegia than for those with complete paraplegia. Finally, we examined the magnitude of correlations between responses to the PF and MF measures. We expected these two measures to be highly correlated, but we also expected to have higher correlations between the PF and MF Access Challenges scales, PF and MF Health Challenges scales, and PF and MF Daily Living Challenges scales. The rationale for these hypotheses is that individuals with comparatively higher mobility might exert themselves more in order to perform otherwise “normal” daily activities, and would thus be more susceptible to feeling exhausted. A wider range of activities also requires more cognitive and logistical planning and worry, for example anticipating access to parking (or lack thereof) and ramps in public spaces, resulting in higher physical and mental fatigability.
Results
Sample Characteristics
The 82-item fatigability survey was administered to a sample of individuals with SCI in 27 states in the US (Table 2). Supplemental Table 1 and Supplemental Figure 1 show readability scores for the item pool.
Table 2.
Sample participant characteristics (N=464)
| Age (Mean years, SD) | 45 | (12) |
| Time Since Injury (Mean, SD) | 13 | (12) |
| Sex (%) | ||
| Male | 222 | (48) |
| Female | 242 | (52) |
| Ethnicity (%) | ||
| Hispanic | 16 | (3) |
| Non-Hispanic | 446 | (96) |
| Race (%) | ||
| White | 424 | (91) |
| Black or African American | 14 | (3) |
| Asian | 6 | (1) |
| Native Hawaiian or Other Pacific Islander | - | - |
| American Indian or Alaska Native | 5 | (1) |
| Other | 14 | (3) |
| Living Arrangements (%) | ||
| Alone with no caregiver support | 70 | (15) |
| Alone but with visiting caregiver support | 62 | (13) |
| With a live-in caregiver who is a family member | 213 | (46) |
| With a live-in caregiver who is not a family member | 7 | (2) |
| With someone who is not your caregiver | 111 | (24) |
| In a nursing home | - | - |
| In some other living arrangement | 1 | (0.2) |
| Education (%) | ||
| 8th grade or less | 44 | (9) |
| Some high school, but did not graduate | 10 | (2) |
| High school graduate or GED | 60 | (13) |
| Some college or 2-year degree | 162 | (35) |
| 4-year college graduate | 104 | (22) |
| More than 4-year college degree | 84 | (18) |
| Employment Status (%) | ||
| Full-time paid work (30 or more hours a week) | 61 | (13) |
| Full-time voluntary work (less than 30 hours a week) | - | - |
| Part-time paid work (30 or more hours a week) | 48 | (10) |
| Part-time voluntary work (less than 30 hours a week) | 51 | (11) |
| Not working, but seeking work | 14 | (3) |
| Not working due to disability | 210 | (45) |
| Student | 33 | (7) |
| Retired | 46 | (10) |
| Worries about financial situation (%) | ||
| All the time | 187 | (40) |
| Occasionally | 162 | (35) |
| Rarely | 90 | (20) |
| Never | 23 | (5) |
| Spinal Cord Diagnosis (%) | ||
| Complete paraplegia | 139 | (30) |
| Incomplete paraplegia | 149 | (32) |
| Complete quadriplegia | 70 | (15) |
| Incomplete quadriplegia | 106 | (23) |
| Type of Wheelchair Used (%) | ||
| Manual (I self-propel) | 321 | (69) |
| Manual (I am pushed) | 39 | (8) |
| Power chair | 160 | (34) |
Note: The numbers for "Type of Wheelchair Used" do not add up to 100 because participants could select a combination of wheelchair options.
CFA Analyses
The hypothesized PF five-factor model was a poor fit to the data (RMSEA=0.095; CFI=0.812; and TLI=0.830). After removing two items with loadings below 0.30, and R2 below 10% (PFAway8 – Receiving a session of physiotherapy, and PFAway11 – Going out to a restaurant), we moved the “Mental tasks” items under the “Daily living challenges” items. This four-factor model had a better, but still less than optimal fit: RMSEA = 0.081; CFI=0.922; and TLI = 0.940 (Supplemental Table 2).
For the MF scale, the initial and modified four-factor models were a poor fit to the data: (RMSEA=0.098, CFI=0.846, TFI=0.851; and RMSEA = 0.088, CFI=0.888, TLI = 0.901) (Supplemental Table 3). Supplemental Tables 4 and 5 show PF and MF item means, item-total correlations, and coefficient alphas.
Correlations among the PF factors and among the MF factors ranged from 0.575 to 0.772 and 0.565 to 0.856, respectively, suggesting the potential for a single general factor that may underlie the items in each scale.25,41 In addition, an exploratory factor analysis showed that the first factor explained 30% of the PF variability, and 35% of the MF variability (at least 20% is desirable), and the eigenvalue ratio (first to second) was 4.11 for the PF scale and 4.33 for the MF scale (ratios in excess of 4 provide support for unidimensionality).19
The bifactor models yielded RMSEA=0.076, CFI=0.931, TLI=0.956 for PF, and RMSEA=0.073, CFI=0.923, TLI=0.911 for MF. 32,41 Tables 3 and 4 show PF and MF bifactor loadings and the I-ECV values (each item’s explained common variance). On both scales certain items suggested some multidimensionality. However, 32 PF items and 28 MF items had stronger loadings on the general factor than on the specific factors, suggesting unidimensionality of the PF and MF scales respectively. The loadings on the general factor of each scale were close to those of the 1-factor model, although slightly lower. Across both PF and MF items, ECVGEN was 0.70, PUC was 0.71, while Omega H was 0.882 (PF) and 0.869 (MF). So, both scales were primarily unidimensional.
Table 3.
Physical Fatigability Bifactor Loadings and I-ECV Values
| Item Content | General Factor |
Health Challenges |
Daily Living Challenges |
Seating Challenges |
Access Challenges |
I-ECV |
|---|---|---|---|---|---|---|
| Sleep problems | 0.377 | 0.725 | 0.213 | |||
| Pain | 0.730 | 0.218 | 0.918 | |||
| Indigestion problems | 0.385 | 0.906 | 0.153 | |||
| Dehydration problems | 0.560 | 0.092 | 0.974 | |||
| Spasticity | 0.419 | 0.284 | 0.685 | |||
| Stress | 0.323 | 0.458 | 0.332 | |||
| Medication side-effects | 0.420 | 0.126 | 0.917 | |||
| Wheelchair transfer to and from bed | 0.477 | 0.320 | 0.690 | |||
| Wheelchair use around the home | 0.700 | 0.496 | 0.666 | |||
| Household chores, such as cleaning and tidying | 0.551 | 0.830 | 0.306 | |||
| Preparing and clearing away a meal | 0.478 | 0.206 | 0.843 | |||
| Eating a meal | 0.555 | 0.278 | 0.799 | |||
| Lack of peace and quiet | 0.476 | 0.276 | 0.748 | |||
| Inadequately adapted home | 0.583 | 0.143 | 0.943 | |||
| Inadequate medical care when at home | 0.374 | 0.083 | 0.953 | |||
| Inadequate non-medical care when at home | 0.380 | 0.107 | 0.927 | |||
| Concentrating for an hour or more (such as reading, writing, or holding a conversation) | 0.604 | 0.108 | 0.969 | |||
| Using a computer for an hour or more | 0.566 | 0.024 | 0.998 | |||
| Letter-writing, form filling or paying bills | 0.678 | 0.038 | 0.997 | |||
| Sitting in a wheelchair for an hour or more | 0.512 | 0.672 | 0.367 | |||
| Poor posture | 0.615 | 0.244 | 0.864 | |||
| Spending all day in your wheelchair | 0.935 | 0.263 | 0.927 | |||
| Pressure management (preventing pressure sores) | 0.496 | 0.335 | 0.687 | |||
| Posture management | 0.745 | 0.078 | 0.989 | |||
| Wheelchair use over a smooth surface | 0.773 | 0.251 | 0.905 | |||
| Wheelchair use over an uneven surface | 0.811 | 0.126 | 0.976 | |||
| Wheelchair transfer to and from car | 0.608 | 0.063 | 0.989 | |||
| Traveling in your vehicle for an hour or more | 0.510 | 0.679 | 0.361 | |||
| Using an adapted taxi | 0.543 | 0.597 | 0.453 | |||
| Using a bus | 0.653 | 0.172 | 0.935 | |||
| Using a train | 0.621 | 0.199 | 0.907 | |||
| Going to a doctor's appointment | 0.968 | 0.210 | 0.955 | |||
| Shopping, such as having access and reaching merchandise | 0.962 | 0.167 | 0.970 | |||
| Attending an event, such as cinema, theater, or a show | 0.518 | 0.435 | 0.586 | |||
| Visiting friends | 0.582 | 0.555 | 0.524 | |||
| Attending a sporting event | 0.702 | 0.530 | 0.637 | |||
| Taking a day trip away from home | 0.643 | 0.570 | 0.560 | |||
| Taking an overnight trip away from home | 0.648 | 0.465 | 0.660 | |||
| Taking a vacation away from home | 0.495 | 0.462 | 0.534 |
Abbreviations: Physical Fatigue (PF); Item explained common variance (I-ECV)
Items stem was: During the past 4 weeks did you experience each of the following? If so, how much physical fatigue did each cause you?
Answer options: No fatigue (0); Mild fatigue (1); Moderate fatigue (2); Extreme fatigue (4).
Table 4.
Mental Fatigability Bifactor Loadings and I-ECV Values
| Item Content | General Factor | Health Challenges |
Daily Living Challenges |
Concentration Challenges |
Access Challenges |
I-ECV |
|---|---|---|---|---|---|---|
| Sleep problems | 0.434 | 0.467 | 0.463 | |||
| Pain | 0.573 | 0.341 | 0.738 | |||
| Poor posture | 0.493 | 0.721 | 0.319 | |||
| Stress | 0.476 | 0.197 | 0.854 | |||
| Medication side-effects | 0.482 | 0.298 | 0.723 | |||
| Wheelchair transfer to and from bed | 0.759 | 0.041 | 0.997 | |||
| Sitting in a wheelchair for an hour or more | 0.704 | 0.316 | 0.832 | |||
| Wheelchair use around the home | 0.778 | 0.360 | 0.824 | |||
| Spending all day in your wheelchair | 0.832 | 0.319 | 0.872 | |||
| Pressure management (preventing pressure sores) | 0.787 | 0.348 | 0.836 | |||
| Posture management | 0.836 | 0.248 | 0.919 | |||
| Household chores, such as cleaning and tidying | 0.723 | 0.365 | 0.797 | |||
| Preparing and clearing away a meal | 0.683 | 0.364 | 0.779 | |||
| Eating a meal | 0.735 | 0.378 | 0.791 | |||
| Lack of peace and quiet | 0.505 | 0.320 | 0.714 | |||
| Inadequately adapted home | 0.526 | 0.574 | 0.456 | |||
| Inadequate medical care when at home | 0.470 | 0.476 | 0.494 | |||
| Concentrating for an hour or more (such as reading, writing, or holding a conversation) | 0.590 | 0.195 | 0.902 | |||
| Using a computer for an hour or more | 0.737 | 0.530 | 0.659 | |||
| Letter-writing, form filling or paying bills | 0.794 | 0.225 | 0.926 | |||
| Wheelchair use over a smooth surface | 0.567 | 0.589 | 0.481 | |||
| Wheelchair use over an uneven surface | 0.468 | 0.782 | 0.264 | |||
| Wheelchair transfer to and from car | 0.303 | 0.785 | 0.130 | |||
| Traveling in your vehicle for an hour or more | 0.774 | 0.065 | 0.993 | |||
| Using an adapted taxi | 0.723 | 0.254 | 0.890 | |||
| Using a bus | 0.736 | 0.075 | 0.990 | |||
| Using a train | 0.761 | 0.272 | 0.887 | |||
| Going to a doctor's appointment | 0.741 | 0.501 | 0.625 | |||
| Shopping, such as having access and reaching merchandise | 0.871 | 0.142 | 0.974 | |||
| Going out to a restaurant | 0.513 | 0.273 | 0.779 | |||
| Attending an event, such as cinema, theater, or a show | 0.648 | 0.419 | 0.705 | |||
| Visiting friends | 0.761 | 0.448 | 0.743 | |||
| Attending a sporting event | 0.806 | 0.413 | 0.792 | |||
| Taking a day trip away from home | 0.697 | 0.563 | 0.605 | |||
| Taking an overnight trip away from home | 0.702 | 0.424 | 0.733 | |||
| Taking a vacation away from home | 0.502 | 0.615 | 0.400 |
Abbreviations: Mental Fatigue (MF); Item explained common variance (I-ECV)
Items stem was: During the past 4 weeks did you experience each of the following? If so, how much mental fatigue did each cause you?
Answer options: No fatigue (0); Mild fatigue (1); Moderate fatigue (2); Extreme fatigue (4).
We assessed local dependence by fitting a one factor CFA model for each scale separately, and evaluating residual correlations. On both scales we found several problematic correlations: 0.201 and 0.203 (PF) and 0.207, 0.211, −0.216, −0.223 (MF). We further examined the effect of including the few locally dependent (LD) items on the IRT item discrimination parameters. For both scales, we first ran a base graded response model with the 39 (PF) and 36 (MF) items respectively. Then we ran alternative models excluding one LD item at a time and compared the item slopes across all models. We found that the effect of the LD items was minimal, so we decided to keep the base model for both scales.
IRT Parameters
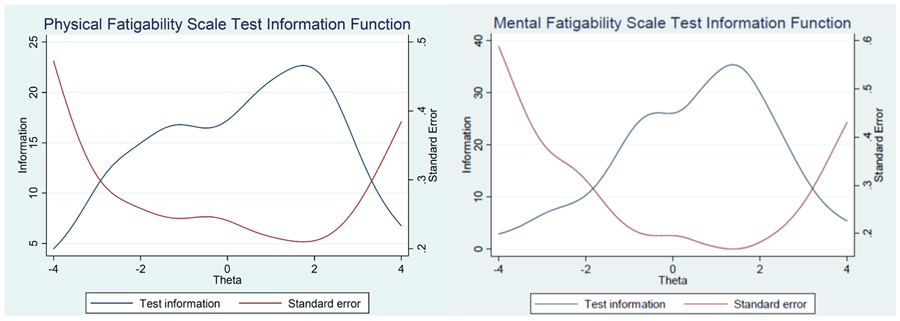
Parameter estimates from the base IRT graded response model, fit in STATA15, are given in Tables 5 and 6. The measurement precision in the theta range between −2.0 and 2.5 is the equivalent of 0.94 reliability for PF and 0.91 for MF (Figure 2). Sixty-eight of the total 75 items showed well-differentiated category characteristic curves (CCC), indicating that each answer choice is the most likely answer at some point along the fatigability trait. In seven of the items the CCCs showed minor problems: in some the “extreme fatigue” option was subsumed under “moderate fatigue,” in others the “mild fatigue” choice was subsumed under “moderate fatigue.”
Table 5.
Physical Fatigue Item Response Theory Parameters
| Scale | Item Content | Slope | Threshold 1 | Threshold 2 | Threshold 3 |
|---|---|---|---|---|---|
| Health Challenges | |||||
| PF Hlth1 | Sleep problems | 1.07 | −2.83 | −0.31 | 1.43 |
| PF Hlth2 | Pain | 1.27 | −2.47 | −0.46 | 0.8 |
| PF Hlth3 | Indigestion problems | 0.89 | −1.98 | 1.56 | 2.94 |
| PF Hlth4 | Dehydration problems | 0.54 | −2.01 | 1.94 | 2.56 |
| PF Hlth6 | Spasticity | 0.99 | −1.60 | 0.48 | 2.34 |
| PF Hlth7 | Stress | 1.13 | −2.01 | 0.27 | 1.71 |
| PF Hlth8 | Medication side-effects | 0.82 | −2.77 | 0.85 | 2.84 |
| Daily Living Challenges | |||||
| PF Home1 | Wheelchair transfer to and from bed | 1.02 | −1.27 | 1.13 | 3.02 |
| PF Home5 | Wheelchair use around the home | 1.68 | −0.32 | 1.17 | 2.44 |
| PF Home9 | Household chores, such as cleaning and tidying | 1.70 | −1.94 | 0.38 | 1.53 |
| PF Home10 | Preparing and clearing away a meal | 2.13 | −1.14 | 0.73 | 2.01 |
| PF Home11 | Eating a meal | 1.50 | 0.62 | 2.03 | 3.98 |
| PF Envr1 | Lack of peace and quiet | 0.77 | −1.94 | 2.29 | 3.88 |
| PF Envr2 | Inadequately adapted home | 1.00 | −2.04 | 1.15 | 2.43 |
| PF Envr3 | Inadequate medical care when at home | 1.04 | −1.46 | 2.15 | 3.61 |
| PF Envr4 | Inadequate non-medical care when at home | 0.95 | −2.08 | 2.03 | 2.89 |
| PF Home3 | Concentrating for an hour or more (such as reading, writing, or holding a conversation) | 1.51 | −0.64 | 0.68 | 2.28 |
| PF Home4 | Using a computer for an hour or more | 1.15 | −1.02 | 0.63 | 3.06 |
| PF Home12 | Letter-writing, form filling or paying bills | 1.13 | −0.53 | 2.36 | 3.41 |
| Seating Challenges | |||||
| PF Home2 | Sitting in a wheelchair for an hour or more | 1.68 | −0.81 | 0.69 | 2.21 |
| PF_Hlth5 | Poor posture | 0.55 | −2.25 | 1.73 | 3.09 |
| PF Home6 | Spending all day in your wheelchair | 1.24 | −2.27 | −0.47 | 1.07 |
| PF Home7 | Pressure management (preventing pressure sores) | 0.91 | −0.53 | 2.22 | 3.44 |
| PF Home8 | Posture management | 1.10 | −1.03 | 1.50 | 3.16 |
| Access Challenges | |||||
| PF Away1 | Wheelchair use over a smooth surface | 1.35 | −0.08 | 1.66 | 3.18 |
| PF Away2 | Wheelchair use over an uneven surface | 1.36 | −1.57 | 0.04 | 1.28 |
| PF Away3 | Wheelchair transfer to and from car | 1.56 | −1.11 | 0.92 | 1.97 |
| PF Away4 | Traveling in your vehicle for an hour or more | 1.42 | −1.35 | 0.38 | 1.85 |
| PF Away5 | Using an adapted taxi | 2.26 | −2.94 | 1.83 | 2.45 |
| PF Away6 | Using a bus | 1.96 | −2.69 | 2.23 | 2.69 |
| PF Away7 | Using a train | 2.39 | −2.71 | 2.03 | 2.47 |
| PF Away9 | Going to a doctor's appointment | 1.15 | −1.61 | 1.28 | 3.06 |
| PF Away10 | Shopping, such as having access and reaching merchandise | 1.69 | −1.01 | 0.56 | 1.77 |
| PF Away12 | Attending an event, such as cinema, theater, or a show | 2.05 | −1.12 | 0.99 | 2.28 |
| PF Away13 | Visiting friends | 2.03 | −1.16 | 1.09 | 1.82 |
| PF Away14 | Attending a sporting event | 1.71 | −1.81 | 1.40 | 2.25 |
| PF Away15 | Taking a day trip away from home | 2.11 | −1.75 | 0.48 | 1.45 |
| PF Away16 | Taking an overnight trip away from home | 1.86 | −2.48 | 0.17 | 1.15 |
| PF Away17 | Taking a vacation away from home | 1.17 | −3.13 | 0.88 | 2.85 |
Abbreviations: Physical Fatigue (PF).
Items stem was: During the past 4 weeks did you experience each of the following? If so, how much physical fatigue did each cause you?
Table 6.
Mental Fatigue Item Response Theory Parameters
| ItemID | Item Content | Slope | Threshold 1 | Threshold 2 | Threshold 3 |
|---|---|---|---|---|---|
| Health Challenges | |||||
| MF Hlth1 | Sleep problems | 0.86 | −3.24 | −0.11 | 1.57 |
| MF Hlth2 | Pain | 0.89 | −3.34 | −0.22 | 1.34 |
| MF Hlth5 | Poor posture | 0.38 | −3.75 | 2.12 | 3.47 |
| MF Hlth7 | Stress | 1.01 | −2.34 | −0.28 | 1.52 |
| MF Hlth8 | Medication side-effects | 0.48 | −3.35 | 1.71 | 3.81 |
| Daily Living Challenges | |||||
| MF Home1 | Wheelchair transfer to and from bed | 1.52 | −0.32 | 1.29 | 2.45 |
| MF Home2 | Sitting in a wheelchair for an hour or more | 1.65 | −0.25 | 1.31 | 1.93 |
| MF Home5 | Wheelchair use around the home | 2.07 | −0.01 | 1.08 | 1.94 |
| MF Home6 | Spending all day in your wheelchair | 1.35 | −1.19 | 0.61 | 1.57 |
| MF Home7 | Pressure management (preventing pressure sores) | 1.32 | −0.41 | 1.92 | 3.32 |
| MF Home8 | Posture management | 1.53 | −0.19 | 1.56 | 2.81 |
| MF Home9 | Household chores, such as cleaning and tidying | 2.22 | −0.78 | 0.72 | 1.67 |
| MF Home10 | Preparing and clearing away a meal | 2.25 | −0.41 | 0.94 | 1.99 |
| MF Home11 | Eating a meal | 2.53 | 0.52 | 1.77 | 2.71 |
| MF Envr1 | Lack of peace and quiet | 0.42 | −2.72 | 2.56 | 3.74 |
| MF Envr2 | Inadequately adapted home | 0.85 | −2.06 | 1.42 | 2.63 |
| MF Envr3 | Inadequate medical care when at home | 0.62 | −1.95 | 2.48 | 3.81 |
| Concentration Challenges | |||||
| MF Home3 | Concentrating for an hour or more (such as reading, writing, or holding a conversation) | 1.85 | −0.70 | 0.57 | 1.93 |
| MF Home4 | Using a computer for an hour or more | 1.62 | −0.46 | 0.66 | 2.66 |
| MF Home12 | Letter-writing, form filling or paying bills | 1.24 | −0.44 | 1.51 | 2.81 |
| Access Challenges | |||||
| MF Away1 | Wheelchair use over a smooth surface | 1.70 | 0.72 | 1.95 | 3.92 |
| MF Away2 | Wheelchair use over an uneven surface | 2.02 | −0.44 | 0.86 | 1.95 |
| MF Away3 | Wheelchair transfer to and from car | 1.78 | −0.66 | 1.32 | 1.96 |
| MF Away4 | Traveling in your vehicle for an hour or more | 2.44 | −0.56 | 0.68 | 1.53 |
| MF Away5 | Using an adapted taxi | 1.49 | −2.47 | 2.60 | 3.01 |
| MF Away6 | Using a bus | 2.11 | −2.46 | 2.40 | 2.61 |
| MF Away7 | Using a train | 2.66 | −2.85 | 2.17 | 2.40 |
| MF Away9 | Going to a doctor's appointment | 1.87 | −1.01 | 1.16 | 2.07 |
| MF Away10 | Shopping, such as having access and reaching merchandise | 3.10 | −0.54 | 0.60 | 1.41 |
| MFAway11 | Going out to a restaurant | 3.36 | −0.12 | 1.16 | 1.61 |
| MF Away12 | Attending an event, such as cinema, theater, or a show | 2.51 | −0.69 | 1.14 | 1.59 |
| MF Away13 | Visiting friends | 2.59 | −0.64 | 1.21 | 2.13 |
| MF Away14 | Attending a sporting event | 1.80 | −1.57 | 1.52 | 2.31 |
| MF Away15 | Taking a day trip away from home | 3.08 | −1.03 | 0.69 | 1.35 |
| MF Away16 | Taking an overnight trip away from home | 2.59 | −1.44 | 0.72 | 1.18 |
| MF Away17 | Taking a vacation away from home | 1.48 | −2.64 | 1.37 | 2.02 |
Abbreviations: Mental Fatigue (MF). Items stem was: During the past 4 weeks did you experience each of the following? If so, how much mental fatigue did each cause you?
Figure 2.
Physical and Mental Fatigability Test Information and Standard Error
The lower axis shows the range of fatigability. The blue curve (test information) shows that the measurement precision, or reliability, in the theta range −2.0 to 2.5 is 0.94 for physical fatigability, and 0.91 for mental fatigability. Both scales display fairly high precision in discriminating among individuals with a relatively wide range of fatigability.
Differential Item Functioning
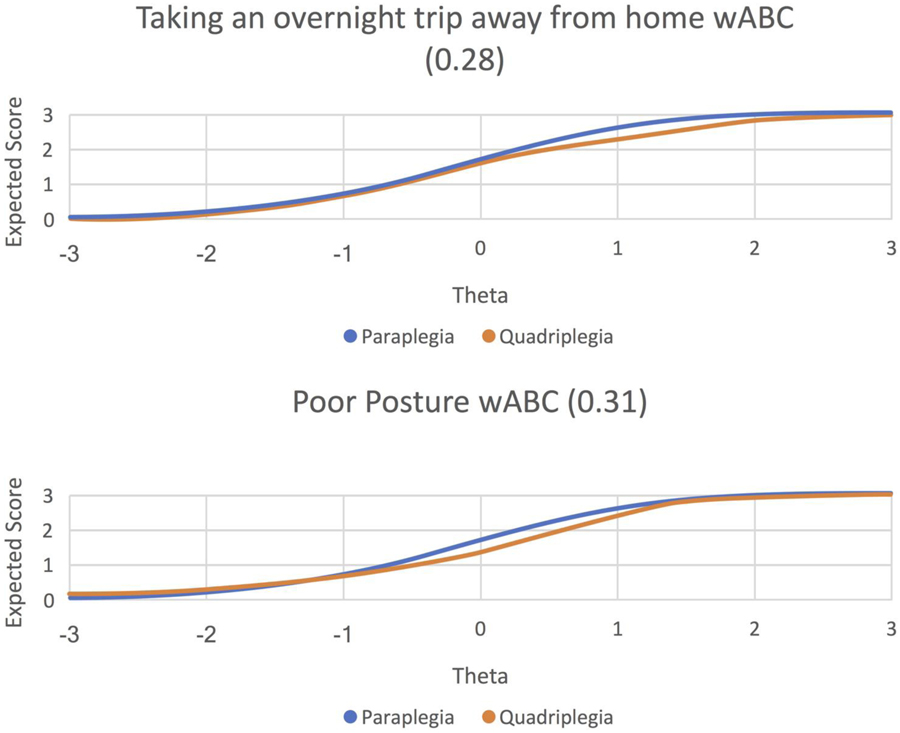
After Benjamini-Hochberg adjustment, there was no significant DIF by age or time since injury. Tables 7 and 8 show chi-square and wABC values with significant DIF by gender and diagnoses for the two measures. Only two items exceeded the 0.24 threshold for non-ignorable DIF in the diagnosis comparison: “Taking an overnight trip away from home” (PF scale) (wABC = 0.28), and “Posture problems” (MF scale) (wABC = 0.31). Given the same level of fatigability, uniformly across the continuum respondents with paraplegia (n=288) were more likely than those with quadriplegia (n=176) to report physical fatigue when taking an overnight trip away from home. For mental fatigue relating to posture problems, at the lower end of the theta range those with paraplegia were less likely than those with quadriplegia to report mental fatigue, but more likely to report it as fatigability increased. Figure 3 shows graphical representations of the effect size for both items. The impact of DIF on the overall mean scores for the two diagnosis groups was small. When DIF was accounted for by estimating item parameters separately for paraplegia and quadriplegia, the mean score difference between the groups was 0.49 SD (PF), and 0.74 SD (MF). When DIF was ignored by constraining all items to have equal parameters across diagnosis groups, the mean differences were 0.42 SD and 0.64 SD for the PF and MF scores, respectively. So adjusting for DIF makes only 0.07 SD (PF) and 0.10 SD (MF) change in the difference between diagnosis groups.
Table 7.
Chi-square and wABC values for physical fatigability items with significant DIF by sex and diagnosis
| Comparison | Item | wABC | Chi-square | p-value |
|---|---|---|---|---|
| Sex | PFHome1 | 0.10 | 24.2 | 0.0001 |
| Sex | PFHome9 | 0.14 | 22.1 | 0.0002 |
| Sex | PFHome10 | 0.08 | 17.5 | 0.0015 |
| Sex | PFHome3 | 0.05 | 14 | 0.0012 |
| Sex | PFHome6 | 0.10 | 17.8 | 0.0013 |
| Sex | PFaway1 | 0.22 | 25.7 | 0.0001 |
| Sex | PFAway3 | 0.13 | 15.2 | 0.0043 |
| Sex | PFAway10 | 0.08 | 13.3 | 0.0100 |
| Sex | PFAway15 | 0.08 | 21.8 | 0.0002 |
| Diagnosis | PFHlth6 | 0.16 | 24.1 | 0.0001 |
| Diagnosis | PFEnvr2 | 0.19 | 29.3 | 0.0001 |
| Diagnosis | PFHome2 | 0.13 | 16.9 | 0.0021 |
| Diagnosis | PFHome3 | 0.21 | 32.7 | 0.0001 |
| Diagnosis | PFHome8 | 0.15 | 27 | 0.0019 |
| Diagnosis | PFAway3 | 0.10 | 16.3 | 0.0027 |
| Diagnosis | PFAway4 | 0.09 | 23 | 0.0001 |
| Diagnosis | PFAway6 | 0.17 | 18.6 | 0.0009 |
| Diagnosis | PFAway13 | 0.07 | 18.9 | 0.0033 |
| Diagnosis | PFAway16 | 0.28 | 20.5 | 0.0004 |
Abbreviations: Weighted area between the curves (wABC).
Table 8.
Chi-square and wABC values for mental fatigability items with significant DIF by sex and diagnosis
| Comparison | Item | wABC | Chi-square | p-value |
|---|---|---|---|---|
| Sex | MFHlth1 | 0.09 | 15.1 | 0.0062 |
| Sex | MFHome8 | 0.06 | 14.4 | 0.0011 |
| Sex | MFEnvr2 | 0.07 | 18.3 | 0.0092 |
| Sex | MFAway14 | 0.07 | 15 | 0.0047 |
| Sex | MFAway15 | 0.06 | 15.1 | 0.0045 |
| Diagnosis | MFHlth1 | 0.12 | 16.1 | 0.0029 |
| Diagnosis | MFHlth5 | 0.31 | 39.1 | 0.0001 |
| Diagnosis | MFHlth7 | 0.10 | 13.8 | 0.0079 |
| Diagnosis | MFHome8 | 0.14 | 21.6 | 0.0002 |
| Diagnosis | MFEnvr3 | 0.10 | 17 | 0.0001 |
| Diagnosis | MFAway16 | 0.10 | 24.4 | 0.0001 |
Abbreviations: Weighted area between the curves (wABC).
Figure 3.
Graphical Representation of Differential Item Functioning Effect Size
Construct Validity
For both scales, F-statistics p-values for paraplegia and incomplete paraplegia groups were significant at p < .01, and means were higher for those who reported having a paraplegia vs quadriplegia, and for those with an incomplete paraplegia vs complete paraplegia, incomplete and complete quadriplegia (Supplemental Tables 6 and 7). The correlation between the two scales was 0.92. The largest significant correlations were found between the PF and MF Access scales (0.86), PF and MF Health scales (0.75), and PF and MF Daily living scales (0.81).
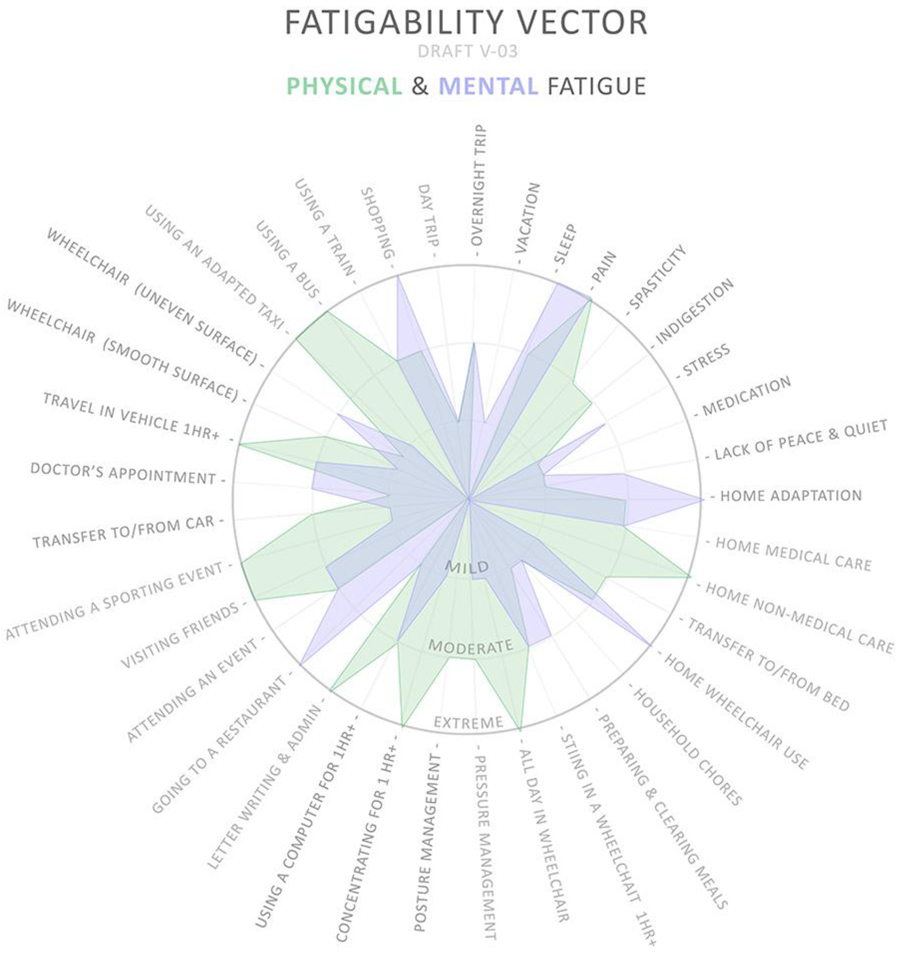
Visualizing Fatigue
To ensure ease of application in clinical settings, patient answers need to be presented in a simple and meaningful way, that delivers an instant picture of a person’s physical and/or mental fatigability footprint, and in doing so, immediately highlights areas for possible intervention.
To visualize a patient’s vulnerability to fatigue, we propose a Fatigability Vector that includes all items retained after the psychometric assessment (Figure 4). To our knowledge, this visualization approach has not been proposed before. In this vector, each survey item has its own spoke with the four answer options. Taken together, they capture the full response plot for both physical and mental fatigue, showing the respondent’s physical and mental fatigability footprint. A clinician can thus identify areas that require immediate intervention, to address extreme fatigability, as well as preemptive intervention in the case of mild and moderate fatigue. The chart can also help compare physical and mental fatigability, and a patient’s footprint over time, showing the result of the intervention over time.
Figure 4.
Combined Physical and Mental Fatigability Vector
The vector displays concentric circles, beginning with no fatigue in the center, then radiating out for increasing levels of fatigue (mild, moderate, and extreme). Around the perimeter of the vector, we have added the range of survey items, such as posture management, attending a sporting event, wheelchair use over an uneven surface, home adaptation issues, and pressure management.
Each survey item, such as home adaptation, has its own spoke in the wheel of the proposed a Fatigability Vector, so when, for example, someone answers the question on home adaptation, they have the four answer choices. The vector captures a hypothetical full response plot where physical and mental fatigability are overlaid, which can be linked and filled with color to show the overall fatigability footprint.
Discussion
We developed and evaluated the psychometric properties of two measures: physical and mental fatigability. The need for two separate scales emerged from our in-depth interviews. During the cognitive interviews conducted prior to the field test (see Figure 1) we found that participants had no trouble differentiating between the two scales, which aligned with our findings from the in-depth interviews. A specific index of susceptibility to fatigue in SCI—that is, fatigability-- can help clinicians establish the level of vulnerability of an individual. It can also highlight issues that might cause fatigue and require further probing, such as correct techniques to self-propel in manual wheelchairs, moving up and down ramps, or doing wheelchair transfers. Adding this index to other SCI-specific instruments, such as the self-reported Spinal Cord Independence Measure III, can increase the focus on patient-centered care in SCI. More broadly, the index could be incorporated into wheelchair assessment and prescription protocols by mobility vendors.
The test information curves for the fatigability measures reported here show that the questions work best for individuals with mild and moderate fatigability, where interventions could ameliorate symptoms. But they are also informative for those with limited fatigability and extreme fatigability, where the need for interventions is more immediate.
This study also found that 18 PF items and 26 MF items had high or very high discrimination power (slopes > 1.35). In addition, the item category characteristics are generally well-differentiated for 68 of the 75 items. For the few items where that is not the case, it might be helpful to collapse one or more of the answer categories into an adjacent response option and offer fewer response options in the future.
Limitations
Socially desirable response bias is a concern with this type of self-reported data, even though the survey was not administered in person or via telephone.42,43 Another limitation is selection bias. Certain types of individuals may be more likely to respond because they are computer-literate, or have access to a peer-group based at a rehabilitation center, while other types of individuals may be more inclined to offer their time to complete the surveys for no remuneration. Non-representative sampling makes the generalizability of findings problematic especially because we did not formally explore the extent to which the measurement process is similar across different measurement situations, for example community vs clinical settings, and modes of administration. A larger and more-representative sample would allow more definitive evaluation of DIF.31 Finally, because the denominator is unknown for this convenience sample, the response rate is unknown.
Conclusions
These findings should be confirmed with larger, representative datasets, which would improve the precision of the estimates. Future research needs to be done to evaluate whether the not applicable response category should be treated differently. Future research should focus on the development of short forms for the two measures, and exploring computer-adaptive test administration of the existing item banks.
Supplementary Material
Funding
Alina Ionela Palimaru was supported by a University of California Los Angeles Dissertation Year Fellowship.
Dr. Hays was supported in part by the Resource Centers for Minority Aging Research/Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under National Institutes of Health/National Institute on Aging (NIH/NIA) grant P30-AG021684
Dr. Cunningham was supported by Resource Centers for Minority Aging Research/Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under National Institutes of Health/National Institute on Aging (NIH/NIA) grant P30-AG021684, and NIH/National Institute for Minority Health and Health Disparities (NIMHD) / 2P20MD000182-11 / Excellence in Partnerships for Community Outreach, Research on Health Disparities and Training Center (Drew-UCLA Project EXPORT Center).
The funders had no role in the study design, data collection, analysis and interpretation of data, writing of the report, or in the decision to submit the article for publication.
List of Abbreviations:
- SCI
(spinal cord injury)
- PF
(physical fatigability)
- MF
(mental fatigability)
- CFA
(confirmatory factor analysis)
- IRT
(item response theory)
- DIF
(differential item functioning)
- wABC
(weighted area between the curves)
- CCC
(category characteristic curves)
- RMSEA
(Root Mean Square Error of Approximation)
- CFI
(Comparative Fit Index)
- TLI
(Tucker-Lewis Index)
- PUC
(percent uncontaminated correlations)
- ECVGEN
(explained common variance on the general dimension)
- I-ECV
(individual explained common variance)
Footnotes
Conflicts of interest
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
The manuscript submitted does not contain information about medical device(s).
Human and animal rights
All procedures performed in this study involving human participants were in accordance with the ethical standards of the UCLA institutional review board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.NSCISC. (2016, May 27). SCI facts and figures at a glance. Retrieved from https://www.nscisc.uab.edu/Public/Facts%202016.pdf
- 2.National Institutes of Health. (2015, September 16). Development of Measures of Fatigability in Older Adults (R21) . Retrieved from RFA Section I Funding: http://grants.nih.gov/grants/guide/rfa-files/RFA-AG-16-013.html#_Section_I._Funding
- 3.Anton HA, Miller WC, & Townson AF (2008). Measuring Fatigue in Persons with Spinal Cord Injury. Arch Phys Med Rehabil, 538–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McColl M, Arnold R, Charlifue S, Glass C, Savic G, & Frankel H (2003). Aging, spinal cord injury, and quality of life: structural relationships. Arch Phys Med Rehabil, 1137–1144. [DOI] [PubMed] [Google Scholar]
- 5.Elliott T (1996). Depression following spinal cord injury. Arch Phys Med Rehabil, 816–823. [DOI] [PubMed] [Google Scholar]
- 6.Hirsch G, Menard M, & Anton H (1991). Anemia in Spinal Cord Injury. Arch Phys Med Rehabil, 195–201. [PubMed] [Google Scholar]
- 7.Hughes R, Swedlund N, Petersen N, & Nosek M (2001). Depression and Women with Spinal Cord Injury. Topics in SCI Rehabilitation, 16–24. [Google Scholar]
- 8.Streeten D, & Anderson G (1998). The role of delayed orthostatic hypotension in the pathogenesis of chronic fatigue. Clin Autonomic Research, 119–124. [DOI] [PubMed] [Google Scholar]
- 9.Widerstrom-Noga E, Felipe-Cuervo E, & Yezierski R (2001). Chronic pain after spinal cord injury: Interference with sleep and daily activities. Arch Phys Med Rehabil, 1571–1577. [DOI] [PubMed] [Google Scholar]
- 10.Gerhart K, Bergstrom E, Charlifue S, Menter R, & Whiteneck G (1993). Long-term spinal cord injury: functional changes over time . Arch Phys Med Rehabil, 1030–1034. [DOI] [PubMed] [Google Scholar]
- 11.Charlifue S, Weitzenkamp D, & Whiteneck G (1999). Longitudinal outcomes in spinal cord injury: aging, secondary conditions, and well-being. Arch Phys Med Rehabil, 1429–1434. [DOI] [PubMed] [Google Scholar]
- 12.Glynn N, Santanasto A, Simonsick E, Boudreau R, Beach S, Schulz R, & Newman A (2015). The Pittsburgh Fatigability Scale for Older Adults: Development and Validation. J Am Geriatr, 130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richardson CA, Glynn NW, Ferrucci LG, & Mackey DC (2015). Walking Energetics, Fatigability, and Fatigue in Older Adults: The Study of Energy and Aging Pilot. J Gerontol A Biol Sci Med Sci, 487–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murphy SL, Alexander N, Levoska M, & Smith D (2013). The Relationship between Fatigue and Subsequent Physical Activity among Older Adults with Symptomatic Osteoarthritis. Arthritis Care Res, 1617–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schnelle J, Buchowski M, Ikizler T, Durkin D, Beuscher L, & Simmons S (2012). Evaluation of Two Fatigability Severity Measures in Elderly Adults. Journal of the American Geriatrics Society, 1527–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang C, & Wu C (2005). The Situational Fatigue Scale: A different approach to measuring fatigue. Quality of Life Research, 1357–1362. [DOI] [PubMed] [Google Scholar]
- 17.Tiesinga L, Dassen T, & Halfens R (1998). DUFS and DEFS: Development, reliability and validity of the Dutch Fatigue Scale and the Dutch Exertion Fatigue Scale. International Journal of Nursing Studies, 115–123. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, D.C.: Author. [PubMed] [Google Scholar]
- 19.Reeve BB, Wyrwich KW, Wu AW, Velikova G, Terwee CB, Synder CF, … Butt Z (2013). ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Quality of Life Research, 22, 1889–1905. [DOI] [PubMed] [Google Scholar]
- 20.Palimaru A, Cunningham WE, Dillistone M, Vargas-Bustamante A, Liu H, & Hays RD (2017). A comparison of perceptions of quality of life among adults with spinal cord injury in the United States versus the United Kingdom. Quality of Life Research, 26(11), 3143–3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marshall GN, Morales LS, Elliott M, Spritzer K, & Hays RD (2001). Confirmatory factor analysis of the Consumer Assessment of Health Plans Study (CAHPS) 1.0 Core Survey. Psychological Assessment, 13(2), 216–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.SAS Institute Inc (2013). SAS/ACCESS® 9.4 Interface to ADABAS: Reference. Cary, NC: SAS Institute Inc. [Google Scholar]
- 23.Muthén L. a. (2015). Mplus User’s Guide (Vol. Seventh Edition). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- 24.Hammell KW, Miller WC, Forwell SJ, Forman BE, & Jacobsen BA (2009). Managing fatigue following spinal cord injury: A qualitative exploration. Disability and Rehabilitation, 31(17), 1437–1445. [DOI] [PubMed] [Google Scholar]
- 25.Brown TA (2006). Confirmatory Factor Analysis for Applied Research. New York, New York: The Guilford Press. [Google Scholar]
- 26.StataCorp. (2015). Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- 27.Tulsky DS, Kisala PA, Tate DG, Spungen AM, & Kirshblum SC (2015). Development and psychometric characteristics of the SCI-QOL Bladder Management Difficulties and Bowel Management Difficulties item banks and short forms and the SCI-QOL Bladder Complications scale. The Journal of Spinal Cord Medicine, 38(3), 288–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jette AM, Slavin MD, Ni P, Kisala PA, Tulsky DS, Heinemann AW, … Williams S (2015). Development and initial evaluation of the SCI-FI/AT. The Journal of Spinal Cord Medicine, 38(3), 409–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lara M, Edelen MO, Eberhart NK, Stucky BD, & Sherbourne CD (2014). Development and validation of the RAND Asthma Control Measure. European Respiratory Journal, 44, 1243–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jackson DL, Gillaspy JA, & Purc-Stephenson R (2009). Reporting practices in confirmatory factor analysis: an overview and some recommendations. Psychological Methods, 14(1), 6–23. [DOI] [PubMed] [Google Scholar]
- 31.Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA, … Cella D (2007). Psychometric evaluation and calibration of health-related quality of life item banks: plans for the patient-reported outcome measurement information system (PROMIS). Medical Care, 45, S22–31. [DOI] [PubMed] [Google Scholar]
- 32.Reise SP, Morizot J, & Hays RD (2007). The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Quality of Life Research, 16, 19–31. [DOI] [PubMed] [Google Scholar]
- 33.Reise SP, Scheines R, Widaman K, & Haviland M (2013). Multidimensionality and structural coefficient bias in structural equation modeling: a bifactor perspective. Educational and Psychological Measurement, 73(1), 5–26. [Google Scholar]
- 34.Embretson SE, & Reise SP (2000). Item Response Theory for Psychologists. Mahwah, New Jersey: Lawrence Erlbaum Associates. [Google Scholar]
- 35.Wellman RJ, Edelen MO, & DiFranza JR (2015). Item Response Theory analysis of the Autonomy over Tobacco Scale (AUTOS). Addictive Behaviors, 45, 195–200. [DOI] [PubMed] [Google Scholar]
- 36.Hays RD, & Revicki D (2005). Reliability and Validity (Including Responsiveness). In Fayers P, & Hays RD, Assessing Quality of Life in Clinical Trials 2nd Edition (pp. 25–39). Oxford: Oxford University Press. [Google Scholar]
- 37.Edelen MO, Stucky BD, & Chandra A (2015). Quantifying 'problematic' DIF within an IRT framework: application to a cancer stigma index. Quality of Life Research, 24, 95–103. [DOI] [PubMed] [Google Scholar]
- 38.Hays RD, Morales LS, & Reise SP (2000). Item Response Theory and health outcomes measurement in the 21st century. Medical Care, 9 Suppl, II28 – II42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, 57(1), 289–300. [Google Scholar]
- 40.Hays RD, & Reeve BB (2010). Measurement and modeling of health-related quality of life. In Killewo J, Heggenhougen HK, & Quah SR, Epidemiology and demography in public health (pp. 195–205). San Diego: Elsevier. [Google Scholar]
- 41.Stucky BD, Edelen MO, Vaughan CA, Tucker JS, & Butler J (2014). The psychometric development and initial validation of the DCI-A short form for adolescent therapeutic community treatment process. Journal of Substance Abuse Treatment, 46, 516–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McHorney CA, Kosinski M, & Ware JE (1994). Comparisons of the costs and quality of norms for the SF-36 health survey collected by mail versus telephone interview: results from a national survey. Medical Care, 551–567. [DOI] [PubMed] [Google Scholar]
- 43.Hays RD, Kim S, Spritzer KL, Kaplan RM, Tally S, Feeny D, … Fryback DG (2009). Effects of mode and order of administration on generic health-related quality of life scores. Value in Health, 1035–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.