Abstract
To investigate computed tomography (CT) diagnostic reference levels for coronavirus disease 2019 (COVID-19) pneumonia by collecting radiation exposure parameters of the most performed chest CT examinations and emphasize the necessity of low-dose CT in COVID-19 and its significance in radioprotection.
The survey collected RIS data from 2119 chest CT examinations for 550 COVID-19 patients performed in 92 hospitals from January 23, 2020 to May 1, 2020. Dose data such as volume computed tomography dose index, dose-length product, and effective dose (ED) were recorded and analyzed. The radiation dose levels in different hospitals have been compared, and average ED and cumulative ED have been studied.
The median dose-length product, volume computed tomography dose index, and ED measurements were 325.2 mGy cm with a range of 6.79 to 1098 mGy cm, 9.68 mGy with a range of 0.62 to 33.80 mGy, and 4.55 mSv with a range of 0.11 to 15.37 mSv for COVID-19 CT scanning protocols in Chongqing, China. The distribution of all observed EDs of radiation received by per patient undergoing CT protocols during hospitalization yielded a median cumulative ED of 17.34 mSv (range, 2.05–53.39 mSv) in the detection and management of COVID-19 patients. The average number of CT scan times for each patient was 4.0 ± 2.0, and the average time interval between 2 CT scans was 7.0 ± 5.0 days. The average cumulative ED of chest CT examinations for COVID-19 patients in Chongqing, China greatly exceeded public limit and the annual dose limit of occupational exposure in a short period.
For patients with known or suspected COVID-19, a chest CT should be performed on the principle of rapid-scan, low-dose, single-phase protocol instead of routine chest CT protocol to minimize radiation doses and motion artifacts.
Keywords: computed tomography, coronavirus disease 2019 pneumonia, effective dose, radiation exposure
1. Introduction
The outbreak of coronavirus disease 2019 (COVID-19) caused by the novel, pathogenic SARS-coronavirus 2 and started December 2019, has rapidly spread across >200 countries.[1] Pneumonia is the one of most common manifestations in COVID-19 that invades and attacks respiratory system, where can appear in the chest computed tomography (CT) imaging of COVID-19 patients.
Chest CT imaging plays an important role in detecting COVID-19 before receiving the reverse transcription-polymerase chain reaction (RT-PCR) nucleic acid testing, and is majorly helpful in screening and management for suspected COVD-19 patients with epidemiologic features compatible with COVID-19 infection particularly but negative RT-PCR tests.[2,3] Therefore, it can be considered a useful test for relieving quickly difficult situations, especially in centers that laboratory tests may not be easily accessible. due to the lack of kits, delay waiting for the results, as well as false negative cases.[4]
Moreover, on the basis of the 7th trial version of diagnosis and treatment of COVID-19,[5] the hospitalized patients should receive follow-up CT to evaluate the changes of pneumonia or quantify the inflammation absorption and dissipation of the lungs in chest CT images during the follow-up scanning, and the discharged patients need also close medical observation by follow-up CT.[6,7] Actually, some suspected patients may receive one or more CT examinations to ensure they are healthy within a short period of time.[4,8] Therefore, medical radiation exposure of multiple CT should be more concerned,[9] especially for special community such as children and pregnant women. But until now, the average accumulation dose per COVID-19 patient within hospitalization has not been well known.
The aim of this study was to investigate the current radiation dose levels for chest CT examinations in COVID-19 patients by collecting the primary dosimetry metrics such as dose-length product (DLP), volume computed tomography dose index (CTDIvol), and effective dose (ED) for each examination and calculating the cumulative ED for each patient, and comparing the differences of those in different designated hospitals admitting COVID-19 patients throughout Chongqing, China. Based on this data, to make radiological technicians know the real radiation exposure levels of COVID-19 patients and the necessity of low-dose CT in COVID-19 and its significance in radioprotection.
2. Materials and methods
2.1. Participants
This study was subject to approval by the Ethics Committee of our hospital. Signed informed consent was exempted due to the retrospective nature of the study. This survey collected the detailed protocols of 2119 non-contrast chest CT examinations from 550 patients with COVID-19 in 92 hospitals consisting of 3 designated hospitals and 89 first-visited hospitals of those throughout Chongqing Municipality. The data were collected from January 23, 2020 to May 1, 2020. Inclusion criteria were as follows: patients with laboratory-confirmed SARS-coronavirus 2 infection by RT-PCR in Chongqing who underwent both chest CT scan and RT-PCR examinations. Exclusion criteria: the CT image quality of the patients did not meet the need of diagnosis for radiologist. Exclusion criteria: failure to provide complete dose reports or incomplete questionnaires impacted on statistical results.
2.2. Data collected
The data collected from each hospital included the scale of hospital, the information and the conditions of patients, chest CT protocols employed, and the CTDIvol and DLP values displayed on dose report of CT scanner during each non-contrast chest CT scan. Examination times, time interval between 2 successive CT scans, and the average value between the minimum and maximum values of CTDIvol, DLP, and ED for each patient were calculated, where ED was calculated using a conversion factor (k) of 0.0145 mSv × mGy−1 × cm−1.[10] The cumulative ED can be obtained by summing all observed EDs of radiation received by per patient undergoing CT protocols during hospitalization.
2.3. Statistical analysis
The statistical analysis and computations were performed using R software (version 3.5.2, R Foundation for Statistical Computing, Vienna, Austria, https://www.r-project.org/). Continuous data were presented as mean ± standard deviation and categorical data were reported as counts and the percentage of the total. The normality and variance homogeneity of continuous variables were evaluated using the Shapiro-Wilk test and Levene test, respectively. Significance analyses of normally distributed and quantitative data with equal variance between groups were performed using unpaired or paired Student t test, while Mann–Whitney U test or Wilcoxon signed-rank test was used for the quantitative data that did not follow a normal distribution. Group comparisons of categorical data were performed with the use of Fisher exact test or chi-square test. The threshold of statistical significance was set to a 2-sided α of <0.05.
3. Results
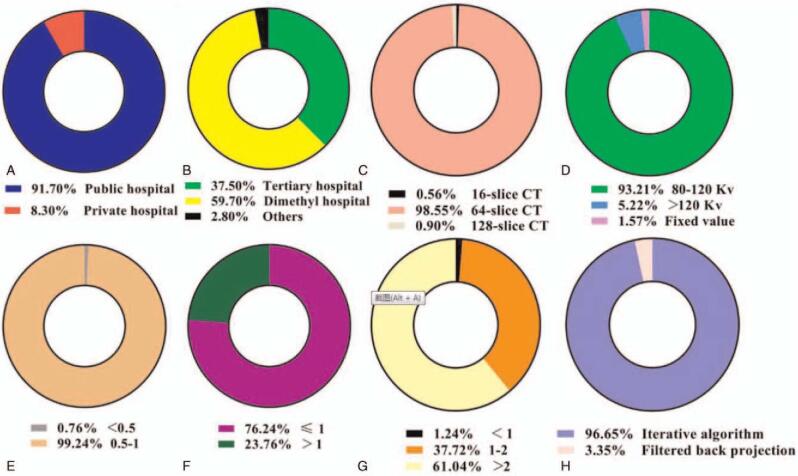
This survey collected the detailed protocols of 2119 non-contrast chest CT examinations from 550 patients with COVID-19 in 92 hospitals consisting of 3 designated hospitals and 89 first-visited hospitals of those. The demographic information of registered patients was presented in Table 1. The basic information and the chest CT scanning protocols for COVID-19 of 92 hospitals including hospital level, multi-slice capability of CT scanners, tube voltage, rotate speed, pitch, imaged slice thickness, and the type of reconstruction algorithms were shown in Fig. 1, of which 504 are public and 46 are private, and the proportion of tertiary hospitals reached 37.5%. All scanners surveyed had multi-slice capability ranging from 2 to 256 slices (Fig. 1), of which 16-slice or 64-slice CT scanners were the most common with tube voltages (range, 80–120 kV), rotate speeds (range, 0.5–1.0 r/min), pitch (range, 0.7–1.5), slice thickness (range, 2–5 mm) using iterative reconstruction algorithm.
Table 1.
The demographic information and clinical characteristics.
| Characteristics | All patients (N = 550) |
| Age, y | 47 (16) |
| Sex | |
| Female | 254 (46.18%) |
| Male | 296 (53.82%) |
| Radiological examination | |
| Only DR | 0 |
| Only CT | 465 (84.5%) |
| CT and DR | 85 (15.5%) |
Figure 1.
The proportion of basic information of the chest CT scanning protocols for COVID-19 in 92 hospitals including (A) hospital nature, (B) hospital level, (C) multi-slice capability, (D) tube voltage, (E) rotate speed, (F) pitch, (G) slice thickness, and (H) types of reconstruction algorithms. COVID-19 = coronavirus disease 2019, CT = computed tomography.
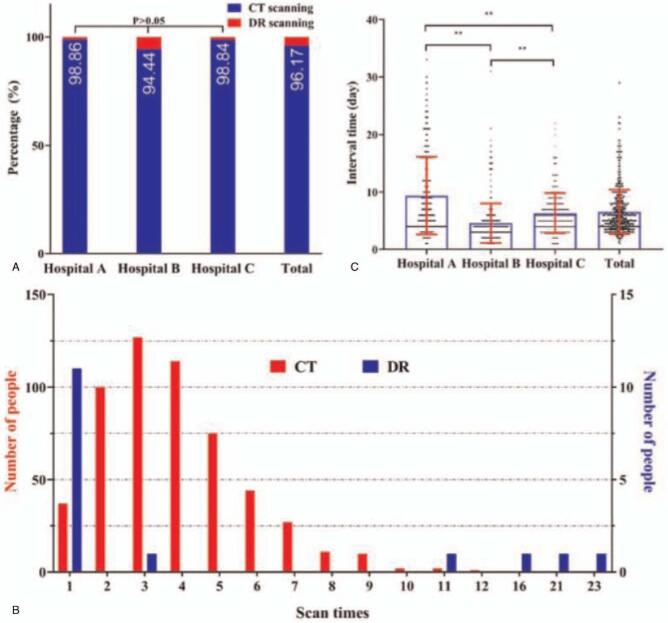
The proportion of CT and digital radiography (DR) scans for detection and management of COVID-19 in 3 designated hospitals of Chongqing, southwest China was shown in Fig. 2A. It indicated that chest CT is the main radiological technique. The frequency distribution of CT and DR scanning times for the 550 COVID-19 patients in Fig. 2B shown that the most patients received the number of CT scans ranges from 2 to 6 during their hospitalization. The time interval between 2 successive CT scans for each COVID-19 patient in these designated hospitals was illustrated in Fig. 2C. The average number of CT scan times for each patient was 4.0 ± 2.0, and the average time interval between 2 CT scans was 7.0 ± 5.0 days.
Figure 2.
The basic information about radiological examination for COVID-19. (A) The proportion of imaging techniques for CT and DR in 3 designated hospitals and the total hospitals. (B) The frequency distribution of CT and DR scanning times. (C) The interactive bar graph and scatter plot applications for showing the time intervals between 2 successive CT scans for COVID-19 patients. COVID-19 = coronavirus disease 2019, CT = computed tomography, DR = digital radiography.
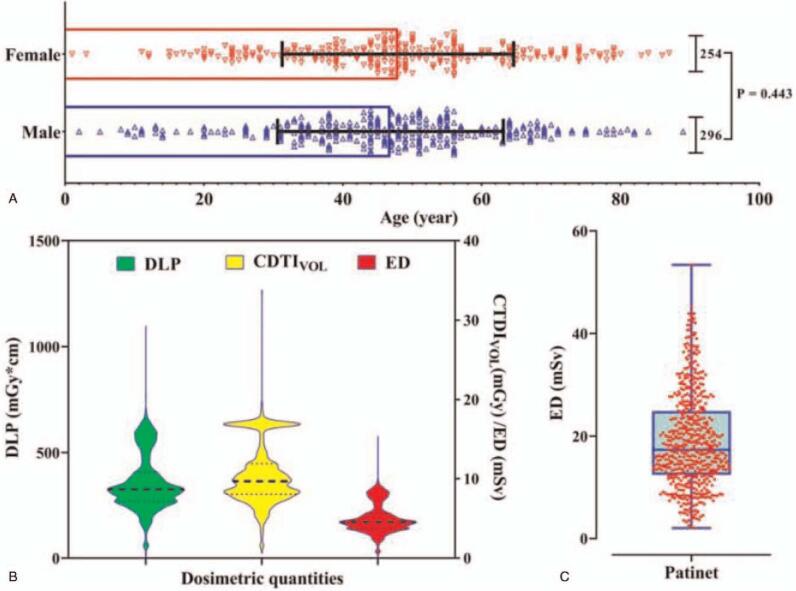
The dosimetry quantities of the surveyed 2119 CT examinations for 550 COVID-19 patients were shown in Fig. 3, of which 254 women and 296 men were included without significant difference in age (Fig. 3A). The median DLP (325.2 mGy cm; range, 6.79–1098 mGy cm), CTDIvol (9.68 mGy; range, 0.62–33.80 mGy), and ED (4.55 mSv; range, 0.11–15.37 mSv) for COVID-19 CT scanning protocols in Chongqing, China were summarized (Table 2), and the corresponding distributions of radiation dose descriptors were shown in Fig. 3B. The distribution of all observed EDs of radiation received by per patient undergoing CT protocols during hospitalization yielded a median cumulative effective dose of 17.34 mSv (range, 2.05–53.39 mSv) for all patients in the detection and management of COVID-19 (Fig. 3C and Table 2).
Figure 3.
The statistical result of 2119 non-enhanced chest CT scans. (A) the age and sex distribution of 550 COVID-19 patients. (B) The violin plot of the radiation exposure parameters such as DLP, CDTIvol, and ED. (C) The violin plot of cumulative ED per patient during hospitalization. COVID-19 = coronavirus disease 2019, CT = computed tomography, CTDIvol = volume computed tomography dose index, DLP = dose-length product, ED = effective dose.
Table 2.
Descriptive statistics of the radiation dose descriptors of the surveyed 2119 CT examinations for 550 COVID-2019 patients in Chongqing, China.
| Median | Range | 25th to 75th percentile | Mean | Standard deviation | |
| CT examinations (N = 2119) | |||||
| DLP, mGy cm | 325.2 | 6.79–1098 | 268.0–405.6 | 355.22 | 130.51 |
| CTDIVOL, mGy | 9.680 | 0.62–33.80 | 8.04–11.92 | 10.48 | 3.79 |
| ED, mSv | 4.55 | 0.11–15.26 | 3.75–5.68 | 4.976 | 1.824 |
| COVID-2019 patient (N = 550) | |||||
| Cumulative ED, mSv | 17.34 | 2.058–53.39 | 12.43–24.89 | 19.07 | 9.25 |
| DLPmax-min, mGy cm | 113.4 | 0.20–659.2 | 47.24–254.3 | 159.43 | 135.50 |
| CTDIVOLmax-min, mGy | 2.25 | 0.32–189.3 | 0.92–7.10 | 4.382 | 9.17 |
| EDmax-min, mSv | 1.58 | 0.003–9.23 | 0.66–3.56 | 2.23 | 1.89 |
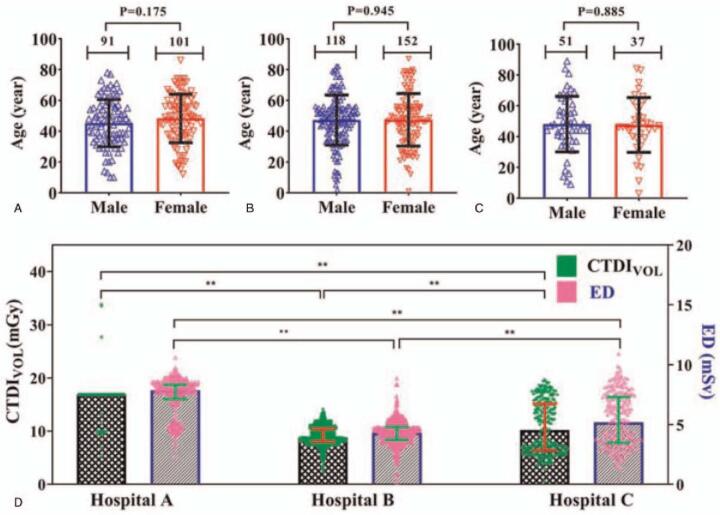
The comparison results of surveyed data from the first-visited hospital and 3 designated hospitals (tertiary hospitals) were shown in Tables 3 and 4. The sex (P = .285) and age (P = .374) of COVID-19 patients from these 3 hospitals were no statistically significant difference (Fig. 4A–C). Our survey found that the CTDIvol, DLP, and ED have obvious significant difference among the 3 designated hospitals (P < .001) and between first-visited and treatment hospitals (P < .001). The COVID-19 patients in Hospital A received a significantly higher effective dose per CT examination (median 7.85 mSv; range, 2.35–10.60 mSv) than did COVID-19 patients in Hospital B (median, 4.31 mSv; range, 0.11–8.86 mSv) and those in Hospital C (median, 5.18 mSv; range, 0.32–10.91 mSv) (P < .001, Fig. 4D). The mean values of CTDIvol, DLP, and ED ranges were 4.38 ± 9.17 mGy, 159.43 ± 135.50 mGy cm, and 2.23 ± 1.89 mSv in multiple CT scans for a patient, particularly the maximum range of ED up to 9.23 mSv for a certain patient. Figure 5 shown a patient received 2 chest CT examinations by a 64-slice detector CT in a period, where the ED of the later scanning were 50% lower than that of the former scanning, while the image quality of both images meets the diagnostic criteria. These findings support the recommendation of low-dose CT in the detection and management of COVID-19.
Table 3.
The compassion of radiation dose exposure parameters between the first-visited and designated hospitals.
| First-visited hospital | Designated hospital | P value | |
| CT scanning times | N = 224 | N = 1895 | |
| CTDIVOL, mGy | 8.91 (7.31–10.81) | 9.78 (8.47–11.02) | .067a |
| DLP, mGy cm | 276.70 (240.98–335.37) | 326.49 (298.92–369.68) | <.001a |
| ED (K = 0.014), mSv | 3.87 (3.37–4.70) | 4.57 (4.18–5.18) | .008a |
Table 4.
The compassion of radiation dose exposure parameters among 3 designated hospitals.
| Hospital A | Hospital B | Hospital C | P value | |
| CT scanning times | N = 383 | N = 1241 | N = 271 | |
| CTDIVOL, mGy | 16.9 (16.9–16.9)∗# | 8.78 (8.04–10.45) ∗† | 10.23 (6.4–15.17)#† | <.001a |
| DLP, mGy cm | 560.7 (509.9–594.6)∗# | 307.3 (266.1–342.6)∗† | 370.0 (248.5–521.0)#† | <.001a |
| ED, mSv | 7.85 (7.14–8.32)∗# | 4.30 (3.72–4.79)∗† | 5.18 (3.47–7.29)#† | <.001a |
Figure 4.
The comparison of radiation exposure parameters among 3 designated hospitals. (A)–(C) The age and sex distribution of COVID-19 patients in Hospital A, B, and C. The interactive bar graph and scatter plot applications for showing the levels of CDTIvol and ED per CT examination for the 3 designated hospitals. COVID-19 = coronavirus disease 2019, CT = computed tomography, CTDIvol = volume computed tomography dose index, ED = effective dose.
Figure 5.
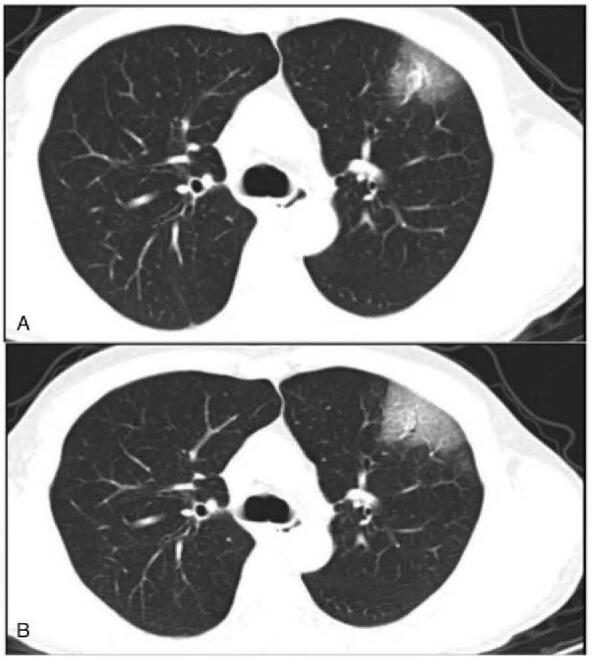
A 49-year-old man received 2 chest CT scans by the same modality within 3 days. (A) Image obtained in the first time CT scan with CTDIvol, DLP, ED were 5.16 mGy, 200.5 mGy cm, and 2.81 mSv. (B) Image obtained in the second time CT scan with CTDIvol, DLP, ED were 1.67 mGy, 68.46 mGy cm, 0.96 mSv.
4. Discussion
CT imaging plays an important role in the diagnosis and management of COVID-19, especially in the early screening of the disease as well as follow up, where throat swab tests may be false-negative due to a low viral load.[11,3] In the 7th version of COVID-19 diagnosis and treatment handbook of the People's Republic of China,[5] CT was considered a major procedure for disease detection before the RT-PCR tests,[12] and moreover COVID-19 patients should receive follow-up CT to monitor the changes of pneumonia for disease progression management during hospitalization.[13,14] In clinical, the patients with COVID-19 received 2 to 5 chest CT examinations within a month.[15] In certain an institution, the high numbers of DR on some patients were found. Due to the lack of CT in primary medical institutions, the rapid progression of COVID-19 disease, only a few of patients suffered from repeated DR examinations. Medical radiation exposure is therefore a concern, and radiation dose management for special patient population including infants, children, young individuals, and pregnant woman is particularly important.
Our survey has covered almost all hospitals that received and treated more than 95% admitted patients with COVID-19 pneumonia in Chongqing, southwest China, including 2119 chest CT imaging from 550 patients. The DLP in the designated hospitals (A, B, and C) is higher than that in the first-visited hospital, and the patients received effective dose seems higher in the designated hospitals, probably because the suspected COVID-19 patients were screened with low-dose CT in the first-visited hospital, while for the confirmed cases conventional CT were used to provide clear images of lung. The 3 major hospitals A, B, and C were the designated hospitals for receiving COVID-19. Once the patients were diagnosed with COVID-19, they will be transferred to the designated hospital for others, so this study mainly discusses the difference of dose level among different COVID-19 patients and among 3 major hospitals. The median DLP, CTDIvol, and ED measurements were 325.2 mGy cm with a range of 6.79 to 1098 mGy cm, 9.68 mGy with a range of 0.62 to 33.80 mGy, and 4.55 mSv with a range of 0.11 to 15.37 mSv for COVID-19 CT scanning protocols in Chongqing, China. The investigation indicates that the CT scanner type, chest CT protocols, and radiation doses in COVID-19 patients varied greatly within the same and between different medical institutions, and <1.13% scans reported median CTDIvol <3 mGy. Considering our results, the radiation risk of COVID-19 patients undergoing standard chest CT scans does not appear to be negligible, and therefore the recommendation of low-dose CT in the screening, diagnosis, and management of COVID-19 is necessary.
Some studies have recommended the use of single-phase, low-dose, and non-contrast chest CT protocols for COVID-19 patients.[16,17] Kang et al[15] implemented a low-dose CT scan protocol at ≤100 kV, 0.6-second exposure time and low tube current with tin filter and iterative reconstruction algorithm with a CTDIvol of 0.39 mGy (Siemens Healthcare). Homayounieh et al[18] reported almost 30% of COVID-19 patients underwent 2 to 8 chest CT examinations within a month and the variation of dose descriptors was obviously prominent in median CTDIvol and DLP. This is consistent with our findings. In Homayounieh study, CTDIvol and DLP are the median from each healthcare site, so Lee[19] considered the actual range of the dose descriptors all over the world must be considerably larger. Our study surveyed the scan protocol and dose descriptors for each patient at the individual level. Up to our knowledge, this is the first study to focus on the individual level-based investigation of medical radiation exposure, CT scan protocols, and radiation dose levels in COVID-19 patients from the medical centers of western China, while this study demonstrates that current CT dose levels are well above previously recommended values (3 mGy). These findings strongly recommend that low-dose chest CT scan protocols must be adopted, if necessary, no matter for screening the patients with suspected COVID-19 or monitoring progression and follow-up, to reduce the risk of cancer caused by high radiation doses.
The International Commission on Radiological Protection introduced the concept of diagnostic reference levels (DRLs) in 1996,[20] American College of Radiology (ACR) issued the DRL of chest CT without contrast is 12 mGy in CTDIvol in 2018,[21] and ACR suggest chest low-dose CT protocol must have a CTDIvol of ≤3 mGy.[22] Of the 2119 CT scans, the average CTDIvol was 10.57 ± 5.53 mGy where the radiation dose level may close to the DRL of Chest non-contrast CT proposed by ACR, but the average accumulate DLP and ED of the multiple scan were 1361.88 ± 663.86 mGy cm and 19.07 ± 9.26 mSv for a patient, and especially some patient received 53.39 mSv radiation within a short period of time. The total effective radiation dose greatly exceeded public limit of 1 mSv in all patients and 39.45% of them exceeded the annual dose equivalent limit, 20 mSv, of occupational exposure in a short team.[23] All the CT images we received meet the diagnostic criteria of COVID-19. Although low-dose CT impairs the diagnostic image quality, especially in the mediastinal window, COVID-19 diagnosis was mostly dependent on the lung window. Moreover, with the deep understanding of COVID-19 image features, it can still be used for auxiliary diagnosis by radiologist. The most direct and effective methods for radiation dose reduction involve decreasing the tube voltage and tube current, the use of automatic tube current modulation, iterative reconstruction, and coarse pitch scanning. To balance the relationship between image quality and dose level to meet the needs of diagnosis, chest low-dose CT scan protocol with CTDIvol <3 mGy is recommended for the follow-up considering the accumulation dose within a short term, and the interval of imaging follow-up depends on the severity degree of disease.
Reasons resulting in such phenomena are as follows: The average chest CT re-examination times is 4.0 ± 3.0, and particularly few patients received multiple chest CT examinations >10 times. So far as I know, there are no evidence about how many times and how often did patient receive chest CT examinations reasonably. Rare application of low-dose CT was found in our survey, only 1.13% CTDIvol <3 mGy. In this survey, 98.58% chest CT examinations were performed by separate 16-slice or 64-slice CT scanners for COVID-19 patients instead of high-end CT scanners (256-slice) that meet the needs of other complex examinations such as CT angiography. This helped to reduce the risk of in-hospital transmission and allowed to avoid time- and resource-consuming room decontamination procedures. Therefore, chest low-dose CT scanning protocol in the screening, diagnosis, and management of COVID-19 is highly recommended, especially in follow-up CT.
Several limitations also exist. First, our study enrolled a relatively small number of samples (550 patients from 92 institutions), and was also a retrospective survey on chest CT practices and protocols for the COVID-19 pneumonia patients in Chongqing, China, which may have generalization restrictions that do not apply to other districts. Second, the precision of the reported dose descriptors may be subject to errors, heterogeneity, and variations caused by manually recorded data from different medical institutions and CT equipments. Third, because the effective dose per DR examination cannot be counted, the cumulative dose of the high numbers of DR examinations was omitted and not compared with that of CT. The multicenter or international studies should be performed to objectively estimate the dose descriptor level in chest CT protocols for COVID-19 and optimize radiation dose management in future studies. Directly automatic acquisition of electronic dose records from PACS would be also sought to reduce manual error under investigation.
In summary, this study provides valuable information on chest CT radiation doses in COVID-19 patients. The survey results shown chest CT plays an important role in the diagnosis, progression monitoring, and treatment response of COVID-19 pneumonia in most medical institutions of Chongqing, China, while the scan protocols and radiation doses in COVID-19 patients presents wide variation across medical institutions. Although several optimization strategies on radiation dose management have already been proposed for CT protocols, there is little clinical use in COVID-19 pneumonia examination across Chongqing hospitals. For patients with known or suspected COVID-19, a chest CT should be performed on the principle of rapid-scan, low-dose, single-phase protocol instead of routine chest CT protocol to minimize radiation doses and motion artifacts.
Author contributions
Conceptualization: Lead: Fajin Lv.
Formal analysis: Equal: Xin Dai, Qihui Gong, Lead: Yineng Zheng.
Funding acquisition: Lead: Fajin Lv.
Investigation: Equal: Yun Wen, Xin Dai, Wengang Liu, Qihui Gong, Lead: Fajin Lv.
Methodology: Equal: Xin Dai, Wengang Liu, Qihui Gong.
Project administration: Lead: Fajin Lv.
Supervision: Equal: Yun Wen, Lead: Fajin Lv.
Validation: Equal: Yun Wen, Xin Dai, Wengang Liu, Lead: Fajin Lv.
Writing – original draft: Yang Zhou, Yineng Zheng, Jiahui Wu.
Writing – review & editing: Yang Zhou, Yineng Zheng, Chaoqiong Huang, Jiahui Wu.
Footnotes
Abbreviations: ACR = the American College of Radiology, COVID-19 = coronavirus disease 2019, CT = computed tomography, CTDIvol = volume computed tomography dose index, DLP = dose-length product, DR = digital radiography, DRLs = diagnostic reference levels, ED = effective dose, RT-PCR = reverse transcription-polymerase chain reaction.
How to cite this article: Zhou Y, Zheng Y, Wen Y, Dai X, Liu W, Gong Q, Huang C, Lv F, Wu J. Radiation dose levels in chest computed tomography scans of coronavirus disease 2019 pneumonia: A survey of 2119 patients in Chongqing, southwest China. Medicine. 2021;100:31(e26692).
YZ and YZ contributed equally to this work.
This study has received funding by Emergency Research Project of Chongqing Medical University (CQMUNCP0201).
Ethical approval: This study was approved by the Medical Ethical Committee of our hospital, in accordance with the provisions of the Declaration of Helsinki and its later amendments or comparable ethical standards. The written informed consent for this retrospective study was waived.
Informed consent: No additional informed consent was required for this retrospective study.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
CT = computerized tomography, DR = digital radiography.
DLPmax-min = DLPmax – DLPmin, CTDIVOLmax-min = CTDIVOLmax – CTDIVOLmin, EDmax-min = EDmax – EDmin.
CT = computerized tomography, CTDIVOL = volume computed tomography dose index, DLP = dose-length product, ED = effective dose.
Data are expressed as medians and interquartile range (25th–75th percentile in parenthesis).
CT = computerized tomography, CTDIVOL = volume computed tomography dose index, DLP = dose-length product, ED = effective dose.
P values are based on Mann–Whitney U test.
Data are expressed as medians and interquartile range (25th–75th percentile in parenthesis).
∗, #, and † represent the statistically significant difference between both groups by multiple comparison.
CT = computerized tomography, CTDIVOL = volume computed tomography dose index, DLP = dose-length product, ED = effective dose.
P values are based on Mann–Whitney U test.
References
- [1].WHO. WHO Coronavirus Disease (COVID-19) Dashboard. Available at: https://covid19.who.int/. Accessed May 28, 2020. [Google Scholar]
- [2].Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 2020;200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology 2019;2020:200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Fan L, Liu S. CT and COVID-19: Chinese experience and recommendations concerning detection, staging and follow-up. Eur Radiol 2020;30:5214–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Diagnosis and treatment protocols of COVID-19 infection (trial version 7). The National Health Commission of the People's Republic of China. Available at: http://en.nhc.gov.cn/2020-03/29/c_78469.htm. Accessed May 28, 2020. [Google Scholar]
- [6].Li Y, Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. Am J Roentgenol 2020;01–7. [DOI] [PubMed] [Google Scholar]
- [7].Xiong Y, Sun D, Liu Y, et al. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest Radiol 2020;55:332–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. Am J Roentgenol 2020;01–7. [DOI] [PubMed] [Google Scholar]
- [9].Elsevier Oxford, Valentin J. The 2007 Recommendations of the International Commission on Radiological Protection. 2007. [Google Scholar]
- [10].Deak PD, Smal Y, Kalender WA. Multisection CT protocols: sex-and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 2010;257:158–66. [DOI] [PubMed] [Google Scholar]
- [11].Guan W-j, Ni Z-y, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. MedRxiv 2020. [Google Scholar]
- [12].Li K, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Investig Radiol 2020;55:327–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Liu J, Chen T, Yang H, et al. Clinical and radiological changes of hospitalised patients with COVID-19 pneumonia from disease onset to acute exacerbation: a multicentre paired cohort study. Eur Radiol 2020;01–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wu J, Wu X, Zeng W, et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Investig Radiol 2020;55:257–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Springer, Kang Z, Li X, Zhou S. Recommendation of Low-Dose CT in the Detection and Management of COVID-19. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology department preparedness for COVID-19: radiology scientific expert panel. Radiology 2020;200988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Radiology 2020;296:172–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Homayounieh F, Holmberg O, Al Umairi R, et al. Variations in CT utilization, protocols, and radiation doses in COVID-19 pneumonia: results from 28 countries in the IAEA study. Radiology 2020;203453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Radiological Society of North America, Lee C. Managing Radiation Dose from Chest CT in COVID-19 Patients. 2020. [Google Scholar]
- [20].Anonymous. Radiological protection and safety in medicine. A report of the International Commission on Radiological Protection. Ann ICRP 1996;26:01–47. [PubMed] [Google Scholar]
- [21].Butler PF, Kanal KM. Diagnostic reference levels for adult patients in the United States. J Am Coll Radiol 2018;15:932–3. [DOI] [PubMed] [Google Scholar]
- [22].Kazerooni EA, Armstrong MR, Amorosa JK, et al. ACR CT accreditation program and the lung cancer screening program designation. J Am Coll Radiol 2015;12:38–42. [DOI] [PubMed] [Google Scholar]
- [23].Weiss W, Larsson C, McKenney C, et al. ICRP Publication 122: radiological protection in geological disposal of long-lived solid radioactive waste. Ann ICRP 2013;42:01–57. [DOI] [PubMed] [Google Scholar]