Abstract
Background:
There are still controversies between the curative effect of acupuncture combined with cupping therapy and western medicine for post-herpetic neuralgia (PHN). Our meta-analysis fully incorporates the research of acupuncture combined with cupping therapy versus Western medicine for PHN, aiming to explore the difference in the efficacy of the 2 therapies, so as to provide guidance for clinical treatment.
Methods:
We searched PubMed, Embase, Cochrane Library, CNKI, Wanfang, CQVIP, CBM, from establishment of the database to September, 2020. Include studies that are clearly defined as PHN or herpes zoster, and exclude duplicate publications; studies with no full text, incomplete information, or inability to extract data; the definition of exposure is quite different from most literature; animal experiments.
Results:
The total effective rate (relative ratio [RR] = 1.21, 95% confidence interval [CI]: 1.12–1.31) and the rate of remarkable effect (RR = 1.46, 95% CI: 1.30–1.63) of acupuncture and moxibustion combined with cupping in the treatment of PHN were significantly higher than that of conventional western medicine. The visual analogue scale score of acupuncture and moxibustion combined with cupping for PHN was significantly lower than that of conventional western medicine treatment (WMD = –1.77, 95% CI [–2.79, –0.75]). In addition, acupuncture and moxibustion combined with cupping therapy significantly reduced the occurrence of PHN compared with conventional western medicine treatment after treatment of acute herpes zoster (RR = 0.30, 95% CI: 0.20–0.45). In order to explore the differences in the efficacy and preventive effects of different types of acupuncture and cupping therapy, we have further conducted a subgroup analysis.
Conclusion:
The effect of acupuncture and moxibustion combined with cupping in the treatment of PHN is significantly higher than that of conventional western medicine, and it can significantly prevent the occurrence of PHN. Chinese medicine should be used more widely in the treatment of PHN.
Keywords: acupuncture and moxibustion, cupping, post-herpetic neuralgia, Western medicine
1. Introduction
Post-herpetic neuralgia (PHN) is caused by herpes zoster mainly due to herpes virus infection. A neuropathic pain that appears in the skin lesion area after the patient's herpes has healed.[1,2] According to relevant survey statistics, the incidence of shingles is about 10% to 19%, which is even higher for the elderly.[3] As the sequelae neuralgia usually lasts from a few months to half a year, it will seriously affect the patient's daily life and work.[4] Research also shows that 45% of patients have symptoms such as anxiety, depression, and lack of concentration.[5]
Modern medicine believes that the pathogenesis of PHN mainly includes peripheral nerve and central nerve pathogenesis.[6,7] The pathogenesis of peripheral nerves mainly includes pathological changes in peripheral nerve function caused by virus infection, abnormal discharge of damaged peripheral neurons due to abnormal conduction, and ectopic sympathetic nerves to sensory neurons causing peripheral nociceptor sensitization.[8,9] The pathogenesis of the central nervous system is the continuous excitement of the ectopic discharge of peripheral neurons after nerve injury, which stimulates the spinal cord and its upper center, as well as abnormally increased excitability of sensory neurons or enhanced synaptic transmission, which leads to the amplification of pain signals.[10] Modern medical treatment of PHN is mainly through oral drugs, physical therapy, nerve block, surgical treatment, mental and psychological intervention, etc.[11–14] Although drug therapy has a certain effect, the pain relief of patients varies greatly. In addition, western medicine treatment has large side effects, long treatment time, and drug dependence.[15] There are various methods of treating PHN with traditional Chinese medicine, such as traditional Chinese medicine, acupuncture, electroacupuncture, cupping, fire acupuncture, etc. A large number of experimental studies and clinical experience have confirmed that traditional Chinese medicine has a unique and accurate effect on PHN treatment.[16] Acupuncture stimulates acupuncture points on the patient's body surface and conducts them through the meridians throughout the body to relieve spasm and pain, promote blood circulation and remove blood stasis, and dredge the meridians. Cupping therapy can promote local microcirculation, reduce the concentration of pain-causing substances, and effectively relieve pain.[17] However, there are still controversies between the curative effect of acupuncture combined with cupping therapy and western medicine for PHN. Our meta-analysis fully incorporates the research of acupuncture combined with cupping therapy versus Western medicine for PHN, aiming to explore the difference in the efficacy of the 2 therapies, so as to provide guidance for clinical treatment.
2. Methods
2.1. Literature inclusion and exclusion criteria
The inclusion criteria were as follows: the study type is a randomized controlled study; the language is limited to Chinese and English.
Exclusion criteria: repeated publication; research without full text, incomplete information or inability to conduct data extraction; the definition of exposure is quite different from most literature; animal experiments; reviews, and systematic reviews.
2.2. Search strategy
In this meta-analysis, we searched PubMed, Embase, Cochrane Library, CNKI, Wanfang, CQVIP, CBM, from establishment of the database to September, 2020. The Chinese search terms are mainly: “herpes zoster,” “posterior neuralgia,” “fire needle,” “electroacupuncture,” “acupuncture,” “cupping,” etc. The English search terms are as follows:(((((Fire-needle[Title/Abstract]) OR (Fire needle[Title/Abstract])) OR (electroacupuncture[Title/Abstract])) OR (acupuncture[Title/Abstract])) AND (cupping[Title/Abstract])) AND (((Shingles[Title/Abstract]) OR (Neuralgia after herpes zoster[Title/Abstract])) OR (PHN[Title/Abstract])).
2.3. Literature screening and data extraction
The literature search, screening, and information extraction were all independently completed by 2 researchers. When there were doubts or disagreements, the decision was made after discussion or consultation with a third party. The data extraction included the author, year, study area, research type, number of cases and outcome indicators, including total effective rate (the percentage of the total number of patients who are effective and cured), remarkable effect rate (the percentage of cured patients in the total number of patients), VAS (Visual Analogue Scale/Score), and the incidence of PHN.
2.4. Literature quality assessment
Two researchers independently carry out the literature quality evaluation, the Cochrane collaboration's tool for assessing risk of bias in randomized controlled trials (RoB 2.0)[18] were used for assessment of risk of bias and decide through discussion or consultation with a third party when opinions are inconsistent. This meta-analysis is performed based on the related items of the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement.[19]
2.5. Data synthesis and statistical analysis
STATA 15.1 (Stata Corp, College Station, TX) was used to analyze the data. RR (relative ratio) (95% Cl) was used as the binary variable, and WMD (95% Cl) combined effect size was used as the continuous variable. I2 is used to evaluate heterogeneity. If the heterogeneity P < .1 and I2 ≤ 50%, it indicates that there is homogeneity between studies, and the fixed effects model is used for combined analysis; if P < .1, I2 > 50%, it indicates that the study. If there is heterogeneity, use sensitivity analysis or subgroup analysis to find the source of heterogeneity. If the heterogeneity is still large, use the random effects model or give up the combination of results and use descriptive analysis. Funnel plot and Egger test was used to analyze publication bias.
3. Results
3.1. The results of literature search
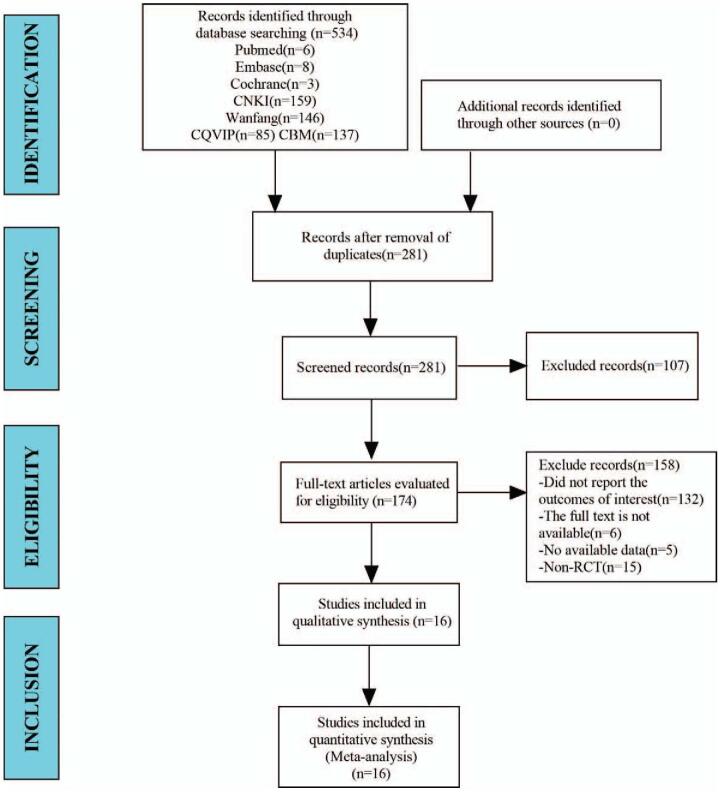
In this study, a total of 534 studies were retrieved from the database. After eliminating duplicate studies, 281 were obtained. After browsing titles and abstracts, 174 studies were obtained. Finally, 16 studies were finally meta-analyzed through full-text reading (Fig. 1).
Figure 1.
Flow diagram for selection of studies.
3.2. Baseline characteristics and quality assessment of the included studies
3.2.1. Baseline characteristics
The baseline characteristics and quality assessment of the included studies are shown in Table 1.
Table 1.
Baseline characteristics.
| Number of cases | Gender (male/female) | Age | Duration of disease (m) | ||||||||
| Study | Research type | Experimental group | Control group | Experimental group | Control group | Experimental group | Control group | Experimental group | Control group | Types of acupuncture and moxibustion | Pain assessment scale |
| Xiong 2007[20] | RCT | 48 | 40 | 20/28 | 16/24 | 50 ± 6 | 48 ± 6 | / | / | Fire needle | / |
| Jin 2009[21] | RCT | 30 | 25 | 17/13 | 12/13 | 52 | 48.5 | / | / | Acupuncture | / |
| Ma 2010[22] | RCT | 20 | 20 | 18/22 | 56.2 | 6.5 | Fire needle | / | |||
| Teng 2014[23] | RCT | 48 | 48 | 53/43 | / | / | / | / | Fire needle | / | |
| Zheng 2014[24] | RCT | 32 | 30 | 13/19 | 13/17 | 45.78 ± 15.28 | 46.30 ± 14.40 | 4.53 ± 1.74(d) | 4.60 ± 1.69(d) | Fire needle | / |
| Li 2014[25] | RCT | 30 | 30 | 17/13 | 15/15 | 61.7 | 60.2 | 9.5 | 8.3 | Electroacupuncture | / |
| Zhang 2015[26] | RCT | 36 | 36 | 22/14 | 19/17 | 62.06 ± 7.34 | 62.18 ± 7.16 | 3.51 ± 2.31 | 3.42 ± 2.55 | Fire needle | / |
| Wu 2017[27] | RCT | 39 | 39 | 18/21 | 17/22 | 59.5 | 61.5 | 1-12 | 1-12 | Fire needle | / |
| Wang 2019[28] | RCT | 39 | 39 | 20/19 | 22/17 | 58.3 ± 3.2 | 59.1 ± 2.8 | 4.2 ± 1.3 | 4.0 ± 1.4 | Fire needle | VAS |
| Tang 2019[29] | RCT | 30 | 30 | 11/19 | 13/17 | 59.5 ± 10.3 | 61.67 ± 8.2 | / | / | Acupuncture | VAS |
| Han 2020[30] | RCT | 55 | 55 | 28/27 | 29/26 | 47.22 ± 8.54 | 46.14 ± 8.62 | / | / | Fire needle | / |
| Zhang 2020[31] | RCT | 32 | 32 | 12/20 | 14/18 | 53.72 ± 15.17 | 54.25 ± 11.19 | / | / | Fire needle | / |
| Li 2010[32] | RCT | 36 | 31 | 15/11 | 12/19 | 43.67 ± 14.64 | 46.45 ± 15.27 | / | / | Electroacupuncture | / |
| Chen 2020[33] | RCT | 30 | 30 | 16/14 | 17/13 | 53.67 ± 5.19 | 55.07 ± 4.85 | 5.79 ± 1.30 | 5.38 ± 1.28 | Electroacupuncture | VAS |
| Huang 2020[34] | RCT | 45 | 45 | 24/21 | 22/23 | 65.8 ± 2.9 | 65.9 ± 2.7 | 7.8 ± 1.2 | 7.9 ± 1.5 | Electroacupuncture | VAS |
| Ming 2020[35] | RCT | 30 | 30 | 13/17 | 11/19 | 54.52 ± 4.97 | 54.32 ± 5.47 | 3.26 ± 1.08 | 2.93 ± 1.15 | Acupuncture | / |
3.2.2. Quality assessment of the included studies
The quality assessment of the included studies is shown in Table 2.
Table 2.
Methodological quality assessment of included studies.
| Study | Bias arising from the randomization process | Bias due to deviations from the intended interventions | Bias due to missing outcome data | Bias in the measurement of the outcome | Bias in the selection of the reported result | Overall bias |
| Xiong 2007[20] | Moderate | High | Low | High | Low | Moderate |
| Jin 2009[21] | Moderate | High | Low | High | Low | Moderate |
| Ma 2010[22] | Moderate | High | Low | High | Low | Moderate |
| Teng 2014[23] | Moderate | High | Low | High | Low | Moderate |
| Zheng 2014[24] | Moderate | High | Low | High | Low | Moderate |
| Li 2014[25] | Moderate | High | Low | High | Low | Moderate |
| Zhang 2015[26] | Moderate | High | Low | High | Low | Moderate |
| Wu 2017[27] | Moderate | High | Low | High | Low | Moderate |
| Wang 2019[28] | Moderate | High | Low | High | Low | Moderate |
| Tang 2019[29] | Moderate | High | Low | High | Low | Moderate |
| Han 2020[30] | Moderate | High | Low | High | Low | Moderate |
| Zhang 2020[31] | Moderate | High | Low | High | Low | Moderate |
| Li 2010[32] | Moderate | High | High | High | Low | Moderate |
| Chen 2020[33] | Moderate | High | Low | High | Low | Moderate |
| Huang 2020[34] | Moderate | High | Low | High | Low | Moderate |
| Ming 2020[35] | Moderate | High | Low | High | Low | Moderate |
3.3. Results of meta-analysis
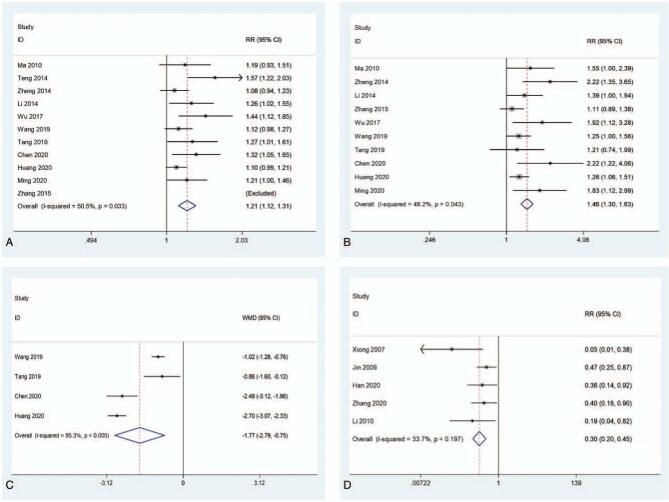
We first explored the efficacy of acupuncture and moxibustion combined with cupping therapy and conventional western medicine in the treatment of PHN, including the difference in total effective rate and the rate of remarkable effect. The results showed that the total effective rate (RR = 1.21, 95% CI: 1.12–1.31, P = .000; I2 = 50.5%, P = .033; enrolling 11 studies) and the rate of remarkable effect (RR = 1.46, 95%CI: 1.30–1.63, P = .000; I2 = 48.2%, P = .043; enrolling 10 studies) of acupuncture and moxibustion combined with cupping in the treatment of PHN were significantly higher than that of conventional western medicine (Fig. 2). In addition, we also summarized the VAS scores after acupuncture and moxibustion combined with cupping therapy and conventional western medicine for PHN. After sensitivity analysis, it was found that the study of Ma[22] had a great influence on the results. After excluding the study, it was found that the VAS score of acupuncture and moxibustion combined with cupping for PHN was significantly lower than that of conventional western medicine treatment (WMD = –1.77, 95% CI [–2.79, –0.75], P = .001; I2 = 95.3%, P = .000; enrolling 4 studies) (Fig. 2).
Figure 2.
The comparison of total effective rate (A), remarkable effect rate (B), VAS score (C), and the prevention of PHN (D) of acupuncture and moxibustion combined with cupping therapy compared with conventional western medicine therapy. VAS = Visual Analogue Scale/Score.
We further explored the difference between acupuncture and moxibustion combined with cupping therapy and conventional western medicine in the prevention of PHN. Studies have found that after acupuncture and cupping treatment of acute herpes zoster, the incidence of PHN is significantly lower than that of conventional western medicine treatment (RR = 0.30, 95% CI: 0.20–0.45, P = .000; I2 = 33.7%, P = .197; enrolling 5 studies) (Fig. 2).
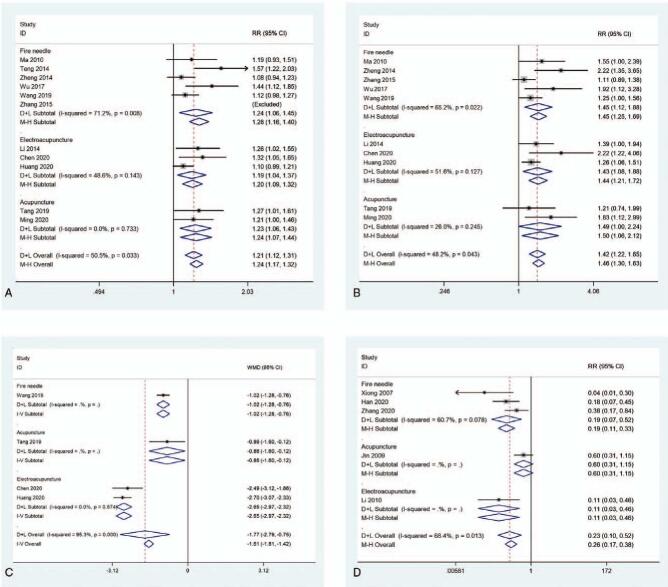
3.4. Subgroup analysis
In order to further explore the difference in efficacy between different types of acupuncture and moxibustion, we conducted a subgroup analysis based on different types of acupuncture and moxibustion. We found that the effective rate of fire-needle (RR = 1.24, 95% CI: 1.06–1.45, P = 0.008; I2 = 71.2%, P = 0.008), electroacupuncture (RR = 1.20, 95% CI: 1.09–1.32, P = .014; I2 = 48.6%, P = .143), and acupuncture (RR = 1.24, 95% CI: 1.07–1.44, P = .006; I2 = 0.0%, P = .733) combined with cupping in the treatment of PHN can be significantly increased by about 1.2 times compared with conventional western medicine treatment (Fig. 3). In the comparison of the rate of remarkable effect, the level of fire-needle (RR = 1.45, 95% CI: 1.12–1.88, P = .005; I2 = 65.2%, P = .022), electroacupuncture (RR = 1.43, 95% CI: 1.08–1.88, P = .011; I2 = 51.6%, P = .127), and acupuncture (RR = 1.50, 95% CI: 1.06–2.12, P = .000; I2 = 26%, P = .245) combined with cupping therapy is also around 1.45 times higher than that of conventional western medicine therapy (Fig. 3). However, there are differences in the VAS scores of different types of acupuncture and moxibustion combined with cupping in the treatment of PHN compared with conventional western medicine treatment. Among them, the VAS score after fire needle combined with cupping treatment for PHN is 1.02 lower than that of conventional western medicine treatment (WMD = –1.02, 95% CI [–1.28, –0.76], P = .000). The VAS score after acupuncture combined with cupping treatment for PHN is 0.86 lower than that of conventional western medicine treatment (WMD = –0.86, 95% CI [–1.60, –0.12], P = .023). However, the VAS score after electroacupuncture combined with cupping treatment for PHN has the most significant decrease (WMD = –2.65, 95% CI [–2.97, –2.32], P = .000; I2 = 0.0%, P = .574) (Fig. 3). Finally, in comparison of preventive effects, the incidence of post-herpetic neuralgia after the treatment of acute herpes zoster with electroacupuncture combined with cupping is the most significantly lower than that after conventional western medicine treatment (RR = 0.11, 95% CI: 0.03 to –0.46, P = .026). In addition, the incidence of PHN after the treatment of acute herpes zoster with fire needle combined with cupping is also significantly lower than that of conventional western medicine (RR = 0.19, 95% CI: 0.11–0.33, P = .006; I2 = 60.7%, P = .078). However, there is no significant difference between the incidence of PHN after acupuncture combined with cupping in the treatment of acute herpes zoster and traditional western medicine (RR = 0.60, 95% CI: 0.31–1.15, P = .122) (Fig. 3).
Figure 3.
The comparison of total effective rate (A), remarkable effect rate (B), VAS score (C), and the prevention of PHN (D) of different types of acupuncture and moxibustion combined with cupping therapy compared with conventional western medicine therapy. PHN = post-herpetic neuralgia, VAS = visual analogue scale/score.
3.5. Publication bias
The funnel plot drawn in this study is as follows. Based on the Egger test result of the funnel plot, P = .001 < .05, indicating that there is a certain publication bias in this study (see Figure S1, Supplemental Digital Content, Supplemental Content, which illustrates that there is a certain publication bias in this study).
3.6. Sensitivity analysis
Sensitivity analysis eliminates each included study one by one, and performs a summary analysis on the remaining studies to assess whether a single included study has an excessive impact on the results of the entire meta-analysis. The results showed that the Ma (2010) study had an excessive influence in the aggregation of VAS scores. In addition, none of the studies had an excessive impact on the results of the meta-analysis, indicating that the results of the remaining studies are stable and reliable (see Figure S2, Supplemental Digital Content–5, Supplemental Content, which illustrates that none of the studies had an excessive impact on the results of the meta-analysis).
4. Discussion
As a traditional Chinese medicine, Chinese Medicine is widely accepted by people for its advantages of small side effects, simplicity and efficiency. Western medicine believes that PHN is caused by local and skin nerve interference and is mainly treated with local or systemic drugs. However, traditional Chinese medicine believes that PHN is mainly due to incomplete heat and damp clearing in liver and spleen meridians, qi and toxic pathogens stagnation, accumulation of yin, internal fire and heat and obstruction of meridians.[36] Acupuncture is an important Traditional Chinese Medicine modality based on the fundamental theory that disease is caused by disruptions in the body's qi.[37] Cupping can eliminate stagnant qi and blood in collaterals.[38] The meta-analysis of Wang et al[39] reported that there was not enough evidence to suggest that acupuncture was superior to pharmacologic therapy in improving global impression or life quality. However, Pei et al[40] reported that acupuncture may reduce pain intensity, relieve anxiety, and improve quality of life in patients with PHN. However, there is currently no research to use evidence-based medicine to conduct meta-analysis to pooled the efficacy of acupuncture combined with cupping in the treatment of PHN. Therefore, in this meta-analysis, we summarized 16 articles and included 1140 patients, analyzed the efficacy of acupuncture and moxibustion combined cupping compared with conventional Western medicine in the treatment of PHN, and summarized the preventive effect of acupuncture and moxibustion combined cupping compared with Western medicine on PHN.
Our summary results found that the total effective rate (RR = 1.21, 95% CI: 1.12–1.31) and the rate of remarkable effect (RR = 1.46, 95% CI: 1.30–1.63) of acupuncture and moxibustion combined with cupping in the treatment of PHN were higher than those of conventional Western medicine. We also found that the VAS score of acupuncture and moxibustion combined with cupping for PHN was significantly lower than that of conventional western medicine treatment. The mechanism of acupuncture and moxibustion combined with cupping in the treatment of PHN may be to regulate the function of local blood vessels and muscles by stimulating local nerves, reducing the symptoms of local smooth muscle spasm, and then exerting a good analgesic effect.[41] In the meta-analysis of Pei et al,[40] it has been found that acupuncture can significantly relieve PHN. Our research further supports the application of Chinese medicine in the treatment of PHN.
In addition, we further explored the preventive effect of acupuncture and moxibustion combined with cupping therapy on PHN, and found that the incidence of PHN after acupuncture and moxibustion combined with cupping treatment of acute herpes zoster was significantly lower than that of conventional western medicine (RR = 0.30, 95% CI: 0.20–0.45, P = .000). The reason may be that after acupuncture and moxibustion combined with cupping treatment of acute herpes zoster, the serum substance P level decreased.[42] Substance P can induce the accumulation of pain-causing and inflammatory substances, forming neurogenic inflammation, leading to persistent or worsening pain.[43] This result further confirms the feasibility of acupuncture and moxibustion combined cupping therapy in the treatment of PHN.
We also conducted a subgroup analysis according to the different types of acupuncture and moxibustion. The pooled results show that electro-acupuncture is the most effective type of and moxibustion in the treatment of PHN, but the best preventive effect is fire needle. These findings can provide more accurate guidance for the treatment of PHN.
In addition, the included studies have few descriptions of adverse reactions and cannot reflect the differences in the safety of the 2 treatments. Therefore, further large-scale clinical trials are needed to explore the advantages and disadvantages of the 2 treatments in terms of safety issues.
There are some limitations to this meta. First, since the included studies did not use blinding and allocation concealment, this may lead to performance and selection bias. Secondly, this meta has moderate heterogeneity, and the VAS score has reached a high degree of heterogeneity, which may be caused by differences in the operation of treatment methods for different groups of people. In future analysis, some large randomized controlled trials are needed to further verify our aggregate results.
5. Conclusion
The effect of acupuncture and moxibustion combined with cupping in the treatment of PHN is significantly higher than that of conventional western medicine, and it can significantly prevent the occurrence of PHN. Chinese medicine should be used more widely in the treatment of PHN.
Author contributions
Data curation: Shenyu Wei, Haijia Zhu, Yue Hu, Yong Liu, Huifeng Yang, Shicheng Zeng, Shiqian Chai, Jingyuan Li.
Writing – original draft: Qiujun Zhou.
Writing – review & editing: Maocan Tao.
Supplementary Material
Footnotes
Abbreviations: PHN = post-herpetic neuralgia, RR = relative ratio, VAS = visual analogue scale/score.
How to cite this article: Zhou Q, Wei S, Zhu H, Hu Y, Liu Y, Yang H, Zeng S, Chai S, Li J, Tao M. Acupuncture and moxibustion combined with cupping for the treatment of post-herpetic neuralgia: a meta-analysis. Medicine. 2021;100:31(e26785).
Ethics approval and consent to participate: The research does not involve patients, so ethical approval was not necessary.
Availability of data and materials: The datasets are available from the corresponding author on reasonable request.
Consent for publication: Not applicable.
Funds for the construction of key specialties of Dermatology under the State Administration of Traditional Chinese Medicine (2A61498).
The authors declare that they have no competing interests.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
References
- [1].Gruver C, Guthmiller KB. Postherpetic Neuralgia. 2020 Oct 15. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. [PubMed] [Google Scholar]
- [2].Thompson RR, Kong CL, Porco TC, Kim E, Ebert CD, Acharya NR. Herpes Zoster and Post-Herpetic Neuralgia: changing incidence rates from 1994 to 2018 in the United States. Clin Infect Dis 2020;ciaa1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hoshi SL, Seposo X, Shono A, Okubo I, Kondo M. Cost-effectiveness of Recombinant Zoster Vaccine (RZV) and Varicella Vaccine Live (VVL) against herpes zoster and post-herpetic neuralgia among adults aged 65 and over in Japan. Vaccine 2019;37:3588–97. [DOI] [PubMed] [Google Scholar]
- [4].Matthews I, Duong M, Parsons VL, et al. Burden of disease from shingles and post-herpetic neuralgia in the over 80 year olds in the UK. PLoS One 2020;15:e0229224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Weinke T, Glogger A, Bertrand I, Lukas K. The societal impact of herpes zoster and postherpetic neuralgia on patients, life partners, and children of patients in Germany. ScientificWorldJournal 2014;2014:08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Billet B, Wynendaele R, Vanquathem NE. A novel minimally invasive wireless technology for neuromodulation via percutaneous intercostal nerve stimulation for post-herpetic neuralgia: a case report with short-term follow-up. Pain Pract 2018;18:374–9. [DOI] [PubMed] [Google Scholar]
- [7].Wong CS, Shen TT, Liaw WJ, Cherng CH, Ho ST. Epidural coadministration of ketamine, morphine and bupivacaine attenuates post-herpetic neuralgia--a case report. Acta Anaesthesiol Sin 1996;34:151–5. [PubMed] [Google Scholar]
- [8].Slavin KV. Peripheral nerve stimulation for neuropathic pain. Neurotherapeutics 2008;5:100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Deogaonkar M, Slavin KV. Peripheral nerve/field stimulation for neuropathic pain. Neurosurg Clin N Am 2014;25:01–10. [DOI] [PubMed] [Google Scholar]
- [10].Bader MS. Herpes zoster: diagnostic, therapeutic, and preventive approaches. Postgrad Med 2013;125:78–91. [DOI] [PubMed] [Google Scholar]
- [11].Owada H, Sumitani M, Inoue R, et al. Peripheral nerve field stimulation successfully manages axial pain after posterior cervical spine surgery: case report. Ann Palliat Med 2020;10:5792–6. [DOI] [PubMed] [Google Scholar]
- [12].Aydin T, Balaban O, Ahiskalioglu A, Alici HA, Acar A. Ultrasound-guided erector spinae plane block for the management of herpes zoster pain: observational study. Cureus 2019;11:e5891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sharif S, Aslam F, Faisal LR, Saleem MA. Comparison of efficacy of two different doses of famciclovir in the prevention and treatment of postherpetic neuralgia. J Ayub Med Coll Abbottabad 2019;31: suppl: S668–71. [PubMed] [Google Scholar]
- [14].Haythornthwaite JA, Clark MR, Pappagallo M, Raja SN. Pain coping strategies play a role in the persistence of pain in post-herpetic neuralgia. Pain 2003;106:453–60. [DOI] [PubMed] [Google Scholar]
- [15].Koshy E, Mengting L, Kumar H, Jianbo W. Epidemiology, treatment and prevention of herpes zoster: a comprehensive review. Indian J Dermatol Venereol Leprol 2018;84:251–62. [DOI] [PubMed] [Google Scholar]
- [16].Wang L, Fang YF, Li QJ, Li JW, Li WL. Effect of pricking and cupping on serum substance P and IL-6 in patients with postherpetic neuralgia. Chin Med Mod Dis Educ China (Chin) 2020;18:92–4. [Google Scholar]
- [17].Lu L. Study on the effect of traditional Chinese acupuncture in the treatment of postherpetic neuralgia. Chin Commun Phys (Chin) 2020;36:116–8. [Google Scholar]
- [18].Yang ZR, Sun F, Zhan SY. [Risk on bias assessment: (2) Revised Cochrane risk of bias tool for individually randomized, parallel group trials (RoB2.0)]. Zhonghua Liu Xing Bing Xue Za Zhi 2017;38:1285–91. Chinese. [DOI] [PubMed] [Google Scholar]
- [19].McKeown S. PRISMA guideline compliance is imperative for systematic review appraisal. Can J Kidney Health Dis 2020;7:2054358120927594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Xiong ZL, Zhang GH. 48 cases of acute herpes zoster treated with fire needle combined with cupping. J Acupunct Moxibust (Chin) 2007;23:38–9. [Google Scholar]
- [21].Jin YW. Clinical observation on 30 cases of herpes zoster treated by acupuncture and cupping. Beijing Trad Chin Med (Chin) 2009;28:369–70. [Google Scholar]
- [22].Ma XP, Li JC, Jiang Y. Curative effect observation on the treatment of neuralgia after herpes zoster with fire-needling combined with dialing and filiform needles. Chin Emerg Med (Chin) 2010;19:1864–6. [Google Scholar]
- [23].Teng XH, Chen HJ. Observation on the efficacy of fire needle combined with cupping in the treatment of herpes zoster. Mod J Integr Trad Chin Western Med (Chin) 2014;23:2338–40. [Google Scholar]
- [24].Zheng GX. Early use of fire needle combined with cupping therapy to prevent neuralgia after herpes zoster. Chengdu Univ Trad Chin Med (Chin) 2014. [Google Scholar]
- [25].Li WN, Cai GL, Wang YZ. Clinical observation of electroacupuncture at Jiaji points combined with puncturing and cupping on 30 cases of postherpetic neuralgia. Mod Diagn Treat 2014;25:1506–7. [Google Scholar]
- [26].Zhang YM, Peng YX, He NS. Clinical observation on the treatment of postherpetic neuralgia (blood stasis) with fire needling combined with pricking and cupping. Sichuan Trad Chin Med (Chin) 2015;33:165–7. [Google Scholar]
- [27].Wu AP. Fire needle cupping combined with oral administration of traditional Chinese medicine for the treatment of postherpetic neuralgia. Chin Folk Remed (Chin) 2017;25:57–8. [Google Scholar]
- [28].Wang N, Zeng SH, Yu MH, Xu HD. Clinical observation on 39 cases of postherpetic neuralgia treated with fire needle combined with puncturing and cupping. Hunan J Trad Chin Med (Chin) 2019;35:73–4. [Google Scholar]
- [29].Tang Q, Wang L, Zhao ZC, Gao L, Fu LN, Cheng G. Silver needle combined with blood puncturing and cupping in the treatment of 30 cases of herpes zoster pain. J Shaanxi Univ Trad Chin Med (Chin) 2019;42:100–2. 106. [Google Scholar]
- [30].Han Y, Qian YJ. Fire needle combined with cupping treatment of patients with herpes zoster shortening the treatment time and reducing the incidence of sequelae neuralgia. Med Diet Health (Chin) 2020;18:36–8. [Google Scholar]
- [31].Zhang LX, Lai YT, Chen TT, Xie SR. Clinical observation of fire needle combined with cupping in the treatment of acute herpes zoster. Guangming Chin Med (Chin) 2020;35:1869–71. [Google Scholar]
- [32].Li Q. Clinical study of electroacupuncture plus tapping and cupping therapy in the treatment of acute herpes zoster. Guangzhou Univ Chin Med (Chin) 2010. [Google Scholar]
- [33].Chen TT. Clinical study of electroacupuncture at Jiaji combined with pricking and cupping in the treatment of neuralgia after herpes zoster. Hubei Univ Trad Chin Med (Chin) 2020. [Google Scholar]
- [34].Huang AP, Gu Z, Xue CC, Xie L. Evaluation of the clinical efficacy of electroacupuncture combined with pricking and cupping in the treatment of postherpetic neuralgia. Chin Gen Pract (Chin) 2020;18:835–8. [Google Scholar]
- [35].Ming XH. Clinical observation on the treatment of post-herpetic neuralgia (qi stagnation and blood stasis type) with plum-blossom needle and cupping method. Hubei Univ Trad Chin Med (Chin) 2020. [Google Scholar]
- [36].Avijgan M, Hajzargarbashi ST, Kamran A, Avijgan M. Postherpetic neuralgia: practical experiences return to traditional chinese medicine. J Acupunct Meridian Stud 2017;10:157–64. [DOI] [PubMed] [Google Scholar]
- [37].Hwang J, Lio PA. Acupuncture in dermatology: an update to a systematic review. J Altern Complement Med 2020;27:12–23. [DOI] [PubMed] [Google Scholar]
- [38].Cui S, Cui J. [Progress of researches on the mechanism of cupping therapy]. Zhen Ci Yan Jiu 2012;37:506–10. [PubMed] [Google Scholar]
- [39].Wang Y, Li W, Peng W, Zhou J, Liu Z. Acupuncture for postherpetic neuralgia: systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e11986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Pei W, Zeng J, Lu L, Lin G, Ruan J. Is acupuncture an effective postherpetic neuralgia treatment? A systematic review and meta-analysis. J Pain Res 2019;12:2155–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Zhang Y, Liang Z, Li S, et al. Fire needle plus cupping for acute herpes zoster: study protocol for a randomized controlled trial. Trials 2020;21:701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Zhang Y, Li SH, Yang L, et al. [Shallow fire-needle acupuncture stimulation plus cupping relieves neuralgia and down-regulates serum substance p level in patients with acute herpes zoster]. Zhen Ci Yan Jiu 2018;43:492–4. [DOI] [PubMed] [Google Scholar]
- [43].Song XX, Jin LY, Li XF, Luo Y, Yu BW. Substance P mediates estrogen modulation proinflammatory cytokines release in intervertebral disc. Inflammation 2020;44:506–17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.