Abstract
Hypertension is the leading cause of increased morbidity and mortality rates worldwide. Despite adherence to therapies is the important determinant of treatment success to reduce apparent resistant hypertension, maintaining good adherence to antihypertensive medications remained the most serious challenge. Thus, this study aimed to assess adherence to antihypertensive medications among adult hypertensive patients in Dessie Referral Hospital.
A cross-sectional study design was conducted among hypertensive patients during May and June 2020. The study participants were selected using a systematic random sampling technique. The collected data were entered into EpiData version 4.4 and exported to SPSS version 25.0 software for data cleaning and analysis. Data were analyzed using bivariable and multivariable logistic regression at a 95% confidence interval (CI). A variable that has a P-value < .05 was declared as statistically significant. Hosmer–Lemeshow test was used to test goodness-of-fit and multicollinearity was tested.
The overall good adherence to antihypertensive medications was 51.9%; 95% CI: (46.8–58.3%) and poor adherence was 48.1%. Factors associated with good adherence were: sex—female adjusted odd ratio (AOR) = 1.31; 95% CI (1.06–2.52), occupational status-employed AOR = 2.24; 95% CI (1.33–3.72), good knowledge of the disease AOR = 2.20; 95% CI (1.34–3.72) and good self-efficacy AOR = 1.38; 95% CI (1.20–2.13).
This study revealed that almost half of the hypertensive patients in Dessie Referral Hospital had good antihypertensive medication adherence. Sex, occupational status, knowledge, and self-efficacy were factors associated with good adherence. Therefore, health education should be given to patients on the importance of complying with medication and patients should be monitored by health extension workers.
Keywords: adherence, antihypertensive medications, hypertension, Morisky scale
1. Introduction
Hypertension (HTN) is a non-communicable global public health threat that afflicts approximately 1.13 billion people worldwide with upwards of 1 in 4 men and 1 in 5 women and an estimated 10.3 million deaths and 208 million disabilities.[1] The prevalence of hypertension varies across the world and country. Africa has the highest prevalence of hypertension (27%) while the Americas has the lowest prevalence of hypertension (18%).[2] The prevalence increment was seen largely in low- and middle-income countries, two-thirds of those with hypertension are in economically developing countries.[3] In Ethiopia the prevalence of hypertension was 19.6%.[4]
Hypertension doubles the risk of cardiovascular diseases such as coronary heart disease,[5] congestive heart failure (CHF), stroke, renal failure, and peripheral arterial diseases.[6] Many countries have not implemented effective public policies to prevent and control hypertension.[1,3] Hypertension treatment and control rates were 10%, and 1% respectively.[7] Although adherence to therapies is a primary determinant of treatment success, approximately only one-half of hypertensive patients adhere to prescribed medications to control high blood pressure.[8] Rapid urbanization and transition from agrarian life to the wage-earning economy of city life continue to fuel increases in average blood pressure levels and prevalence of HTN.[7]
The worldwide burden of hypertension is attributed to morbidity, premature death, and cost to society and make preventing and treating hypertension is a public health challenge.[9] Poor medication adherence can cause negative health outcomes such as worsening disease or even death or the impact can be both personal and economic, as a result of increased demands for healthcare resources if there is deterioration in patients’ health.[10] Many factors can affect adherence to medications to control HTN such as social support, knowledge, attitude, behavioral factors, and sociodemographic characteristics. Therefore, attention to these barriers is necessary, and to improve adherence follow the most important strategies like patient education on hypertension, its treatment modalities, and its long-term complications; and patient engagement building on the foundation of education.[11,12]
Good adherence to hypertension medication is a decisive and collective action which saves millions of hypertensive patients’ life. Failure to adhere to medications puts hypertensive patients at risk for further complications and death. The prevalence of HTN has been widely reported[13–15] but adherence to hypertension medication has not been adequately described particularly in the study area. Therefore, this study was designed to assess adherence to antihypertensive medications among adult hypertensive patients attending chronic follow-up units of Dessie Referral Hospital (DRH), Northeastern Ethiopia.
2. Methods and materials
2.1. Study area
The study was carried out in DRH that is under South Wollo Zone. South Wollo Zone is one of the 13 zones found in Amhara regional state, Ethiopia. Its major city administration is Dessie town located 401 km away from Addis Ababa, the capital city of Ethiopia, and 480 km from Bahir Dar, the capital city of Amhara regional state. DRH is the only Referral Hospital in South Wollo zone province serving about 7 million people including the neighboring regions.
2.2. Study design, period, and population
An institution-based cross-sectional study was conducted during May and June 2020 among adult hypertensive patients attending chronic follow-up units of DRH. The source populations were all hypertensive patients who were on antihypertensive therapy and attending chronic follow-up units of DRH. The study populations were all registered adult hypertensive patients who fulfilled the inclusion criteria and were available during the time of data collection. All hypertensive patients who were 18 years and older and on anti-hypertensive treatment at least for 6 months before the commencement of the study were included.
2.3. Sample size determination and sampling techniques
The sample size was determined using single population proportion formula with the assumptions of expected proportion of adherence to hypertension medication 67%,[16]Zα/2 value at 95% confidence interval (CI) was 1.96 and 5% margin of error. After considered a 10% non-response rate from the calculated sample size of 340, the final sample size was 374. Study participants were selected using a systematic sampling technique with a sampling interval of 3 by considering the 1st comers as starting point till the sample size was saturated at exit time.
2.4. Outcome variable measurement
The outcome variable of this study was good or poor adherence to medications among hypertensive patients. The level of medication adherence among hypertensive patients was measured using the four-item Morisky Medication Adherence Scale (MMAS-4).[17] Good adherence was determined when those study participants scored 0 on the Morisky 4 item self-reported medication adherence scale whereas poor adherence refers to those study participants who scored ≥1 on the MMAS-4 scale.
2.5. Operational definitions
Adherence: The extent to which a persons’ behavior corresponds with recommendations from health care providers.
Comorbidities: respondents with one or more medical conditions in addition to HTN. Knowledge about hypertension: respondents with scores above the mean value on hypertension evaluation of lifestyle and management scale were taken as having good knowledge about hypertension.
Social support: is the support gained from family and non-family members. In this study, respondents whose score was above the mean value on the Duke social support and stress scale were taken as having social support.
Self-efficacy is the belief in one's capabilities to organize and execute the courses of action required to produce given attainment. In this study, respondents who scored above the mean value on the 6 items chronic disease self-efficacy scale were considered as having good self-efficacy to cope up and manage their disease.
2.6. Data collection and quality control
Data were collected using a face to face interviewer-administered questionnaire. The questionnaire was adapted from different reviewed literatures.[18–21] Primarily the questions were prepared in English and translated to Amharic, which is a local language, and then retranslated back to English by bilingual experts to ensure its consistency.
Two data collectors and 1 supervisor who were Bachelor of Science nurses were recruited. All data collectors and supervisor had previous experience in data collection. The training was given to data collectors and supervisor for 1 day about data collection, how to fill the information on a structured questionnaire, the ethical aspect in approaching the participants as well as the aim of the study and contents of the instruments. Data collectors approached the participants politely and respectfully at the time of the interview. The supervisor monitored the data collection process of the data collectors daily and if a problem happened they tried to solve it or contact the principal investigator by mobile or physically. Principal investigator and supervisor made daily on spot-checking for completeness of the questionnaire.
To assure the data quality, the questionnaire was pretested in 10% of the selected hypertensive patients at Kemissie Hospital which was not included in the study to assess the content, approach of the questionnaire and to amend unclear and vague issues on the questionnaire. Each questionnaire was checked for completeness, missed values, and unlikely responses; that incomplete questionnaire and checklist were omitted from the analysis.
2.7. Data management and analysis
The collected data were coded and entered into EpiData version 4.4 and exported to Statistical Package for Social Sciences (SPSS) version 25.0 for data cleaning and analysis. Mean with standard deviation were reported for continuous variables and categorical variables proportion were reported. Data were analyzed using a binary logistic regression model at 95% CI and variables with P-value < .25 during the bivariable analysis were entered into a multivariable logistic regression analysis to see the relative effect of confounding variables and interaction of variables. Adjusted odd ratio (AOR) with 95% CI was performed to determine the strength of association of variables with a P-value <.05 was declared as statistically significant. The Hosmer–Lemeshow goodness-of-fit statistic was used to assess whether the necessary assumptions for the application of multiple logistic regression were fulfilled. Multicollinearity was tested using the variance inflation factor (VIF) and tolerance test.
3. Results
3.1. Socio-demographic characteristics of participants
Among the total study participants, 366 were included in the study and 8 participants were refused to participate, yielding a response rate of 97.9%. The mean (±SD) age of participants was 51 ± 17.3 years while the majority of the respondents (40.1%) had the age of >55 years. Most study participants were women 244 (66.7%) (Table 1).
Table 1.
Sociodemographic characteristics of respondents in Dessie Referral Hospital, Northeast Ethiopia, 2020 (n = 366).
| Variables | Category | Frequency (n = 366) | Percentage (100%) |
| Age | 18–35 | 79 | 21.6 |
| 36–45 | 84 | 23.0 | |
| 46–55 | 56 | 15.3 | |
| >55 | 147 | 40.1 | |
| Sex | Male | 122 | 33.3 |
| Female | 244 | 66.7 | |
| Residence | Urban | 220 | 60.1 |
| Rural | 146 | 39.9 | |
| Religion | Orthodox | 99 | 27.0 |
| Muslim | 194 | 53.0 | |
| Protestant | 38 | 10.4 | |
| Catholic | 35 | 9.6 | |
| Ethnicity | Amhara | 326 | 89.1 |
| Oromo | 14 | 3.8 | |
| Tigre | 26 | 7.1 | |
| Marital status | Single | 165 | 45.1 |
| Married | 201 | 54.9 | |
| Educational status | Illiterate | 77 | 21.0 |
| Informal education | 53 | 14.5 | |
| Primary school | 83 | 22.7 | |
| Secondary school | 42 | 11.5 | |
| College and above | 111 | 30.3 | |
| Occupational status | Farmer | 75 | 20.5 |
| Governmental employee | 47 | 12.8 | |
| Private employee | 63 | 17.2 | |
| Private business | 61 | 16.7 | |
| Non-employed | 14 | 3.8 | |
| Laborer | 60 | 16.4 | |
| Retired | 46 | 12.6 | |
| Monthly income (USD [United States Dollars], $)∗ | No regular income | 77 | 21.0 |
| <30 | 41 | 11.2 | |
| 30–58 ETB | 119 | 32.5 | |
| 58.1–88 | 74 | 20.3 | |
| >88 | 55 | 15.0 |
3.2. Adherence to anti-hypertensive medications
Out of the total study participants, 138 (37.7%) of them missed their medication due to forgetfulness. Only 16.4% of respondents were careless about taking antihypertensive medications (Table 2). Out of the total 366 participants, 51.9% (n = 190; 95% CI [46.8–58.3%]) were adherent to the medication regimen whereas the remaining were not (Fig. 1).
Table 2.
Frequency and percentage distribution of adherence to antihypertensive medications among hypertensive patients in Dessie Referral Hospital Chronic Follow up Unit, Northeast Ethiopia, 2020 (n = 366).
| Variables | Category | Frequency (n = 366) | Percentage (100%) |
| Ever forget to take AHTN medicine | Yes | 138 | 37.7 |
| No | 228 | 62.3 | |
| Being careless at times about taking AHTN medicine | Yes | 60 | 16.4 |
| No | 306 | 83.6 | |
| Sometimes stopping to take AHTN medicine if feel worse when taking it | Yes | 85 | 23.2 |
| No | 281 | 76.8 | |
| Sometimes stopping to take AHTN medicine if feel better | Yes | 72 | 19.7 |
| No | 294 | 80.3 | |
Figure 1.
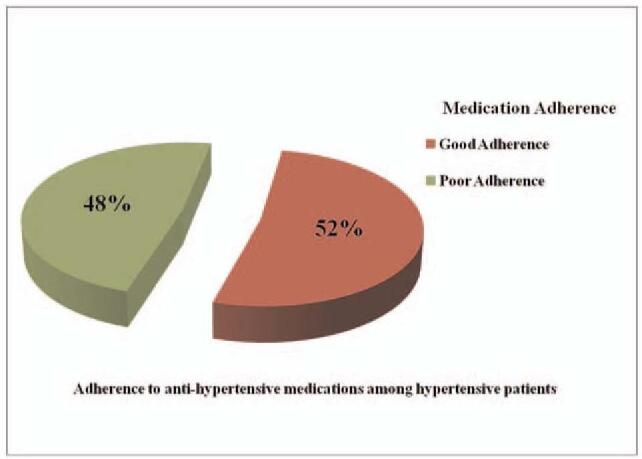
Graphic representation of medication adherence among hypertensive patients attending chronic follow up units of Dessie Referral Hospital, Northeast Ethiopia, 2020.
3.3. Bivariable and multivariable analysis
The bivariable analysis showed significant associations between antihypertensive medication adherence and sex, residence, marital status, occupational status, number of medications type, presence of morbidities, knowledge, and self-efficacy.
In multivariable logistic regression analysis sex, occupational status, knowledge of the disease, and self-efficacy kept their significant association with anti-hypertensive medication adherence. Therefore multivariable analysis model revealed that female hypertensive patients were 1.3 times more likely to adhere to anti-hypertensive medications than male patients (AOR = 1.31; 95% CI [1.06–2.52]). Similarly, those employed hypertensive patients were almost 2 times more likely to had good anti-hypertensive medication adherence than those unemployed (AOR = 2.24; 95% CI [1.33–3.72]). The odds of adherence were 2 times more likely to occur on those who had good knowledge about hypertension as compared with the counterpart (AOR = 2.20, 95% CI [1.34–3.72]). Hypertensive patients who had good self-efficacy were 1.4 times more likely to be adherent than those who had poor self-efficacy (AOR = 1.38, 95% CI [1.20–2.13]) (Table 3).
Table 3.
Factors associated with medication adherence among hypertensive patients attending chronic follow up units of Dessie Referral Hospital, Northeast Ethiopia, 2020 (n = 366).
| Medication adherence | |||||
| Variables | Adherent (n = 190) | Non-adherent (n = 176) | COR (95% CI) | AOR (95% CI) | |
| Sex | Male | 62 (50.8) | 60 (49.2) | 1.00 | 1.00 |
| Female | 114 (46.7) | 130 (53.3) | 1.18 (0.76–2.34)∗ | 1.31 (1.06–2.52)∗∗ | |
| Residence | Urban | 116 | 104 | 1.09 (0.71–1.65)∗ | |
| Rural | 74 | 72 | 1.00 | ||
| Marital status | Single | 73 (44.2) | 92 (55.8) | 1.00 | 1.00 |
| Married | 117 (58.2) | 84 (41.8) | 1.76 (1.16–2.66)∗ | ||
| Occupational status | Employed | 100 (54.9) | 82 (45.1) | 1.27 (0.85–1.92)∗ | 2.24 (1.33–3.72)∗∗ |
| Unemployed | 90 (48.9) | 94 (51.1) | 1.00 | 1.00 | |
| Presence of comorbidities | Yes | 108 (49.1) | 112 (50.9) | 1.00 | |
| No | 82 (56.2) | 64 (43.8) | 1.33 (0.87–2.02)∗ | ||
| Number of medications type | ≤3 | 157 (57.3) | 117 (42.7) | 2.40 (1.47–3.91)∗ | |
| >3 | 33 (35.9) | 59 (64.1) | 1.00 | 1.00 | |
| Knowledge level | Good | 128 (61.5) | 80 (38.5) | 2.48 (1.62–3.79)∗ | 2.20 (1.34–3.72)∗∗ |
| Poor | 62 (39.2) | 96 (60.8) | 1.00 | 1.00 | |
| Self-efficacy | Good efficacy | 113 (56.5) | 87 (43.5) | 1.50 (0.99–2.27)∗ | 1.38 (1.20–2.13)∗∗ |
| Poor efficacy | 77 (46.4%) | 89 (53.6) | 1.00 | 1.00 | |
4. Discussion
Out of 366 patients, 66.7% of them were women. Regarding anti-hypertensive medications, 62.3% of patients missed their medication due to forgetfulness. We found that sex, occupational status, knowledge of the disease, and self-efficacy had a statistically significant association with antihypertensive medication adherence among adult hypertensive patients.
The overall rate of good adherence to antihypertensive medications as measured using MMAS-4 in DRH was 51.9% (n = 190; 95% CI [46.8–58.3%]). The finding of this study was comparable with studies conducted in India 57.2%,[22] China 52.0%,[23] Jordan 56%,[24] and Eastern Nigeria 52.5%.[11] Perhaps this might be due to methodological similarity and use of a similar tool.
This adherence level was lower than studies conducted in China 65.1%,[25] Canada 77.0%,[26] Southwest Ethiopia 67.2%,[27] and Jimma University Specialized Hospital 61.8%.[28] The inconsistency might be due to the differences in the study population, sample size, method of measurement, cultural and health perception on hypertension.
On the other hand, the current study finding was surprisingly higher than studies conducted in Korea 39.2%,[29] Italy 41.5%,[30] and Nedjo General Hospital in West Ethiopia 31.4%.[31] The possible reasons for this discrepancy might include the difference in time of the study, sample size, and socio-cultural difference of study participants.
This study identified factors significantly associated with antihypertensive medication adherence. Female patients were more likely to be adherent to antihypertensive medications than male patients. This finding was supported by studies conducted in Jordan,[24] Romania,[32] Addis Ababa,[33] and Gondar.[34] This can be explained by the fact that naturally women are careful and follow their prescriptions better. It might be due to that men are responsible mostly for outdoor activities which lead them not to access their medication easily and even the outside duty make them forget medications. And also men might tend to discontinue their medication due to alcohol and khat consumption than women.
The occupational status of hypertensive patients was associated with medication adherence; those employed hypertensive patients were more likely to have good antihypertensive medication adherence than unemployed. This was consistent with studies in China,[25] Jordan,[24] and Addis Ababa.[35] The possible explanation might be that employed patients had increased social support, better structuring of time, and improved psychosocial or mental well-being to adhere to their medications. It might also be due to that employed patients’ increased material well-being, for example, improved food security and housing quality and reduced poverty to access medical service.
The likely hood of having good antihypertensive medication adherence for hypertensive patients with good knowledge of the disease was high as compared with those with poor knowledge. This result was supported by studies in Malaysia,[8] Hawassa,[16] Gondar,[34] and Debre Tabor.[36] This was possibly explained as knowledgeable patients might have a good understanding and awareness of the severity of hypertension if the medications are not taken as health care professionals prescribed.
This study revealed that those hypertensive patients who had good self-efficacy were more likely to be adherent to antihypertensive medications. This finding was supported by studies in China[25] and Charlotte, NC metropolitan.[37] The possible explanation might be having good self-efficacy encouraged good self-control and positive beliefs about hypertension which increases adherence to antihypertensive medication regimes.
5. Strength and limitations of the study
5.1. Strength
The tools used for the measurement of antihypertensive medication adherence, knowledge, social support, and self-efficacy assessment are internationally tested. It had a representative sample and a good response rate. The study participants were adequately informed about the relevance of this study and the importance of telling the truth. Additionally, the data collectors employed were working out of the chronic illness clinics. There were sufficient references to discuss the results in a situation from international to local.
5.2. Limitations
This study used self-reporting as the only method of measuring adherence which could result in overestimation of adherence since this method has the disadvantages of recall bias and eliciting only socially acceptable responses. In addition, this study did not consider hypertensive patients who did not visit health facilities during the data collection period and who had follow-up in private health facilities. Hence, it might be difficult to generalize the findings to the general population.
6. Conclusion
This study revealed that almost half of the hypertensive patients in DRH had good antihypertensive medication adherence. Sex, occupational status, knowledge of the disease, and self-efficacy were factors associated with good antihypertensive medication adherence. Based on the findings of this study nurses/doctors should give health education to patients at every clinic visit on the importance of complying with medication, patients should be educated that antihypertensive drugs are for life use, hypertensive patients should be monitored by health extension workers, strategies should be on the possibilities of giving antihypertensive drugs free of charge and in every health sectors.
Acknowledgments
The authors would like to extend their special thanks to data collectors, the supervisor, and the study participants for their valuable contribution to the study. The last but not the least they also thank Lisa Penttila for language editing of the manuscript.
Author contributions
Conceptualization: Atsedemariam Andualem.
Data curation: Atsedemariam Andualem.
Formal analysis: Atsedemariam Andualem.
Funding acquisition: Atsedemariam Andualem.
Investigation: Atsedemariam Andualem.
Methodology: Atsedemariam Andualem.
Project administration: Atsedemariam Andualem.
Resources: Atsedemariam Andualem.
Software: Atsedemariam Andualem.
Supervision: Atsedemariam Andualem, Tiliksew Liknaw, Afework Edmealem.
Validation: Atsedemariam Andualem, Tiliksew Liknaw, Afework Edmealem, Mihrete Gedefaw.
Visualization: Atsedemariam Andualem, Tiliksew Liknaw, Afework Edmealem.
Writing – original draft: Atsedemariam Andualem, Mihrete Gedefaw.
Writing – review & editing: Atsedemariam Andualem, Tiliksew Liknaw, Afework Edmealem, Mihrete Gedefaw.
Footnotes
Abbreviations: DRH = Dessie Referral Hospital, HTN = hypertension, MMAS-4 = four items; Morisky Medication Adherence Scale.
How to cite this article: Andualem A, Liknaw T, Edmealem A, Gedefaw M. Adherence to antihypertensive medications among adult hypertensive patients attending chronic follow-up units of Dessie Referral Hospital, Northeastern Ethiopia: a cross-sectional study. Medicine. 2021;100:31(e26818).
Data Availability: The datasets generated or analyzed during this study are available from the corresponding author but will be shared for only reasonable request to protect participants’ anonymity.
Ethics and consent to participate: Wollo University, College of Medicine and Health Sciences Research and Community Service (RCS) Ethical review committee approved this study and gave Ethical clearance and supportive letter. A supportive letter was given to the hospital and permission was obtained to start data collection. After gaining written consent from each respondent by assuring confidentiality, data collection was commenced anonymously.
Wollo University fully covered the financial issues to handle this research.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Average exchange rate of I $ USD to Ethiopia birr (ETB) during May and June 2020 was I $ USD = 34.1 ETB.
AOR = adjusted odds ratio, COR = Crude odds ratio, CI = confidence interval.
Variables having P < .25 in bivariable analysis.
Statistically significant at P-value < .05 in the multivariable analysis, 1.00 = reference category.
References
- [1].Mendis S, O’Brien E, Seedat YK, Yusuf S. Hypertension and diabetes: entry points for prevention and control of the global cardiovascular epidemic. Int J Hypertens 2013;2013:878460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Adeloye D, Basquill C. Estimating the prevalence and awareness rates of hypertension in Africa: a systematic analysis. PLoS One 2014;9:e104300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Campbell NR, Khalsa T, Lackland DT, et al. World Stroke Organization; International Diabetes Federation; International Council of Cardiovascular Prevention and Rehabilitation; International Society of Nephrology. High Blood Pressure 2016: Why Prevention and Control Are Urgent and Important. The World Hypertension League, International Society of Hypertension, World Stroke Organization, International Diabetes Foundation, International Council of Cardiovascular Prevention and Rehabilitation, International Society of Nephrology. J Clin Hypertens (Greenwich) 2016;18:714–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kibret KT, Mesfin YM. Prevalence of hypertension in Ethiopia: a systematic meta-analysis. Public Health Rev 2015;36:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Owais A, Suchdev PS, Schwartz B, et al. Maternal knowledge and attitudes towards complementary feeding in relation to timing of its initiation in rural Bangladesh. BMC Nutr 2019;5:07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Arokiasamy P, Uttamacharya, Kowal P, et al. Chronic noncommunicable diseases in 6 low- and middle-income countries: findings from wave 1 of the world health organization's study on global ageing and adult health (SAGE). Am J Epidemiol 2017;185:414–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].O’Carroll R, Dennis M, Johnston M, Sudlow C. Improving adherence to medication in stroke survivors (IAMSS): a randomised controlled trial: study protocol. BMC Neurol 2010;10:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ramli A, Ahmad NS, Paraidathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence 2012;6:613–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fisher NDL, Curfman G. Hypertension-A Public health challenge of global proportions. JAMA 2018;320:1757–9. [DOI] [PubMed] [Google Scholar]
- [10].Vrijens B, Antoniou S, Burnier M, de la Sierra A, Volpe M. Current situation of medication adherence in hypertension. Front Pharmacol 2017;8:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Okwuonu CG, Ojimadu NE, Okaka EI, Akemokwe FM. Patient-related barriers to hypertension control in a Nigerian population. Int J Gen Med 2014;7:345–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Roldan PC, Ho GY, Ho PM. Updates to adherence to hypertension medications. Curr Hypertens Rep 2018;20:34. [DOI] [PubMed] [Google Scholar]
- [13].Jaddou HY, Batieha AM, Khader YS, Kanaan AH, El-Khateeb MS, Ajlouni KM. Hypertension prevalence, awareness, treatment and control, and associated factors: results from a national survey, Jordan. Int J Hypertens 2011;2011:828797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Singh S, Shankar R, Singh GP. Prevalence and associated risk factors of hypertension: a cross-sectional study in urban Varanasi. Int J Hypertens 2017;2017:5491838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Awoke A, Awoke T, Alemu S, Megabiaw B. Prevalence and associated factors of hypertension among adults in Gondar, Northwest Ethiopia: a community based cross-sectional study. BMC Cardiovasc Disord 2012;12:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Getenet A, Tesfa M, Ferede A, Molla Y. Determinants of adherence to anti-hypertensive medications among adult hypertensive patients on follow-up in Hawassa Referral Hospital: a case-control study. JRSM Cardiovasc Dis 2019;8:2048004019892758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Oliveira-Filho AD, Morisky DE, Costa FA, Pacheco ST, Neves SF, Lyra DP, Jr. Improving post-discharge medication adherence in patients with CVD: a pilot randomized trial. Arq Bras Cardiol 2014;103:503–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Tibebu A, Mengistu D, Bulto LN. Adherence to prescribed antihypertensive medications and associated factors for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Int J Health Sci (Qassim) 2017;11:47–52. [PMC free article] [PubMed] [Google Scholar]
- [19].Meinema JG, van Dijk N, Beune EJ, Jaarsma DA, van Weert HC, Haafkens JA. Determinants of adherence to treatment in hypertensive patients of African descent and the role of culturally appropriate education. PLoS One 2015;10:e0133560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Freund T, Gensichen J, Goetz K, Szecsenyi J, Mahler C. Evaluating self-efficacy for managing chronic disease: psychometric properties of the six-item Self-Efficacy Scale in Germany. J Eval Clin Pract 2013;19:39–43. [DOI] [PubMed] [Google Scholar]
- [21].Schapira MM, Fletcher KE, Hayes A, et al. The development and validation of the hypertension evaluation of lifestyle and management knowledge scale. J Clin Hypertens (Greenwich) 2012;14:461–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bhandari S, Sarma PS, Thankappan KR. Adherence to antihypertensive treatment and its determinants among urban slum dwellers in Kolkata, India. Asia Pac J Public Health 2015;27:N74–84. [DOI] [PubMed] [Google Scholar]
- [23].Hsu YH, Mao CL, Wey M. Antihypertensive medication adherence among elderly Chinese Americans. J Transcult Nurs 2010;21:297–305. [DOI] [PubMed] [Google Scholar]
- [24].Alefan Q, Huwari D, Alshogran OY, Jarrah MI. Factors affecting hypertensive patients’ compliance with healthy lifestyle. Patient Prefer Adherence 2019;13:577–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS One 2013;8:e62775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Natarajan N, Putnam W, Van Aarsen K, Beverley Lawson K, Burge F. Adherence to antihypertensive medications among family practice patients with diabetes mellitus and hypertension. Can Fam Physician 2013;59:e93–100. [PMC free article] [PubMed] [Google Scholar]
- [27].Mekonnen HS, Gebrie MH, Eyasu KH, Gelagay AA. Drug adherence for antihypertensive medications and its determinants among adult hypertensive patients attending in chronic clinics of referral hospitals in Northwest Ethiopia. BMC Pharmacol Toxicol 2017;18:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Asgedom SW, Atey TM, Desse TA. Antihypertensive medication adherence and associated factors among adult hypertensive patients at Jimma University Specialized Hospital, southwest Ethiopia. BMC Res Notes 2018;11:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Sung SK, Lee SG, Lee KS, Kim DS, Kim KH, Kim KY. First-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims review. Clin Ther 2009;31:1309–20. [DOI] [PubMed] [Google Scholar]
- [30].Degli Esposti L, Saragoni S, Benemei S, et al. Adherence to antihypertensive medications and health outcomes among newly treated hypertensive patients. Clinicoecon Outcomes Res 2011;3:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Berisa HD, Dedefo MG. Non-adherence related factors to antihypertensive medications among hypertensive patients on follow up at Nedjo General Hospital in West Ethiopia. The Open Public Health J 2018;11: doi: 10.2174/1874944501811010062. [Google Scholar]
- [32].Tilea I, Petra D, Voidazan S, Ardeleanu E, Varga A. Treatment adherence among adult hypertensive patients: a cross-sectional retrospective study in primary care in Romania. Patient Prefer Adherence 2018;12:625–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Hareri HA, Abebe M. Assessments of adherence to hypertension medications and associated factors among patients attending tikur anbessa specialized hospital renal unit, Addis Ababa, Ethiopia 2012. Int J Nurs Sci 2013;3:01–6. [Google Scholar]
- [34].Ambaw AD, Alemie GA, W/Yohannes SM, Mengesha ZB. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health 2012;12:282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hareri HA, Abebe M, Asefaw T. Assessments of adherence to hypertension managements and its influencing factors among hypertensive patients attending black lion hospital chronic follow up unit, Addis Ababa, Ethiopia-a cross-sectional study. Int J Pharm Sci Res 2013;4:1086–95. [Google Scholar]
- [36].Teshome DF, Bekele KB, Habitu YA, Gelagay AA. Medication adherence and its associated factors among hypertensive patients attending the Debre Tabor General Hospital, northwest Ethiopia. Integr Blood Press Control 2017;10:01–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Warren-Findlow J, Seymour RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health 2012;37:15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]


