Key Points
RIC-HSCT yields favorable outcomes for patients with high-risk CLL-RT, especially when performed in early remission.
Exposure to novel agents confers at least equal outcomes, whereas use of TBI-containing RIC seems to lead to inferior PFS, OS, and GRFS.
Visual Abstract
Abstract
Allogeneic hematopoietic stem cell transplantation (HSCT) may potentially cure patients with chronic lymphocytic leukemia (CLL) and Richter’s transformation (CLL-RT) or CLL without RT, but the impact of novel agents on HSCT is unclear. CLL-RT patients have a grave prognosis, and their outcomes after HSCT are uncertain. We conducted a retrospective analysis of all 58 CLL patients, including 23 CLL-RT patients, who underwent reduced intensity conditioning (RIC) HSCT at Memorial Sloan Kettering Cancer Center (New York, NY) between September 2006 and April 2017. With a median follow-up of 68 months (range, 24-147 months), 5-year progression-free survival (PFS) was 40% (95% confidence interval [CI], 28%-56%), and overall survival (OS) was 58% (95% CI, 48%-74%). The 1-year graft-versus-host disease/relapse-free survival (GRFS) was 38% (95% CI, 25%-50%). Patients with CLL-RT and CLL patients without RT had comparable outcomes. In both cohorts, treatment-sensitive response and ≤3 previous lines of therapy produced superior PFS and OS. Outcomes were agnostic to adverse cytogenetic and molecular features. Novel agents did not have a negative impact on HSCT outcomes. Total body irradiation (TBI)-containing RIC yielded inferior PFS, OS, and GRFS. CLL-RT patients older than age 55 years who had an HSCT Comorbidity Index score of ≥2 demonstrated inferior OS. This study, which is the largest series of RIC-HSCT for patients with CLL-RT, provides evidence supporting RIC-HSCT in early remission courses for patients with CLL-RT and poor-risk CLL patients. TBI-containing RIC should be considered with caution.
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) offers a potentially curative option for patients with chronic lymphocytic leukemia (CLL) and Richter’s transformation (CLL-RT) or CLL without RT. RT occurs in up to 10% of CLL patients, usually associated with histologic transformation to a diffuse large B-cell lymphoma, although Hodgkin lymphoma transformation has also been well described.1,2 Historically, CLL-RT patients have a poor prognosis, attributable to low rates and short duration of response to intensive chemoimmunotherapy induction regimens, with overall survival (OS) of ∼8 months.3 In a single-center retrospective analysis, patients with CLL-RT who responded to induction and proceeded to consolidation with HSCT experienced improved long-term survival at 3 years (75%; n = 7) in contrast to chemotherapy-sensitive patients who were not consolidated with HSCT (25%; n = 35) or those with relapsed or refractory CLL-RT who underwent HSCT or autologous hematopoietic stem cell transplantation (auto-HSCT) as salvage therapy (21%; n = 13; P = .019).3 Although patients with CLL-RT seem to benefit from postremission consolidation with HSCT, the outcomes of HSCT in those patients have not been thoroughly investigated. The largest series to date describing HSCT outcomes of patients with CLL-RT include 10 patients from the MD Anderson Cancer Center4 and 25 patients from the European Group for Blood and Marrow Transplantation (EBMT) Registry, of whom 18 patients received reduced intensity conditioning (RIC).
With these limited data, the American Society for Transplantation and Cell Therapy (ASTCT) has recommended HSCT for all CLL-RT patients who had demonstrated an objective response to anthracycline-based chemotherapy, with RIC recommended whenever it was indicated.5 In this study, we provide the analysis of outcomes of the largest reported database of CLL-RT patients undergoing RIC-HSCT and identify factors that may have an impact on HSCT outcomes. We also compare the outcomes of CLL-RT patients with those of CLL patients without RT who were undergoing RIC-HSCT.
In addition, despite its curative potential, HSCT for CLL patients in Europe and the United States has markedly declined with the recent approval of novel targeted pathway inhibitors such as ibrutinib, venetoclax, or idelalisib.6 However, few studies have investigated the possible impact of previous exposure to these novel agents on HSCT outcomes.7-9 With this study, we aimed to help further determine the impact of exposure to novel agents on post-HSCT outcomes in patients with CLL and those with CLL-RT.
Methods
Trial design and participants
We identified 61 patients who underwent HSCT for CLL with or without RT at Memorial Sloan Kettering Cancer Center (MSKCC) between 15 September 2006, and 26 April 2017 (Table 1). Only patients who received RIC were included; those who received myeloablative conditioning (MAC; n = 3) were excluded, based on Center for International Blood & Marrow Transplant Research (CIBMTR) definitions.10,11 In all, 23 (39.7%) of the 58 CLL patients who underwent RIC-HSCT had RT.
Table 1.
Patient, CLL, and transplantation characteristics
| Characteristic | CLL-RT patients | CLL patients with no RT | All CLL patients |
|---|---|---|---|
| No. of patients | 23 | 35 | 58 |
| Sex | |||
| Female | 5 | 8 | 13 |
| Male | 18 | 27 | 45 |
| Median age, y (range) | 57.6 (36.3-69.6) | 54.5 (43.4-67.9) | 55 (36.3-69.6) |
| Median time from diagnosis to HSCT, mo | 73.9 (7.9-241.2) | 65.8 (13.1-206.0) | 73.1 (7.9-241.2) |
| Rai stage | |||
| 0 | 5 | 3 | 8 |
| 1 | 10 | 15 | 25 |
| 2 | 5 | 9 | 14 |
| 3 | 1 | 5 | 6 |
| 4 | 2 | 3 | 5 |
| Patients with adverse cytogenetics or molecular features | 14 (60.9) | 30 (85.7) | 44 (75.9) |
| TP53 mutation/del17p | 4 | 12 | 16 |
| IGHV unmutated | 8 | 5 | 13 |
| ZAP70+ | 0 | 8 | 8 |
| del11q | 4 | 16 | 20 |
| Complex | 2 | 7 | 9 |
| HSCT Comorbidity Index score | |||
| 0 | 9 | 11 | 20 |
| 1-2 | 3 | 16 | 19 |
| 3-4 | 7 | 6 | 13 |
| ≥5 | 4 | 2 | 6 |
| Disease response status at time of HSCT | |||
| CR | 7 | 2 | 9 |
| PR | 12 | 23 | 35 |
| SD | 0 | 9 | 9 |
| PD | 4 | 1 | 5 |
| Median No. of previous lines of therapy (range) | Total: 3 (1-9); 2 (1-4) for RT | 3 (1-10) | 3 (1-10) |
| Previous use of novel agent | 2 (8.7) | 9 (25.7) | 11 (19.0) |
| Novel agent | |||
| Ibrutinib | 2 | 8 | 9 |
| Venetoclax | 1 | 4 | 5 |
| Idelalisib/duvelisib | 0 | 3 | 3 |
| Conditioning regimen | |||
| Rituximab-fludarabine-cyclophosphamide-TBI 200 | 14 | 18 | 32 |
| Fludarabine-cyclophosphamide-TBI 200 | 1 | 3 | 4 |
| Fludarabine-cyclophosphamide-thiotepa-TBI 400 | 2 | 2 | 4 |
| Fludarabine-melphalan | 4 | 4 | 8 |
| Fludarabine-melphalan-thiotepa | 2 | 2 | 4 |
| Rituximab-fludarabine-busulfan | 0 | 3 | 3 |
| Fludarabine-busulfan | 0 | 3 | 3 |
| Use of ATG | |||
| Yes | 10 | 13 | 23 |
| No | 13 | 22 | 35 |
| Graft source | |||
| MRD PBSC | 6 | 13 | 19 |
| MUD PBSC | 6 | 13 | 19 |
| Haplo PBSC | 2 | 0 | 2 |
| Haplo bone marrow | 0 | 2 | 2 |
| MMUD PBSC | 4 | 3 | 7 |
| Cord blood transplant | 5 | 4 | 9 |
Haplo, HLA-haploidentical; MMUD, HLA-mismatched unrelated donor; MRD, HLA-matched related donor; MUD, HLA-matched unrelated donor; PBSC, peripheral blood stem cell; TBI 200, total body irradiation 200 cGy; TBI 400, total body irradiation 400 cGy.
CLL patients with TP53 mutations and del17p and all CLL-RT patients were considered for HSCT at their first remission. For other patients, disease refractoriness, tempo of disease progression or relapse, and alternative therapeutic options were considered before HSCT, and the risks and benefits of each were weighed in a multidisciplinary consortium.
Based on HLA-matching, stem cell source, comorbidity, and eligibility, patients underwent HSCT either per institutional standard (rituximab, fludarabine, cyclophosphamide, and total body irradiation 200 cGy (TBI-200) for patients with B-cell non-Hodgkin lymphoma (NHL) or per enrollment on protocols NCT00425802, NCT00387959, NCT00739141, and NCT01027000 (described and registered at www.clinicaltrials.gov).12-14 Distribution of HSCT conditioning regimens, stem cell sources, and use of antithymocyte globulin (ATG) are summarized in Table 1. The cutoff date for data analysis was February 16, 2021. A waiver of authorization for this retrospective review was obtained from the MSKCC Institutional Review and Privacy Board. The study was conducted in accordance with the Declaration of Helsinki. Histologic diagnoses of CLL with or without RT were performed internally by a hematopathologist, with confirmation of a clonal rearrangement involving the IGH gene identified in isolated CLL and RT cells when possible. Otherwise, architecture and immunophenotype were analyzed for suspected clonal relationship. Patients with clonally distinct diffuse large B-cell lymphoma and CLL were excluded.
Outcomes and statistical analysis
Response assessments were defined according to the 2018 International Workshop on Chronic Lymphocytic Leukemia criteria and by using Lugano criteria for RT.15,16 We defined treatment-sensitive disease as partial response (PR) or complete response (CR) to the last line of therapy before HSCT. We categorized as treatment-refractory those with stable disease (SD) or progression of disease (PD) to the last line of treatment before HSCT. Graft-versus-host disease (GVHD) and GVHD relapse-free survival (GRFS) were defined as the time from HSCT to grade 3 to 4 acute GVHD (aGVHD), chronic GVHD (cGVHD) requiring systemic treatment, relapse or PD, or death, whichever came first.17 Cumulative incidence functions were used to estimate the incidence of grade 2 to 4 aGVHD, cGVHD, nonrelapse mortality (NRM), and relapse or PD; comparisons across clinical characteristics were examined using Gray’s test. OS, progression-free survival (PFS), and GFRS were estimated using Kaplan‐Meier methods, and comparisons across clinical characteristics were examined using the log-rank test.
Variables included age, sex, time from diagnosis to HSCT, Rai staging, cytogenetic risks, disease response status at the time of HSCT, number of previous lines of therapy, use of a novel agent (eg, BTK, Bcl-2, and PI3K inhibitors) before HSCT, RT histology, HSCT-Comorbidity Index (HSCT-CI) score, graft source, use of TBI-containing RIC, and use of ATG with conditioning. Multivariable models were built with all univariable covariates with P < .05. All statistical analyses were performed with R v3.4.4 software (R Core Development Team, Vienna, Austria).
Results
Study population
We identified 58 patients who underwent RIC-HSCT at MSKCC for CLL, including 23 patients with RT (39.7%), between 15 September 2006, and 26 April 2017. The median follow-up was 89 months (range, 46-176 months); demographic and clinical characteristics of patients are summarized in Table 1. The median age of patients was 55.0 years (range, 36.3-69.6 years), and the majority of patients (77.6%) were male (n = 45). The median time from CLL diagnosis to HSCT was 73.1 months (range, 7.9-241.2 months). Patients received a median number of 3 lines of therapy before HSCT (range, 1-10 lines of therapy).
Outcomes for all 58 CLL patients
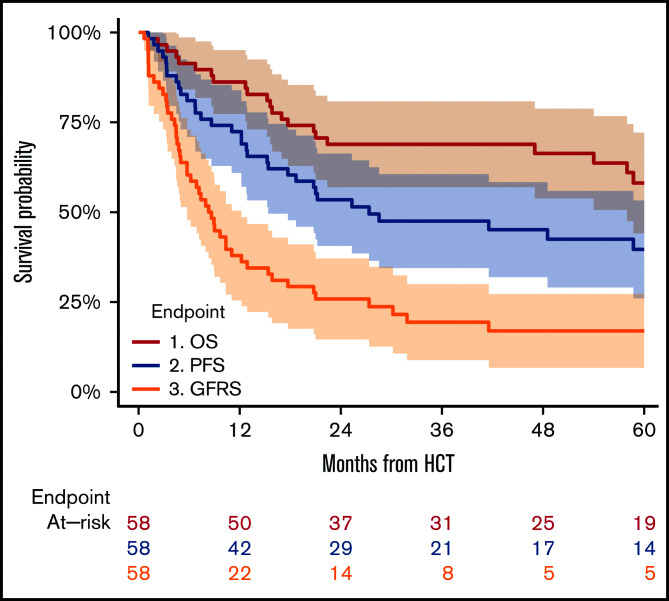
All patients achieved engraftment. For the entire cohort, NRM was 12% at 12 months after HSCT. PFS rates at 12, 24, and 60 months were 72% (95% confidence interval [CI], 61%-84%), 53% (95% CI, 41%-66%), and 40% (95% CI, 28%-56%), respectively, whereas corresponding OS rates were 86% (95% CI, 77%-95%), 69% (95% CI, 57%-81%), and 58% (95% CI, 48%-74%), respectively. The cumulative incidence of PD was 26% (95% CI, 15%-37%) at 24 months. The cumulative incidence of grade 2 to 4 aGVHD at day +100 was 29% (95% CI, 18%-41%), and for cGVHD, it was 33% (95% CI, 21%-45%) at 12 months and 36% (95% CI, 24%-49%) at 24 months after HSCT. GRFS was 38% (95% CI, 25%-50%) at 12 months. GRFS, PFS, and OS estimates for the entire population are illustrated in Figure 1.
Figure 1.
Survival outcomes of CLL patients from the time of HSCT. Data include 1. OS, 2. PFS, and 3. GRFS.
Univariable factors that have an impact on HSCT outcomes for all CLL patients
Patient history and demographic factors.
Although HSCT-CI score and age were not prognostic, female sex was associated with a higher rate of cGVHD (24-month estimates: 27% [95% CI, 14%-40%] vs 69% [95% CI, 33%-94%]; P = .02). This difference did not result in a significant difference in PD, PFS, GRFS, or OS between sexes.
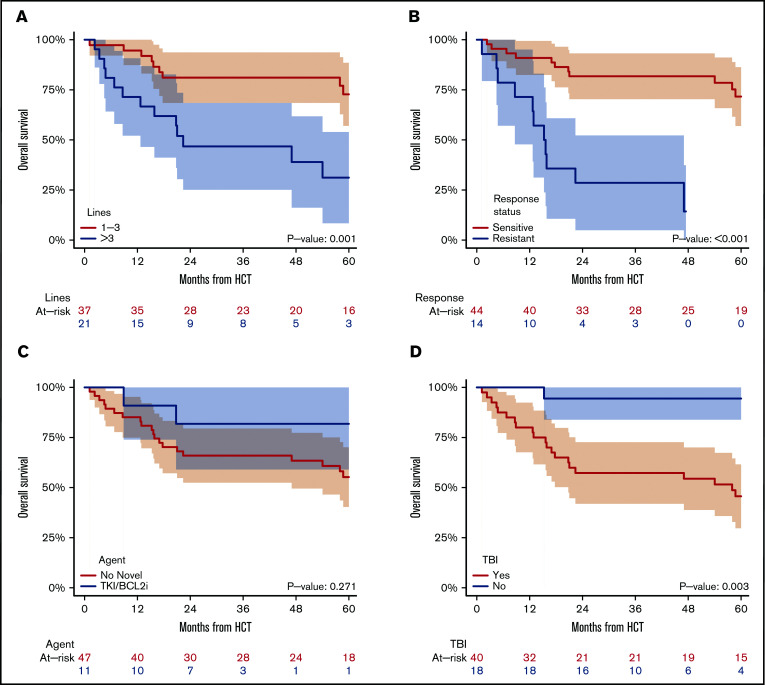
Patients with >3 previous lines of therapy experienced significantly inferior 24-month PFS (24% [95% CI, 6%-42%] vs 70% [95% CI, 56%-85%]; P < .001) and OS (47% [95% CI, 25%-68%] vs 81% [95% CI, 68%-94%]; P = .001; Figure 2A). This group incurred increased NRM (39% [95% CI, 18%-60%] vs 11% [95% CI, 1%-21%]; P = .005), despite a trend toward lower incidence of cGVHD (24% [95% CI, 6%-42%] vs 43% [95% CI, 27%-59%]; P = .055) compared with those with ≤3 previous lines of therapy. In contrast, the time from diagnosis to transplant was not prognostic.
Figure 2.
OS of CLL patients from the time of transplant. Patients are stratified by number of previous lines of therapy (A), remission status at the time of transplantation (B) (treatment-sensitive: CR or PR; refractory: SD or PD), use of novel agent (C), and use of TBI-containing conditioning regimen (D). Bcl-2i, Bcl-2 inhibitor; TKI, tyrosine kinase inhibitor.
CLL disease factors.
Advanced disease stage and molecular and/or cytogenetic risks were not associated with HSCT outcomes. The most significant prognostic factor was the response status at the time of HSCT; those with treatment-sensitive disease had lower rates of 24-month NRM (14% [95% CI, 4%-24%] vs 43% [95% CI, 17%-69%]; P = .004), higher PFS (68% [95% CI, 54%-82%] vs 7% [95% CI, <1%-21%]; P < .001), OS (82% [95% CI, 70%-93%] vs 29% [95% CI, 5%-52%]; P < .001; Figure 2B), and GRFS (32% [95% CI, 18%-46%] vs 7% [95% CI, <1%-21%]; P = .05). The difference in cumulative incidence of PD in patients with treatment-sensitive vs refractory disease was not significant (24-month estimates of 18% [95% CI, 7%-30%] vs 50% [95% CI, 24%-76%]; P = .104).
Exposure to novel agents.
In total, 11 patients (19%) were exposed to at least 1 novel agent before HSCT (Table 1); we did not observe any differences in these patients relative to those without previous exposure to novel agents: rates of grade 2 to 4 aGVHD at day 100 (27% [95% CI, 1%-54%] vs 30% [95% CI, 17%-43%]; P = .703), cumulative incidence of 24-month cGVHD (27% [95% CI, 1%-54%] vs 38% [95% CI, 24%-52%]; P = .483), NRM (9% [95% CI, <1%-26%] vs 23% [95% CI, 11%-36%]; P = .242), PFS (55% [95% CI, 25%-84%] vs 53% [95% CI, 39%-67%]; P = .673), OS (82% [95% CI, 59%-100%] vs 66% [95% CI, 52%-80%]; P = .271; Figure 2C), or GRFS (27% [95% CI, 1%-54%] vs 26% [95% CI, 13%-38%]; P = .581).
Transplant platform.
Although HLA-matched graft sources resulted in expected lower rates of grade 2 to 4 aGVHD at day 100 of 18% (95% CI, 6%-31%) vs 50% (95% CI, 28%-72%) (P = .05) for mismatched grafts, these did not have an impact on the cumulative incidence of cGVHD, relapse, NRM, PFS, OS, or GRFS outcomes. By contrast, TBI-containing conditioning was associated with inferior 24-month PFS (42% [95% CI, 27%-58%] vs 78% [95% CI, 59%-97%]; P = .009), OS (57% [95% CI, 42%-73%] vs 94% [95% CI, 84%-100%]; P = .003; Figure 2D), and GRFS (12-month estimates: 30% [95% CI, 16%-40%] vs 56% [95% CI, 33%-79%]; P = .033), although it did not have an impact on cumulative incidence of PD, NRM, grade 2 to 4 aGVHD at day 100, or cGVHD.
CLL-RT vs CLL without RT.
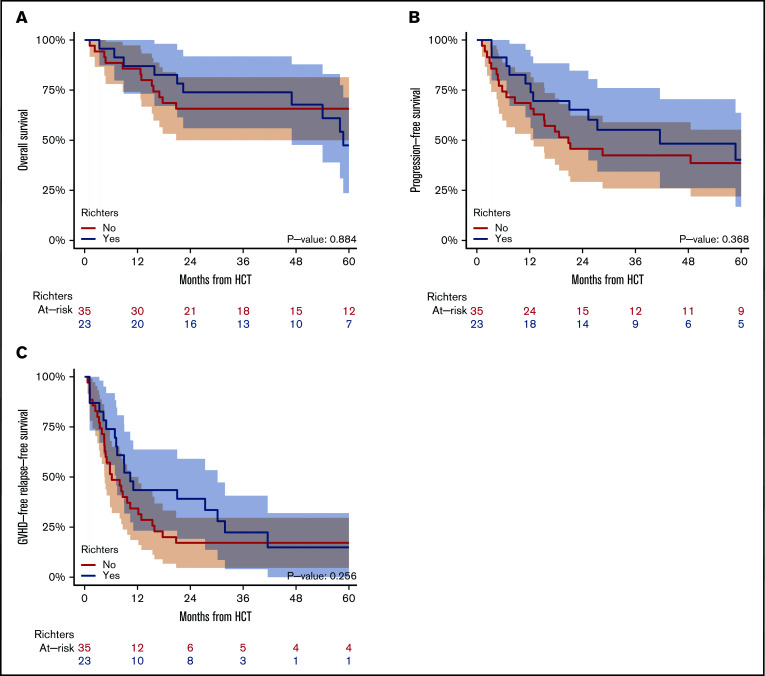
The 23 CLL patients with RT and 35 CLL patients without RT had comparable outcomes, including rates of grade 2 to 4 aGVHD (22% [95% CI, 5%-39%] vs 34% [95% CI, 19%-50%]; P = .126), 24-month cumulative incidence of cGVHD (35% [95% CI, 15%-54%] vs 37% [95% CI, 21%-53%]; P = .565), NRM (13% [95% CI, <1%-27%] vs 26% [95% CI, 11%-40%]; P = .32), OS (74% [95% CI, 56%-92%] vs 66% [95% CI, 50%-81%]; P = .884; Figure 3A), PFS (65% [95% CI, 46%-85%] vs 46% [95% CI, 29%-62%]; P = .638; Figure 3B), or GRFS (39% [95% CI, 19%-59%] vs 17% [95% CI, 5%-30%]; P = .256; Figure 3C).
Figure 3.
Survival outcomes of CLL patients from the time of HSCT. Patients are stratified by manifestation of RT, including OS (A), PFS (B), and GRFS (C).
Multivariable analysis.
In multivariable analysis for the entire population, disease treatment response status at time of HSCT, number of previous lines of therapy, and use of TBI conditioning were included to explore their impact on OS. Treatment-sensitive response at time of HSCT remained favorable and the use of TBI remained unfavorable, whereas having received >3 previous lines of therapy was no longer significant, as shown in Table 2.
Table 2.
Multivariable analysis for the entire cohort
| Variable | N | OS HR (95% CI) | P | |
|---|---|---|---|---|
| Treatment-sensitive response | Yes | 44 | (reference) | .002 |
| No | 14 | 5.19 (1.82-14.84) | ||
| ≤3 lines of therapy | Yes | 37 | (reference) | .337 |
| No | 21 | 1.60 (0.61-4.19) | ||
| TBI conditioning | Yes | 40 | (reference) | .033 |
| No | 18 | 0.11 (0.01-0.83) |
HR, hazard ratio.
Factors that had an impact on HSCT outcomes for the CLL-RT cohort
In the CLL-RT cohort, those who received >3 previous total lines of therapy (for CLL and/or CLL-RT) experienced inferior 24-month PFS (30% [95% CI, 2%-58%] vs 92% [95% CI, 78%-100%]; P = .007) and OS (50% [95% CI, 19%-81%] vs 92% [95% CI, 78%-100%]; P = .021) and a trend toward increased NRM (30% [95% CI, 2%-58%] vs 0; P = .059) in contrast to patients with ≤3 previous lines of therapy. Likewise, treatment-sensitive disease was associated with a lower incidence of PD (P = .05) and a trend toward improved OS (P = .081). In addition, patients age 55 years or younger demonstrated superior 24-month OS compared with those older than age 55 years (80% [95% CI, 55%-100%] vs 69% [95% CI, 44%-94%]; P = .046), despite similar incidence of NRM (P = .403), aGVHD (P = .778), cGVHD (P = .311), PD (P = .616), PFS (P = .407), and GRFS (P = .752). Similarly, patients with a higher HSCT-CI score of ≥2 had poorer OS compared with those with lower score of 0 to 1 (58% [95% CI, 30%-86%] vs 91% [95% CI, 74%-100%]; P = .018; Figure 4), mostly attributable to a trend toward increased 24-month cumulative incidence of NRM (25% [95% CI, 1%-49%] vs 0% [95% CI, not applicable]; P = .069). HSCT-CI did not have an impact on cumulative incidence of aGVHD, cGVHD, PD, PFS, or GRFS. The time from CLL diagnosis to transplantation, use of ATG, and matching HLA grafts were not found to have a significant impact on HSCT outcomes in the CLL-RT cohort; the role of other demographic, transplantation, or disease characteristics could not be adequately examined because of the small size of the population. For the same reason, multivariable analysis could not be performed.
Figure 4.
OS of CLL-RT patients. Patients are stratified by number of previous lines of therapy (A), age (B), and HSCT-CI score (C).
Patient outcomes after HSCT relapse
In all, 8 (34.8%) of 23 patients had PD after HSCT, among whom only 2 (25%) are still alive: 1 achieved a CR after tapering immunosuppression (IS) and remains in CR 7.5 years later; the other patient received sequential lines of chemoimmunotherapy followed by radiation for refractory disease before proceeding with a salvage myeloablative donor-derived auto-HSCT and remained in CR for 11 years after his original HSCT. The 6 other CLL-RT patients who relapsed after HSCT died as a result of PD or treatment complications: 3 received salvage regimens that included novel agents with or without chemoimmunotherapy and had little to no response; 1 received rituximab plus prednisone (during concurrent explosive PD and infection); and 1 patient received salvage chemotherapy followed by a second HSCT and achieved a CR but died as a result of GVHD acquired thereafter.
In addition, 12 (34.3%) of 35 CLL patients without RT had PD after HSCT, of whom 6 patients (50%) are still alive: 1 patient with early PD achieved a CR after tapering IS and concurrent induction with rituximab, remaining in CR 4 years after HSCT; 3 received novel agents with or without chemoimmunotherapy or donor lymphocyte infusions leading to PR, slow PD, or SD, and they are still alive after 4 years, 5 years, and 10 years after HSCT; 1 received ibrutinib plus donor lymphocyte infusions leading to a PR, followed by chimeric antigen receptor (CAR)-modified Epstein-Barr virus cytotoxic T lymphocytes, achieved CR, and is alive 5.5 years after HSCT; 1 was refractory to 3 lines of novel agents and developed RT with PD for which he received zanubrutinib plus nivolumab before receiving CAR T cells, which led to CR and late PD for which combination ibrutinib plus lenalidomide was started. He achieved SD and is still alive 7.5 years after HSCT. Six patients died after relapse: 4 received combinations of novel agents; 1 received rituximab during concurrent early PD and GVHD; 1 relapsed with RT and received sequential chemoimmunotherapy with continued PD.
Causes of death
In total, 31 deaths occurred by the time of data cutoff, including 12 deaths for the CLL-RT population. The most common cause of death in the whole population was GVHD (45.2%), followed by PD (35.5%), infection (6.5%), and cardiac toxicity (6.5%). One patient (3.8%) died as a result of secondary melanoma, and 1 (3.8%) died as a result of unknown causes (Table 3).
Table 3.
Causes of death
| Cause of death | CLL-RT (n = 23) |
CLL without RT (n = 35) |
All CLL patients (n = 58) |
|---|---|---|---|
| Total deaths | 12 | 19 | 31 |
| PD | 5 | 6 | 11 |
| GVHD | 5 | 9 | 14 |
| Infection | 1 | 1 | 2 |
| Cardiac | 1 | 1 | 2 |
| Other/unknown | 0 | 2 | 2 |
Discussion
Herein, we report a single-center retrospective series of CLL patients in the modern era, including the largest cohort of RT patients undergoing RIC-HSCT yet reported. Our analysis confirms the curative potential of RIC-HSCT for CLL patients, demonstrating once again that HSCT overcomes traditional adverse cytogenetic and molecular features.18-21 Similarly, as previously reported, we demonstrated that patients with treatment-sensitive disease and those who had received ≤3 previous lines of treatment had improved PFS and OS.22
Surprisingly, our data suggest that TBI-containing RIC regimens result in inferior outcomes for PFS, OS, and GRFS. The impact on OS was further confirmed on multivariable analysis. Our findings were somewhat unexpected, considering our previously reported institutional favorable outcomes using fludarabine, cyclophosphamide, and TBI-containing RIC with peritransplant rituximab for patients with B-cell NHL undergoing HSCT.12 Similarly, a large series from the Fred Hutchinson Cancer Research Center has shown equally promising outcomes for 212 CLL patients who received TBI-based RIC-HSCT with or without peritransplant rituximab.23 However, all patients in the Seattle group series received TBI-based conditioning, perhaps on the basis of their previous institutional data that suggested a potential benefit of TBI in MAC regimens.24 This is consistent with results from the CIBMTR Registry, which showed that TBI-containing MAC for CLL patients resulted in outcomes similar to those with chemotherapy-only MAC.25 Nevertheless, our findings confirmed results from the Chronic Leukemia Working Party of the EBMT,26 which show that TBI-containing RIC regimens increased the risk of all-cause mortality in CLL patients. The authors proposed a possible explanation that consisted of stronger CLL-specific activity conferred with the fludarabine-containing regimens. However, in our cohort, all patients except those who received TBI also received fludarabine as part of their conditioning, thereby suggesting that the effect of TBI may be independent of exposure to fludarabine. Interestingly, the CIBMTR Lymphoma Working Committee recently presented registry data illustrating that a higher dose of TBI (400 cGy vs 200 cGy) for patients with NHL undergoing TBI-containing RIC-HSCT led to significantly higher rates of NRM and overall mortality without increasing the risk of GVHD, concluding that 200 cGy was the optimal TBI dosing in those patients.27 In our cohort, 36 (90%) of 40 patients who underwent TBI-containing RIC received 200 cGy dosing and only 4 (10%) received 400 cGy. Thus, the TBI dosing intensity is unlikely the reason for our finding.
In addition, the CIBMTR recently published data regarding the impact of various RIC regimens on HSCT outcomes for NHL patients, and patients who received fludarabine, cyclophosphamide, and 200 cGy of TBI conditioning were among those with the best outcomes, which were superior to outcomes of patients who received more intensive fludarabine-melphalan 140 mg/m2 conditioning.28 Our findings suggest that, unlike patients with other NHL histologies, patients with CLL might not benefit from TBI-containing regimens. A previous study from Denmark reported that patients with CLL had lower response rates to low doses of radiation at irradiated sites compared with patients with other indolent NHL histologies. The overall response rate was 71% vs 87%, respectively, and CR rates especially were much lower: 25% vs 78%.29 TP53 and del17p aberrations along with del11q, del13q, and CD38 expression might confer enhanced radiation resistance on CLL cells.30 In our study, patients who received TBI-containing RICs had statistically nonsignificant increased incidence of PD, NRM, and grade 2 to 4 aGVHD. Taken together, we suspect that TBI-containing RICs for patients with CLL might be associated with multifactorial morbidity and mortality features via suboptimal antitumor effects. In addition, there is a possibly increased combined risk of severe GVHD as reported by the GVHD Working Group of the Japan Society of Hematopoietic Cell Transplantation31; this would require deep and prolonged IS that would ultimately result in augmented risks of combined PD, end-organ toxicity,32 and infection. Our findings, along with those from EBMT, suggest that TBI-based RIC should not be used, even with caution, in CLL patients. The impact of TBI should be further explored within the CIBMTR Registry of CLL patients with or without RT in the absence of randomized prospective trials.
Patients exposed to novel agents seem to have favorable outcomes, with 82% OS at 2 years, although that rate is statistically nonsignificant compared with that for novel agent–naïve patients in our size-limited study. A retrospective study from the EBMT Registry suggested that previous exposure to ibrutinib seemed to be associated with increased posttransplant relapse,8 but our experiences, included in a recent multicenter, international, retrospective cohort study of CLL patients undergoing HSCT after having received ≥1 novel agents,7 does not corroborate this finding. A recent single-center retrospective analysis of 108 patients with high-risk CLL, among whom 30 had received a novel agent before receiving HSCT, suggested favorable outcomes for patients who received previous novel therapy with 3-year PFS and OS of 72% and 87%, respectively, vs 58% and 69%, respectively, for patients who received only chemoimmunotherapy, but these differences were not statistically significant (P = .3 and P = .22, respectively).9 Taken together, these findings and ours suggest that exposure to novel agents before HSCT does not have a negative impact on outcomes and perhaps might be advantageous. Data from larger registries are needed to more definitely answer this question. Our results confirm that remission status remains the most significant prognostic factor for CLL patients undergoing RIC-HSCT.33
CLL-RT patients and CLL patients without RT who underwent RIC-HSCT at our institution had comparable outcomes. This is the largest reported series of CLL-RT patients undergoing RIC-HSCT, and our findings illustrate the similarly significant roles of treatment-sensitive response status and number of lines of therapies on HSCT outcomes. Notably, we also found that, unlike in CLL patients without RT, HSCT Comorbidity Index score and age influenced OS outcomes with patients age 55 years or younger and patients with score 0 to 1 surviving longer than those older than age 55 years with score ≥2, despite similar NRM, aGVHD, cGVHD, PD, PFS, and GRFS for patients in both age groups. One plausible explanation is that patients with CLL-RT generally received more intensive induction chemoimmunotherapeutic regimens, which could potentially have a greater impact on older patients with more comorbidities. This would result in higher HSCT-CI scores approaching significance (median score of 3 for patients older than age 55 years vs a score of 0.5 for those age 55 years or younger; P = .06). Relapse after HSCT remains a major cause of death in patients with CLL-RT, as expected given the intrinsic aggressiveness of RT histology.1
Our study is limited by its retrospective design and its restriction to 1 single-center experience. Our data inherently lack information on the denominator for all CLL-RT patients not referred to or offered HSCT, which generates a potential selection bias in favor of this cohort. Interestingly, the German CLL Study Group recently explored the outcomes and treatment courses of CLL patients with or without RT starting from time of presentation in a meta-analysis.3 Of 2795 CLL patients, 103 patients (3.5%) had RT; the median OS after diagnosis of RT was 9.4 months. Only 3 patients with RT received allo-HSCT for a corresponding median OS of 17.9 months. The authors could not explain the low numbers of HSCTs, with age unlikely to be a reason (median age of RT patients was only 65 years), whereas a lack of sufficient remissions was possible (overall response rates of 30% to 50% and up to 67% in 1 trial included in the meta-analysis).34 Accordingly, our patients with RT who proceeded to HSCT might have been chosen as a result of selection bias, perhaps based on response, fitness, or other factors, although our patients included a significant proportion with poor HSCT-CI score, advanced age, and/or multirefractory disease tempo. Therefore, it is still valuable to describe the favorable outcomes of CLL-RT patients who proceeded with consolidation HSCT. However, with the increasing use of novel agents over chemoimmunotherapy for CLL in recent years, our study may not fully represent the current practice of sequencing therapeutic interventions and does not fully assess the impact of such agents.
Taken together, our study provides evidence in support of the Guidelines from the ASTCT, which recommend that all patients with CLL-RT should receive postremission consolidation with HSCT with curative intent.5,35 HSCT overcomes adverse molecular, staging, and cytogenetic features, and patients with CLL with or without RT who possess adverse phenotypic characteristics should be considered for early HSCT before the cumulative toxicity of multiple lines of therapy. Furthermore, our data favor the use of RIC regimens that do not contain TBI for CLL patients undergoing HSCT. It remains challenging to determine the optimal sequencing of therapies for patients with high-risk CLL and/or CLL-RT. Our findings suggest that novel agents are likely of greater benefit before HSCT because no patients who relapsed after HSCT achieved any deep, durable remission with novel agents delivered after HSCT. However, patients who received immune effector cells after HSCT relapse achieved CRs (although they were occasionally transient) and have remained alive. Similarly, other researchers have published the efficacy of allo-HSCT after patients with hematologic malignancies received CAR T cells, including patients with CLL.36 Perhaps, a combined modality approach with concurrent T-cell–depleted allo-HSCT with donor-derived CAR T cells would optimize the graft-versus-leukemia effect while minimizing the GVHD effect. To answer this question, our institution has opened a phase 1 trial exploring this concept (clinicaltrials.gov Identifier: NCT04556266). Larger, multicenter registry and prospective studies should be undertaken to corroborate our findings and further determine the role of HSCT for managing patients with CLL with or without RT in the era of novel agents and immune effector cell therapies.
Acknowledgments
The authors acknowledge our institution’s staff and investigators and all patients who contributed to the completion of this study.
This work was supported in part by a grant from the National Cancer Institute, National Institutes of Health (NIH) Cancer Center Support (P30 CA008748).
The authors are solely responsible for the content of this article and do not necessarily represent the official views of the NIH.
Authorship
Contribution: O.B.L. and C.S.S. designed the study, performed the research, analyzed the data, and wrote the paper; S.M.D. analyzed the data; O.B.L., P.B.D., D.M.P., B.G., G.K., J.W.Y., H.R.C.-M., J.N.B., E.B.P., A.A.J., S.A.G., M.A.P., and C.S.S. treated patients and provided study material; M.A.M. provided study material; L.E.R., A.D.Z., and A.R.M. reviewed the manuscript and made insightful clinical points; and all authors participated in the discussion, reviewed and approved the final version of the article, and had access to all the data.
Conflict-of-interest disclosure: O.B.L. served on an advisory board for MorphoSys. L.E.R. served as a consultant for AbbVie, AstraZeneca, Janssen, Pharmacyclics, Lilly Oncology, and Vaniam Group; received grant funding from the American Society of Hematology, Pfizer, and Aptose Biosciences (paid to the institution) outside of the submitted work; and has minority ownership interest in Abbott Laboratories. P.B.D. served on an advisory board for Kite. J.W.Y. has common stock in Amgen, Merck, and Pfizer. J.N.B. received research funding from Angiocrine Bioscience, Gamida Cell, and Merck. A.D.Z. received research grants from AbbVie, Adaptive Biotechnologies, Bristol Myers Squibb, BeiGene, Genentech/Roche, and MEI Pharma, consulting fees from Amgen, AstraZeneca, BeiGene, Genentech/Roche, Janssen, JUNO/Celgene/Bristol Myers Squibb, Kite/Gilead, MEI Pharma, Pfizer, Pharmacyclics, and Sandoz/Novartis, and serves on the scientific advisory board of Adaptive Biotechnologies, Lymphoma Research Foundation. A.R.M. received grants from Loxo, Sunesis, Regeneron, and DTRM, grants and other funding from Celgene, grants and personal fees from Pharmacyclics, Janssen, Genentech, AbbVie, Adaptive, and AstraZeneca, grants, personal fees, and other funding from TG Therapeutics, and personal fees from Beigene. S.A.G. has received research funding from Miltenyi Biotec, has consulted for and received research funding from Amgen, Actinium, Celgene, Johnson & Johnson, Bristol Myers Squibb, Sanofi, Pfizer, and Takeda, and has consulted for Jazz Pharmaceuticals, GlaxoSmithKline, Novartis, Kite, and Spectrum Pharmaceuticals. M.A.P. has served on advisory boards for MolMed, NexImmune, Medigene, and Servier, received honoraria and served on advisory boards for AbbVie, Bellicum, Bristol Myers Squibb, Nektar Therapeutics, Novartis, Omeros, and Takeda, consulted for and received honoraria from Merck, and received research funding from Kite/Gilead, Incyte, and Miltenyi Biotec. C.S.S. served as a consultant on advisory boards for Juno Therapeutics, Sanofi-Genzyme, Spectrum Pharmaceuticals, Novartis, Genmab, Precision Biosciences, Kite, Celgene, Gamida Cell, and GlaxoSmithKline and received research funding from Juno Therapeutics, Celgene, Precision Biosciences, and Sanofi68 Genzyme. The remaining authors declare no competing financial interests.
Correspondence: Oscar B. Lahoud, Memorial Sloan Kettering Cancer Center, 1101 Hempstead Turnpike, Uniondale, NY 11553; e-mail: lahoudo@mskcc.org.
References
- 1.Tsimberidou AM, Keating MJ.. Richter syndrome: biology, incidence, and therapeutic strategies. Cancer. 2005;103(2):216-228. [DOI] [PubMed] [Google Scholar]
- 2.Bockorny B, Codreanu I, Dasanu CA.. Hodgkin lymphoma as Richter transformation in chronic lymphocytic leukaemia: a retrospective analysis of world literature. Br J Haematol. 2012;156(1):50-66. [DOI] [PubMed] [Google Scholar]
- 3.Tsimberidou AM, O’Brien S, Khouri I, et al. Clinical outcomes and prognostic factors in patients with Richter’s syndrome treated with chemotherapy or chemoimmunotherapy with or without stem-cell transplantation. J Clin Oncol. 2006;24(15):2343-2351. [DOI] [PubMed] [Google Scholar]
- 4.Kharfan-Dabaja MA, Bazarbachi A.. Hematopoietic stem cell allografting for chronic lymphocytic leukemia: a focus on reduced-intensity conditioning regimens. Cancer Contr. 2012;19(1):68-75. [DOI] [PubMed] [Google Scholar]
- 5.Kharfan-Dabaja MA, Kumar A, Hamadani M, et al. Clinical practice recommendations for use of allogeneic hematopoietic cell transplantation in chronic lymphocytic leukemia on behalf of the Guidelines Committee of the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2016;22(12):2117-2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gribben JG. How and when I do allogeneic transplant in CLL. Blood. 2018;132(1):31-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roeker LE, Dreger P, Brown JR, et al. Allogeneic stem cell transplantation for chronic lymphocytic leukemia in the era of novel agents. Blood Adv. 2020;4(16):3977-3989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dreger P, Michallet M, Bosman P, et al. Ibrutinib for bridging to allogeneic hematopoietic cell transplantation in patients with chronic lymphocytic leukemia or mantle cell lymphoma: a study by the EBMT Chronic Malignancies and Lymphoma Working Parties. Bone Marrow Transplant. 2019;54(1):44-52. [DOI] [PubMed] [Google Scholar]
- 9.Kim HT, Shaughnessy CJ, Rai SC, et al. Allogeneic hematopoietic cell transplantation after prior targeted therapy for high-risk chronic lymphocytic leukemia. Blood Adv. 2020;4(17):4113-4123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bacigalupo A, Ballen K, Rizzo D, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15(12):1628-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giralt S, Ballen K, Rizzo D, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant. 2009;15(3):367-369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sauter CS, Barker JN, Lechner L, et al. A phase II study of a nonmyeloablative allogeneic stem cell transplant with peritransplant rituximab in patients with B cell lymphoid malignancies: favorably durable event-free survival in chemosensitive patients. Biol Blood Marrow Transplant. 2014;20(3):354-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bolaños-Meade J, Reshef R, Fraser R, et al. Three prophylaxis regimens (tacrolimus, mycophenolate mofetil, and cyclophosphamide; tacrolimus, methotrexate, and bortezomib; or tacrolimus, methotrexate, and maraviroc) versus tacrolimus and methotrexate for prevention of graft-versus-host disease with haemopoietic cell transplantation with reduced-intensity conditioning: a randomised phase 2 trial with a non-randomised contemporaneous control group (BMT CTN 1203). Lancet Haematol. 2019;6(3):e132-e143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ponce DM, Sauter C, Devlin S, et al. A novel reduced-intensity conditioning regimen induces a high incidence of sustained donor-derived neutrophil and platelet engraftment after double-unit cord blood transplantation. Biol Blood Marrow Transplant. 2013;19(5):799-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hallek M, Cheson BD, Catovsky D, et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018;131(25):2745-2760. [DOI] [PubMed] [Google Scholar]
- 16.Cheson BD, Fisher RI, Barrington SF, et al. ; United Kingdom National Cancer Research Institute . Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059-3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holtan SG, DeFor TE, Lazaryan A, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125(8):1333-1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dreger P, Döhner H, Ritgen M, et al. ; German CLL Study Group . Allogeneic stem cell transplantation provides durable disease control in poor-risk chronic lymphocytic leukemia: long-term clinical and MRD results of the German CLL Study Group CLL3X trial. Blood. 2010;116(14):2438-2447. [DOI] [PubMed] [Google Scholar]
- 19.Khouri IF, Saliba RM, Admirand J, et al. Graft-versus-leukaemia effect after non-myeloablative haematopoietic transplantation can overcome the unfavourable expression of ZAP-70 in refractory chronic lymphocytic leukaemia. Br J Haematol. 2007;137(4):355-363. [DOI] [PubMed] [Google Scholar]
- 20.Sorror ML, Storer BE, Sandmaier BM, et al. Five-year follow-up of patients with advanced chronic lymphocytic leukemia treated with allogeneic hematopoietic cell transplantation after nonmyeloablative conditioning. J Clin Oncol. 2008;26(30):4912-4920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schetelig J, de Wreede LC, van Gelder M, et al. Risk factors for treatment failure after allogeneic transplantation of patients with CLL: a report from the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant. 2017;52(4):552-560. [DOI] [PubMed] [Google Scholar]
- 22.Brown JR, Kim HT, Li S, et al. Predictors of improved progression-free survival after nonmyeloablative allogeneic stem cell transplantation for advanced chronic lymphocytic leukemia. Biol Blood Marrow Transplant. 2006;12(10):1056-1064. [DOI] [PubMed] [Google Scholar]
- 23.Shadman M, Maloney DG, Storer B, et al. Rituximab-based allogeneic transplant for chronic lymphocytic leukemia with comparison to historical experience. Bone Marrow Transplant. 2020;55(1):172-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doney KC, Chauncey T, Appelbaum FR; Seattle Bone Marrow Transplant Team. Allogeneic related donor hematopoietic stem cell transplantation for treatment of chronic lymphocytic leukemia. Bone Marrow Transplant. 2002;29(10):817-823. [DOI] [PubMed] [Google Scholar]
- 25.Sabloff M, Sobecks RM, Ahn KW, et al. Does total body irradiation conditioning improve outcomes of myeloablative human leukocyte antigen-identical sibling transplantations for chronic lymphocytic leukemia? Biol Blood Marrow Transplant. 2014;20(3):421-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dreger P, Brand R, Hansz J, et al. ; Chronic Leukemia Working Party of the EBMT . Treatment-related mortality and graft-versus-leukemia activity after allogeneic stem cell transplantation for chronic lymphocytic leukemia using intensity-reduced conditioning. Leukemia. 2003;17(5):841-848. [DOI] [PubMed] [Google Scholar]
- 27.Hamadani M, Khanal M, Ahn KW, et al. Higher total body irradiation dose intensity in fludarabine/TBI-based reduced-intensity conditioning regimen is associated with inferior survival in non-Hodgkin lymphoma patients undergoing allogeneic transplantation. Biol Blood Marrow Transplant. 2020;26(6):1099-1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghosh N, Ahmed S, Ahn KW, et al. Association of reduced-intensity conditioning regimens with overall survival among patients with non-Hodgkin lymphoma undergoing allogeneic transplant. JAMA Oncol. 2020;6(7):1011-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jóhannsson J, Specht L, Mejer J, Jensen BA.. Phase II study of palliative low-dose local radiotherapy in disseminated indolent non-Hodgkin’s lymphoma and chronic lymphocytic leukemia. Int J Radiat Oncol Biol Phys. 2002;54(5):1466-1470. [DOI] [PubMed] [Google Scholar]
- 30.Ouillette P, Fossum S, Parkin B, et al. Aggressive chronic lymphocytic leukemia with elevated genomic complexity is associated with multiple gene defects in the response to DNA double-strand breaks. Clin Cancer Res. 2010;16(3):835-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nakasone H, Fukuda T, Kanda J, et al. ; GVHD working group of the Japan Society of Hematopoietic Cell Transplantation . Impact of conditioning intensity and TBI on acute GVHD after hematopoietic cell transplantation. Bone Marrow Transplant. 2015;50(4):559-565. [DOI] [PubMed] [Google Scholar]
- 32.Glezerman IG, Jhaveri KD, Watson TH, et al. Chronic kidney disease, thrombotic microangiopathy, and hypertension following T cell-depleted hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2010;16(7):976-984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krämer I, Stilgenbauer S, Dietrich S, et al. Allogeneic hematopoietic cell transplantation for high-risk CLL: 10-year follow-up of the GCLLSG CLL3X trial. Blood. 2017;130(12):1477-1480. [DOI] [PubMed] [Google Scholar]
- 34.Al-Sawaf O, Robrecht S, Bahlo J, et al. Richter transformation in chronic lymphocytic leukemia (CLL)-a pooled analysis of German CLL Study Group (GCLLSG) front line treatment trials. Leukemia. 2021;35(1):169-176. [DOI] [PubMed] [Google Scholar]
- 35.Majhail NS, Farnia SH, Carpenter PA, et al. Indications for autologous and allogeneic hematopoietic cell transplantation: Guidelines from the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2015;21(11):1863-1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shadman M, Gauthier J, Hay KA, et al. Safety of allogeneic hematopoietic cell transplant in adults after CD19-targeted CAR T-cell therapy. Blood Adv. 2019;3(20):3062-3069. [DOI] [PMC free article] [PubMed] [Google Scholar]