Abstract
While religion/spirituality strongly protects against drug use (Cheney et al. in J Drug Issues 44(1):94–113, 2014), little is known about gender differences in the association of religion/spirituality on simultaneous polysubstance use (SPU) among those who use prescription opioids. Data come from a community-based study that recruited community members from the St Louis area (N = 632). Participants were asked whether they used prescription opioids when not prescribed for them or in ways other than prescribed in the past 12 months. Religion/spirituality was categorized as high, medium, or low based on personal views on the importance of religion and spirituality, attendance at religious services, and advice seeking from religious leaders. SPU was defined as non-medical use of opioids simultaneously with use of cocaine, alcohol, ecstasy, or marijuana. Multivariate logistic regression determined the association between religion/spirituality, demographic variables, and SPU. Men with high levels of religion/spirituality had 63 % decreased odds of SPU compared with men with low levels. Other variables associated with SPU in men were four or more arrests (AOR 2.21), multiple sex partners (AOR 2.11), and opioid use without a prescription (AOR 3.04). Women with high or medium levels of religion/spirituality had 58 and 62 % decreased odds of SPU compared with women with low levels. Variables that predicted SPU in women also included 4+ arrests (AOR 5.00) and never being married (AOR 2.13). Being African-American was associated with decreased odds of SPU in women (AOR 0.32). Overall, a high level of religion/spirituality was associated with lower odds of SPU. Gender differences in this association were evident, whereas women with even a medium level of religion/spirituality had significantly decreased odds of SPU. Future drug prevention and interventions should consider the relevance of religion/spirituality in SPU.
Keywords: Religion and spirituality, Prescription opioids, Simultaneous polysubstance use
Introduction
Drug use and abuse are long-standing public health issues that affect nearly 3.8 million Americans each year (Olthius et al. 2013). Prescription drug use—such as opioid use—has now become the third most common substance use problem after alcohol and marijuana (Benotsch et al. 2011, 2013). Since the late 1980s, the rate of sales per person for prescription opioids has increased 627 % (Cassidy et al. 2014). Moreover, studies have shown that those who illegally use drugs usually use more than one substance (Trenz et al. 2013). Research by Benotsch et al. (2011) found that those reporting the non-medical use of prescription drugs were also more likely to also report using poppers, ecstasy, cocaine, marijuana, alcohol, and methamphetamines. However, research in this area has mainly focused on college students, adolescents, and persons in drug treatment (Puffer et al. 2012).
Simultaneous polysubstance use (SPU), the act of using multiple illicit substances at the same time, has been noted in many substance-using populations such as prescription opioid abusers (Olthius et al. 2013). Those who engage in SPU are known to mix even more potent illicit drugs with their drug of choice, increasing the risk of additional negative effects (Trenz et al. 2013; Olthius et al. 2013). Furthermore, other negative consequences including crime, social and economic consequences, and risky sexual behaviors have been associated with SPU (Moss et al. 2014; Trenz et al. 2013; Puffer et al. 2012).
The development of effective interventions to reduce SPU may be complicated as studies show that interventions based on behavior change vary widely among individuals (Sofuoglu et al. 2013). Although the effectiveness is difficult to determine, elements of religion and spirituality are increasingly being included in behavioral interventions (Elkonin et al. 2014). Nearly all (95 %) of Americans report a belief in a God or a higher power, with 75 % of them indicating that religion/spirituality influences the decisions they make (Billioux et al. 2014). Religion/spirituality has been shown to be associated with a decrease in risky behaviors including drug use (Cheney et al. 2014; Hobern 2014; Elkonin et al. 2014; Luquis et al. 2012; Moore et al. 2013; O’brien et al. 2013; Wilkerson et al. 2013; Gmel et al. 2013). Although some studies have shown women to be more involved in religion/spirituality than men, other studies have found no evidence to support these findings (Luquis et al. 2012; Reid-Arndt et al. 2011; Simpson et al. 2008). However, current research indicates that gender differences in the association between religion/spirituality and health behaviors and perceptions do exist. Particularly in men, religion/spirituality has been shown to influence drug use behaviors, sexual behaviors, and general health perceptions than in women (Luquis et al. 2012; Reid-Arndt et al. 2011; Staton-Tindall et al. 2008). Because of these factors, more attention should be paid to the association between religion/spirituality and SPU, especially by gender.
Thus, the aim of these analyses is to add to the knowledge of the effect of religion/spirituality in the presence of other risky behaviors on the simultaneous use of prescription opioids with other substances. These analyses were conducted among a community recruited sample of drug users, who are often underrepresented in research. We hypothesized not only that religion/spirituality will be protective against SPU, but that a dose response relationship will be observed, where higher levels of religion/spirituality will be associated with lower odds of SPU. We also hypothesized that the relationship between religion/spirituality and SPU will be stronger among men.
Methods
Overall Outreach and Data Collection
The sample for this cross-sectional study is 632 participants from the National Institute on Drug Abuse (NIDA)-funded Prescription, Misuse, Abuse, and Dependence study (R01DA20791, PI: Cottler). The study recruited adults 18 years or older with a special emphasis on those 25 years of age and under and those 50 and over. Community members were recruited from various community locations in the St Louis Metropolitan Statistical area. The main purpose of the study was to develop a reliable assessment of DSM-IV opioid, stimulant, and sedative use disorders. To be included in these analyses, participants had to have given consent and to have reported either using prescription opioids other than prescribed or using them when not prescribed to them in the past 12 months. This study was approved by the Institutional Review Board (IRB) of Washington University of St. Louis.
Assessment
The Risk Behavior Assessment (RBA), originally developed by the NIDA for studies with HIV/AIDS risk behaviors, was modified for use in this study based on additional questions tested in focus groups. The modified questions were found to be highly reliable (Shacham and Cottler 2010). Questions used in these analyses included: religion/spirituality in the past 12 months, non-medical use of prescription opioids and SPU in the past 12 months, and general demographic information.
Exposure Variable
A composite variable for religion/spirituality was created based on answers to three questions: (1) How important is religion/spirituality to you? (2) In the past 12 months, have you sought the help or advice of a priest, rabbi, or other member of the religious community? and (3) In the past 12 months, how often have you attended religious services at a church, mosque, temple, shrine, or synagogue? These questions are similar to other questions that have been used to measure religion/spirituality (Billioux et al. 2014). From these three questions, religion/spirituality was defined as high, medium, or low. Participants considered low on religion/spirituality reported that religion/spirituality was not at all or was somewhat important, that they never or rarely attended religious services, and they did not seek advice from a member of a religious community member in the past 12 months. Those who were categorized as high on religion/spirituality reported that religion/spirituality was very important, that they sometimes or often attended religious services, and that they sought advice from a member of a religious community member in the past 12 months. Participants with all other combinations of views of religion/spirituality, attendance at religious activities, and religious advice seeking were categorized as having a medium level of religion/spirituality.
Outcome Variable
To assess the outcome variable simultaneous polysubstance use (SPU), participants, who were all prescription opioid users, were asked "In the last 12 months have you used prescription opioids and (a–d) together? (a) alcohol, (b) marijuana, (c) ecstasy/MDMA, (d) crack/cocaine." Participants who reported using prescription opioids in combination with any of these drugs were considered SPU.
Analysis
Bivariate analyses and multivariate logistic regression determined the association between religion/spirituality, gender and other demographic variables, and SPU. All analyses were conducted using SAS statistical software 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Demographics
Our sample consisted of 632 participants of whom 66 % met the criteria for SPU. As shown in Table 1, the most commonly used substance with prescription opioids was alcohol. Of the 11 different SPU patterns, alcohol was involved in eight of those patterns. Alcohol and marijuana, together with opioids, was the next most common with 13 % reporting this pattern. Other common patterns were marijuana and opioids (9 %), and alcohol, marijuana, and cocaine (8 %). Ecstasy was the least reported drug used in conjunction with the non-medical use of prescription opioids.
Table 1.
Drug patterns among simultaneous polysubstance users (N = 415)
| Opioid use + | Frequency | % |
|---|---|---|
| Alcohol only | 141 | 22.31 |
| Alcohol + marijuana | 81 | 12.82 |
| Alcohol + cocaine | 35 | 5.54 |
| Alcohol + marijuana + cocaine | 53 | 8.39 |
| Alcohol + ecstasy/MDMA | 1 | 0.16 |
| Alcohol + marijuana + ecstasy/MDMA or Alcohol + marijuana + ecstasy/MDMA + cocaine | 22 | 3.48 |
| Marijuana only | 54 | 8.54 |
| Marijuana + ecstasy/MDMA | 4 | 0.63 |
| Marijuana + cocaine | 2 | 0.32 |
| Crack/cocaine only | 21 | 3.32 |
| Ecstasy/MDMA | 1 | 0.16 |
As shown in Table 2, the majority of the sample was male and had never married. Over half of the sample (56 %) self-identified as African-American. Of those who were non-African-American, the vast majority (85 %) were Caucasian. One-fifth (20 %) of the sample was between the ages of 18 and 25 or had at least three sexual partners in the last 12 months. Over one-fourth reported three or more children (30 %) or grew up believing there was a pill for everything (28 %). When those who engaged in SPU were compared to those who did not engage in SPU, we found that users were significantly less likely to be African-Americans, male, younger, never been married, to have used prescription opioids without a prescription, to have a greater arrest history, and to have had more sexual partners in the past 12 months.
Table 2.
Demographic characteristics of the sample (N = 632)
| Demographic characteristics | SPU (N = 415, 66 %) | No SPU (N = 217, 34 %) | Total in sample (N = 632, 100 %) | P value |
|---|---|---|---|---|
| High R/S vs. low | 85 (20 %) | 67 (31 %) | 169 (27 %) | <.001 |
| Medium R/S vs. low | 198 (48 %) | 113 (52 %) | 311 (49 %) | |
| Low R/S | 132 (32 %) | 37 (17 %) | 152 (24 %) | |
| African-American | 222 (53 %) | 134 (62 %) | 356 (56 %) | .047 |
| Men | 244 (59 %) | 105 (48 %) | 349 (55 %) | .012 |
| 18–25 years | 101 (24 %) | 26 (12 %) | 127 (20 %) | <001 |
| Used Rx opioids without a prescription | 332 (80 %) | 133 (61 %) | 465 (75 %) | <0001 |
| High-school diploma or less | 300 (72 %) | 147 (68 %) | 447 (70 %) | .233 |
| Arrested 4+ | 220 (53 %) | 85 (39 %) | 305 (48 %) | <001 |
| 3+ sex partners in the past 12 months | 100 (24 %) | 24 (11 %) | 124 (20 %) | <001 |
| Never been married | 250 (60 %) | 100 (46 %) | 350 (55 %) | <001 |
| 3+ children | 119 (29 %) | 71 (33 %) | 190 (30 %) | .29 |
| Pill for everything vs. no pill for everything | 61 (28 %) | 118 (28 %) | 179 (28 %) | .932 |
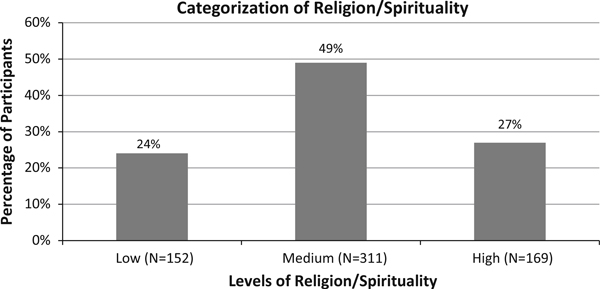
Religion/Spirituality
Of the 349 men and 283 women recruited into this study, the majority (64 %) reported that religion/spirituality was very important to them. Half of the sample either attended a church, mosque, temple, shrine, synagogue often (28 %) or sometimes (22 %) in the past 12 months, and 32 % had sought the advice of a priest, minister, rabbi, or another member of the religious community in the past 12 months. Based on these responses, nearly one quarter, 24 %, were categorized into low spirituality, 49 % were classified into medium, and 27 % were classified into high spirituality (see Fig. 1). Using Chi-square analyses, religion/spirituality was also shown to be significantly associated with SPU (see Table 2).
Fig. 1.
Religion/spirituality
Unadjusted Associations Predicting Simultaneous Polysubstance Use
In the unadjusted bivariate associations predicting SPU in men, those with high levels of religion/spirituality had 60 % decreased odds of SPU compared with men with low levels of religion/spirituality (see Table 3). There were no statistically significant differences between men with medium levels of religion/spirituality and those with low levels of religion/spirituality. Women with high and medium levels of religion/spirituality had 69 and 64 % reduced odds of SPU compared with women with low levels of religion/spirituality, respectively.
Table 3.
Unadjusted logistic regression predicting SPU (N = 632)
| Variables | Men (N = 349) |
Women (N = 283) |
||
|---|---|---|---|---|
| Odds ratios | 95 % Wald confidence limits | Odds ratios | 95 % Wald confidence limits | |
| High R/S vs. low | 0.40 | 0.20–.78 | 0.31 | 0.15–0.63 |
| Medium R/S vs. low | 0.65 | 0.36–1.18 | 0.36 | 0.19–0.63 |
| Low R/S | 1.00 | − | 1.00 | − |
| African-American vs. non-African-American | 0.98 | 0.62–1.56 | 0.50 | 0.30–0.82 |
| 25 yrs. or younger vs. 26+ | 1.85 | .98–3.50 | 3.16 | 1.59–6.28 |
| High-school diploma or less vs. more than high school | 1.29 | 0.78–2.13 | 1.14 | 0.69–1.90 |
| 3+ Children vs. 2 or less | 1.36 | 0.77–2.40 | .65 | 0.40–1.05 |
| Used Rx opioids/pain medicines without a prescription vs. none | 3.04 | 1.79–5.18 | 1.97 | 1.18–3.26 |
| Never been married vs. married or once married | 1.446 | 0.91–2.30 | 2.08 | 1.28–3.37 |
| Arrest (4+) vs. never | 1.79 | 0.95–3.36 | 2.73 | 1.47–5.09 |
| Arrested (1–3) vs. never | 1.77 | 0.83–3.75 | 1.65 | .94–2.90 |
| Never been arrested | 1.00 | − | 1.00 | − |
| Pill for everything vs. no pill for everything | 1.68 | .96–2.94 | 0.70 | 0.41–1.16 |
| 3+ Sex partners in past 12 months vs. <3 | 2.12 | 1.13–4.00 | 3.11 | 1.49–6.53 |
There were several covariates that were significantly related to SPU in the models. Men who either had three or more sex partners or used prescription opioids without aprescription in the past 12 months had 2.12 and 3.04 times the odds of SPU, respectively, than their counterparts. The latter was the strongest effect in our model for men. Interestingly, a trend toward SPU was also evident for men who grew up believing that there was a pill for everything compared with men who did not believe that. A trend toward SPU was also seen in men who had four or more arrests and who were between the ages of 18 and 25 compared with their counterparts. Since these variables marginally missed significance, they may be clinically meaningful and were retained in the adjusted models due to the potential importance of these factors. Age, race, and education were not significant predictors of SPU in men in the unadjusted model.
Regarding women, those who were African-American had 50 % decreased odds of SPU than women who were not African-American, while younger women had 3.16 times increased odds of engaging in SPU than those who were older. Arrest history was also a statistically significant predictor of SPU in the unadjusted model, with women arrested 4+ times having nearly three times the odds of SPU compared with women who had never been arrested. Women who either had 3+ sex partners in the past 12 months, used prescription opioids without a prescription in the past 12 months, or had never married had 3.11, 1.97, and 2.08 times the odds of SPU, respectively, compared with their counterparts. Educational status and growing up with a belief that there was a pill for everything were not significantly associated with SPU among women.
Adjusted Associations Predicting Simultaneous Polysubstance Use
In the adjusted multivariate model predicting SPU in men, those with high levels of religion/spirituality had 63 % decreased odds of SPU compared with men with low levels of religion/spirituality, even when controlling for the various demographic and behavioral factors (see Table 4). Medium levels of religion/spirituality were not related to SPU among men. Several covariates showed significant relationships with SPU in the adjusted model. For example, 4+ arrests and three or more partners were associated with increased odds of SPU (AOR 2.21, 2.11). Men who used prescription opioids without a prescription also had increased odds of SPU compared with men who did not engage in that behavior (AOR 2.47). There was a trend for men who grew up with a belief that there was a pill for everything to have increased odds of SPU. Race, marital status, and education were not significant predictors of SPU in men in the adjusted model.
Table 4.
Adjusted multivariate logistic regression predicting SPU (N = 632)
| Variables | Men (N = 349) |
Women (N = 283) |
||
|---|---|---|---|---|
| Odds ratios | 95 % Wald confidence limits | Odds ratios | 95 % Wald confidence limits | |
| High R/S vs. low | 0.37 | 0.18–.78 | 0.42 | 0.19–0.95 |
| Medium R/S vs. low | 0.62 | 0.32–1.20 | 0.38 | 0.19–0.78 |
| Low R/S | 1.00 | – | 1.00 | – |
| African-American vs. non-African-American | 0.87 | 0.50–1.51 | 0.32 | 0.16–0.65 |
| 25 years or younger vs. 26+ | 1.66 | .79–3.49 | 1.56 | .64–3.83 |
| 3+ children vs. 2 or less | – | – | .96 | 0.52–1.78 |
| Used Rx opioids/pain medicines without a prescription vs. none | 2.47 | 1.38–4.41 | 1.49 | 0.82–2.70 |
| Never been married vs. married or once married | – | – | 2.13 | 1.08–4.20 |
| Arrest (4+) vs. never | 2.21 | 1.01–4.85 | 5.00 | 2.33–10.74 |
| Arrested (1–3) vs. never | 2.08 | 0.90–4.83 | 2.94 | 1.49–5.80 |
| Never been arrested | 1.00 | – | 1.00 | – |
| Pill for everything vs. no pill for everything | 1.73 | 0.95–3.14 | – | – |
| 3+ sex partners in past 12 months vs. <3 | 2.11 | 1.08–4.12 | 1.90 | 0.83–4.37 |
Variable not included in model due to a lack of significance in unadjusted model
Regarding women, the adjusted multivariate model predicting SPU controlling for demographic and behavioral factors revealed that those with high levels of religion/spirituality had 58 % reduced odds of SPU use compared with women with low levels. Furthermore, those with medium levels of religion/spirituality had 62 % reduced odds of SPU compared with women with low levels. Additionally, those who were African-American had 68 % decreased odds of SPU compared with those who were not African-American, while those who were never married had increased odds of engaging in SPU compared with those who were married (AOR 2.13). Arrest history continued to be significantly associated with SPU in the adjusted model. Women who were arrested 1–3 or 4+ times had significantly higher odds of SPU than women who had never been arrested (AOR 2.94 and 5.00). Age, educational status, growing up with a belief that there was a pill for everything, and 3+ sex partners in the past 12 months were not significant predictors of SPU in the multivariate model for women.
Discussion
In these analyses, we explored the association between religion/spirituality and SPU among opioid users by gender. Results supported our first hypothesis that religion/spirituality was associated with decreased odds of SPU. Overall, respondents with high levels of religion/spirituality had lower odds of SPU. Our second hypothesis, that this relationship would be more profound in men, was not supported. Though there were no significant differences in religion/spirituality by gender, significant gender differences in the association between religion/spirituality and SPU were evident. Men with high religion/spirituality had a substantial decrease in odds of SPU compared with men with low levels, while women with high and medium levels of religion/spirituality had substantial decreases in odds of SPU compared with women with low levels. Thus, we can infer that religion/spirituality was more beneficial to women than men in these analyses.
Other results yielded some expected and unexpected findings. Since African-Americans have been shown to have decreased odds of drug use when compared to non-African-Americans (Newcomb et al. 2014; Valdiserri et al. 2014), it was not surprising that African-American women had decreased odds of SPU when compared to non-African-American women. However, it was surprising that that this trend existed, but was not statistically significant. Furthermore, young adults also have been shown to be at elevated risk for drug use in other studies (Haggerty et al. 2015; Kerridge et al. 2015; Wong et al. 2013); however, our findings did not indicate this increased risk of SPU associated with being younger in the adjusted model, though this was evident in the bivariate and unadjusted association. While other studies have found links between education level and drug use (Boden et al. 2006), our study did not find any such association. These discrepancies may in part be due to the fact that this sample was comprised of substance users. Different results may have been found if non-substance-using participants were also included in this sample, as studies show that this population has higher degree attainment then substance users (Maggs et al. 2015; Boden et al. 2006).
Another interesting finding in our study was that among men, those who responded yes to the question "Did you grow up thinking there was a pill for everything?" showed a trend toward increased odds of SPU compared with men who did not in the unadjusted and adjusted models; however, this trend was not even found among women in the unadjusted model. This finding in men may support the self-medication theory. Individuals who believe that there is a pill for everything may misuse prescription opioids and other illegal substances in adulthood to cope with problems. A positive relationship between religion/spirituality and increased problems in life has been reported (Diener et al. 2011), and both factors have been associated with drug use (Moscati and Mezuk 2014). Further evidence is needed to support this idea.
In the multivariate regression model, arrest history was shown to be associated with SPU for both men and women. This was expected since those involved in the criminal justice system have also been shown to be at higher risk for drug use (Harner and Riley 2013). However, this association differed in strength between the genders. Men who had been arrested four or more times had twice the odds of SPU than men who did not reach that threshold. In contrast, women who had been arrested 1–3 times or four or more times had nearly three and five times the odds of SPU respectively, than women who had never been arrested. Lastly, risky sexual behaviors such as multiple sex partners have also been shown to be associated with drug use (Dyer et al. 2013; Islam et al. 2013; Chorba et al. 2012). Men who had three or more sex partners in the past 12 months had twice the odds of engaging in SPU than men who had less than three sexual partners in the past 12 months; however, this association was not found among women.
Limitations and Strengths
This study, as with any study, is not without limitations. A main limitation lies in the fact that this analysis is cross-sectional and cannot establish temporal relationships. Participants were not selected at random, which indicates that the findings of the study may not be generalizable to all those who engage in SPU. Further in-depth, longitudinal research in representative samples is needed to confirm these findings. Additionally, the study relied on self-report data on a sensitive topic and may be prone to the social desirability bias. However, strengths featured in these analyses include a rich dataset on a heavily understudied population of drug users, a large sample of substance users, and the evaluation of an abbreviated measure of religion/spirituality. Assessing personal relationships with a higher power, attendance at religious events, and advice seeking from religious leaders may be a more holistic way to capture religion/spirituality.
Conclusion
Though prior research has shown religion/spirituality to be helpful in promoting healthy behaviors, incorporation of this element in practice is limited (Elkonin et al. 2014). This study provides further evidence of the association between religion/spirituality and reduced odds of drug use even in a very risky subpopulation of drug users: those who engage in SPU. Furthermore, this analysis suggests that the association between religion/spirituality and the reduced odds of SPU is more profound in women than in men. Future drug prevention and interventions, especially those targeting females, should consider incorporating religious and spiritual components to potentially decrease SPU.
Acknowledgments
This study was funded by the McKnight Doctoral Fellowship (Abenaa Acheampong), R01DA20791 (PI: Cottler) and the Fogarty International Centre Indo-US Training Program in Non-Communicable Diseases (Grant No. D 43-TW009120; Sonam O Lasopa, Fellow; PI: Cottler). The authors also acknowledges the UF Department of Epidemiology, College of Medicine, College of Public Health and Health Profession, and all the participants in this study.
References
- Benotsch EG, Koester S, Luckman D, Martin AM, & Cejka A (2011). Non-medical use of prescription drugs and sexual risk behavior in young adults. Addictive Behaviors, 36(1/2), 152–155. [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Zimmerman R, Cathers L, McNulty S, Pierce J, Heck T, et al. (2013). Non-medical use of prescription drugs, polysubstance use, and mental health in transgender adults. Drug and Alcohol Dependence, 132(1/2), 391–394. doi: 10.1016/j.drugalcdep.2013.02.027. [DOI] [PubMed] [Google Scholar]
- Billioux VG, Sherman SG, & Latkin C (2014). Religiosity and HIV-related drug risk behavior: A multidimensional assessment of individuals from communities with high rates of drug use. Journal of Religion and Health, 53(1), 37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, & Horwood L (2006). Illicit drug use and dependence in a New Zealand birth cohort. Australian and New Zealand Journal of Psychiatry, 40(2), 156–163. [DOI] [PubMed] [Google Scholar]
- Cassidy TA, DasMahapatra P, Black RA, Wieman MS, & Butler SF (2014). Changes in prevalence of prescription opioid abuse after introduction of an abuse-deterrent opioid formulation. Pain Medicine, 15(3), 440–451. doi: 10.1111/pme.12295. [DOI] [PubMed] [Google Scholar]
- Cheney AM, Curran GM, Booth BM, Sullivan SD, Stewart KE, & Borders TF (2014). The religious and spiritual dimensions of cutting down and stopping cocaine use a qualitative exploration among African Americans in the south. Journal of Drug Issues, 44(1), 94–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorba T, Fletcher F, Hennessey K, Kroeger K, Lansky A, Leichliter J, et al. (2012). Integrated prevention services for HIV infection, viral hepatitis, sexually transmitted diseases, and tuberculosis for persons who use drugs illicitly: Summary guidance from CDC and the US Department of Health and Human Services. US Department of Health and Human Services, Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- Diener E, Tay L, & Myers DG (2011). The religion paradox: If religion makes people happy, why are so many dropping out? Journal of Personality and Social Psychology, 101(6), 1278–1290. doi: 10.1037/a0024402. [DOI] [PubMed] [Google Scholar]
- Dyer TP, Regan R, Wilton L, Harawa NT, Wang L, & Shoptaw S (2013). Differences in substance use, psychosocial characteristics and HIV-related sexual risk behavior between Black men who have sex with men only (BMSMO) and Black men who have sex with men and women (BMSMW) in six US cities. Journal of Urban Health, 90(6), 1181–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkonin D, Brown O, & Naicker S (2014). Religion, spirituality and therapy: Implications for training. Journal of Religion and Health, 53(1), 119–134. doi: 10.1007/s10943-012-9607-8. [DOI] [PubMed] [Google Scholar]
- Gmel G, Mohler-Kuo M, Dermota P, Gaume J, Bertholet N, Daeppen J, et al. (2013). Religion is good, belief is better: Religion, religiosity, and substance use among young Swiss men. Substance Use and Misuse, 48(12), 1085–1098. doi: 10.3109/10826084.2013.799017. [DOI] [PubMed] [Google Scholar]
- Haggerty KP, Skinner ML, Catalano RF, Abbott RD, & Crutchfield RD (2015). Long-term effects of staying connected with your teen on drug use frequency at age 20. Prevention Science, 16(4), 538–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harner HM, & Riley S (2013). The impact of incarceration on women’s mental health responses from women in a maximum-security prison. Qualitative Health Research, 23(1), 26–42. [DOI] [PubMed] [Google Scholar]
- Hobern K (2014). Religion in sexual health: A staff perspective. Journal of Religion and Health, 53(2), 461–468. doi: 10.1007/s10943-012-9650-5. [DOI] [PubMed] [Google Scholar]
- Islam MM, Topp L, Conigrave KM, Haber PS, White A, & Day CA (2013). Sexually transmitted infections, sexual risk behaviours and perceived barriers to safe sex among drug users. Australian and New Zealand Journal of Public Health, 37(4), 311–315. [DOI] [PubMed] [Google Scholar]
- Kerridge BT, Saha TD, Chou SP, Zhang H, Jung J, Ruan WJ, et al. (2015). Gender and nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. Drug and Alcohol Dependence, 156, 47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luquis R, Brelsford G, & Rojas-Guyler L (2012). Religiosity, spirituality, sexual attitudes, and sexual behaviors among college students. Journal of Religion and Health, 51(3), 601–614. doi: 10.1007/s10943-011-9527-z. [DOI] [PubMed] [Google Scholar]
- Maggs JL, Staff J, Kloska DD, Patrick ME, O’Malley PM, & Schulenberg J (2015). Predicting young adult degree attainment by late adolescent marijuana use. Journal of Adolescent Health, 57(2), 205–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore E, Berkley-Patton J, & Hawes S (2013). Religiosity, alcohol use, and sex behaviors among college student-athletes. Journal of Religion and Health, 52(3), 930–940. doi: 10.1007/s10943-011-9543-z. [DOI] [PubMed] [Google Scholar]
- Moscati A, & Mezuk B (2014). Losing faith and finding religion: Religiosity over the life course and substance use and abuse. Drug & Alcohol Dependence, 136, 127–134. doi: 10.1016/j.drugalcdep.2013.12.018. Epub 2014 Jan 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss H, Chen CM, & Yi H (2014). Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug and Alcohol Dependence,. doi: 10.1016/j.drugalcdep.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Newcomb ME, Birkett M, Corliss HL, & Mustanski B (2014). Sexual orientation, gender, and racial differences in illicit drug use in a sample of US high school students. American Journal of Public Health, 104(2), 304–310. doi: 10.2105/AJPH.2013.301702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’brien L, Denny S, Clark T, Flemming T, Teevale T, & Robinsom E (2013). The impact of religion and spirituality on the risk behaviours of young people in Aotearoa, New Zealand. Youth Studies Australia, 32(4), 25–37. [Google Scholar]
- Olthius JV, Darredeau C, & Barrett SP (2013). Substance use initiation: The role of simultaneous polysubstance use. Drug & Alcohol Review, 32(1), 67–71. doi: 10.1111/j.1465-3362.2012.00470.x. [DOI] [PubMed] [Google Scholar]
- Puffer E, Skalski L, & Meade C (2012). Changes in religious coping and relapse to drug use among opioid-dependent patients following inpatient detoxification. Journal of Religion and Health, 51(4), 1226–1238. doi: 10.1007/s10943-010-9418-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid-Arndt SA, Smith ML, Yoon D, & Johnstone B (2011). Gender differences in spiritual experiences, religious practices, and congregational support for individuals with significant health conditions. Journal of Religion, Disability & Health, 15(2), 175–196. doi: 10.1080/15228967.2011.566792. [DOI] [Google Scholar]
- Shacham E, & Cottler L (2010). Sexual behaviors among club drug users: Prevalence and reliability. Archives of Sexual Behavior, 39(6), 1331–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson DB, Cloud DS, Newman JL, & Fuqua DR (2008). Sex and gender differences in religiousness and spirituality. Journal of Psychology & Theology, 36(1), 42–52. [Google Scholar]
- Sofuoglu M, DeVito EE, Waters AJ, & Carroll KM (2013). Cognitive enhancement as a treatment for drug addictions. Neuropharmacology, 64, 452–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staton-Tindall M, Oser CB, Duvall JL, Havens JR, Webster J, Leukefeld CG, et al. (2008). Male and female stimulant use among rural kentuckians: The contribution of spirituality and religiosity. Journal of Drug Issues, 38(3), 863–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trenz RC, Scherer M, Duncan A, Harrell PT, Moleko A, & Latimer WW (2013). Latent class analysis of polysubstance use, sexual risk behaviors, and infectious disease among South African drug users. Drug and Alcohol Dependence, 132(3), 441–448. doi: 10.1016/j.drugalcdep.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdiserri R, Khalsa J, Dan C, Holmberg S, Zibbell J, Holtzman D, et al. (2014). Confronting the emerging epidemic of HCV infection among young injection drug users. American Journal of Public Health, 104(5), 816–821. doi: 10.2105/AJPH.2013.301812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkerson JJ, Smolensk D, Brady S, & Rosser BB (2013). Performance of the Duke Religion Index and the Spiritual Well-Being Scale in online samples of men who have sex with men. Journal of Religion and Health, 52(2), 610–621. doi: 10.1007/s10943-012-9594-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong CF, Silva K, Kecojevic A, Schrager SM, Bloom JJ, Iverson E, et al. (2013). Coping and emotion regulation profiles as predictors of nonmedical prescription drug and illicit drug use among high-risk young adults. Drug and Alcohol Dependence, 132(1), 165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]