Abstract
AIM
To compare the visual acuity (VA), comfort, and patient preference in a soft toric contact lens (TCL) versus soft spherical contact lens (SCL) in low astigmatic subjects during the contact lens (CL) trial.
METHODS
This subject-masked, block randomized, 2×2 crossover study recruited 40 neophyte subjects (80 eyes) aged 18 to 33y with astigmatism in the range of 0.75-1.25 D with or without spherical power from -6.00 D to +6.00 D. The participants were scheduled for two days CL trial and were fitted with the best-fit SCL and TCL. After 4h of wear, they were assessed objectively for high contrast VA and subjective vision, comfort, and preference.
RESULTS
The responses of 36 subjects (response rate 90%) with a mean age of 23.02±2.97y (range 18 to 33y) were analyzed. One-line improvement of monocular VA in the logMAR chart was reported to TCL as compared to SCL (-0.044±0.06 vs 0.04±0.03 logMAR, P=0.01) but the binocular vision remained similar (-0.12±0.07 vs -0.14±0.04 logMAR, P=0.38). Subjects felt a noticeable difference in clarity when shifted to TCL as compared to the SCL. The satisfaction with vision (vision quality) was significantly better with TCL (P=0.03). The fatigue with TCL was graded less at 2.5±0.6, compared to SCL at 4.6±1.3 (P=0.04). Thirty-three participants (91.6%) preferred to use contact lens of which 26 participants (79%) preferred TCL.
CONCLUSION
The findings suggest that VA and comfort are better with TCL as compared to SCL which is only observed if the patient was offered both offering SCL with spherical equivalent power alone as the first option can mislead the practitioner; TCL trial should be the first choice of the lens in low-to-moderate astigmatism.
Keywords: astigmatism, comfort, spherical contact lens, toric contact lens, visual acuity
INTRODUCTION
Astigmatism is a common refractive error. Approximately 47% of astigmatic patients have an error of >0.75 diopters (D) cylinders and almost one-third of potential contact lens (CL) wearers require astigmatic correction[1]. However, eye care practitioner (ECP) prescribes soft toric contact lenses (TCL) only for approximately 25% of patients, ranging from 6% of lenses in Russia to 48% in Portugal[2]. Considering a cutoff of 0.75 D, 44.8% of patients would need TCL in India[3].
For patients with low to moderate astigmatism, ECP prescribe astigmatic glasses. However, CL wearers are fitted with a soft spherical contact lens (SCL) in the form of a spherical equivalent. Shreds of evidence from industry sales records show that TCL constitutes less than 20% of CL sales in India. Possibly due to the easy availability of spherical trails, easy fitting procedures, relatively lower cost, the common practice is to first try a spherical equivalent and recommend spherical equivalent powers in low astigmatic patients. In the absence of large, randomized clinical studies, real-world, patient perspective and prospective studies could help ECPs choose between TCL and SCL for low astigmatic potential CL patients.
This study aimed to compare the subjective and objective responses of TCL and SCL trials in individuals with low astigmatism. The results were expected to give a better understanding of whether TCL trials are necessary to provide potential CL users with a better choice of refractive correction for low astigmatism.
SUBJECTS AND METHODS
Ethical Approval
This cross-sectional study was approved by the Institutional Ethical Committee of Amity University, Gurugram, India, and adhered to the tenets of the Declaration of Helsinki (2008). It was conducted between January and March 2016 at the Amity Optometry Clinic. Informed consent was obtained prior to the conduct of the study.
Patient Selection and Procedure
The study enrolled 40 (80 eyes) non-presbyopic neophytes (who had not used CL previously) participants aged 18 to 40y. Their non-cycloplegic ocular refraction at the corneal plane had to be between 0.75 to 1.25 D cylinders with/without spherical power up to ±6.00 D. Eligible participants underwent a comprehensive eye examination, and participants contraindicated for CL wear were excluded.
For the subjects eligible, two sets of CLs are ordered based on empirical calculation: one set of SCL (Acuvue Oasys, Johnson and Johnson) and another set of TCL (Acuvue Oasys for astigmatism, Johnson and Johnson), and subjects were scheduled for two days trail visit. Block randomization was performed to select the type of lenses to be fitted on each visit. The subjects were blinded to the type of lens they wore on, the two different visits, but the examiner could not be blinded due to the nature of the study. The pre-fitting assessment, fitting (insertion and removal), and post fitting assessment were completed following a standardized protocol by a trained optometrist for consistency. After 20min of inserting the lens, the lens fitting was assessed by judging the coverage, centration, and movement in SCL and additionally rotation, and stability in the TCL. On achieving the ideal fit, subjects were asked to continue to wear the CLs for the day to carry out their routine activities and return to the clinic for evaluation after 4h of wear. On return to the clinic, visual acuity (VA) was tested with a high contrast logMAR chart and over-refraction was performed using the retinoscope (Heine beta 200).
Following the examination, a validated questionnaire was provided for each lens to the subjects in which they were asked to subjectively rate their quantity of vision (monocularly), quality of vision (satisfaction with vision), and comfort in each eye on a Likert scale of 1 (very good) to 5 (very bad). Subjects also rated fatigue/eyestrain after CL on a scale of 0 (no fatigue) to 10 (very fatigue). On completing the questionnaire, the lenses were removed and discarded. The crossover portion of the study with the other lens was completed on a different day depending on the subject's convenience but within one week of the first trial. However, on both visits uniform procedures were followed.
Statistical Analysis
Sensitivity power analysis using a computer program (Gpower 3.0) showed that the effect size between the two groups was 1.20 (large) with power (1-β) set at 0.80 and α=0.05, two-tailed. The sample size taken was considered adequate for the study. The statistical analysis was performed using Statistical Package for Social Science (SPSS) version 21. Descriptive test was performed for demographic data, and nonparametric Wilcoxon tests were used to compare the subjective and objective responses of the participants between the two lens trials. P values of less than 0.05 were considered significant.
RESULTS
A total of 40 participants (80 eyes) were initially recruited for the study. With a response rate of 90%, the responses of 36 subjects (17 males and 19 females) with a mean age of 23.02±2.97y (18-33y) were evaluated. The characteristics of the subjects recruited are as shown in Table 1.
Table 1. Demographic and clinical characteristics of the subjects.
| Characteristics | Male (n=17) | Female (n=19) | Total (n=36) |
| Age (y) | 23.64±3.19 | 22.47±2.91 | 23.02±2.97 |
| Spherical power (range), D | -1.70±1.64 (0.00 to -5.75) | -0.33±2.25 (-4.00 to +6.00) | -1.33±2.09 (-4.00 to +6.00) |
| Cylindrical power (range), D | -0.88±0.14 (-0.75 to -1.25) | -0.88±0.19 (-0.75 to -1.25) | -0.88±0.17 (-0.75 to -1.25) |
| BCVA with glasses, logMAR | 0.022±0.006 | 0.020±0.008 | 0.021±0.007 |
BCVA: Best-corrected visual acuity; logMAR: Logarithmic minimum angle of resolution.
mean±SD
An average of 1.12±0.40 lenses was required to achieve an optimal fit for SCL, and took 1.42±0.33 lenses for TCL. A rotation of lesser than 5 degrees in the primary gaze with the TCL was considered acceptable. The monocular VA with SCL and TCL was 0.04±0.03 and -0.044±0.06 logMAR, respectively. The improvement in monocular VA with TCL compared to the SCL was approximately one line in the logMAR chart (P=0.01). However, the binocular VA remained similar: -0.14±0.04 and -0.12±0.07 logMAR for SCL and TCL, respectively (P=0.38). Over-refraction revealed a significantly higher myopic spherical component of -0.08±0.10 D in SCL compared to 0.04±0.13 D in TCL (P<0.01). The mean difference between TCL and SCL on the monocular vision quantity rated was 0.683±0.051 (P=0.02). After four hour of CL wear, subject-reported responses for monocular vision quantity (clarity of vision monocularly) and vision quality (satisfaction) were analyzed and presented in Figure 1.
Figure 1. Subject-reported responses rated for visual acuity.
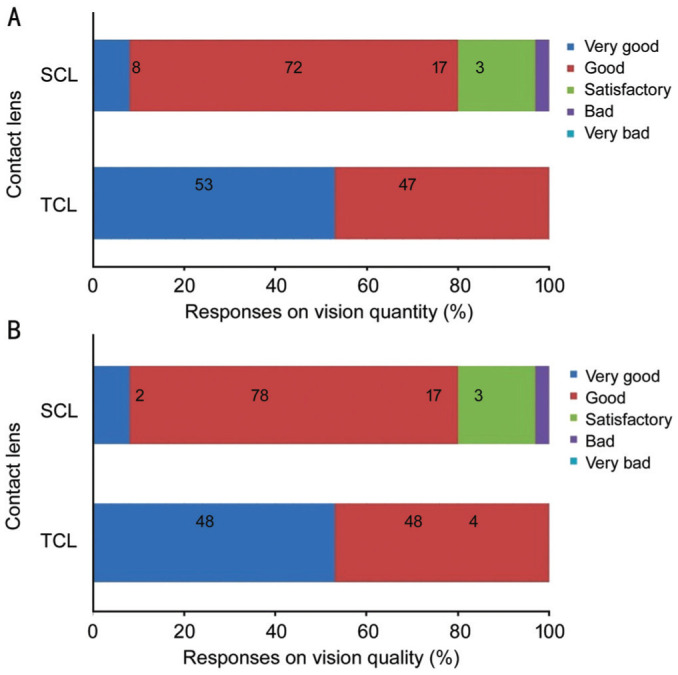
A: Responses on vision quantity; B: Responses on vision quality.
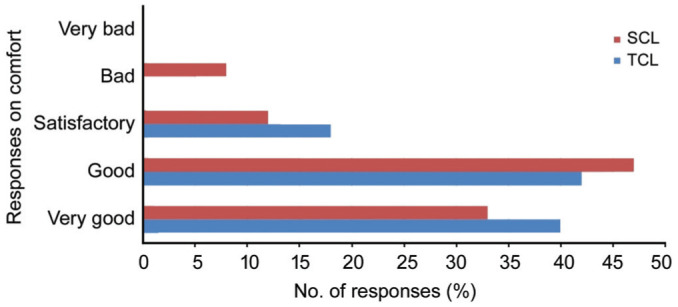
Subjects felt a noticeable difference in clarity when shifted to TCL as compared to the SCL. The satisfaction with vision (vision quality) was significantly better with TCL (P=0.03). Both the lenses were graded to be almost equally comfortable on wear (P=0.77; Figure 2). The fatigue with TCL was rated 2.5±0.6, while it was graded significantly higher with SCL at 4.6±1.3 (P=0.04). Thirty-three participants (91.6%) preferred to use CL for their refractive correction. Out of them, 26 participants (79%) reported a preference for TCL while the others choose SCL.
Figure 2. Subjective response on comfort with SCL and TCL.
DISCUSSION
Anecdotal evidence reports that ECP and users are fairly satisfied with compensated spherical powers in low astigmatism. In India, it is a common practice to mask small cylindrical errors and prescribe SCL due to lesser cost. This study tried to assess the visual parameters and preference of TCL compared to SCL in low-to-moderate astigmatic subjects.
In this study, both objective and subjective findings favoured the use of TCL in low astigmatism. While the SCL was tried, 80% of the subjects ranked their vision as ‘very good’ and ‘good’; however, this percentage shoot-up to 100% when they were fitted with TCL. The improvements in subjective vision reported here are consistent with previous reports that highlighted the vision benefits of prescribing TCL[4]–[6]. Offering the SCL first gave a false impression that the quality is satisfactory. The subject realized the improvement only after he wore TCL. The reaction was immediate, and the subjects could appreciate it immediately on insertion of the CL.
VA improved monocularly by one-line logMAR with TCL as compared to the SCL, reporting similar outcomes to those studied elsewhere[7]. These findings justify the assumption of the acceptance of the spherical soft lens by practitioners. However, the findings after both CL trails reveal that the optimal vision should be reported only after trying TCL. The monocular response rate of patients was better with TCL as compared to SCL on vision quantity compared to the binocular quantity. The subjects also reported a better quality of vision (satisfaction with vision) with the TCL as compared to SCL as revealed in a previous study[8]. This could be attributed to improved vision with TCL and could be a determinant for TCL preference.
Subjective results showed no significant difference in the initial comfort between the two choices, consistent with previous literature[6]. Both TCL and SCL used in this study used the same material (senofilcon A), water content (38%), and surface treatment of the lens. The study disagrees with the associations of TCL with discomfort due to lens rotation and complex fitting. The study found that the subjective response fatigue was more with SCL than TCL. Electromyography-measured eyestrain was also determined that TCL wearers have reduced eye strain than SCL users[9]. Squeezing of eyes and constant strain to focus best could be demonstrated in four hours of trial itself. This was the visual comfort that led to satisfaction.
CL was the choice of refractive correction for 91.6% of participants. As expected, the preference of TCL over SCL 80%, however, higher than those reported elsewhere[6]–[7]. These higher preferences could be attributed to our study subjects (university students) where the visual requirements and acceptance are different from those of the older population. Overall results show that TCL provides better vision and less ocular fatigue for the first-time CL users. ECP should perform TCL trials and not judge the acceptance of spherical equivalent lens trails. The spherical equivalent trial misleads ECP in low astigmatic CL recommendation. Use of TCL exhibit better overall driving performance and driving-specific visual abilities compared to spherical lenses[10]. Moreover, correcting astigmatism with CL is associated with improved quality of life[7]. The complexity of fitting, high cost to patients, and poor availability of trials are perceived barriers in prescribing toric lenses and there is a need to address the barriers. Drop out in patients with residual astigmatism is evident and correct CL recommendation by ECP could prevent dropout.
The current study's is limited using one type of lenses for the trails. The TCL designs and stabilization techniques may confound the subjective responses. The participants were not introduced to the use of CL solution, insertion and removal techniques and CL maintenance, which could interfere the CL preference. The other limitations include the number of participants and non-blinding of examiner. Future studies could be address these limitation with randomised contralled trails on a larger group of subjects.
The subjective and objective results suggest that VA and comfort are better with TCL as compared to SCL in low-to-moderate astigmatism. The acceptance of CL was high, and subjects preferred TCL over SCL. Practitioners should recommend TCL as the first option to astigmatic patients and not attempt spherical equivalent trial to judge the acceptance. Masking astigmatism and prescribing spherical equivalent trial can mislead ECPs in low astigmatic CL recommendation.
Acknowledgments
The authors acknowledge the management and faculties of the Department of Optometry and Vision Science, Amity University Gurugram for the technical support to conduct this study. We also thank Mr. Dhanapati Sharma, Lecturer, Royal University of Bhutan for reviewing our manuscript and editing language.
Conflicts of Interest: Chaudhry M, None; Sah SP, None; Sharma IP, None; Mondal S, None.
REFERENCES
- 1.Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011;37(1):20–25. doi: 10.1097/ICL.0b013e3182048fb9. [DOI] [PubMed] [Google Scholar]
- 2.Morgan PB, Efron N, Woods CA, International Contact Lens Prescribing Survey Consortium An international survey of toric contact lens prescribing. Eye Contact Lens. 2013;39(2):132–137. doi: 10.1097/ICL.0b013e318268612c. [DOI] [PubMed] [Google Scholar]
- 3.Hashemi H, Fotouhi A, Yekta A, Pakzad R, Ostadimoghaddam H, Khabazkhoob M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J Curr Ophthalmol. 2018;30(1):3–22. doi: 10.1016/j.joco.2017.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sulley A, Young G, Lorenz KO, Hunt C. Clinical evaluation of fitting toric soft contact lenses to current non-users. Ophthalmic Physiol Opt. 2013;33(2):94–103. doi: 10.1111/opo.12028. [DOI] [PubMed] [Google Scholar]
- 5.Richdale K, Berntsen DA, Mack CJ, Merchea MM, Barr JT. Visual acuity with spherical and toric soft contact lenses in low-to moderate-astigmatic eyes. Optom Vis Sci. 2007;84(10):969–975. doi: 10.1097/OPX.0b013e318157c6dc. [DOI] [PubMed] [Google Scholar]
- 6.Cho P, Cheung SW, Charm J. Visual outcome of Soflens Daily Disposable and Soflens Daily Disposable for Astigmatism in subjects with low astigmatism. Clin Exp Optom. 2012;95(1):43–47. doi: 10.1111/j.1444-0938.2011.00649.x. [DOI] [PubMed] [Google Scholar]
- 7.Cox SM, Berntsen DA, Bickle KM, Mathew JH, Powell DR, Little BK, Lorenz KO, Nichols JJ. Efficacy of toric contact lenses in fitting and patient-reported outcomes in contact lens wearers. Eye Contact Lens. 2018;44(Suppl 1):S296–S299. doi: 10.1097/ICL.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 8.Gaib SN, Vasudevan B. Low toric soft contact lens acceptance study. Cont Lens Anterior Eye. 2015;38(3):194–198. doi: 10.1016/j.clae.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Berntsen DA, Cox SM, Bickle KM, Mathew JH, Powell DR, Seidman SH, Little BK, Lorenz KO, Nichols JJ. A randomized trial to evaluate the effect of toric versus spherical contact lenses on vision and eyestrain. Eye Contact Lens. 2019;45(1):28–33. doi: 10.1097/ICL.0000000000000528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cox DJ, Banton T, Record S, Grabman JH, Hawkins RJ. Does correcting astigmatism with toric lenses improve driving performance? Optom Vis Sci. 2015;92(4):404–411. doi: 10.1097/OPX.0000000000000554. [DOI] [PubMed] [Google Scholar]


