Abstract
AIM
To investigate the suitability of a modified Hughes procedure, which consists of conjunctival flap with auricular cartilage grafting in reconstructing large full thickness upper and lower eyelid defect.
METHODS
Patients with full thickness eyelid carcinoma involving more than 50% margin length who underwent surgical resection were retrospectively reviewed in the study. The defects were reconstructed using conjunctival flap with auricular cartilage grafting, covered with myocutaneous flap above. Followed-up time ranged from 12 to 24mo. Outcomes were classified as “good”, “fair”, and “poor” by evaluating the margin appearance, eyelid appearance, and complications.
RESULTS
A total of 42 patients were enrolled in the study (26 males, 16 females, mean age, 68.6±7.7y, range: 53 to 82y). The mean defect widths measured 23.2±2.9 mm (range, 17 to 28 mm). The mean posterior lamellar defect height was 5.5±1.3 mm (4 to 8 mm). Thirty-seven patients had a “good” outcome (88.1%), 5 patients had a “fair” outcome (11.9%), and no one had a “poor” outcome.
CONCLUSION
Conjunctival flap with auricular cartilage grafting and myocutaneous flap grafting is an effective procedure in reconstructing large full thickness upper and lower eyelid defect. It can not only achieve satisfied reconstruction, but also preserve intact tarsal plate of the opposite eyelid, avoiding retraction or entropion.
Keywords: auricular cartilage grafting, conjunctival flap, full thickness eyelid defect, Hughes procedure
INTRODUCTION
Repairing conjunctival and tarsal defect is one of the key steps to achieve normal eyelid appearance and position in reconstructing large full thickness eyelid defect. Hughes procedure is commonly used under this situation. The risks of this procedure can include retraction, ectropion in reconstructed eyelids and entropion in opposite eyelids[1]–[3]. These complications may be due to insufficient obtained tarsus to cover the whole defect region, and disruption of lid stability by over harvesting of donor tarsus. Besides, Hughes procedure is not commonly used in upper eyelid reconstruction due to the limited height of lower lid tarsal plate-often not sufficient to repair upper lid tarsal defects sufficiently[3].
In this study, we designed a modified Hughes procedure using auricular cartilage as the substitute of tarsal plate combined with conjunctival flap to repair tarsal and conjunctival defect. After that, the anterior defect was covered by myocutaneous flap. The surgical outcomes are evaluated and discussed in detail.
SUBJECTS AND METHODS
Ethical Approval
The study followed the tenets of the Declaration of Helsinki and was approved by the Ethics committee of Eye Hospital of Wenzhou Medical University. Informed consents and clinical photograph publication permissions were obtained from all patients.
A retrospective chart review was performed for all patients undergoing eyelid defect reconstruction following carcinoma resection at the Eye Hospital of Wenzhou Medical University between January 2014 to September 2019. Patients with eyelid defect more than 50% of the entire eyelid margin length after eyelid carcinoma resection were enrolled in the study. Exclusion criteria were: 1) eyelid defect width less than 50% of the margin length; 2) intact tarsal plate or margin after tumor excision; 3) less than 12mo of follow-up; 4) orbital invasion by the eyelid tumor.
A total of 42 patients (42 eyelids) were enrolled in the study. The eyelid defects were reconstructed using conjunctival flap and auricular cartilage grafting as the posterior lamella. This was covered with local myocutaneous flap as the anterior lamella. Tarsorrhaphy was performed to secure the reconstructed margin to the opposite eyelid margin; the eye was then kept closed for 3mo. Follow-up visit was set at 1wk, 1, 3, 6, and 12mo. Patients followed-up for more than 12mo were enrolled as well. The eyelid appearance, margin position and appearance, scar formation and complications were evaluated and scored by 2 independent surgeons at the final follow-up visit. The margin position was recorded by margin reflex distance-1 (MRD1, vertical distance between the upper eyelid margin to the central pupillary light reflex) and margin reflex distance-2 (MRD2, vertical distance between central pupillary light reflex to the lower eyelid margin)[4]. The outcomes were graded as “good” with the score greater than or equal to 7, “fair” with the score between 5 to 6, and “poor” with the score less than or equal to 4 (Table 1).
Table 1. Eyelid reconstruction evaluating score rubric.
| Criteria | Points |
Score | ||
| 0 | 1 | 2 | ||
| Margin position | Noticeable retraction/ptosis, MRD more than 2 mm compared with contralateral eyelid | Mild retraction/ptosis, MRD between 1 to 2 mm compared with contralateral eyelid | No retraction/ptosis, MRD less than 1 mm compared with contralateral eyelid | |
| Margin appearance | No distinct margin | Notching, or noticeable thinning of margin | Distinct margin with smooth curve | |
| Lateral and medial canthal angle | Canthus disrupted | Rounded | Sharp and crisp | |
| Other complications | Noticeable entropion or ectropion | Mild entropion or ectropion | No entropion or ectropion | |
MRD: Marginal reflex distance (The distance between the corneal light reflex to the center of the eyelid margin).
The outcome measurements were analyzed by SPSS 19.0 software (USA). The pre and post MRD1/MRD2 were compared by paired-samples t-test (P<0.05 was considered statistically significant). Quantitative variables were presented as mean±standard deviation.
Surgical Procedure
The region of the carcinoma was marked and excised with the patient under local anaesthesia combined with sedation. Reconstruction started when the excision margin was confirmed negative by frozen section (Figure 1A-1B).
Figure 1. Clinical photos of the procedure of conjunctival flap combined with auricular cartilage grafting.
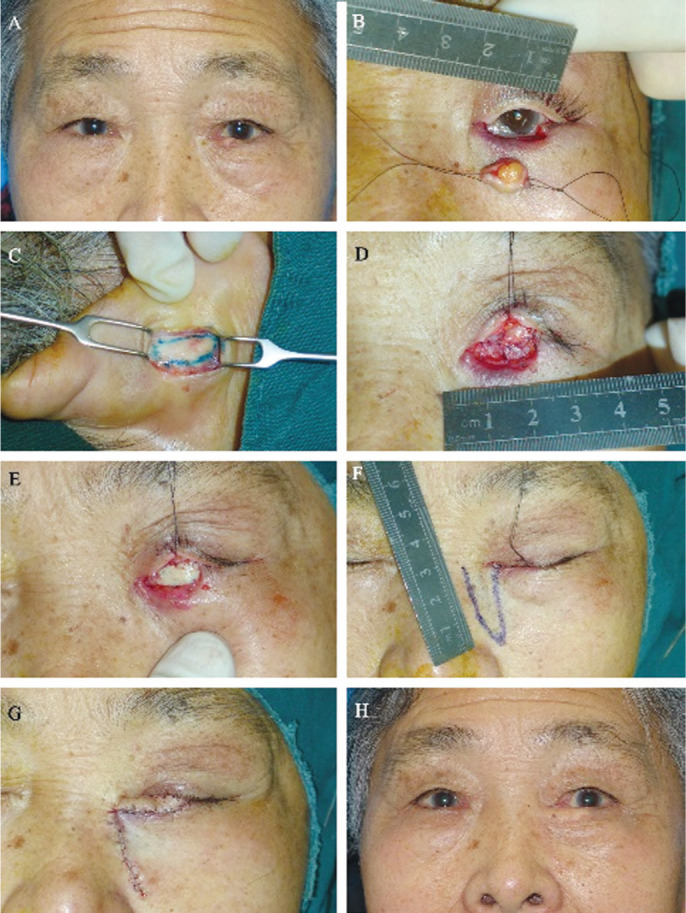
A: A 70-year-old woman presented with sebaceous carcinoma in left lower eyelid. B: The size of the posterior lamellar defect was 5×17 mm2 after complete excision. Part of the lower canaliculus was also excised. C: The auricular cartilage was exposed by a postauricular skin incision. D: The conjunctival flap of the upper eyelid was advanced and fixed with the residual conjunctiva of the defect region. The conjunctiva of the defect region was also dissected and advanced to facilitate the suture. E: The tarsal defect was repaired by the auricular cartilage. The residual lower canaliculus was intubated by a silicone tube to maintain the lacrimal passage free, and the tube was wrapped by a piece of lip mucosa to repair the canalicular defect. F: A triangular rotating myocutaneous flap was designed to repair the anterior lamellar defect. G: The immediate appearance of complete reconstruction. The reconstructed margin was fixed with the upper eyelid margin. H: The postoperative 12mo appearance of the reconstructed lower eyelid. There was no eyelid retraction, and the curve of the margin was smooth.
Auricular Cartilage Harvesting
About 1 to 2 mL of 2% lidocaine with 1:100 000 epinephrine was first injected to the posterior auricular region. The auricular cartilage graft was harvested from the conchal lateral wall through a post-auricular incision as a rectangular strip of the right ear (Figure 1C). The graft was then temporarily preserved in a mixture of gentamicin and normal saline. The auricular skin incision was closed by 5-0 absorbable subcutaneous suture (Vicryl, Johnson, USA) and 6-0 non-absorbable skin suture (Nylon, Lingqiao, China).
Conjunctival Flap Preparation and Auricular Cartilage Grafting
The opposite eyelid was first everted to expose the tarsus and conjunctiva. The boundary of the conjunctival flap was then marked along the edge of the tarsal plate. Injection of 1 to 2 mL of 2% lidocaine with 1:100 000 epinephrine assists in separating the conjunctiva from the underlying Müller's muscle in upper lid or lower eyelid retractor (LER) in lower lid. The conjunctival flap was then dissected towards the fornix above the Müller's muscle or LER until sufficient area was harvested. The conjunctival flap was advanced and fixed with the residual conjunctiva of the defect region by 6-0 absorbable sutures (Vicryl, Johnson, USA; Figure 1D). Then, the auricular cartilage was fashioned appropriately to fit the defect contour. The thickness and contour of cartilage was trimmed to fit the residual tarsus. The convex/concave side of the cartilage was partially incised to adjust to fit the curvature of eyeball. Then, the medial and lateral end of the cartilage were secured to the residual tarsus using 6-0 absorbable sutures (Vicryl, Johnson, USA; Figure 1E). Anterior lamellar defect was repaired depending on the width and height of the defect. In cases that defect area involved in upper eyelid, advanced blepharoplasty skin-muscle flap or lateral rotational myocutaneous flap was applied to cover the defect area. In lower eyelid defect repair, Tripier orbicularis myocutaneous flap, lateral rotational myocutaneous flap, or nasojugal myocutaneous flap was applied to achieve complete repair (Figure 1F). Tarsorrhaphy was then performed at the defect area: the opposite eyelid margin was split by gray line incision at a depth of 2 to 3 mm. Then the tarsal plate of opposite eyelid was stitched with the subcutaneous lamella of the reconstructed margin by 6-0 absorbable sutures (Vicryl, Johnson, USA), and the anterior lamella of opposite eyelid was stitched with the skin surface of the reconstructed margin by 6-0 non-absorbable sutures (Nylon, Lingqiao, China), respectively (Figures 1G, 2). Compressed bandage was applied for 2d; and the skin sutures were removed 7d after the surgery.
Figure 2. Diagrams of tarsorrhaphy following full thickness eyelid defect reconstruction.
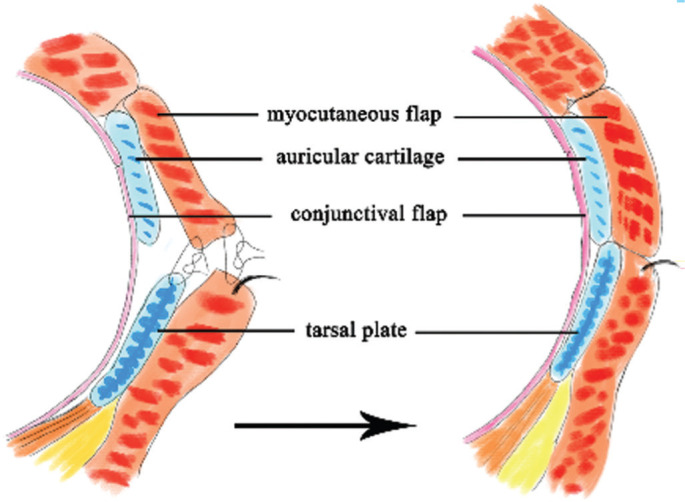
The donor eyelid margin was split by gray line incision at a depth of 2 to 3 mm. A 6-0 absorbable suture was applied to stitch the tarsal plate of donor eyelid with the subcutaneous lamella of the reconstructed margin. The anterior lamella of donor eyelid was stitched with the skin surface of the reconstructed margin by 6-0 nylon suture.
The eyelid margin division was performed under local anesthesia 3mo after surgery. The conjunctival flap was cut at 1 to 2 mm above the reconstructed margin and then advanced to cover the margin. The sutures were removed 7d after the division surgery.
RESULTS
From January 2014 to September 2019, a total of 42 eyelids (42 patients, 26 males and 16 females) were enrolled in the study, with a mean age of 68.6±7.7y (range: 53 to 82y). Causes included sebaceous carcinoma (27 eyelids, 64.3%), basal cell carcinoma (13 eyelids, 30.9%), and squamous cell carcinoma (2 eyelids, 4.8%). Thirty-one lower eyelids and 11 upper eyelids were involved. Patients were followed-up for 14.3±3.1mo (range: 12 to 24mo) without recurrence or metastasis. There were no statistical differences (sample t-test, 11 eyelids, t=-1.0, P=0.34) of MRD1 between the reconstructed upper eyelids and the contralateral upper eyelids in patients underwent upper eyelid reconstruction. In patients underwent lower eyelid reconstruction, the MRD2 of the operated eyelids was statistically larger (sample t-test, 31 eyelids, t=2.4, P=0.049) than that of the contralateral eyelids. At the last follow-up visit, assessment of surgical outcome showed 37 patients achieved “good” score (37 eyelids, score=7.1±0.2, Figures 1H, 3A), 5 patients were scored as “fair” (5 eyelids, score=5.5±0.5), and no one was scored as “poor” (Table 2). Four of the 5 patients with “fair” outcome underwent lower eyelid reconstruction. In cases with “fair” outcome, the mean marginal defect width was 25.1±2.1 mm (range: 21 to 28 mm), and the mean defect height was 5.1±1.4 mm (range: 5 to 7 mm), which were both larger than cases with “good” outcome. Two patients had rounded lateral canthus and mild lower eyelid retraction, two patients had notching of margin and mild lower eyelid retraction. The last one of the 5 patients had mild retraction and notching of margin in upper eyelid. (Figure 3B). There were no entropion, retraction, or other complications of the opposite eyelids observed during the follow-up period.
Figure 3. Clinical photos of patients underwent full thickness eyelid defect reconstruction with “good” outcome.
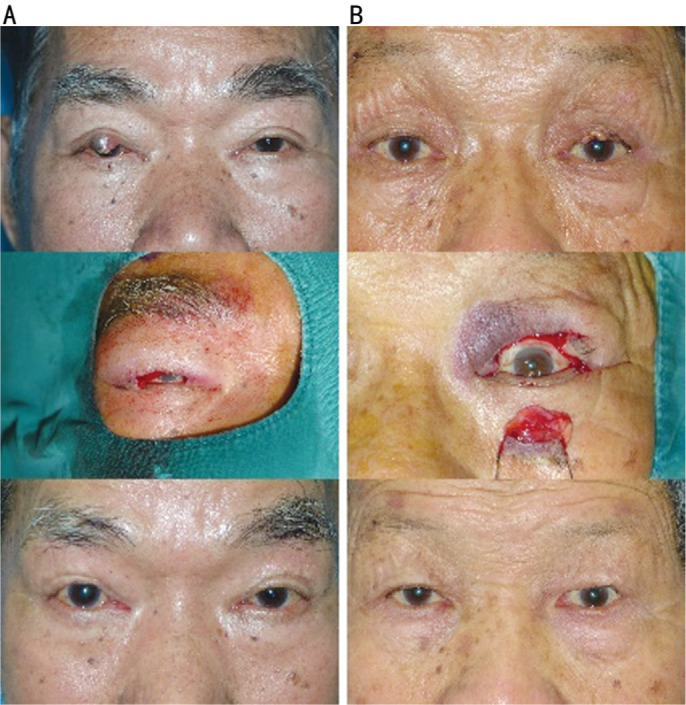
A: A 78-year-old man presented with sebaceous carcinoma in the right upper eyelid. The size of the defect area was 17×6 mm2 after the carcinoma resection. At the 12th month follow-up visit, the reconstructed upper eyelid had satisfied appearance and position. The outcome was graded as “good”. B: A 76-year-old man presented with sebaceous carcinoma in the left upper eyelid. The size of the defect area was 20×8 mm2 after complete resection. At the 12th month follow-up visit, the reconstructed upper eyelid had mild notching of margin and mild retraction at primary gaze. The outcome was graded as “fair”.
Table 2. Clinical features of patients underwent eyelid defect reconstruction.
| Characteristics | Value (mean±SD) |
| Marginal defect width (mm) | |
| Total (n=42) | 23.2±2.9 (17 to 28) |
| Upper eyelid (n=11) | 21.1±2.7 (17 to 25) |
| Lower eyelid (n=31) | 24.0±2.7 (20 to 28) |
| Defect height of posterior lamellar (mm) | |
| Total (n=42) | 5.5±1.3 (4 to 8) |
| Upper eyelid (n=11) | 6.3±1.5 (5 to 8) |
| Lower eyelid (n=31) | 5.1±0.9 (4 to 7) |
| MRD1a (mm) | |
| Reconstructed upper eyelids | 2.7±0.4 (2-3) |
| Contralateral upper eyelids | 2.8±0.3 (2-3) |
| MRD2b(mm) | |
| Reconstructed lower eyelids | 4.6±0.2 (4.5-5) |
| Contralateral lower eyelids | 4.5±0.3 (4-5) |
| Reconstructing score (0-8) | |
| Good (7-8) | 37 (88.1%) |
| Fair (5-6) | 5 (11.9%) |
| Poor (0-4) | 0 |
aMRD1: Marginal reflex distance-1. The distance between the corneal light reflex to the center of the upper eyelid margin; bMRD2: Marginal reflex distance-2. The distance between the corneal light reflex to the center of the lower eyelid margin.
DISCUSSION
The enrolled cases in this study had full thickness eyelid defect after carcinoma resection. The most common cause of our cases is sebaceous carcinoma (27 eyelids, 64.3%), which involves large area of tarsal plate. Hughes procedure is commonly used to reconstruct the posterior lamellar defect of eyelid under this situation. Harvesting tarsoconjunctival flap is the key step in Hughes procedure. However, because of the limited amount of tarsal plate that can be harvested, the tarsoconjunctival flap may not be able to provide sufficient support for the defect region in cases with large eyelid defect[5]. Excessive resection of the tarsal plate is more likely to cause retraction or entropion in the opposite eyelid[1],[6]. In our procedure, the tarsal plate of the opposite eyelid was kept intact when harvesting the conjunctival flap. And, auricular cartilage was applied to substitute the tarsal plate to cover the defect area. This is the main modification to prevent retraction or entropion of the opposite eyelid.
Various autogenous graft materials for eyelid reconstruction have been investigated and tried, these include: nasal septal cartilage or nasal septal cartilage mucosa composite, palatal mucosa, and auricular cartilage[7]–[9]. According to our experience, nasal septal cartilage or nasal septal cartilage mucosa composite is too stiff to fit the curvature of the eyeball, and palatal graft has risk of contraction postoperatively and is not stiff enough to support the eyelid defect. Although these composed grafts have mucosa, the postoperative contracture and secretion may raise ocular discomforts. Besides, harvesting nasal septal cartilage mucosa composite is relatively complicating and has risk of causing penetration of nasal septum. Auricular cartilage can be a stable tarsal plate substitute due to its various advantages. First, the cartilage possesses reasonable rigidity, good biological compatibility, nonabsorbable and low incidence of late shrinking or thinning. This provides sufficient support to maintain the normal shape of eyelid margin and resist the postoperative scar contracture. Second, it has a spherical surface and thus could fit well to the bulbar surface. Partially incising the convex/concave side of the cartilage could improve the conformity of cartilage graft to the eyeball as well. Third, the amount of auricular cartilage is more abundant than donor tarsal plate, allowing full coverage of tarsal plate defects. Harvesting auricular cartilage is easier than harvesting palatal mucosa or nasal septum as well. In order to obtain adequate amount of auricular cartilage while preserving the shape of the auricle and hiding the incision, we harvested the cartilage graft from the conchal lateral wall through a post-auricular incision. In elderly patient with fragile auricular cartilage, the perichondrium and fascia of the convex side would be harvested simultaneously to prevent the cartilage from breaking when sutured. The perichondrium of the concave side should be preserved to prevent perforation of auricle.
Given the low metabolic requirement of auricular cartilage, conjunctival flap generally provides sufficient blood supply to the posterior side of auricular cartilage graft[10]–[11]. Thus, the conjunctival flap was dissected between upper eyelid Müller's muscle and conjunctiva in preparation for lower eyelid defect repair. On the other hand, the dissection plane is done between the LER and conjunctiva in preparation for upper eyelid defect repair. We believe thorough dissection to release the attachment between the Müller's muscle or LER is the key to preventing eyelid retraction of the opposite eyelid. This allows conjunctival flap to be moved with minimum tension. In our study, no obvious retraction of opposite eyelid was observed during the follow-up period.
After these modifications mentioned above, satisfactory results were achieved in all patients. The 11 cases which had upper eyelid involvement (largest height of defect reached 8 mm) were all reconstructed completely with satisfying outcomes in this study. The MRD1 of the reconstructed upper eyelid remained comparable to the fellow eye-no/mild ptosis or retraction were observed during the follow-up period.
This principle can be utilized to repair extensive defects. One of the cases had squamous cell carcinoma involving 75% upper eyelid, lateral canthus and 20% of lower eyelid. Following the same principle, the residual conjunctiva adjacent to upper and lower eyelid excision area was mobilized and fixed together to repair the conjunctival defect, and then an auricular cartilage was used to cover the tarsal defect of both eyelids. The anterior lamella was reconstructed by local advanced myocutaneous flap. The outcome of this patient was scored as 7 at the last follow-up visit (Figure 4).
Figure 4. Clinical photos of a patient underwent surgical repair after squamous cell carcinoma resection in upper and lower eyelids.
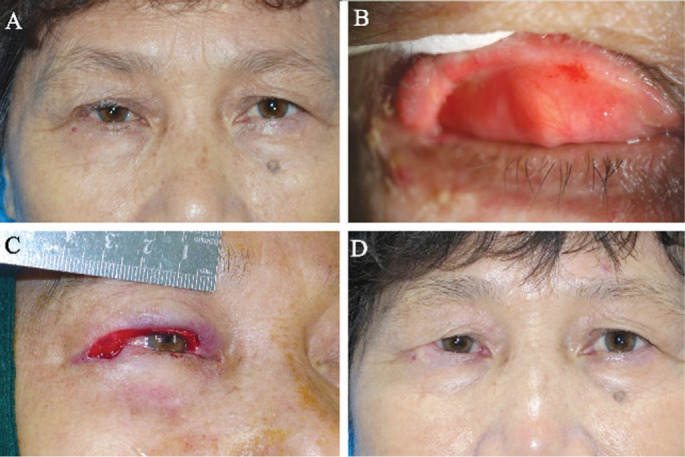
A: A 70-year-old women presented with persistent upper eyelid irritation with abnormal secretion for 10mo. B: Marginal and palpebral conjunctival hyperemia was observed, involving lateral canthus. C: Over 75% length of upper eyelid margin and 20% length of lower eyelid margin was excised. D: At the 12th month follow-up visit, the difference of the height of the upper eyelid between the fellow eyes was within 1 mm. The reconstructed eyelid was observed mild lateral canthus shorten without entropion.
For upper lid reconstructions, there were no statistical differences in mean MRD1 between the reconstructed upper eyelids and the fellow eye-suggesting that our approach provides sufficient support to prevent retraction. In our study, the anterior lamella reconstruction in upper eyelid was carefully designed by using vertically advanced myocutaneous flap (7 cases), horizontally advanced myocutaneous flap (3 cases), and semicircular rotational myocutaneous flap (n=1). Local myocutaneous advancement flap was most used to repair the anterior lamellae given that cancer tends to occur in the elderly, whom often have some upperlid dermatochalasis; and a wider brow to lid margin distance is often present in Orientals (Figure 3). While Cutler-Beard procedure has been reported to be an effective technique to reconstruct the anterior lamellar defect of upper eyelid, in our experience, the stretching of full thickness eyelid flap beneath the margin bridge potentially leads to more trauma to the lower eyelid, which may in turn lead to retraction or ectropion. This potential morbidity is made worse in Orientals who have higher risk of scar contracture.
As for lower lid reconstructions, 4 of 31 patients were observed mild retraction, which led to the mean MRD2 of the reconstructed lower eyelid greater than that of the fellow eyelid (P=0.049). However, the biggest difference in MRD2 between the reconstructed eyelids and fellow eyelids were within 2 mm. There were no/mild complaints about appearance nor any discomfort among these patients. This may be related to late myocutaneous flap or scar contracture, which suggests that a larger myocutaneous flap with a better design may be helpful in preventing this in the future.
At the last of the first stage surgery, tarsorrhaphy was performed and the eye was kept closed for 3mo. In previous reports, eye kept closed for 2wk or shorter time is sufficient for conjunctival flap recovery[2],[12]. However, the reconstructed conjunctiva and myocutaneous flap will continue to contract for months. These processes contribute to the complications of retraction/entropion in upper lid or retraction/ectropion in lower lid. Moreover, scar contracture is relatively more severe in Orientals, which should be paid more attention to[13]–[14]. In our study, the purpose of tarsorrhaphy is to resist both the conjunctival and myocutaneous scar contracture rather than avoiding dehiscence. Lid adhesion for 3mo can effectively resist early full thickness contracture of reconstructed eyelid and maintain normal position of eyelid. Besides, eyelid adhesion was involved in one eye, and patients were explained before surgery. All patients were willing to accept 3mo of eye closure to achieve better aesthetic and functional recovery; and the closure of one eye had little effect on old patients' daily life.
There are several limitations in our surgical technique. First, since auricular cartilage graft could not provide blood supply to the anterior lamella, local myocutaneous flap is the primary choice of anterior lamella reconstruction. Free skin grafting could not be applied due to lack of blood supply. This increased the surgical difficulty dramatically. Second, the size of concha may be insufficient to cover the eyelid defect in some patients. Under this circumstance, an experienced and skillful surgeon was needed to harvest adequate cartilage in other part of the auricle. In our study, 3 patients had cartilage harvested from the scapha as the size of the concha was too small. Post-operatively, these 3 patients were assessed and scored 7, 7, and 8 at the final follow-up visit, respectively.
In summary, conjunctival flap with auricular cartilage grafting and myocutaneous flap grafting is an effective procedure for reconstruction of large full thickness upper and lower eyelid defect. It could achieve satisfactory post-reconstruction appearance and avoid complications of the opposite eyelid such as retraction and entropion as well.
Acknowledgments
Chen X designed the study, performed the surgeries, and revised the article. Chen B collected the data, searched the literature, and wrote the article. Woo DM, Liu J, Zhu XY, Lin YY, and Ma YJ helped to collect the data.
Foundation: Supported by Wenzhou Municipal Science and Technology Bureau (No.Y20180719).
Conflicts of Interest: Chen B, None; Woo DM, None; Liu J, None; Zhu XY, None; Lin YY, None; Ma YJ, None; Chen X, None.
REFERENCES
- 1.Alghoul M, Pacella SJ, McClellan WT, Codner MA. Eyelid reconstruction. Plast Reconstr Surg. 2013;132(2):288e–302e. doi: 10.1097/PRS.0b013e3182958e6b. [DOI] [PubMed] [Google Scholar]
- 2.Hishmi AM, Koch KR, Matthaei M, Bölke E, Cursiefen C, Heindl LM. Modified Hughes procedure for reconstruction of large full-thickness lower eyelid defects following tumor resection. Eur J Med Res. 2016;21(1):27. doi: 10.1186/s40001-016-0221-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ooms LSS, Beets MR, Grosfeld EC, Beems EM, Krekels GA, Smit JM, Hoogbergen MM. Reconstruction of the lower eyelid using Hughes' tarsoconjunctival flap: follow up of 28 cases. J Plast Reconstr Aesthetic Surg. 2014;67(7):e177–e179. doi: 10.1016/j.bjps.2014.01.039. [DOI] [PubMed] [Google Scholar]
- 4.Putterman AM. Margin reflex distance (MRD) 1, 2, and 3. Ophthalmic Plast Reconstr Surg. 2012;28(4):308–311. doi: 10.1097/IOP.0b013e3182523b7f. [DOI] [PubMed] [Google Scholar]
- 5.Alghoul MS, Bricker JT, Vaca EE, Purnell CA. Lower eyelid reconstruction: a new classification incorporating the vertical dimension. Plast Reconstr Surg. 2019;144(2):443–455. doi: 10.1097/PRS.0000000000005882. [DOI] [PubMed] [Google Scholar]
- 6.Aggarwal S, Shah CT, Kirzhner M. Modified second stage Hughes tarsoconjunctival reconstruction for lower eyelid defects. Orbit. 2018;37(5):335–340. doi: 10.1080/01676830.2017.1423351. [DOI] [PubMed] [Google Scholar]
- 7.Suga H, Ozaki M, Narita K, Kurita M, Shiraishi T, Ohura N, Takushima A, Harii K. Comparison of nasal septum and ear cartilage as a graft for lower eyelid reconstruction. J Craniofacial Surg. 2016;27(2):305–307. doi: 10.1097/SCS.0000000000002295. [DOI] [PubMed] [Google Scholar]
- 8.Wearne MJ, Sandy C, Rose GE, Pitts J, Collin JR. Autogenous hard palate mucosa: the ideal lower eyelid spacer? Br J Ophthalmol. 2001;85(10):1183–1187. doi: 10.1136/bjo.85.10.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang M, Zhao Y. Reconstruction of full-thickness lower eyelid defect using superficial temporal artery island flap combined with auricular cartilage graft. J Craniofac Surg. 2015;26(2):576–579. doi: 10.1097/SCS.0000000000001430. [DOI] [PubMed] [Google Scholar]
- 10.Brenner KA, McConnell MP, Evans GR, Calvert JW. Survival of diced cartilage grafts: an experimental study. Plast Reconstr Surg. 2006;117(1):105–115. doi: 10.1097/01.prs.0000195082.38311.f4. [DOI] [PubMed] [Google Scholar]
- 11.Smith RJ, Malet T. Auricular cartilage grafting to correct lower conjunctival fornix retraction and eyelid malposition in anophthalmic patients. Ophthalmic Plast Reconstr Surg. 2008;24(1):13–18. doi: 10.1097/IOP.0b013e31815efe35. [DOI] [PubMed] [Google Scholar]
- 12.Memarzadeh K, Gustafsson L, Blohmé J, Malmsjö M. Evaluation of the microvascular blood flow, oxygenation, and survival of tarsoconjunctival flaps following the modified Hughes procedure. Ophthalmic Plast Reconstr Surg. 2016;32(6):468–472. doi: 10.1097/IOP.0000000000000598. [DOI] [PubMed] [Google Scholar]
- 13.Fanous N, Zari S. Universal trichloroacetic acid peel technique for light and dark skin. JAMA Facial Plast Surg. 2017;19(3):212–219. doi: 10.1001/jamafacial.2016.1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeJong H, Abbott S, Zelesco M, Spilsbury K, Ziman M, Kennedy BF, Martin L, Wood FM. Objective quantification of burn scar stiffness using shear-wave elastography: Initial evidence of validity. Burns. 2020;46(8):1787–1798. doi: 10.1016/j.burns.2020.05.009. [DOI] [PubMed] [Google Scholar]


