Short abstract
The increase in young onset colorectal cancer and the complex care needs of young cancer patients spurred the development of the Center for Young Onset Colorectal Cancer at the Memorial Sloan Kettering Cancer Center. This article describes the lessons of the first 2 years at the Center, including development of the program and specific services provided.
Keywords: Colon cancer, Implementation, Program evaluation, Young onset colorectal cancer
The incidence of young onset colorectal cancer (YO‐CRC), which includes adults diagnosed at 20–49 years of age, is increasing at an alarming rate for unclear reasons. In fact, the rates of colon and rectal cancer in young adults have been rising by 1%–2% annually since the mid‐1990s [1, 2], and models project that 25% of rectal cancer cases will be in patients <50 years of age by 2030 [3]. Similar trends have also been found in several other countries, raising concern worldwide [4].
The cause of rising CRC incidence in younger patients is unknown, and it is unclear if YO‐CRC has distinct biology from CRC arising in patients >50 years (i.e., average onset CRC). Prior studies have suggested that YO‐CRC may be associated with more aggressive disease biology, with recent study results indicating patients with YO‐CRC are significantly more likely to present with stage III or IV disease and more left‐sided tumors compared with patients with average onset CRC [5, 6, 7, 8, 9]. However, interpretation of these data is complicated by the fact that adults <50 years of age have not traditionally been screened for CRC [1, 10] under U.S. Preventative Services Task Force guidelines [11], which are based on the median age of CRC diagnosis of 67 years [12]. The rise is in sporadic CRC and not due to a known genetic predisposition [13].
The increasing incidence of YO‐CRC has led to calls for action to improve the understanding of risk factors, clinical behavior, and genetic characteristics of these patients [10, 14, 15, 16, 17, 18, 19, 20]. In addition, patients with YO‐CRC face unique challenges and care needs compared with those with average onset CRC and of those in younger age groups for whom major centers have established adolescent and young adult (AYA) programs. These factors spurred the development of the Memorial Sloan Kettering Cancer Center (MSK) Center for Young Onset Colorectal Cancer, the first and largest center worldwide solely dedicated to the needs of patients diagnosed with CRC who are younger than 50 years of age. Here, we describe our 2‐year experience with the Center, including the rationale and methods for developing the program, as well as the specific services incorporated to address the unique challenges that affect patients with YO‐CRC. In addition, we highlight the development and lessons from the first 2 years of a YO‐CRC program at a cancer center.
Developing a Young Onset Colorectal Program
The Center is designed with a dual purpose to address clinical and investigational objectives. The primary goal of the Center is to provide coordinated and systematic clinical care to comprehensively address the unique needs of patients with YO‐CRC (Fig. 1). The secondary goal is to establish a research infrastructure to study the etiology of YO‐CRC and ultimately improve outcomes. Initially the Center drew upon the pre‐existing multidisciplinary support service infrastructure at MSK, with specific services selected based upon patient and caregiver survey data from the Colorectal Cancer Alliance [20] and our experience with treating this population. We included patients under the age of 50 as this is the population of people with colorectal cancer in whom, until very recently, routine screening colonoscopies were not recommended. The survey highlighted how the psychosocial needs and priorities of YO‐CRC patients differ considerably from those of patients with average onset disease and younger patients who meet criteria for enrollment in AYA programs. A significant challenge for patients with YO‐CRC is the impact of the illness on their families. In the recent Alliance survey of patients with YO‐CRC, 80% of respondents had dependents younger than age 18 years when diagnosed [20]. Among patients with YO‐CRC, 62% reported financial hardship, and 64% reported taking a leave of absence or terminating a job or schooling because of their diagnosis [20], which can have long‐term consequences on career development and/or education trajectory. Additional financial challenges stem from the lack of standardized health insurance coverage in the U.S. and the many expenses associated with a cancer diagnosis [21]. The physical and emotional consequences of CRC and its treatment may persist for many decades and can significantly impact patients [22, 23, 24, 25, 26, 27].
Figure 1.
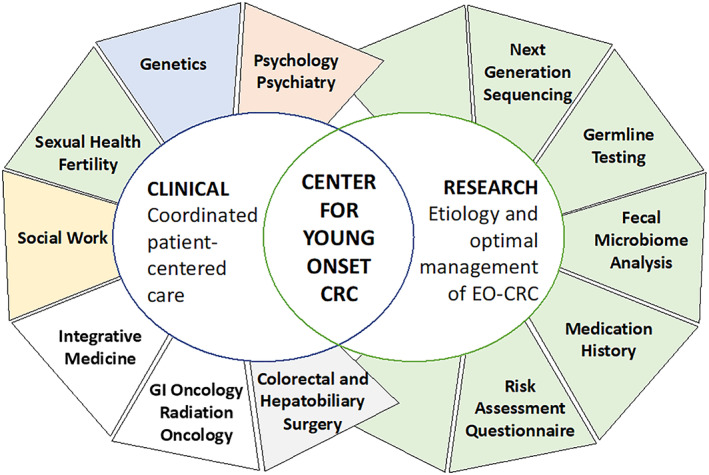
The Memorial Sloan Kettering Center for Young Onset Colorectal Cancer's coordinated clinical program involves gastrointestinal oncology, colorectal surgery, hepatobiliary surgery, radiation oncology, and gastroenterology, as well as support services, such as social work, fertility, sexual health, genetics, nutrition, integrative medicine, and psychology/psychiatry. In addition to these clinical services, patients are also approached for enrollment in research protocols involving tumor profiling, germline testing, and stool collection for microbiome analysis. Abbreviations: GI, gastrointestinal; CRC, colorectal cancer; EO‐CRC, early onset colorectal cancer.
[Correction added after online publication, June 19, 2021: Figure 1 was replaced.]
Fertility and sexual health are also major concerns; however, 64% of survey participants indicated that a medical professional did not talk to them about fertility preservation during diagnosis or treatment [20]. Sexual dysfunction has been reported to be one of the most common long‐term effects of CRC treatment [28] and may be of particular concern for young adult patients [29]. Based on these data, we identified psychosocial services, fertility, and sexual health as the key clinical programmatic elements.
Coordinated Clinical Care
Within the first 2 years of opening, 751 patients were enrolled into the Center (Fig. 2; Table 1). Because of the need for psychosocial support for patients with YO‐CRC and caregivers established in the literature [20], one of the first major priorities of the Center was early connection to psychosocial resources. We hired a dedicated social worker and reserved new psychiatry appointments for patients with YO‐CRC. Our social worker contacts all patients shortly after their initial visit. In the first 2 years, the social worker provided ongoing support to more than half of the patients and families, assisting them with their psychosocial needs and with the financial burdens associated with the diagnosis by connecting them to appropriate financial assistance programs at MSK and in the community.
Figure 2.
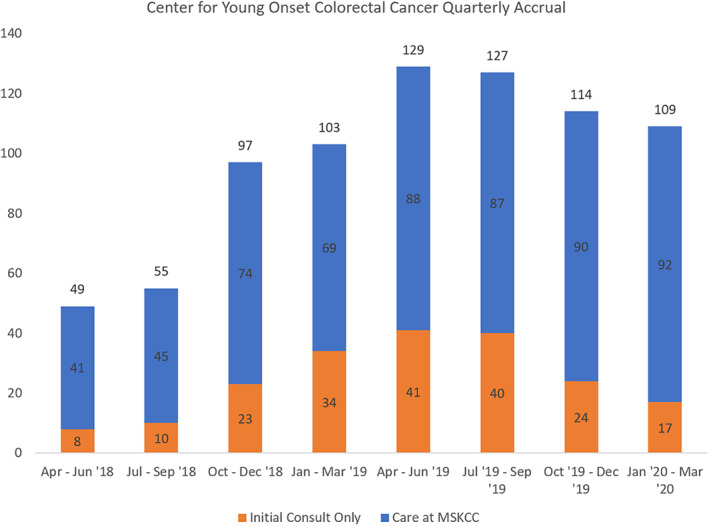
Quarterly accrual from April 2018 through March 2020. Abbreviation: MSKCC, Memorial Sloan Kettering Cancer Center.
Table 1.
Patient demographic and clinical characteristics from April 2018 through March 2020
| Characteristics | n (%) |
|---|---|
| Total no. of patients | 751 |
| Age, yr | |
| <20 | 3 (0.4) |
| 20–29 | 42 (5.6) |
| 30–39 | 232 (30.9) |
| 40–49 | 474 (63.1) |
| Median age at diagnosis (range), yr | 42.8 (37.1–46.7) |
| Sex | |
| Male | 417 (55.5) |
| Female | 334 (44.5) |
| Stage | |
| I | 41 (5.5) |
| II | 109 (14.5) |
| III | 270 (36.0) |
| IV | 331 (44.0) |
| Diagnosis | |
| Colon | 399 (51.1) |
| Rectal | 352 (46.9) |
| Race | |
| White | 561 (74.7) |
| Black | 64 (8.5) |
| Asian | 80 (10.7) |
| Native American | 1 (0.1) |
| Other | 31 (4.1) |
| Unknown | 14 (1.9) |
| Ethnicity | |
| Hispanic or Latino | 8 (1.1) |
| Non‐Hispanic or Latino | 743 (98.9) |
A second key aim of the Center is to ensure that all patients with YO‐CRC are screened for fertility needs. In order to reliably incorporate a discussion of patients’ wishes regarding fertility into their initial visits, we counseled the primary oncologists’ teams (physicians and nurses) about the importance of discussing fertility at diagnosis. Patients who wish to further discuss fertility‐related issues are then referred to the Fertility Nurse Specialists in MSK's Cancer and Fertility Program. We also incorporated sexual health in the initial Center welcome packet, in which patients are introduced to the MSK Sexual Health Service, a team of doctors, nurses, social workers, and psychologists experienced in treating specific sexual health concerns triggered by cancer. Patients are also referred to the Nutrition and Integrative Medicine Services 4–6 weeks after the start of treatment. Rationale behind inclusion of ancillary services to which the Center refers can be found in Table 2.
Table 2.
Ancillary service rationale
| Ancillary service | Rationale |
|---|---|
| Social Work | Patients with YO‐CRC have significant psychosocial needs atypical of the patient with average onset CRC, as well as needs outside of the typical AYA population. A dedicated social worker with a focus on patients with YO‐CRC was hired to meet these needs. |
| Fertility | CCA data indicated that a majority of patients with YO‐CRC did not speak to a fertility specialist before or during their treatment, even though patients reported infertility and/or early menopause resulting from treatment. Intentional, early intervention with fertility was deemed a key programmatic element. |
| Sexual Health | Sexual dysfunction has been reported as one of the most common long‐term effects of CRC treatment. In consultation with our sexual medicine group, early education about sexual health services and early intervention when necessary are needed to reduce these effects. |
| Nutrition | A focus on early access to nutrition services was identified as a key component because of expected nutritional challenges that may result from multimodality treatment. |
| Integrative Medicine | Integrative medicine services were found to reduce side effects in some patients with CRC. Education about and referral to these services were included in the program. |
| Psychiatry and Psychology | Providers with a focus on treating this patient population reserved psychiatry visits for high acuity patients with YO‐CRC. |
Abbreviations: AYA, Adolescent and Young Adult; CCA, Colorectal Cancer Alliance; CRC, colorectal cancer; YO‐CRC, young onset colorectal cancer.
Given their complex psychosocial needs, Center patients are offered information on relevant psychosocial resources in the community and at MSK, including support groups and MSK's Patient and Caregiver Peer Support Program, which links long‐term patients, survivors, and caregivers with new patients by age. In addition, we created an online community group specific to YO‐CRC through MSK's online program, Connections, to address feelings of social isolation.
We approach all patients to enroll in a young onset research protocol, which includes targeted next‐generation sequencing–based tumor profiling, germline testing, stool collection for fecal microbiome analysis, and risk factor survey data. Patients with clinically significant germline variants are contacted by the Clinical Genetics Service, which provides counseling regarding additional screening needs and implications for family members. Since the opening of the Center, 83% (623/660) and 79% (594/660) of patients consented to tumor genomic and germline testing, respectively. Results from this comprehensive testing will be synthesized to help elucidate the etiology of YO‐CRC. In addition to this established protocol, we are opening a prospective study to evaluate the effects of chemotherapy and chemoradiotherapy for early‐stage disease on female and male hormone levels and to prospectively evaluate sexual health via several quality‐of‐life assessments.
Early Program Lessons Learned
Following the opening of the Center in March 2018, we prospectively identified patients with YO‐CRC based on intake records. Despite the clear needs established in the literature, there were mixed responses to our outreach services, which may be in part related to inherent bias in the Alliance survey leading to selection of services that do not apply to our population. However, we noted that one third of social work attempts to contact patients by phone were not answered and from this we learned that patient communication is an important challenge that may contribute to mixed responses to outreach. Younger patients are more likely to interact in the virtual setting and less likely to engage in phone calls and extensive counseling. The number of patients with YO‐CRC enrolled in the online MSK patient portal (97%, 728/751) is notably higher than the number of patients with average onset CRC (>50 years) enrolled during the same time period (69%, 3,415/4,949).
In order to better understand potential barriers to ancillary service use and further evaluate the optimal time to approach patients, we administered a patient satisfaction survey to existing patients (Tables 3, 4). We asked patients to rate utility of ancillary services through a Likert‐type scale in the categories of not helpful at all, not very helpful, not sure, somewhat helpful, and very helpful. We also asked patients about intervention timing and barriers to access. Based on the completed surveys (n = 91), the majority of patients who used these ancillary services did find them helpful, which aligns with Colorectal Cancer Alliance data [20, 27]. Nutrition, sexual health, and psychology/psychiatry referrals were found to be most helpful.
Table 3.
Patient‐reported service utility
| Ancillary service used | Positive service utility a |
|---|---|
| Social Work (n = 49) | 71% |
| Nutrition (n = 52) | 89% |
| Fertility (n = 18) | 78% |
| Sexual Health (n = 16) | 88% |
| Integrative Medicine (n = 30) | 70% |
| Psychology/Psychiatry (n = 16) | 88% |
Patient rating 4 or 5 (somewhat helpful or very helpful).
Table 4.
Patient‐reported preferred ancillary service timing
| Ancillary service timing | Timing was appropriate | First visit | First treatment visit | 1–2 months into treatment | 2–4 months into treatment | 4+ months into treatment | Barriers to access a |
|---|---|---|---|---|---|---|---|
| Social Work (n = 55) | 78% | 0% | 9% | 9% | 0% | 4% | 0% |
| Nutrition (n = 66) | 71% | 12% | 9% | 2% | 0% | 3% | 3% |
| Fertility (n = 28) | 64% | 10% | 11% | 0% | 0% | 4% | 11% |
| Sexual Health (n = 36) | 31% | 13% | 22% | 17% | 3% | 14% | 0% |
| Integrative Medicine (n = 54) | 56% | 6% | 13% | 4% | 7% | 4% | 11% |
| Psychology/Psychiatry (n = 30) | 40% | 3% | 20% | 3% | 0% | 27% | 7% |
Barriers mentioned include cost, insurance coverage issues and distance from clinic.
Patient interest in these ancillary services may be affected by the timing of introduction. Our current model presents Center resources at the patient's initial consult. We acknowledge that this is a time when patients are inundated with information about their treatment options, extent of disease, and life expectancy, yet most patients still found current timing for social work, nutrition, and fertility services to be appropriate. Although 36% of patients indicated a preference for sexual health services before starting treatment, ideal timing for introduction of sexual health services remains unclear because of mixed responses. The same can be said of psychology/psychiatry services because responses were polarized, with 23% of respondents preferring services prior to treatment and 27% of respondents preferring services 4 or more months into treatment. As the Center continues to expand, we will further explore the appropriate timing for ancillary interventions.
Future Directions
Our program lessons learned have already offered us insight into this patient population. In mid‐2020, we transitioned to online contact as the main method of communication with our patients. Although our survey data indicate that patients with YO‐CRC find utility in ancillary services, additional information is still needed about optimal timing. It is also important to note that the racial and ethnic composition of our institution's patient population is not representative of those affected by CRC in the general population, which limits extrapolation to other centers. The rate of young onset cancer is increasing for several other gastrointestinal tumors, particularly gastric, appendiceal, and pancreatic cancers [5, 30, 31, 32]. As such, we are seeing more young adult patients facing similar challenges to patients with YO‐CRC, and we are expanding the Center to include patients with all gastrointestinal malignancies. We will continue to refine our program using patient and institutional stakeholder feedback to optimally address the unique needs of our patients. Our program has inspired the development of similar programs at other major cancer centers, which are critical to improve care of young adults with colorectal cancer.
Disclosures
Andrea Cercek: Bayer, Incyte, GSK (C/A), Settle Genetics, RGenix, GSK (RF); Robin Mendelsohn: Exact Sciences (C/A); Julio Garcia‐Aguilar: Intuitive Surgical, Medtronic, Ethicon (H); Zsofia Stadler: Adverum Biotechnologies, Allergan, Genentech/Roche, Novartis, Neurogene, Gyroscope Tx, Optos Plc, Regeneron, RegenexBio (C/A—immediate family member). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
Acknowledgments
We thank The Society of Memorial Sloan Kettering for its philanthropic funding.
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
Disclosures of potential conflicts of interest may be found at the end of this article.
References
- 1. Siegel RL, Fedewa SA, Anderson WF et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst 2017;109:djw322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Siegel RL, Miller KD, Goding Sauer A et al. Colorectal cancer statistics, 2020. CA Cancer J Clin 2020;70:145–164. [DOI] [PubMed] [Google Scholar]
- 3. Bailey CE, Hu CY, You YN et al. Increasing disparities in the age‐related incidences of colon and rectal cancers in the United States, 1975‐2010. JAMA Surg 2015;150:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Siegel RL, Torre LA, Soerjomataram I et al. Global patterns and trends in colorectal cancer incidence in young adults. Gut 2019;68:2179–2185. [DOI] [PubMed] [Google Scholar]
- 5. Virostko J, Capasso A, Yankeelov TE et al. Recent trends in the age at diagnosis of colorectal cancer in the US National Cancer Data Base, 2004–2015. Cancer 2019;125:3828–3835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gausman V, Dornblaser D, Anand S et al. Risk factors associated with early‐onset colorectal cancer. Clin Gastroenterol Hepatol 2019. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen FW, Sundaram V, Chew TA et al. Advanced‐stage colorectal cancer in persons younger than 50 years not associated with longer duration of symptoms or time to diagnosis. Clin Gastroenterol Hepatol 2017;15:728–737.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kim TJ, Kim ER, Hong SN et al. Long‐term outcome and prognostic factors of sporadic colorectal cancer in young patients: A large institutional‐based retrospective study. Medicine (Baltimore) 2016;95:e3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Myers EA, Feingold DL, Forde KA et al. Colorectal cancer in patients under 50 years of age: a retrospective analysis of two institutions' experience. World J Gastroenterol 2013;19:5651–5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Edwards BK, Ward E, Kohler BA et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 2010;116:544–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. U.S. Preventive Services Task Force , Bibbins‐Domingo K, Grossman DC et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA 2016;315:2564–2575. [DOI] [PubMed] [Google Scholar]
- 12. Howlader N, Noone A, Krapcho M et al. SEER Cancer Statistics Review, 1975‐2013. Bethesda, MD: National Cancer Institute, 2016. [Google Scholar]
- 13. Silla IO, Rueda D, Rodríguez Y et al. Early‐onset colorectal cancer: A separate subset of colorectal cancer. World J Gastroenterol 2014;20:17288–17296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wolf AMD, Fontham ETH, Church TR et al. Colorectal cancer screening for average‐risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin 2018;68:250–281. [DOI] [PubMed] [Google Scholar]
- 15. Davis DM, Marcet JE, Frattini JC et al. Is it time to lower the recommended screening age for colorectal cancer? J Am Coll Surg 2011;213:352–361. [DOI] [PubMed] [Google Scholar]
- 16. Fernandes GDS, Chatila WK, Yaeger R et al. Genomic landscape, clinical characteristics and outcomes of early onset (EO) compared with average onset (AO) colorectal cancer (CRC). J Clin Oncol 2018;36(suppl 15):3520a. [Google Scholar]
- 17. Siegel RL, Miller KD, Jemal A. Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970‐2014. JAMA 2017;318:572–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Park L, O'Connell K, Herzog K et al. Clinicopathologic features of young onset colorectal cancer patients: Results from a large cohort at a single cancer center. Am J Gastroenterol 2017;112:S111–S112a. [Google Scholar]
- 19. Ahnen DJ, Wade SW, Jones WF et al. The increasing incidence of young‐onset colorectal cancer: A call to action. Mayo Clin Proc 2014;89:216–224. [DOI] [PubMed] [Google Scholar]
- 20. 2017 Young Onset Colorectal Cancer Survey Report . Collorectal Cancer Alliance Web site, 2018. Available at https://www.ccalliance.org/about/never-too-young/survey/2017-young-onset-colorectal-cancer-survey-report. Accessed November 15, 2019.
- 21. Berchick E. Who are the uninsured? United States Census Bureau Web site, 2018. Available at https://www.census.gov/library/stories/2018/09/who-are-the-uninsured.html. Accessed February 6, 2020. [Google Scholar]
- 22. Grano C, Fernandes M, Bucci S et al. Self‐efficacy beliefs, faecal incontinence and health‐related quality of life in patients born with anorectal malformations. Colorectal Dis 2018;20:711–718. [DOI] [PubMed] [Google Scholar]
- 23. Kindred MM, Pinto BM, Dunsiger SI. Association of body esteem with fitness and body fat among colorectal cancer survivors: Secondary analyses from a randomized trial. Int J Behav Med 2019;26:619–628. [DOI] [PubMed] [Google Scholar]
- 24. Han CJ, Yang GS, Syrjala K. Symptom experiences in colorectal cancer survivors after cancer treatments: A systematic review and meta‐analysis. Cancer Nurs 2020;43:E132–E158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kunitake H, Russell MM, Zheng P et al. Quality of life and symptoms in long‐term survivors of colorectal cancer: Results from NSABP protocol LTS‐01. J Cancer Surviv 2017;11:111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Benedict C, Philip EJ, Baser RE et al. Body image and sexual function in women after treatment for anal and rectal cancer. Psychooncology 2016;25:316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Colorectal Cancer Alliance . Never Too Young Survey Report 2020. Colorectal Cancer Alliance Web site, 2020. Available at https://www.ccalliance.org/about/never-too-young/survey. Accessed February 12, 2020.
- 28. Traa MJ, De Vries J, Roukema JA et al. The sexual health care needs after colorectal cancer: The view of patients, partners, and health care professionals. Support Care Cancer 2014;22:763–772. [DOI] [PubMed] [Google Scholar]
- 29. Canty J, Stabile C, Milli L et al. Sexual function in women with colorectal/anal cancer. Sex Med Rev 2019;7:202–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Singh H, Koomson AS, Decker KM et al. Continued increasing incidence of malignant appendiceal tumors in Canada and the United States: A population‐based study. Cancer 2020;126:2206–2216. [DOI] [PubMed] [Google Scholar]
- 31. Tavakkoli A, Singal AG, Waljee AK et al. Racial disparities and trends in pancreatic cancer incidence and mortality in the United States. Clin Gastroenterol Hepatol 2020;18:171–178.e10. [DOI] [PubMed] [Google Scholar]
- 32. Bergquist JR, Leiting JL, Habermann EB et al. Early‐onset gastric cancer is a distinct disease with worrisome trends and oncogenic features. Surgery 2019;166:547–555. [DOI] [PubMed] [Google Scholar]


