Abstract
Abstract
Background
Gender disparities exist in the careers of women in medicine. This review explores the qualitative literature to understand how gender influences professional trajectories, and identify opportunities for intervention.
Methods
A systematic review and thematic synthesis included articles obtained from PubMed, Cochrane Central Register of Controlled Trials (Ovid), EMBASE (Ovid), APA PsycInfo (Ovid), and GenderWatch (ProQuest) on June 26 2020, updated on September 10, 2020. Included studies explored specialty choice, leadership roles, practice setting, burnout, promotion, stigma, mentoring, and organizational culture. Studies taking place outside of the USA, using only quantitative data, conducted prior to 2000, or focused on other health professions were excluded. Data were extracted using a standardized extraction tool and assessed for rigor and quality using a 9-item appraisal tool. A three-step process for thematic synthesis was used to generate analytic themes and construct a conceptual model. The study is registered with PROSPERO (CRD42020199999).
Findings
Among 1524 studies identified, 64 were eligible for analysis. Five themes contributed to a conceptual model for the influence of gender on women’s careers in medicine that resembles a developmental socio-ecological model. Gender influences career development externally through culture which valorizes masculine stereotypes and internally shapes women’s integration of personal and professional values.
Conclusion
Medical culture and structures are implicitly biased against women. Equitable environments in education, mentoring, hiring, promotion, compensation, and support for work-life integration are needed to address gender disparities in medicine. Explicit efforts to create inclusive institutional cultures and policies are essential to support a diverse workforce.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06836-z.
KEY WORDS: physician careers, gender, careers in medicine
Introduction
Despite decades of increasing representation, professional disparities persist for women in medicine. Women represent 41% of medical faculty but are less likely than men to achieve the rank of professor (OR = 0.57) or to remain in academic careers (OR = 0.68).1 They earn less, with estimates of salary differences from $11,691 to $16,982 adjusted for specialty, rank, and research performance.2–4 Men dominate leadership roles. In 2019, 18% of department chairs and 19% of deans were women.5 Women physicians suffer burnout at higher rates than men (50.7 vs. 38.2%).6
Addressing the gender gap: the paradox between increasing representation without increasing academic success, is challenging without a deeper understanding of the roots of the problem.7 Quantitative studies document patterns of different burdens of responsibilities at home8,9 and report that women are more likely to work part-time or stop a tenure clock to accommodate family building and quality of life.10 Students’ specialty choices reflect gendered patterns. 11 Reports reveal women facing gender-based harassment and discrimination,12 implicit bias, and chart a course of differences in mentorship.13 Differences in professional skills such as negotiation have been shown.14
Do women’s choices put them on alternate career trajectories? Or do these patterns reflect external deterministic forces? Quantitative literature has mapped professional disparities but not explained why they exist or led to solutions. Qualitative research examines “language and behavior in natural settings… to capture expressive information not conveyed in quantitative data about beliefs, values, feelings, and motivations that underlie behaviors.”15 This review aims to explore the experience of women in medicine in the qualitative literature to understand the role gender plays in the professional experiences for women in medicine and identify targets for change.
Search Strategy and Selection Criteria
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.16 The review protocol was registered in PROSPERO (CRD42020199999, https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=199999). There was no funding source for this study.
Identification
A systematic literature search was created by two medical librarians (JM, JN) in consultation with the remaining authors. The searches were performed with keyword and subject heading lists for each of the three main concepts: gender, career, and qualitative studies. The full search strategy for each database is included in Appendix 1. PubMed, Cochrane Central Register of Controlled Trials (Ovid), EMBASE (Ovid), APA PsycInfo (Ovid), and GenderWatch (ProQuest) were searched on June 26, 2020, and September 10, 2020. No language or date limit was imposed on searches. A search strategy using the same concepts was performed for grey literature in GenderWatch (ProQuest) and APA PsycInfo (Ovid). Grey literature, including conference abstracts, dissertations, and theses, were included in the initial results if they were related to medicine/medical education. Authors conducted additional hand-searching through known journals and reference tracking of known articles to ensure that no relevant studies were missed.
Screening and Eligibility
Two reviewers independently screened and selected each article for inclusion. Qualitative data were defined as non-numerical data obtained through interviews, surveys, focus groups, observation, review of documents, and other first-hand sources. Peer-reviewed articles were included that focused on specialty choice, career paths, leadership, practice setting and structure, burnout, promotion, evaluation and stigma, mentoring, role models, organizational culture, and harassment. Because women’s professional and domestic roles differ between countries, this article excluded studies taking place outside of the USA. Studies that only analyzed quantitative data, did not break out results by gender, collected data prior to 2000, or focused on other health professions were also excluded. Abstracts, white papers, reviews, commentaries, and dissertations were excluded. It is important to note all articles reviewed considered gender as a binary construct and did not collect demographic data on gender identity or sexual orientation.
Inclusion
Reviewers extracted data using a standardized tool developed for this study, recording the focus of each study, the population sampled and methods, the themes identified, and conclusion of the study and other elements of each paper as outlined in Appendix 2. All reviewers (AFW, BT, JS, CH, GQ) extracted data from a sample article to ensure inter-rater reliability using Krippendorff’s alpha.17 All authors reviewed and abstracted the same paper until we achieved our desired reliability of .95 (two attempts). Then, a single reviewer independently extracted data from the remaining articles, with an additional reviewer serving as the second reader to assess rigor and quality of the articles. This was done using a set of nine items adapted from Hawker and colleagues.18 These two independent raters scored each element (1 (very poor)–4 (good)) producing a score from 9 to 36 points. The average score was used to assign an overall quality grade, as described in Appendix 3. AFW reviewed all extracted data and resolved inconsistencies.
Members of the research team considered the ways in which their interactions with the data extraction might be influenced by their gender, professional backgrounds, experiences, and prior assumptions. Two extractors were from non-clinical backgrounds (CH and GQ), and three extractors were clinicians (AFW, BT, JS). All authors were cis-gender women except JN, a cis-gender man.
Analysis
Thematic synthesis occurred through a three-step process to facilitate translation of concepts from one context to another.19 Structured summaries and key concepts from each study were created. Descriptive themes were based on these key concepts, and examining the summary findings. Through serial discussions, the authors identified analytic themes that described crosscutting concepts. Examining the way these themes related to each other led to the development of a conceptual model describing influence of gender on the personal and professional context of women’s careers in medicine. Authors made notes during the extraction process and creation of themes that supported examination of reflexivity during the analysis. As a group of mostly women authors, particular note was taken to reveal instances when personal experiences of gender on careers in medicine influenced interpretation of findings.
Findings
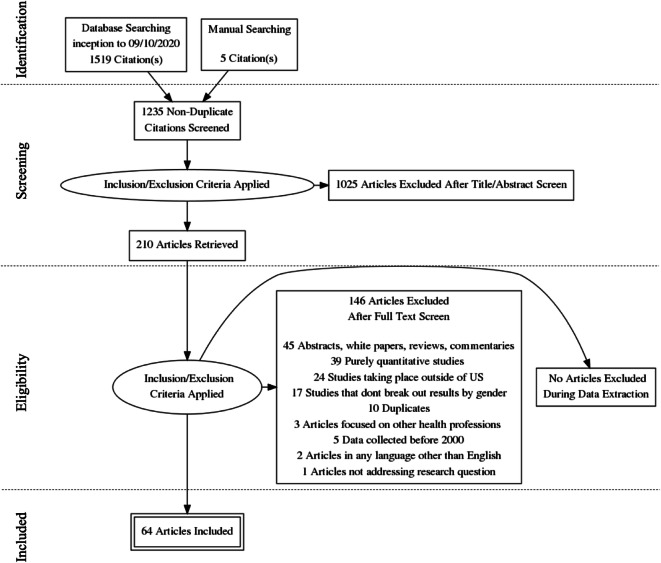
In total, 1524 citations were identified (Fig. 1). After removing duplicates, 1230 citations were screened against title and abstract. Full-text review of 205 studies identified 59 for inclusion. Five additional studies were identified through manual searching of references, resulting in 64 studies included (Appendix 4). These included 49 qualitative and 15 mixed-methods studies, most commonly relying on thematic analysis (17 studies) and grounded theory (16 studies). Findings drew from data obtained in interviews (35 studies), surveys (10 studies), focus groups (2 studies), or a combination of sources (12 studies). Textual analysis of written materials (performance evaluations, personal statements) was used in 5 studies. Participants included attending physicians (34 studies), medical students (8 studies), residents (6 studies), or a mix of participants (16 studies). Surgery was the most commonly represented specialty (1). The review included 44 high-quality, 19 medium-quality, and 1 low-quality studies.
Figure 1.
PRISMA diagram.
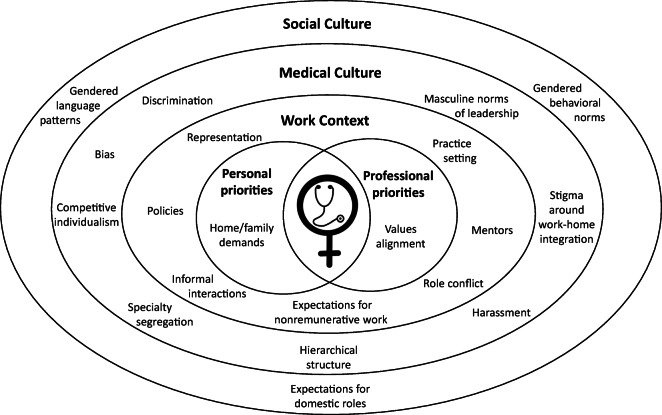
Five analytic themes were identified cutting across the eleven descriptive themes used during extraction (Appendix 5). To illustrate the interaction between these themes, the authors created a conceptual model for the influence of gender on women’s careers in medicine (Fig. 2).
Figure 2.
Conceptual model. Gender exerts influence internally on values and aspirations and externally through expectations for professional behavior and interactions. Integration of professional and personal spheres requires addressing these tensions. The pressures from larger social forces can be mitigated through a supportive culture and practices within the local context.
Gendered Language and Behavior Inform How Women Are Perceived by Others and How They Orient to Medicine
“It’s hard to be the golden boy when you’re neither a boy nor golden.”—a Native American woman physician20
Seven studies directly explored the language used by and about women in medicine. Gendered differences existed between men and women in performance evaluations of students,21 residency applications,22–24 critiques of research grants,25 and faculty perceptions of women chairs.26,27 This language reflects both gendered stereotypes as well as differences in values expected of and espoused by women. This language highlights a contrast between expectations for women and implicitly masculine professional norms. Performance evaluations reflect the expectation that women MD-PhD students should exhibit more stereotypically masculine behavior for success.21 Analysis of residency applications22,23 as well as recommendation letters24 focused on men’s achievements and leadership potential and women’s caring and “team-focus.” National Institutes of Health (NIH) grant applications described male investigators as “leaders” and “innovators” while describing female investigators as having “expertise.”25 Faculty members described female chairs’ focus on communal behavior and consensus-building.26,27
The language used by and about women in medicine reflects communal, team-focused, nurturing values. While these are considered positive traits, they also contrast with the agentic behavior and competitive individualism considered the norm for success. This association of stereotypically masculine language with professional norms contributes to different professional outcomes in terms of recognition and advancement for women. It also raises the potential for bias and microaggressions.
For Women, Alignment Between Personal and Professional Priorities Is Essential to Career Success and Satisfaction
“Women feel squeezed. They feel squeezed in terms of family responsibilities and balancing those with their academic responsibilities”—Female professor28
Across 20 studies, alignment of personal values with professional experience translated to success and satisfaction for women. Most studies focused on academic medicine, with studies exploring aspirations of medical students,29 practicing faculty,28,30–34 and successful senior leaders.35–39 Four studies focused on women physicians in rural practice,40–43 and two studies explored women physicians’ professional experience coming from Native American20 and Latina44 backgrounds. Three studies explored physician burnout.45–47
Many professional aspirations are shared by men and women: productivity in research, clinical care, and teaching. However, women emphasize certain values that align with gendered expectations: collaboration, community, mentoring, consensus-building, teaching, and career flexibility.28 Men value these areas but, as time passes, may prioritize them less to focus on research and clinical outcomes that translate to success and recognition, while women make professional choices to continue engaging in these activities.30,33,34 Work-life integration and aligning work with values exert influence on professional choices.29 Salary was explicitly not a factor in their decision-making.32
Successful women in academic medicine described satisfaction when they experienced a sense of control and clarity of values.35,36 Similar themes were observed in studies of medical school deans,37 emergency medicine chairs,38 and leaders in otolaryngology.39 These women emphasized the importance of personally meaningful work, schedule flexibility, spousal support, and collaborative team research. Outside of academia, the same pattern existed for women in rural practice, who placed value on relationships with patients and colleagues, and found satisfaction when the work was supported by their own families.40–43 Native American women physicians20 and Latina physicians44 made choices to integrate their cultural identities into professional paths.
Attrition and burnout result when women do not achieve this kind of alignment. Frustrations with a competitive, biased environment and few models for integrating work and life were described in studies of women leaving academic medicine,31 neurologists,45 practicing surgeons,46 and surgical trainees and faculty.47,48 These patterns may contribute to differences in salary observed for women if women are choosing less lucrative work in order to align professional activities with personal values and accommodate work-life integration.
Unconscious Bias Is Reflected in a Culture that Tolerates Gender-Based Discrimination and Harassment
“The girls must work 3 times as hard and then wait twice as long for the same rewards...I have hope that surgery will change as more women get into the field.”—Female surgeon48
In 16 studies, dominant masculine values were described in a medical culture celebrating competitive individualism and permitting bias and discrimination.28,49–54 One study described the academic health center as a gendered organization, reinforcing inequities through both formal expectations and policy and informal workplace interactions.55
Overt bias plays a determining role in professional paths for students experiencing inequities, discrimination, and harassment.21,56 Faculty leaving their positions also reported gender-based harassment and discrimination as well as family-related reasons for leaving.57 A large survey of members of an online physician mothers group concluded that culture and structures drive discrimination, leading to negative psychological and professional outcomes for physician mothers and their families.58 Gender discrimination and harassment were common experiences for women in surgery residency and practice.39,48,59,60 Women, thus isolated, survived by self-silencing or downplaying femininity, cultivating dual identities, as well as making professional decisions to work in more comfortable professional environments.
Stigma Against Efforts to Balance Work and Home Demands Undermines Policies and Practices Intended to Improve Equity
“The power is still with the male hierarchy in general. The men are playing golf on Sunday and making deals. I want to spend Sundays with my kids…, and I think the women who get to the highest levels got there by being men.”—Woman faculty member61
In 5 studies, policies intended to address inequities were met with stigma that undermined their intended effect. Two studies explored pregnancy in surgery fields62 and otolaryngology63 residency and described women feeling the strain of demands, lacking community around work-family integration, and feeling guilty that their pregnancy inconvenienced colleagues. Two studies explored perceptions around part-time work for faculty, and in both internal medicine,64 and pediatrics,65 faculty supported the presence of part-time policies but questioned the perceived commitment and long-term ambitions of part-time faculty. One study of women in senior positions demonstrated links between family leave policies and academic success.66
Paths to Leadership and Advancement for Women Require Navigating Conflicting Ideals, Cultivating Skills, and Creating Community
“Women my age who…fought the good fight…for the next generation of women, I think the next generation of women…don’t really want to be like us. Moreover, they won’t do what I did to get here.”—Woman dean37
Throughout 21 studies on women in leadership and mentorship, both men and women identified masculine archetypes of leadership, beginning in preclinical medical school courses,67 in choosing career paths,56 and in clinical leadership.68 Women experienced social values conflict when demonstrating agentic behavior and engaging in self-promotion.68,69 To facilitate success, women need not only personal attributes (perseverance, resilience, positive outlook) and skills (communication, organization, collaboration) but also supports at home and at work.54,70,71
Studies of mentoring reflect the influence of gender.72,73 A mosaic approach to multiple mentors across domains of life and during a career were important for women’s professional success.70,74 Professional development programs that aimed to improve leadership skills and create communities of professional support were shown to improve women’s success.75,76 Efforts to encourage specific skill development such as negotiation77 as well as general leadership development programs78 were well-received. However, studies of former participants in such programs continued to describe barriers from the sociocultural environment stalling the transformational effects of achieving a critical mass of women faculty. Graduates described persistent gender bias and limitations in the advancement of women.79
Conceptual model: (Fig. 2) Gender exerts influence internally on values and aspirations, and externally through expectations for professional behavior and interactions. Integration of professional and personal spheres requires addressing these tensions. The pressures from larger social forces can be mitigated through a supportive culture and practices within the local context.
Discussion
This analysis suggests that gender works both internally and externally on women’s careers in medicine: by influencing women’s aspirations and also by external pressures reinforcing gender stereotypes. To align their values within work and integrate demands of personal life, women make choices that result in the career disparities observed in specialty choice, salary, promotion, and leadership roles. A masculine cultural bias that values clinical and research outcomes above other contributions such as teaching and community-building reflects how these activities are reimbursed in medicine.
The model for the influence of gender on careers in medicine described visually and conceptually resembles socio-ecological models of human development, which state that interactions and relationships of an individual’s surroundings inform development.80,81 While surrounding cultural bias may take longer to change, and internalized gendered perspectives may persist, local work contexts can create structure and culture to improve inequities.82,83 Societal norms are evolving. More younger men in medicine feel burdened by work-home conflict.46 Rather than focusing on “fixing” women, efforts to support diversity should address a system that does not account fairly for different contributions and structural rigidity that makes it difficult to accommodate domestic priorities.84
Feminist scholar Judith Butler describes the way women acquire and demonstrate gendered behavior over the course of their lives as “doing gender.”85 Women in medicine appear to be “doing gender” by seeking out paths that align with feminine stereotypes and address demands of work-home integration. Seeing this gendered behavior as benign has the potential to mask inequalities.86 Women’s contributions are undervalued, and their priorities are ignored. As doctors, women display compassion and empathy, listening to their patients on average longer than men. This behavior harms clinical productivity numbers but improves health outcomes.87,88 Differences in burnout observed between men and women cease to exist in models that take differences in physicians’ personal and professional lives into account.6 As specialties that better align with traditionally feminine values become associated with women, salary and prestige decreases.89,90 Recently, women are taking on more roles in dean positions. However, these are more often in education, diversity, student and faculty affairs areas, rather than clinical or research leadership.5 Leaders in those areas steward priorities and practices of the research and clinical mission of academic medical centers. Without deliberate intervention, women’s contributions will continue to be undervalued.
In light of these findings, institutions might consider taking action to create processes and local culture that supports equity and work-home integration. These include reconsidering metrics used for performance evaluation, proactively examining assumptions about leadership, and creating mentorship systems and skills training to support all faculty. Policies such as family leave and tenure clock adjustments may exist, but concerted organizational efforts to remove stigma around use of those policies and train faculty to recognize unconscious bias are essential to the success of women in medicine.
The strength of this review was the ability to consolidate meaning from different contexts through thematic synthesis. However, certain limitations must inform interpretation of the findings of this review. The authorship team included only one man. While the team endeavored to include reflexivity into the process of analyzing and summarizing the data, the personal experience of gender in the professional lives of the co-authors inevitably informed perspectives on the review. As noted earlier, all studies viewed gender as binary, which is out of sync with current social norms recognizing transgender, non-binary, and gender fluid identities. We conclude the subjects in these studies were either cis-gender people or transgender people without the option to disclose their gender identity. Most participants in the included studies were women, rather than studies of men and women, which raises the possibility that men’s voices have been unrepresented. Furthermore, bias may be present as included studies lack ethnic diversity. The majority of studies focused on academic medicine, limiting representation from other practice settings. The specialty of surgery is disproportionately represented. The perspective of fields with significant representation by women, such as pediatrics and obstetrics and gynecology, are less well-represented. Among the studies included, there were four reports on the same population.11,29,48,49 There were also two sets of papers that included overlapping populations by Jones and colleagues32,33 as well as by Isaac and colleagues.25,26
This work leaves some questions unanswered. It is not clear whether women bring these formed values systems into medicine, or whether they are shaped by gendered expectations in and out of the workplace. Are leadership styles expressing gendered preferences, or shaped because women are penalized for expressing styles that transgress gender norms? Do expectations at home influence women’s emphasis on teams and community, to better support efforts to integrate work and home demands? Future research should explore how women process these pressures throughout their professional development, and how they express and reflect other identities they may bear as racial, ethnic, religious, and sexual and gender minorities.
Conclusion
Despite significant representation by women, assumptions based on out-of-date stereotypes associated with men—and for that matter white, heterosexual, cis-gender, and affluent men—dominate medicine today. Without proactive interventions to create fair and supportive workplaces, the potential of a diverse workforce will not be realized. We must re-imagine what it means to be a “good doctor,” and make sure our structures for education, recruitment, mentoring, reimbursement, and promotion reflect those values.
Supplementary Information
Search Strategies (DOCX 37 kb)
Data Extraction Tool (DOCX 14 kb)
Quality Assessment (DOCX 26 kb)
Studies Included (DOCX 37 kb)
Description of Themes and representative studies (DOCX 17 kb)
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pololi LH, Civian JT, Brennan RT, Dottolo AL, Krupat E. Experiencing the culture of academic medicine: Gender matters, a national study. J Gen Intern Med. 2013;28(2):201–7. doi: 10.1007/s11606-012-2207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carr PL, Raj A, Kaplan SE, Terrin N, Breeze JL, Freund KM. Gender differences in academic medicine: Retention, rank, and leadership comparisons from the national faculty survey. Acad Med. 2018;93(11):1694–9. doi: 10.1097/ACM.0000000000002146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in the salaries of physician researchers. JAMA. 2012;307(22):2410–7. doi: 10.1001/jama.2012.6183. [DOI] [PubMed] [Google Scholar]
- 4.Ash AS, Carr PL, Goldstein R, Friedman RH. Compensation and advancement of women in academic medicine: Is there equity? Ann Intern Med. 2004;141(3):205–12. doi: 10.7326/0003-4819-141-3-200408030-00009. [DOI] [PubMed] [Google Scholar]
- 5.Freund KM, Raj A, Kaplan SE, et al. Inequities in academic compensation by gender: A follow-up to the national faculty survey cohort study. Acad Med. 2016;91(8):1068–1073. doi: 10.1097/ACM.0000000000001250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Association of Medical Colleges. 2018-2019 The State of Women in Academic Medicine: Exploring Pathways to Equity | AAMC [cited 2020 Sep 30]. Available from: https://www.aamc.org/data-reports/data/2018-2019-state-women-academic-medicine-exploring-pathways-equity
- 7.Marshall AL, Dyrbye LN, Shanafelt TD, et al. Disparities in burnout and satisfaction with work-life integration in U.S. physicians by gender and practice setting. Acad Med. 2020;95(9):1435–43. doi: 10.1097/ACM.0000000000003521. [DOI] [PubMed] [Google Scholar]
- 8.Hamel MB, Ingelfinger JR, Phimister E, Solomon CG. Women in academic medicine - Progress and challenges. N Engl J Med. 2006;355(3):310–2. doi: 10.1056/NEJMe068143. [DOI] [PubMed] [Google Scholar]
- 9.Buddeberg-Fischer B, Stamm M, Buddeberg C, Bauer G, Hämmig O, Knecht M, et al. The impact of gender and parenthood on physicians’ careers - Professional and personal situation seven years after graduation. BMC Health Serv Res. 2010;10(1):40. doi: 10.1186/1472-6963-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ly DP, Seabury SA, Jena AB. Hours worked among US dual physician couples with children, 2000 to 2015. JAMA Intern Med. 2017;177(10):1524. doi: 10.1001/jamainternmed.2017.3437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fox G, Schwartz A, Hart KM. Work-family balance and academic advancement in medical schools. Acad Psychiatry. 2006;30(3):227–34. doi: 10.1176/appi.ap.30.3.227. [DOI] [PubMed] [Google Scholar]
- 12.Azizzadeh A, McCollum CH, Miller CC, Holliday KM, Shilstone HC, Lucci A. Factors influencing career choice among medical students interested in surgery. Curr Surg. 2003;60(2):210–3. doi: 10.1016/S0149-7944(02)00679-7. [DOI] [PubMed] [Google Scholar]
- 13.Carr PL, Ash AS, Friedman RH, et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132(11):889–96. doi: 10.7326/0003-4819-132-11-200006060-00007. [DOI] [PubMed] [Google Scholar]
- 14.Kawase K, Carpelan-Holmström M, Kwong A, Sanfey H. Factors that can promote or impede the advancement of women as leaders in surgery: Results from an international survey. World J Surg. 2016;40(2):258–66. doi: 10.1007/s00268-015-3332-x. [DOI] [PubMed] [Google Scholar]
- 15.Berkwits M, Inui TS. Making use of qualitative research techniques. Journal of general internal medicine. 1998;13(3):195. doi: 10.1046/j.1525-1497.1998.00054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hayes AF, Krippendorff K. Answering the call for a standard reliability measure for coding data. Communication methods and measures. 2007;1(1):77–89. doi: 10.1080/19312450709336664. [DOI] [Google Scholar]
- 18.Hawker S, Payne S, Kerr C, Hardey M, Powell J. Appraising the evidence: Reviewing disparate data systematically. Qual Health Res. 2002;12(9):1284–99. doi: 10.1177/1049732302238251. [DOI] [PubMed] [Google Scholar]
- 19.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):1–10. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elliott BA, Dorscher J, Wirta A, Hill DL. Staying connected: Native American women faculty members on experiencing success. Acad Med. 2010;85(4):675–9. doi: 10.1097/ACM.0b013e3181d28101. [DOI] [PubMed] [Google Scholar]
- 21.Heffron AS, Braun KM, Allen-Savietta C, et al. Gender can influence student experiences in MD-PhD training. Journal of Women’s Health. 2021;30(1):90–102. doi: 10.1089/jwh.2019.8094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ostapenko L, Schonhardt-Bailey C, Sublette JW, Smink DS, Osman NY. Textual analysis of general surgery residency personal statements: topics and gender differences. J Surg Educ. 2018;75(3):573–81. doi: 10.1016/j.jsurg.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 23.Osman NY, Schonhardt-Bailey C, Walling JL, Katz JT, Alexander EK. Textual analysis of internal medicine residency personal statements: themes and gender differences. Med Educ. 2015;49(1):93–102. doi: 10.1111/medu.12487. [DOI] [PubMed] [Google Scholar]
- 24.Turrentine FE, Dreisbach CN, St Ivany AR, Hanks JB, Schroen AT. Influence of gender on surgical residency applicants’ recommendation letters. J Am Coll Surg. 2019;228(4):356. doi: 10.1016/j.jamcollsurg.2018.12.020. [DOI] [PubMed] [Google Scholar]
- 25.Magua W, Zhu X, Bhattacharya A, et al. Are female applicants disadvantaged in national institutes of health peer review? Combining algorithmic text mining and qualitative methods to detect evaluative differences in R01 reviewers’ critiques. J Women’s Heal. 2017;26(5):560–70. doi: 10.1089/jwh.2016.6021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Isaac C, Griffin L. Women chairs in academic medicine: engendering strategic intuition. J Health Organ Manag. 2015;29(4 PG-498–514):498–514. doi: 10.1108/JHOM-08-2013-0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Isaac C, Griffin L, Carnes M. A qualitative study of faculty members’ views of women chairs. J Womens Health (Larchmt) 2010;19(3):533–46. doi: 10.1089/jwh.2009.1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carr PL, Gunn CM, Kaplan SA, Raj A, Freund KM. Inadequate progress for women in academic medicine: findings from the national faculty study. J Womens Health (Larchmt) 2015;24(3):190–9. doi: 10.1089/jwh.2014.4848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanfey HA, Saalwachter-Schulman AR, Nyhof-Young JM, Eidelson B, Mann BD. Influences on medical student career choice: gender or generation? Arch Surg. 2006;141(11):1086–94. doi: 10.1001/archsurg.141.11.1086. [DOI] [PubMed] [Google Scholar]
- 30.Carr PL, Pololi L, Knight S, Conrad P. Collaboration in academic medicine: reflections on gender and advancement. Acad Med. 2009;84(10):1447–53. doi: 10.1097/ACM.0b013e3181b6ac27. [DOI] [PubMed] [Google Scholar]
- 31.Levine RB, Lin F, Kern DE, Wright SM, Carrese J. Stories from early-career women physicians who have left academic medicine: a qualitative study at a single institution. Acad Med. 2011;86(6):752–8. doi: 10.1097/ACM.0b013e318217e83b. [DOI] [PubMed] [Google Scholar]
- 32.Borges NJ, Navarro AM, Grover AC. Women physicians: choosing a career in academic medicine. Acad Med. 2012;87(1):105–14. doi: 10.1097/ACM.0b013e31823ab4a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jones RD, Chapman CH, Holliday EB, et al. Qualitative assessment of academic radiation oncology department chairs’ insights on diversity, equity, and inclusion: progress, challenges, and future aspirations. Int J Radiat Oncol Biol Phys. 2018;101(1):30–45. doi: 10.1016/j.ijrobp.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 34.Jones RD, Griffith KA, Ubel PA, Stewart A, Jagsi R. A mixed-methods investigation of the motivations, goals, and aspirations of male and female academic medical faculty. Acad Med. 2016;91(8):1089–97. doi: 10.1097/ACM.0000000000001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kalet AL, Fletcher KE, Ferdman DJ, Bickell NA. Defining, navigating, and negotiating success: the experiences of mid-career Robert Wood Johnson Clinical Scholar women. J Gen Intern Med. 2006;21(9):920–5. doi: 10.1007/BF02743138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kalet A, Lusk P, Rockfeld J, Schwartz K, Fletcher KE, Deng R, et al. The challenges, joys, and career satisfaction of women graduates of the Robert Wood Johnson clinical scholars program 1973–2011. J Gen Intern Med. 2020;35(8):2258–65. doi: 10.1007/s11606-020-05715-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Humberstone E. Women deans’ perceptions of the gender gap in American medical deanships. Educ Health (Abingdon) 2017;30(3):248–53. doi: 10.4103/efh.EfH_291_16. [DOI] [PubMed] [Google Scholar]
- 38.Guptill M, Reibling ET, Clem K. Deciding to lead: A qualitative study of women leaders in emergency medicine. Int J Emerg Med. 2018;11(1):47. doi: 10.1186/s12245-018-0206-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meyer TK, Bergmark R, Zatz M, Sardesai MG, Litvack JR, Starks AA. barriers pushed aside: insights on career and family success from women leaders in academic otolaryngology. Otolaryngol - Head Neck Surg (United States) 2019;161(2):257–64. doi: 10.1177/0194599819841608. [DOI] [PubMed] [Google Scholar]
- 40.Stutzman K, Ray Karpen R, Naidoo P, et al. Support for rural practice: female physicians and the life-career interface. Rural Remote Health. 2020;20(1):5341. doi: 10.22605/RRH5341. [DOI] [PubMed] [Google Scholar]
- 41.Phillips J, Hustedde C, Bjorkman S, et al. Rural women family physicians: strategies for successful work-life balance. Ann Fam Med. 2016;14(3):244–51. doi: 10.1370/afm.1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hustedde C, Paladine H, Wendling A, et al. Women in rural family medicine: a qualitative exploration of practice attributes that promote physician satisfaction. Rural Remote Health. 2018;18(2):4355. doi: 10.22605/RRH4355. [DOI] [PubMed] [Google Scholar]
- 43.Paladine HL, Hustedde C, Wendling A, Sola O, Prasad R, Bjorkman S, et al. The role of rural communities in the recruitment and retention of women physicians. Women Health. 2020;60(1):113–22. doi: 10.1080/03630242.2019.1607801. [DOI] [PubMed] [Google Scholar]
- 44.Flores GM. Pursuing medicina [medicine]: Latina physicians and parental messages on gendered career choices. Sex Roles. 2019;81(1):59–73. doi: 10.1007/s11199-018-0979-4. [DOI] [Google Scholar]
- 45.LaFaver K, Miyasaki JM, Keran CM, et al. Age and sex differences in burnout, career satisfaction, and well-being in US neurologists. Neurology. 2018;91(20):1928–41. doi: 10.1212/WNL.0000000000006497. [DOI] [PubMed] [Google Scholar]
- 46.Lu PW, Columbus AB, Fields AC, Melnitchouk N, Cho NL. Gender differences in surgeon burnout and barriers to career satisfaction: a qualitative exploration. J Surg Res. 2020;247:28–33. doi: 10.1016/j.jss.2019.10.045. [DOI] [PubMed] [Google Scholar]
- 47.Dahlke AR, Johnson JK, Greenberg CC, et al. Gender differences in utilization of duty-hour regulations, aspects of burnout, and psychological well-being among general surgery residents in the United States. Ann Surg. 2018;268(2):204–11. doi: 10.1097/SLA.0000000000002700. [DOI] [PubMed] [Google Scholar]
- 48.Longo P, Straehley CJ. Whack! I’ve hit the glass ceiling! Women’s efforts to gain status in surgery. Gend Med. 2008;5(1):88–100. doi: 10.1016/S1550-8579(08)80011-3. [DOI] [PubMed] [Google Scholar]
- 49.Pololi L, Conrad P, Knight S, Carr P. A study of the relational aspects of the culture of academic medicine. Acad Med. 2009;84(1):106–14. doi: 10.1097/ACM.0b013e3181900efc. [DOI] [PubMed] [Google Scholar]
- 50.Pololi LH, Jones SJ. Women faculty: an analysis of their experiences in academic medicine and their coping strategies. Gend Med. 2010;7(5):438–50. doi: 10.1016/j.genm.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 51.Carr PL, Szalacha L, Barnett R, Caswell C, Inui T. A “Ton of feathers”: Gender discrimination in academic medical careers and how to manage it. J Womens Health (Larchmt) 2003;12(10):1009–18. doi: 10.1089/154099903322643938. [DOI] [PubMed] [Google Scholar]
- 52.Pingleton SK, Jones EV, Rosolowski TA, Zimmerman MK. Silent Bias: Challenges, obstacles, and strategies for leadership development in academic medicine-lessons from oral histories of women professors at the University of Kansas. Acad Med. 2016;91(8):1151–7. doi: 10.1097/ACM.0000000000001125. [DOI] [PubMed] [Google Scholar]
- 53.Evans DP, Sales JM, Krause KH, Del Rio C. You have to be twice as good and work twice as hard: a mixed-methods study of perceptions of sexual harassment, assault and women’s leadership among female faculty at a research university in the USA. Glob Heal Epidemiol Genomics. 2019;4:e6. doi: 10.1017/gheg.2019.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kass RB, Souba WW, Thorndyke LE. Challenges confronting female surgical leaders: overcoming the barriers. J Surg Res. 2006;132(2):179–87. doi: 10.1016/j.jss.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 55.Balmer DF, Courts KA, Dougherty B, Tuton LW, Abbuhl S, Hirshfield LE. Applying the theory of gendered organizations to the lived experience of women with established careers in academic medicine published ahead of print. Teach Learn Med. 2020;2020:1–10. doi: 10.1080/10401334.2020.1767106. [DOI] [PubMed] [Google Scholar]
- 56.Babaria P, Abedin S, Berg D, Nunez-Smith M. “I’m too used to it”: A longitudinal qualitative study of third year female medical students’ experiences of gendered encounters in medical education. Soc Sci Med. 2012;74(7):1013–20. doi: 10.1016/j.socscimed.2011.11.043. [DOI] [PubMed] [Google Scholar]
- 57.Martinez LR, O’Brien KR, Hebl MR. Fleeing the ivory tower: gender differences in the turnover experiences of women faculty. J Womens Health (Larchmt) 2017;26(5):580–6. doi: 10.1089/jwh.2016.6023. [DOI] [PubMed] [Google Scholar]
- 58.Halley MC, Rustagi AS, Torres JS, et al. Physician mothers’ experience of workplace discrimination: a qualitative analysis. BMJ. 2018;363:k4926. doi: 10.1136/bmj.k4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bernardi K, Shah P, Lyons NB, Olavarria OA, Alawadi ZM, Leal IM, et al. Perceptions on gender disparity in surgery and surgical leadership: A multicenter mixed methods study. Surgery. 2020;167(4):743–50. doi: 10.1016/j.surg.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 60.Barnes KL, McGuire L, Dunivan G, Sussman AL, McKee R. Gender bias experiences of female surgical trainees. J Surg Educ. 2019;76(6):e1–14. doi: 10.1016/j.jsurg.2019.07.024. [DOI] [PubMed] [Google Scholar]
- 61.Helitzer DL, Newbill SL, Cardinali G, Morahan PS, Chang S, Magrane D. Changing the culture of academic medicine: critical mass or critical actors? J Womens Health (Larchmt) 2017;26(5):540–548. doi: 10.1089/jwh.2016.6019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rangel EL, Castillo-Angeles M, Changala M, Haider AH, Doherty GM, Smink DS. Perspectives of pregnancy and motherhood among general surgery residents: A qualitative analysis. Am J Surg. 2018;216(4):754–9. doi: 10.1016/j.amjsurg.2018.07.036. [DOI] [PubMed] [Google Scholar]
- 63.Cole S, Arnold M, Sanderson A, Cupp C. Pregnancy during otolaryngology residency: Experience and recommendations. Am Surg. 2009;75(5):411–5. doi: 10.1177/000313480907500512. [DOI] [PubMed] [Google Scholar]
- 64.Harrison RA, Gregg JL. A time for change: an exploration of attitudes toward part-time work in academia among women internists and their division chiefs. Acad Med. 2009;84(1):80–6. doi: 10.1097/ACM.0b013e3181900ebd. [DOI] [PubMed] [Google Scholar]
- 65.Kahn JA, Degen SJ, Mansour ME, et al. Pediatric faculty members’ attitudes about part-time faculty positions and policies to support part-time faculty: a study at one medical center. Acad Med. 2005;80(10):931–9. doi: 10.1097/00001888-200510000-00013. [DOI] [PubMed] [Google Scholar]
- 66.Gunn CM, Freund KM, Kaplan SA, Raj A, Carr PL. Knowledge and perceptions of family leave policies among female faculty in academic medicine. Women’s Heal Issues. 2014;24(2):e205–10. doi: 10.1016/j.whi.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wayne NL, Vermillion M, Uijtdehaage S. Gender differences in leadership amongst first-year medical students in the small-group setting. Acad Med. 2010;85(8):1276–81. doi: 10.1097/ACM.0b013e3181e5f2ce. [DOI] [PubMed] [Google Scholar]
- 68.Kolehmainen C, Brennan M, Filut A, Isaac C, Carnes M. Afraid of being “Witchy with a ‘B’”: A qualitative study of how gender influences residents’ experiences leading cardiopulmonary resuscitation. Acad Med. 2014;89(9):1276–81. doi: 10.1097/ACM.0000000000000372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ellinas EH, Fouad N, Byars-Winston A. Women and the decision to leave, linger, or lean in: predictors of intent to leave and aspirations to leadership and advancement in academic medicine. J Womens Health (Larchmt). 2018;27(3):324–332. [DOI] [PubMed]
- 70.Cochran A, Elder WB, Neumayer LA. Characteristics of effective mentorship for academic surgeons: a grounded theory model. Ann Surg. 2019;269(2):269–74. doi: 10.1097/SLA.0000000000002487. [DOI] [PubMed] [Google Scholar]
- 71.Levine RB, Mechaber HF, Reddy ST, Cayea D, Harrison RA. A good career choice for women. Acad Med. 2013;88(4):527–34. doi: 10.1097/ACM.0b013e31828578bb. [DOI] [PubMed] [Google Scholar]
- 72.McNamara MC, McNeil MA, Chang J. A pilot study exploring gender differences in residents’ strategies for establishing mentoring relationships. Med Educ Online. 2008;13:7. doi: 10.3402/meo.v13i.4476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bettis J, Thrush CR, Slotcavage RL, Stephenson K, Petersen E, Kimbrough MK. What makes them different? An exploration of mentoring for female faculty, residents, and medical students pursuing a career in surgery. Am J Surg. 2019;218(4):767–71. doi: 10.1016/j.amjsurg.2019.07.029. [DOI] [PubMed] [Google Scholar]
- 74.Farrugia G, Zorn CK, Williams AW, Ledger KK. A qualitative analysis of career advice given to women leaders in an academic medical center. JAMA Netw Open. 2020;3(7):e2011292. doi: 10.1001/jamanetworkopen.2020.11292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Columbus AB, Lu PW, Hill SS, Fields AC, Davids JS, Melnitchouk N. Factors associated with the professional success of female surgical department chairs: a qualitative study. JAMA surgery. 2020;155(11):1028–33. doi: 10.1001/jamasurg.2020.3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Thompson-Burdine JA, Telem DA, Waljee JF, et al. Defining Barriers and facilitators to advancement for women in academic surgery. JAMA Netw Open. 2019;2(8):e1910228. doi: 10.1001/jamanetworkopen.2019.10228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lin MP, Lall MD, Samuels-Kalow M, et al. Impact of a women-focused professional organization on academic retention and advancement: perceptions from a qualitative study. Acad Emerg Med. 2019;26(3):303–16. doi: 10.1111/acem.13699. [DOI] [PubMed] [Google Scholar]
- 78.Welch JL, Jimenez HL, Walthall J, Allen SE. The women in emergency medicine mentoring program: an innovative approach to mentoring. J Gr Med Educ. 2012;4(3):362–6. doi: 10.4300/JGME-D-11-00267.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Helitzer DL, Newbill SL, Cardinali G, Morahan PS, Chang S, Magrane D. Narratives of participants in national career development programs for women in academic medicine: Identifying the opportunities for strategic investment. J Women’s Heal. 2016;25(4):360–70. doi: 10.1089/jwh.2015.5354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–31. doi: 10.1037/0003-066X.32.7.513. [DOI] [Google Scholar]
- 81.Kilanowski JF. Breadth of the Socio-Ecological Model. Journal of Agromedicine. 2017;22(4):295–297. doi: 10.1080/1059924X.2017.1358971. [DOI] [PubMed] [Google Scholar]
- 82.Westring AF, Speck RM, Dupuis Sammel M, et al. Culture matters: The pivotal role of culture for women’s careers in academic medicine. Acad Med 2014;89(4). [DOI] [PMC free article] [PubMed]
- 83.Valantine HA. Where are we in bridging the gender leadership gap in academic medicine? Acad Med. 2020;95(10):1475–6. doi: 10.1097/ACM.0000000000003574. [DOI] [PubMed] [Google Scholar]
- 84.Magrane D, Helitzer D, Morahan P, et al. Systems of career influences: a conceptual model for evaluating the professional development of women in academic medicine. J Womens Health (Larchmt) 2012;21(12):1244–51. doi: 10.1089/jwh.2012.3638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Butler J. Performative Acts and gender constitution: an essay in phenomenology and feminist Theory. Theatr J. 1988;40(4):519. doi: 10.2307/3207893. [DOI] [Google Scholar]
- 86.Risman BJ. From doing to undoing: gender as we know it. Gender & Society. 2009;23(1):81–84. doi: 10.1177/0891243208326874. [DOI] [Google Scholar]
- 87.Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS One. 2013;8(4):e61526. doi: 10.1371/journal.pone.0061526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Linzer M, Harwood E. Gendered expectations: do they contribute to high burnout among female physicians? J Gen Intern Med. 2018;33(6):963–5. doi: 10.1007/s11606-018-4330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Valian V. Beyond gender schemas: improving the advancement of women in academia. Hypatia. 2005;20(3):198–213. doi: 10.1111/j.1527-2001.2005.tb00495.x. [DOI] [Google Scholar]
- 90.Pelley E, Carnes M. When a Specialty Becomes “Women’s Work”: Trends in and implications of specialty gender segregation in medicine. Acad Med. 2020;95(10):1499–506. doi: 10.1097/ACM.0000000000003555. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search Strategies (DOCX 37 kb)
Data Extraction Tool (DOCX 14 kb)
Quality Assessment (DOCX 26 kb)
Studies Included (DOCX 37 kb)
Description of Themes and representative studies (DOCX 17 kb)