Abstract
Background
Although early follow-up after discharge from an index admission (IA) has been postulated to reduce 30-day readmission, some researchers have questioned its efficacy, which may depend upon the likelihood of readmission at a given time and the health conditions contributing to readmissions.
Objective
To investigate the relationship between post-discharge services utilization of different types and at different timepoints and unplanned 30-day readmission, length of stay (LOS), and inpatient costs.
Design, Setting, and Participants
The study sample included 583,199 all-cause IAs among 2014 Medicare fee-for-service beneficiaries that met IA inclusion criteria.
Main Measures
The outcomes were probability of 30-day readmission, average readmission LOS per IA discharge, and average readmission inpatient cost per IA discharge. The primary independent variables were 7 post-discharge health services (institutional outpatient, primary care physician, specialist, non-physician provider, emergency department (ED), home health care, skilled nursing facility) utilized within 7 days, 14 days, and 30 days of IA discharge. To examine the association with post-discharge services utilization, we employed multivariable logistic regressions for 30-day readmissions and two-part models for LOS and inpatient costs.
Key Results
Among all IA discharges, the probability of unplanned 30-day readmission was 0.1176, the average readmission LOS per discharge was 0.67 days, and the average inpatient cost per discharge was $5648. Institutional outpatient, home health care, and primary care physician visits at all timepoints were associated with decreased readmission and resource utilization. Conversely, 7-day and 14-day specialist visits were positively associated with all three outcomes, while 30-day visits were negatively associated. ED visits were strongly associated with increases in all three outcomes at all timepoints.
Conclusion
Post-discharge services of different types and at different timepoints have varying impacts on 30-day readmission, LOS, and costs. These impacts should be considered when coordinating post-discharge follow-up, and their drivers should be further explored to reduce readmission throughout the health care system.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06708-6.
KEY WORDS: all-cause index admission, unplanned 30-day readmission, post-discharge services utilization, service types, Hospital Readmission Reduction Program
INTRODUCTION
Early follow-up after hospital discharge provides an opportunity to assess patient health and to provide care to reduce adverse health outcomes and 30-day readmissions.1–8 Medical researchers have therefore identified barriers to early follow-up (e.g., limited resources to coordinate follow-up care, patient non-compliance) and designed interventions to promote follow-up.1,7,9–15
However, some researchers have questioned the value of early follow-up because its efficacy may depend upon the likelihood of readmission at a given time after discharge9,16–18 and upon the health conditions contributing to readmissions.7,16 Among Medicare patients in the Centers for Medicare and Medicaid Services (CMS)’ initial Hospital Readmission Reduction Program (HRRP), approximately one-third of 30-day readmissions occurred within 7 days of discharge from the index admission (IA), and two-thirds occurred within 15 days, which might be earlier than scheduled follow-up care.2 Furthermore, 30-day readmissions occur for a wide range of diagnoses different from the primary diagnosis of IA because recently discharged patients frequently experience changes in comorbidities or develop new health conditions.2,19–24
Nonetheless, most prior studies have focused on the potential benefits of early follow-up care. Little is known about patients’ patterns of post-discharge services utilization and their outcomes, although patients utilize post-discharge services of different types and at different times to address various health care needs, and their effects on readmission and readmission resource utilization vary. Indeed, post-discharge services could improve health to reduce 30-day readmission or, alternatively, could identify post-discharge health problems that should be treated in the inpatient setting rather than office-based clinics. For example, prior research has shown that intensive primary care follow-up increased readmission among sicker patients, potentially due to physicians’ detection or patients’ complaints of medical problems unresolved during IA.25
The present study used Medicare claims data for all-cause IA to examine how post-discharge services of 7 different types (institutional outpatient, primary care physician (PCP), specialist, non-physician provider, emergency department (ED), home health care, skilled nursing facility) and at 3 different timepoints were associated with 30-day unplanned readmission, readmission length of stay (LOS), and readmission inpatient costs.
METHODS
Data Sources and Study Population
Our study used 2014 Medicare claims including data from the Master Beneficiary Summary File, Medicare Provider Analysis and Review (inpatient and skilled nursing facilities), institutional outpatient services, carrier services (ED and office-based health services across various medical provider specialties), and home health care. The initial study sample included Medicare fee-for-service (FFS) patients hospitalized for acute illness between February 1 and November 30. Health services utilization that occurred in January and December was used to account for health services 30 days prior to IA and 30 days after discharge, respectively.
We defined all-cause IA using criteria from the CMS 2014 Measure Updates and Specification Report (CMS-MUSR).26,27 These criteria excluded admissions if (i) the primary diagnosis was medical treatment of cancer, rehabilitation, or psychiatric in nature; (ii) the discharge status was dead in hospital, left hospital against medical advice, or transferred to another acute care facility; and (iii) the patient unenrolled in Medicare FFS plans or died within 30 days of discharge. The unit of analysis was IA, and only admissions subsequent to IA were used to identify readmissions. When a patient was readmitted multiple times within 30 days of discharge from IA, only the first readmission was counted, and additional readmissions within this period were not counted as either new IA or readmission per CMS criterion.2,26 An individual could have multiple IAs if subsequent admissions occurred more than 30 days after a prior discharge and met inclusion criteria.
We assessed readmission resource utilization per IA discharge among all IA discharges. Some researchers have measured resource utilization among readmitted patients only. However, this methodology does not assess the effect of post-discharge services utilization adequately because changes in readmission resource utilization depend upon both the probability of readmission and resources utilized by readmitted patients.
The University of Nebraska Medical Center Institutional Review Board approved this study.
Data Elements
Outcomes
The study had 3 co-primary outcomes: a binary outcome of unplanned 30-day readmission, average readmission LOS per IA discharge, and average readmission inpatient cost per IA discharge. Planned readmission was identified using the CMS-MUSR planned readmission algorithm, which specified diagnoses and procedures for which admissions were frequently planned.26 Inpatient cost was measured as total charges allowed by CMS, which were the sum of CMS reimbursements and beneficiaries’ out-of-pocket payments.
Primary Independent Variables
The primary independent variables were 7 binary variables of post-discharge health services: institutional outpatient services (e.g., hospital outpatient department), office-based PCPs (general practice, family practice, internal medicine, obstetrics/gynecology, geriatrics), office-based specialists, office-based non-physician providers (e.g., nurse practitioner, physician assistant, physical therapist, rehabilitation), ED visit that did not result in readmission, home health care, and skilled nursing facility.
Utilization of each post-discharge service was measured within 7 days, 14 days, and 30 days of IA discharge to investigate the relationship between post-discharge services at different times and 30-day readmission, LOS, and costs. Given that 30-day readmission was defined as occurring anytime between 0 and 30 days of discharge, we defined 30-day post-discharge service as utilization occurring between IA discharge and unplanned 30-day readmission for patients who were readmitted or within 30 days of IA discharge for patients who were not readmitted. Services utilized on the readmission date (or 1 day prior to readmission for ED visits) were excluded. We defined 7-day and 14-day post-discharge services utilization similarly.
The outcome variable of readmission competes with the primary independent variable of health services utilization by necessity. For example, for a patient readmitted 9 days after IA discharge, 14-day post-discharge services were defined as service utilized between IA discharge and readmission at 9 days because any post-discharge services utilized after readmission could not influence this readmission despite occurring within 14 days of IA discharge. If a patient was not readmitted within 14 days of IA discharge, 14-day post-discharge services were defined as any services utilized within 14 days of discharge.
Other Explanatory Variables
Explanatory variables included pre-IA health services utilization of the 7 types listed above and characteristics of IA (weekend admission, surgical intervention, LOS during IA, discharge status). We also controlled for age categories, gender, race/ethnicity, the 20 most frequent IA discharge diagnoses by ICD-9 codes, Elixhauser comorbidity index, health insurance status (dual eligibility for Medicare and Medicaid, participation in Medicare Part D), and geographic region (Northeast, Midwest, South, West).
Statistical Analysis
To examine the association of post-discharge services utilization with unplanned 30-day readmission, we employed multivariable logistic regressions. To analyze the association of post-discharge services utilization with LOS and inpatient costs, we used multivariable two-part models28,29 because the overwhelming majority of patients were not readmitted and thus had zero readmission LOS and costs. In the first part of the two-part model, logistic regression was used to estimate whether patients had no readmission versus readmission (indicated by zero versus any LOS or costs). In the second part of the model, generalized linear models with a log-link function and gamma distribution accounted for LOS and costs conditional upon any positive outcome, to control skewed nature and outliers of these variables.30 The estimation coefficients of two-part models were converted into average marginal effects (AMEs), which represent the differences in adjusted predicted outcome between a comparison group and a reference group. AME allows us to combine the effects of post-discharge services in both parts and to interpret them in terms of the outcome value (i.e., days for LOS, dollars for cost).
For each outcome variable, we ran three estimations in which 7-day, 14-day, and 30-day post-discharge services utilizations were primary independent variables, respectively.
We performed a subsample analysis for the 6 conditions included in the HRRP (acute myocardial infarction, heart failure, pneumonia, coronary artery bypass graft surgery, chronic obstructive pulmonary disease, total hip arthroplasty and/or total knee arthroplasty). We also conducted a sensitivity analysis by constructing a categorical variable for each post-discharge service (0, 1, 2, 3–5, ≥6 visits) and comparing its effects with the estimates from the main analysis. All estimates were adjusted with a robust option and clustered by county.
RESULTS
The study population included 583,199 all-cause IAs. The probability of 30-day unplanned readmission was 0.1176. Among these readmissions, 33.9% and 58.8% occurred within 7 days and 14 days of discharge, respectively, similar to the trends for 3 diseases included in the CMS’ initial HRRP.2 Among readmitted patients, the average LOS and inpatient costs were 5.67 days and $48,030, respectively. As a result, among all IA discharges, the average readmission LOS and inpatient costs per IA discharge (i.e., probability of readmission multiplied by LOS or costs conditional on readmission) were 0.67 days and $5648, respectively (Table 1).
Table 1.
Unplanned 30-Day Readmission, Hospital Length of Stay, and Inpatient Costs (n = 583,199)
| Among all-cause index admissions (IAs) | |
|---|---|
| Unplanned 30-day readmission, n (probability) | 68,508 (0.1176) |
| Average readmission length of stay per IA discharge, days (SD) | 0.67 (2.59) |
| Average inpatient costs per IA discharge, dollars (SD) | 5648 (27,426) |
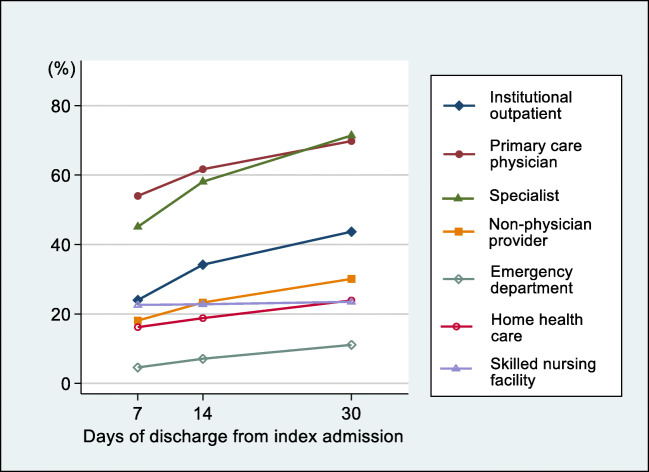
The mean age was 78.2 years, 57.8% were female, and 83.2% were non-Hispanic white. Fifty-eight percent (58.4%) of IAs was attributable to the 20 most frequent primary IA diagnoses (Table 2). Utilization of each post-discharge service is detailed in Figure 1.
Table 2.
Patient Sociodemographics, Health Services Utilization Prior to Index Admission (IA), Characteristics of IA, Primary Diagnoses, Elixhauser Comorbidity Index, and Geographic Regions (n = 583,199)
| n (%) | |
|---|---|
| Age category | |
| 65–70 | 132,545 (22.7) |
| 71–75 | 113,286 (19.4) |
| 76–80 | 106,854 (18.3) |
| 81–85 | 99,183 (17.0) |
| 86–90 | 80,294 (13.8) |
| 91 or above | 51,037 (8.8) |
| Women | 336,832 (57.8) |
| Race/ethnicity | |
| Non-Hispanic white | 485,045 (83.2) |
| Black | 50,140 (8.6) |
| Hispanic | 29,208 (5.0) |
| Other | 18,806 (3.2) |
| Health services in 30 days prior to IA | |
| Institutional outpatient | 274,104 (47.0) |
| Office-based primary care physician | 306,110 (52.5) |
| Office-based specialist | 413,136 (70.8) |
| Office-based non-physician provider | 289,266 (49.6) |
| Emergency department | 135,837 (23.3) |
| Home health care | 33,831 (5.8) |
| Skilled nursing facility | 5767 (1.0) |
| IA weekend admission | 142,047 (24.4) |
| Surgical intervention during IA | 338,613 (58.1) |
| Length of stay category in IA | |
| 1 day | 75,890 (13.0) |
| 2 days | 111,008 (19.0) |
| 3 days | 128,902 (22.1) |
| 4–5 days | 131,637 (22.6) |
| 6–10 days | 102,066 (17.5) |
| 11 days or longer | 33,696 (5.8) |
| Discharge status in IA | |
| Home, self-care | 294,818 (50.6) |
| Home, with care | 113,334 (19.4) |
| Skilled nursing facility | 136,696 (23.4) |
| Rehabilitation | 33,616 (5.8) |
| Hospice | 4735 (0.8) |
| 20 most frequent diagnoses in IA | |
| All other diagnoses (reference) | 242,868 (41.6) |
| Osteoarthritis and allied disorders | 44,328 (7.6) |
| Septicemia | 33,343 (5.7) |
| Heart failure | 30,473 (5.2) |
| Cardiac dysrhythmias | 25,551 (4.4) |
| Pneumonia | 23,046 (4.0) |
| Chronic bronchitis | 17,185 (2.9) |
| Other disorders of urethra and urinary tract | 16,645 (2.9) |
| Acute myocardial infarction | 16,418 (2.8) |
| Fracture of neck of femur | 15,764 (2.7) |
| Acute renal failure | 15,156 (2.6) |
| Occlusion of cerebral arteries | 14,898 (2.6) |
| Complications peculiar to certain specified procedures | 12,579 (2.2) |
| Other forms of chronic ischemic heart disease | 12,205 (2.1) |
| Other cellulitis and abscess | 10,476 (1.8) |
| General symptoms | 9935 (1.7) |
| Intestinal obstruction without mention of hernia | 9602 (1.6) |
| Diverticula of intestine | 9427 (1.6) |
| Disorders of fluid, electrolyte, and acid-base balance | 8642 (1.5) |
| Other diseases of lung | 7780 (1.3) |
| Symptoms involving respiratory system and other chest | 6878 (1.2) |
| Elixhauser comorbidity index (mean (SD)) | 3.7 (2.1) |
| Dual eligibility for Medicare and Medicaid | 104,851 (18.0) |
| Participation in Medicare Part D | 396,019 (67.9) |
| Region | |
| Northeast | 118,898 (20.4) |
| Midwest | 135,885 (23.3) |
| South | 238,988 (41.0) |
| West | 89,428 (15.3) |
Figure 1.
Post-discharge health services utilization within 7 days, 14 days, and 30 days of discharge from index admission (n = 583,199).
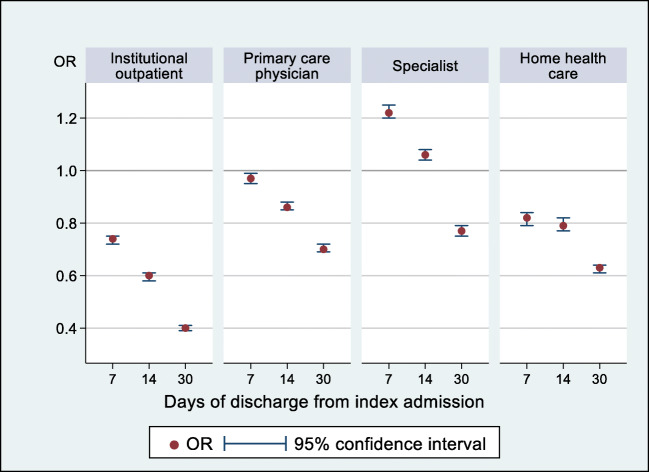
In multivariable logistic regressions (Fig. 2), institutional outpatient visits were most substantially associated with decreased unplanned 30-day readmission, with odds ratio (OR) 0.74 (95% confidence interval (CI) 0.72 to 0.75) at 7 days post-discharge and OR 0.40 (95% CI 0.39 to 0.41) at 30 days post-discharge. Conversely, 7-day (OR 1.22; 95% CI 1.20 to 1.25) and 14-day (OR 1.06; 95% CI 1.04 to 1.08) specialist visits were associated with increased readmission, while 30-day visits (OR 0.77; 95% CI 0.75 to 0.79) were associated with decreased readmission.
Figure 2.
Association of post-discharge health services utilization within 7 days, 14 days, and 30 days of discharge from index admission with unplanned 30-day readmission (n = 583,199). Notes: (i) In multivariable logistic models, odds ratio (OR) and 95% confidence interval (CI) were adjusted for 7 different types of post-discharge care (institutional outpatient, primary care physician, specialist, non-physician provider, emergency department, home health care, skilled nursing facility) and all other explanatory variables listed in Table 2. (ii) p <0.05 if 95% CI does not include one. (iii) Full estimation results are presented in Appendix Table 1, panel A.
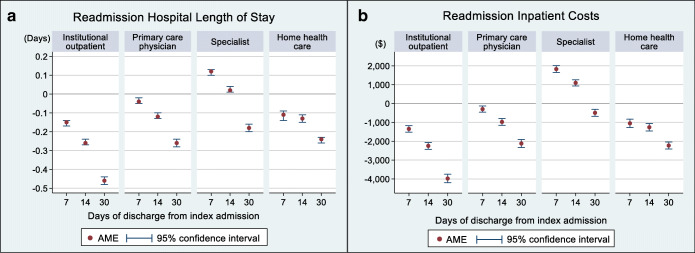
The multivariable two-part models for LOS (Fig. 3A) showed that average readmission LOS per IA discharge was lower by 0.15 days (AME −0.15; 95% CI −0.17 to −0.14) among patients with institutional outpatient visits within 7 days of discharge compared to those without. The AME of 7-day institutional outpatient visits on LOS is a difference in adjusted predicted LOS with and without visits. In our analysis, adjusted predicted LOS per IA discharge was 0.56 days and 0.71 days with and without visits, yielding AME −0.15 days. The AME is statistically significant at the 0.05 level if the 95% CI does not include zero. The AME of 30-day institutional outpatient visits was strengthened to −0.46 days (95% CI −0.48 to −0.44). Specialist visits within 7 days of IA discharge increased LOS by 0.12 days (AME 0.12; 95% CI 0.10 to 0.13), but negative association was observed with visits within 30 days of IA discharge (AME −0.18; 95% CI −0.20 to −0.16).
Figure 3.
Association of post-discharge health services utilization within 7 days, 14 days, and 30 days of discharge with 30-day readmission hospital length of stay (a) and readmission inpatient costs (b) (n = 583,199). Notes: (i) In multivariable two-part models, average marginal effect (AME) and 95% confidence interval (CI) were adjusted for 7 different types of post-discharge care (institutional outpatient, primary care physician, specialist, non-physician provider, emergency department, home health care, skilled nursing facility) and all other explanatory variables listed in Table 2. (ii) The AME represents the difference in adjusted predicted outcome (i.e., 30-day readmission hospital length of stay per IA discharge, and inpatient costs per IA discharge) between patients who did and did not utilize each post-discharge service. (iii) p <0.05 if 95% CI does not include zero. (iv) Full estimation results for 30-day readmission length of stay, and costs are presented in Appendix Tables 2 and 3 (panel A), respectively.
For inpatient costs (Fig. 3B), 7-day and 30-day post-discharge institutional outpatient visits reduced average readmission inpatient costs per IA discharge by $1345 (AME −1345; 95% CI −1516 to −1173) and $3977 (AME −3977; 95% CI −4203 to −3750), respectively. On the contrary, 7-day (AME 1829; 95% CI 1648 to 2011) and 14-day (AME 1099; 95% CI 934 to 1263) post-discharge specialist visits were associated with increased costs, while 30-day visits were associated with decreased costs (AME −492; 95% CI −674 to −309).
Home health care and PCP visits exhibited pattern similar to institutional outpatient visits for 30-day unplanned readmissions, LOS, and costs. Notably, ED visits were strongly associated with increases in three outcomes at all timepoints. There were no significant trends in readmission associated with non-physician provider visits and skilled nursing facilities. Full estimation results are presented in Appendix Tables 1, 2, and 3, panel A.
Estimates of subsample analyses showed that utilization of institutional outpatient, specialist, and skilled nursing facility care was more effective to reduce LOS and costs for the 6 conditions included in the HRRP than for all-cause IA. Full estimation results are presented in Appendix Tables 1, 2, and 3, panel B. Sensitivity analysis estimates were similar to those from the main analyses except that increases in the number of 7-day institutional outpatient visits did not continuously reduce 30-day readmission and costs.
DISCUSSION
Using Medicare claims data for all-cause IA, we found that institutional outpatient, home health care, and PCP visits at all post-discharge timepoints were associated with reduced 30-day unplanned readmissions, LOS, and inpatient costs. For specialist visits, 7-day and 14-day post-discharge visits were associated with an increase in readmission and resource utilization while 30-day visits were associated with a decrease in outcomes. ED visits at all timepoints were associated with increases in three outcomes.
As such, this study suggests that efforts to coordinate and encourage utilization of post-discharge services may be most effective if focused on certain types of services and timepoints. This focus is particularly important given that diverse health problems such as post-discharge syndrome, varying severity of unresolved illness, and new conditions,2,19–24,31,32 as well as poor quality care during IA,1,8,25,31,33–35 contribute to readmissions. Of note, in our study, only 18.1% of readmissions occurred for the same primary diagnosis as IA. Furthermore, previous, nationally representative inpatient data suggest that the leading diagnoses contributing to 7-day and 30-day readmissions are largely the same but their ranks vary, implying that changes in severity of illness or principal diagnosis over time contribute to readmission.2,17
This study makes several novel contributions to the literature. First, we accounted for all-cause IA because the Medicare Payment Advisory Commission has proposed expanding its readmission penalty program to cover all-cause IA.36 Most readmission studies have focused on the 6 specific diagnoses covered under the HRRP and provided no data regarding the generalizability of interventions or outcomes for other health conditions.1,2,8,22,31,35,37 Second, our study is the first to characterize 7 different types of post-discharge services and investigate their impact at 3 different timepoints. Most previous research has focused only on 7-day follow-up interventions conducted either by PCPs or any type of medical providers.1,8,25,31–35,37 However, their results have been mixed, partly because a single component or the aggregate of all care did not accurately assess the role of each type of service.1,35 In our analyses, utilization of 7 different types of post-discharge services was interdependent, and estimates of each service varied substantially when certain post-discharge services were excluded from multivariable regression. Third, we assessed the association of post-discharge services utilization with LOS and inpatient costs. Although a major goal of HRRP is reduction of unnecessary readmission resource utilization, most prior studies used unplanned 30-day readmission rate as a proxy due to lack of information.1,6–8,10,13,16,31,35,37
This is an observational study, and we cannot explicitly determine why the impact of post-discharge services varies by service types and timing. However, one potential explanation is that varying health conditions and needs determine patients’ choice of service types and timepoints, which, in turn, explain their associations with readmissions and resource utilization. Intuitively, patients with specific, high-risk concerns would be more likely to seek early visits to specialists, who might identify health problems for which inpatient care is necessary.38 Then, at timepoints further from IA discharge, patients may visit specialists due to less urgent health conditions, which would contribute to improved health status and reduced readmission. On the other hand, early PCP visits have the potential to provide holistic care to address multiple lingering health concerns and mitigate both the effects of potential relapse and post-discharge syndrome. Home health care was strongly associated with decreased readmission and resource utilization at all times, potentially because patients need these services for general health problems, not that these services were specifically effective to control particular readmission risks. Overall, the effects of post-discharges services of different types varied at early timepoints following discharge. However, their cumulative effects became similar at timepoints further from IA, contributing to reduced readmission and resource utilization regardless of the type of services.
ED visits are different than all other services as they are not scheduled, and generally, patients try to avoid them. In our study, ED visits were positively associated with all 3 outcomes at all timepoints, possibly due to high health risks and poor access to other post-discharge services.
Despite patients’ and providers’ best intentions, post-discharge follow-up can be delayed for many reasons. As a result, in 2013, the CMS adopted transitional care management services, which provide payment incentives for scheduling follow-up appointments within 14 days of discharge.39,40 However, in 2015, only 7.0% of eligible discharges among Medicare FFS beneficiaries included billing for this service,15 possibly implying limited clinical capacity for early follow-up or slow uptake of this billing code. Despite limited use of these billing codes, in our study, patients usually utilized post-discharge services, and approximately two-thirds of patients visited PCPs or specialists within 14 days of IA discharge. Of note, the rate of home health care utilization was approximately one-third of PCP visits, but both were similarly effective to reduce readmission and resource utilization. Accordingly, expansion of home health care could be an effective tool to reduce expensive post-discharge services and readmission resource utilization.
In 2011, the estimated annual Medicare cost of readmission was $26 billion, of which $17 billion was considered potentially avoidable.41,42 While the rate of unplanned readmission decreased substantially in the last decade,43 most readmissions remain unplanned1,33,43,44 and impose a significant economic burden on the health care system.15,31,34,35,37,45 Nonetheless, very few prior studies have investigated factors influencing LOS and costs associated with readmission,38,46,47 and due to the lack of information, researchers have often used readmission rates as a proxy for readmission resource utilization. Our study suggests that changes in readmission rates are not proportional to readmission resource utilization and alone cannot provide adequate knowledge to design interventions to contain costs.
Our study has several important limitations. First, in an observational study, we cannot control for potential unobserved confounders that may influence post-discharge services utilization (e.g., changes in post-discharge health status) and readmissions (e.g., patient engagement and compliance with treatment plan). Second, we do not have information on patient socioeconomic status that may influence readmission patterns.31,48 In this vein, we included two insurance status variables and clustered the observations by county, reasoning that the residents of each county would have similar dwelling, social, and medical infrastructure characteristics. Third, our results may not be generalizable beyond Medicare FFS beneficiaries because Medicare FFS does not require PCP referral or care within a provider network, thereby allowing flexibility in post-discharge services.
In summary, this study highlights the association of post-discharge services of different types and at different timepoints with unplanned 30-day readmission and resource utilization. These findings may inform strategies to reduce unplanned 30-day readmission and to guide medical resource utilization more effectively.
Supplementary Information
(PDF 212 kb)
Author Contribution
Dr. Tak had full access to all of the data in the study and takes the responsibility for the integrity of the data and the accuracy of the data analysis. All authors have made substantial contributions to this manuscript and attest to the validity and legitimacy of the data, as well as its interpretation.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 2.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shen E, Koyama SY, Huynh DN, et al. Association of a dedicated post-hospital discharge follow-up visit and 30-day readmission risk in a Medicare advantage population. JAMA Intern Med. 2017;177(1):132–135. doi: 10.1001/jamainternmed.2016.7061. [DOI] [PubMed] [Google Scholar]
- 4.Lee KK, Yang J, Hernandez AF, Steimle AE, Go AS. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365–372. doi: 10.1097/MLR.0000000000000492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McAlister FA, Youngson E, Kaul P, Ezekowitz JA. Early follow-up after a heart failure exacerbation. Circ Heart Fail. 2016;9(9). [DOI] [PubMed]
- 6.Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of early post-discharge follow-up by a primary care physician and 30-Day rehospitalization among older adults. J Gen Intern Med. 2015;30(5):565–571. doi: 10.1007/s11606-014-3106-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brooke BS, Stone DH, Cronenwett JL, et al. Early primary care provider follow-up and readmission after high-risk surgery. JAMA Surg. 2014;149(8):821–828. doi: 10.1001/jamasurg.2014.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664–1670. doi: 10.1001/archinternmed.2010.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eastwood CA, Quan H, Howlett JG, King-Shier KM. Factors associated with 7-day rehospitalization after heart failure admission. J Cardiovasc Nurs. 2017;32(4):339–347. doi: 10.1097/JCN.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 10.Baker H, Oliver-McNeil S, Deng L, Hummel SL. Regional hospital collaboration and outcomes in Medicare heart failure patients: see you in 7. JACC Heart Fail. 2015;3(10):765–773. doi: 10.1016/j.jchf.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collins S, Storrow AB, Albert NM, et al. Early management of patients with acute heart failure: State of the art and future directions. A consensus document from the Society for Academic Emergency Medicine/Heart Failure Society of America Acute Heart Failure Working Group. J Cardiac Fail. 2015;21(1):27–43. doi: 10.1016/j.cardfail.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bradley EH, Curry L, Horwitz LI, et al. Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes. 2013;6(4):444–450. doi: 10.1161/CIRCOUTCOMES.111.000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: A systematic review. Am J Med. 2012;125(9):915–921. doi: 10.1016/j.amjmed.2012.01.035. [DOI] [PubMed] [Google Scholar]
- 14.Leduc N, Tannenbaum TN, Bergman H, Champagne F, Clarfield AM, Kogan S. Compliance of frail elderly with health services prescribed at discharge from an acute-care geriatric ward. Med Care. 1998;36(6):904–914. doi: 10.1097/00005650-199806000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Bindman AB, Cox DF. Changes in health care costs and mortality associated with transitional care Management services after a discharge among Medicare beneficiaries. JAMA Intern Med. 2018;178(9):1165–1171. doi: 10.1001/jamainternmed.2018.2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jackson C, Shahsahebi M, Wedlake T, Dubard CA. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115–122. doi: 10.1370/afm.1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fingar K, Barrett M, Jiang J. A Comparison of All-Cause 7-Day and 30-Day Readmissions, 2014. Statistical Brief #230. Rockville, MD: Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP); 2017.
- 18.Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35(10):1867–1875. doi: 10.1377/hlthaff.2016.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tak HJ, Chen LW, Wilson FA, et al. Post-discharge services for different diagnoses than index hospitalization predict decreased 30-day readmissions among Medicare beneficiaries. J Gen Intern Med. 2019;34(9):1766–1774. doi: 10.1007/s11606-019-05115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brownlee SA, Blackwell RH, Blanco BA, et al. Impact of post-hospital syndrome on outcomes following elective, ambulatory surgery. Ann Surg. 2017;266(2):274–279. doi: 10.1097/SLA.0000000000001965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoyer EH, Needham DM, Atanelov L, Knox B, Friedman M, Brotman DJ. Association of impaired functional status at hospital discharge and subsequent rehospitalization. J Hosp Med. 2014;9(5):277–282. doi: 10.1002/jhm.2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyen HQ, Chu L, Amy Liu IL, et al. Associations between physical activity and 30-day readmission risk in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11(5):695–705. doi: 10.1513/AnnalsATS.201401-017OC. [DOI] [PubMed] [Google Scholar]
- 23.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441–1447. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 26.Horwitz LI, Grady JN, Dorsey KB, et al. 2014 Measure Updates and Specification Report: Hospital-Wide All-Cause Unplanned Readmission –Version 3.0. Prepared for the Centers for Medicare and Medicaid Services. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation; 2014. [Google Scholar]
- 27.Horwitz LI, Partovian C, Lin Z, et al. Hospital-Wide (All-Condition) 30-Day Risk-Standardized Readmission Measure: Measure Methodology Report. Prepared for the Centers for Medicare and Medicaid Services. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation; 2011. [Google Scholar]
- 28.Mullahy J. Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J Health Econ. 1998;17(3):247–281. doi: 10.1016/S0167-6296(98)00030-7. [DOI] [PubMed] [Google Scholar]
- 29.Belotti F, Dep P, Manning W, Norton E. TPM: Two-part models. Stata J. 2015;15(1):3–20. doi: 10.1177/1536867X1501500102. [DOI] [Google Scholar]
- 30.Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465–488. doi: 10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 31.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grafft CA, McDonald FS, Ruud KL, Liesinger JT, Johnson MG, Naessens JM. Effect of hospital follow-up appointment on clinical event outcomes and mortality. Arch Intern Med. 2010;170(11):955–960. doi: 10.1001/archinternmed.2010.105. [DOI] [PubMed] [Google Scholar]
- 33.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 34.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–1107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hackbarth G, Berenson R, Miller M. Report to the Congress: Medicare and the Health Care Delivery System. Medicare Payment Advisory Comission: Washington, D.C; 2013. [Google Scholar]
- 37.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 38.Hockenberry JM, Burgess JF, Glasgow J, Vaughan-Sarrazin M, Kaboli PJ. Cost of readmission: can the Veterans Health Administration (VHA) experience inform national payment policy? Medical Care. 2013;51(1):13–19. doi: 10.1097/MLR.0b013e31825c2fec. [DOI] [PubMed] [Google Scholar]
- 39.Medicare Learning Network. Transitional Care Management Services. ICN 908628. Centers for Medicare and Medicaid Services, Department of Health and Human Services. 2016. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Transitional-Care-Management-Services-Fact-Sheet-ICN908628.pdf. Accessed June 1, 2019.
- 40.Bindman AB, Blum JD, Kronick R. Medicare’s transitional care payment--a step toward the medical home. N Engl J Med. 2013;368(8):692–694. doi: 10.1056/NEJMp1214122. [DOI] [PubMed] [Google Scholar]
- 41.Hines A, Barrett M, Jiang J, Steiner C. Conditions with the Largest Number of Adult Hosptial Readmissions by Payer, 2011. Statistical Brief #172. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [PubMed]
- 42.Manning J, Zhao S, Anshutz M, Carman C, Philipson K. Performance of the Massachusetts Health Care System Series: Focus on Provider Quality. Boston, MA: Center for Health Information and Analysis; 2015. [Google Scholar]
- 43.Crosson F, Christianson J, Miller M. Report to the Congress: Medicare Payment Policy. Washington, D.C.: Medicare Payment Advisory Commission; 2017. [Google Scholar]
- 44.Carey K, Stefos T. The cost of hospital readmissions: evidence from the VA. Health Care Manag Sci. 2016;19(3):241–248. doi: 10.1007/s10729-014-9316-9. [DOI] [PubMed] [Google Scholar]
- 45.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301(6):603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 46.Chen LM, Jha AK, Guterman S, Ridgway AB, Orav EJ, Epstein AM. Hospital cost of care, quality of care, and readmission rates: penny wise and pound foolish? Arch Intern Med. 2010;170(4):340–346. doi: 10.1001/archinternmed.2009.511. [DOI] [PubMed] [Google Scholar]
- 47.Toth M, Holmes M, Van Houtven C, Toles M, Weinberger M, Silberman P. Rural-urban differences in the effect of follow-up care on postdischarge outcomes. Health Serv Res. 2017;52(4):1473–1493. doi: 10.1111/1475-6773.12543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ashton CM, Wray NP. A conceptual framework for the study of early readmission as an indicator of quality of care. Soc Sci Med. 1996;43(11):1533–1541. doi: 10.1016/S0277-9536(96)00049-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 212 kb)