Introduction
Spending on Alzheimer’s disease and related dementias (ADRD) is estimated at nearly $200 billion annually, an amount expected to nearly double by 2040.1 The extensive medical and long-term care needs, including high hospital rates and use of post-acute care that drive spending in this population, are best served through coordination among providers across care settings.2
Accountability for patient care coordination and spending has increased under Medicare's Bundled Payments for Care Improvement Advanced (BPCI-A) program, which holds hospitals accountable for spending during the 90-day post-discharge period. Research suggests that bundled payment models have reduced medical and surgical spending, particularly in post-acute care settings.3 However, the impact of these payment models on older patients with ADRD has not been explored. To decrease spending under BPCI-A, hospitals may seek to avoid admitting patients with ADRD or seek to discharge patients to lower acuity post-acute care settings.
To better understand bundled payments in the context of ADRD, we evaluated the prevalence of ADRD across the episodes included in BPCI-A and the association between ADRD and 90-day spending among hospitals participating in the BPCI-A program.
Methods
We used a 20 percent sample of Medicare fee-for-service claims (MedPAR, carrier files, outpatient institutional files) for older (≥ 65 years) beneficiaries discharged from acute care hospitals between January 1, 2013, and September 30, 2016 (the period used by CMS to determine target prices for model years 1 and 2 of BPCI-A). We identified hospital participation in the BPCI-A program using public data from CMS. We estimated the unadjusted prevalence of ADRD4 for the 29 episodes included in BPCI-A.5 We then estimated generalized linear models, adjusted for hospital and patient characteristics, to evaluate the association between ADRD and total 90-day spending, 90-day spending for skilled nursing facilities, and 90-day spending for inpatient rehabilitation. These associations were estimated across overall (adjusting for specific episodes with indicator variables) and for the 5 most common episodes in BPCI-A (sepsis, heart failure, pneumonia, chronic obstructive pulmonary disease (COPD), and cardiac arrhythmia).
Results
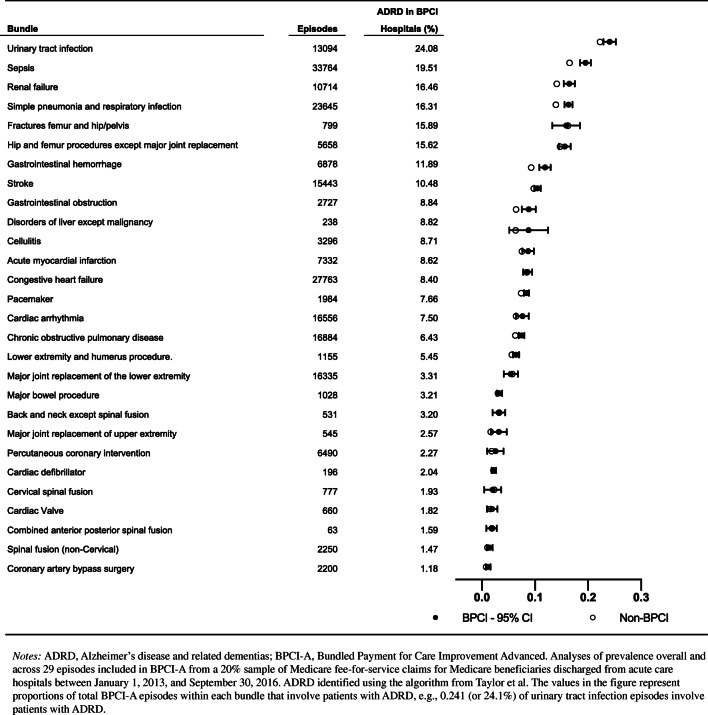
We identified 219,037 episode observations from 713 hospitals participating in BPCI-A, including 25,706 episode observations (11.7%) from patients with ADRD. We identified 2,007,780 discharges from 3,407 hospitals not participating in BPCI-A, including 181,548 episode observations (9.04%) from patients with ADRD.
Among hospitals participating in BPCI-A, unadjusted prevalence of ADRD patients in episodes was 11.7% overall, ranging from 1–24% (Fig. 1). It was low for elective cardiac procedures (~ 1–2% for CABG and cardiac valve) and spinal fusion (~ 1–2%), moderate for chronic obstructive pulmonary disease (~ 6%) and cardiac conditions (~ 8–9% for congestive heart failure, arrhythmia, and AMI), high for other incident events (10% for stroke, 12% for gastrointestinal hemorrhage), and highest for infections (16% for pneumonia, 20% for sepsis, and 24% for urinary tract infection). The prevalence of ADRD was very similar for hospitals not participating in BPCI-A.
Figure 1.
Prevalence of Alzheimer’s disease and related dementias in episodes among BPCI-A and non-BPCI-A hospitals.
ADRD was associated with a 4% increase in total 90-day spending ($883 [$20,876 vs. $19,993], p < 0.001) and a 26% increase in 90-day post-acute spending ($952 [$4,565 vs. $3,613], p < 0.001) (Fig. 2). Total 90-day spending was also consistently higher for ADRD patients for the 5 highest-volume episodes: differences of $1,012 for sepsis, $825 for CHF, $766 for pneumonia, $646 for COPD, and $602 for cardiac arrhythmia (p < 0.001 for all episodes). Similar patterns were observed for SNF spending across the highest-volume episodes.
Figure 2.
Incremental association between Alzheimer’s disease and related dementias status and episode spending for most common episodes in BPCI-A.
Discussion
In this national study of bundled payments, we observed high variation in the prevalence of ADRD patients across clinical episodes. There was limited inclusion of these patients into elective joint and cardiac procedures but greater inclusion into medical bundles including urinary tract infection, pneumonia, and sepsis. Across episodes, the prevalence of ADRD was similar between hospitals participating and not participating in BPCI-A. ADRD was associated with somewhat greater total spending and much greater spending on post-acute care.
One limitation of our study stems from our lack of access to spending related to home health. While a relatively small component of episode spending, future research should examine patterns for home health spending for patients with ADRD.
Reducing post-acute care is a key mechanism for savings in BPCI-A. Because ADRD is associated with higher episode spending, our findings highlight the importance of closely monitoring the experience of these patients under BPCI-A to ensure they are receiving appropriate care. An unpublished CMS contractor report found that, for some episodes, BPCI (the precursor to BPCI-A) was associated with relatively larger reductions in 90-day spending for patients with ADRD for some episodes, without consistent evidence of a decline in quality measures.6 Understanding these effects in BPCI-A—with a different composition of episodes selected by hospitals—is critical. This is particularly important for episodes like sepsis and pneumonia that are common among patients with ADRD and also highly prevalent under BPCI-A.
Authors’ Contribution
Author GJH was supported by the University of Michigan Older Americans Independence Center Research Education Core (AG024824) and University of Michigan Pepper Center pilot (AG024824) during the analyses and drafting of the manuscript.
Funding
Author GJH is supported by the Agency for Healthcare Research and Quality (1R03HS025838-01A1) and the University of Michigan Older Americans Independence Center Research Education Core (AG024824) and University of Michigan Pepper Center pilot (AG024824).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mehta KM, Yeo GW. Systematic review of dementia prevalence and incidence in United States race/ethnic populations. Alzheimers Dement. 2017;13(1):72–83. doi: 10.1016/j.jalz.2016.06.2360. [DOI] [PubMed] [Google Scholar]
- 2.Thyrian JR, Hertel J, Wucherer D, et al. Effectiveness and Safety of Dementia Care Management in Primary Care: A Randomized Clinical Trial. JAMA Psychiatry. 2017;74(10):996–1004. doi: 10.1001/jamapsychiatry.2017.2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Navathe AS, Troxel AB, Liao JM, et al. Cost of Joint Replacement Using Bundled Payment Models. JAMA Intern Med. 2017;177(2):214–222. doi: 10.1001/jamainternmed.2016.8263. [DOI] [PubMed] [Google Scholar]
- 4.Taylor DH, Jr, Ostbye T, Langa KM, Weir D, Plassman BL. The accuracy of Medicare claims as an epidemiological tool: the case of dementia revisited. J Alzheimers Dis. 2009;17(4):807–815. doi: 10.3233/JAD-2009-1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CMS. Bundled Payments for Care Improvement (BPCI) Initiative: General Information. Centers for Medicare & Medicaid Services. Available at: https://innovation.cms.gov/innovation-models/bundled-payments. Published 2020. Accessed April 17, 2020.
- 6.CMS Bundled Payments for Care Improvement Initiative Models 2-4: Year 5 Evaluation & Monitoring Annual Report. Published 2018. Available at: https://downloads.cms.gov/files/cmmi/bpci-models2-4-yr5evalrpt.pdf Accessed: July 15, 2020.