Abstract
Fluid management is an important component of perioperative care for patients undergoing neurosurgery. The primary goal of fluid management in neurosurgery is the maintenance of normovolemia and prevention of serum osmolarity reduction. To maintain normovolemia, it is important to administer fluids in appropriate amounts following appropriate methods, and to prevent a decrease in serum osmolarity, the choice of fluid is essential. There is considerable debate about the choice and optimal amounts of fluids administered in the perioperative period. However, there is little high-quality clinical research on fluid therapy for patients undergoing neurosurgery. This review will discuss the choice and optimal amounts of fluids in neurosurgical patients based on the literature, recent issues, and perioperative fluid management practices.
Keywords: Albumin, Colloids, Crystalloid solutions, Fluid therapy, Hemodynamics, Neurosurgery
INTRODUCTION
Fluid management is part of the basic care in many clinical situations. Perioperative fluid therapy in patients undergoing neurosurgery is a vital component of anesthetic practice and critical care. There is increasing evidence that intraoperative fluid therapy may influence postoperative outcomes [1–3].
The main purpose of fluid management in neurosurgical anesthesia is to prevent brain damage caused by inadequate cerebral perfusion and provide a good surgical environment. Therefore, it is essential to maintain hemodynamic stability and proper cerebral perfusion pressure during neurosurgery.
Hemodynamic alterations and electrolyte imbalances often occur during neurosurgery because of the frequent use of diuretics to relieve increased intracranial cerebral pressure and edema. In addition, depending on the type of surgery, large amounts of fluids may need to be administered to correct preoperative hypovolemia and perioperative unstable hemodynamics, and prevent cerebral vasospasm.
An extensive debate about the choice and optimal dose of fluid for hemodynamic stability and improved outcomes exists.
This review is intended to assist in the clinical applications and research on fluid therapy during neurosurgery by reviewing recent issues and literature on perioperative fluid therapy in various surgical fields, including neurosurgery.
CHOICE OF FLUID IN NEUROSURGICAL PATIENTS
The general principle of fluid therapy for neurosurgery is to maintain normal blood volume and prevent a decrease in plasma osmolarity. In a normal blood-brain barrier (BBB), the movement of water between the plasma and brain is mainly influenced by the osmotic gradient. Therefore, in neurosurgery, the osmolarity of the fluid is the most important factor to prevent cerebral edema.
A crystalloid fluid contains small molecular substances without high molecular substances, and it is classified as hypotonic, isotonic, or hypertonic according to its osmolarity. Lactated Ringer's solution (LR), a commonly used crystalloid, is hypotonic at 273 mOsm/L. Low plasma osmolarity can cause cerebral edema. Therefore, hypotonic solutions, such as LR, are avoided, while normal saline (NS) has traditionally been used as the main fluid in patients with neurosurgery [4].
Since a reduction in oncotic pressure without changing the osmolarity increases cerebral edema in animal models of brain injury [5], colloid solutions have been known to prevent the severe reduction of colloidal oncotic pressure when used appropriately. However, the European Society of Intensive Care Medicine (ESICM) task force recommended against the use of colloids in patients with brain injury [6], continuing the debate about the use of colloids in neurosurgery.
Crystalloid solutions
Hypotonic solutions, such as the LR solution, are avoided in neurosurgical patients to minimize cerebral fluid accumulation. In contrast, NS, an isotonic crystalloid, has been widely used in neurosurgery because it is thought to reduce the risk of cerebral edema [7]. However, since NS has equal amounts of sodium and chloride (154 mEq/L), hyperchloremic metabolic acidosis occurs when a large amount of NS is administered because its chloride concentration is higher than the normal plasma chloride concentration (96–106 mEq/L).
Numerous laboratory and clinical studies have reported a dose-dependent association between hyperchloremia and the use of NS [8–10]. Hyperchloremic acidosis is associated with acute kidney injury (AKI) during abdominal surgery [9]. In a large, propensity-matched retrospective study of 22,851 patients who underwent a non-cardiac surgery, postoperative hyperchloremia resulted in acute metabolic acidosis, leading to increased 30-days mortality and length of hospital stay [10]. A large retrospective study on abdominal surgery showed that patients treated with balanced crystalloids had better outcomes, including mortality, postoperative infection, need for renal replacement therapy (RRT), need for transfusions, electrolyte imbalance, and acidosis than those treated with NS [9].
Meanwhile, the adverse outcomes of NS were not observed in a randomized control study of critically ill patients [11,12], non-critically ill patients [13], and postoperative patients who underwent neurosurgery [14]. In a recent meta-analysis, the balanced crystalloid solution was beneficial in significantly reducing postoperative hyperchloremia and metabolic acidosis, but the evidence was insufficient to compare the effects of buffered and non-buffered crystalloids on mortality and organ failure [15].
In contrast, balanced salt solutions (BSSs) replace chloride ions with lactate, acetate, and gluconate, which prevents the occurrence of hyperchloremic metabolic acidosis [16]. A BSS is the most common choice of resuscitation fluid in clinical practice [17]. In patients who underwent craniotomy, the NS group had higher sodium and chloride levels and had more patients with marked acidosis than in the BSS group [18].
However, though LR is a balanced crystalloid solution, it is hypotonic. A decrease of 1 mOsm/L in the plasma osmolality results in an increase of 19 mmHg in the pressure of fluid movements across the BBB, and a 3% decrease in the plasma osmolarity results in cerebral edema with a 3% increase in the brain volume and 30% decrease in the intracranial blood cerebrospinal fluid volume [16,19]. Prehospital resuscitation with LR compared to NS was associated with increased mortality in patients with traumatic brain injuries (TBI) [20]. Therefore, LR is not suitable for neurosurgical patients. Instead, isotonic BSS, excluding hypotonic solutions, such as LR, has emerged as a fluid of choice for patients undergoing neurosurgery [21].
An isotonic balanced solution reduces the incidence of hyperchloremic metabolic acidosis and electrolyte imbalances in patients with brain injury, but the intracranial pressure is not different compared with NS [22]. Although a balanced solution has a clear benefit of reducing hyperchloremic metabolic acidosis, its advantage of reducing morbidity and mortality is not clear and requires evaluation.
High-quality data comparing NS and balanced solutions in perioperative and neurosurgical patients are not yet available. Based on the above evidence, although evidence is still lacking, an isotonic balanced solution is preferred over NS in neurosurgical patients because of the lower risk of metabolic acidosis and renal injury.
Colloid solutions
Large insoluble molecules in colloid solutions increase the intravascular oncotic pressure. In an animal model of brain injury, oncotic pressure reduction without changing the osmolarity increased cerebral edema [5]. Colloid solutions have commonly been used to decrease cerebral edema and improve hemodynamics during neurosurgery [23].
1. Hydroxyethyl starch (HES)
Several randomized trials have shown that HES has adverse effects on kidney function. The routine clinical application of HES in patients with severe sepsis in the VISEP study [24] was associated with higher rates of acute renal failure and RRT than LR. Similarly, two large trials comparing colloids and crystalloids in patients with severe sepsis, the 6S trial [25] and CHEST trial [26], showed an increased incidence of AKI and need for RRT.
In contrast, there was no difference in the incidence of renal failure and mortality between saline and HES 130/0.4 in patients with severe sepsis in the CRYSTMAS trial [27]. Likewise, the CRISTAL study, a large, randomized trial, [28], compared the effects of colloids and crystalloids in critically ill patients with hypovolemia and found no significant differences in the 28-day mortality and need for RRT.
Due to the conflicting results, a systematic review and meta-analysis that included the above trials concluded that HES significantly increased the risk of mortality and AKI in critically ill patients [29]. The ESICM task force on colloid volume therapy in critically ill patients recommended against the use of 6% HES 130 in patients with severe sepsis or at risk of AKI. They also recommended not to use colloids in patients with head injuries [6]. Based on accumulating evidence, the European Medicines Agency has restricted the use of HES in critically ill patients, and the United States Food and Drug Administration has added a black box warning. A recent meta-analysis comparing colloids versus crystalloids for fluid resuscitation in critically ill patients showed little or no difference in mortality with moderate-certainty evidence, though starches slightly increased the need for blood transfusion and RRT [30]. However, the heterogeneity of protocols and results in the aforementioned research continues to cause controversy on the recommendations on HES restrictions.
There is some opposing evidence on the restricted use of HES in patients with neurosurgery.
Some animal models and in vitro studies have shown protective effects of HES on the BBB [31–33]. Two early randomized control trials comparing HES with crystalloid solutions in patients with ischemic stroke reported no differences in the safety, hemodynamic efficacy, and complication rates [34,35].
HES has been sometimes used to maintain an optimal volume status to prevent delayed cerebral ischemia (DCI) due to cerebral vasospasm following a subarachnoid hemorrhage (SAH) as a component of the triple H-therapy. Compared to the standard therapy group, the goal-directed fluid therapy (GDFT) with a HES bolus group showed reduced frequencies of vasospasm and cardiopulmonary complications [36]. A recent retrospective study compared SAH patients who received HES with those who received crystalloids and found no significant difference in RRT [37]. Another retrospective study showed no positive correlation between the cumulative doses of HES and serum creatinine in SAH patients who had a normal renal function and concluded that the administration of HES 6% 130/0.4 is safe in SAH patients without pre-existing renal insufficiency. However, caution is warranted in the period of repetitive administration of contrast media [38]. It is noteworthy that the incidence of AKI did not increase despite the substantial amount of HES used in the above trials.
However, there is still no evidence of the superiority of the use of HES in patients undergoing neurosurgery. The possible negative effects, such as renal injury and coagulopathy, should be considered, and HES should be used with caution in neurosurgical patients, in line with the do not harm principle.
2. Albumin
In animal studies, high-concentration albumin therapy improved local cerebral blood flow (CBF), reduced infarct size and brain swelling, and improved neurological function [39–41]. In a retrospective study of patients with SAH, there was a higher proportion of patients with good outcomes at 3 months in the albumin group than in the non-albumin group, although there was no significant difference in the incidence of symptomatic vasospasm [42].
However, the SAFE trial, a multicenter, randomized, double-blinded trial, compared 4% albumin and NS in critically ill patients and showed no significant difference in the outcomes, such as mortality, proportions of organ failures, duration of intensive care unit (ICU) stay, duration of hospital stay, duration of mechanical ventilation, and duration of RRT [43]. However, in the subgroup analysis, the relative risk (RR) of death of trauma patients in the albumin group compared to the saline group (RR = 1.36) was higher than that in the patients without trauma (RR = 0.96). This difference in the RR of death was because more brain injury patients were assigned to the albumin group than to the saline group.
A post-hoc analysis of a subgroup of patients with TBI in the SAFE trial, the SAFE-TBI study, showed that the 2-year mortality of patients with severe brain injury was significantly higher in the albumin group than in the saline group [44]. A post-hoc follow-up analysis of severe TBI suggested that increased intracranial pressure may have contributed to the high mortality in the albumin group [7]. The results of the SAFE trial and post-hoc analysis continue to influence albumin use in patients with TBI [45].
However, these results should be considered with caution. The SAFE-TBI trial has its own limitations in post hoc subgroup analysis. The mortality of TBI patients was not the primary endpoint of the SAFE trial, and the trial design was not randomized for TBI analysis. Furthermore, the 4% human albumin used in the SAFE study is a hypo-osmolar solution that may potentially increase the intracranial pressure and cause cerebral edema [46].
Experimental SAH models on animals have demonstrated the beneficial effects of albumin [39,47,48], and there has been some evidence on the beneficial effects of albumin in SAH patients [49,50].
The ALISAH trial [49], designed to determine the feasibility and safety of albumin administration in SAH patients, was terminated as two serious complications of pulmonary edema were reported. Patients receiving 1.25 g/kg/d of 25% albumin for 7 days demonstrated better neurological outcomes than those receiving a lower dose. Follow-up analysis of the ALISAH trial showed that higher doses of albumin were associated with a lower incidence of vasospasm, DCI, and cerebral infarction [50]. However, these results should be interpreted with caution. The said trial had an inadequate sample size and insufficient power because it was not designed to study the beneficial effects of albumin.
The ALIAS pilot trial suggested that high-dose albumin therapy has potential neuroprotective effects after ischemic stroke [51]. However, the ALIAS part 1 trial was suspended after safety analysis revealed an increased incidence of pulmonary edema and mortality [52]. The ALIAS part 2 trial, which was modified by adding exclusion criteria and safety measures, was also suspended because of the high incidence of pulmonary edema in the albumin group [53]. The pooled analysis of the data from the ALIAS part 1 and 2 trials showed no difference in the 90-day neurological outcomes and mortality between the 25% albumin and saline groups. However, there was an increased risk of pulmonary edema and intracerebral hemorrhage in the patients administered with albumin 25% at 2 g/kg [54]. Based on this evidence, the ESICM recommends against the use of high-dose albumin in patients with acute ischemic stroke and the use of low- (4%) or high-dose (20–25%) albumin in neurointensive care patients [55].
Although controversies still exist based on the above evidence, the use of albumin in the perioperative period of neurosurgery remains questionable. The potential risks and benefits of albumin administration should be assessed on a case-by-case basis.
HOW TO ADMINISTER THE OPTIMAL AMOUNT OF FLUIDS IN NEUROSURGICAL PATIENTS
The primary goal of perioperative fluid management during neurosurgery is to maintain hemodynamic stability and an adequate CBF. There is a growing body of evidence that intraoperative fluid therapy influences postoperative outcomes [1–3].
Restrictive versus liberal fluid therapy in major surgeries
Traditional intraoperative fluid regimens, which include preoperative dehydration, third space loss, and insensible loss, tend to induce a positive fluid balance that is related to postoperative complications [1].
In the recent decade, several randomized controlled studies have compared restricted fluid therapy with liberal fluid therapy in patients undergoing major abdominal surgeries. Brandstrup et al. [2] showed that patients in the liberal group gained body weight and had more complications than the restrictive group.
After this trial, numerous studies on abdominal surgery showed positive results for restricted fluid therapy, leading to a gradual shift to the trend of using fluid restriction during surgery with the concept of zero-balance. However, in two large observational studies, the zero-balance concept has been concerning due to the possibility of worse outcomes, including AKI associated with excessive restriction [56,57].
Recently, RELIEF trial compared restrictive fluid therapy while maintaining perioperative zero balance with liberal fluid therapy [3]. The results showed that the patients in the restriction group had increased rates of surgical site infection and high risks of AKI.
Based on this recent evidence, worse perioperative outcomes have been observed in patients with both overhydration and excessive fluid restriction. Therefore, fluid optimization is essential for perioperative fluid management. It should also be noted that the amounts of administered volume in the liberal and restricted volume therapies were inconsistent and slightly different for each study [58]. In particular, the postoperative weight gain of the restrictive group in an earlier study by Brandstrup et al. [2] was comparable to the liberal group of the RELIEF study [3]. As such, an excessive restriction can result in worse outcomes, such as AKI.
GDFT based on dynamic parameters
To achieve the optimal fluid volume status, it is essential to avoid overhydration and excessive restriction and develop individually optimized fluid regimens using objective parameters. These objective parameters should be targeted preoperatively and measured perioperatively.
GDFT, a recently emerging fluid regimen, is a type of fluid administration that optimizes pre-defined targets based on directly measured hemodynamic parameters (Fig. 1), such as the cardiac output, stroke volume (SV), stroke volume variation (SVV), pulse pressure variation (PPV), systolic pressure variation (SPV), pleth variability index (PVI), and other factors [1].
Fig. 1.
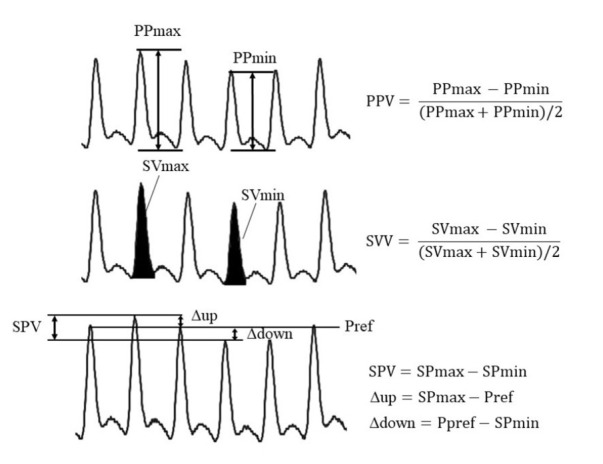
Dynamic parameters derived from the arterial pressure wave. Mechanical ventilation induces periodic changes in the arterial waveform. Various parameters are derived from this periodic change. Pulse pressure (PP) is the difference between the systolic and diastolic pressures. The area under curve of the arterial pressure wave represents the stroke volume (SV). Systolic pressure variation (SPV) is the difference between the maximum and minimal systolic pressures. SPV consists of two components, delta up (Δup) and delta down (Δdown), by reference pressure (Pref). Pref is the systolic pressure measured at the end of expiration or during apnea. PPV: pulse pressure variation, SVV: stroke volume variation.
Favorable outcomes and decreased costs have been shown for patients who underwent GDFT during a major abdominal surgery [59-61]. Although the certainty of the evidence was very low, a meta-analysis comparing GDFT and restrictive fluid therapy in major non-cardiac surgeries showed that the mortality was slightly low in the GDFT group, and there were no differences between the two groups in the complication rate and length of hospital stay [1]. Unlike other studies, including this meta-analysis, one study [62] found that the total infused volume was higher in the restrictive group (basal crystalloid infusion ranging from 4 to 10 ml/kg/h) than in the GDFT group. A limitation of this meta-analysis was the lack of a definition of restrictive fluid therapy. GDFT consists of a given basal infusion and repeated boluses of fluids (usually colloids) to achieve a predefined target. The basal infusion rate is particularly important to compare GDFT with other fluid regimens.
GDFT during neurosurgery
In two retrospective studies of patients with SAH, a positive net fluid balance was independently associated with poor outcomes [63,64]. However, as it is difficult to compare restrictive and liberal fluid therapies in neurosurgical patients who must maintain euvolemia, recent studies on GDFT have been conducted. There have been some studies to optimize fluid administration using continuously measured dynamic parameters, such as SVV, PPV, and PVI for patients undergoing neurosurgery.
The SVV is a sensitive predictor of fluid responsiveness before and during brain surgery [65–67]. After the induction of anesthesia and before the start of the surgical procedure, the SVV more sensitively predicted an increase of more than 10% in the SV by LR solution infusion compared to the mean arterial pressure, heart rate, cardiac output, and central venous pressure (CVP) in neurosurgical patients [65]. An SVV of 9.5% was concluded as the optimal threshold (sensitivity: 78.6%, specificity: 93%) for predicting a > 5% increase in the SV after a 100-ml colloid solution infusion [66]. The target of the SVV of GDFT can affect clinical outcomes for supratentorial brain tumor resection [67]. Comparing two GDFT regimens for supratentorial tumor resection (with threshold SVV values set at 10 for the low SVV group and at 18 for the high SVV group), the low SVV group had lower postoperative serum lactate levels, shorter length of ICU stay, and a lower incidence of postoperative neurologic events than the high SVV group [67]. Comparing the GDFT group managed fluid by hemodynamic parameters including the SVV with the control group managed fluid by the therapeutic decision of the attending anesthesiologist, the former had less administered fluids, shorter length of ICU stay, lower ICU costs, and lower lactate levels than the control group [68].
The PPV and PVI have also been reported to be good predictors of fluid reactivity during brain surgery [69–72]. Between the CVP group, which maintained a CVP of 5–10 cmH2O, and the PPV group, which maintained a PPV below 13%, in patients undergoing a brain tumor surgery, the latter had better postoperative hemodynamic stability and less postoperative fluid requirement [69]. The PPV-guided GDFT during supratentorial tumor resection had a comparable brain relaxation scale, low serum lactate levels, more intraoperative fluids, and higher urine output than the standard care group [70]. In the sitting position for neurosurgery, measuring the PPV and PVI with an ear sensor predicted fluid responsiveness well, but the PVI could not be predicted with a finger sensor. However, the PVI measured with an ear sensor was limited by an unreliable signal in 26% of the patients [71].
A study on children undergoing neurosurgery showed different results. Comparing the PVI, ΔVpeak (respiratory variations in aortic blood flow peak velocity), arterial pressure, CVP, heart rate, inferior vena cava diameter, SPV (including delta up [Δup] and delta down [Δdown]), and PPV in pediatric patients undergoing neurosurgery, the PVI and ΔVpeak predicted the fluid response well, but the PPV and other static and dynamic parameters were reported to be unpredictable [72].
Considering that hemodynamic changes are relatively common in neurosurgery, GDFT, which provides individualized optimal fluid status, is a promising fluid management strategy.
CONCLUSION
Despite numerous studies on perioperative fluid management, there is insufficient evidence to draw definitive conclusions regarding fluid management in neurosurgical patients.
Although evidence is still lacking, isotonic balanced crystalloid solutions should be considered the first-choice fluid, while hypotonic solutions should be avoided. Furthermore, colloid solutions should be used with caution, and their potential risks and benefits should be considered.
To achieve an optimal fluid volume status while avoiding overhydration and excessive restriction, the amount and duration of fluid administration should be considered, and an individualized fluid strategy is recommended using GDFT based on dynamic fluid parameters.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
Not applicable.
REFERENCES
- 1.Wrzosek A, Jakowicka-Wordliczek J, Zajaczkowska R, Serednicki WT, Jankowski M, Bala MM, et al. Perioperative restrictive versus goal-directed fluid therapy for adults undergoing major non-cardiac surgery. Cochrane Database Syst Rev. 2019;12:CD012767. doi: 10.1002/14651858.CD012767.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brandstrup B, Tønnesen H, Beier-Holgersen R, Hjortsø E, Ørding H, Lindorff-Larsen K, et al. Danish Study Group on Perioperative Fluid Therapy. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641–8. doi: 10.1097/01.sla.0000094387.50865.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D, et al. Australian and New Zealand College of Anaesthetists Clinical Trials Network and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med. 2018;378:2263–74. doi: 10.1056/NEJMoa1801601. [DOI] [PubMed] [Google Scholar]
- 4.Tommasino C, Picozzi V. Volume and electrolyte management. Best Pract Res Clin Anaesthesiol. 2007;21:497–516. doi: 10.1016/j.bpa.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Drummond JC, Patel PM, Cole DJ, Kelly PJ. The effect of the reduction of colloid oncotic pressure, with and without reduction of osmolality, on post-traumatic cerebral edema. Anesthesiology. 1998;88:993–1002. doi: 10.1097/00000542-199804000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Reinhart K, Perner A, Sprung CL, Jaeschke R, Schortgen F, Johan Groeneveld AB, et al. European Society of Intensive Care Medicine. Consensus statement of the ESICM task force on colloid volume therapy in critically ill patients. Intensive Care Med. 2012;38:368–83. doi: 10.1007/s00134-012-2472-9. [DOI] [PubMed] [Google Scholar]
- 7.Cooper DJ, Myburgh J, Heritier S, Finfer S, Bellomo R, Billot L, et al. SAFE-TBI Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group. Albumin resuscitation for traumatic brain injury: is intracranial hypertension the cause of increased mortality? J Neurotrauma. 2013;30:512–8. doi: 10.1089/neu.2012.2573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quilley CP, Lin YS, McGiff JC. Chloride anion concentration as a determinant of renal vascular responsiveness to vasoconstrictor agents. Br J Pharmacola. 1993;108:106–10. doi: 10.1111/j.1476-5381.1993.tb13447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaw AD, Bagshaw SM, Goldstein SL, Scherer LA, Duan M, Schermer CR, et al. Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann Surg. 2012;255:821–9. doi: 10.1097/SLA.0b013e31825074f5. [DOI] [PubMed] [Google Scholar]
- 10.McCluskey SA, Karkouti K, Wijeysundera D, Minkovich L, Tait G, Beattie WS. Hyperchloremia after noncardiac surgery is independently associated with increased morbidity and mortality: a propensity-matched cohort study. Anesth Analg. 2013;117:412–21. doi: 10.1213/ANE.0b013e318293d81e. [DOI] [PubMed] [Google Scholar]
- 11.Semler MW, Self WH, Wanderer JP, Ehrenfeld JM, Wang L, Byrne DW, et al. SMART Investigators and the Pragmatic Critical Care Research Group. Balanced crystalloids versus saline in critically ill adults. N Engl J Med. 2018;378:829–39. doi: 10.1056/NEJMoa1711584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young P, Bailey M, Beasley R, Henderson S, Mackle D, McArthur C, et al. SPLIT Investigators; ANZICS CTG. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: the SPLIT randomized clinical trial. JAMA. 2015;314:1701–10. doi: 10.1001/jama.2015.12334. [DOI] [PubMed] [Google Scholar]
- 13.Self WH, Semler MW, Wanderer JP, Wang L, Byrne DW, Collins SP, et al. SALT-ED Investigators. Balanced crystalloids versus saline in noncritically ill adults. N Engl J Med. 2018;378:819–28. doi: 10.1056/NEJMoa1711586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hassan MH, Hassan WMNW, Zaini RHM, Shukeri WFWM, Abidin HZ, Eu CS. Balanced fluid versus saline-based fluid in post-operative severe traumatic brain injury patients: acid-base and electrolytes assessment. Malays J Med Sci. 2017;24:83–93. doi: 10.21315/mjms2017.24.5.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odor PM, Bampoe S, Dushianthan A, Bennett-Guerrero E, Cro S, Gan TJ, et al. Perioperative administration of buffered versus non-buffered crystalloid intravenous fluid to improve outcomes following adult surgical procedures: a Cochrane systematic review. Perioper Med (Lond) 2018;7:27. doi: 10.1186/s13741-018-0108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dąbrowski W, Woodcock T, Rzecki Z, Malbrain MLNG. The use of crystalloids in traumatic brain injury. Anaesthesiol Intensive Ther. 2018;50:150–9. doi: 10.5603/AIT.a2017.0067. [DOI] [PubMed] [Google Scholar]
- 17.Hammond NE, Taylor C, Finfer S, Machado FR, An Y, Billot L, et al. Fluid-TRIPS and Fluidos Investigators; George Institute for Global Health, The ANZICS Clinical Trials Group, BRICNet, and the REVA research Network. Patterns of intravenous fluid resuscitation use in adult intensive care patients between 2007 and 2014: an international cross-sectional study. PLoS One. 2017;12:e0176292. doi: 10.1371/journal.pone.0176292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hafizah M, Liu CY, Ooi JS. Normal saline versus balanced-salt solution as intravenous fluid therapy during neurosurgery: effects on acid-base balance and electrolytes. J Neurosurg Sci. 2017;61:263–70. doi: 10.23736/S0390-5616.16.03221-5. [DOI] [PubMed] [Google Scholar]
- 19.Hladky SB, Barrand MA. Mechanisms of fluid movement into, through and out of the brain: evaluation of the evidence. Fluids Barriers CNS. 2014;11:26. doi: 10.1186/2045-8118-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rowell SE, Fair KA, Barbosa RR, Watters JM, Bulger EM, Holcomb JB, et al. The impact of pre-hospital administration of lactated Ringer's solution versus normal saline in patients with traumatic brain injury. J Neurotrauma. 2016;33:1054–9. doi: 10.1089/neu.2014.3478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15. doi: 10.1227/NEU.0000000000001432. [DOI] [PubMed] [Google Scholar]
- 22.Roquilly A, Loutrel O, Cinotti R, Rosenczweig E, Flet L, Mahe PJ, et al. Balanced versus chloride-rich solutions for fluid resuscitation in brain-injured patients: a randomised double-blind pilot study. Crit Care. 2013;17:R77. doi: 10.1186/cc12686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Exo JL, Shellington DK, Bayir H, Vagni VA, Janesco-Feldman K, Ma L, et al. Resuscitation of traumatic brain injury and hemorrhagic shock with polynitroxylated albumin, hextend, hypertonic saline, and lactated Ringer's: effects on acute hemodynamics, survival, and neuronal death in mice. J Neurotrauma. 2009;26:2403–8. doi: 10.1089/neu.2009.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, et al. German Competence Network Sepsis (SepNet). Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39. doi: 10.1056/NEJMoa070716. [DOI] [PubMed] [Google Scholar]
- 25.Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Åneman A, et al. 6S Trial Group; Scandinavian Critical Care Trials Group. Hydroxyethyl starch 130/0.42 versus Ringer's acetate in severe sepsis. N Engl J Med. 2012;367:124–34. doi: 10.1056/NEJMoa1204242. [DOI] [PubMed] [Google Scholar]
- 26.Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, et al. CHEST Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901–11. doi: 10.1056/NEJMoa1209759. [DOI] [PubMed] [Google Scholar]
- 27.Guidet B, Martinet O, Boulain T, Philippart F, Poussel JF, Maizel J, et al. Assessment of hemodynamic efficacy and safety of 6% hydroxyethylstarch 130/0.4 vs. 0.9% NaCl fluid replacement in patients with severe sepsis: the CRYSTMAS study. Crit Care. 2012;16:R94. doi: 10.1186/cc11358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Annane D, Siami S, Jaber S, Martin C, Elatrous S, Declère AD, et al. CRISTAL Investigators. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA. 2013;310:1809–17. doi: 10.1001/jama.2013.280502. [DOI] [PubMed] [Google Scholar]
- 29.Zarychanski R, Abou-Setta AM, Turgeon AF, Houston BL, McIntyre L, Marshall JC, et al. Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. JAMA. 2013;309:678–88. doi: 10.1001/jama.2013.430. [DOI] [PubMed] [Google Scholar]
- 30.Lewis SR, Pritchard MW, Evans DJ, Butler AR, Alderson P, Smith AF, et al. Colloids versus crystalloids for fluid resuscitation in critically ill people. Cochrane Database Syst Rev. 2018;8:CD000567. doi: 10.1002/14651858.CD000567.pub7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gerhartl A, Hahn K, Neuhoff A, Friedl HP, Förster CY, Wunder C, et al. Hydroxyethylstarch (130/0.4) tightens the blood-brain barrier in vitro. Brain Res. 2020;1727:146560. doi: 10.1016/j.brainres.2019.146560. [DOI] [PubMed] [Google Scholar]
- 32.Schick MA, Burek M, Förster CY, Nagai M, Wunder C, Neuhaus W. Hydroxyethylstarch revisited for acute brain injury treatment. Neural Regen Res. 2021;16:1372–6. doi: 10.4103/1673-5374.300978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chi OZ, Lu X, Wei HM, Williams JA, Weiss HR. Hydroxyethyl starch solution attenuates blood-brain barrier disruption caused by intracarotid injection of hyperosmolar mannitol in rats. Anesth Analg. 1996;83:336–41. doi: 10.1097/00000539-199608000-00023. [DOI] [PubMed] [Google Scholar]
- 34.Woessner R, Grauer MT, Dieterich HJ, Bepperling F, Baus D, Kahles T, et al. Influence of a long-term, high-dose volume therapy with 6% hydroxyethyl starch 130/0.4 or crystalloid solution on hemodynamics, rheology and hemostasis in patients with acute ischemic stroke. Results of a randomized, placebo-controlled, double-blind study. Pathophysiol Haemost Thromb. 2003;33:121–6. doi: 10.1159/000077819. [DOI] [PubMed] [Google Scholar]
- 35.Rudolf J; HES in Acute Stroke Study Group. Hydroxyethyl starch for hypervolemic hemodilution in patients with acute ischemic stroke: a randomized, placebo-controlled phase II safety study. Cerebrovasc Dis. 2002;14:33–41. doi: 10.1159/000063721. [DOI] [PubMed] [Google Scholar]
- 36.Mutoh T, Kazumata K, Ishikawa T, Terasaka S. Performance of bedside transpulmonary thermodilution monitoring for goal-directed hemodynamic management after subarachnoid hemorrhage. Stroke. 2009;40:2368–74. doi: 10.1161/STROKEAHA.109.547463. [DOI] [PubMed] [Google Scholar]
- 37.Bercker S, Winkelmann T, Busch T, Laudi S, Lindner D, Meixensberger J. Hydroxyethyl starch for volume expansion after subarachnoid haemorrhage and renal function: results of a retrospective analysis. PLoS One. 2018;13:e0192832. doi: 10.1371/journal.pone.0192832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kunze E, Stetter C, Willner N, Koehler S, Kilgenstein C, Ernestus RI, et al. Effects of fluid treatment with hydroxyethyl starch on renal function in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2016;28:187–94. doi: 10.1097/ANA.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 39.Huh PW, Belayev L, Zhao W, Busto R, Saul I, Ginsberg MD. The effect of high-dose albumin therapy on local cerebral perfusion after transient focal cerebral ischemia in rats. Brain Res. 1998;804:105–13. doi: 10.1016/s0006-8993(98)00674-x. [DOI] [PubMed] [Google Scholar]
- 40.Belayev L, Saul I, Huh PW, Finotti N, Zhao W, Busto R, et al. Neuroprotective effect of high-dose albumin therapy against global ischemic brain injury in rats. Brain Res. 1999;845:107–11. doi: 10.1016/s0006-8993(99)01952-6. [DOI] [PubMed] [Google Scholar]
- 41.Belayev L, Liu Y, Zhao W, Busto R, Ginsberg MD. Human albumin therapy of acute ischemic stroke: marked neuroprotective efficacy at moderate doses and with a broad therapeutic window. Stroke. 2001;32:553–60. doi: 10.1161/01.str.32.2.553. [DOI] [PubMed] [Google Scholar]
- 42.Suarez JI, Shannon L, Zaidat OO, Suri MF, Singh G, Lynch G, et al. Effect of human albumin administration on clinical outcome and hospital cost in patients with subarachnoid hemorrhage. J Neurosurg. 2004;100:585–90. doi: 10.3171/jns.2004.100.4.0585. [DOI] [PubMed] [Google Scholar]
- 43.Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, SAFE Study Investigators A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247–56. doi: 10.1056/NEJMoa040232. [DOI] [PubMed] [Google Scholar]
- 44.SAFE Study Investigators. Australian and New Zealand Intensive Care Society Clinical Trials Group. Australian Red Cross Blood Service. George Institute for International Health. Myburgh J, Cooper DJ, Finfer S, Bellomo R, Norton R, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84. doi: 10.1056/NEJMoa067514. [DOI] [PubMed] [Google Scholar]
- 45.Huijben JA, Volovici V, Cnossen MC, Haitsma IK, Stocchetti N, Maas AIR, et al. CENTER-TBI investigators and participants. Variation in general supportive and preventive intensive care management of traumatic brain injury: a survey in 66 neurotrauma centers participating in the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) study. Crit Care. 2018;22:90. doi: 10.1186/s13054-018-2000-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Van Aken HK, Kampmeier TG, Ertmer C, Westphal M. Fluid resuscitation in patients with traumatic brain injury: what is a SAFE approach? Curr Opin Anaesthesiol. 2012;25:563–5. doi: 10.1097/ACO.0b013e3283572274. [DOI] [PubMed] [Google Scholar]
- 47.Wang L, Li M, Xie Y, Xu L, Ye R, Liu X. Preclinical efficacy of human albumin in subarachnoid hemorrhage. Neuroscience. 2017;344:255–64. doi: 10.1016/j.neuroscience.2016.12.033. [DOI] [PubMed] [Google Scholar]
- 48.Belayev L, Pinard E, Nallet H, Seylaz J, Liu Y, Riyamongkol P, et al. Albumin therapy of transient focal cerebral ischemia: in vivo analysis of dynamic microvascular responses. Stroke. 2002;33:1077–84. doi: 10.1161/hs0402.105555. [DOI] [PubMed] [Google Scholar]
- 49.Suarez JI, Martin RH, Calvillo E, Dillon C, Bershad EM, Macdonald RL, et al. ALISAH Investigators. The Albumin in Subarachnoid Hemorrhage (ALISAH) multicenter pilot clinical trial: safety and neurologic outcomes. Stroke. 2012;43:683–90. doi: 10.1161/STROKEAHA.111.633958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Suarez JI, Martin RH, Calvillo E, Bershad EM, Venkatasubba Rao CP. Effect of human albumin on TCD vasospasm, DCI, and cerebral infarction in subarachnoid hemorrhage: the ALISAH study. Acta Neurochir Suppl. 2015;120:287–90. doi: 10.1007/978-3-319-04981-6_48. [DOI] [PubMed] [Google Scholar]
- 51.Palesch YY, Hill MD, Ryckborst KJ, Tamariz D, Ginsberg MD. The ALIAS pilot trial: a dose-escalation and safety study of albumin therapy for acute ischemic stroke--II: neurologic outcome and efficacy analysis. Stroke. 2006;37:2107–14. doi: 10.1161/01.STR.0000231389.34701.b5. [DOI] [PubMed] [Google Scholar]
- 52.Ginsberg MD, Palesch YY, Martin RH, Hill MD, Moy CS, Waldman BD, et al. ALIAS Investigators. The albumin in acute stroke (ALIAS) multicenter clinical trial: safety analysis of part 1 and rationale and design of part 2. Stroke. 2011;42:119–27. doi: 10.1161/STROKEAHA.110.596072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ginsberg MD, Palesch YY, Hill MD, Martin RH, Moy CS, Barsan WG, et al. ALIAS and Neurological Emergencies Treatment Trials (NETT) Investigators. High-dose albumin treatment for acute ischaemic stroke (ALIAS) Part 2: a randomised, double-blind, phase 3, placebo-controlled trial. Lancet Neurol. 2013;12:1049–58. doi: 10.1016/S1474-4422(13)70223-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martin RH, Yeatts SD, Hill MD, Moy CS, Ginsberg MD, Palesch YY; ALIAS Parts 1 and 2 and NETT Investigators. ALIAS (albumin in acute ischemic stroke) trials: analysis of the combined data from parts 1 and 2. Stroke. 2016;47:2355–9. doi: 10.1161/STROKEAHA.116.012825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oddo M, Poole D, Helbok R, Meyfroidt G, Stocchetti N, Bouzat P, et al. Fluid therapy in neurointensive care patients: ESICM consensus and clinical practice recommendations. Intensive Care Med. 2018;44:449–63. doi: 10.1007/s00134-018-5086-z. [DOI] [PubMed] [Google Scholar]
- 56.Shin CH, Long DR, McLean D, Grabitz SD, Ladha K, Timm FP, et al. Effects of intraoperative fluid management on postoperative outcomes: a hospital registry study. Ann Surg. 2018;267:1084–92. doi: 10.1097/SLA.0000000000002220. [DOI] [PubMed] [Google Scholar]
- 57.Thacker JK, Mountford WK, Ernst FR, Krukas MR, Mythen MM. Perioperative fluid utilization variability and association with outcomes: considerations for enhanced recovery efforts in sample US surgical populations. Ann Surg. 2016;263:502–10. doi: 10.1097/SLA.0000000000001402. [DOI] [PubMed] [Google Scholar]
- 58.Bundgaard-Nielsen M, Secher NH, Kehlet H. 'Liberal' vs. 'restrictive' perioperative fluid therapy--a critical assessment of the evidence. Acta Anaesthesiol Scand. 2009;53:843–51. doi: 10.1111/j.1399-6576.2009.02029.x. [DOI] [PubMed] [Google Scholar]
- 59.Benes J, Giglio M, Brienza N, Michard F. The effects of goal-directed fluid therapy based on dynamic parameters on post-surgical outcome: a meta-analysis of randomized controlled trials. Crit Care. 2014;18:584. doi: 10.1186/s13054-014-0584-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Corcoran T, Rhodes JE, Clarke S, Myles PS, Ho KM. Perioperative fluid management strategies in major surgery: a stratified meta-analysis. Anesth Analg. 2012;114:640–51. doi: 10.1213/ANE.0b013e318240d6eb. [DOI] [PubMed] [Google Scholar]
- 61.Michard F, Mountford WK, Krukas MR, Ernst FR, Fogel SL. Potential return on investment for implementation of perioperative goal-directed fluid therapy in major surgery: a nationwide database study. Perioper Med (Lond) 2015;4:11. doi: 10.1186/s13741-015-0021-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Colantonio L, Claroni C, Fabrizi L, Marcelli ME, Sofra M, Giannarelli D, et al. A randomized trial of goal directed vs. standard fluid therapy in cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. J Gastrointest Surg. 2015;19:722–9. doi: 10.1007/s11605-015-2743-1. [DOI] [PubMed] [Google Scholar]
- 63.Kissoon NR, Mandrekar JN, Fugate JE, Lanzino G, Wijdicks EF, Rabinstein AA. Positive fluid balance is associated with poor outcomes in subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2015;24:2245–51. doi: 10.1016/j.jstrokecerebrovasdis.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 64.Martini RP, Deem S, Brown M, Souter MJ, Yanez ND, Daniel S, et al. The association between fluid balance and outcomes after subarachnoid hemorrhage. Neurocrit Care. 2012;17:191–8. doi: 10.1007/s12028-011-9573-0. [DOI] [PubMed] [Google Scholar]
- 65.Li J, Ji FH, Yang JP. Evaluation of stroke volume variation obtained by the FloTrac™/Vigileo™ system to guide preoperative fluid therapy in patients undergoing brain surgery. J Int Med Res. 2012;40:1175–81. doi: 10.1177/147323001204000338. [DOI] [PubMed] [Google Scholar]
- 66.Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, et al. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg. 2001;92:984–9. doi: 10.1097/00000539-200104000-00034. [DOI] [PubMed] [Google Scholar]
- 67.Wu CY, Lin YS, Tseng HM, Cheng HL, Lee TS, Lin PL, et al. Comparison of two stroke volume variation-based goal-directed fluid therapies for supratentorial brain tumour resection: a randomized controlled trial. Br J Anaesth. 2017;119:934–42. doi: 10.1093/bja/aex189. [DOI] [PubMed] [Google Scholar]
- 68.Luo J, Xue J, Liu J, Liu B, Liu L, Chen G. Goal-directed fluid restriction during brain surgery: a prospective randomized controlled trial. Ann Intensive Care. 2017;7:16. doi: 10.1186/s13613-017-0239-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sundaram SC, Salins SR, Kumar AN, Korula G. Intra-operative fluid management in adult neurosurgical patients undergoing intracranial tumour surgery: randomised control trial comparing pulse pressure variance (PPV) and central venous pressure (CVP) J Clin Diagn Res. 2016;10:UC01–5. doi: 10.7860/JCDR/2016/18377.7850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hasanin A, Zanata T, Osman S, Abdelwahab Y, Samer R, Mahmoud M, et al. Pulse pressure variation-guided fluid therapy during supratentorial brain tumour excision: a randomized controlled trial. Open Access Maced J Med Sci. 2019;7:2474–9. doi: 10.3889/oamjms.2019.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bapteste L, Carrillon R, Javelier S, Guyotat J, Desgranges FP, Lehot JJ, et al. Pulse pressure variations and plethysmographic variability index measured at ear are able to predict fluid responsiveness in the sitting position for neurosurgery. J Neurosurg Anesthesiol. 2020;32:263–7. doi: 10.1097/ANA.0000000000000587. [DOI] [PubMed] [Google Scholar]
- 72.Byon HJ, Lim CW, Lee JH, Park YH, Kim HS, Kim CS, et al. Prediction of fluid responsiveness in mechanically ventilated children undergoing neurosurgery. Br J Anaesth. 2013;110:586–91. doi: 10.1093/bja/aes467. [DOI] [PubMed] [Google Scholar]