Abstract
Background
Coronavirus disease (COVID-19)-associated coagulopathy is most often characterized by elevated D-dimer, interleukin-6, and plasma fibrinogen concentrations as well as hypercoagulability in thromboelastometry with increased clot firmness in the EXTEM, INTEM, and FIBTEM assays. Clinically, it manifests with a very high incidence of thrombosis, particularly in the pulmonary system, whereas bleeding complications are infrequent.
Case
Here, we describe two critically ill patients with COVID-19 admitted to our intensive care unit demonstrating different thromboelastometry and biomarker patterns. One patient presented with hypercoagulability and the other patient with hypocoagulability and fibrinolysis shutdown in thromboelastometry. The pathophysiology and the potential impact on treatment options are discussed.
Conclusions
A combination of biomarkers and thromboelastometry results can be helpful in the future to decide which therapeutic strategy might be most appropriate for critically ill patients with COVID-19. This would be an important step to establish precision medicine in this high-risk patient population.
Keywords: Anticoagulants, COVID-19, Fibrinolysis, Hemostasis, Thrombelastography, Thrombosis
Coronavirus disease (COVID-19)-associated coagulopathy is most often characterized by elevated D-dimer, interleukin-6 (IL-6), and plasma fibrinogen concentrations as well as hypercoagulability in thromboelastometry with increased clot firmness in the EXTEM, INTEM, and FIBTEM assays [1]. Clinically, it manifests with a very high incidence of thrombosis, particularly in the pulmonary system, whereas bleeding complications are infrequent [2]. In contrast, sepsis-associated coagulopathy due to bacterial infection is characterized by hypocoagulability in thromboelastometry which has been shown to be a good predictor of increased mortality [3]. Here, we describe two critically ill patients with COVID-19 admitted to our intensive care unit (ICU) at Brighton and Sussex University Hospitals NHS Trust presenting with different thromboelastometry phenotypes, clinical courses, and outcomes.
Case Reports
The NHS Institutional Review Board waived the requirement of informed consent from each patient.
Case 1
A 48-year-old South Asian woman (Patient A) from Bangladesh (height 168 cm, weight 80 kg) was admitted to the medical ward for three days after which she was transferred to the ICU; she had cough and increasing dyspnea for three days before hospital admission. Comorbidities included hypertension, hypercholesterinemia, coronary artery disease, previous stroke (fully recovered), and type 2 diabetes. On admission, her laboratory results were as follows: hemoglobin (Hb): 143 g/L, white blood cells (WBC): 9.0 × 109/L, lymphocytes: 1.4 × 109/L, platelets: 261 × 109/L, international normalized ratio (INR): 1.1, D-dimer: 510 μg/L, fibrinogen plasma concentration: 8.4 g/L, and C-reactive protein (CRP): 52 mg/L. Her chest radiograph showed cardiomegaly and extensive bilateral peripherally predominant ground-glass opacities. Polymerase chain reaction (PCR) result was positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and negative for influence/respiratory syncytial virus (RSV). Blood cultures were negative. The patient was treated with nasal oxygen therapy and antibiotics (ceftriaxone and doxycycline, according the hospital’s COVID-19 protocol). Antiviral therapy and dexamethasone were not administered. Later, CRP increased to 137 mg/L on the second day of hospitalization. The patient was transferred to the ICU on the third day because of increased respiratory rate and oxygen requirement. ROTEM performed 2 hours after ICU admission (Fig. 1A) revealed that Patient A was hypercoagulable with the EXTEM assay showing an increased clot firmness with an amplitude of clot firmness 5 minutes after coagulation time (CT) (A5) of 65 mm and a maximum clot firmness (MCF) of 78 mm, indicating hypercoagulability with a high risk of thrombosis [4]. FIBTEM also showed increased clot firmness (A5 41 mm and MCF 50 mm), indicating increased fibrinogen concentration and fibrin polymerization. Furthermore, the EXTEM lysis index 60 minutes after CT (LI60) was 97%, i.e., in the physiologic range (82–97.9%), whereas FIBTEM LI60 was 100% [5]. Treatment consisted of continuation of antibiotics, enoxaparin 40 mg twice a day in view of ROTEM results, and high flow nasal oxygen and intermittent face mask continuous positive airway pressure (CPAP) therapies. The patient did not need intermittent positive pressure ventilation (IPPV) or any vasoactive support. Laboratory results on the second day in the ICU were as follows: Hb: 131 g/L, WBC: 10.8 × 109/L, platelet count: 307 × 109/L, INR: 1.1, activated partial thromboplastin time (APTT) ratio: 1.3, D-dimer: 510 μg/L, and CRP: 196 mg/L. The patient recovered well and was transferred from the ICU to the medical ward after two days in the ICU with a CRP of 73 mg/L and was discharged three days later with a prescription of her usual medication plus enoxaparin 40 mg once daily for 2 weeks. The patient did not show any clinical signs of thrombosis during her hospital stay.
Fig. 1.
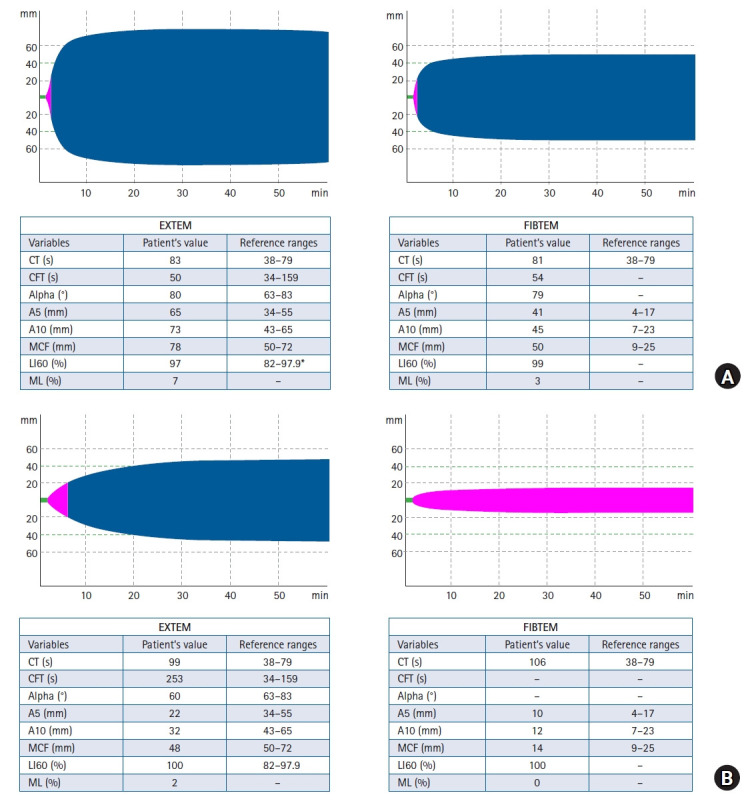
ROTEM graphs and results of Patient A and Patient B. (A) Critically ill Patient A with COVID-19, with a hypercoagulable phenotype. (B) Critically ill Patient B with COVID-19 with a hypocoagulable phenotype. EXTEM: extrinsically activated (tissue factor) thromboelastometric assay, FIBTEM: extrinsically activated thromboelastometric assay with the addition of cytochalasin to eliminate platelet contribution to clot firmness, CT: coagulation time, CFT: clot formation time, alpha: alpha angle, A5: amplitude of clot firmness 5 minutes after CT, A10: amplitude of clot firmness 10 minutes after CT, MCF: maximum clot firmness, LI60: lysis index in percentage of maximum clot firmness 60 minutes after CT, ML: maximum lysis during run time, *Reference range for physiological fibrinolysis in EXTEM as published by Stettler et al. [5].
Case 2
A 68-year-old Caucasian man (Patient B) from the United Kingdom (height 177 cm, weight 85 kg) was admitted with cough and a week-long increasing dyspnea, before which he was healthy. His wife and daughter probably had COVID-19 with resolving symptoms, and they were all living in the same house. The patient markedly experienced shortness of breath on the day of admission to the emergency department (ED) and, therefore, called an ambulance. His laboratory results on admission were as follows: Hb: 140 g/L, creatinine: 117 μmol/L, WBC: 8.6 × 109/L, lymphocytes: 0.2 × 109/L, platelet count: 126 × 109/L, INR: 1.4, APTT ratio: 1.3, D-dimer > 20,000 μg/L (i.e., higher than the upper limit of the measurement range), fibrinogen plasma concentration: 6.8 g/L, and CRP: 336 mg/L. His chest radiograph showed dense bilateral mid-zone and right lower zone consolidation. PCR result was positive for SARS-CoV-2 and negative for influenza/RSV. Blood cultures showed coagulase-negative staphylococci. The patient was treated with antibiotics (ceftriaxone and doxycycline, according the hospital’s COVID-19 protocol). Antiviral therapy and dexamethasone were not administered. As the patient was severely hypoxemic in the ED, he was transferred directly to the ICU. Orotracheal intubation and IPPV (positive end-expiratory pressure 15 mmHg) were performed about 3 hours after ICU admission as respiratory effort was not improved by face mask CPAP therapy. Chest radiography repeated after intubation showed bilateral interstitial lung changes similar to the imaging conducted earlier on the same day. Prone position did not improve oxygenation. Laboratory results on the next day were as follows: Hb: 133 g/L, creatinine: 265 μmol/L, WBC: 16.3 × 109/L, platelet count: 56 × 109/L, INR: 1.6, APTT ratio: 1.5, D-dimer: 4,340 μg/L, fibrinogen plasma concentration: 2.9 g/L, and CRP: 478 mg/L. By ROTEM, Patient B presented with hypocoagulability in the EXTEM assay with a prolonged CT of 99 s, clot formation time (CFT) of 253 s, and decreased clot firmness amplitudes (A5, 22 mm and MCF, 48 mm) (Fig. 1B). Furthermore, EXTEM and FIBTEM analyses demonstrated a complete fibrinolysis shutdown [5]. Both hypocoagulability and fibrinolysis shutdown have been shown to be associated with increased mortality in bacterial sepsis [3,6]. The FIBTEM trace was within normal limits which may be owing to impaired fibrin polymerization, given that fibrinogen concentration was elevated. The patient deteriorated within a few hours of ICU admission and died the following day despite invasive ventilation, norepinephrine for hypotension, and renal replacement therapy for acute kidney failure. Patient B did not show any clinical signs of thrombosis during his hospital stay.
Discussion
We have presented two cases that illustrate the additional value of using thromboelastometry to monitor patients with COVID-19. Increased clot firmness in EXTEM and INTEM (amplitude of clot firmness 10 minutes after CT (A10) > 61.5 mm or MCF > 68 mm) assays has been shown to be associated with an increased incidence of thrombosis in adults and neonates undergoing cardiac and non-cardiac surgery [4]. Furthermore, increased clot firmness in the FIBTEM assay (MCF > 25 mm) has been shown to be associated with an increased incidence of thrombosis in patients with cirrhosis and hepatocellular carcinoma as well as in patients with thrombophilic predisposition after liver transplantation [7,8]. Thromboelastometry in Patient A showed hypercoagulability despite upper normal ranged D-dimer levels and a normal INR. Patients with D-dimer > 3,000 µg/L and/or sepsis-induced coagulopathy score ≥ 4 seem to benefit from increased anticoagulation [9]. However, in critically ill patients with COVID-19, the incidence of thrombosis and pulmonary embolism is high despite pharmacological thromboprophylaxis [2].
The case of Patient B demonstrated that not all critically ill patients with COVID-19 present the same thromboelastometric pattern. This might be attributed to ethnic and genetic difference, such as gene polymorphisms, bacterial superinfection, or the phase of the disease. Both hypocoagulability and fibrinolysis shutdown, as presented by Patient B, have been shown to be associated with increased mortality in cases involving bacterial sepsis [3,6]. Furthermore, lymphocytopenia has been shown to be associated with poor outcomes in COVID-19 [10]. Although thrombocytopenia, which is an important determinant of clot firmness, is rare in COVID-19, it is associated with poor outcomes in the patient population [7,11]. Furthermore, the mismatch between FIBTEM MCF (14 mm) and Clauss fibrinogen plasma concentration (6.8 g/L) in Patient B might reflect an acquired factor XIII deficiency, which often occurs in sepsis, cirrhosis, acute renal failure, and malignancies [12]. Unfortunately, factor XIII activity is not available for Patient B, which leaves this interpretation speculative. The rapid deterioration of Patient B with acute renal failure and a fatal outcome is in-line with the data published by Wright et al. [13] showing that patients with the combination of high D-dimer (> 2,600 µg/L, here > 20,000 µg/L) and fibrinolysis shutdown (lysis 30 minutes after maximum amplitude in thrombelastography (TEG LY30) of 0% or ROTEM LI60 of 100%) are associated with the highest incidence of thrombosis (50%) and acute renal failure (80%). Here, increased D-dimers and fibrinolysis shutdown may reflect an imbalance in hemostasis with increased clot formation but impaired fibrinolysis – similar to disseminated intravascular coagulation. It remains to be determined whether fibrinolytic therapy with recombinant tissue plasminogen activator (rtPA) has a therapeutic role in critically ill patients with COVID-19 who cannot be oxygenated adequately despite mechanical ventilation and prone positioning. Notably, extracorporeal membrane oxygenation is associated with very high mortality in patients with COVID-19, particularly in patients with hyperinflammation characterized by high IL-6 levels. Although this might support the use of fibrinolytic therapy with rtPA in these patients, Campello et al. [14] demonstrated that a FIBTEM MCF < 14.5 mm is highly predictive of bleeding complications (such as hemorrhagic stroke) after rtPA. Therefore, hypocoagulability in thromboelastometry, particularly a FIBTEM MCF < 14.5 mm should be considered a contraindication for fibrinolytic therapy in critically ill patients with COVID-19.
Nevertheless, this case report has several limitations. First, no follow-up ROTEM analyses are available for these patients. Accordingly, the presented ROTEM analyses only represent a snapshot of the COVID-19-associated coagulopathy that can be considered as a dynamic process. Here, different thromboelastometric phenotypes may represent different conditions of the patients or different phases of the coagulopathy. Second, the cut-off values for fibrinolysis shutdown established in trauma and bacterial sepsis cases have been used as clear cut-off values for fibrinolysis shutdown in COVID-19-associated coagulopathy have not been established yet. Further studies are needed to characterize COVID-19-associated coagulopathy and its differences from trauma- and sepsis-induced coagulopathy.
These two cases demonstrate that the thromboelastometric phenotype can be different and thromboelastometry can easily distinguish between hyper- and hypocoagulability in critically ill patients with COVID-19. Furthermore, thromboelastometry can identify patients with fibrinolysis shutdown [5,6]. The combination of thromboelastometry parameters (EXTEM and FIBTEM CT, CFT, A5, A10, MCF and LI60) and conventional biomarkers (D-dimer, Clauss fibrinogen, and IL-6) might be superior in predicting clinical outcomes such as thrombosis, renal failure and death in patients with COVID-19 than each diagnostic test alone. Therefore, these test combinations can be helpful in the future to decide which therapeutic strategy might be the most appropriate one in critically ill patients with COVID-19. This would be an important step to establish precision medicine not only in thromboelastometry-guided bleeding management but also in this high-risk patient population [15].
Footnotes
Conflicts of Interest
Klaus Görlinger is working as the Medical Director of Tem Innovations since July 2012. Robert Kong and Nevil Hutchinson reported no potential conflict of interest relevant to this article.
Author Contributions
Robert Kong (Conceptualization; Investigation; Writing – review & editing)
Nevil Hutchiinson (Conceptualization; Investigation; Writing – review & editing)
Klaus Görlinger (Conceptualization; Writing – original draft)
References
- 1.Spiezia L, Boscolo A, Poletto F, Cerruti L, Tiberio I, Campello E, et al. COVID-19-related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020;120:998–1000. doi: 10.1055/s-0040-1710018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dolhnikoff M, Duarte-Neto AN, de Almeida Monteiro RA, da Silva LFF, de Oliveira EP, Saldiva PH, et al. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020;18:1517–9. doi: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adamzik M, Langemeier T, Frey UH, Görlinger K, Saner F, Eggebrecht H, et al. Comparison of thrombelastometry with simplified acute physiology score II and sequential organ failure assessment scores for the prediction of 30-day survival: a cohort study. Shock. 2011;35:339–42. doi: 10.1097/SHK.0b013e318204bff6. [DOI] [PubMed] [Google Scholar]
- 4.Hincker A, Feit J, Sladen RN, Wagener G. Rotational thromboelastometry predicts thromboembolic complications after major non-cardiac surgery. Crit Care. 2014;18:549. doi: 10.1186/s13054-014-0549-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stettler GR, Moore EE, Moore HB, Nunns GR, Silliman CC, Banerjee A, et al. Redefining postinjury fibrinolysis phenotypes using two viscoelastic assays. J Trauma Acute Care Surg. 2019;86:679–85. doi: 10.1097/TA.0000000000002165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adamzik M, Eggmann M, Frey UH, Görlinger K, Bröcker-Preuss M, Marggraf G, et al. Comparison of thromboelastometry with procalcitonin, interleukin 6, and C-reactive protein as diagnostic tests for severe sepsis in critically ill adults. Crit Care. 2010;14:R178. doi: 10.1186/cc9284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zanetto A, Senzolo M, Vitale A, Cillo U, Radu C, Sartorello F, et al. Thromboelastometry hypercoagulable profiles and portal vein thrombosis in cirrhotic patients with hepatocellular carcinoma. Dig Liver Dis. 2017;49:440–5. doi: 10.1016/j.dld.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 8.Kamel Y, Hassanin A, Ahmed AR, Gad E, Afifi M, Khalil M, et al. Perioperative thromboelastometry for adult living donor liver transplant recipients with a tendency to hypercoagulability: a prospective observational cohort study. Transfus Med Hemother. 2018;45:404–12. doi: 10.1159/000489605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–9. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bedreli S, Sowa JP, Malek S, Blomeyer S, Katsounas A, Gerken G, et al. Rotational thromboelastometry can detect factor XIII deficiency and bleeding diathesis in patients with cirrhosis. Liver Int. 2017;37:562–8. doi: 10.1111/liv.13254. [DOI] [PubMed] [Google Scholar]
- 13.Wright FL, Vogler TO, Moore EE, Moore HB, Wohlauer MV, Urban S, et al. Fibrinolysis shutdown correlation with thromboembolic events in severe COVID-19 infection. J Am Coll Surg. 2020;231:193–203.e1. doi: 10.1016/j.jamcollsurg.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campello E, Farina F, Spiezia L, Maggiolo S, Palmieri A, Sartorello F, et al. Thromboelastometry profiles in patients undergoing thrombolytic therapy for acute ischaemic stroke. Thromb Haemost. 2016;115:1231–4. doi: 10.1160/TH15-10-0798. [DOI] [PubMed] [Google Scholar]
- 15.Görlinger K, Pérez-Ferrer A, Dirkmann D, Saner F, Maegele M, Calatayud ÁA, et al. The role of evidence-based algorithms for rotational thromboelastometry-guided bleeding management. Korean J Anesthesiol. 2019;72:297–322. doi: 10.4097/kja.19169. [DOI] [PMC free article] [PubMed] [Google Scholar]


