Abstract
Background
New Zealand's Immunisation Programme is an important pillar in the war against COVID-19, making high vaccine uptake essential. This study sought to: (1) identify potential vaccine uptake rates among New Zealanders prior to programme rollout; (2) understand reasons for unlikelihood/likelihood of vaccine uptake; and, (3) explore sociodemographic differences in risk of and reasons for vaccine hesitancy.
Methods
Data were collected in March 2021 (n = 1,284) via a web-based survey. Respondents were a diverse sample of New Zealanders who were part of a large, pre-existing social research sampling frame. Multinomial and logit regressions were estimated to examine sociodemographic predictors of vaccine hesitancy and reasons for likelihood/hesitancy.
Findings
Overall, 70% reported they would likely take the vaccine once available (i.e., very likely or somewhat likely). Being younger and less educated were correlated with greater vaccine hesitancy risk (i.e., very unlikely, somewhat likely, or unsure). Women were more likely than men to say they were unsure (Relative Risk Ratio = 1.60) vs. either likely or unlikely and to identify concerns regarding personal health, such as potential side effects, as a reason. Men identified concerns surrounding trust in vaccines and the perceived exaggerated risk of COVID-19 to them and the population.
Interpretation
Although a majority intend to take the COVID-19 vaccine once available, a sizeable minority who were more likely to be young, female, and less educated, were unsure about or unlikely to get the vaccine, primarily due to perceptions of unknown future side effects. Ethnicity was not statistically associated with vaccine hesitancy, suggesting that public health efforts aimed at increasing vaccine acceptance among Māori and Pacific peoples—subgroups most at-risk of COVID-19 infection and morbidity—should focus on inequities in health care access to increase uptake.
Keywords: COVID-19, Vaccination, Vaccine, Vaccine hesitancy, Pandemic, New Zealand
RESEARCH IN CONTEXT.
Evidence before this study
While an extant amount of survey data and literature exists to monitor the COVID-19 vaccine rollout and vaccine hesitancy in developed countries that are most impacted by the COVID-19 pandemic, there appears scant evidence on potential vaccine uptake in New Zealand—a country that had yet to make vaccines available to the general population and where there was minimal community transmission of the virus.
We searched in PubMed and Google Scholar for studies using data collected in New Zealand, including terms such as “COVID-19 vaccine”, “New Zealand vaccine hesitancy” and “COVID-19 New Zealand.” In addition, we went directly to New Zealand's Ministry of Health website—the government institution responsible for New Zealand's COVID-19 Immunisation Programme—for information on surveying conducted by or on behalf of the Ministry. Given the limited number of empirical studies on potential COVID-19 vaccine uptake in New Zealand, we considered all publications, regardless of peer-review status. Prior studies on COVID-19 vaccine uptake in New Zealand included in our review of the existing literature relied on social science research marketing panels that, while diverse, may not necessarily be representative of the New Zealand population. Despite different time periods for data collection and analytical samples being derived from different panels, there was consistency across these studies in terms of estimated vaccine uptake, ranging from 69-74%.
Added value of this study
To our knowledge, this is the first study that assesses COVID-19 vaccine hesitancy in New Zealand in a multivariate framework, simultaneously assessing a range of sociodemographic predictors to understand the relative importance of these different factors, such as gender, ethnicity, and age. In line with bivariate results from prior studies, we found that young people and those with less education were less likely to say they would take the vaccine. In contrast to prior studies, however, in a multivariate framework identifying as Māori or Pacific was no longer statistically associated with vaccine hesitancy, with population characteristics of these ethnic subgroups (primarily, being younger and less educated) accounting for the bivariate associations. We also found that women were more likely than men to be unsure they would take the vaccine, whereas men were more definitive in terms of both being more unlikely or likely to take the vaccine than being unsure—a finding masked by different vaccine hesitancy measurement in prior studies.
Implications of all the available evidence
The available evidence on COVID-19 vaccine hesitancy in New Zealand's adult population is clear that a majority of New Zealanders are likely to take the COVID-19 vaccine once it becomes available to them. There is consistently, however, approximately 30% of the population who are still unsure or unlikely to take the vaccine. These people tend to be younger and less educated, suggesting a target group for public health promotions aimed at increasing confidence in the vaccine. Importantly, our findings suggest that public health focus on perceived hesitancy in the Māori and Pacific populations—subgroups that are particularly at-risk of COVID-19 infection and morbidity—may be misplaced. Instead, public health efforts should focus on combating the known inequities in health care access that may increase the risk that vaccine intention among these groups does not translate into uptake.
Alt-text: Unlabelled box
One of the key public health tools in the fight against COVID-19 is an effective vaccination programme. Effectiveness means achieving high uptake among the general adult population, ideally sufficient to generate local herd-immunity. [1] Effectiveness also means equitable access, acceptability and delivery so as to avoid disparities in care and disease outcomes.[2] New Zealand's COVID-19 elimination strategy has been one of the most effective responses to the pandemic in the world, [3] resulting in a low number of community-transmitted infections and 26 deaths since the beginning of the pandemic. [4] Given this strategy, however, widespread COVID-19 vaccine acceptance is an essential element for relaxing border controls and other strict public health measures that aim to stop community transmission, such as intermittent lockdowns. [5]
New Zealand's COVID-19 Immunisation Programme plans to vaccinate the entire adult population (16 years and over) with the two-dose Pfizer/BioNTech vaccine. The Pfizer/BioNTech vaccine has (currently, and at the time of data collection for this study) a higher rate of efficacy and fewer adverse reactions than other COVID-19 vaccines, although all medically-approved vaccines have been proven safe and effective. [6], [7], [8], [9] A four-stage approach began in February 2021 which rolled out vaccines first to border and Managed Isolation Quarantine (MIQ) facility workers and those in their households, followed by other high-risk frontline workers. Those at high-risk of getting very sick from COVID-19 began receiving vaccinations in June. It is anticipated (at the time this article is written) that vaccination among the general population will roll out in July 2021 in a staggered approach starting with older age groups (60 years and older), working down to the youngest group (those aged 16-34 years) having access to the vaccine in October 2021. [10]
A significant threat to the Immunisation Programme and the health of New Zealanders is low COVID-19 vaccine uptake. As other countries with high rates of COVID-19 transmission and mortality begin their COVID-19 vaccination programmes, rates of vaccine hesitancy have tended to decline over time, such as in the UK and US. [11,12]
In Australia, New Zealand's closest neighbour geographically who has also experienced limited COVID-19 spread and whose public health and policy responses have been similar, the rates of vaccine hesitancy have remained stagnant and potentially increased over time. For example, one survey conducted in April 2020 found 86% of Australians would take the vaccine once offered to them. [13] However later surveys have estimated the proportion of Australians unlikely to take the vaccine increasing to 24% by June 2020, [14] and another survey in April 2021 suggesting one-third of Australians were unlikely to get vaccinated. [15] These studies have also found sociodemographic disparities in vaccine hesitancy, with young people and those with lower educational attainment more likely to be vaccine hesitant. [13,14]
There is limited understanding of COVID-19 vaccine hesitancy in New Zealand. A research factsheet from the Ministry of Health using data collected between March 26 and April 1 2021 noted that likelihood of vaccine uptake has remained consistent with prior estimates, with approximately 69% of the adult population likely to take the COVID-19 vaccine once it becomes available to them. [16] This proportion aligns with more thorough research for the Ministry of Health from data collected in both September and December 2020, and another survey conducted in July 2020 where 74% said they intended to get vaccinated against COVID-19, [17] although there were signs that people were becoming less certain that they would take the vaccine over time and that certainty may be unequal within important population subgroups. [18] Women, younger people, and Māori (Indigenous New Zealanders; 17% of the population [19]) and Pacific peoples (those from or with ancestry from islands in the Pacific region; 8% of the population [19]) reported higher rates of vaccine hesitancy. These patterns are cause for greater concern, especially among Māori and Pacific, who face higher risks from COVID-19 disease, [20] and which are situated within the context of broader pre-existing patterns of inequitable access to health care and in health outcomes generally, [21], [22], [23], [24] and in vaccination coverage, specifically. [25,26]
Reasons for COVID-19 vaccine hesitancy most often included concerns around the vaccine's safety and potential side effects. [11] Given increases in misinformation and conspiracy theories regarding COVID-19 vaccination in recent months [27] and a majority of New Zealanders indicating they get some information about COVID-19 vaccine from social media [18]—an environment particularly adept at spreading COVID-19 misinformation [28,29]—it is important to gauge how these hesitancy rates may have changed leading up to vaccine roll-out, and therefore, how the strategy must adapt to support the COVID-19 elimination strategy and avoid exacerbating health inequities.
Moreover, these recent studies have focused on the negative reasons why people are unlikely to get the vaccine and have not focussed on the positive reasons why one might take the vaccine, which may be just as salient from a public policy perspective. For example, one study using data collected between June-July 2020 found that the most common reasons New Zealanders would be vaccinated were to protect themselves (62%) and their family (62%), to avoid getting seriously ill (52%), and to feel safe around other people (51%). People were less likely to report they would get the vaccine because their doctor recommended it (23%). [30]
To address these gaps, this study has three primary research questions. First, what are the rates of COVID-19 vaccine hesitancy and acceptability among a diverse sample of New Zealanders (n = 1,284) prior to the nationwide COVID-19 Immunisation Programme rollout to the general population (scheduled for July 2021)? Second, what are the sociodemographic predictors of vaccine hesitancy and acceptance? Importantly, we examine this question in a multivariate framework to understand the relative importance of specific sociodemographic predictors, expecting to find that certain characteristics that have been emphasised in prior research as key drivers of vaccine acceptance inequities, such as ethnicity, may be partially explained by other factors overrepresented in these groups (e.g., lower educational attainment, young age population profile). Third, what are the reasons why people are vaccine hesitant and the reasons why others are likely to get the vaccine, and how do these reasons differ by sociodemographic characteristics? Understanding this reasoning can point to sources of health resilience within the COVID-19 elimination strategy, such as motivations for vaccine acceptance among groups with higher rates of vaccine hesitancy, and can ensure that a comprehensive vaccination programme includes opportunities to maximise access to, confidence in, and motivation to vaccinate among the general population and important sub-groups. Moreover, in a globalised world the findings can provide insight into vaccination intention among populations least exposed to detrimental health ramifications during pandemics, but whose willingness to be vaccinated is important for global success in defeating viruses and infectious disease.
1. Methods
1.1. Data and sample
Data come from the Life in Lockdown survey, a longitudinal data collection effort aimed at examining the impact of the nationwide Alert Level 4 lockdown (March-April 2020) on New Zealanders’ economic and social wellbeing. [31] The web-based, self-administered survey was designed by researchers at the Roy McKenzie Centre for the Study of Families and Children and the Institute for Governance and Policy Studies at Victoria University of Wellington. Colmar Brunton—a social research firm—contacted participants via email through their existing social marketing sampling frame of over 100,000 New Zealanders. Using known information on several key sociodemographic characteristics of sampling frame members, typically underrepresented survey takers (e.g., Māori and Pacific ethnicity, young men) were sent a survey invitation first, with other groups contacted in batches on subsequent days.1 Respondents in the first survey wave (i.e., Wave 1) who clicked on the survey link were taken to a set of screening questions, where respondents were then screened by gender, age, income, region, and ethnicity to ensure a socio-demographically-diverse sample, with weights created to infer nationally-representative estimates. The survey concluded once 2,000 responses were collected.2
Data were collected in April 2020 (Wave 1; n = 2,002) when New Zealand was in its strictest lockdown stage (Alert Level 4), in July 2020 when the country was back in its most relaxed stage (Level 1; Wave 2; n = 1,466; 73% of Wave 1 respondents), and one year later between March 16-21, 2021, when New Zealand was also in Alert Level 1 (Wave 3; n =1,310; 65% of Wave 1 respondents). COVID-19 vaccine uptake questions were only asked at Wave 3. The final analytical sample consists of 1,284 respondents aged 18 years and older who participated in Wave 3 of the study (dropping 692 from the initial 2,002 Wave 1 respondents who exited the study by Wave 3) and who answered questions on vaccine hesitancy (dropping 23 who were either missing or preferred not to answer the question). Three respondents who identified as gender diverse were excluded because of multicollinearity issues in the models.3 Those who exited the study were more likely to be younger and identify as an ethnic minority, have slightly lower levels of educational attainment, and moderately more likely to report being male than those who remained.4
More information on the study design can be found in the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) in Table A2 in the appendix. [32]
Variables. The key outcome variables were likelihood of and reasons for COVID-19 vaccine uptake or hesitancy. These questions and response options came from the Opinions and Lifestyle Survey, a weekly survey conducted in Great Britain during the COVID-19 pandemic [33] and the Understanding Society survey, a UK household longitudinal study, [34] and were only asked at Wave 3 (March 2021). To measure vaccine hesitancy, respondents were asked “How likely are you to get vaccinated for the coronavirus (COVID-19) once the vaccine is available to you?”, with response options including Very unlikely, Somewhat unlikely, Unsure, Somewhat likely, and Very likely. Respondents were also able to indicate whether they had already received the vaccine (no one in this sample) or prefer not to say (n = 8; excluded from the analytical sample). For the multinomial regressions predicting vaccine hesitancy, responses were recoded into three groups: 1) unlikely (combining very unlikely and somewhat unlikely); 2) unsure; and, 3) likely (combining very likely and somewhat likely).
Respondents who indicated that they were very unlikely, somewhat unlikely, or unsure if they would take the vaccine were given a list of potential reasons, including the option to specify non-listed reasons, for why they were unlikely to take the vaccine. Respondents who chose more than one reason were subsequently asked to identify the most important reason of those that they selected. Symmetrically, respondents who indicated they were very likely or somewhat likely to take the vaccine were asked a similarly structured series of questions, where they were asked to identify the reasons why they were likely to take the vaccine.5
We explore differences in vaccine hesitancy across a range of sociodemographic characteristics that may influence uptake, including those previously shown to be associated with vaccine hesitancy (e.g., age, gender, ethnicity, education), and also other potential variables that tap into people's social support (e.g., household structure), exposure to others (e.g., work status), and potential virus exposure (e.g., differences in prior community spread across regions). These variables were collected across the study waves. Sociodemographic characteristics collected at Wave 1 included: age (coded into six dummy variables indicating respondent aged 18-24 years; 35-44 years; 45-54 years; 55-64 years; or 65 years and older); gender (1 = female)6; ethnicity (mutually-exclusive dummy variables indicating European/Pākehā; Māori; Pacific; Asian; Other ethnicity (predominately Indian))7; and educational attainment (three dummy variables indicating primary/secondary school education; diploma; or university/postgraduate degree); Nativity (1 = New Zealand born) was captured in Wave 2. Respondents’ annual household income (series of dummy variables ranging from household incomes at NZ$30,000 per annum or less through to over NZ$150,000),8 household structure (two parents with dependent children; single parent; living alone; partnered with no dependent children; some other living arrangement), work status (employed; unemployed; not in the labour force), and public health unit region (12 dummy variables)9 were captured at Wave 3.10
Analyses. We examined vaccine hesitancy and reasons for hesitancy or uptake using both a bivariate and multivariate approach. Multinomial logistic regressions were used to assess competing risks between being unlikely, unsure, or likely to get the vaccine. First, we examined the competing risks of being likely to take the vaccine as the reference group versus unlikely and unsure. Second, we examined the competing risk of being unlikely to take the vaccine as the reference group versus unsure in order to have competing risk comparisons across all three categories. Six logit regressions were used to predict the odds of identifying the six most cited reasons why respondents were unlikely or unsure they would get the vaccine among those who indicated they were unlikely or unsure of getting the vaccine. This process was replicated among the sample who said they were likely to get the vaccine, predicting the six most cited reasons why. All covariates were included in the multivariate models. All data cleaning and analyses were conducted in Stata. Multiple imputation was used for the small amount of item-level missing data on five independent variables (<1.0% of analytical data).11 Listwise deletion would have resulted in 259 respondents dropped from the vaccine hesitancy analyses (20.2% of the analytic sample), 77 respondents dropped from the analyses of reasons for vaccine hesitancy (20.5% of the analytic sample), and 182 respondents dropped from analyses of reasons for vaccine acceptance (20.0% of the analytic sample). The multiple imputation constructed 100 imputed datasets which were analysed through the suite of mi estimate commands. Weights were applied to the bivariate statistics that adjusted to New Zealand adult population proportions for age, gender, income, region, and household structure.
1.2. Role of funding source
There was no funding source for this study.
1.3. Human ethics approval
Human ethics approval (Application ID 0000029123) was granted as a Category B study (low risk) by the Victoria University of Wellington Human Ethics Committee.
2. Results
2.1. COVID-19 vaccine hesitancy and uptake likelihood
Table 1 presents COVID-19 vaccine hesitancy for the total sample and across key sociodemographic characteristics, as well as description of the sample. Overall, 70.7% of the sample indicated they were very likely (56.0%) or somewhat likely (14.8%) to take the vaccine once it became available to them. Of the 14.2% that were unlikely to take the vaccine, 9.6% said they were very unlikely and 4.6% said they were somewhat unlikely. A further 15.1% said they were unsure.
Table 1.
Likelihood of getting the COVID-19 vaccine (n = 1,284)
| Total |
Very unlikely | Somewhat unlikely | Unsure | Somewhat likely | Very likely | ||
|---|---|---|---|---|---|---|---|
| n | Column % | % | % | % | % | % | |
| Total | 1,284 | 100.00 | 9.60 | 4.60 | 15.07 | 14.77 | 55.96 |
| Age (years) | |||||||
| 18-24 | 81 | 8.69 | 10.98 | 8.78 | 18.20 | 15.97 | 46.08 |
| 25-34 | 175 | 18.51 | 11.92 | 5.08 | 16.68 | 13.45 | 52.86 |
| 35-44 | 255 | 13.82 | 10.24 | 2.62 | 20.70 | 19.16 | 47.28 |
| 45-54 | 290 | 19.91 | 8.40 | 5.99 | 13.11 | 21.35 | 51.15 |
| 55-64 | 256 | 20.21 | 7.77 | 4.33 | 17.22 | 13.41 | 57.27 |
| 65+ | 223 | 18.87 | 9.59 | 2.52 | 7.95 | 7.06 | 72.87 |
| Gender | |||||||
| Female | 550 | 51.72 | 8.20 | 4.08 | 17.71 | 14.52 | 55.49 |
| Male | 734 | 48.28 | 11.10 | 5.15 | 12.24 | 15.04 | 56.47 |
| Ethnicity | |||||||
| European/Pākehā | 798 | 65.86 | 8.62 | 4.51 | 15.08 | 12.36 | 59.43 |
| Māori | 165 | 13.32 | 13.59 | 7.86 | 13.71 | 18.70 | 46.14 |
| Pacific | 81 | 5.41 | 7.87 | 5.83 | 15.94 | 19.12 | 51.23 |
| Asian | 134 | 8.92 | 10.31 | 2.04 | 18.25 | 25.52 | 43.88 |
| Other | 106 | 6.50 | 11.75 | 1.34 | 12.77 | 12.80 | 61.35 |
| Nativity | |||||||
| NZ born | 829 | 76.79 | 9.65 | 4.62 | 15.98 | 14.94 | 54.81 |
| Not born in NZ | 293 | 23.21 | 8.67 | 2.63 | 16.46 | 11.89 | 60.36 |
| Educational attainment | |||||||
| Primary/Secondary school | 336 | 27.42 | 12.65 | 2.90 | 18.27 | 14.61 | 51.57 |
| Diploma | 425 | 33.79 | 12.05 | 6.41 | 15.21 | 12.11 | 54.23 |
| Undergraduate/Postgraduate degree | 512 | 38.79 | 5.35 | 4.31 | 12.58 | 17.43 | 60.34 |
| Annual household income (NZ$) | |||||||
| $50,000 or less | 360 | 37.91 | 9.80 | 4.63 | 15.79 | 13.19 | 56.59 |
| $50,001-$70,000 | 186 | 14.52 | 12.74 | 7.99 | 16.67 | 10.95 | 51.65 |
| $70,001-$100,000 | 240 | 18.63 | 7.34 | 4.21 | 15.37 | 17.35 | 55.73 |
| $100,001-$150,000 | 236 | 18.09 | 6.63 | 4.75 | 14.01 | 21.01 | 53.61 |
| More than $150,000 | 167 | 10.86 | 8.21 | 2.94 | 8.05 | 10.62 | 70.18 |
| Family structure | |||||||
| Two parents with dependent children | 401 | 20.44 | 12.61 | 3.24 | 16.96 | 20.06 | 47.13 |
| Single parent | 64 | 4.61 | 19.29 | 9.54 | 19.92 | 11.55 | 39.71 |
| Living alone | 130 | 16.19 | 9.59 | 7.79 | 11.56 | 13.10 | 57.96 |
| Partner, no dependent children | 528 | 45.64 | 7.73 | 4.16 | 14.20 | 12.12 | 61.78 |
| Other | 161 | 13.12 | 8.01 | 2.52 | 17.78 | 18.95 | 52.73 |
| Work status | |||||||
| Employed | 881 | 65.61 | 9.00 | 4.72 | 16.06 | 15.92 | 54.29 |
| Unemployed | 69 | 5.57 | 11.36 | 8.17 | 21.64 | 19.27 | 39.56 |
| Not working | 334 | 28.82 | 10.63 | 3.61 | 11.54 | 11.29 | 62.93 |
| Public Health Unit region | |||||||
| Northland | 49 | 3.93 | 12.97 | 5.71 | 15.48 | 1.66 | 64.18 |
| Auckland | 432 | 33.13 | 8.21 | 3.61 | 14.85 | 17.18 | 56.15 |
| Waikato, Northern Ruapehu | 126 | 9.77 | 7.92 | 8.07 | 20.65 | 12.95 | 50.41 |
| Whakatane, Tauranga, Rotorua, Taupo | 66 | 6.24 | 17.00 | 5.05 | 13.71 | 9.58 | 54.65 |
| Gisborne/Tairawhiti | 18 | 0.87 | 8.39 | 0.00 | 22.86 | 7.07 | 61.69 |
| Hawke's Bay | 43 | 3.33 | 3.08 | 4.70 | 16.98 | 9.32 | 65.92 |
| Taranaki | 33 | 2.33 | 18.35 | 0.00 | 17.66 | 10.41 | 53.57 |
| Manawatu, Whanganui, South Ruapehu | 66 | 4.83 | 8.88 | 0.00 | 20.23 | 23.46 | 47.43 |
| Wellington, Hutt Valley, Wairarapa | 148 | 11.06 | 10.88 | 3.65 | 9.37 | 13.58 | 62.52 |
| Nelson-Marlborough | 40 | 3.52 | 6.58 | 17.92 | 9.19 | 14.45 | 51.85 |
| Canterbury, West Coast | 180 | 13.62 | 4.30 | 3.91 | 16.48 | 17.72 | 57.59 |
| Otago, Southland | 83 | 7.37 | 20.13 | 4.71 | 12.38 | 13.29 | 49.49 |
Unweighted ns, weighted %s. Sum of subgroups may not total to 1,284 due to missing values.
Examining key sociodemographic characteristics, younger people reported lower rates of vaccine acceptance compared to older groups, ranging from 62.1% of 18-24 years saying they were very likely or somewhat likely to take the vaccine through to 79.9% of those aged 65 years and older. Men were more definitive in their likelihood of vaccine uptake. Although women and men reported similar rates of vaccine acceptance (70.0% vs. 71.5%, respectively), 16.3% of men reported they were unlikely to take the vaccine compared with 12.3% of women. A greater share of women (17.7%) compared to men (12.2%) said they were unsure they would get the vaccine.
Respondents who identified as Māori reported lower rates of vaccine acceptance (64.8% vs. 70.7% among the total sample) and higher rates of being unlikely to take the vaccine (21.5% vs. 14.2% among the total sample).There were statistically similar rates of likelihood and unlikelihood of vaccine uptake among the remaining ethnic groups. A greater share of those born overseas reported they would likely take the vaccine (72.3%) compared to those born in New Zealand (69.8%).
Those with undergraduate or postgraduate degrees reported higher rates of vaccine acceptance (77.8% vs. 66.3% and 66.2% among those with only primary/secondary school education or a post-secondary education diploma, respectively). Higher income households also reported higher rates of vaccine acceptance and lower rates of vaccine hesitancy compared with lower income households.
Table 2 tests the robustness of these bivariate associations using multinomial logistic regression models to identify which associations remain statistically significant predictors of vaccine hesitancy, net of other sociodemographic factors. In line with the bivariate findings, age was statistically associated with being unsure versus likely get the vaccine, however there was not a statistically significant difference in the likelihood of being unlikely to get the vaccine versus likely. Those aged 25-34 years old were closed to four and half times (Relative Risk Ratio [RRR] = 4.42, 95% Confidence Intervals [CI] [2.03, 9.61]) more likely at risk of saying they were unsure they would take the vaccine (vs. likely) compared to those 65 years and older. Those aged 35-44 years were three and a half times (RRR = 3.51, [1.62, 7.59]) as likely to be at risk of saying they were unsure if they would take the vaccine (vs. likely) compared to those 65 years or older, whereas those aged 55-64 years were over twice as likely (RRR = 2.36, [1.20, 4.67]) to be at risk of being unsure (vs. likely) compared with those 65 years or older. There was no statistical difference in vaccine hesitancy between the youngest age group (i.e., 18-24 years), those aged 45-54 years, and those aged 65 years and older.
Table 2.
Multinomial regressions predicting COVID-19 vaccine acceptance (n = 1,284)
| Reference: Likely |
Reference: Unlikely |
|||||
|---|---|---|---|---|---|---|
| vs. unlikely |
vs. unsure |
vs. unsure |
||||
| RRR | [95% CI] | RRR | [95% CI] | RRR | [95% CI] | |
| (std. err.) | (std. err.) | (std. err.) | ||||
| Age (ref: 65+ years) | ||||||
| 18-24 years | 2.37 | [0.99 - 5.69] | 1.99 | [0.80 - 4.91] | 0.84 | [0.26 - 2.66] |
| (1.06) | (0.92) | (0.49) | ||||
| 25-34 years | 1.83 | [0.85 - 3.95] | 4.42 | [2.03 - 9.61] | 2.41 | [0.89 - 6.56] |
| (0.72) | (1.75) | (1.23) | ||||
| 35-44 years | 1.16 | [0.54 - 2.49] | 3.51 | [1.62 - 7.59] | 3.02 | [1.11 - 8.22] |
| (0.45) | (1.38) | (1.54) | ||||
| 45-54 years | 1.09 | [0.55 - 2.17] | 1.79 | [0.85 - 3.75] | 1.64 | [0.64 - 4.21] |
| (0.38) | (0.68) | (0.79) | ||||
| 55-64 years | 1.44 | [0.77 - 2.69] | 2.36 | [1.20 - 4.67] | 1.64 | [0.70 - 3.88] |
| (0.46) | (0.82) | (0.72) | ||||
| Gender (ref: male) | ||||||
| Female | 0.74 | [0.51 - 1.08] | 1.60 | [1.14 - 2.24] | 2.15 | [1.36 - 3.39] |
| (0.14) | (0.28) | (0.50) | ||||
| Ethnicity (ref: European/Pākehā) | ||||||
| Māori | 1.53 | [0.95 - 2.46] | 1.10 | [0.66 - 1.81] | 0.72 | [0.39 - 1.33] |
| (0.37) | (0.28) | (0.23) | ||||
| Pacific | 1.02 | [0.48 - 2.20] | 1.23 | [0.65 - 2.33] | 1.20 | [0.49 - 2.95] |
| (0.40) | (0.40) | (0.55) | ||||
| Asian | 1.15 | [0.58 - 2.31] | 1.55 | [0.87 - 2.77] | 1.34 | [0.59 - 3.06] |
| (0.41) | (0.46) | (0.56) | ||||
| Other | 0.97 | [0.47 - 2.03] | 0.74 | [0.36 - 1.54] | 0.76 | [0.29 - 1.98] |
| (0.37) | (0.28) | (0.37) | ||||
| Nativity (ref: NZ born) | ||||||
| Not born in NZ | 0.95 | [0.57 - 1.58] | 1.03 | [0.65 - 1.63] | 1.08 | [0.58 - 2.02] |
| (0.24) | (0.24) | (0.34) | ||||
| Educational attainment (ref: undergraduate/ postgraduate degree) | ||||||
| Primary/Secondary school | 1.80 | [1.09 - 2.96] | 1.82 | [1.16 - 2.86] | 1.01 | [0.55 - 1.88] |
| (0.46) | (0.42) | (0.32) | ||||
| Diploma | 2.47 | [1.59 - 3.85] | 1.53 | [1.01 - 2.32] | 0.62+ | [0.36 - 1.08] |
| (0.56) | (0.33) | (0.18) | ||||
| Annual household income (ref: More than $150,000) | ||||||
| $50,000 or less | 1.38 | [0.68 - 2.80] | 1.99 | [0.99 - 3.98] | 1.44 | [0.58 - 3.57] |
| (0.50) | (0.70) | (0.67) | ||||
| $50,001-$70,000 | 1.52 | [0.77 - 3.02] | 1.68 | [0.85 - 3.35] | 1.11 | [0.45 - 2.70] |
| (0.53) | (0.59) | (0.50) | ||||
| $70,001-$100,000 | 0.96 | [0.49 - 1.91] | 1.76 | [0.93 - 3.32] | 1.82 | [0.77 - 4.34] |
| (0.34) | (0.57) | (0.81) | ||||
| $100,001-$150,000 | 0.94 | [0.47 - 1.85] | 1.26 | [0.67 - 2.38] | 1.34 | [0.56 - 3.22] |
| (0.32) | (0.41) | (0.60) | ||||
| Family structure (ref: Two parents, dependent children) | ||||||
| Single parent | 1.58 | [0.78 - 3.21] | 1.04 | [0.48 - 2.25] | 0.66 | [0.27 - 1.62] |
| (0.57) | (0.41) | (0.30) | ||||
| Living alone | 0.78 | [0.42 - 1.47] | 0.44 | [0.21 - 0.93] | 0.56 | [0.23 - 1.38] |
| (0.25) | (0.17) | (0.26) | ||||
| Partner, no dependent children | 0.56 | [0.34 - 0.92] | 1.05 | [0.67 - 1.65] | 1.89 | [1.02 - 3.50] |
| (0.14) | (0.24) | (0.60) | ||||
| Other | 0.45 | [0.23 - 0.89] | 0.87 | [0.49 - 1.54] | 1.94 | [0.86 - 4.36] |
| (0.16) | (0.25) | (0.80) | ||||
| Work status (ref: employed) | ||||||
| Unemployed | 1.08 | [0.52 - 2.26] | 0.76 | [0.35 - 1.62] | 0.70 | [0.27 - 1.81] |
| (0.41) | (0.29) | (0.34) | ||||
| Not working | 1.13 | [0.67 - 1.91] | 0.71 | [0.43 - 1.18] | 0.63 | [0.33 - 1.21] |
| (0.30) | (0.18) | (0.21) | ||||
| Region (ref: Auckland) | ||||||
| Northland | 1.61 | [0.71 - 3.65] | 1.08 | [0.44 - 2.69] | 0.67 | [0.22 - 2.01] |
| (0.67) | (0.50) | (0.38) | ||||
| Waikato, Northern Ruapehu | 1.10 | [0.59 - 2.02] | 1.09 | [0.62 - 1.93] | 1.00 | [0.47 - 2.12] |
| (0.34) | (0.32) | (0.38) | ||||
| Whakatane, Tauranga, Rotorua, Taupo | 1.68 | [0.84 - 3.35] | 0.84 | [0.37 - 1.93] | 0.50 | [0.19 - 1.31] |
| (0.59) | (0.36) | (0.25) | ||||
| Gisborne/Tairawhiti | 0.86 | [0.18 - 4.21] | 1.66 | [0.47 - 5.88] | 1.93 | [0.32 - 11.79] |
| (0.70) | (1.07) | (1.78) | ||||
| Hawke's Bay | 0.49 | [0.14 - 1.74] | 1.26 | [0.55 - 2.93] | 2.56 | [0.63 - 10.43] |
| (0.32) | (0.54) | (1.83) | ||||
| Taranaki | 1.09 | [0.40 - 2.96] | 0.75 | [0.24 - 2.35] | 0.69 | [0.17 - 2.73] |
| (0.56) | (0.44) | (0.48) | ||||
| Manawatu, Whanganui, South Ruapehu | 1.13 | [0.50 - 2.55] | 1.49 | [0.75 - 2.97] | 1.31 | [0.51 - 3.39] |
| (0.47) | (0.52) | (0.64) | ||||
| Wellington, Hutt Valley, Wairarapa | 0.68 | [0.36 - 1.31] | 0.66 | [0.37 - 1.20] | 0.97 | [0.43 - 2.20] |
| (0.23) | (0.20) | (0.41) | ||||
| Nelson-Marlborough | 1.07 | [0.42 - 2.74] | 0.66 | [0.22 - 2.03] | 0.62 | [0.16 - 2.34] |
| (0.51) | (0.38) | (0.42) | ||||
| Canterbury, West Coast | 0.79 | [0.44 - 1.44] | 0.96 | [0.58 - 1.58] | 1.21 | [0.59 - 2.46] |
| (0.24) | (0.24) | (0.44) | ||||
| Otago, Southland | 1.89 | [1.00 - 3.58] | 0.55 | [0.25 - 1.22] | 0.29 | [0.12 - 0.73] |
| (0.62) | (0.22) | (0.14) | ||||
| Constant | 0.10 | [0.04 - 0.27] | 0.04 | [0.01 - 0.10] | 0.37 | [0.11 - 1.32] |
| (0.04) | (0.02) | (0.33) | ||||
| Pseudo R2 | .07 | .07 | .07 | |||
| N | 1,284 | 1,284 | 1,284 | |||
RRR = Relative risk ratio. CI = Confidence intervals.
Women were not statistically different to men in their risk of being unlikely to receive the vaccine versus being likely, net of other sociodemographic characteristics. Women, however, were more likely to be unsure they would get the vaccine compared with men. Women were 60.0% (RRR = 1.60, [1.14, 2.24]) greater risk of being unsure versus likely to get the vaccine compared with men, but also over twice as likely (RRR = 2.15, [1.36, 3.39]) of being unsure than unlikely to get the vaccine compared with men. Taken together, men were as likely as women to be at risk of saying they were unlikely to get the vaccine, whereas women were more likely to be unsure.
Higher educational attainment was strongly related to being likely to take the vaccine. Those without university or postgraduate degrees were most at risk of being unlikely to get the vaccine, with those with a primary/secondary school qualification only being 1.8 times (RRR = 1.80, [1.09, 2.96]) and those with a post-secondary diploma 2.5 times (RRR = 2.47, [1.59, 3.85]) at greater risk of being unlikely to take the vaccine (vs. likely). Those without university/postgraduate degrees were also at greater risk of being unsure than likely. Neither household income or ethnicity was correlated with vaccine hesitancy.
2.2. Reasons for vaccine hesitancy
Among those who were unsure or unlikely to take the COVID-19 vaccine, 40.1% selected just one reason, 24.8% selected two reasons, 14.6% gave three reasons, and a further 11.8% offered four or more reasons. The remaining 8.7% offered no explicit reason.12
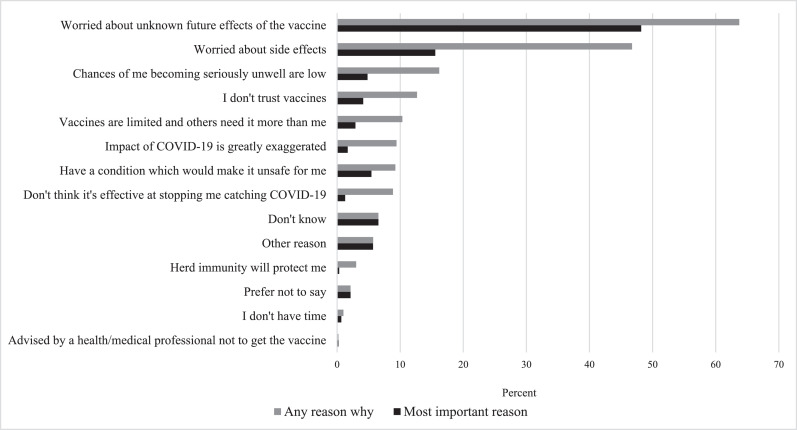
Figure 1 displays the reasons why respondents were unlikely to or unsure about receiving the COVID-19 vaccine. The primary concerns were potential unknown long-term effects (63.7% of vaccine hesitant respondents), followed by those concerned about the side effects (46.7%), and those who thought their chances of becoming seriously ill if they caught COVID-19 were low (16.2%). Very few respondents cited being protected by herd immunity (3.0% of those unlikely or unsure; 15 people), not having time (1.0%; five people), or being advised by a health or medical professional to not get the vaccine (0.21%; one person) as a reason.
Figure 1.
Reasons why unlikely or unsure of getting the COVID-19 vaccine (n = 375)
Note. Weighted %s.
Respondents were also asked, of the reasons they identified, which was the most important reason. The pattern of results were similar to when respondents were asked to select any number of reasons—that is, reasons that a larger proportion of respondents suggested was influencing their vaccine hesitancy were also more likely to be selected as the most important reason. Worried about unknown future effects of the vaccines was most often listed as the most important reason, with close to half (48.2%) of respondents selecting this reason, followed by being worried about the side effects (15.6%).
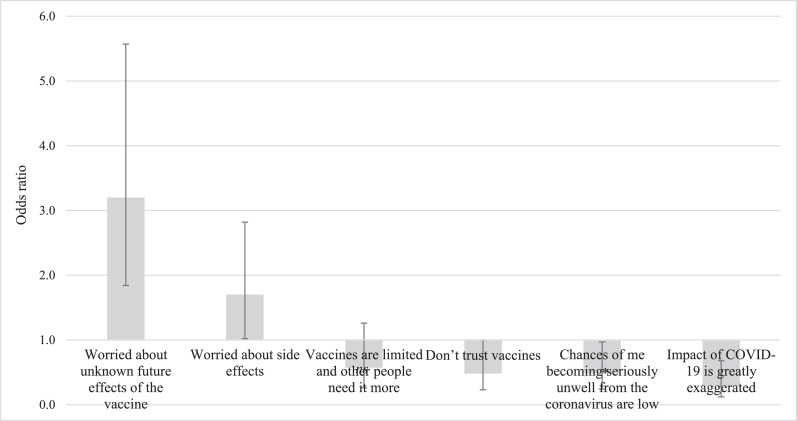
Several key findings emerged when estimating a series of logit regressions to examine the association between key sociodemographic characteristics and reasons for being unlikely or unsure of taking the vaccine (Figure 2).13 First, women were more likely than men to report reasons related to the potential impact of the vaccine on their health, with women over three times more likely (Odds Ratio [OR] = 3.20, [1.84, 5.57]) to say they were worried about unknown future effects of the vaccine and 1.7 times more likely (OR = 1.7, [1.02, 2.28]) to say they were worried about vaccine's side effects. Women were less likely than men to say that the chances were low they would become seriously unwell if they caught COVID-19 (OR = 0.48, [0.24, 0.97]) and that the impact of COVID-19 was being greatly exaggerated (OR = 0.29, [0.12, 0.68]). People aged between 25-34 years, 35-44 years, 45-54 years, and 55-64 years were between 2.6 and 4.6 times more likely to report they were worried about unknown future vaccine effects than people aged 65 and older.
Figure 2.
Odds likelihood of reporting reason for women compared to men (n = 375)
Note. Errors bars represent 95% confidence intervals. Error bars that overlap at 1.0 on the y-axis indicate differences between women and men were not statistically significant at traditional levels. Models control for: age, ethnicity, nativity, educational attainment, household income, household structure, work status, and region of residence. Full model results presented in Table A2 in the appendix.
2.3. Reasons for likelihood of COVID-19 vaccine uptake
Those who reported they were likely to take the COVID-19 vaccine were more likely than vaccine hesitant respondents to cite multiple reasons for their choice. This was despite potential vaccine takers having fewer response options available to select than vaccine hesitant respondents. A small majority (51.0%) of likely vaccine takers selected four reasons or more, 12.2% selected three reasons, 9.3% selected two reasons, and 25.5% selected one reason. Two percent gave no reason.14
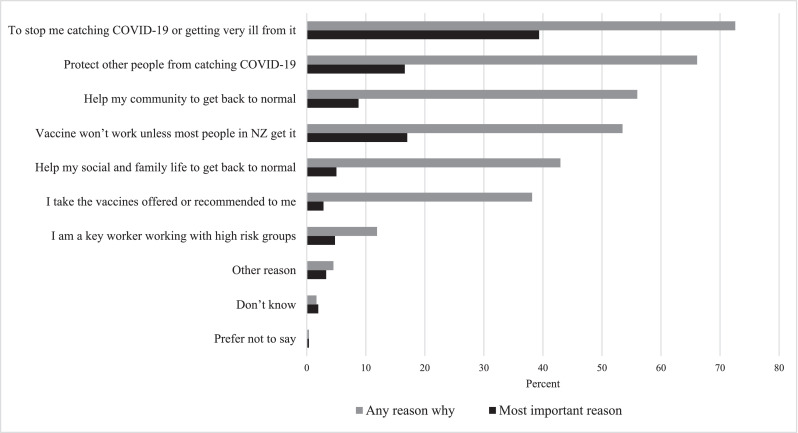
Figure 2 displays the reasons why respondents were likely to receive the vaccine. Close to three-quarters of respondents (72.6%) cited they wanted to prevent catching COVID-19 or getting very ill from it and two-thirds (66.1%) identified protecting others from catching COVID-19. Another 56.0% said to help their community get back to normal and 53.5% cited that they would get the vaccine because it would not work unless most people in New Zealand got the vaccine. Among those who selected ‘other’ and gave a reason (3.3%), the majority noted the ability to travel as being important in their decision (Figure 3).
Figure 3.
Reasons likely to take the COVID-19 vaccine (n = 909)
Note. Weighted %s.
When asked to identify the most important reason why they were likely to take the vaccine, there was more variability in responses among those likely to get the vaccine than those who were unlikely. Close to four in ten (39.4%) of likely vaccine takers said the most important reason influencing them to get the vaccine was to stop them from catching COVID-19 or getting very ill if they caught it. Protecting other people from catching COVID-19 and the vaccine not working unless most people in New Zealand got it were both identified as the most important reason by 17.0% of the sample. Helping the community get back to normal was identified by 8.8% of the sample as being the most important reason for getting the vaccine.
Examining the associations between key sociodemographic characteristics and reason for being likely to take the COVID-19 vaccine through a series of logit regression models, age, gender, ethnicity, education, and income were all statistically significant predictors.15 Those aged 18-24 years (OR = 0.33, [0.14, 0.74]) and 25-34 years (OR = 0.38, [0.18, 0.78]) were less likely to report that a reason for getting the vaccine was to stop them from catching or getting very ill from COVID-19 compared to those 65 years and older. Those 35-44 years (OR = 0.30, [0.16, 0.56]), 45-54 years (OR = 0.41, [0.24, 0.72]), and 55-64 years (OR = 0.59, [0.36, 0.97]) were less likely to report that they took the vaccines offered to them compared to those 65 years and older. Women were more likely than men to report that helping protect others from catching COVID-19 (OR = 1.35, [1.00, 1.82]), protecting other people from catching COVID-19 (OR = 1.64, [1.20, 2.23]), and taking vaccines recommended to them (OR = 1.49, [1.10, 2.02]) as reasons for getting the vaccine once available. Those who identified as Asian were less likely than other ethnicities to report all but two of the reasons—to help allow their social and family life to get back to normal and because they take the vaccines offered or recommended to them—for getting the vaccine.
Those with university/postgraduate degrees were more likely than those without university/postgraduate degrees to cite most reasons, with one exception: there were no education differences in identifying “taking vaccines that are recommended” as a reason. Similarly, those in the highest income bracket (household incomes over NZ$150,000 per annum) were more likely than lower income brackets to identify helping allow their social and family life get back to normal, helping allow their community get back to normal, and that the vaccine won't work unless most people in New Zealand get it as reasons they would likely get the vaccine. There were few income differences in identifying “to stop me catching COVID-19 or getting very ill from it,” “to help protect others from catching COVID-19,” and taking the vaccines recommended to them as reasons for likely getting the vaccine.
3. Discussion
The success of New Zealand's elimination strategy in curbing the impact of COVID-19 on population health and reopening New Zealand's international borders is contingent on high and equitable uptake of the COVID-19 vaccine. This study aimed to examine New Zealanders’ intended likelihood of receiving the vaccine in the lead up to the rollout to the general population, targeted to begin in May 2021 for adults at high-risk of getting very sick from COVID-19 disease and in July 2021 for the rest of the adult population. In addition, this study examined sociodemographic correlates of intended vaccination as well as the reasons why people were likely or unlikely to get the vaccine. Several key findings emerged.
In line with prior studies on New Zealanders’ COVID-19 vaccine hesitancy, 71% of respondents said they were either very likely or somewhat likely to take the vaccine once it became available. This rate of vaccine likelihood was consistent despite data for this study being collected in mid-to-late March just after concerns around potential increased risk of blood clots from the AstraZeneca vaccine saw multiple European countries suspend their vaccination programme. [35] Again, consistent with prior New Zealand research, bivariate associations between individual sociodemographic characteristics and vaccine likelihood showed that younger people, women, and those who identified as Māori were less likely to report they would get the vaccine, whereas those with higher educational attainment and higher household incomes were more likely to report they would be getting the vaccine. The socioeconomic gradient in vaccine hesitancy is consistent with studies of vaccine hesitancy in Australia. [13,14]
Importantly, however, several of these associations attenuated once they were examined in a multivariate framework. In this model, net of other sociodemographic variables, Māori were no longer at greater risk of vaccine hesitancy, compared to other ethnic groups. Thus, it is likely that other sociodemographic characteristics that are overrepresented in the Māori population (vs. the general population) account for much of the disparity regarding vaccine hesitancy seen in the initial bivariate findings. Namely, the Māori population is younger, has lower levels of educational attainment, and is underrepresented among the highest income bracket—all factors that appear to have stronger correlations with vaccine hesitancy than ethnicity once examined simultaneously.
This finding is important because ensuring that the components of a comprehensive COVID-19 vaccination strategy are appropriately targeted and do not exacerbate health inequities is critical for programme effectiveness. These results do not negate the need to counter vaccine hesitancy, nor the need for a Māori-focused and –led approach to COVID-19 vaccination. Inequities in vaccination delivery are consistent and compelling in New Zealand with Māori and Pacific rates of vaccination delivery and timeliness in childhood consistently lower than non-Māori, non-Pacific people. [36,37] In childhood, this lower vaccination delivery has also been demonstrated to reflect poor health care access rather than parental intentions to vaccinate their children. [38] The broader literature has demonstrated that equitable health care delivery for Māori (and Pacific), such as with the immunisation programme, will require Māori governance and leadership, culturally-responsive health care delivery, resourcing of trusted community providers, and supports for access. [39], [40], [41], [42] It is known that the current primary health care system in New Zealand fails to deliver on these points, and fails to meet legal obligations to Māori. [43] Ongoing attention needs to be paid to the critical combination of heightened risk of mortality and morbidity from COVID-19 disease for Māori and Pacific populations [13] and the systemic racism within New Zealand's health system that will result in inability to translate rates of vaccination intention into vaccine access and uptake. [44]
While the findings suggest that there are no or negligible ethnic differences in people's trust and understanding of the importance of getting the vaccine, these findings, and their implications, are consistent with the success of Māori community-led responses that went beyond government initiatives and policies aimed at preventing the spread of COVID-19—for example, the establishment of community-based lockdown roadblocks and trialling new contact tracing technologies such as Bluetooth cards. [45], [46], [47], [48]
Another important finding was that women were slightly less likely to say they would get the vaccine than men, however this disparity was driven primarily by women saying they were “unsure” they would not get it (17.7% vs. 12.2%, respectively). Indeed, men were more likely to report that they were very unlikely than women. While prior research has noted women are less likely to say they would get the vaccine, the disparity between our findings and prior research may be driven by the inclusion of an “unsure” category in the middle of the scale, which seems to better reflect women's intention to get the vaccine than being confined to “somewhat or very unlikely” or “somewhat or very likely” (with “don't know” and “not really sure” outside the Likert scale). In sum, women appear less definitive in terms of being unlikely to get the vaccine and may be more easily nudged towards taking the vaccine.
Gender also appeared to be statistically significantly associated with different reasons for vaccine hesitancy. Women were more likely than men to identify potential risks to their personal health, such as unknown future vaccine effects or potential side effects as reasons for being unlikely to receive the vaccine, whereas men were more likely to report broader concerns around the trustworthiness of vaccines generally, being confident they would not get seriously ill should they contract COVID-19, and feeling that the pandemic has been exaggerated.
Finally, people who reported they were likely to get the vaccine were, on average, more likely to identify multiple reasons for their decision, compared to the average number of reasons identified among those unlikely to get the vaccine. Moreover, the most important reason cited was also more heavily concentrated in the most popular reason among those unlikely to get the vaccine. For example, 48% who were unsure/unlikely they would get the vaccine said the most important reason was because of worry about unknown future vaccine effects. The most important reason was more dispersed among likely vaccine takers with 39% selecting the most popular reason (to stop them from catching COVID-19 or getting very ill) as also the most important reason. Taken together, this suggests there are wide range of positive benefits that can be employed to demonstrate the utility of the vaccine to those who are currently hesitant, in addition to efforts around dispelling fears around vaccine safety and science.
This study has several limitations. First, although the study sample is sociodemographically diverse, weighting was applied to replicate population-level sociodemographics, and our estimates of COVID-19 vaccine hesitancy are in line with existing New Zealand studies, the findings may not necessarily be extrapolated to the general population. Indeed, by virtue of being an online survey, participants must have access to an electronic device and the internet and, hence, are likely slightly more advantaged. It also would not include those living in institutionalised settings, such as prisons or supported living situations. Combined with the study findings that those younger and from lower socioeconomic groups were more vaccine hesitant could potentially mean that the estimated socioeconomic and age disparities in vaccine hesitancy may be wider, and that the overall rate of vaccine hesitancy may be higher than reported.
Second, the findings are correlational not causal. There are likely confounding variables not included in the models, such as urbanicity which has been shown to matter for COVID-19 vaccine in other countries, [49] or factors that are unmeasurable that explain some of the statistically significant associations. For example, health literacy, which we did not capture in our survey, has been found to be associated with both educational attainment and lower rates of vaccine hesitancy and likely explains some of the statistical association between education and vaccine acceptance. [50]
Overall, a majority of New Zealand adults in our sample are likely to take the COVID-19 vaccine when the Immunisation Programme opens to the general population. There remains, however, a sizeable proportion who are unsure about or unlikely to take the vaccine. Public health initiatives should promote the safety and science of the vaccine, message that individual uptake increases the vaccine's efficacy for the whole community, and have a particular focus on younger and less educated populations. Moreover, public health efforts will need to combat known inequities in health care access that may increase the risk that vaccine intention does not translate into uptake among subgroups, such as Māori and Pacific, who are at heightened risk of COVID-19 infection and morbidity.
Contributors
Dr. Kate Prickett and Dr. Hanna Habibi conceived of the research question and developed the survey that collected the data. Dr. Habibi cleaned the data and conducted the analyses. Dr. Prickett reviewed the code and analyses. Dr. Prickett, Dr. Habibi, and Dr. Polly Atatoa Carr contributed to the data interpretation. Dr. Prickett developed the first manuscript draft. All authors edited the manuscript, provided a critical review, and approved the final manuscript. Dr. Prickett and Dr. Habibi assessed the underlying data. They take responsibility for the underlying data and analysis accuracy and integrity.
Data sharing agreement
Deidentified participant data and program code used to produce the results for this study, along with a data dictionary, are available upon request from the lead author, Kate Prickett (kate.prickett@vuw.ac.nz). Consent to publish with the data must be sought from Kate Prickett.
Funding
N/a.
Declaration of Competing Interest
The authors declare no conflicts of interest.
Acknowledgements
N/a
Footnotes
We note an unforeseen implication of this strategy: due to the lockdown being an unusual period, subgroups that are typically harder-to-reach responded faster than usual, ending with an overrepresention of, for example, young men. Survey weights correct for this overrepresentation.
It is not possible to calculate a typical response rate (number responded / number contacted) given the survey closed once around 2,000 responses were reached. For example, those who were extended an invitation to participate may have responded had the survey not closed. As another, others would have tried to participate but would have been screened out had their particular quota of sociodemographic characteristics been met.
The cut-off of around 2,000 respondents was due to costs of implementing the survey, which are a combination of fixed costs for survey development and programming/scripting, and variable costs for number of survey responses. Approximately 2,000 respondents for Wave 1 was deemed a reasonably safe number of respondents in order to have a sample size of at least 1,000 in the Wave 2 follow-up survey (based on a 50% rate of attrition). The actual response rate for Waves 2 and 3 exceeded expectations.
All three respondents said they were “very likely” to take the COVID-19 vaccine.
More information on sociodemographic differences betweeen those in the analytical sample versus those who attrited from the study can be found in Table A1 in the appendix.
The survey questions and response on likelihood of COVID-19 vaccine uptake and reasons for acceptance/hesitancy can be found in Table A3 in the appendix.
We do not report results for the three respondents who identified as gender diverse.
Respondents were able to select multiple ethnicities, which were then recoded in prioritised, mutually-exclusive categories in the following order: Māori, Pacific; Asian; NZ European/Pākeha; Other ethnicities.
These categories convert to around US$21,000 / €17,600 or less in the lowest income category through to over US$105,000 / €88,200 in the highest income category, as of June 2021.
Public health unit areas represent regions that administer public health services. Moreover, areas with large urban centres were more likely to have Managed Isolation Quarantines facilities, and hence, higher risk of COVID-19 transmission into the community. In particular, Auckland city was most impacted, experiencing three additional regional lockdowns in response to community transmission from infections in MIQ during the year since the nationwide lockdown (March-April 2020). Information on urbanicity/rurality was not collected.
Income, household structure, work status, and public health unit region were time-varying variables captured at each data collection. We use the measures captured at wave 3, and hence, most temporal to the outcome being examined.
Covariates with missing data included nativity (n = 162 missing); educational attainment (n = 11); household income (n = 95); age (n = 4); and, ethnicity (n = 3).
Full set of results presented in Table A4 in the appendix.
Full set of results presented in Table A5 in the appendix.
Full set of results presented in Table A6 in the appendix.
Full set of results presented in Table A7 in the appendix.
Appendix
Table A1, Table A2, Table A3, Table A4, Table A5, Table A6, Table A7.
Table A1.
Comparison of key sociodemographic characteristics at Wave 1 between those in the analytical sample, those attrited by Wave 3, and those missing vaccine acceptance data
| Study sample (n = 1,284) |
Missing at Wave 3 (n = 692) |
Participated in W3 but missing vaccine data (n = 23) |
||||
|---|---|---|---|---|---|---|
| n | Column % | n | Column % | n | Column % | |
| Age (years) | ||||||
| 18-24 | 81 | 6.33 | 154 | 22.38 | 1 | 4.55 |
| 25-34 | 175 | 13.67 | 182 | 26.45 | 5 | 22.73 |
| 35-44 | 255 | 19.92 | 124 | 18.02 | 7 | 31.82 |
| 45-54 | 290 | 22.66 | 86 | 12.50 | 6 | 27.27 |
| 55-64 | 256 | 20.00 | 74 | 10.76 | 2 | 13.64 |
| 65+ | 223 | 17.42 | 68 | 9.88 | 0 | 0.00 |
| Gender | ||||||
| Female | 550 | 42.83 | 279 | 40.49 | 10 | 45.45 |
| Male | 734 | 57.17 | 410 | 59.51 | 12 | 54.55 |
| Ethnicity | ||||||
| European/Pākehā | 798 | 62.15 | 405 | 58.78 | 11 | 50.00 |
| Māori | 165 | 12.85 | 103 | 14.95 | 3 | 13.64 |
| Pacific | 81 | 6.31 | 73 | 10.60 | 3 | 13.64 |
| Asian | 134 | 10.44 | 51 | 7.40 | 1 | 4.55 |
| Other | 106 | 8.26 | 57 | 8.27 | 4 | 18.18 |
| Educational attainment | ||||||
| Primary/Secondary school | 336 | 26.31 | 214 | 32.23 | 2 | 10.00 |
| Diploma | 425 | 33.36 | 191 | 28.77 | 7 | 35.00 |
| Undergraduate/Postgraduate degree | 512 | 40.22 | 259 | 39.01 | 11 | 55.00 |
Unweighted ns and %s. Sum of subgroups may not add up to total sample n due to missing values.
Table A2.
Checklist for Reporting Results of Internet E-Surveys (CHERRIES)
| Item category | Checklist item | Description |
|---|---|---|
| Design | Survey design | Information on the survey design, sampling frame, and analytical sample can be found in the Methods section. |
| Ethics | Ethics approval | Human ethics approval (Application ID 0000029123) was granted as a Category B study (low risk) by the Victoria University of Wellington Human Ethics Committee. |
| Informed consent | Informed consent was provided on the introduction screen of the survey. Respondents were informed the survey should take approximately 10 minutes to complete and the reasons for the study. The respondents were provided information on who the research team was, that we did not have access to information that would identify them, and the name, email, and contact phone number for the Victoria University of Wellington Human Ethics Committee convenor should they have concerns. | |
| Data protection | There is no identifying information stored with the data nor available to the study team, such as names, birthdates, or IP addresses. The anonymised data are only accessible to the Life in Lockdown research team. | |
| Development and pre-testing | Development and testing | The survey was developed by the Life in Lockdown team. The programming and scripting was conducted by Colmar Brunton. Testing of the usability and technical functionality of the electronic questionnaire was performed by both the Life in Lockdown research team and Colmar Brunton before fielding the questionnaire. |
| Recruitment process | Open survey versus closed survey | The survey was closed and only accessible by email invite with a unique survey link. |
| Contact mode | Potential participants were contacted directly via email. | |
| Advertising the survey | There was no advertising of the survey. | |
| Survey administration | Web/E-mail | Survey links were sent directly via email to potential participants. Participants were part of a large existing social marketing sampling frame. See the Methods section for more information on the sampling frame and how participants were selected. |
| Context | See the Methods section for more information on the sampling frame. See the Discussion section for information on potential bias within the sample. | |
| Mandatory/voluntary | Voluntary. | |
| Incentives | Survey respondents were offered 10 Fly Buys points for participating in the survey. Fly Buys is a large reward-based business loyalty system in New Zealand, covering many large businesses. | |
| Time/Date | Data for Wave 3 were collected in March 2021. Data from Wave 1 and Wave 2 were collected in April 2020 and July 2020, respectively. | |
| Randomisation of items or questionnaires | Not performed. | |
| Adaptive questioning | Adaptive questioning was used in multiple instances, including around work circumstances, household structure, and family wellbeing. | |
| Number of items | The Wave 3 survey had 48 items. This, however, includes skip patterns and no respondent would have answered all 48 items. The median survey completion time was 10 minutes. | |
| Number of screens (pages) | Information not accessible. | |
| Response rates | Unique site visitor | Information not accessible. |
| View rate | Information not accessible. | |
| Participation rate | Information not accessible. See footnote i for a discussion on participation and response rates. | |
| Completion rate | 100% | |
| Preventing multiple entries from the same individual | Cookies used | Not used. |
| IP check | Not used. | |
| Log file analysis | Not used. | |
| Registration | Participants were emailed with a unique survey link that could only be accessed from their personal email account and valid once. | |
| Analysis | Handling of incomplete questionnaires | There were no incomplete questionnaires, although there was some missingness on item-level responses. Multiple imputation was conducted on the small amount of missing analytical data, with models estimated across the 100 imputed datasets. |
| Questionnaires submitted with an atypical timestamp | Two questionnaire responses who completed the survey in a time frame deemed impossible (i.e., less than three minutes) were discarded. | |
| Statistical correction | Weights were constructed to adjust the sample to the New Zealand adult population proportions on age, gender, income, region, and household structure. |
Table A3.
Survey questions on COVID-19 vaccine hesitancy/acceptance and reasons for vaccine hesitancy/acceptance
| 1. How likely are you to get vaccinated for the coronavirus (Covid-19) once the vaccine is available to you? | |
| Very unlikely | 1 |
| Somewhat unlikely | 2 |
| Unsure | 3 |
| Somewhat likely | 4 |
| Very likely | 5 |
| I have already received at least one dose of the Covid-19 vaccine | 10 |
| Prefer not to say | 6 |
| N/A | 7 |
| ASK 2a IF 1 = (1 | 2 | 3) | |
| ASK 3a IF 1 = (4 | 5) | |
| 2a. For what reasons would you be unlikely to get a vaccine for coronavirus (Covid-19) if it was offered to you? | |
| (Check all that apply) | |
| I am worried about unknown future effects of the vaccine | 1 |
| I am worried about side effects | 2 |
| Vaccines are limited and other people need it more than me | 3 |
| I don't trust vaccines | 4 |
| The chances of me becoming seriously unwell from the coronavirus are low | 5 |
| The impact of the coronavirus is being greatly exaggerated | 6 |
| I don't think it would be effective at stopping me catching the coronavirus | 7 |
| I have a condition which would make it unsafe for me | 8 |
| Herd immunity will protect me even if I don't have the vaccine | 9 |
| I don't have time | 10 |
| I have been advised by a health or medical professional not to get the vaccine | 11 |
| Other (please tell us) | 12 |
| Don't know | 88 |
| Prefer not to say | 99 |
| ASK 2b if a response other than only “Don't know” or “Prefer not to say” are given AND 2A=MR | |
| Skip to end of section if only “Don't know” and “Prefer not to say” selected. | |
| 2b. Of those reasons you selected, what would you say is the most important reason you would be unlikely to get the vaccine? | |
| (Choose 1 only) | |
| [Populate the answer options selected from 2a] | n |
| Don't know | 11 |
| Prefer not to say | 12 |
| Skip to next section | |
| 3a. For what reasons are you likely to get a vaccine for coronavirus (Covid-19) if it was offered to you? | |
| (Check all that apply) | |
| To stop me catching the coronavirus or getting very ill from it | 1 |
| To help allow my social and family life to get back to normal | 2 |
| To help allow my community to get back to normal | 3 |
| To help protect other people from catching the coronavirus | 4 |
| Because the vaccine won't work unless most people in New Zealand get it | 5 |
| Because I am a key worker working with high risk groups | 6 |
| Because I take the vaccines offered or recommended to me | 7 |
| Other (please tell us) | 8 |
| Don't know | 88 |
| Prefer not to say | 99 |
| 3b. Of those reasons you selected, what would you say is the most important reason you will likely get the vaccine? | |
| (Choose 1 only) | |
| [Populate the answer options selected from 3a] | n |
| Don't know | 11 |
| Prefer not to say | 12 |
Table A4.
Reasons why unlikely to or unsure of getting the vaccine (n = 375)
| n | % | |
|---|---|---|
| All reasons why not | ||
| I am worried about unknown future effects of the vaccine | 235 | 63.73 |
| I am worried about side effects | 184 | 46.74 |
| Vaccines are limited and other people need it more than me | 41 | 10.34 |
| I don't trust vaccines | 50 | 12.67 |
| The chances of me becoming seriously unwell from the coronavirus are low | 60 | 16.18 |
| The impact of the coronavirus is being greatly exaggerated | 39 | 9.42 |
| I don't think it would be effective at stopping me catching the coronavirus | 35 | 8.85 |
| I have a condition which would make it unsafe for me | 31 | 9.23 |
| Herd immunity will protect me even if I don't have the vaccine | 15 | 3.02 |
| I don't have time | 5 | 1.00 |
| I have been advised by a health or medical professional not to get the vaccine | 1 | 0.21 |
| Other (please specify) | 25 | 5.72 |
| Don't know | 28 | 6.55 |
| Prefer not to say | 8 | 2.13 |
| Number of reasons cited | ||
| Gave no reason | 36 | 8.68 |
| 1 reason | 139 | 40.10 |
| 2 reasons | 94 | 24.81 |
| 3 reasons | 57 | 14.57 |
| 4 or more reasons | 49 | 11.84 |
| Most important reason | ||
| I am worried about unknown future effects of the vaccine | 171 | 48.19 |
| I am worried about side effects | 60 | 15.57 |
| Vaccines are limited and other people need it more than me | 11 | 2.90 |
| I don't trust vaccines | 16 | 4.14 |
| The chances of me becoming seriously unwell from the coronavirus are low | 15 | 4.83 |
| The impact of the coronavirus is being greatly exaggerated | 7 | 1.69 |
| I don't think it would be effective at stopping me catching the coronavirus | 6 | 1.27 |
| I have a condition which would make it unsafe for me | 19 | 5.45 |
| Herd immunity will protect me even if I don't have the vaccine | 2 | 0.34 |
| I don't have time | 4 | 0.67 |
| I have been advised by a health or medical professional not to get the vaccine | 1 | 0.21 |
| Other (please specify) | 24 | 5.70 |
| Don't know | 28 | 6.55 |
| Prefer not to say | 8 | 2.13 |
Unweighted ns, weighted %s.
Table A5.
Logit regression predicting reasons why vaccine hesitant (n = 375)
| Worried about unknown future effects of the vaccine |
Worried about side effects |
Vaccines are limited and other people need it more than me |
I don't trust vaccines |
Chances of me becoming seriously unwell from the coronavirus are low |
Impact of the coronavirus is being greatly exaggerated |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
Model 6 |
|||||||
| OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | |
| Age (ref: 65+ years) | ||||||||||||
| 18-24 years | 1.55 | [0.44 - 5.47] | 0.27 | [0.08 - 0.94] | 0.29 | [0.02 - 3.41] | 0.82 | [0.14 - 4.68] | 1.15 | [0.26 - 5.04] | 0.24 | [0.03 - 1.76] |
| (1.00) | (0.17) | (0.37) | (0.73) | (0.87) | (0.24) | |||||||
| 25-34 years | 4.15 | [1.36 - 12.63] | 0.79 | [0.28 - 2.23] | 1.14 | [0.24 - 5.47] | 0.45 | [0.10 - 1.98] | 0.83 | [0.22 - 3.11] | 0.21 | [0.04 - 1.05] |
| (2.36) | (0.42) | (0.91) | (0.34) | (0.56) | (0.17) | |||||||
| 35-44 years | 4.63 | [1.52 - 14.10] | 0.50 | [0.17 - 1.42] | 1.54 | [0.32 - 7.48] | 0.33 | [0.07 - 1.47] | 0.31 | [0.07 - 1.29] | 0.13 | [0.03 - 0.70] |
| (2.63) | (0.27) | (1.24) | (0.25) | (0.23) | (0.11) | |||||||
| 45-54 years | 2.59 | [0.94 - 7.14] | 0.57 | [0.22 - 1.50] | 0.90 | [0.20 - 4.05] | 0.57 | [0.15 - 2.24] | 0.39 | [0.10 - 1.47] | 0.23 | [0.05 - 1.04] |
| (1.34) | (0.28) | (0.69) | (0.40) | (0.26) | (0.18) | |||||||
| 55-64 years | 3.16 | [1.22 - 8.18] | 0.67 | [0.27 - 1.66] | 0.70 | [0.17 - 2.87] | 0.98 | [0.27 - 3.52] | 0.64 | [0.20 - 2.11] | 0.51 | [0.13 - 2.01] |
| (1.53) | (0.31) | (0.50) | (0.64) | (0.39) | (0.36) | |||||||
| Gender (ref: male) | ||||||||||||
| Female | 3.20 | [1.84 - 5.57] | 1.70 | [1.02 - 2.82] | 0.57 | [0.26 - 1.26] | 0.48 | [0.23 - 1.00] | 0.48 | [0.24 - 0.97] | 0.29 | [0.12 - 0.68] |
| (0.91) | (0.44) | (0.23) | (0.18) | (0.17) | (0.13) | |||||||
| Ethnicity (ref: European/Pākehā) | ||||||||||||
| Māori | 0.49 | [0.24 - 1.01] | 0.81 | [0.42 - 1.56] | 0.73 | [0.24 - 2.22] | 1.12 | [0.41 - 3.11] | 0.61 | [0.23 - 1.60] | 0.70 | [0.22 - 2.20] |
| (0.18) | (0.27) | (0.41) | (0.58) | (0.30) | (0.41) | |||||||
| Pacific | 0.45 | [0.16 - 1.27] | 0.47 | [0.18 - 1.26] | 1.22 | [0.27 - 5.47] | 1.14 | [0.30 - 4.36] | 2.13 | [0.62 - 7.31] | n/r | |
| (0.24) | (0.24) | (0.93) | (0.78) | (1.34) | ||||||||
| Asian | 1.10 | [0.41 - 2.90] | 1.71 | [0.67 - 4.33] | 0.81 | [0.20 - 3.36] | 1.21 | [0.37 - 3.91] | 0.57 | [0.14 - 2.40] | 0.29 | [0.05 - 1.66] |
| (0.54) | (0.81) | (0.59) | (0.72) | (0.42) | (0.26) | |||||||
| Other | 0.27 | [0.09 - 0.80] | 0.32 | [0.11 - 0.96] | 0.81 | [0.17 - 3.75] | 1.44 | [0.36 - 5.82] | 1.85 | [0.49 - 7.03] | 0.20 | [0.03 - 1.17] |
| (0.15) | (0.18) | (0.63) | (1.03) | (1.26) | (0.18) | |||||||
| Nativity (ref: NZ born) | ||||||||||||
| Not born in NZ | 0.51 | [0.23 - 1.16] | 0.66 | [0.31 - 1.40] | 1.52 | [0.48 - 4.81] | 0.70 | [0.26 - 1.87] | 4.23 | [1.39 - 12.86] | 0.92 | [0.27 - 3.18] |
| (0.21) | (0.25) | (0.89) | (0.35) | (2.40) | (0.58) | |||||||
| Educational attainment (ref: undergraduate/ postgraduate degree) | ||||||||||||
| Primary/Secondary school | 0.75 | [0.38 - 1.49] | 0.49 | [0.25 - 0.94] | 0.49 | [0.18 - 1.29] | 1.02 | [0.37 - 2.80] | 0.71 | [0.31 - 1.64] | 0.94 | [0.32 - 2.78] |
| (0.26) | (0.16) | (0.24) | (0.53) | (0.30) | (0.52) | |||||||
| Diploma | 0.99 | [0.53 - 1.87] | 1.03 | [0.57 - 1.85] | 0.37 | [0.15 - 0.93] | 1.78 | [0.78 - 4.10] | 0.50 | [0.23 - 1.09] | 1.08 | [0.42 - 2.77] |
| (0.32) | (0.31) | (0.17) | (0.76) | (0.20) | (0.52) | |||||||
| Annual household income (ref: More than $150,000) | ||||||||||||
| $50,000 or less | 0.70 | [0.26 - 1.90] | 1.13 | [0.44 - 2.91] | 1.04 | [0.24 - 4.40] | 4.61 | [0.86 - 24.74] | 1.70 | [0.37 - 7.74] | 1.04 | [0.21 - 5.26] |
| (0.36) | (0.55) | (0.77) | (3.95) | (1.31) | (0.86) | |||||||
| $50,001-$70,000 | 1.00 | [0.36 - 2.77] | 1.56 | [0.60 - 4.08] | 0.82 | [0.18 - 3.79] | 4.35 | [0.81 - 23.27] | 2.01 | [0.43 - 9.33] | 0.76 | [0.14 - 4.13] |
| (0.52) | (0.77) | (0.64) | (3.72) | (1.57) | (0.65) | |||||||
| $70,001-$100,000 | 1.84 | [0.68 - 5.03] | 1.66 | [0.66 - 4.15] | 1.35 | [0.33 - 5.53] | 2.22 | [0.41 - 11.95] | 1.53 | [0.35 - 6.67] | 0.56 | [0.10 - 3.03] |
| (0.94) | (0.78) | (0.97) | (1.91) | (1.15) | (0.48) | |||||||
| $100,001-$150,000 | 0.87 | [0.33 - 2.30] | 0.88 | [0.34 - 2.23] | 1.12 | [0.27 - 4.69] | 4.29 | [0.83 - 22.30] | 1.99 | [0.43 - 9.12] | 1.42 | [0.29 - 6.91] |
| (0.43) | (0.42) | (0.82) | (3.61) | (1.55) | (1.15) | |||||||
| Family structure (ref: Two parents, dependent children) | ||||||||||||
| Single parent | 1.39 | [0.46 - 4.19] | 0.46 | [0.18 - 1.21] | 1.26 | [0.23 - 6.87] | 0.99 | [0.29 - 3.37] | 0.72 | [0.19 - 2.70] | 0.71 | [0.16 - 3.18] |
| (0.78) | (0.23) | (1.09) | (0.62) | (0.49) | (0.54) | |||||||
| Living alone | 0.91 | [0.33 - 2.46] | 0.31 | [0.12 - 0.79] | 2.50 | [0.64 - 9.75] | 0.19 | [0.04 - 1.03] | 0.18 | [0.04 - 0.81] | 0.29 | [0.06 - 1.36] |
| (0.46) | (0.15) | (1.74) | (0.16) | (0.14) | (0.23) | |||||||
| Partner, no dependent children | 1.31 | [0.65 - 2.67] | 0.78 | [0.41 - 1.50] | 2.81 | [1.01 - 7.88] | 0.45 | [0.17 - 1.17] | 0.41 | [0.17 - 1.02] | 0.12 | [0.04 - 0.43] |
| (0.47) | (0.26) | (1.48) | (0.22) | (0.19) | (0.08) | |||||||
| Other | 0.66 | [0.27 - 1.59] | 0.95 | [0.40 - 2.21] | 1.40 | [0.32 - 6.16] | 0.73 | [0.22 - 2.39] | 0.39 | [0.12 - 1.21] | 0.86 | [0.23 - 3.18] |
| (0.30) | (0.41) | (1.06) | (0.44) | (0.22) | (0.57) | |||||||
| Work status (ref: employed) | ||||||||||||
| Unemployed | 2.53 | [0.77 - 8.32] | 1.57 | [0.56 - 4.36] | 0.83 | [0.16 - 4.43] | 0.79 | [0.19 - 3.25] | 0.76 | [0.18 - 3.26] | 1.66 | [0.37 - 7.42] |
| (1.54) | (0.82) | (0.71) | (0.57) | (0.56) | (1.27) | |||||||
| Not working | 1.19 | [0.58 - 2.45] | 0.62 | [0.32 - 1.21] | 0.59 | [0.18 - 1.94] | 0.75 | [0.28 - 2.01] | 1.01 | [0.41 - 2.47] | 1.36 | [0.46 - 4.05] |
| (0.44) | (0.21) | (0.36) | (0.38) | (0.46) | (0.76) | |||||||
| Region (ref: Auckland) | ||||||||||||
| Northland | 2.02 | [0.56 - 7.36] | 0.99 | [0.31 - 3.15] | 4.56 | [1.03 - 20.24] | 1.06 | [0.19 - 5.98] | 1.49 | [0.33 - 6.73] | 4.25+ | [0.78 - 23.19] |
| (1.33) | (0.58) | (3.47) | (0.94) | (1.15) | (3.68) | |||||||
| Waikato, Northern Ruapehu | 1.96 | [0.78 - 4.94] | 1.31 | [0.57 - 3.04] | 1.64 | [0.45 - 5.99] | 1.02 | [0.32 - 3.28] | 2.27 | [0.80 - 6.47] | 1.65 | [0.38 - 7.11] |
| (0.93) | (0.56) | (1.08) | (0.61) | (1.21) | (1.23) | |||||||
| Whakatane, Tauranga, Rotorua, Taupo | 1.49 | [0.51 - 4.38] | 1.43 | [0.51 - 3.96] | 0.50 | [0.06 - 4.44] | 1.34 | [0.39 - 4.63] | 0.83 | [0.20 - 3.53] | 4.93 | [1.22 - 19.93] |
| (0.82) | (0.74) | (0.56) | (0.85) | (0.61) | (3.51) | |||||||
| Gisborne/Tairawhiti | 0.07 | [0.01 - 0.78] | 0.45 | [0.07 - 2.94] | n/r | 1.71 | [0.16 - 18.80] | n/r | n/r | |||
| (0.09) | (0.43) | (2.09) | ||||||||||
| Hawke's Bay | 3.44 | [0.72 - 16.36] | 1.95 | [0.52 - 7.26] | 0.71 | [0.08 - 6.67] | 1.27 | [0.22 - 7.43] | 1.13 | [0.21 - 6.09] | 0.77 | [0.08 - 7.84] |
| (2.74) | (1.31) | (0.81) | (1.14) | (0.97) | (0.91) | |||||||
| Taranaki | 6.44 | [0.68 - 61.13] | 1.12 | [0.26 - 4.83] | 1.55 | [0.15 - 16.45] | 0.85 | [0.09 - 8.45] | 0.92 | [0.08 - 10.19] | 1.53 | [0.14 - 16.91] |
| (7.40) | (0.84) | (1.86) | (1.00) | (1.13) | (1.88) | |||||||
| Manawatu, Whanganui, South Ruapehu | 1.70 | [0.60 - 4.86] | 1.43 | [0.54 - 3.81] | 2.14 | [0.51 - 8.96] | 0.24 | [0.03 - 1.98] | 0.65 | [0.16 - 2.62] | 1.86 | [0.38 - 9.13] |
| (0.91) | (0.71) | (1.56) | (0.26) | (0.46) | (1.51) | |||||||
| Wellington, Hutt Valley, Wairarapa | 1.09 | [0.43 - 2.76] | 0.72 | [0.29 - 1.78] | 1.53 | [0.40 - 5.83] | 1.02 | [0.28 - 3.70] | 1.03 | [0.28 - 3.75] | 1.44 | [0.29 - 7.10] |
| (0.52) | (0.33) | (1.04) | (0.67) | (0.68) | (1.17) | |||||||
| Nelson-Marlborough | 0.41 | [0.09 - 1.80] | 1.34 | [0.33 - 5.47] | 0.93 | [0.09 - 9.65] | 0.68 | [0.07 - 7.03] | 0.65 | [0.07 - 6.34] | n/r | |
| (0.31) | (0.96) | (1.11) | (0.81) | (0.76) | ||||||||
| Canterbury, West Coast | 1.19 | [0.53 - 2.70] | 0.84 | [0.39 - 1.81] | 1.72 | [0.51 - 5.76] | 0.77 | [0.24 - 2.47] | 1.28 | [0.45 - 3.61] | 1.11 | [0.30 - 4.08] |
| (0.50) | (0.33) | (1.06) | (0.46) | (0.68) | (0.74) | |||||||
| Otago, Southland | 1.65 | [0.57 - 4.76] | 0.52 | [0.20 - 1.36] | 1.47 | [0.32 - 6.81] | 0.45 | [0.09 - 2.34] | 2.95 | [0.97 - 9.03] | 2.17 | [0.49 - 9.52] |
| (0.89) | (0.25) | (1.15) | (0.38) | (1.68) | (1.64) | |||||||
| Constant | 0.58 | [0.14 - 2.37] | 2.58 | [0.67 - 9.94] | 0.09 | [0.01 - 0.76] | 0.17 | [0.02 - 1.40] | 0.17 | [0.02 - 1.26] | 1.20 | [0.15 - 9.75] |
| (0.42) | (1.78) | (0.10) | (0.18) | (0.17) | (1.28) | |||||||
| Pseudo R2 | .16 | .10 | .10 | .10 | .12 | .17 | ||||||
| n | 375 | 375 | 375 | 375 | 375 | 375 | ||||||
Standard errors in parentheses. CI = Confidence intervals. OR = Odds ratios.
n/r = not reported due to multicollinearity issues:
Model 3: No people living in the Gisborne/Tairawhiti public health unit region reported “Vaccines are limited and other people need it more than me”. Gisborne/Tairawhiti was collapsed with Hawke's Bay for the estimation.
Model 5: No people living in the Gisborne/Tairawhiti public health unit region reported “Chances of me becoming seriously unwell from the coronavirus are low”. Gisborne/Tairawhiti was collapsed with Hawke's Bay for the estimation.
Model 6: No Pacific people reported "The impact of the coronavirus is being greatly exaggerated". Pacific was collapsed with 'Other' ethnicity for the estimation. No people living in the Gisborne/Tairawhiti or Nelson-Marlborough public health unit regions reported “The impact of coronavirus is being greatly exaggerated”. Gisborne/Tairawhiti was collapsed with Hawke's Bay and Nelson-Marlborough with Canterbury, West Coast for the estimation.
Table A6.
Reasons why likely to get the vaccine (n = 909)
| n | % | |
|---|---|---|
| All reasons why (W3, QE3a) | ||
| To stop me catching the coronavirus or getting very ill from it | 665 | 72.58 |
| To help allow my social and family life to get back to normal | 389 | 42.96 |
| To help allow my community to get back to normal | 523 | 55.99 |
| To help protect other people from catching the coronavirus | 591 | 66.12 |
| Because the vaccine won't work unless most people in New Zealand get it | 488 | 53.48 |
| Because I am a key worker working with high risk groups | 109 | 11.90 |
| Because I take the vaccines offered or recommended to me | 331 | 38.17 |
| Other (please specify) | 35 | 4.52 |
| Don't know | 11 | 1.65 |
| Prefer not to say | 4 | 0.37 |
| Number of reasons | ||
| Gave no reason | 15 | 2.02 |
| 1 reason | 243 | 25.46 |
| 2 reasons | 82 | 9.31 |
| 3 reasons | 109 | 12.20 |
| 4 or more reasons | 460 | 51.01 |
| All reasons why (W3, QE3a) | ||
| To stop me catching the coronavirus or getting very ill from it | 367 | 39.36 |
| To help allow my social and family life to get back to normal | 41 | 5.02 |
| To help allow my community to get back to normal | 85 | 8.77 |
| To help protect other people from catching the coronavirus | 154 | 16.61 |
| Because the vaccine won't work unless most people in New Zealand get it | 148 | 17.02 |
| Because I am a key worker working with high risk groups | 42 | 4.78 |
| Because I take the vaccines offered or recommended to me | 28 | 2.83 |
| Other (please specify) | 25 | 3.28 |
| Don't know | 15 | 1.94 |
| Prefer not to say | 4 | 0.37 |
Unweighted ns, weighted %s.
Table A7.
Logit regression predicting reasons why respondents likely to receive the vaccine (n = 909)
| To stop me catching the coronavirus or getting very ill from it |
To help allow my social and family life to get back to normal |
To help allow my community to get back to normal |
To help protect other people from catching the coronavirus |
Because the vaccine won't work unless most people in New Zealand get it |
Because I take the vaccines offered or recommended to me |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
Model 6 |
|||||||
| OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | |
| Age (ref: 65+ years) | ||||||||||||
| 18-24 years | 0.33 | [0.14 - 0.74] | 1.37 | [0.67 - 2.79] | 0.91 | [0.44 - 1.89] | 0.97 | [0.44 - 2.11] | 2.07+ | [0.97 - 4.43] | 0.52 | [0.25 - 1.08] |
| (0.14) | (0.50) | (0.34) | (0.38) | (0.80) | (0.19) | |||||||
| 25-34 years | 0.38 | [0.18 - 0.78] | 0.71 | [0.38 - 1.32] | 0.69 | [0.37 - 1.30] | 0.84 | [0.44 - 1.61] | 0.89 | [0.47 - 1.67] | 0.56 | [0.29 - 1.06] |
| (0.14) | (0.23) | (0.22) | (0.28) | (0.29) | (0.18) | |||||||
| 35-44 years | 0.53 | [0.26 - 1.06] | 0.73 | [0.40 - 1.32] | 0.88 | [0.49 - 1.61] | 0.79 | [0.43 - 1.46] | 0.71 | [0.39 - 1.29] | 0.30 | [0.16 - 0.56] |
| (0.19) | (0.22) | (0.27) | (0.25) | (0.22) | (0.10) | |||||||
| 45-54 years | 0.53 | [0.28 - 1.02] | 0.92 | [0.53 - 1.57] | 0.90 | [0.53 - 1.54] | 1.02 | [0.58 - 1.78] | 0.77 | [0.45 - 1.33] | 0.41 | [0.24 - 0.72] |
| (0.18) | (0.25) | (0.25) | (0.29) | (0.21) | (0.12) | |||||||
| 55-64 years | 0.67 | [0.36 - 1.23] | 0.86 | [0.52 - 1.41] | 1.08 | [0.66 - 1.77] | 0.72 | [0.44 - 1.20] | 0.89 | [0.54 - 1.45] | 0.59 | [0.36 - 0.97] |
| (0.21) | (0.22) | (0.27) | (0.19) | (0.22) | (0.15) | |||||||
| Gender (ref: male) | ||||||||||||
| Female | 1.12 | [0.80 - 1.56] | 1.28 | [0.95 - 1.72] | 1.35 | [1.00 - 1.82] | 1.64 | [1.20 - 2.23] | 0.97 | [0.72 - 1.31] | 1.49 | [1.10 - 2.02] |
| (0.19) | (0.19) | (0.20) | (0.26) | (0.15) | (0.23) | |||||||
| Ethnicity (ref: European/Pākehā) | ||||||||||||
| Māori | 0.99 | [0.60 - 1.63] | 1.25 | [0.80 - 1.97] | 1.12 | [0.72 - 1.75] | 1.12 | [0.70 - 1.80] | 0.87 | [0.56 - 1.36] | 0.83 | [0.52 - 1.33] |
| (0.25) | (0.29) | (0.26) | (0.27) | (0.20) | (0.20) | |||||||
| Pacific | 0.72 | [0.38 - 1.37] | 1.65 | [0.91 - 2.99] | 0.78 | [0.43 - 1.41] | 0.94 | [0.50 - 1.75] | 0.42 | [0.23 - 0.76] | 0.85 | [0.46 - 1.57] |
| (0.24) | (0.50) | (0.24) | (0.30) | (0.13) | (0.27) | |||||||
| Asian | 0.46 | [0.27 - 0.81] | 0.99 | [0.59 - 1.67] | 0.41 | [0.24 - 0.70] | 0.52 | [0.31 - 0.89] | 0.25 | [0.15 - 0.44] | 0.58 | [0.32 - 1.04] |
| (0.13) | (0.26) | (0.11) | (0.14) | (0.07) | (0.17) | |||||||
| Other | 0.62 | [0.34 - 1.13] | 0.82 | [0.47 - 1.43] | 0.83 | [0.47 - 1.45] | 0.46 | [0.26 - 0.81] | 0.33 | [0.19 - 0.58] | 0.45 | [0.24 - 0.86] |
| (0.19) | (0.23) | (0.24) | (0.13) | (0.10) | (0.15) | |||||||
| Nativity (ref: NZ born) | ||||||||||||
| Not born in NZ | 0.83 | [0.53 - 1.27] | 0.84 | [0.57 - 1.22] | 0.82 | [0.56 - 1.22] | 0.95 | [0.65 - 1.41] | 0.81 | [0.54 - 1.20] | 0.97 | [0.65 - 1.44] |
| (0.18) | (0.16) | (0.16) | (0.19) | (0.16) | (0.20) | |||||||
| Educational attainment (ref: undergraduate/ postgraduate degree) | ||||||||||||
| Primary/Secondary school | 0.67 | [0.43 - 1.03] | 0.60 | [0.41 - 0.89] | 0.54 | [0.37 - 0.80] | 0.57 | [0.38 - 0.85] | 0.66 | [0.45 - 0.98] | 0.87 | [0.58 - 1.30] |
| (0.15) | (0.12) | (0.11) | (0.12) | (0.13) | (0.18) | |||||||
| Diploma | 0.64 | [0.43 - 0.95] | 0.75 | [0.53 - 1.07] | 0.75 | [0.53 - 1.08] | 0.73 | [0.50 - 1.05] | 0.67 | [0.47 - 0.96] | 0.80 | [0.55 - 1.15] |
| (0.13) | (0.14) | (0.14) | (0.14) | (0.12) | (0.15) | |||||||
| Annual household income (ref: More than $150,000) | ||||||||||||
| $50,000 or less | 0.52 | [0.27 - 1.00] | 0.45 | [0.26 - 0.79] | 0.43 | [0.24 - 0.76] | 0.64 | [0.35 - 1.15] | 0.46 | [0.26 - 0.82] | 0.58 | [0.33 - 1.05] |
| (0.17) | (0.13) | (0.13) | (0.19) | (0.14) | (0.17) | |||||||
| $50,001-$70,000 | 0.70 | [0.37 - 1.32] | 0.56 | [0.33 - 0.97] | 0.64 | [0.36 - 1.11] | 0.80 | [0.45 - 1.43] | 0.49 | [0.28 - 0.85] | 0.92 | [0.53 - 1.61] |
| (0.23) | (0.16) | (0.18) | (0.24) | (0.14) | (0.26) | |||||||
| $70,001-$100,000 | 0.65 | [0.36 - 1.17] | 0.61 | [0.37 - 1.00] | 0.55 | [0.33 - 0.91] | 0.72 | [0.42 - 1.23] | 0.42 | [0.25 - 0.71] | 0.67 | [0.40 - 1.12] |
| (0.20) | (0.15) | (0.14) | (0.20) | (0.11) | (0.18) | |||||||
| $100,001-$150,000 | 0.68 | [0.38 - 1.19] | 0.51 | [0.31 - 0.83] | 0.68 | [0.41 - 1.12] | 0.65 | [0.39 - 1.08] | 0.54 | [0.33 - 0.90] | 0.74 | [0.45 - 1.22] |
| (0.20) | (0.13) | (0.17) | (0.17) | (0.14) | (0.19) | |||||||
| Family structure (ref: Two parents, dependent children) | ||||||||||||
| Single parent | 0.71 | [0.33 - 1.52] | 1.56 | [0.75 - 3.26] | 1.01 | [0.48 - 2.12] | 1.01 | [0.47 - 2.17] | 1.04 | [0.49 - 2.21] | 0.92 | [0.40 - 2.11] |
| (0.27) | (0.59) | (0.38) | (0.39) | (0.40) | (0.39) | |||||||
| Living alone | 0.93 | [0.51 - 1.70] | 0.80 | [0.45 - 1.40] | 0.86 | [0.49 - 1.49] | 0.92 | [0.52 - 1.61] | 1.00 | [0.58 - 1.75] | 0.63 | [0.35 - 1.15] |
| (0.28) | (0.23) | (0.24) | (0.26) | (0.28) | (0.19) | |||||||
| Partner, no dependent children | 1.23 | [0.79 - 1.91] | 0.94 | [0.62 - 1.41] | 0.91 | [0.60 - 1.36] | 0.97 | [0.64 - 1.47] | 0.90 | [0.59 - 1.35] | 0.98 | [0.64 - 1.51] |
| (0.28) | (0.19) | (0.19) | (0.21) | (0.19) | (0.21) | |||||||
| Other | 1.35 | [0.77 - 2.36] | 1.08 | [0.65 - 1.80] | 1.04 | [0.63 - 1.74] | 1.23 | [0.72 - 2.09] | 0.68 | [0.40 - 1.13] | 0.82 | [0.47 - 1.41] |
| (0.39) | (0.28) | (0.27) | (0.33) | (0.18) | (0.23) | |||||||
| Work status (ref: employed) | ||||||||||||
| Unemployed | 1.03 | [0.51 - 2.11] | 1.02 | [0.52 - 1.99] | 1.19 | [0.61 - 2.33] | 0.76 | [0.39 - 1.49] | 1.30 | [0.67 - 2.54] | 0.94 | [0.45 - 1.97] |
| (0.38) | (0.35) | (0.41) | (0.26) | (0.44) | (0.36) | |||||||
| Not working | 1.66 | [0.99 - 2.77] | 1.15 | [0.74 - 1.80] | 1.57 | [1.01 - 2.47] | 1.15 | [0.73 - 1.82] | 1.01 | [0.65 - 1.58] | 1.31 | [0.83 - 2.07] |
| (0.43) | (0.26) | (0.36) | (0.27) | (0.23) | (0.31) | |||||||
| Region (ref: Auckland) | ||||||||||||
| Northland | 1.16 | [0.44 - 3.06] | 0.72 | [0.33 - 1.56] | 0.65 | [0.30 - 1.41] | 1.40 | [0.59 - 3.34] | 1.44 | [0.64 - 3.22] | 0.96 | [0.43 - 2.13] |
| (0.57) | (0.28) | (0.26) | (0.62) | (0.59) | (0.39) | |||||||
| Waikato, Northern Ruapehu | 1.03 | [0.58 - 1.85] | 0.73 | [0.44 - 1.21] | 0.63 | [0.38 - 1.05] | 1.09 | [0.64 - 1.86] | 1.14 | [0.68 - 1.91] | 0.86 | [0.51 - 1.48] |
| (0.31) | (0.19) | (0.16) | (0.30) | (0.30) | (0.24) | |||||||
| Whakatane, Tauranga, Rotorua, Taupo | 0.87 | [0.41 - 1.85] | 0.96 | [0.49 - 1.89] | 0.68 | [0.35 - 1.34] | 0.82 | [0.41 - 1.64] | 0.50+ | [0.25 - 1.01] | 0.69 | [0.32 - 1.49] |
| (0.34) | (0.33) | (0.23) | (0.29) | (0.18) | (0.27) | |||||||
| Gisborne/Tairawhiti | 0.52 | [0.14 - 1.92] | 1.06 | [0.32 - 3.48] | 1.44 | [0.37 - 5.63] | 0.63 | [0.19 - 2.12] | 1.54 | [0.43 - 5.47] | 2.56 | [0.71 - 9.17] |
| (0.35) | (0.64) | (1.00) | (0.39) | (1.00) | (1.67) | |||||||
| Hawke's Bay | 0.66 | [0.28 - 1.54] | 1.32 | [0.61 - 2.85] | 0.75 | [0.34 - 1.65] | 0.99 | [0.44 - 2.21] | 0.86 | [0.39 - 1.90] | 2.04 | [0.91 - 4.55] |
| (0.29) | (0.52) | (0.30) | (0.41) | (0.35) | (0.84) | |||||||
| Taranaki | 0.95 | [0.34 - 2.64] | 0.44 | [0.16 - 1.17] | 0.44 | [0.18 - 1.08] | 0.43 | [0.18 - 1.04] | 0.88 | [0.36 - 2.16] | 1.88 | [0.77 - 4.60] |
| (0.50) | (0.22) | (0.20) | (0.19) | (0.40) | (0.86) | |||||||
| Manawatu, Whanganui, South Ruapehu | 0.83 | [0.39 - 1.75] | 0.81 | [0.41 - 1.61] | 0.52 | [0.27 - 1.04] | 0.88 | [0.43 - 1.77] | 1.10 | [0.55 - 2.18] | 1.10 | [0.55 - 2.22] |
| (0.32) | (0.28) | (0.18) | (0.31) | (0.39) | (0.39) | |||||||
| Wellington, Hutt Valley, Wairarapa | 0.88 | [0.53 - 1.47] | 0.66 | [0.42 - 1.03] | 0.68 | [0.43 - 1.07] | 0.98 | [0.61 - 1.57] | 0.89 | [0.56 - 1.41] | 1.27 | [0.79 - 2.03] |
| (0.23) | (0.15) | (0.16) | (0.24) | (0.21) | (0.30) | |||||||
| Nelson-Marlborough | 0.51 | [0.22 - 1.20] | 0.38 | [0.16 - 0.93] | 0.65 | [0.29 - 1.47] | 0.97 | [0.42 - 2.26] | 1.20 | [0.52 - 2.78] | 0.91 | [0.38 - 2.14] |
| (0.22) | (0.17) | (0.27) | (0.42) | (0.51) | (0.40) | |||||||
| Canterbury, West Coast | 1.19 | [0.72 - 1.96] | 0.68 | [0.44 - 1.05] | 0.93 | [0.60 - 1.44] | 1.11 | [0.70 - 1.75] | 1.19 | [0.77 - 1.85] | 1.64 | [1.05 - 2.57] |
| (0.30) | (0.15) | (0.21) | (0.26) | (0.27) | (0.37) | |||||||
| Otago, Southland | 0.93 | [0.47 - 1.85] | 0.54 | [0.29 - 1.03] | 0.58 | [0.31 - 1.07] | 0.99 | [0.53 - 1.88] | 0.71 | [0.38 - 1.31] | 0.73 | [0.37 - 1.43] |
| (0.33) | (0.18) | (0.18) | (0.32) | (0.22) | (0.25) | |||||||
| Constant | 10.03 | [4.23 - 23.81] | 2.27 | [1.10 - 4.67] | 4.26 | [2.03 - 8.94] | 3.61 | [1.69 - 7.70] | 5.47 | [2.58 - 11.60] | 1.47 | [0.70 - 3.09] |
| (4.42) | (0.84) | (1.61) | (1.40) | (2.10) | (0.56) | |||||||
| Pseudo R2 | .06 | .05 | .05 | .04 | .07 | .07 | ||||||
| N | 909 | 909 | 909 | 909 | 909 | 909 | ||||||
References
- 1.Schaffer DeRoo S, Pudalov N, Fu L. Planning for a COVID-19 Vaccination Program. JAMA. 2020;323:2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 2.Tugwell P, de Savigny D, Hawker G, Robinson V. Applying clinical epidemiological methods to health equity: the equity effectiveness loop. BMJ. 2006;332:358–361. doi: 10.1136/bmj.332.7537.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker M, Wilson N, Anglemyer A. Successful Elimination of Covid-19 Transmission in New Zealand. N Engl J Med. 2020;383:e56. doi: 10.1056/NEJMc2025203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.New Zealand: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data. World Health Organization, 2021. https://covid19.who.int/region/wpro/country/nz (accessed 8 May 2021).
- 5.Bloomfield A. COVID-19, 20, 21: lessons from New Zealand's 2020 response for 2021 and beyond. NZMJ. 2021;134:1175–8716. [PubMed] [Google Scholar]
- 6.Katella K. Comparing the COVID-19 vaccines: How are they different? Yale Medicine: Family Health. 2021;16 https://www.yalemedicine.org/news/covid-19-vaccine-comparison June. (accessed 21 June 2021) [Google Scholar]
- 7.Meo SA, Bukhari IA, Akram J, Meo AS, Klonoff DC. COVID-19 vaccines: comparison of biological, pharmacological characteristics and adverse effects of Pfizer/BioNTech and Moderna Vaccines. Eur Rev Med Pharmacol Sci. 2021;25:1663–1669. doi: 10.26355/eurrev_202102_24877. [DOI] [PubMed] [Google Scholar]
- 8.Abu-Raddad LJ, Chemaitelly H, Butt AA. Effectiveness of the BNT162b2 Covid-19 vaccine against the B.1.1.7 and the B.1.351 variants. N Engl J Med. 2021:1–3. doi: 10.1056/NEjMc2104974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haas EJ, Angulo FJ, McLaughlin JM. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. The Lancet. 2021;397:1819–1829. doi: 10.1016/S0140-6736(21)00947-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministry of Health NZ . Ministry of Health NZ; 2021. Our COVID-19 vaccine rollout plan. https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-vaccines/covid-19-getting-vaccine/covid-19-vaccine-rollout accessed 21 June 2021. [Google Scholar]
- 11.YouGov. COVID-19: Willingness to be vaccinated. 2021. https://yougov.co.uk/topics/international/articles-reports/2021/01/12/covid-19-willingness-be-vaccinated (accessed 21 June 2021).
- 12.Daly M, Jones A, Robinson E. Public trust and willingness to vaccinate against COVID-19 in the US from October 14, 2020, to March 29, 2021. JAMA. 2021;325:2397–2399. doi: 10.1001/jama.2021.8246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ. Sydney Health Literacy Lab COVID-19 group. Willingness to vaccinate against COVID-19 in Australia. The Lancet Infectious Diseases. 2020;21:318–319. doi: 10.1016/S1473-3099(20)30559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rhodes A, Hoq M, Measey M, Danchin M. Intention to vaccinate against COVID-19 in Australia. The Lancet Infectious Diseases. 2021;21 doi: 10.1016/S1473-3099(20)30724-6. e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crowe D. Almost one-third of adult Australians say they're unlikely to get COVID vaccination: Survey. Sydney Morning Herald. 2021 https://www.smh.com.au/politics/federal/almost-one-third-of-adult-australians-say-they-re-unlikely-to-get-covid-vaccination-survey-20210518-p57szo.html 19 May. accessed 21 June 2021. [Google Scholar]
- 16.Ministry of Health NZ . Ministry of Health NZ; 2021. At a glance: COVID-19 vaccine research insights. https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-vaccines/covid-19-vaccine-strategy-planning-insights/covid-19-vaccine-research-insights accessed 21 June 2021. [Google Scholar]
- 17.Thaker J. The persistence of vaccine hesitancy: COVID-19 vaccination intention in New Zealand. Journal of Health Communication. 2021;26:104–111. doi: 10.1080/10810730.2021.1899346. [DOI] [PubMed] [Google Scholar]
- 18.Horizon Research. covid-19 vaccine report. Ministry of Health NZ, 2020 https://www.health.govt.nz/system/files/documents/pages/horizon_research_covid-19_vaccine_report_december_2020_final.pdf (accessed 12 May 2021).
- 19.Stats NZ . Wellington: Stats NZ; 2021. Ethnic group summaries reveal New Zealand's multicultural make-up. https://www.stats.govt.nz/news/ethnic-group-summaries-reveal-new-zealands-multicultural-make-up accessed 12 May 2021. [Google Scholar]
- 20.Steyn N, Binny R, Hannah K, Hendy S, James A, Kukutai T. Estimated inequities in COVID-19 infection fatality rates by ethnicity for Aotearoa New Zealand. NZMJ. 2021;133:1175–8716. [PubMed] [Google Scholar]
- 21.Graham R, Masters-Awatere B. Experiences of Māori of Aotearoa New Zealand's public health system: a systematic review of two decades of published qualitative research. Aust NZ J Public Health. 2020;44:193–200. doi: 10.1111/1753-6405.12971. [DOI] [PubMed] [Google Scholar]
- 22.Marriott L, Sim D. Indicators of Inequality for Māori and Pacific People. The Journal of New Zealand Studies. 2015;20:24–50. doi: 10.26686/jnzs.v0i20.3876. [DOI] [Google Scholar]
- 23.Minister of Health . Wellington: Ministry of Health NZ; 2016. New Zealand Health Strategy: Future direction. https://www.health.govt.nz/system/files/documents/publications/new-zealand-health-strategy-futuredirection-2016-apr16.pdf accessed 12 May 2021. [Google Scholar]
- 24.Palmer S, Gray H, Huria T, Lacey C, Beckert L, Pitama S. Reported Māori consumer experiences of health systems and programs in qualitative research: a systematic review with meta-synthesis. International Journal for Equity in Health. 2019;18:1–12. doi: 10.1186/s12939-019-1057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marek L, Hobbs M, McCarthy J, Wiki J, Tomintz M, Campbell M. Investigating spatial variation and change (2006–2017) in childhood immunisation coverage in New Zealand. Social Science & Medicine. 2020;264:1–9. doi: 10.1016/j.socscimed.2020.113292. [DOI] [PubMed] [Google Scholar]
- 26.Whitehead J, Scott N, Atatoa Carr P, Lawrenson R. Will access to COVID-19 vaccine in Aotearoa be equitable for priority populations? The New Zealand Medical Journal. 2021;134:25–34. [PubMed] [Google Scholar]
- 27.Sharpe M. Covid-19 vaccines: DHB criticised Ministry of Health for rollout delays, warns of flourishing conspiracy theories. Stuff. 2021 https://www.stuff.co.nz/national/health/coronavirus/124684983/covid19-vaccines-dhb-criticised-ministry-of-health-for-rollout-delays-warns-of-flourishing-conspiracy-theories accessed 12 May 2021. [Google Scholar]
- 28.Ball P, Maxmen A. The epic battle against coronavirus misinformation and conspiracy theories. Nature news feature. 2020 doi: 10.1038/d41586-020-01452-z. https://www.nature.com/articles/d41586-020-01452-z accessed 21 June 2021. [DOI] [PubMed] [Google Scholar]
- 29.Islam MS, Sarkar T, Khan SH. COVID-19-related infodemic and its impact on public health: A global social media analysis. American Journal of Tropical Medicine and Hygiene. 2020;103:1621–1629. doi: 10.4269/ajtmh.20-0812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Menon V, Thaker J. Massey University; Wellington, New Zealand: 2020. Aotearoa New Zealand Public Attitudes to COVID-19 Vaccine. https://mro.massey.ac.nz/handle/10179/15567 accessed 12 May 2021. [Google Scholar]
- 31.Prickett K, Fletcher M, Chapple S, Doan N, Smith C. Victoria University of Wellington.; 2020. Life in lockdown: The economic and social effect of lockdown during Alert Level 4 in New Zealand. http://researcharchive.vuw.ac.nz/handle/10063/9022 accessed 12 May 2021. [Google Scholar]
- 32.Eysenbach G. Improving the quality of web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) Journal of Medical Internet Research. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Opinions and Lifestyle Survey QMI - Office for National Statistics. Ons.gov.uk. 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/methodologies/opinionsandlifestylesurveyqmi (accessed 12 May 2021).
- 34.University of Essex, Institute for Social and Economic Research. Understanding Society: COVID-19 Study, 2020-2021 (4th edn).2020. doi: 10.5255/UKDA-SN-8644-3 (accessed 12 May 2021).
- 35.Meredith S. Germany, France, Spain and Italy become latest countries to suspend AstraZeneca vaccine over blood clot fears. CNBC. 2021 https://www.cnbc.com/2021/03/15/covid-ireland-netherlands-suspend-astrazeneca-vaccine-amid-blood-clot-fears.html accessed 12 May 2021. [Google Scholar]
- 36.Ministry of Health NZ . Wellington: Ministry of Health NZ; 2021. National and DHB immunisation data. https://www.health.govt.nz/our-work/preventative-health-wellness/immunisation/immunisation-coverage/national-and-dhb-immunisation-data accessed 12 May 2021. [Google Scholar]
- 37.Nowlan M., Willing E., Turner N. Influences and policies that affect immunisation coverage-a summary review of literature. NZMJ. 2019;132:1175–8716. [PubMed] [Google Scholar]
- 38.Grant C, Chen M, Bandara D, Marks E, Gilchrist C, Lewycka S. Antenatal immunisation intentions of expectant parents: Relationship to immunisation timeliness during infancy. Vaccine. 2016;34:1379–1388. doi: 10.1016/j.vaccine.2016.01.048. [DOI] [PubMed] [Google Scholar]
- 39.Ellison-Loschmann L, Pearce N. Improving Access to Health Care Among New Zealand's Maori Population. Am J Public Health. 2006;96:612–617. doi: 10.2105/AJPH.2005.070680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rolleston A, Cassim S, Kidd J, Lawrenson R, Keenan R, Hokowhitu B. Seeing the unseen: evidence of kaupapa Māori health interventions. AlterNative: An International Journal of Indigenous Peoples. 2020;16:129–136. doi: 10.1177/1177180120919166. [DOI] [Google Scholar]
- 41.Rolleston A, Doughty R, Poppe K. The effect of a 12-week exercise and lifestyle management programme on cardiac risk reduction: A pilot using a kaupapa Māori philosophy. International Journal of Indigenous Health. 2017;12:116–130. doi: 10.18357/ijih121201716905. [DOI] [Google Scholar]
- 42.Pitama S, Wells J, Faatoese A, Tikao-Mason K, Robertson P, Huria T. A Kaupapa Māori approach to a community cohort study of heart disease in New Zealand. Aust NZ J Public Health. 2011;35:249–255. doi: 10.1111/j.1753-6405.2011.00702.x. [DOI] [PubMed] [Google Scholar]
- 43.Came H, O'Sullivan D, Kidd J, McCreanor T. The Waitangi Tribunal's WAI 2575 report: implications for decolonizing health systems. Health and Human Rights Journal. 2020;22:209–220. [PMC free article] [PubMed] [Google Scholar]
- 44.Ministry of Justice. Waitangi Tribunal Report 2019. Wellington: New Zealand Ministry of Justice, 2019. https://forms.justice.govt.nz/search/Documents/WT/wt_DOC_152801817/Hauora%20W.pdf (accessed 12 May 2021).
- 45.Cram F. Mahi aroha: Māori work in times of trouble and disaster as an expression of a love for the people. Kōtuitui: New Zealand Journal of Social Sciences Online. 2021 doi: 10.1080/1177083X.2021.1879181. online. [DOI] [Google Scholar]
- 46.Harris M, Williams D. Community checkpoints are an important and lawful part of NZ's Covid response. The Spinoff. 2020 https://thespinoff.co.nz/society/10-05-2020/community-checkpoints-an-important-and-lawful-part-of-nzs-covid-response/ accessed 12 May 2021. [Google Scholar]
- 47.Severinsen C, Ware F, Came H, Murray L. COVID-19 and Indigenous knowledge and leadership: (Re)centring public health curricula to address inequities. Aust NZ J Public Health. 2021;45:6–8. doi: 10.1111/1753-6405.13065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Whaitiri D. NZ Herald; 2020. Local Focus: Covid card experiment underway in Ngongotahā. https://www.nzherald.co.nz/nz/local-focus-covid-card-experiment-underway-in-ngongotaha/XBL4CSMBIQCNMIJQKNGSD6IKBY/ accessed 12 May 2021. [Google Scholar]
- 49.Murthy BP, Sterrett N, Weller D. Disparities in COVID-19 vaccination coverage between urban and rural countries—United States, December 14, 2020-April 10, 2021. Morbidity and Mortality Weekly Report. 2021;70:759–764. doi: 10.15585/mmwr.mm7020e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McCaffery KJ, Dodd RH, Cvejic E. Health literacy and disparities in COVID-19-related knowledge, attitudes, beliefs and behaviours in Australia. Public Health Res Prac. 2020;30:1–9. doi: 10.17061/phrp30342012. [DOI] [PubMed] [Google Scholar]