Abstract
Background
Coronavirus (COVID-19) forced surgical evolution worldwide. The extent to which national evidence-based recommendations, produced by the current authors early in 2020, remain valid, is unclear. To inform global surgical management and a model for rapid clinical change, this study aimed to characterize surgical evolution following COVID-19 through a multifaceted systematic review.
Methods
Rapid reviews were conducted targeting intraoperative safety, personal protective equipment and triage, alongside a conventional systematic review identifying evidence-based guidance for surgical management. Targeted searches of PubMed and Embase from 31 December 2019 were repeated weekly until 7 August 2020, and systematic searches repeated monthly until 30 June 2020. Literature was stratified using Evans’ hierarchy of evidence. Narrative data were analysed for consistency with earlier recommendations. The systematic review rated quality using the AGREE II and AMSTAR tools, was registered with PROSPERO, CRD42020205845. Meta-analysis was not conducted.
Results
From 174 targeted searches and six systematic searches, 1256 studies were identified for the rapid reviews and 21 for the conventional systematic review. Of studies within the rapid reviews, 903 (71.9 per cent) had lower-quality design, with 402 (32.0 per cent) being opinion-based. Quality of studies in the systematic review ranged from low to moderate. Consistency with recommendations made previously by the present authors was observed despite 1017 relevant subsequent publications.
Conclusion
The evidence-based recommendations produced early in 2020 remained valid despite many subsequent publications. Weaker studies predominated and few guidelines were evidence-based. Extracted clinical solutions were globally implementable. An evidence-based model for rapid clinical change is provided that may benefit surgical management during this pandemic and future times of urgency.
From 174 targeted searches and six systematic searches, 1,256 studies were identified for the rapid reviews and 21 for the conventional systematic review; of studies within the rapid reviews, 903 (71.9%) had lower-quality design, with 402 (32%) being opinion-based, quality in the systematic review ranged from low to moderate. Our April 2020 evidence-based recommendations for surgical practice during COVID-19 remained clinically valid despite 1,017 relevant subsequent publications, and extracted clinical solutions were globally implementable. An evidence-based model for rapid clinical change is provided that may benefit surgical management during the COVID-19 era and future times of urgency.
Introduction
Coronavirus (COVID-19) has challenged surgical practice worldwide1, forcing staff to adapt and departments to restructure2. Surgery on patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) produces poor outcomes3,4 making appropriate preoperative screening a necessity5. Transmission capability6 and biodistribution7 of the virus threaten the safety of operating room staff, especially those exposed to surgical smoke and aerosol-generating procedures8,9. Disruption associated with the pandemic may burden surgical systems for close to a year10, despite vaccination at population level and adaptations in management to cope with SARS-CoV-2 mutations.
Ideological differences in both operative and non-operative delivery of care existing within the global surgery community11 have increased since COVID-19. This heterogeneity was reflected in the early operative recommendations, based mainly on expert opinions, and left considerable uncertainty12,13. Past consensus collaborations with a common philosophy have improved surgical safety worldwide14,15, and there is need for similar efforts to maintain effective surgical care during the COVID-19 era16.
Evidence-based principles have previously guided surgical innovation at an international level17. In April 2020, observing the need for rapid clinical change in response to COVID-19, the authors used this philosophy to produce guidance for the urgent adaptation of surgical services on a national scale18. Targeted rapid reviews were combined with the advice of clinical experts to produce evidence-based recommendations for three aspects of practice: safety of intraoperative practice for open versus laparoscopic surgery19,20, use of personal protective equipment (PPE)21,22 and surgical triage23,24. As time has passed and the COVID-19 literature has grown25, it is unclear if these recommendations remain valid.
Although reliable models exist for clinical change in surgical management17, none achieve this in the rapid fashion required for urgent circumstances. As the COVID-19 pandemic has forced a uniquely rapid series of modifications to surgical services worldwide, understanding changes in the surgical literature since the identification of SARS-CoV-226 may benefit the development of a model for rapid evidence-based adaptations of surgical services.
To inform surgical practice during the COVID-19 era with an evidence-based model for rapid clinical change in surgical management, a multifaceted systematic review was conducted. This aimed to characterize the evolution of surgery since the identification of SARS-CoV-2, through rapid reviews targeting three aspects of surgical care (intraoperative safety19,20, PPE21,22 and surgical triage23,24) complementing a conventional systematic review of published evidence-based guidance for surgical practice during the pandemic.
Methods
The rapid data sharing that followed the COVID-19 outbreak25 prompted a multifaceted approach to systematic review1. All searches were staggered temporally to identify subtle updates to the evidence base. Both rapid review and conventional systematic review methodologies were utilized in a complementary fashion within a multifaceted approach. The same rapid review methodology used during April 202019–24,27 was implemented to characterize the evolution in the surgical literature during the pandemic. Searches targeting the three aforementioned areas of interest19–24 were repeated at approximately weekly intervals. In contrast, conventional systematic review methodology was repeated at monthly intervals to evaluate the quality and evolution of published guidance for surgery derived from a formal literature search.
No language or publication restrictions were applied. The research questions and inclusion criteria were established a priori. As some articles were published in preprint or ‘in press’ form in addition to their final publication format25, searches were date-restricted by date of database entry rather than date of publication. Duplicates were removed when identified, with the earliest record retained. Searches were supplemented by consultation of current reviews and original research relating to surgery during the COVID-19 pandemic identified through targeted searches of PubMed and Google Scholar.
Rapid reviews
Searches sought to identify studies of any design, in any setting, directly relevant to three surgical topic areas: safety of intraoperative practice (including endoscopy procedures of the gastrointestinal or respiratory tract)19,20, use of PPE21,22 and surgical triage23,24. Due to the similarity in PPE requirements for surgical and non-surgical staff, studies relevant to PPE in non-surgical settings were also sought. Six search strings were developed targeting safe intraoperative practice19,20, PPE21,22 and surgical triage23,24 in PubMed (incorporating MEDLINE) and Embase. These six searches were retrospectively conducted four times per month at approximately weekly intervals from 31 December 2019 (identification of SARS-CoV-2)26 to 7 August 2020, producing 174 searches over 29 time points across this time frame.
A single reviewer screened titles and abstracts for relevance to the three dilemmas19–24, and reviewed full texts of relevant articles to extract data using a standard extraction form. Where full texts could not be obtained, data extraction was performed using the study abstract if possible. Screening results and data extraction were regularly cross-checked by three reviewers at intervals of 7–14 days between May and August 2020. Disagreements were resolved by consensus, with one reviewer acting as arbitrator if required. Data were extracted for study design, major themes and statements that updated the surgical literature from the rapid reviews developed in April 202019–24. Extracted data from studies with design ranking above ‘poor’ for all dimensions within Evans’ hierarchy of evidence28, or those providing novel data to the surgical literature, were favoured in data synthesis. Following data extraction and thematic analysis of extracted narrative data, four reviewers inspected the authors’ initial evidence-based recommendations (developed in April 2020)19–24 for accuracy as of August 2020.
Data were synthesized in narrative and tabular formats. Outcomes of interest were: the proportion of relevant studies of weaker or stronger design according to Evans’ hierarchy of evidence28, proportion of each study design, major themes within the narrative data of the relevant studies, and consistency of narrative data in August 2020 with the April 2020 evidence-based recommendations19–24.
Conventional systematic review
Conventional systematic review was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines29. The study protocol was prospectively registered on PROSPERO (CRD42020205845). Studies were eligible for inclusion if they provided or summarized recommendations at the specialty level or more broadly for surgical practice during the COVID-19 pandemic, and outlined a search strategy in the article or abstract that identified at least one database or search term. Studies of any design, in any setting, were searched for within PubMed (incorporating MEDLINE) and Embase using the search terms (surgery* OR surgical* OR surgeon*) AND (‘COVID-19’ OR coronavirus OR ‘SARS-CoV-2’ OR ‘2019-nCoV’ OR ‘corona virus’ OR ‘COVID’). This search was repeated six times, at monthly intervals, between 31 December 2019 and 30 June 2020.
Two reviewers independently screened titles and abstracts, reviewed full texts and extracted data using a standard extraction form. Screening of titles and abstracts was facilitated through use of a web application (Rayyan, Qatar Computing Research Institute, Ar-Rayyan, Qatar)30. Disagreements were resolved by consensus, with a third reviewer acting as arbitrator if required. Data were extracted for study design, setting, surgical specialty or area, methodological quality information, major themes, and statements providing recommendations for surgical practice during COVID-19.
Data were synthesized from all included studies in both narrative and tabular formats. The search did not identify any original research eligible for inclusion, so the likelihood of publication bias could not be assessed. The primary outcome was methodological quality of the included studies, which was independently assessed by two reviewers using the Assessment of Multiple Systematic Reviews (AMSTAR) tool31 for included systematic reviews, and the Appraisal of Guidelines, Research and Evaluation (AGREE II) tool32 for all other included studies. The secondary outcome was dissemination of data within the peer-reviewed literature, which was inferred from individual numbers of citations according to targeted searches of Scopus (until 27 August 2020). For any studies unable to be identified on Scopus, numbers of citations were obtained through targeted searches of Google Scholar (until 27 August 2020). Four reviewers evaluated thematic evolution in extracted narrative data. Meta-analysis was not conducted due to heterogeneity within the included studies.
Results
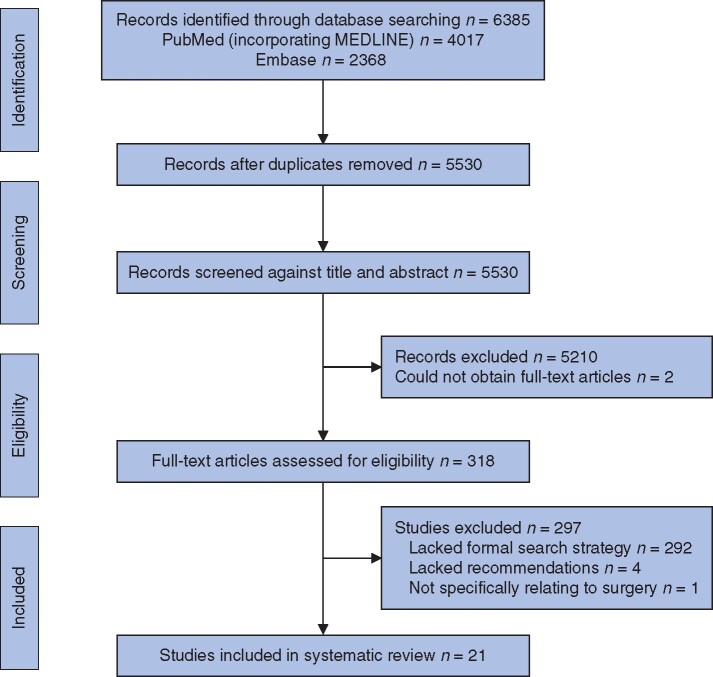
Via 174 targeted searches staggered at approximately weekly intervals over 29 time points between 31 December 2019 and 7 August 2020, a total of 5238 records (4116 unique reports) were identified, of which 1256 were included in the rapid reviews (Table S1). The six systematic searches, at six time points at monthly intervals between 31 December 2019 and 30 June 2020, identified a total of 6385 records (5530 unique reports). From this total, 318 full-text articles were retrieved, of which 21 studies were included in the systematic review (Fig. 1 and Figs S1–S6). Two full texts could not be obtained for evaluation, despite eligibility being identified on screening of title and abstract33,34.
Fig. 1.
Overall study selection for the conventional systematic review within this study
Rapid reviews
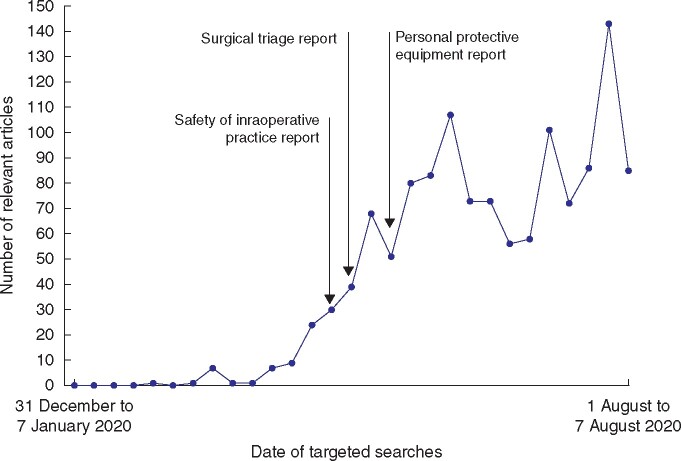
The weekly volume of studies relevant to the surgical areas of interest19–24 increased with time during the pandemic, peaking between 22 July and 31 July, when 143 studies were retrieved (Fig. 2). After the publication of the authors’ initial recommendations20,22,24, 1017 relevant articles were retrieved. Of the relevant studies within the rapid reviews, 903 (72 per cent) had a lower-quality design (Fig.S7)28, with 402 (32 per cent) being opinion-based evidence or letters (Table 1).
Fig. 2.
Weekly volume of relevant articles included in rapid reviews
Table 1.
Composition of body of evidence from 1256 records included in the rapid reviews
| Study design |
Records
(n = 1256) |
|---|---|
| Lower-quality studies* | 903 (71.9) |
| Opinion-based evidence and letters | 402 (32.0) |
| Expert consensus recommendations | 209 (16.6) |
| Narrative review or recommendations | 186 (14.8) |
| Case reports | 17 (1.4) |
| Descriptive or methodology studies | 68 (5.4) |
| Simulation studies, including cadaver or animal models | 21 (1.7) |
| Higher-quality studies† | 353 (28.1) |
| Observational studies | 43 (3.4) |
| Cross-sectional survey studies | 86 (6.8) |
| Systematic reviews | 37 (2.9) |
| Evidence-based guidance or recommendations | 48 (3.8) |
| Randomized controlled trials | 2 (0.2) |
| Prospective audits | 8 (0.6) |
| Scoping reviews | 41 (3.3) |
| Rapid reviews | 3 (0.2) |
| Retrospective data analyses | 78 (6.2) |
| Case series | 6 (0.5) |
| Case-control studies | 1 (0.1) |
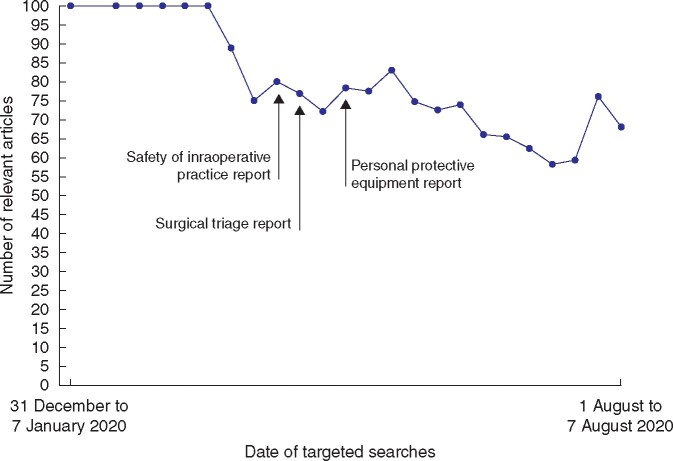
The majority of relevant studies were of lower quality throughout the 7-month time frame (median 77 (i.q.r. 71–92) per cent for searches retrieving at least one relevant study), although the proportion reduced in the latter weeks (Fig. 3). Opinion-based evidence and letters formed the largest proportion of relevant studies (median 32 (i.q.r. 18–40) per cent), predominating in all months apart from March and April (Table S2, Figs S8 and S9). Expert consensus recommendations were the most frequent study design between 1 March and 30 April (median 72 (i.q.r. 44–100) per cent for March, median 32 (i.q.r. 25–39) per cent for April), and formed a median of 16 (i.q.r. 11–28) per cent for the overall time frame (Table S2 and Fig.S10).
Fig. 3.
Weekly proportion of lower-quality evidence within the surgical literature during the COVID-19 pandemic
The first relevant study, chronologically, classified as stronger evidence was an observational study identified in the final search of March 202035. Observational studies were more prevalent later in the time frame, particularly in June 2020 (median 6 (i.q.r. 5–7) per cent), peaking in the final week of analysis with 11 per cent (Table S2 and Fig.S11). Retrospective data analyses were the most common forms of stronger evidence (median 4 (i.q.r. 0–7) per cent) (Table 1, Fig.S12). However, these were only retrieved after 15 April, peaking between 1 July and 31 July 2020 (median 8 (i.q.r. 7–11) per cent) (Table S2 and Fig.S13).
From the 174 targeted searches, 48 (4 per cent) evidence-based recommendations were retrieved (median 2 (i.q.r. 0–4) per cent), compared with 209 (17 per cent) expert consensus recommendations in the same time frame (median 16 (i.q.r. 11–28) per cent) (TablesS1 and S2). The earliest evidence-based recommendations were retrieved in the first week of April 2020. Expert consensus recommendations were retrieved at rates ranging from two to 13 times that of evidence-based recommendations between 1 April and 31 July 2020 (Figs S14 and S15).
Conventional systematic review
The conventional systematic review identified 21 studies across six continents and various surgical specialties (Table 2). Three studies (14 per cent) were retrieved in April12,36,37, nine (43 per cent) in May16,38–45 and nine (43 per cent) in June 202046–54. Regarding study type, eleven (52 per cent) were scoping reviews12,16,37,38,40,44,46,48–50,53, eight (38 per cent) systematic reviews36,39,41,42,45,47,51,54 and two (10 per cent) were narrative reviews that fulfilled the inclusion criteria43,52.
Table 2.
Characteristics of studies providing or summarizing evidence-based recommendations for surgery during COVID-19 included in systematic review
| Study (month, year) | Study design | Region | Surgical specialty or area | Methodological quality |
Number of citations* | |
|---|---|---|---|---|---|---|
| AGREE II score (%) | Average AMSTAR score (/11) | |||||
| COVIDSurg Collaborative12 (April, 2020) | Scoping review | International | Surgical care | 49 | – | 126 |
| Hirschmann et al. 36 (April, 2020) | Systematic review | International | Orthopaedic and trauma surgery | – | 3 | 21 |
| Zimmermann and Nkenke37 (April, 2020) | Scoping review | Austria | Oral and maxillofacial surgery | 32 | – | 18 |
| Boccalatte et al. 38 (May, 2020) | Scoping review | Argentina | Head and neck, and otolaryngology | 27 | – | 2 |
| De Simone et al. 39 (May, 2020) | Systematic review | International | Emergency surgery | – | 1 | 8 |
| Germano et al. 40 (May, 2020) | Scoping review | Italy | Neurosurgery | 26 | – | 3 |
| Hojaij et al. 41 (May, 2020) | Systematic review | Brazil | Surgical practice | – | 3 | 3 |
| Moletta et al. 42 (May, 2020) | Systematic review | Italy | Surgery | – | 5 | 4 |
| Puliatti et al. 43 (May, 2020) | Narrative review with database stated | International | Urology | 34 | – | 20 |
| Soreide et al. 16 (May, 2020) | Scoping review | International | Surgical services | 48 | – | 85 |
| Spock et al. 44 (May, 2020) | Scoping review | USA | Transnasal surgery | 46 | – | 0 |
| Welsh Surgical Research Initiative Collaborative45 (May, 2020) | Systematic review | UK | Operating theatre practice | – | 7·5 | 1 |
| Daigle et al.46 (June, 2020) | Scoping review | Canada | Oculofacial plastic and orbital surgery | 63 | – | 1 |
| Heldwein et al. 47 (June, 2020) | Systematic review | International | Urology | – | 5 | 0 |
| Krajewska et al. 48 (June, 2020) | Scoping review | Poland | Head and neck, and otolaryngology | 49 | – | 0 |
| Lagos et al. 49 (June, 2020) | Scoping review | Chile | Otolaryngology | 47 | – | 0** |
| Mintz et al. 50 (June, 2020) | Scoping review | International | Laparoscopy and laparotomy | 42 | – | 3 |
| Pini Prato et al. 51 (June, 2020) | Systematic review | International | Minimally invasive paediatric surgery | – | 3 | 0 |
| Shokri et al. 52 (June, 2020) | Narrative review with databases stated | USA | Facial plastic and reconstructive surgery | 37 | – | 0 |
| Viswanathan et al. 53 (June, 2020) | Scoping review | India | Spinal surgery | 34 | – | 0** |
| Wang et al. 54 (June, 2020) | Systematic review | International | Orthopaedic surgery | – | 4 | 0 |
According to Scopus as of 27 August 2020.
Unable to be identified on Scopus, thus according to Google Scholar as of 27 August 2020.
Methodological quality scores ranged from low to moderate for the 21 studies (Table 2). Of the 13 studies appraised using the AGREE II instrument12,16,37,38,40,43,44,46,48–50,52,53, only one (score 63 per cent)46 scored over 50 per cent. Scores of the other 12 studies ranged from 26–49 per cent. Seven (88 per cent) of the included systematic reviews36,39,41,42,47,51,54 received average AMSTAR scores below 6 (range 1–5), indicating poor methodological quality. Only one systematic review54 received an average AMSTAR score above 6 (7.5), indicating good methodological quality.
Numbers of citations for the 21 studies ranged from 044,47–49,51–54 to 12612 (median 2 (i.q.r. 0–8). However, there were quantitative discrepancies when each month was grouped, with earlier evidence-based recommendations cited more often. For studies retrieved in April 202012,36,37, the median number of citations was 21 (i.q.r. 20–74), compared with 3 (i.q.r. 2–8) for May16,38–45 and 0 (i.q.r. 0–0) for June46–54.
Consistency of surgical literature
Ongoing monitoring of narrative data between 31 December 2019 and 7 August 2020 identified no substantive thematic changes over time (Table S3). Despite substantial heterogeneity in study design, narrative data relevant to the three aspects of surgical care19–24 consistently concurred with the authors’ recommendations, apart from a small number of low-quality studies recommending an open approach over the laparoscopic alternative to minimize the risk of SARS-CoV-2 transmission to operating room staff55. As the pandemic progressed, thematic consistency was observed in all areas despite 1017 relevant publications. After accounting for inherent differences in specialty, there was no significant narrative contradiction in the evidence-based recommendations within the conventional systematic review.
Following consideration of the total body of surgical literature published between 31 December 2019 and 7 August 2020, inspection of the initial evidence-based recommendations made in the authors’ three rapid reviews (developed in April 2020)19,21,23 revealed no strong evidence subsequently published (as of 7 August 2020) to justify significant change in any recommendation (Table S4).
Discussion
This study has provided a comprehensive characterization of the surgical literature and its temporal evolution during the COVID-19 pandemic. Lower-quality studies predominated, with opinion-based articles and letters the most common communications. Quality did not improve over time despite the increasing number of relevant publications. Clinical recommendations were mostly based on expert consensus, opinion or narrative review. There was a dearth of evidence-based guidance, which ranged from low to moderate methodological quality and for which numbers of citations reflected month of database entry. Evidence-based recommendations developed by the present authors in April 2020 remained clinically valid as of 7 August 2020 despite the large number of relevant publications during this intervening period. Although relevant studies of strong design have been published after the final search was completed56, these data have generally concurred with the present study. The initial evidence-based recommendations from April 2020 remain valid.
Declaration of the COVID-19 pandemic57 was followed by the proliferation of a large volume of related literature, demonstrating unprecedented responsiveness by peer-reviewed medical journals25. However, this did not result in corresponding benefit for clinical practice. Most studies were found to be of lower-quality design, and 4 months of further literature did not highlight significant modification to the present authors’ early-stage, evidence-based recommendations13.
Rapid reviews with clearly specified research questions can produce similar clinical conclusions to systematic reviews, albeit with lower certainty27. The authors’ April 2020 rapid reviews targeting specific clinical dilemmas18 provided reliable and timely evidence-based solutions19–24.
The quality of surgical literature has been a topic of past controversy58. Although improved through consensus efforts valuing evidence-based principles17, the present study reveals that COVID-19 may have caused this issue to resurface. The predominance of expert opinion suggests that the global surgery community may have reverted to traditional eminence-based medicine59. Deviating from objective data risks differing clinical approaches being advised, potentially compromising safety60. Increasing ideological heterogeneity could confound attempts to achieve collective goals for global surgery11. A continued increase in global caseload61 implies a substantial challenge may be created for the future.
The present study addressed multiple challenges for surgery during the pandemic1 identifying clinical solutions that are relatively inexpensive and implementable on a global scale. Surgery on patients infected with SARS-CoV-2 may cause postoperative morbidity and mortality3,4, and this should be understood for preoperative risk–benefit assessment. Adequate delay after infection should be allowed to ensure safety for patients undergoing elective procedures62,63. Operations on COVID-19 patients should ideally occur in designated theatres with negative-pressure ventilation12, and suspected COVID-19 patients should wear a surgical mask during perioperative theatre transport21. Appropriate preoperative screening for active SARS-CoV-2 infection using patient history and reverse transcription-polymerase chain reaction is essential5. Triage should consider local COVID-19 prevalence and hospital resources23, and methods of ensuring a safe resumption of elective surgery despite high prevalence have been described64. Although caution was advised for laparoscopic surgery throughout the pandemic, the present study found no evidence that laparoscopy presented a greater risk to theatre staff than open surgery with respect to SARS-CoV-2 transmission. However, given theoretical aerosol transmission risk, capture devices should be used with energy sources producing surgical smoke8 and desufflation of pneumoperitoneum should be performed using a suction irrigator system attached to a high-efficiency particulate air filter19. Given evidence of multisystem biodistribution7, all biological material should be treated as a potential SARS-CoV-2 source. PPE with aerosol precautions (N95 respirator or equivalent)65 can provide adequate protection against SARS-CoV-266, and is essential during surgical emergencies, aerosol-generating procedures or when a patient is not confirmed to be COVID-19 negative21.
The present study included the use of temporally staggered searches to capture subtle updates in a rapidly evolving evidence base potentially missed by searches at a single time point. Synthesis of a large amount of narrative data provided inexpensive potential clinical solutions. To increase worldwide applicability and reduce the risk of bias, searches were not limited by language67 and globally accepted methods were used for classifying strength of evidence28, reporting methodology29 and risk of bias assessment31,32. Despite these strengths, this study has limitations. The most significant of which was potential bias accompanying the selection of relevant studies for the rapid reviews. The rapid reviews targeted key dilemmas for pandemic surgery19–24. In spite of ensuring clinical relevance, this may have limited scope. The paucity of strong evidence in the reviews prompted caution regarding statistical bias within included studies. Heterogeneity in study design prevented meta-analysis, requiring data synthesis in multiple formats for maximal clinical utility and acknowledgement of likely biases.
Characterization of temporal changes in the surgical literature through a multifaceted systematic review confirmed correctness of an evidence-based approach tailored to surgical management during the COVID-19 pandemic. Synthesis of these results will provide surgical staff with an enhanced understanding of the trustworthiness and dissemination of the recommendations within the provided studies, that will allow them to decide whether they should adopt the recommendations for clinical care of surgical patients at their local healthcare institutions. Combination of findings from this study with the authors’ experience during the COVID-19 pandemic provides an evidence-based model for rapid clinical change in surgical management (Table 3).
Table 3.
Evidence-based model for rapid clinical change in surgical management based on data and experience during the COVID-19 pandemic
| Time | State of literature | Required action |
|---|---|---|
| – | Predominantly reports of similar past phenomena, almost no articles directly relevant to current phenomenon | Acknowledgement of need for rapid clinical change in surgical management |
| 0–2 weeks | Predominantly reports of similar past phenomena, literature relevant to current phenomenon begins to be populated by opinion-based evidence | Working group comprising researchers with literature review experience and clinical experts urgently convened; scoping searches of prior literature regarding similar past phenomena and initial evidence relevant to current phenomenon |
| ∼2 weeks | Small evidence base relevant to current phenomenon predominated by opinion-based articles | Clinical experts assess suitability of prior literature regarding similar past phenomena for contributing to recommendations for current phenomenon, and draft initial guidance based on findings from scoping searches that is not disseminated |
| ∼2–3 weeks | Rapid growth predominated by opinion-based evidence, initial studies of stronger design begin to be published | Rapid reviews targeting clinical dilemmas specific to the current phenomenon. Aim to identify relevant literature and gaps in understanding of current phenomenon |
| ∼3 weeks | Predominantly opinion-based evidence, very few studies of stronger design | Clinical experts develop evidence-based guidance based on findings of rapid reviews targeting clinical dilemmas specific to the current phenomenon |
| 3–4 weeks | Predominantly opinion-based evidence, few studies of stronger design | Reports of rapid reviews containing evidence-based guidance refined within working group |
| ∼4 weeks | Predominantly opinion-based evidence, few studies of stronger design | Reports begin to be rapidly circulated in non-refereed format to surgical staff on a large scale through relevant surgical societies |
| ∼4 weeks–4 months | Rapid growth predominated by opinion-based evidence, however proportion of studies of stronger design increases with time | Rapid review methodology targeting clinical dilemmas repeated weekly; non-refereed reports and evidence-based guidance updated based on findings from regular rapid reviews; reports published in peer-reviewed setting |
| ∼1 year | Unknown | Rapid review methodology targeting clinical dilemmas specific to current phenomenon conducted to confirm clinical validity of evidence-based guidance |
The authors hope that these findings provide a crucial lesson for global surgery. Widespread adoption of evidence-based methodology targeting specific clinical dilemmas may facilitate the reorganization of surgical systems in a reliable and unified fashion. This model may be valuable for coordinating surgical responses during the COVID-19 era and future times of urgent need.
Supplementary Material
Acknowledgements
There was no funding source for this study. The authors thank the members of the Royal Australasian College of Surgeons (RACS) Clinical Expert COVID-19 Working Group (Trevor Collinson, Prof Peter Hewett, Prof Thomas Hugh, Prof Robert Padbury, Prof Mark Frydenberg, Prof Richard Douglas and Jen Kok), the RACS Evidence Synthesis Team combining the Australian Safety and Efficacy Register of New Interventional Procedures-Surgical (ASERNIP-S) and Research, Audit and Academic Surgery (Penny Williamson, Lorwai Tan, Kristin Weidenbach, Helena Kopunic, Ning Ma, Magdalena Moshi, Danielle Stringer, Joanna Duncan and Nathan Procter), and Vanessa Beavis (representing the Australian and New Zealand College of Anaesthetists), Chloe Ayres (representing the Royal Australian and New Zealand College of Obstetricians and Gynaecologists), Vicky Lu (representing the Royal Australian and New Zealand College of Ophthalmologists), James Churchill (representing the Royal Australasian College of Surgeons Trainees’ Association) and Shane Kelly (representing St John of God Healthcare), who contributed to the development of our initial rapid reviews. The authors owe further thanks to Kristin Weidenbach, Academic Editorial Manager of the RACS, for copyediting the final version of this report.
Disclosure. The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS Open online.
References
- 1. Kibbe MR. Surgery and COVID-19. JAMA 2020;324:1151–1152 [DOI] [PubMed] [Google Scholar]
- 2. Zarzaur BL, Stahl CC, Greenberg JA, Savage SA, Minter RM.. Blueprint for restructuring a department of surgery in concert with the health care system during a pandemic: The University of Wisconsin Experience. JAMA Surg 2020;155:628–635 [DOI] [PubMed] [Google Scholar]
- 3. COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020;396:27–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Doglietto F, Vezzoli M, Gheza F, Lussardi GL, Domenicucci M, Vecchiarelli L. et al. Factors associated with surgical mortality and complications among patients with and without Coronavirus Disease 2019 (COVID-19) in Italy. JAMA Surg 2020;155:691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kovoor JG, Tivey DR, Williamson P, Tan L, Kopunic HS, Babidge WJ. et al. Screening and testing for COVID-19 before surgery. ANZ J Surg 2020;90:1845–1856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN. et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382:1564–1567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang W, Xu Y, Gao R, Lu R, Han K, Wu G. et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020;323:1843–1844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mowbray NG, Ansell J, Horwood J, Cornish J, Rizkallah P, Parker A. et al. Safe management of surgical smoke in the age of COVID-19. Br J Surg 2020;107:1406–1413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Livingston EH. Surgery in a time of uncertainty: a need for universal respiratory precautions in the operating room. JAMA 2020;323:2254–2255 [DOI] [PubMed] [Google Scholar]
- 10. COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020;107:1440–1449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shawar YR, Shiffman J, Spiegel DA.. Generation of political priority for global surgery: a qualitative policy analysis. Lancet Glob Health 2015;3:e487–e495 [DOI] [PubMed] [Google Scholar]
- 12. COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020;107:1097–1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kovoor JG, Tivey DR, Babidge WJ, Maddern GJ.. COVID-19: a test of evidence-based surgery. Br J Surg 2020; DOI: 10.1093/bjs/znaa027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP. et al. ; Safe Surgery Saves Lives Study Group. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009;360:491–499 [DOI] [PubMed] [Google Scholar]
- 15. Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA. et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015;386:569–624 [DOI] [PubMed] [Google Scholar]
- 16. Soreide K, Hallet J, Matthews JB, Schnitzbauer AA, Line PD, Lai PBS. et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg 2020;107:1250–1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, Nicholl J. et al. ; Balliol Collaboration. No surgical innovation without evaluation: the IDEAL recommendations. Lancet 2009;374:1105–1112 [DOI] [PubMed] [Google Scholar]
- 18. Maddern GJ. Evidence, not eminence, in coronavirus disease 2019. ANZ J Surg 2020;90:1537. [DOI] [PubMed] [Google Scholar]
- 19. Tivey DR, Davis SS, Kovoor JG, Babidge WJ, Tan L, Hugh TJ. et al. Safe surgery during the coronavirus disease 2019 crisis . ANZ J Surg 2020;90:1553–1557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Royal Australasian College of Surgeons. Guidelines for Safe Surgery: Open versus Laparoscopic. https://www.surgeons.org/-/media/Project/RACS/surgeons-org/files/news/covid19-information-hub/2020-04-15-recommendations-on-safe-surgery-laparoscopic-vs-open.pdf?rev=be7927abd03a4a9e976ba944c7c4279a&hash=4E3579010C47C9324C1DB8F8E82F89CD (accessed 26 September 2020)
- 21. Tan L, Kovoor JG, Williamson P, Tivey DR, Babidge WJ, Collinson TG. et al. Personal protective equipment and evidence-based advice for surgical departments during COVID-19. ANZ J Surg 2020;90:1566–1572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Royal Australasian College of Surgeons. Guidelines for Personal Protective Equipment. https://www.surgeons.org/-/media/Project/RACS/surgeons-org/files/news/covid19-information-hub/2020-05-05-covid19-ppe-guidelines.pdf?rev=3a25d9e9f4c444ac8c398b7d7cc7f00a&hash=05156A2797FB43C4AE4F94354C94528B (accessed 26 September 2020)
- 23. Babidge WJ, Tivey DR, Kovoor JG, Weidenbach K, Collinson TG, Hewett PJ. et al. Surgery triage during the COVID-19 pandemic. ANZ J Surg 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Royal Australasian College of Surgeons. Surgery Triage: Responding to the COVID-19 Pandemic. https://www.surgeons.org/-/media/Project/RACS/surgeons-org/files/news/covid19-information-hub/2020-04-22_racs-triage-of-surgery-web.pdf?rev=c28712668d7f45f19ca9df53b77011ea&hash=82A77A9AD9B8A5E23807E449386B80E1 (accessed 26 September 2020)
- 25. Glasziou PP, Sanders S, Hoffmann T.. Waste in covid-19 research. BMJ 2020;369:m1847. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Pneumonia of Unknown Cause – China. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ (accessed 28 July 2020)
- 27. Watt A, Cameron A, Sturm L, Lathlean T, Babidge W, Blamey S. et al. Rapid versus full systematic reviews: validity in clinical practice? ANZ J Surg 2008;78:1037–1040 [DOI] [PubMed] [Google Scholar]
- 28. Evans D. Hierarchy of evidence: a framework for ranking evidence evaluating healthcare interventions. J Clin Nurs 2003;12:77–84 [DOI] [PubMed] [Google Scholar]
- 29. Moher D, Liberati A, Tetzlaff J, Altman DG;. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A.. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C. et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G. et al. ; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ 2010;182:E839–842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Carracedo D, Alcaraz A, Allona A, Gutierrez JL, Lopez-Fando L, Medina RA. et al. Robotic and laparosocpic urological surgery during COVID-19 pandemia. Arch Esp Urol 2020;73:463–470 [PubMed] [Google Scholar]
- 34. Puche-Sanz I, Sabio-Bonilla A, Sanchez-Conde V, Jimenez-Dominguez AC, Tamayo-Gomez A, Vila-Brana P. et al. [Emergency surgery during COVID-19 pandemia]. Arch Esp Urol 2020;73:353–359 [PubMed] [Google Scholar]
- 35. Ong SWX, Tan YK, Sutjipto S, Chia PY, Young BE, Gum M. et al. Absence of contamination of personal protective equipment (PPE) by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Infect Control Hosp Epidemiol 2020;41:614–616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hirschmann MT, Hart A, Henckel J, Sadoghi P, Seil R, Mouton C.. COVID-19 coronavirus: recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports Traumatol Arthrosc 2020;28:1690–1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zimmermann M, Nkenke E.. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J Craniomaxillofac Surg 2020;48:521–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Boccalatte LA, Larranaga JJ, Perez Raffo GM, Teijido CA, Garcia FG, Staneloni MI. et al. Brief guideline for the prevention of COVID-19 infection in head and neck and otolaryngology surgeons. Am J Otolaryngol 2020;41:102484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. De Simone B, Chouillard E, Di Saverio S, Pagani L, Sartelli M, Biffl WL. et al. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann R Coll Surg Engl 2020;102:323–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Germano A, Raffa G, Angileri FF, Cardali SM, Tomasello F.. Coronavirus disease 2019 (COVID-19) and neurosurgery: literature and neurosurgical societies recommendations update. World Neurosurg 2020;139:e812–e817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hojaij FC, Chinelatto LA, Boog GHP, Kasmirski JA, Lopes JVZ, Sacramento FM.. Surgical practice in the current COVID-19 pandemic: a rapid systematic review. Clinics (Sao Paulo )2020;75:e1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Moletta L, Pierobon ES, Capovilla G, Costantini M, Salvador R, Merigliano S. et al. International guidelines and recommendations for surgery during Covid-19 pandemic: a systematic review. Int J Surg 2020;79:180–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Puliatti S, Eissa A, Eissa R, Amato M, Mazzone E, Dell'Oglio P. et al. COVID-19 and urology: a comprehensive review of the literature. BJU Int 2020;125:E7–E14 [DOI] [PubMed] [Google Scholar]
- 44. Spock T, Kessler R, Lerner D, Filip P, Del Signore A, Colley P. et al. Endoscopic skull base surgery protocol from the frontlines: transnasal surgery during the COVID-19 pandemic. Otolaryngol Head Neck Surg 2020;163:482–490 [DOI] [PubMed] [Google Scholar]
- 45. Welsh Surgical Research Initiative Collaborative. Recommended operating room practice during the COVID-19 pandemic: systematic review. BJS Open 2020;4:748–756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Daigle P, Leung V, Yin V, Kalin-Hajdu E, Nijhawan N.. Personal protective equipment (PPE) during the COVID-19 pandemic for oculofacial plastic and orbital surgery. Orbit 2020; DOI: 10.1080/01676830.2020.1781200 [DOI] [PubMed] [Google Scholar]
- 47. Heldwein FL, Loeb S, Wroclawski ML, Sridhar AN, Carneiro A, Lima FS. et al. A systematic review on guidelines and recommendations for urology standard of care during the COVID-19 pandemic. Eur Urol Focus 2020;6:1070–1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Krajewska (Wojciechowska J, Krajewski W, Zub K, Zatoński T.. Review of practical recommendations for otolaryngologists and head and neck surgeons during the COVID-19 pandemic. Auris Nasus Larynx 2020;47:544–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lagos AE, Ramos PH, Andrade T.. Protection for otolaryngologic surgery in the COVID-19 pandemic. OTO Open 2020;4:2473974X20934734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Mintz Y, Arezzo A, Boni L, Baldari L, Cassinotti E, Brodie R. et al. The risk of COVID-19 transmission by laparoscopic smoke may be lower than for laparotomy: a narrative review. Surg Endosc 2020;34:3298–3305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pini Prato A, Conforti A, Almstrom M, Van Gemert W, Scuderi MG, Khen-Dunlop N. et al. Management of COVID-19-positive pediatric patients undergoing minimally invasive surgical procedures: systematic review and recommendations of the Board of European Society of Pediatric Endoscopic Surgeons. Front Pediatr 2020;8: 259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Shokri T, Saadi RA, Liaw J, Bann DV, Patel VA, Goyal N. et al. Facial plastic and reconstructive surgery during the COVID-19 pandemic: implications in craniomaxillofacial trauma and head and neck reconstruction. Ann Plast Surg 2020;85:S166–S170 [DOI] [PubMed] [Google Scholar]
- 53. Viswanathan VK, Subramanian S, Rao AK.. Principles for managing patients with spinal ailments in the coronavirus disease 2019 era: what do we know so far? An evidence-based, narrative review. Asian Spine J 2020;14:572–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wang Y, Zeng L, Yao S, Zhu F, Liu C, Di Laura A. et al. Recommendations of protective measures for orthopedic surgeons during COVID-19 pandemic. Knee Surg Sports Traumatol Arthrosc 2020;28:2027–2035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Angelos G, Dockter AG, Gachabayov M, Latifi R, Bergamaschi R.. Emergency colorectal surgery in a COVID-19 pandemic epicenter. Surg Technol Int 2020;36:18–21 [PubMed] [Google Scholar]
- 56. Puylaert CAJ, Scheijmans JCG, Borgstein ABJ, Andeweg CS, Bartels-Rutten A, Beets GL. et al. Yield of screening for COVID-19 in asymptomatic patients prior to elective or emergency surgery using chest CT and RT-PCR (SCOUT): Multicenter Study. Ann Surg 2020;272:919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.World Health Organization. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed 3 September 2020 )
- 58. Horton R. Surgical research or comic opera: questions, but few answers. Lancet 1996;347:984–985 [DOI] [PubMed] [Google Scholar]
- 59. Ergina PL, Cook JA, Blazeby JM, Boutron I, Clavien PA, Reeves BC. et al. ; Balliol Collaboration. Challenges in evaluating surgical innovation. Lancet 2009;374:1097–1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Barkun JS, Aronson JK, Feldman LS, Maddern GJ, Strasberg SM, Balliol C, et al. ; Balliol Collaboration. Evaluation and stages of surgical innovations. Lancet 2009;374:1089–1096 [DOI] [PubMed] [Google Scholar]
- 61. Dong E, Du H, Gardner L.. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kovoor JG, Scott NA, Tivey DR, Babidge WJ, Scott DA, Beavis VS. et al. Proposed delay for safe surgery after COVID-19. ANZ J Surg 2021;91:495–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. COVIDSurg Collaborative, GlobalSurg Collaborative.. Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia 2021;76:748–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gammeri E, Cillo GM, Sunthareswaran R, Magro T.. Is a ‘COVID-19-free’ hospital the answer to resuming elective surgery during the current pandemic? Results from the first available prospective study. Surgery 2020;168:572–577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schunemann HJ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020;395:1973–1987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Liu M, Cheng SZ, Xu KW, Yang Y, Zhu QT, Zhang H. et al. Use of personal protective equipment against coronavirus disease 2019 by healthcare professionals in Wuhan, China: cross-sectional study. BMJ 2020;369:m2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Juni P, Holenstein F, Sterne J, Bartlett C, Egger M.. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol 2002;31:115–123 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.