Abstract
Background Coronary heart disease has multiple risk factors, including air pollution. Numerous pathophysiological mechanisms have been identified with increasing levels of air pollution, mainly with ozone (O3), nitrogen dioxide (NO2), sulphur dioxide (SO2), particulate matter (PM10), fine particulate matter (PM2.5) and carbon monoxide (CO). In Mexico, the pollution level is reported using an air quality index called IMECA. Methods All patients with STEMI admitted at Hospital Español were collected between 2012 and 2019 (N = 348). We conducted a retrospective analysis using the air pollution exposure at the time of each event (lag0), the previous 24 h (lag1), 48 h (lag2), 72 h (lag3) and 5-day cumulative lag. The level of air pollution was analyzed independently using IMECA and particle concentrations. The data was divided in two groups: days with one of more STEMI’s (MI group) and days free of events (Control group), using ANCOVA to evaluate the difference between means of both groups taking into account confounders. Results: For days with one or more cardiovascular event, a significant increase in SO2 was observed at lag1; similar increase was found in CO, PM2.5, SO2 at lag2. For the 5-day cumulative lag, SO2 and PM2.5 showed a significant increase. No differences were found using the IMECA levels in both groups. Conclusions: The elevated concentrations levels of CO, SO2 and PM2.5 showed significant association with STEMI at different time points before the event. Ozone, PM10 and NO2 showed no difference between groups. IMECA levels showed no association with STEMI in our study.
Keywords: ST elevation myocardial infarction, Air pollution
1. Introduction
Air pollution has been a recognized risk factor for cardiovascular disease in short- and long-term exposure. The particles known to be involved are particulate matter (PM), ozone (O3), carbon monoxide (CO), sulfur dioxide (SO2) and nitrogen dioxide (NO2). The particulate matter includes PM10 (inhalable particles with diameters that are 10 µm and smaller) and PM2.5 (fine inhalable particles, with diameters that are generally 2.5 µm and smaller).
Different pathophysiologic mechanisms have been recognized in multiple studies through the years. The activation of the inflammatory cascade has been proposed as one of the main culprits. Increased interleukin 1 beta, interleukin 6 and tumor necrosis factor alpha levels have been documented [1]. Peters et al demonstrated in 2001 a linear increase in C-reactive protein values with total air particles [2]. This proinflammatory effect is linked with a hypercoagulable state. Seaton proposed that the ultra-fine particles in air pollution cause alveolar inflammation, initiating changes in blood coagulation and promoting secretion of cytokynes that may induce a respiratory event in susceptible patients [3]. Healthy individuals exposed to diesel exhaust inhalations increase thrombus formation and platelet activation [4]. Changes in the cardiac autonomic function during higher air pollution levels are also well documented, through ambulatory electrocardiographic monitoring, demonstrating an increased mean heart rate and a decreased heart rate variability [5].
In Mexico, as many other countries in the world, the air pollution levels are reported using an air quality index, called IMECA (Índice Mexicano de Calidad del Aire). This index was built using the Pollutant Standard Index (PSI) from the United States of America, and to date, they share many similarities. The IMECA measures 6 particles (CO, SO2, O3, NO2, PM10 and PM2.5), transforming the concentration values to a score system [6]. The value is published each hour for the population of Mexico City, and is determined from the particle that scores the highest during that hour, obtaining a single digit that represents the air quality. According to that score, air quality can be classified as good (score from 0 to 50 points), regular (51–100 points), bad (101–150 points), very bad (151–200 points) and extremely bad (greater than201 points). Each grade is associated with a different color, so the general population can understand easily each stage, and act appropriately [7].
Some studies have tried to associate acute air pollution fluctuations with cardiovascular events. The results have been scarce and somewhat controversial. Nonetheless, evidence keeps growing towards a link between the two.
Ruidavets et al found in 635 patients, an increase in relative risk for myocardial infarction for O3 concentrations measured on the day of the event (lag0) and the previous day (lag1) [8]. Two years later, a study in Utah with 12,865 patients, revealed an increase in relative risk of 4.5% for every 10 ug/m3 increase in PM2.5. The association was made with the concentrations at lag0 [9]. The RISCAT study in Tuscany found a similar result analyzing PM10, NO2 and CO during lag0 [10].
More recent studies have focused in ST elevation myocardial infarction (STEMI). A study in Belgium with 11,428 patients, noticed an increase of 2.6%, 2.8% and 5.1% in relative risk for STEMI for every 10 ug/m3 increase in PM10, PM2.5 and NO2 respectively [11].
Not all studies have found positive results. One of the most important, the CARDIO-ARSIF trial published in 2015 included 11,978 patients with STEMI, and analyzed the concentrations of all 6 mayor particles during lag0 and lag1. No significant association was found [12].
To our knowledge, there are no studies comparing the incidence of STEMI with the IMECA levels. Our research group was trying to find out if the IMECA correlates with cardiovascular events the same way as the concentration levels, and if these levels show the same pattern as previous studies.
The main objective of our study was to find out if an increase in the reported concentration levels was associated with a similar increase in the incidence of STEMI. We analyzed the concentrations levels of each particle during lag0, lag1, lag 2, lag3 and a cumulative five-day lag, and compared it to the number of cases of STEMI in our hospital.
As a secondary objective, we analyzed if the reported IMECA levels showed a similar association with the incidence of STEMI.
2. Methods
We designed a retrospective, observational study, including all patients admitted at Hospital Español in Mexico City with the diagnosis of ST elevation myocardial infarction, from January 2012 to April 2019. All patients were required to have coronary angiography to confirm the diagnosis. Patients without obstructive coronary disease were excluded from our study. If the symptoms started more than 24 h before admission, the patient was also excluded.
The air pollution levels were extracted from the official site www.aire.cdmx.gob.mx. We collected the data for each day from 2012 to 2019, for all 6 particles analyzed in the air quality index (SO2 ppm, NO2 ppm, CO ppm, O3 ppm, PM2.5 µg/m3 and PM10 µg/m3). We also collected the IMECA score for each day. The meteorological data was extracted from www.meteored.mx. We chose temperature and atmospheric pressure as the main confounders because of previous evidence of the relation between these variables and the rate of STEMI [13].
Before starting the database of our study, the protocol was submitted to the research committee. All the information collected was only used for the purpose for which it was requested.
The statistical analysis was made using the software SPSS 25th edition. All data was divided in two groups: days that had 1 or more cardiovascular event (STEMI group), and the days without any event (no STEMI group). The days that had no cardiovascular events were used as a control group. In both groups all 6 particles and the IMECA levels were independently analyzed during lag0, lag1, lag2, lag3 and a cumulative 5-day lag (The 0–3 days lag indicates the 24-hours averages of the pollutants the day of the event, 1 day before, 2 days before and 3 days before the event; the cumulative lag is the average of the pollutants levels through the 5 days prior to the event). The means with the respective standard deviation were calculated. All variables were tested for normal distribution with the Kolmogorov-Smirnov test. All data were normally distributed. We analyzed the difference in means between two independent groups taking into account the possible effect of confounders (temperature and atmospheric pressure) using ANCOVA test, with a two-tailed distribution. A p-value ≤ 0.05 was considered significant (95% confidence interval).
3. Results
We analyzed a total of 2667 days, between January 2012 and April 30th 2019, in which we had 348 STEMI cases fulfilling our inclusion criteria. The average age of our population was 64.9 ± 13.5 years, 79% were male (275 patients) and 21% were female (73 patients). 28% of our patients had diabetes, 52% had arterial hypertension, 22% dyslipidemia, and 57% were previous smokers.
In the comparison of days using the concentration levels of each particle, the results showed no significant difference for CO during exposure at lag0, as shown in Table 1.
Table 1.
Results at different exposure times.
| PARTICLE | No STEMI (n = 2351) | STEMI (n = 348) | P* | |
|---|---|---|---|---|
|
CO |
Lag0 | 0.6540 ± 0.232 ppm | 0.6810 ± 0.227 ppm | 0.489 |
| Lag1 | 0.652 ± 0.23 ppm | 0.690 ± 0.237 ppm | 0.128 | |
| Lag2 | 0.652 ± 0.231 ppm | 0.696 ± 0.239 ppm | 0.009 | |
| Lag3 | 0.652 ± 0.231 ppm | 0.690 ± 0.232 ppm | 0.067 | |
| Cumulative lag | 0.653 ± 0.198 ppm | 0.688 ± 0.189 ppm | 0.064 | |
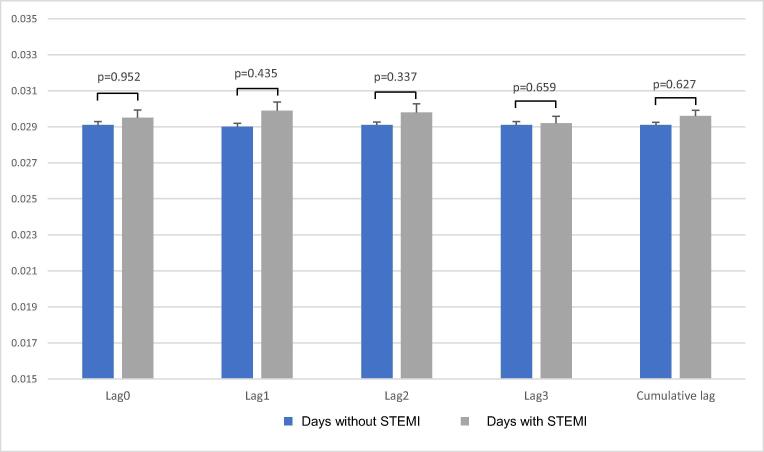
| NO2 | Lag0 | 0.0291 ± 0.009 ppm | 0.0295 ± 0.008 ppm | 0.952 |
| Lag1 | 0.0290 ± 0.009 ppm | 0.0299 ± 0.009 ppm | 0.435 | |
| Lag2 | 0.0291 ± 0.008 ppm | 0.0298 ± 0.009 ppm | 0.337 | |
| Lag3 | 0.0291 ± 0.009 ppm | 0.0292 ± 0.007 ppm | 0.659 | |
| Cumulative lag | 0.0291 ± 0.007 ppm | 0.0296 ± 0.006 ppm | 0.627 | |
| O3 | Lag0 | 0.0595 ± 0.019 ppm | 0.057 ± 0.0195 ppm | 0.676 |
| Lag1 | 0.0595 ± 0.019 ppm | 0.0576 ± 0.020 ppm | 0.738 | |
| Lag2 | 0.0595 ± 0.019 ppm | 0.0575 ± 0.0190 ppm | 0.323 | |
| Lag3 | 0.0593 ± 0.019 ppm | 0.0588 ± 0.020 ppm | 0.583 | |
| Cumulative lag | 0.0595 ± 0.016 ppm | 0.0580 ± 0.0169 ppm | 0.78 | |
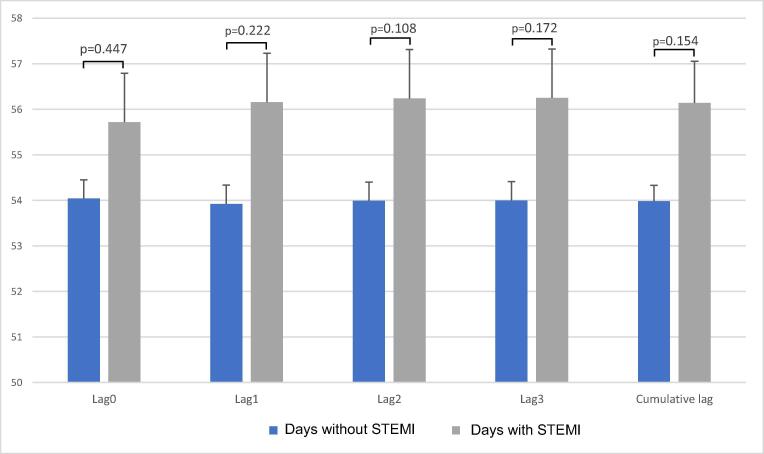
| PM10 | Lag0 | 54.04 ± 20.66 µg/m3 | 55.716 ± 21.15 µg/m3 | 0.447 |
| Lag1 | 53.92 ± 20.57 µg/m3 | 56.156 ± 21.62 µg/m3 | 0.222 | |
| Lag2 | 53.99 ± 20.68 µg/m3 | 56.24 ± 20.88 µg/m3 | 0.108 | |
| Lag3 | 54.00 ± 20.82 µg/m3 | 56.25 ± 20.09 µg/m3 | 0.172 | |
| Cumulative lag | 53.98 ± 17.62 µg/m3 | 56.14 ± 17.38 µg/m3 | 0.154 | |
| SO2 | Lag0 | 0.0060 ± 0.005 ppm | 0.0065 ± 0.006 ppm | 0.882 |
| Lag1 | 0.0059 ± 0.005 ppm | 0.0070 ± 0.006 ppm | 0.03 | |
| Lag2 | 0.006 ± 0.005 ppm | 0.0069 ± 0.006 ppm | 0.039 | |
| Lag3 | 0.006 ± 0.005 ppm | 0.0069 ± 0.006 ppm | 0.075 | |
| Cumulative lag | 0.006 ± 0.003 ppm | 0.0068 ± 0.004 ppm | 0.018 | |
| PM2.5 | Lag0 | 23.21 ± 9.3 µg/m3 | 24.10 ± 9.6 µg/m3 | 0.284 |
| Lag1 | 23.18 ± 9.27 µg/m3 | 24.17 ± 9.80 µg/m3 | 0.207 | |
| Lag2 | 23.19 ± 9.3 µg/m3 | 24.5 ± 9.34 µg/m3 | 0.029 | |
| Lag3 | 23.20 ± 9.35 µg/m3 | 24.4 ± 9.65 µg/m3 | 0.081 | |
| Cumulative lag | 23.19 ± 7.1 µg/m3 | 24.32 ± 7.28 µg/m3 | 0.028 | |
| IMECA | Lag0 | 45.80 ± 16.4 | 46.94 ± 17.08 | 0.574 |
| Lag1 | 45.76 ± 16.43 | 47.27 ± 17.31 | 0.266 | |
| Lag2 | 45.78 ± 16.49 | 47.37 ± 17.09 | 0.217 | |
| Lag3 | 45.77 ± 16.61 | 47.36 ± 16.258 | 0.251 | |
| Cumulative lag | 45.77 ± 14.03 | 47.22 ± 14.07 | 0.275 | |
Difference in means of the concentration levels of each particle and IMECA at different exposure times.
*Adjusted for temperature and atmospheric pressure
For exposure at lag1, a significant difference was found in SO2 (SO2 in STEMI group 0.0070 ± 0.006 ppm, no STEMI group 0.0059 ± 0.0054 ppm, (p = 0.030)). The rest of the particles showed no significant difference.
When analyzing the means in lag2, we can observe a significant difference in CO (CO in STEMI group 0.695 ± 0.239 ppm, no STEMI group 0.652 ± 0.231 ppm, (p = 0.009)), SO2 (SO2 in STEMI group 0.0069 ± 0.006 ppm, no STEMI group 0.0060 ± 0.005 ppm (p = 0.039)) and PM2.5 (PM2.5 in STEMI group 24.5 ± 9.34 µg/m3, no STEMI group 23.19 ± 9.3 µg/m3, (p = 0.029)).
Lag3 showed no significant difference between each particle. Lastly, when analyzing the cumulative 5-day lag, we found significant difference in groups for SO2 (SO2 in STEMI group 0.0068 ± 0.0044 ppm, no STEMI group 0.0060 ± 0.0037 ppm (p = 0.018)) and PM2.5 (PM2.5 in STEMI group 24.32 ± 7.2 µg/m3, no STEMI group 23.19 ± 7.18 µg/m3, (p = 0.028)) Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6.
Fig. 1.
Group comparison of carbon monoxide means at different exposure times.
Fig. 2.
Group comparison of nitrogen dioxide means at different exposure times.
Fig. 3.
Group comparison of ozone means at different exposure times.
Fig. 4.
Group comparison of PM10 means at different exposure times.
Fig. 5.
Group comparison of sulfur dioxide means at different exposure times.
Fig. 6.
Group comparison of PM2.5 means at different exposure times.
When analyzing the IMECA levels, no significant differences were found between the two groups. During the day of the cardiovascular event, the means were: IMECA in STEMI group 46.94 ± 17.08, no STEMI group 45.80 ± 16.4 (p = 0.57); comparing against exposure of lag1 and lag2, the results were similar; reported IMECA in STEMI group 47.27 ± 17.31, no STEMI group 45.76 ± 16.43 (p = 0.266) for lag1; and IMECA in STEMI group 47.37 ± 17.09, no STEMI group 45.78 ± 16.49 (p = 0.217) for lag2. Cumulative 5-day lag also showed no statistical difference between groups.
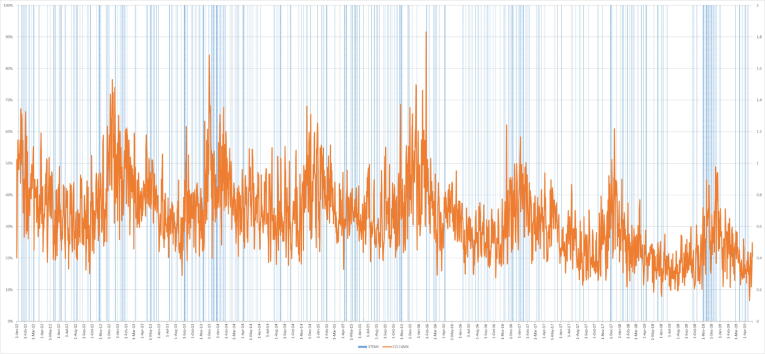
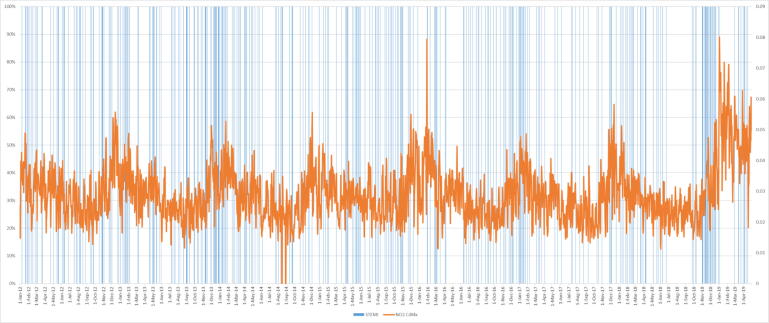
During the total of days analyzed in our study, 61% of the time Mexico City had good quality of air, according to the IMECA levels and the classification aforementioned; 38.5% of the time was regular quality, and the remaining days were bad quality Fig. 7, Fig. 8, Fig. 9, Fig. 10, Fig. 11, Fig. 12.
Fig. 7.
Relationship between CO and STEMI through time.
Fig. 8.
Relationship between NO2 and STEMI through time.
Fig. 9.
Relationship between ozone and STEMI through time.
Fig. 10.
Relationship between PM10 and STEMI through time.
Fig. 11.
Relationship between SO2 and STEMI through time.
Fig. 12.
Relationship between PM2.5 and STEMI through time.
4. Discussion
The concentration levels of different pollutants showed an association with myocardial events. These results are similar to previous air pollution studies. Not all particles resulted in a positive association, and the ones that did, were during different exposure times.
In our study, none of the particles showed a difference between groups at lag0. We believe that air pollution at lag0 does not reflect the real exposure that the patient had before the cardiovascular event. The cases were classified according to the day of the STEMI, not by the hour, so cases that occurred during early hours in the morning would not match against the levels of that current day.
The difference in groups when analyzing exposure at lag1, and lag2 was stronger and more particles were associated. This stronger relation between the air pollution levels on the days prior to the myocardial event could highlight the importance of the subacute inflammatory process. As mentioned before, the proinflammatory state has been well demonstrated and plays a mayor role in plaque vulnerability and platelet function. This subacute effect is further emphasized when we analyze the cumulative lag, showing that the pollution levels from 5 days before are closely linked with an increased risk.
Only ozone, NO2 and PM10 showed no difference between groups regardless of the exposure day. Ozone has been associated with cardiovascular effects in experimental settings with controlled exposure, but real-world evidence has failed to reproduce these results consistently, as noted by Mustafic in a recent metanalysis [14]. In our results, ozone was the only particle found in less concentrations during the days without myocardial infarction, although this difference was not statistically significant. NO2 and PM10 levels were higher in the STEMI group, but did not reach significance.
The IMECA levels reported did not associate with an increase in cardiovascular events in our study. We found a few explanations as to why we got these results. One of the reasons a quality index may not associate directly with more cardiovascular events could be that not all particles have been successfully associated with an increased risk. As previously mentioned, the air quality index is a simplified way of describing the concentration levels, and is reported as a single figure representing the highest score of any of the particles measured. Because of this, the level of IMECA analyzed could be guided by a less harmful particle, misrepresenting the actual cardiovascular risk.
Another explanation closely related to the one before, is that when we have only one numeric value, the rest of the particles are not considered regardless of the concentration level at that moment of time. We could be encountering scenarios where all particles are at a high concentration level, or where only one of them is elevated, and the IMECA level would be the same. Because of the exaggerated simplification, having a bad quality of air index may or may not reflect a harmful concentration of particles related to STEMI.
The lack of association between the air quality index and cardiovascular events is a topic that needs further investigation. The IMECA is only applied in Mexico, but these results could be extrapolated into any air quality index around the world. The similarities between all indexes are far greater than the differences. If bigger studies keep showing the same results, it could lead to a major change in the way the air quality is published.
Also, the preventive measures are guided according to the air quality index levels. No measures are applied when the air quality is good or regular (from 0 to 100 points). Analysis of our data showed that 99% of the time, Mexico City was in that range. But the concentration levels of each particle could prove that these aren’t always safe levels of air pollution, changing the recommendations we could make to high-risk patients.
Our study had limitations that we need to consider. When trying to associate air pollution to cardiovascular events, we face many confounding factors. We have taken into account the most common environmental factors associated with cardiovascular events, but coronary heart disease is a multifactorial disorder, and the patients in our study could have been exposed to other risk factors not accounted for.
The real exposure that the patient had to air pollution is also hard to pinpoint. In Mexico City we have more than 40 monitoring areas that report the air pollution levels each hour. Our study analyzed the mean concentration in the whole city and also in the area near our hospital. But it’s difficult to track the movement each patient had around the city to accurately determine the exposure level. Also, the time spent outdoors could influence the results.
Lastly, our study only took into consideration patients that were admitted in our hospital. We are not taking into consideration patients that went to other units, of fatal cardiovascular events, incurring in a selection bias.
5. Conclusion
The elevated concentrations levels of CO, SO2 and PM2.5 showed significant association with STEMI at different time points before the event. Ozone, PM10 and NO2 showed no difference between groups regardless of the exposure day.
IMECA levels showed no association with STEMI in our study, during any of the exposure days analyzed. All preventive measures for the general population are guided by the air quality indexes around the world. Further research needs to prove if this strategy is adequate, or if the concentration levels of each particle is a better parameter for public health recommendations.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
I wish to acknowledge the help provided by the Cardiology Department at Hospital Español.
Acknowledgement of grant support
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Tsai D.H., Amyai N., Marques-Vidal P., Wang J.L., Riediker M., Mooser V., Paccaud F., Waeber G., Vollenweider P., Bochud M. Effects of particulate matter on inflammatory markers in the general adult population. Part Fibre Toxicol. 2012;9:24. doi: 10.1186/1743-8977-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peters A., Fröhlich M., Döring A., Immervoll T., Wichmann H.E., Hutchinson W.L., Pepys M.B., Koenig W. Particulate air pollution is associated with an acute phase response in men Results from the MONICA–Augsburg Study. Eur. Heart J. 2001;22(14):1198–1204. doi: 10.1053/euhj.2000.2483. [DOI] [PubMed] [Google Scholar]
- 3.Seaton A., MacNee W., Donaldson K., Godden D. Particulate air pollution and acute health effects. Lancet. 1995;345(8943):176–178. doi: 10.5555/uri:pii:S0140673695901736. [DOI] [PubMed] [Google Scholar]
- 4.Lucking A.J., Lundback M., Mills N.L., Faratian D., Barath S.L., Pourazar J., Cassee F.R., Donaldson K., Boon N.A., Badimon J.J., Sandstrom T., Blomberg A., Newby D.E. Diesel exhaust inhalation increases thrombus formation in man. Eur. Heart J. 2008;29(24):3043–3051. doi: 10.1093/eurheartj/ehn464. Epub 2008 Oct 24. [DOI] [PubMed] [Google Scholar]
- 5.Pope C.I., Verrier R., Lovett E., Larson A., Raizenne M., Kanner R., Schwartz J., Villegas G., Gold D., Dockery D. Heart rate variability associated with particulate air pollution. Am Heart J. 1999;138:890–899. doi: 10.1016/s0002-8703(99)70014-1. [DOI] [PubMed] [Google Scholar]
- 6.- Martínez Manautou E, Romero Álvarez H, Ordóñez de la Mora BR, Tolivia Melendez E, et al. El índice mexicano de calidad del aire (IMEXCA). Memorándum técnico. SMA/DGS At/02-78.
- 7.SEDEMA. Norma ambiental por el Distrito Federal NADF-008-AMBT-2017. Noviembre 2018.
- 8.Ruidavets J.B., Cournot M., Cassadou S., Giroux M., Meybeck M., Ferrières J. Ozone air pollution is associated with acute myocardial infarction. Circulation. 2005;111(5):563–569. doi: 10.1161/01.CIR.0000154546.32135.6E. [DOI] [PubMed] [Google Scholar]
- 9.Pope C.A., 3rd, Muhlestein J.B., May H.T., Renlund D.G., Anderson J.L., Horne B.D. Ischemic heart disease events triggered by short-term exposure to fine particulate air pollution. Circulation. 2006;114(23):2443–2448. doi: 10.1161/CIRCULATIONAHA.106.636977. [DOI] [PubMed] [Google Scholar]
- 10.Nuvolone D., Balzi D., Chini M., Scala D., Giovannini F., Barchielli A. Short-term association between ambient air pollution and risk of hospitalization for acute myocardial infarction: results of the cardiovascular risk and air pollution in Tuscany (RISCAT) study. Am. J. Epidemiol. 2011;174(1):63–71. doi: 10.1093/aje/kwr046. [DOI] [PubMed] [Google Scholar]
- 11.- Argacha, Francois & Collart, Philippe & Wauters, Aurélien & Kayaert, Peter & Lochy, Stijn & Schoors, D & Sonck, Jeroen & de Vos, T & Forton, M & Brasseur, O & Beauloye, Christophe & Gevaert, Sofie & Evrard, Patrick & Coppieters, Yves & Sinnaeve, P & Claeys, M.J.. (2016). Air pollution and ST-elevation myocardial infarction: A case-crossover study of the Belgian STEMI registry 2009–2013. Int J Cardiol. 2016 Nov 15;223:300-305. doi: 10.1016/j.ijcard.2016.07.19 [DOI] [PubMed]
- 12.Caussin C., Escolano S., Mustafic H., Bataille S., Tafflet M., Chatignoux E., Lambert Y., Benamer H., Garot P., Jabre P., Delorme L., Varenne O., Teiger E., Livarek B., Empana J.-P., Spaulding C., Jouven X. CARDIO-ARSIF Registry Investigators. Short-term exposure to environmental parameters and onset of ST elevation myocardial infarction. The CARDIO-ARSIF registry. Int. J. Cardiol. 2015;183:17–23. doi: 10.1016/j.ijcard.2015.01.078. [DOI] [PubMed] [Google Scholar]
- 13.Chen K., Breitner S., Wolf K., Hampel R., Meisinger C., Heier M., von Scheidt W., Kuch B., Peters A., Schneider A., KORA Study Group Temporal variations in the triggering of myocardial infarction by air temperature in Augsburg, Germany, 1987-2014. Eur. Heart J. 2019;40(20):1600–1608. doi: 10.1093/eurheartj/ehz116. PMID: 30859207. [DOI] [PubMed] [Google Scholar]
- 14.Mustafic H., Jabre P., Caussin C., Murad M.H., Escolano S., Tafflet M., Perier M.C., Marijon E., Vernerey D., Empana J.P., Jouven X. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. JAMA. 2012;307:713–721. doi: 10.1001/jama.2012.126. [DOI] [PubMed] [Google Scholar]