Abstract
Background
Older children have higher SARS-CoV-2 infection rates than younger children. We investigated SARS-CoV-2 infection, seroprevalence and seroconversion rates in staff and students following the full reopening of all secondary schools in England.
Methods
Public Health England (PHE) invited secondary schools in six regions (East and West London, Hertfordshire, Derbyshire, Manchester and Birmingham) to participate in SARS-CoV-2 surveillance during the 2020/21 academic year. Participants had nasal swabs for RT-PCR and blood samples for SARS-CoV-2 antibodies at the beginning (September 2020) and end (December 2020) of the autumn term. Multivariable logistic regression was used to assess independent risk factors for seropositivity and seroconversion.
Findings
Eighteen schools in six regions enrolled 2,209 participants, including 1,189 (53.8%) students and 1,020 (46.2%) staff. SARS-CoV-2 infection rates were not significantly different between students and staff in round one (5/948; [0.53%] vs. 2/876 [0.23%]; p = 0.46) or round two (10/948 [1.05%] vs. 7/886 [0.79%]; p = 0.63), and similar to national prevalence. None of four and 7/15 (47%) sequenced strains in rounds 1 and 2 were the highly transmissible SARS-CoV-2 B.1.1.7 variant. In round 1, antibody seropositivity was higher in students than staff (114/893 [12.8%] vs. 79/861 [9.2%]; p = 0.016), but similar in round 2 (117/893 [13.1%] vs.117/872 [13.3%]; p = 0.85), comparable to local community seroprevalence. Between the two rounds, 8.7% (57/652) staff and 6.6% (36/549) students seroconverted (p = 0.16).
Interpretation
In secondary schools, SARS-CoV-2 infection, seropositivity and seroconversion rates were similar in staff and students, and comparable to local community rates. Ongoing surveillance will be important for monitoring the impact of new variants in educational settings.
Research in context.
Evidence before this study
Some reports suggested larger outbreaks affecting staff and students in secondary schools compared to primary schools. Recent observations studies following the full reopening of schools in the US and Europe have reported COVID-19 cases in staff and students, but very little evidence of in-school transmission. Most reports involved passive surveillance, with testing of symptomatic individuals for acute infection followed by active case finding to identify secondary cases.
Added value of this study
We found infection rates among secondary school staff and students were similar to community infection rates at the beginning (September 2020) and end (December 2020) of the autumn term. None of the strains at the beginning of term and half the sequenced strains at the end of term belonged to the highly transmissible and more aggressive B.1.1.7 variant. Antibody positivity rates were higher in students than staff at the beginning of term but similar 9 weeks later, and comparable to local community seroprevalence. Seroconversion rates during the autumn term were also similar between staff and students, and associated with number of positive cases in school, but not with size of school or size of class.
Implications of all the available evidence
SARS-CoV-2 infection and seroprevalence rates in secondary school staff and students were comparable to community rates, but higher than primary schools and lower than other institutional settings, such as care homes, hospitals or prisons. The emergence of the B.1.1.7 variant of concern in December 2020 will require close monitoring when schools reopen after the latest national lockdown in March 2020.
Alt-text: Unlabelled box
1. Introduction
The emergence and rapid spread of SARS-CoV-2, the virus responsible for COVID-19, in December 2019 forced many countries to impose national lockdown to control the pandemic [[1], [2], [3]]. In England, the first imported cases of COVID-19 were confirmed at the end of January 2021 and increased rapidly from early March 2021, leading to school closures on 20 March 2020, followed by wider lockdown on 23 March 2020 [4]. Cases continued to increase until mid-April before plateauing and declined until the end of May 2020 [5]. From 01 June 2020, preschools, some primary and two secondary school years partially reopened for face-to-face teaching as part of the easing of national lockdown [6]. Strict infection control practices were implemented in schools, including physical distancing, hand and surface sanitisation, and smaller class sizes organised into bubbles that did not physically or socially interact with each other [6]. Very few infections and outbreaks were identified in educational settings during the summer half-term [7], and, along with similar positive experiences in other countries that reopened after their national lockdown [2,8], led to the full reopening of all schools in September 2020 [6].
Secondary school-aged children have higher SARS-CoV-2 infection rates than primary school-aged children [9], with larger and more extensive COVID-19 outbreaks reported in secondary schools compared to primary schools [[10], [11], [12]]. We, therefore, initiated prospective surveillance in 18 schools across six English regions to assess the risk of SARS-CoV-2 infection in students and staff from September 2020 until the end of the autumn term in December 2020. In addition to nasal swabs to test for acute SARS-CoV-2 infection, we collected blood samples to test for SARS-CoV-2 antibodies, which provide a more robust measure of prior symptomatic, asymptomatic or mild, transient SARS-CoV-2 infection. We compared antibody seroprevalence in participating schools with local community rates and estimated seroconversion rates and risk factors for seroconversions among seronegative students and staff.
2. Methods
The COVID-19 Surveillance in Secondary School KIDs (sKIDsPLUS) protocol is available online ( HYPERLINK " https://www.gov.uk/guidance/covid-19-paediatric-surveillance) [13]. The protocol was approved by PHE Research Ethics Governance Group (reference Nr0228; 24 August 2020). The study involved testing secondary school students for SARS-CoV-2 infection and antibodies at the start (22 September–17 October) and end (3–17 December) of the autumn term of the 2020/21 academic year. Schools were approached in areas where a paediatric investigation team could be assembled: Derbyshire, West London, East London, Greater Manchester, Hertfordshire and Birmingham.
The schools were open full-time for in-person teaching, albeit strict infection control measures in place and very limited extracurricular or after-school activities for students [6]. As per national guidance, face masks and face coverings were not recommended in classrooms, but staff and children in secondary schools were advised to wear them in communal areas outside the classroom if physical distancing was difficult to maintain [6]. Headteachers in participating schools emailed the study information pack to staff, parents of students aged <16 years and students aged ≥16. Participants or their parent/guardian provided informed consent online via Snap Survey, and completed a short questionnaire prior to the sampling day. The questionnaire requested information about demographics, risk factors and COVID-19 symptoms or confirmed infections in the household. Enrolment was open for new participants between rounds 1 and 2. Headteachers in participating schools provided information about average bubble sizes, school absences (>10 days), numbers isolating at home and confirmed cases in students and staff for the term. A team of clinicians, nurses, phlebotomists and administrative staff attended the school on the sampling days. Local anaesthetic cream was offered to all students before blood sampling. A member of the school staff was present with each student. Participating students and staff had a nasal swab and a blood sample taken by the investigation team.
2.1. Laboratory testing
The swabs were tested by a triplex reverse transcription quantitative PCR (RT-qPCR) assay for the detection of ORF1ab and E gene regions of SARS-CoV-2 with simultaneous detection of an exogenous internal control using the Applied Biosystems Quantstudio 7-flex thermocycler (ThermoFisher Scientific, UK). The ORF1ab gene primers/probes published by the China CDC were combined with the E gene primers/probe published Corman et al. [14,15]. A positive RT-qPCR result was reported to the participant, local investigator, head teacher and local PHE health protection team (HPT), typically within 48 hours of the sample being taken. The participant and household members self-isolated as per national guidance. Public health risk assessment was undertaken with the school to decide additional measures, including identification and isolation of the participant's contacts inside and outside school premises. Serology was performed on the Abbott Architect using a chemiluminescent microparticle immunoglobulin G (IgG) immunoassay targeting the nucleoprotein (SARS-CoV-2 IgG, Abbott Commerce Chicago, USA) with a seropositivity threshold of 0.8 [16].
2.2. Statistical analysis
Data were managed in R-Studio and Microsoft Access and analysed in Stata SE (version 15.1). Data that did not follow a normal distribution are described as median with interquartile ranges. Categorical data are described as proportions and compared with the Chi2-test or Fisher's exact. SARS-CoV-2 infection rate and antibody seroprevalence, with 95% confidence intervals (CI), were compared between secondary school students and staff and the Office for National Statistics (ONS) Coronavirus Infection Survey regional seroprevalence (spike protein antibody target) for the corresponding time periods [17,18]. Non-overlapping 95% CIs were used to assess statistical significance between student or staff rates and ONS estimates. Antibody seroconversion rates with 95% confidence intervals were calculated for participants who were tested in both rounds and were negative in their first round of testing.
Tests for association with participant drop-out at round 2, SARS-CoV-2 antibody positivity and antibody seroconversion were performed using logistic regression. To assess the characteristics of students and staff who dropped out in round 2, univariate and multivariable logistic regression was used, adjusted for sex, age, ethnicity, school area and Round 1 antibody test results. Participants were classified as included in each round if they provided a blood or swab sample in that round. Univariable analysis including all participants was performed initially, followed by a multivariable analysis including participants with complete data. For SARS-CoV-2 antibody positivity and antibody seroconversion, a multivariable regression model was built using age, sex, ethnicity and school area a priori, and factors found to be associated with SARS-CoV-2 antibody positivity or antibody seroconversion in the univariable analysis. Variation between schools was allowed for via a school-level random effect.
2.3. Role of funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. SNL and GI had access to the data and had final responsibility to submit for publication.
3. Results
Eighteen secondary schools in six school areas enrolled and all participated in both rounds of sKIDsPLUS. In round 1, there were 1,825 participants, comprising of 948 (51.9%) students and 877 (48.1%) staff (Supplementary Fig. S1, Table 1). In round 2, 367 participants did not return for their second test (239 [25.2%] students, 128 [14.6%] staff) and 384 new participants (241 students, 143 staff) were enrolled, resulting in 1,842 participants (950 [51.6%] students, 892 [48.4%] staff) in round 2. The demographics of participants in the two rounds were similar (Table 1), but drop out between rounds 1 and 2 was associated with Asian ethnicity and school area in students, and school area and being aged 30–39 years in staff (Supplementary Table S2).
Table 1.
Characteristics of staff and students from 18 secondary schools participating in sKIDs Plus in the autumn term, 2020.
| Total |
Round 1 |
Round 2 |
|||||
|---|---|---|---|---|---|---|---|
| Total | Students | Staff | Total | Students | Staff | ||
| Sex | |||||||
| Male | 765 (34.6) | 645 (35.3) | 373 (39.3) | 272 (31.0) | 625 (33.9) | 362 (38.1) | 263 (29.5) |
| Female | 1436 (65.0) | 1174 (64.3) | 569 (60.0) | 605 (69.0) | 1212 (65.8) | 583 (61.4) | 629 (70.5) |
| Non-binary | 6 (0.3) | 4 (0.2) | 4 (0.4) | 0 (0.0) | 4 (0.2) | 4 (0.4) | 0 (0.0) |
| Not known | 2 (0.1) | 2 (0.1) | 2 (0.2) | 0 (0.0) | 1 (0.1) | 1 (0.2) | 0 (0.0) |
| Age category | |||||||
| 11-12 | 399 (18.1) | 325 (17.8) | 325 (34.3) | 314 (17.0) | 314 (33.1) | ||
| 13-14 | 478 (21.6) | 381 (20.9) | 381 (40.2) | 376 (20.4) | 376 (39.6) | ||
| 15-16 | 170 (7.7) | 135 (7.4) | 135 (14.2) | 139 (7.5) | 139 (14.6) | ||
| 17-18 | 142 (6.4) | 107 (5.9) | 107 (11.3) | 121 (6.6) | 121 (12.7) | ||
| 19-29 | 185 (8.4) | 161 (8.8) | 161 (18.4) | 169 (9.2) | 169 (18.9) | ||
| 30-39 | 280 (12.7) | 243 (13.3) | 243 (27.7) | 236 (12.8) | 236 (26.5) | ||
| 40-49 | 250 (11.3) | 219 (12.0) | 219 (25.0) | 216 (11.7) | 216 (24.2) | ||
| 50-59 | 255 (11.5) | 211 (11.6) | 211 (24.1) | 226 (12.3) | 226 (25.3) | ||
| 60+ | 50 (2.3) | 43 (2.4) | 43 (4.9) | 45 (2.4) | 45 (5.0) | ||
| Ethnicity | |||||||
| White | 1577 (71.4) | 1325 (72.6) | 608 (64.1) | 717 (81.8) | 1342 (72.9) | 623 (65.6) | 719 (80.6) |
| Black | 97 (4.4) | 77 (4.2) | 43 (4.5) | 34 (3.9) | 77 (4.2) | 44 (4.6) | 33 (3.7) |
| Asian | 333 (15.1) | 256 (14.0) | 170 (17.9) | 86 (9.8) | 258 (14.0) | 158 (16.6) | 100 (11.2) |
| Mixed | 125 (5.7) | 103 (5.6) | 78 (8.2) | 25 (2.9) | 104 (5.6) | 80 (8.4) | 24 (2.7) |
| Other | 59 (2.7) | 51 (2.8) | 38 (4.0) | 13 (1.5) | 46 (2.5) | 33 (3.5) | 13 (1.5) |
| Unknown | 18 (0.8) | 13 (0.7) | 11 (1.2) | 2 (0.2) | 15 (0.8) | 12 (1.3) | 3 (0.3) |
| School Area | |||||||
| Derbyshire | 552 (25.0) | 456 (25.0) | 213 (22.5) | 243 (27.7) | 448 (24.3) | 209 (22.0) | 239 (26.8) |
| East London | 531 (24.0) | 423 (23.2) | 224 (23.6) | 199 (22.7) | 420 (22.8) | 222 (23.4) | 198 (22.2) |
| Greater Manchester | 173 (7.8) | 145 (7.9) | 87 (9.2) | 58 (6.6) | 139 (7.5) | 82 (8.6) | 57 (6.4) |
| Hertfordshire | 171 (7.7) | 167 (9.2) | 102 (10.8) | 65 (7.4) | 132 (7.2) | 75 (7.9) | 57 (6.4) |
| West London | 333 (15.1) | 248 (13.6) | 146 (15.4) | 102 (11.6) | 300 (16.3) | 188 (19.8) | 112 (12.6) |
| Birmingham | 449 (20.3) | 386 (21.2) | 176 (18.6) | 210 (24.0) | 403 (21.9) | 174 (18.3) | 229 (25.7) |
| Median (IQR) number of participants by school | 108 (80-120) | 102 (82-122) | |||||
| Total | 2,209 | 1825 | 948 | 877 | 1842 | 950 | 892 |
IQR: interquartile range
3.1. SARS-CoV-2 infection rates
Nasal swabs for SARS-CoV-2 RT-qPCR in round 1 were positive in 0.38% (7/1,824; 95% CI, 0.15–0.79) participants and were not significantly different between students (5/948; 0.53%, 95% CI: 0.17–1.23) and staff (2/876; 0.23%, 95% CI: 0.03–0.82; p = 0.46) (Table 2). In round 2, SARS-CoV-2 RT-qPCR positivity was 0.93 (17/1834; 95% CI, 0.54-–1.48) and, again, did not differ significantly between students (10/948; 1.05%; 95% CI: 0.51–1.93) and staff (7/886; 0.79%; 95% CI: 0.32–1.62; p = 0.63). These were similar to national infection rates for the corresponding time periods in the ONS Coronavirus Infection Survey for round 1 (0.21%; 95% CI: 0.18–0.24) and round 2 (1.18; 95% CI:1.12–1.25). Where known (13/17, 76.5%), 38.5% (5/13) of participants positive in round 2 reported COVID-19 symptoms between testing rounds, 4 within a week of their positive test, the other had tested positive for SARS-CoV-2 almost a month earlier.
Table 2.
SARS-COV-2 PCR and antibody results in students and staff from 18 schools participating in sKIDs Plus in round 1 (September) and round 2 (December).
| Round 1 |
Round 2 |
|||||
|---|---|---|---|---|---|---|
| Total | Students | Staff | Total | Students | Staff | |
| PCR results | ||||||
| Negative | 1,817 (99.6) | 943 (99.5) | 874 (99.8) | 1,817 (99.1) | 938 (98.9) | 879 (99.2) |
| Positive | 7 (0.4) | 5 (0.5) | 2 (0.2) | 17 (0.9) | 10 (1.1) | 7 (0.8) |
| Total | 1,824 | 948 | 876 | 1,834 | 948 | 886 |
| Antibody results | ||||||
| Negative | 1,561 (89.0) | 779 (87.2) | 782 (90.8) | 1,531 (86.7) | 776 (86.9) | 755 (86.6) |
| Positive | 193 (11.0) | 114 (12.8) | 79 (9.2) | 234 (13.3) | 117 (13.1) | 117 (13.4) |
| Total | 1,754 | 893 | 861 | 1,765 | 893 | 872 |
3.2. SARS-CoV-2 genome sequencing
Four (57.1%) and 15 (88.2%) positive samples from rounds 1 and 2, respectively, were successfully sequenced. None were the B1.1.7 variant in round 1 compared to seven (46.7%) in round 2, including four in London, two in the Birmingham and one in Derbyshire.
3.3. Antibody prevalence
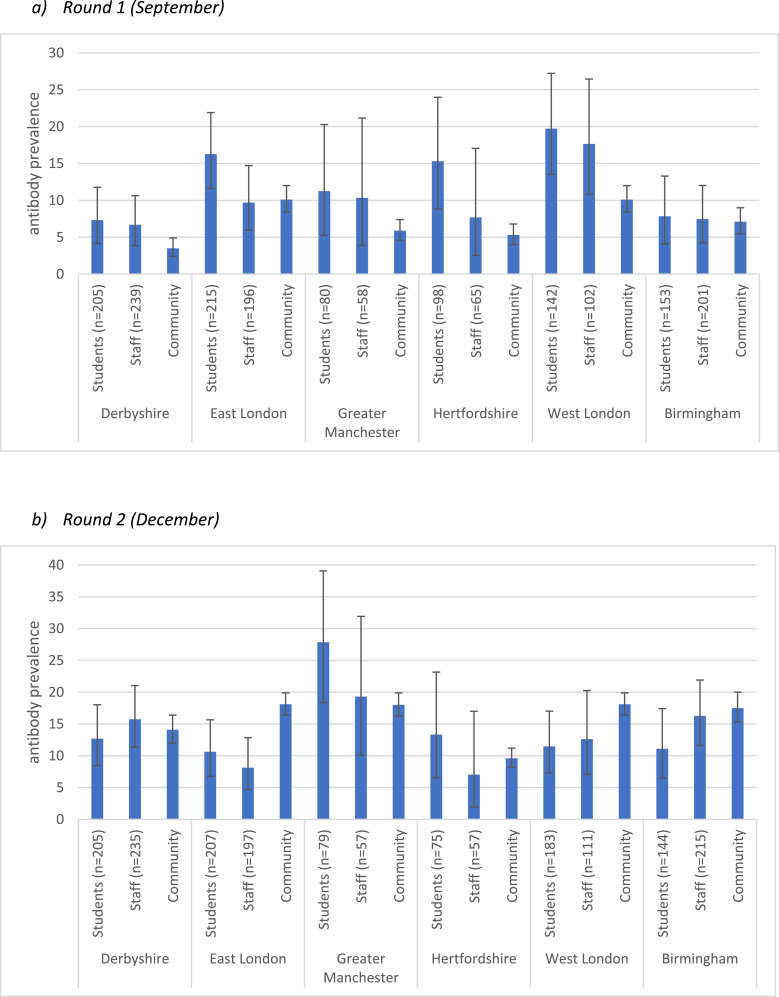
SARS-CoV-2 antibody positivity was 11.0% (193/1754; 95%CI: 9.6–12.6) in round 1 and 13.3% (234/1765; 95% CI: 11.7–14.9; p = 0.041) in round 2 (Table 2). In round 1, antibody positivity was higher in students (114/893 [12.8%], 95% CI: 10.6–15.1) than staff (79/861 [9.2%], 95% CI: 7.3–11.3; p = 0.016), but similar in round 2 (students: 117/893 [13.1%], 95% CI: 11.0–15.5; staff: 117/872 [13.4%], 95% CI: 11.2–15.9; p = 0.85). Significant changes in antibody positivity between the two rounds were only observed for staff (p = 0.005), not students (p = 0.83). Differences in antibody positivity were observed by school area in rounds 1 (p < 0.001) and 2 (p = 0.001). When compared to local community seroprevalence, antibody positivity in students was higher in West London and Hertfordshire in round 1 and lower for both students and staff in East London in round 2 (Fig. 1).
Fig. 1.
Student, staff and community prevalence (percent) of SARS-COV-2 antibodies for the six school areas in rounds 1 and 2. Community prevalence source: Office for National Statistics, 2021, Coronavirus (COVID-19) Infection Survey, antibody data for the UK: 16 March 2021. (data from 17 September to 14 October 2020 and 10 December 2020 to 6 January 2021.[18] (a) Round 1 (September). (b) Round 2 (December).
Multivariable regression, adjusted for all other variables in the model and clustering by school, was used to assess predictors of antibody positivity in rounds 1 and 2 (Tables 3,4). Clustering by school was not significant for students in either round and only significant for staff in round 1 (p = 0.0088). In round 1 antibody positivity in students was associated with school area, year group and additional children in the household and, in round 2, with Black ethnicity and the number of positive cases in the school. In staff, antibody positivity in round 1 was associated with being male and, in round 2, with ethnicity and the number of positive cases in the school during the autumn term.
Table 3.
Risk factors for antibody positivity in students participating rounds 1 (a) and 2 (b) of secondary school surveillance for SARS-CoV-2, England.
OR = odds ratio; IQR = Interquartile Range; CI = confidence interval.
| a) | |||||
| Antibody positive | Univariable analysis | Multivariable analysis adjusted for clustering by school (p = 1.0) | |||
| N = 893 | N = 719 | ||||
| Factor | n/N (%) | OR (95% CI) | P value | OR (95% CI) | P value |
| Sex | |||||
| Female | 63/532 (11.8) | REF | REF | 0.86 | |
| Male | 51/355 (14.4) | 1.25 (0.84–1.86) | 0.27 | 1.05 (0.63–1.73) | |
| Non–binary/Missing | 0/6 (0.0) | ||||
| Year Group | |||||
| Years 7–9 | 56/475 (11.8) | REF | 0.013 | REF | 0.0031 |
| Years 10–11 | 43/241 (17.8) | 1.62 (1.06–2.50) | 2.31 (1.37–3.88) | ||
| 6th form/College | 15/177 (8.5) | 0.69 (0.38–1.26) | 0.97 (0.46–2.02) | ||
| Ethnicity | |||||
| White | 63/567 (11.1) | REF | 0.01 | REF | 0.15 |
| Black | 10/41 (24.4) | 2.58 (1.21–5.51) | 1.99 (0.73–5.46) | ||
| Asian | 24/164 (14.6) | 1.37 (0.83–2.27) | 1.38 (0.73–2.61) | ||
| Mixed | 7/73 (9.6) | 0.85 (0.37–1.93) | 1.04 (0.42–2.55) | ||
| Other | 10/37 (27.0) | 2.96 (1.37–6.41) | 2.74 (1.15–6.54) | ||
| Missing | 0/11 (0.0) | ||||
| School area | |||||
| Derbyshire | 15/205 (7.3) | 0.93 (0.42–2.04) | 0.0042 | 0.85 (0.31–2.33) | 0.012 |
| East London | 35/215 (16.3) | 2.28 (1.14–4.56) | 2.39 (0.97–5.93) | ||
| Greater Manchester | 9/80 (11.3) | 1.49 (0.60–3.70) | 2.03 (0.71–5.85) | ||
| Hertfordshire | 15/98 (15.3) | 2.12 (0.95–4.75) | 2.63 (0.97–7.10) | ||
| West London | 28/142 (19.7) | 2.89 (1.40–5.93) | 3.33 (1.39–7.99) | ||
| Birmingham | 12/153 (7.8) | REF | REF | ||
| Additional children in household | |||||
| per additional child | 0.75 (0.58–0.97) | 0.027 | 0.77 (0.59–1.00) | 0.048 | |
| median size (IQR) | 1 (0–2) | ||||
| Additional household members | |||||
| per additional member | 0.98 (0.86–1.11) | 0.72 | |||
| median size (IQR) | 3 (3–4) | ||||
| Parental occupation | |||||
| Neither healthcare or key worker | 71/570 (12.5) | REF | 0.77 | ||
| Key worker | 31/245 (12.7) | 1.02 (0.65–1.60) | |||
| Healthcare worker | 12/78 (15.4) | 1.28 (0.66–2.48) | |||
| School Capacity | |||||
| per 1 increase in students per year | 1.00 (0.99–1.00) | 0.18 | |||
| median (IQR)* | 1215 (793–1500) | ||||
| % FSM | |||||
| per % increase in FSM | 1.00 (0.98–1.02) | 0.68 | |||
| median (IQR) * | 17.6 (9.2–20.7) | ||||
| |||||
| Antibody positive | Univariable analysis | Multivariable analysis adjusted for clustering by school (p = 1.0) | |||
| N = 893 | N = 878 | ||||
| Factor | n/N (%) | OR (95% CI) | P value | OR (95% CI) | P value |
| Sex | |||||
| Female | 62/550 (11.3) | REF | REF | 0.26 | |
| Male | 55/339 (16.2) | 1.52 (1.03–2.25) | 0.035 | 1.31 (0.82–2.08) | |
| Non–binary/Missing | 0/4 (0.0) | ||||
| Year Group | |||||
| Years 7–9 | 62/464 (13.4) | REF | 0.0031 | REF | 0.18 |
| Years 10–11 | 42/233 (18.0) | 1.43 (0.93–2.19) | 1.29 (0.82–2.04) | ||
| 6th form–College | 13/196 (6.6) | 0.46 (0.25–0.86) | 0.64 (0.31–1.32) | ||
| Ethnicity | |||||
| White | 72/591 (12.2) | REF | 0.14 | REF | 0.053 |
| Black | 11/41 (26.8) | 2.64 (1.27–5.50) | 3.35 (1.52–7.38) | ||
| Asian | 19/147 (12.9) | 1.07 (0.62–1.84) | 1.12 (0.61–2.05) | ||
| Mixed | 10/72 (13.9) | 1.16 (0.57–2.37) | 1.32 (0.63–2.80) | ||
| Other | 5/31 (16.1) | 1.39 (0.52–3.72) | 1.48 (0.53–4.12) | ||
| Missing | 0/11 (0.0) | ||||
| School area | |||||
| Derbyshire | 26/205 (12.7) | 1.16 (0.60–2.25) | 0.0071 | 1.20 (0.55–2.60) | 0.60 |
| East London | 22/207 (10.6) | 0.95 (0.48–1.88) | 1.25 (0.54–2.93) | ||
| Greater Manchester | 22/79 (27.8) | 3.09 (1.51–6.32) | 1.93 (0.86–4.34) | ||
| Hertfordshire | 10/75 (13.3) | 1.23 (0.53–2.86) | 1.73 (0.57–5.19) | ||
| West London | 21/183 (11.5) | 1.04 (0.52–2.07) | 1.45 (0.56–3.74) | ||
| West Midlands | 16/144 (11.1) | REF | REF | ||
| Additional children in household | |||||
| per additional child | 0.94 (0.74–1.19) | 0.57 | |||
| median size (IQR) | 1 (0–2) | ||||
| Additional household members | |||||
| per additional member | 1.02 (0.87–1.18) | 0.84 | |||
| median size (IQR) | 3 (3–4) | ||||
| Parental occupation | |||||
| Neither healthcare or key worker | 79/576 (13.7) | REF | 0.53 | ||
| Key worker | 32/249 (12.9) | 0.93 (0.60–1.44) | |||
| Healthcare worker | 6/68 (8.8) | 0.61 (0.25–1.45) | |||
| School Capacity | |||||
| Per 10 student increase | 1.01 (1.00–1.01) | 0.049 | 1.00 (0.99–1.01) | 0.79 | |
| Median size (IQR) * | 1215 (793–1380) | ||||
| Average students year | |||||
| per 1 increase in students per year | 1.00 (1.00–1.00) | 0.83 | |||
| median (IQR) * | 192 (160–300) | ||||
| % FSM | |||||
| per % increase in FSM | 1.03 (1.01–1.06) | 0.001 | 1.01 (0.98–1.04) | 0.60 | |
| median (IQR) * | 17.5 (9.2–20.7) | ||||
| Number of positive cases in school | |||||
| per 1 additional case | 1.01 (1.01–1.02) | <0.001 | 1.01 (1.00–1.03) | 0.027 | |
| median (IQR) * | 35 (15–56) | ||||
based on included students and not school
Table 4.
Risk factors for antibody positivity in staff participating rounds 1 (a) and 2 (b) of secondary school surveillance for SARS-CoV-2, England.
OR = odds ratio; IQR = Interquartile Range; CI = confidence interval
| a) | |||||
| Antibody positive | Univariable analysis | Multivariable analysis adjusted for clustering by school (p = 0.0088) | |||
| N = 861 | N = 857 | ||||
| Factor | n/N (%) | OR (95% CI) | P value | OR (95% CI) | P value |
| Sex | |||||
| Female | 45/594 (7.6) | REF | 0.016 | REF | 0.010 |
| Male | 34/267 (12.7) | 1.78 (1.11–2.85) | 1.93 (1.17–3.19) | ||
| Year Group | |||||
| 19–29 | 15/158 (9.5) | 1.21 (0.60–2.47) | 0.57 | 1.20 (0.58–2.51) | 0.33 |
| 30–39 | 19/239 (7.9) | REF | REF | ||
| 40–49 | 17/212 (8.0) | 1.01 (0.51–2.00) | 1.13 (0.55–2.30) | ||
| 50–59 | 25/209 (12.0) | 1.57 (0.84–2.95) | 1.95 (1.00–3.80) | ||
| 60+ | 3/43 (7.0) | 0.87 (0.25–3.07) | 1.16 (0.31–4.27) | ||
| Ethnicity | |||||
| White | 56/705 (7.9) | REF | 0.051 | REF | 0.30 |
| Black | 7/33 (21.2) | 3.12 (1.30–7.51) | 2.57 (0.96–6.90) | ||
| Asian | 11/85 (12.9) | 1.72 (0.86–3.43) | 1.63 (0.77–3.45) | ||
| Mixed | 4/24 (16.7) | 2.32 (0.77–7.02) | 1.79 (0.53–6.05) | ||
| Other | 1/13 (7.7) | 0.97 (0.12–7.56) | 0.99 (0.12–8.23) | ||
| Missing | 0/1 (0.0) | ||||
| School area | |||||
| Derbyshire | 16/239 (6.7) | 0.89 (0.43–1.85) | 0.052 | 1.01 (0.31–3.29) | |
| East London | 19/196 (9.7) | 1.33 (0.66–2.70) | 1.18 (0.39–3.52) | ||
| Greater Manchester | 6/58 (10.3) | 1.43 (0.53–3.87) | 1.97 (0.45–8.58) | 0.77 | |
| Hertfordshire | 5/65 (7.7) | 1.03 (0.36–2.96) | 1.27 (0.24–6.60) | ||
| North London | 18/102 (17.6) | 2.66 (1.28–5.53) | 2.26 (0.66–7.75) | ||
| Birmingham | 15/201 (7.5) | REF | REF | ||
| Additional household members | |||||
| per additional member | 0.97 (0.82–1.16) | 0.77 | |||
| median size (IQR) | 2 (1–3) | ||||
| Additional children in household | |||||
| per additional child | 0.91 (0.71–1.17) | 0.48 | |||
| median size (IQR) | 0 (0–1) | ||||
| Other household occupation | |||||
| Neither healthcare or key worker | 49/574 (8.5) | REF | 0.50 | ||
| Key worker | 26/259 (10.0) | 1.20 (0.73–1.97) | |||
| Healthcare worker | 4/28 (14.3) | 1.79 (0.60–5.36) | |||
| School Capacity | |||||
| Per 10 student increase | 0.99 (0.99–1.00) | 0.032 | 1.00 (0.99–1.01) | 0.54 | |
| Median size (IQR) * | 1300 (1075–1500) | ||||
| % FSM | |||||
| per % increase in FSM | 1.01 (0.98–1.03) | 0.56 | |||
| median (IQR) * | 19.7 (14.3–29.4) | ||||
| omitted due to small sample size; * based on included staff and not school | |||||
| b) | |||||
| Antibody positive | Univariable analysis | Multivariable analysis adjusted for clustering by school (p = 0.11) | |||
| N = 872 | N = 870 | ||||
| Factor | n/N (%) | OR (95% CI) | P value | OR (95% CI) | P value |
| Sex | |||||
| Female | 79/611 (12.9) | REF | 0.52 | REF | 0.23 |
| Male | 38/261 (14.6) | 1.15 (0.76–1.74) | 1.30 (0.84–2.02) | ||
| Year Group | |||||
| 19–29 | 25/164 (15.2) | 1.55 (0.85–2.83) | 0.59 | 1.65 (0.89–3.08) | 0.42 |
| 30–39 | 24/231 (10.4) | REF | REF | ||
| 40–49 | 29/213 (13.6) | 1.36 (0.76–2.42) | 1.32 (0.73–2.39) | ||
| 50–59 | 33/219 (15.1) | 1.53 (0.87–2.68) | 1.70 (0.95–3.05) | ||
| 60+ | 6/45 (13.3) | 1.33 (0.51–3.46) | 1.25 (0.46–3.35) | ||
| Ethnicity | |||||
| White | 87/704 (12.4) | REF | 0.094 | REF | 0.011 |
| Black | 9/32 (28.1) | 2.78 (1.24–6.19) | 4.18 (1.72–10.16) | ||
| Asian | 17/97 (17.5) | 1.51 (0.85–2.66) | 2.07 (1.11–3.86) | ||
| Mixed | 3/24 (12.5) | 1.01 (0.30–3.47) | 1.33 (0.37–4.74) | ||
| Other | 1/13 (7.7) | 0.59 (0.08–4.60) | 0.76 (0.09–6.29) | ||
| Missing | 0/2 (0.0) | ||||
| School area | |||||
| Derbyshire | 37/235 (15.7) | 0.96 (0.58–1.59) | 0.058 | 0.94 (0.46–1.91) | 0.49 |
| East London | 16/197 (8.1) | 0.45 (0.24–0.85) | 0.48 (0.20–1.14) | ||
| Greater Manchester | 11/57 (19.3) | 1.23 (0.58–2.61) | 1.14 (0.42–3.06) | ||
| Hertfordshire | 4/57 (7.0) | 0.39 (0.13–1.14) | 0.55 (0.15–2.06) | ||
| North London | 14/111 (12.6) | 0.74 (0.38–1.45) | 1.02 (0.38–2.71) | ||
| West Midlands | 35/215 (16.3) | REF | REF | ||
| Additional household members | |||||
| per additional member | 1.01 (0.88–1.17) | 0.85 | |||
| median size (IQR) | 2 (1–3) | ||||
| Additional children in household | |||||
| per additional child | 0 (0–1) | 1.17 (0.97–1.42) | 0.10 | ||
| median size (IQR) | |||||
| Other household occupation | |||||
| Neither healthcare or key worker | 70/587 (11.9) | REF | 0.18 | ||
| Key worker | 42/254 (16.5) | 1.46 (0.97–2.21) | |||
| Healthcare worker | 5/31 (16.1) | 1.42 (0.53–3.82) | |||
| School Capacity | |||||
| Per 10 student increase | 1.00 (1.00–1.01) | 0.61 | |||
| Median size (IQR) * | 1300 (1075–1500) | ||||
| Ave year size | |||||
| per 1 increase in students per year | 1.00 (1.00–1.00) | 0.73 | |||
| median (IQR) * | 197 (160–300) | ||||
| % FSM | |||||
| per % increase in FSM | 1.02 (1.00–1.04) | 0.12 | |||
| median (IQR) * | 19.7 (14.3–29.4) | ||||
| Number of positive cases in school | |||||
| per 1 additional case | 1.01 (1.01–1.02) | <0.001 | 1.01 (1.00–1.02) | 0.021 | |
| median (IQR) * | 35 (18–66) | ||||
| Students a week | |||||
| 0–19 | 2/39 (5.1) | 0.29 (0.07–1.25) | |||
| 20–99 | 6/67 (9.0) | 0.52 (0.20–1.32) | 0.23 | ||
| 100–200 | 28/176 (15.9) | REF | |||
| 200+ | 36/248 (14.5) | 0.90 (0.52–1.54) | |||
| Missing | 45/342 (13.2) | ||||
* based on included staff and not school
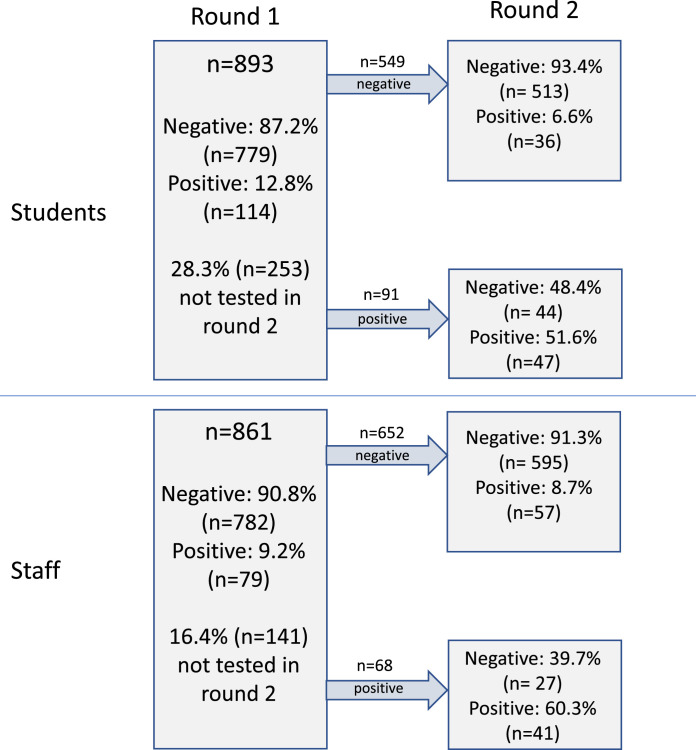
3.4. Seroconversion
Overall, 61.6% (1360/2209) of participants had antibody results for both rounds of testing, including 1,201 (88.3%) who were negative in round 1 (Fig. 2). The median time between testing rounds was 9.3 weeks (IQR: 9.1–11). The seroconversion rate was 7.7% (93/1201; 95% CI: 6.3–9.4) and did not differ between staff (57/652, 8.7%, 95% CI: 6.7–11.2) and students (36/549, 6.6%, 95% CI: 4.6–9.0) (p = 0.16) but differed by school area (p < 0.001). Where known (91/93, 97.8%), COVID-19 symptoms among participants who seroconverted between the two rounds were reported in 33.3% (12/36) of students compared to 76.4% (42/55) of staff (p < 0.001). When asked, 60.4% (29/48) of staff completing the questionnaire considered that they had acquired the infection in school compared to (36.4% (12/33) of students (p = 0.033), and 16.7% (8/48) and 36.4% (12/33), respectively, had not known they were infected over the autumn term. More participants (60.9%; 28/46) who were positive and reported COVID-19 symptoms between testing rounds thought they acquired the infection at school than participants who reported no COVID-19 symptoms (37.1%; 13/35; p = 0.034). Using multivariable logistic regression, seroconversion in students and staff was associated with the number of positive cases in the school during the autumn term and for staff was additionally associated with Black ethnicity and the number of children in the household, but not with size of the household, healthcare or other key workers in the household, school or class size, or proportion of students on free school meals (Supplementary Tables S3 and S4).
Fig. 2.
Results of the participants tested in both rounds of sKIDs Plus
4. Discussion
Active prospective surveillance following full reopening of secondary schools in England identified acute SARS-CoV-2 infection in 0.38% and 0.93% of participants at the start and end of the autumn term of the 2020/21 academic year. While infection rates were higher in students than in staff in both rounds, the differences were not statistically significant. Genome sequencing identified nearly half the SARS-CoV-2 strains in December 2020 as the novel B1.1.7 variant compared to none in September 2020. At the start of the autumn term, SARS-CoV-2 antibody positivity rates were significantly higher at 12.8% in students compared to 9.2% in staff but similar at 13.1% and 13.4%, respectively at a median of 9.3 weeks later. Antibody seroprevalence rates in students and staff were generally similar to regional community rates, both at the start and end of the Autumn term, albeit with wide confidence intervals. Among participants who were seronegative at the start of the autumn term, seroconversion rates were 6.6% in students and 8.7% in staff by the end of term. Seroconversion was significantly associated with the number of positive cases in school during the autumn term. Around 33.3% of students who seroconverted reported COVID-19 symptoms compared to 76.4% among staff (p < 0.001).
The UK experience following full reopening of all school years in the autumn term was different to the partial reopening of some primary and secondary school years in the previous summer mini-term [7]. Nationally, SARS-CoV-2 infection rates were higher across all age-groups including children, and there were more infections and outbreaks reported in educational settings during the autumn term [9,19]. Using the same methodology in primary schools, the SARS-CoV-2 antibody seroconversion rate was 5% among staff and students [20], and a lower proportion of primary schools than secondary schools experienced a COVID-19 outbreak during the first half of the autumn term.
An important question to consider is whether the infections occur within or outside the school premises. We have consistently found that SARS-CoV-2 infection rates in school-aged children correlated with local community infection rates in adults, during periods of high and low community infection prevalence, during school holidays and after partial and full reopening of schools in England [7,9]. During the summer months, when schools were closed, older teenagers and young adults had some of the highest SARS-CoV-2 infection rates in England [9]. In the current surveillance, too, we observed high infection and antibody seropositivity rates among secondary school students at the start of the autumn term, indicating that they had acquired the infection in the community. Higher community infection rates allow more opportunities for virus introduction into educational settings.
The reopening of schools, especially full reopening of all school years, will increase the risk of SARS-CoV-2 infection, because of increased person-to-person contact inside and outside school premises (public transport, families gathering during school drop-offs and pick-ups, etc.), which in-turn will have a small but measurable impact on the reproduction number for SARS-CoV-2 [21]. There is, however, increasing evidence that the risk of SARS-CoV-2 transmission within school premises is very low, [22–24] especially among students [19]. In North Carolina, for example, surveillance of 11 school districts with more than 90,000 students and staff attending school in-person for 9 weeks, found 773 community-acquired SARS-CoV-2 infections, while contact tracing found only 32 additional infections that were acquired within school [24]. Among 17 rural Wisconsin schools, too, COVID-19 incidence among 4,876 students and 654 staff members during August 31–November 29, 2020, was lower (3,453 cases per 100,000) than in the county overall (5,466 per 100,000) [23]. Of the 191 cases identified in students and staff members, only seven (3.7%), all among students, were linked to in-school spread [23]. In New York City, COVID-19 prevalence in public schools was similar to or less than estimates of prevalence in the community for all weeks during October 9–December 18, 2020 [25]. Additionally, of 36,423 school-based close contacts, only 191 (0.5%) subsequently tested positive for COVID-19 and the likely index case was an adult for 78.0% of secondary cases [25]. Outside the US, public health investigations found that just over half the cases in secondary school clusters in the Netherlands were acquired outside school, mainly during intensive contact with friends or classmates in their free time, and most infections were restricted to small groups of students without affecting teachers [26]. These schools received extensive public health support including contact tracing but, without regular screening of staff and students, asymptomatic infection and silent transmission with school premises could not be ruled out.
Nonetheless, school staff and parents remain apprehensive about acquiring SARS-CoV-2 in school, especially from students who are more likely to have asymptomatic infection [27]. Indeed, 60% of staff and 36% of student Seroconverters believed they were infected with SARS-CoV-2 at school when asked. Additionally, in secondary schools was associated with the number of positive cases in school during the autumn term and, at the end of the term, seropositivity rates were similar among staff and students overall. Suggesting that at least some of the infections occurred inside school premises. That seroprevalence rates among staff and students were similar to local community infections rates, however, is reassuring because, if widespread silent transmission following asymptomatic infection was occurring in schools, then seropositivity and seroconversion rates would have been much higher than local community rates, as reported in up to two-thirds of residents and staff in care homes, irrespective of symptom status or PCR-positivity [28]. Other institutional settings including hospitals [29], prisons [30], and detention centres [31] have also reported much higher antibody seroprevalence rates during the current pandemic.
In secondary schools, we found no evidence of clustering of SARS-CoV-2 RT-PCR positive cases or seroconversions among staff or students, which would have indicated in-school transmission. Additionally, neither the size of the school or class, nor the proportion of students on free school meal (an indicator of socioeconomic status) were associated with seroconversion among staff or students. Reassuringly, too, recent analyses by the UK ONS also found that teachers were not at increased risk of COVID-19 or COVID-19 related deaths compared to other professions [32].
It is likely that, although implemented with varying success in the participating schools, the nationally-recommended infection control measures are helping control the spread of the virus inside school premises [6]. The contribution of the different infection control measures in preventing SARS-CoV-2 transmission is, however, not known and requires further study. In UK secondary schools, for examples, staff and students were only recommended to wear face coverings in communal areas outside the classroom during the autumn term [6]. Following the emergence of new SARS-CoV-2 variants of concern in December 2020, schools were closed as part of national lockdown and, when they reopened fully on 08 March 2021, additional measures were recommended, including twice-weekly rapid testing for staff and students and continuous use of face covering whilst in school premises [33,34].
The strength of this surveillance lies in the rapid recruitment of secondary schools to monitor SARS-CoV-2 infection and transmission as soon as they reopened after national lockdown in September 2020. There were some limitations. We only recruited schools in regions where we had paediatric investigation teams that were able to take blood samples from large numbers of staff and students. Our schools are, therefore, not intended to be representative of all secondary schools in England. In participating schools, we avoided recruiting some secondary school years with end-of-year national examinations to minimise disruption of their education, and, only a proportion of staff and students consented to taking part in sKIDsPLUS. We are also unable to comment on the transmissibility or disease severity of B.1.1.7 variant because schools were closed as part of national lockdown in mid-December as soon as cases started increasing and did not fully reopen until March 2020 when community SARS-CoV-2 infections rates were very low. Additionally, we used the Abbott platform to measure nucleoprotein antibodies, which develop quickly following infection but then wanes faster over time than spike protein antibodies. As a result, some participants infected with SARS-CoV-2 early in the pandemic may have seroreverted using our selected antibody assay platform. Caution must be taken when comparing with regional antibody seroprevalence in the ONS Coronavirus Infection Survey, which tested for spike antibodies. Finally, as already discussed, we were unable to assess whether the confirmed infections occurred within or outside the school premises. We are currently conducting a larger national School Infection Survey (SIS) involving 150 schools across England during the 2020/21 academic year [35]. This survey will also include outbreak investigations to better understand infection and transmission within educational settings.
SARS-CoV-2 infection and seroconversion rates were higher in secondary compared to primary school students following the full reopening of all schools in England, but lower than other institutional settings, likely because of the infection control measures that have been implemented in educational settings. Keeping schools open must remain a top priority for all countries and maintaining low community infection rates is critical for reducing opportunities for virus introduction into educational settings.
The UK commitment to vaccinate all adults means that all school staff and all parents will have been offered a COVID-19 vaccine before the start of the 2021/22 academic year in September 2021. This will not only help maintain low community infection rates down but also protect both these groups should they be exposed to the virus. Whether children should also be vaccinated against COVID-19 is debatable and the UK, like any other country, will need to make a decision when a vaccine is licensed for <16 year-olds. In the meantime, ongoing surveillance in educational settings will be important for monitoring the impact of new variants in educational and other institutional settings.
Funding
This surveillance was funded by the Department of Health and Social Care (DHSC)
Data sharing statement
Applications for relevant anonymised data should be submitted to the Public Health England Office for Data Release. Any query on the study should be sent to the corresponding author.
Declaration of Competing Interest
MR reports that The Immunisation and Countermeasures Division has provided vaccine manufacturers with post-marketing surveillance reports on pneumococcal and meningococcal infection which the companies are required to submit to the UK Licensing authority in compliance with their Risk Management Strategy. A cost recovery charge is made for these reports. RB and EL reports other from GSK, other from Sanofi, other from Pfizer, outside the submitted work. JW reports grants from NIHR Health Protection Research Unit in Immunisation during the conduct of this study. MK reports grants from Gilead Sciences Inc, outside the submitted work. JG reports grants from Public Health England, during the conduct of the study. All other authors have nothing to declare.
Acknowledgments
The authors would like to thank the schools, headteachers, staff, families and their very brave children who took part in the sKIDsPLUS surveillance. The authors would also like to thank the staff in the Immunisation Department and in the Virus Reference Department (VRD) at PHE Colindale, as well as Sero-epidemiology Unit (SEU) at PHE Manchester for supporting the sKIDS surveillance.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.100948.
Appendix. Supplementary materials
References
- 1.European Centre For Disease Prevention and Control (ECDC). COVID-19 in children and the role of school settings in COVID-19 transmission. https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-schools-transmission-August%202020.pdf. Published 06 August 2020.
- 2.Levinson M, Cevik M, Lipsitch M. Reopening primary schools during the pandemic. N Engl J Med. 2020 doi: 10.1101/2020.07.19.20157362. 2020 Jul 24;2020.07.19.20157362Preprint. [DOI] [PubMed] [Google Scholar]
- 3.Viner RM, Russell SJ, Croker H. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4(5):397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prime Minister's Office. Prime Minister's statement on coronavirus (COVID-19): 23 March 2020. https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020. Published 23 March 2020. Accessed 05 August 2020.
- 5.Public Health England (PHE). Weekly Coronavirus Disease 2019 (COVID-19) Surveillance Report: summary of COVID-19 surveillance systems. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/880925/COVID19_Epidemiological_Summary_w17.pdf. Published 2020.
- 6.Department for Education (Dfe). Guidance for full opening: schools. https://www.gov.uk/government/publications/actions-for-schools-during-the-coronavirus-outbreak/guidance-for-full-opening-schools Published 27 July 2020. Accessed 05 August 2020.
- 7.Ismail S, Saliba V, Lopez-Bernal J, Ramsay M, Ladhani S. SARS-CoV-2 infection and transmission in educational settings: cross-sectional analysis of clusters and outbreaks in England. Lancet Infect Dis. 2020;8:S1473–S3099. doi: 10.1016/S1473-3099(20)30882-3. Dec(20)30882-3. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viner RM, Bonell C, Drake L. Reopening schools during the COVID-19 pandemic: governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Arch Dis Child. 2021;106:111–113. doi: 10.1136/archdischild-2020-319963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mensah A, Sinnathamby M, Zaidi A. SARS-CoV-2 infections in children following the full re-opening of schools and the impact of national lockdown: prospective, national observational cohort surveillance, July-December 2020, England. J Infect. 2021 doi: 10.1016/j.jinf.2021.02.022. (online ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fontanet A, Tondeur L, Madec Y. Cluster of COVID-19 in northern France: a retrospective closed cohort study. MedRxiv. 2020 doi: 10.1101/2020.04.18.20071134. [DOI] [Google Scholar]
- 11.Fontanet A, Grant R, Tondeur L. SARS-CoV-2 infection in primary schools in northern France: a retrospective cohort study Inan area of high transmission. MexRxIV. 2020 doi: 10.1101/2020.06.25.20140178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stein-Zamir C, Abramson N, Shoob H. A large COVID-19 outbreak in a high school 10 days after schools' reopening, Israel, May 2020. Euro Surveill. 2020;25(29) doi: 10.2807/1560-7917.ES.2020.25.29.2001352. 2001310.2002807/2001560-2007917.ES.2002020. 2001325.2001329.2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ladhani SN, Amin-Chowdhury Z, Amirthalingam G, Demirjian A, Ramsay ME. Prioritising paediatric surveillance during the COVID-19 pandemic. Arch Dis Child. 2020;105(7):613–615. doi: 10.1136/archdischild-2020-319363. [DOI] [PubMed] [Google Scholar]
- 14.Niu P, Liu R, Zhao L. Three novel real-time RT-PCR assays for detection of COVID-19 virus. China CDC Wkly. 2020;2(25):453–457. doi: 10.46234/ccdcw2020.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corman VM, Landt O, Kaiser M. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. pii=2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Public Health England (PHE). Evaluation of the Abbott SARS-CoV-2 IgG for the detection of anti-SARS-CoV-2 antibodies. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/890566/Evaluation_of_Abbott_SARS_CoV_2_IgG_PHE.pdf. Published 08 June 2020.
- 17.Office for National Statistics (ONS). Coronavirus (COVID-19) infection survey. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/coronaviruscovid19infectionsurveydata. Published 2020. Accessed February 07, 2021.
- 18.Office for National Statistics (ONS). Coronavirus (COVID-19) Infection Survey, antibody data for the UK: 16 March 2021. (data from 17 September to 14 October 2020 and 10 December 2020 to 6 January 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19infectionsurveyantibodydatafortheuk/latest. Published 2021. Accessed 15 March 2021, 2021.
- 19.Aiano F, Mensah A, McOwat K. COVID-19 outbreaks following full reopening of primary and secondary schools in England: cross-sectional national surveillance, November 2020. Lancet Eur. 2021;6:100120. doi: 10.1016/j.lanepe.2021.100120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ladhani S, Baawuah F, Beckmann J. Prospective active National surveillance of preschools and primary schools for SARS-CoV-2 Infection and transmission in England, June 2020. Lancet Child Adolesc Health. 2021 doi: 10.2139/ssrn.3764198. 2020 (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y, Campbell H, Kulkarni D. The temporal association of introducing and lifting non-pharmaceutical interventions with the time-varying reproduction number (R) of SARS-CoV-2: a modelling study across 131 countries. Lancet Infect Dis. 2021;21(2):193–202. doi: 10.1016/S1473-3099(20)30785-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Macartney K, Quinn HE, Pillsbury AJ. Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child Adolesc Health. 2020;4(11):807–816. doi: 10.1016/S2352-4642(20)30251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Falk A, Benda A, Falk P, Steffen S, Wallace Z, Hoeg TB. COVID-19 cases and transmission in 17 K-12 schools - Wood County, Wisconsin, August 31-November 29, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(4):136–140. doi: 10.15585/mmwr.mm7004e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zimmerman KO, Akinboyo IC, Brookhart MA. Incidence and secondary transmission of SARS-CoV-2 infections in schools for the abc science collaborative. Pediatrics. 2021;147(4) doi: 10.1542/peds.2020-048090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varma JK, Thamkittikasem J, Whittemore K. COVID-19 infections among students and staff in New York City public schools. Pediatrics. 2021 doi: 10.1542/peds.2021-050605. March 2021Online ahead of Print. [DOI] [PubMed] [Google Scholar]
- 26.National Institute for Public Health and the Environment (RIVM) TN. Children and COVID-19. https://www.rivm.nl/en/novel-coronavirus-covid-19/children-and-covid-19. Published 2020.
- 27.Viner RM, Mytton OT, Bonell C. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr. 2021;175(2):143–156. doi: 10.1001/jamapediatrics.2020.4573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ladhani SN, Jeffery-Smith A, Patel M. High prevalence of SARS-CoV-2 antibodies in care homes affected by COVID-19: prospective cohort study, England. EClinicalMedicine. 2020;28 doi: 10.1016/j.eclinm.2020.100597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martyn E.M., Whitaker H, Gil E. Disproportionate impact of SARS-CoV-2 on ethnic minority and frontline healthcare workers: a cross-sectional seroprevalence survey at a North London hospital. J Infect. 2021;82(6):276–316. doi: 10.1016/j.jinf.2021.02.027. Epub 2021 Mar 4. PMID: 33676961; PMCID: PMC7930734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan J, Burke K., Bedard R. COVID-19 in the New York City jail system: epidemiology and health care response, March-April 2020. Public Health Rep. 2021;136(3):375–383. doi: 10.1177/0033354921999385. 2021:33354921999385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Openshaw JJ, Travassos MA. COVID-19 outbreaks in U.S. immigrant detention centers: the urgent need to adopt CDC guidelines for prevention and evaluation. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Office for National Statistics. Coronavirus (COVID-19) related deaths by occupation, England and Wales: deaths registered up to and including 20 April 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/coronaviruscovid19relateddeathsbyoccupationenglandandwales/deathsregistereduptoandincluding20april2020. Published 2020.
- 33.Department for Education (DfE). Guidance: Coronavirus (COVID-19) asymptomatic testing in schools and colleges. https://www.gov.uk/government/publications/coronavirus-covid-19-asymptomatic-testing-in-schools-and-colleges/coronavirus-covid-19-asymptomatic-testing-in-schools-and-colleges. Published 15 december 2020. Accessed 18 December, 2020.
- 34.Department for Education (DfE). Schools coronavirus (COVID-19) operational guidance, February 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/964351/Schools_coronavirus_operational_guidance.pdf. Published 2021. Accessed 01 February 2021, 2021.
- 35.Office for National Statistics (ONS). COVID-19 schools infection survey round 1, England: November 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/covid19schoolsinfectionsurveyround1england/november2020 Published 17 December 2020. Accessed 22 December 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.