Abstract
In the central nervous system, immunologic surveillance and response are carried out, in large part, by microglia. These resident macrophages derive from myeloid precursors in the embryonic yolk sac, migrating to the brain and eventually populating local tissue prior to blood-brain barrier formation. Preserved for the duration of lifespan, microglia serve the host as more than just a central arm of innate immunity, also contributing significantly to the development and maintenance of neurons and neural networks, as well as neuroregeneration. The critical nature of these varied functions makes the characterization of key roles played by microglia in neurodegenerative disorders, especially Alzheimer’s disease, of paramount importance. While genetic models and rudimentary pharmacologic approaches for microglial manipulation have greatly improved our understanding of central nervous system health and disease, significant advances in the selective and near complete in vitro and in vivo depletion of microglia for neuroscience application continue to push the boundaries of research. Here we discuss the research efficacy and utility of various microglial depletion strategies, including the highly effective CSF1R inhibitor models, noteworthy insights into the relationship between microglia and neurodegeneration, and the potential for therapeutic repurposing of microglial depletion and repopulation.
Keywords: Alzheimer's disease, clodronate liposomes, CSF1R, depletion, microglia, neurodegeneration, neuroregeneration, repopulation
Microglia in Health and Disease
The brain is often described as immune privileged, functionally protected from cellular and noncellular effectors of peripheral immunity. This mixed blessing is assumed to result from a number of unique tissue characteristics, including the highly restrictive blood-brain barrier, a lack of typical lymphatic vessels, and a purported finite army of only moderately efficient antigen presenting cells, the microglia (reviewed in Forrester et al., 2018). These resident macrophages serve as the tissue-specific arm of innate immunity in the central nervous system (CNS), tirelessly surveilling the parenchyma for potential injury, insult, or infection. As sentinels, microglia are able to recognize a myriad of environmental threats via an array of cell-surface receptors, including but not limited to complement and FC receptors (link microglia to acellular effectors of the innate and adaptive immune systems) (Lunnon et al., 2011; reviewed in Crehan et al., 2012), scavenger receptors (a structurally diverse family of receptors that mediate the uptake of endogenous proteins and lipids, as well as various pathogens) (reviewed in Wilkinson and El Khoury, 2012), and the toll-like receptors (so-called pathogen-associated molecular pattern receptors that bind evolutionary conserved molecules on pathogens) (reviewed in Su et al., 2016). Following threat detection, microglia undergo rapid morphologic and physiologic transformation, initiating a number of canonical responses that lead to pathogen neutralization and clearance (Stopper et al., 2018). Importantly, such inflammatory responses are not intrinsically deleterious, and microglia cycle through both pro- and anti-inflammatory states, creating a balance that ultimately benefits the host. However, exacerbated or protracted pro-inflammatory responses, or diminished anti-inflammatory activities, can drive disequilibrium and disruption of these precisely orchestrated processes, resulting in neuron dysfunction and cell death, in addition to other neuropathologic outcomes. Indeed, this so-called neuroinflammation is thought to contribute to the pathogenesis of many neurodegenerative disorders, including Alzheimer’s disease (AD) (reviewed in Streit et al., 2004).
Microglia serve as much more than just local protection, however, also acting as key cellular regulators of CNS homeostasis, providing direct support to neurons and assisting in the formation and maintenance of the expansive neural networks that drive nervous system function (reviewed in Pósfai et al., 2019). To this end, microglia play an integral role in neurodevelopment, helping to orchestrate the complex and highly dynamic processes of synapse formation, elimination, and remodeling, ultimately contributing to memory formation, memory extinction, and synaptic plasticity (Parkhurst et al., 2013; Nguyen et al., 2020; Wang et al., 2020a). These activities persist throughout the entirety of an organism’s life span as microglia tirelessly prune and refine synapses (reviewed in Cowan and Petri, 2018). Not surprisingly, however, microglial dysfunction has been implicated in a number of neurological disorders characterized by disruption to neurodevelopmental, disequilibrium of neural networks, and the eventual degeneration of neurons themselves (reviewed in Chung et al., 2015).
These diverse yet often subtle roles played by microglia in health and disease have presented noteworthy challenges to studying their overall station in brain. Moreover, overlapping functions with other supportive CNS cells, as well as numerous indistinguishable similarities to monocyte-derived macrophages crossing over from the periphery, have further complicated experimental inquiries. Over the last decade, simple experimental approaches have been developed that efficiently and effectively eliminate microglia from the adult rodent brain, thereby allowing for more detailed interrogation of microglial functions in-vivo. These so-called microglial depletion studies have so far helped to fill gaps in our understanding of both basic and more complex microglial biology, and may even offer much needed therapeutic opportunities for neurodegenerative diseases, as well as other CNS damage or dysfunction. Here we review the most effective methodologies, the value of these depletion strategies for deciphering microglial function under both healthy and pathologic conditions, and the realistic potential. We begin by briefly discussing microglia. Specifically, this review will cover the current literature on microglia and AD and use this as an example on the method of microglia depletion methodology, but other ailments will also be discussed.
Search Strategy
For the present review, we searched the literature published from the time periods of January 1, 2010–October 15, 2020 using keywords such as “microglia depletion and neurodegeneration” on PubMed and Google scholar. In addition, we also used modifications of the above main keywords to thoroughly search the literature. The major inclusion criteria preferred the literature comprising “microglia depletion.”
Depletion of Microglia
Experimental approaches used to characterize the broad functional repertoire of microglia in the context of health and diseases have relied on both pharmacologic and genetic methodologies. The high efficiency of pharmacology provided opportunity for identifying and effectively describing many of the rudimentary immunologic roles played by microglia in the CNS. For example, we now know that microglia serve as specialized sensors, continuously and skillfully surveilling brain parenchyma for any tissue damage or disruption (Nimmerjahn et al., 2005). In turn, damage- and pathogen-associated molecular patterns reproducibly activate microglia through interaction with cell-surface pattern recognition receptors, including members of the toll-like receptor family (Su et al., 2016). In addition, it is known that individual activation signatures commonly produce a number of simultaneous molecular outcomes, as is the case with stimulation of the purinergic ionotropic receptor, P2X7, which results in production of reactive oxygen species, synthesis and secretion of the cytokines interleukin-1β and interleukin-18, and increased phagocytosis (reviewed in Bhattacharya and Biber, 2016). Regardless, activated microglia exhibit polarization toward one of two recognizable macrophage phenotypes, M1 or M2, although that interpretation remains open for debate (reviewed in Ransohoff, 2016). Genetic approaches, especially transgenic animals, allowed for disruptive molecular targeting, leading to more precise definitions of these key functional elements, likewise improving our understanding of the diverse nature of microglial activities beyond simple tissue-specific immunity For instance, we now know that microglia control senile plaque formation in AD, in part through stimulation of the chemokine receptor CXCR3 (Krauthausen et al., 2015). They also influence developmental synaptic refinement through activation of TREM 2, a cell-surface triggering receptor and important genetic risk factor for AD involved in microglial migration, proliferation, and viability (Mazaheri et al., 2017). And of particular interest, microglia regulate synaptogenesis and developmental apoptosis of neurons in brain through release of growth factors, including nerve growth factor and brain-derived neurotrophic factor (reviewed in Bessis et al., 2007 and Reemst et al., 2016). Still, these experimental approaches have been necessarily limiting, allowing for the dissection of microglial function one molecular piece at a time, but unable to fully appreciate the finished puzzle (Heppner et al., 2005; Goldmann et al., 2013). The first genetic strategies for microglial depletion, including models based on Cd11b-HSVTK and diptheria toxin, presented significant challenges, including only short-lived depletion, cognitive impairments, BBB compromise, side effects associated with the inducers tamoxifen and ganciclovir, among other deficits. Genetic models now offer greatly improved temporal, spatial, and target manipulation of microglia with noteworthy examples including CX3CR1CreER/+:Csf1rFlox/Flox, Csf1rΔFIRE/ΔFIRE, Csf1r–/–, and Sall1creER/+ Csf1rflox/flox (reviewed in Green et al., 2020; Wu et al., 2020). Yet even as such models offer advanced precision and indefinite depletion, they require thoughful, time-consuming genetic crossing, and cannot be extrapolated to human use.
Microglial depletion synchronously ablates this entire catalogue of functions, providing a more holistic lens through which to study these complicated relationships. Two unique pharmacologic strategies for elimination of parenchymal microglia have so far been optimized, each taking advantage of unique microglial characteristics. The first attempts to deplete microglial populations exploited clodronate, a well-studied drug of the bisphosphonate class used clinically to treat disorders of dysfunctional bone metabolism, including hypercalcemia caused by excessive bone resorption, osteolytic bone metastases, and hyperparathyroidism (reviewed in Frediani and Bertoldi, 2015). When packaged in liposomes, clodronate is rapidly taken up by phagocytic cells where it induces apoptosis. Therefore, the selectivity of liposomes (phagocytes) and their route of administration (intracerebroventricular) have the potential to provide target specificity for microglia in the CNS, respectively (Lee et al., 2012; Asai et al., 2015). Indeed, administration of clodronate liposomes (Clo-Lip) does not specifically deplete microglia, but instead ablates most circulating and tissue-specific macrophages, including but not limited to alveolar (Gonzalez et al., 2007), testicular (Bergh et al., 1993), and colon derived macrophages (Kruse et al., 2013). Further, this pharmacologic method relies on central administration of Clo-Lip via stereotaxic intracerebral or intracerebroventricular injection, and exhibits reduced duration of depletion, making longitudinal investigations especially prohibitive since multiple clodronate doses would be required over the course of a single study (reviewed in Rooijen and Sanders, 1994; Serrats et al., 2010; Han et al., 2019a). Use of Clo-Lip can also result in significant molecular consequences, including impairment of vascular integrity, disruption of ATP metabolism in neurons, and robust upregulation of proinflammatory molecules (Han et al., 2019b), factors that make the prospect of therapeutic application in humans untenable. Interestingly, prior to in vivo studies, liposome-mediated clodronate delivery was used in vitro to eliminate contaminating microglia from primary mixed glial cultures (Kumamaru et al., 2012), as well as ex vivo to deplete microglia in an organotypic hippocampal culture model of excitotoxicity (Vinet et al., 2012). The second, and far superior, depletion strategy exploits CSF1R, a constituent of the quantitative transcriptome in adult murine microglia, confirming genetic overlap with peripheral macrophages (Elmore et al., 2014). Development and survival of CD45+/c-Kit–/CX3CR1+ macrophages from the embryonic yolk sac, cells that eventually migrate to the brain to become microglia, depend on CSF1R and its cognate ligand, CSF-1 (Erblich et al., 2011; Nandi et al., 2012; Elmore et al., 2014). Several small molecule inhibitors of CSF1R have been developed that effectively block receptor activation and downstream signaling, resulting in ablation of greater than 99% of microglia in treated mice (Elmore et al., 2014). The extremely high efficacy of CSFR1 inhibitors, especially PLX5622, PLX3397, and GW2580 (Figure 1), combined with the use of simple experimental designs (no requirement for responsive transgenic animals), establishes this technique as the preferred experimental method over clodronate-loaded liposomes or complicated genetic models. However, recent reports call into question the microglial selectivity of CSF1R inhibitors, particularly PLX5622, observing suppression of both circulating and tissue-specific macrophages (e.g. lung and liver) that persisted for weeks after treatment (Lei et al., 2020). The authors also noted that bone marrow-derived macrophages exhibited impaired phagocytosis and cytokine response following LPS challenge (Lei et al., 2020). While these findings support additional review of remaining CSF1R inhibitor specificity and selectivity, these compounds have allowed for unparalleled interrogation of critical microglial functions in both health and disease. It is worth noting that although the utility of genetic models is largely overshadowed by CSF1R inhibitors, and even Clo-Lip approaches, they do offer superior specificity and selectivity. Here we review recent work in neurodegeneration that specifically utilize various microglial depletion strategies for investigation.
Figure 1.
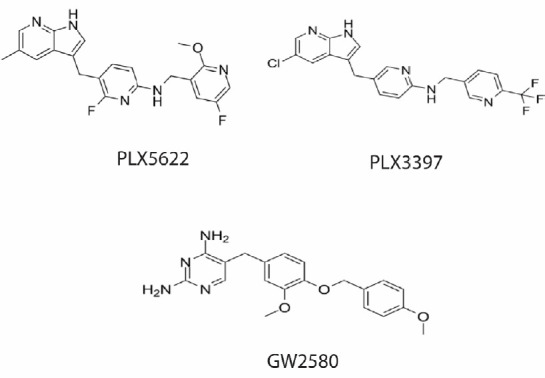
Structures of commonly used CSF1R small molecule inhibitors.
The Role of Microglia in Alzheimer’s Disease and Other Neurodegenerative Disorders
As a group, neurodegenerative diseases are characterized by loss of neuron function and connectivity, frequently resulting in cell death. One of the most studied and appreciated examples is AD, a slowly progressive, incurable neurodegenerative disorder of the aged that presents clinically with select memory loss and dementia (reviewed in Masters et al., 2015). Affected brains exhibit abnormal accumulation of extracellular amyloid-containing senile plaques, as well as intracellular neurofibrillary tangles composed of the hyperphosphorylated microtubule-associated tau protein (reviewed in Masters et al., 2015). In addition, reactivate microglia associate with AD lesions, evidence of failed attempts to stave off or reverse the harmful effects of these neurotoxic peptides. This arrested pro-inflammatory state is thought to appear during prodromal stages of AD and persist through advanced disease. Although well intentioned, this so-called neuroinflammation significantly impairs normal microglial functions leading to tissue damage, and in this way may facilitate AD pathophysiology. However, the exact role played by microglia remains incompletely understood and therefore represents a critical line of investigation. Given the substantial evidence supporting this, an attempt to elucidate the roles of microglia in AD pathogenesis is crucial. Additionally, the purported long lifespan of microglia makes them a potentially valuable therapeutic target for treatment of age-dependent brain diseases like AD (Additional Box 1 (64.4KB, pdf) ).
Evidence to date identifies microglia as key players in the maintenance of senile plaques in AD (Olmos-Alonso et al., 2016). Microglial depletion using the inhibitor PLX5622 was recently shown to impair plaque formation and significantly limit the number of dystrophic neurites developed in 5xFAD mice, a transgenic line that reproduces many of the pathologic features of AD (Spangenberg et al., 2019). Interestingly, subsequent repopulation of microglia resulted in the reseeding of amyloid plaques to the same extent as untreated age-matched controls. Importantly, depletion did not appear to alter amyloid precursor protein processing or amyloid levels in 5xFAD mice, although a shift in amyloid localization from brain parenchyma to vasculature was observed, suggesting an attempt at vascular clearance. Interestingly, RNA-seq analysis found no significant alterations in the expression of AD-risk genes (e.g. Ache, Ptk2b) to explain the microglia-dependent changes. These findings support the theory that microglia are able to adopt deleterious phenotypes that have the potential to promote the pathophysiology of neurodegenerative diseases. Moreover, it appears likely that activated pre-depleted pools produce an inflammatory environment sufficiently persistent to rapidly activate repopulating pools, thereby conferring neuroinflammatory behaviors to new cells. These results were independently confirmed with the PLX3397 inhibitor which significantly reduced fibrillar and pre-fibrillar oligomers, as well as intracellular amyloid deposition and neuritic plaques (Sosna et al., 2018). Specifically, the authors reported marked reductions in soluble fibrillar oligomers in brain and pre-fibrillar oligomers in plasma from 5XFAD mice. In addition, the study found that microglial depletion was associated with improved cognitive performance on fear conditioning tests, behavioral outcomes likewise supported by Ortega-Martinez and colleagues in transgenic mice expressing either FAD-linked PS1 or PS1M146V/+ and treated with PLX5622 (Ortega-Martinez et al., 2019). Moreover, microglial depletion rescued proliferation, differentiation, and survival of adult hippocampal neural progenitor cells using an environmentally enriched paradigm, conditions normally predicted to cause deficits in PS1 mice. Of special note, while microglial depletion in other amyloid models successfully prevented neuron loss (Fuhrmann et al., 2010) and cognitive improvement (Dagher et al., 2015), the number of plaques remained unchanged. Even more intriguing, data from one study suggests that microglia may act to stabilize plaque size, thereby restricting plaque growth and subsequent synaptic loss (Zhao et al., 2017). Importantly, the study used a Cx3CR1-iDTR transgenic model to deplete microglia, and analyzed plaque burden using only Congo-red (e.g. no confirmatory thioflavin S fluorescent staining) rather than a more robust ELISA assay. Collectively, these findings suggest both beneficial and detrimental roles for microglia in AD, although differences in transgenic mice, depletion, and experimental design (especially timing) may account for the contradictory observations.
AD is also pathologically characterized by formation of intraneuronal neurofibrillary tangles composed of aggregated bundles of hyperphosphorylated tau. In addition to AD, abnormal metabolism of tau in neurons and glia is associated with neurodegenerative diseases that include frontotemporal dementia, chronic traumatic encephalopathy, and even posttraumatic stress disorder, making continued research in this area broadly relevant (reviewed in Spillantini and Goedert, 2013). Depletion studies in murine tauopathy models have likewise shed light on the role of microglia in AD. For example, misfolded microtubule-associated protein tau is known to leak into the extracellular environment, whether purged from affected neurons as a protective measure or released from dying cells (reviewed in Perea et al., 2018). Once in the interstitium, tau pathology propagates throughout the brain with a stereotypic pattern that correlates with specific cognitive decline (reviewed in Graykowski et al., 2020). One study found that microglia contribute to this pathologic spread by phagocytosing tau, packaging it into exosomes, and then releasing it where it can be taken up and neutralized by neighboring cells (Asai et al., 2015). They also reported significant reduction in tau propagation following microglial depletion in mice treated with either a CSF1R inhibitor or intracerebroventricular administration of clodronate liposomes, presumably through reduced phagocytosis and secretion of tau-containing exosomes. Others groups have observed similar results using tau P301S transgenic mice (Mancuso et al., 2019). Interestingly, this study utilized a less common CSF1R inhibitor, JNJ-52, and found reduced production of pro-inflammatory molecules, as well as significantly decreased tau phosphorylation at AT8 sites and insoluble tau levels. As with microglial and amyloid studies, variations in selected animal models and depletion strategies have complicated broader interpretations of the exact relationship between microglia and tauopathies, justifying additional investigation. Of course, even in light of compelling evidence for the attenuation of tau pathology by microglia, some have suggested that microglial depletion does little to mitigate tau pathology in AD (Bennett et al., 2018). Surprisingly, this study found that PLX3397 administration resulted in a roughly 30% reduction of microglia, compared to the near 99% depletion achieved by the majority of groups using CSF1R inhibitors. Consequently, they found that in Tg4510 transgenic mice, microglial depletion did not impact tau burden, levels or phosphorylation status, and did not result in changes to disease-associated microglial transcripts (e.g. Trem2). Nevertheless, as with current literature regarding the relationship between microglial depletion and amyloid burden, more studies are needed.
Likewise, depletion strategies have proven useful in deciphering the role of microglia in other neurodegenerative disorders. MS is a demyelinating, neuroinflammatory disease of the CNS characterized by disease-associated microglia (DAM), although their precise pathologic contributions remain ambiguous. To this end, CSF1R inhibitors have been used in experimental autoimmune encephalomyelitis (EAE) mice, a widely accepted animal model of MS, to study the contribution of microglia to disease progression. For example, Nissen and colleagues found that weight loss and mobility impairments were mitigated, and myelination and immune activation showed marked improvement, in EAE mice treated with PLX5622 (Nissen et al., 2018). Interestingly, the authors identified a shift in inflammatory phenotype (e.g. decreased iNOS-positive microglia), reduced spinal cord demyelination, and an increase in mature oligodendrocyte. It is important to note that previous studies in EAE found that microglial ablation by genetic means significantly reduced disease progression (Heppner et al., 2005; Mildner et al., 2009). However, a group investigating secondary progressive multiple sclerosis utilizing EAE mice found that microglial depletion following PLX3397 administration actually led to a worsening of disease characterized by exacerbated demyelination, inflammation, axonal degeneration, CD4+ T cell proliferation, and increased mortality (Tanabe et al., 2019). As with the AD studies cited herein, these incongruous results suggest that microglia have the capacity to play both neuroprotective and neurodegenerative roles in MS, supporting the need for additional inquiry. Indeed, similarly paradoxical results have also been reported for depletion studies conducted in models of traumatic brain injury (TBI).
TBI is defined by a heterogenous set of clinical outcomes, and represents a major cause of death and disability (reviewed in Blennow et al., 2016). Not surprisingly, chronically activated disease-associated microglia are an important pathologic hallmark of TBI as well, with the resulting neuroinflammation thought to promote neurodegeneration (reviewed in Donat et al., 2017). For example, increased neurodegeneration was observed with intracerebroventricular administration of clodronate-loaded liposomes following closed head injury in neonatal rats, a model of pediatric brain injury, which the authors attribute to decreased clearance of dying cells (Hanlon et al., 2019). Interestingly, another group found that intravenous administered of clodronate liposomes prior to closed cortical impact (CCI) injury in adult rats increased blood-brain barrier permeability (Aertker et al., 2019). In regard to these findings, it is important to note the relative timing of depletion, as well as its systemic nature, effectively ablating monocytes, macrophages, and microglia, and therefore requiring a more thoughtful interpretation of the interaction between peripheral and central responders to injury. The higher efficacy, small-molecule CSF1R inhibitors have also been used in similar TBI studies, and as with models of AD and MS, results have been largely inconsistent. An imaging study found that pre-CCI administration of PLX5622 successfully prevented injury-induced deficits in cerebral energetic metabolism as measured by hyperpolarized [1-13C] lactate-to-pyruvate ratios and pyruvate dehydrogenase activity (Guglielmetti et al., 2017). Unfortunately, in the absence of corresponding pathologic or behavioral data, it is difficult to translate these findings to the greater body of depletion studies. A recent study from Willis et al. (2020) found that sustained pre-injury microglial depletion achieved by continuous PLX5622 administration had no appreciable effect on spatial learning and memory deficits, or hippocampal neurogenesis, typically seen with rodent CCI models. The authors, however, did find that repopulation of microglia attenuated TBI-induced spatial learning and memory deficits, as well as stimulated interleukin-6-dependent functional neurogenesis in the hippocampus following injury. Another group partially substantiated these results, finding that depletion of chronically active microglia with PLX5622 administration allowed for a pool of less reactive, ramified microglia to repopulate the injured brain during a critical period of neurodegeneration, reducing neuroinflammation, neuronal death, and small cortical lesions (Henry et al., 2020). Together, these studies highlight the potential value of microglial depletion and repopulation as a powerful therapeutic strategy for treatment of TBI, and possible other neurodegenerative diseases.
While similar depletion approaches have been used to investigate the involvement of microglia in the pathophysiology of other neurodegenerative disorders, including Parkinson’s disease (Yang et al., 2018; Neal et al., 2020; Oh et al., 2020) and amyotrophic lateral sclerosis (Lee et al., 2012; Martínez-Muriana et al., 2016), existing literature is sparse and more research is needed.
That being said, pharmacologic depletion and repopulation of microglia as both research tools and potential therapeutic interventions are not strictly limited to neurodegenerative diseases, as other maladies of the CNS may benefit. Indeed, exciting data has been generated from models of stroke (Szalay et al., 2016; Otxoa-de-Amezaga et al., 2019), depression (Cai et al., 2020; Wang et al., 2020b; Zhang et al., 2020), epilepsy (Feng et al., 2019; Liu et al., 2020), spinal cord injury (Gerber et al., 2018), glioblastoma (Butowski et al., 2016) and retinal degeneration (Zhang et al., 2018), among others.
Therapeutic Potential of Microglial Repopulation
While work investigating the effects of microglial depletion on models of neurodegeneration has vastly expanded our understanding and appreciation of the myriad functions served by microglia in health and disease, evidence for the benefits of their repopulation in brain may be cause for greater excitement. Only recently have studies begun to parse the cellular mechanisms that drive and shape repopulated tissue (Zhang et al., 2018; Zhan et al., 2019), as well as explore relevant therapeutic potential, and yet the work that has been done looks to be the start of a very compelling story. Importantly, microglial depletion in the living animal has thus far proven safe for the host, with no observed disruption to normal brain functions (Willis et al., 2020). In addition, depletion efficacy in the CNS commonly exceeds 99%, followed by rapid and complete repopulation (Elmore et al., 2014; Bruttger et al., 2015; Yao et al., 2016). Here, it is worth noting that, as a group, CSF1R inhibitors have been shown to be the most effective depletion approach, with PLX5622 in particular displaying the highest potency and selectivity (Liu et al., 2019). Especially relevant, these compounds show efficacy in rodents as well as nonhuman primates (Hillmer et al., 2017). Given the discussion thus far, the evidence regarding the potential therapeutic value of microglial repopulation is understandably mixed. One study found depletion and repopulation of microglia in adult wild type mice associated with changes in the brain microenvironment, activating astrocytes, and decreasing neuronal markers and blood vessel integrity (Han et al., 2019a). Similarly, repopulation of microglia following depletion in adult, aged mice gave rise to a nacent pool of cells that still responded to immune challenge with the same hyperactivation of their predecessors (O’Neil et al., 2018). It has also been noted that repopulation effectiveness in the adult rodent brain is dependent on the extent of microglial depletion, and that repeated repopulation decreases efficiency (Najafi et al., 2018). However, even though selective depletion from the hippocampus in wild type mice, or systemic elimination, were shown to alter performance on certain learning and memory tasks, and disrupt social behaviors, microglial repopulation completely restored observed deficits (Torres et al., 2016). In organotypic hippocampal slice culture, repopulation helped to temper subsequent proinflammatory responses, with tissue exhibiting reduced responsivity to a variety of inflammagens (Coleman et al., 2020), and in wild type mice repopulation resolved neuroinflammation and facilitated recovery after neuron loss (Rice et al., 2017). Repopulating microglia were even shown to play a beneficial role in a model of severe sepsis, helping to restore systemic inflammatory balance (Michels et al., 2019). Moreover, microglial depletion and repopulation reversed age-related alterations to hippocampal architecture, among other deficits, and increased neurogenesis and dendritic spine densities (Elmore et al., 2018). A variety of disease states also appear to improve with microglial repopulation. One group found that pro-inflammatory microglia associated with neurodegenerative environments can undergo necroptosis, a form of programmed inflammatory cell death, thereby creating a niche for regenerated microglia capable of remyelinating damaged neurons in a type-1 IFN signaling-dependent manner (Lloyd et al., 2019). In the SOD1G93A mouse model of ALS, repopulation of microglia is able to slow disease progression and extend lifespan (Lee et al., 2012). Notably, this study repopulated microglia through bone marrow repopulation and found that mSOD1 levels were reduced in the newly populated microglial pool. And as mentioned previously, repopulation of microglia significantly improved outcomes following CCI (Willis et al., 2020).
These and other studies provide strong support for continued investigation into the development of neurodegenerative therapies based on the microglial depletion and repopulation methods described here. However, additional lines of inquiry remain, with basic questions still requiring answers. For example, more work is needed to evaluate the effects of latency to repopulation, or duration of microglial depletion, on therapeutic efficacy. In addition, if prospective treatment regimens necessitate long-term microglial depletion, then consideration must be given to the potentially confounding effects of protracted absence of microglia on an already pathologic environment. It will also be important to thoroughly characterize repopulating pools of microglia, especially those determinants mediating pathogen recognition, healthy inflammatory response, and regeneration, so that preferred activities can be selectively stimulated and coordinated for maximum benefit.
The Future
The more we learn about microglia, the more we learn about the brain – the good and the bad – and the better positioned we are to move the science of CNS health and disease forward. As a research tool, microglial depletion will continue to serve as an important driver of scientific discovery in the field of neuroscience, especially given our, as yet, incomplete understanding of microglial biology and the diseases characterized by them. One interesting outcome from the development of depletion techniques is the potential to adapt these methodologies for the targeting of other cell types in the CNS. For example, astrocytes represent the most abundant cell in brain, and similar to microglia, are involved in both normal and pathologic processes (reviewed in Sofroniew and Vinters, 2010). Genetic depletion of astrocytes has been shown to cause rapid loss of neurons and consequential motor impairment resulting from imbalances in redox homeostasis (Schreiner et al., 2015). In Theiler’s murine encephalomyelitis, a virally-induced murine model of MS, ganciclovir-mediated depletion of astrocytes was shown to mitigate clinical symptoms with concomitant downregulation of pro-inflammatory molecules (Allnoch et al., 2019). As with the specific pharmacologic depletion methods discussed here, analogous strategies could be imagined for the efficient, discrete elimination of astrocytes or oligodendrocytes for subsequent study of glial biology.
The development of CSF1R inhibitors for selective depletion of microglia in brain also created the potential for future therapeutic intervention of neurodegenerative diseases. Although efficacy in human disease has yet to be achieved, work in both science and medicine press ahead. In 2016, it was reported that orally administered PLX3397 was well tolerated by study subjects and readily crossed the blood-brain barrier in an early phase clinical trial for GBM (Butowski et al., 2016). As above, in one form or another, the tools are available and more time is needed.
Conclusion
Microglia play a number of essential roles in both CNS health and disease, many more than the moniker of “resident macrophages of the brain” would suggest. A variety of microglial depletion techniques have provided exciting new opportunity to identify and study novel functions in vitro, ex vivo, and in vivo. Elimination of microglia in healthy animals has confirmed many of the housekeeping duties already ascribed to these cells, but also uncovered the broader impact that associated activities, especially those other than inflammatory, have on the host brain. In addition, mounting evidence from related studies strongly support microglia as critical regulators of neuron development and homeostasis, especially relating to neuroregeneration. The application of depletion strategies to rodent models of various neurodegenerative diseases has also significantly advanced our understanding of specific pathophysiology, and opened the door to potentially powerful therapeutic avenues. While more work is certainly needed to better define the molecular determinants that drive microglia toward friend or foe, as well as their value as therapeutic targets, microglial depletion shows great promise in the continued study of neurodegeneration and neuroregeneration in science and medicine.
Additional files:
Additional file 1 (81.2KB, pdf) : Open peer review report 1.
Additional Box 1 (64.4KB, pdf) : Life span and turnover of microglia.
Life span and turnover of microglia
Footnotes
Conflicts of interest: None.
Financial support: This work was supported by DePaul University grant URC450622 (to EC).
Copyright license agreement: The Copyright License Agreement has been signed by both authors before publication.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewer: David J. Loane, School of Biochemistry and Immunology, Trinity College, Ireland.
Funding: This work was supported by DePaul University grant URC450622 (to EC).
References
- 1.Aertker BM, Kumar A, Prabhakara KS, Smith P, Furman NET, Hasen X, Cox CS, Bedi SS. Pre-injury monocyte/macrophage depletion results in increased blood-brain barrier permeability after traumatic brain injury. J Neurosci Res. 2019;97:698–707. doi: 10.1002/jnr.24395. [DOI] [PubMed] [Google Scholar]
- 2.Allnoch L, Baumgärtner W, Hansmann F. Impact of astrocyte depletion upon inflammation and demyelination in a murine animal model of multiple sclerosis. Int J Mol Sci. 2019;20:3922. doi: 10.3390/ijms20163922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asai H, Ikezu S, Tsunoda S, Medalla M, Luebke J, Haydar T, Wolozin B, Butovsky O, Kügler S, Ikezu T. Depletion of microglia and inhibition of exosome synthesis halt tau propagation. Nat Neurosci. 2015;18:1584–1593. doi: 10.1038/nn.4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bennett RE, Bryant A, Hu M, Robbins AB, Hopp SC, Hyman BT. Partial reduction of microglia does not affect tau pathology in aged mice. J Neuroinflammation. 2018;15:311. doi: 10.1186/s12974-018-1348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergh A, Damber JE, van Rooijen N. The human chorionic gonadotrophin-induced inflammation-like response is enhanced in macrophage-depleted rat testes. J Endocrinol. 1993;136:415–420. doi: 10.1677/joe.0.1360415. [DOI] [PubMed] [Google Scholar]
- 6.Bessis A, Béchade C, Bernard D, Roumier A. Microglial control of neuronal death and synaptic properties. Glia. 2007;55:233–238. doi: 10.1002/glia.20459. [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharya A, Biber K. The microglial ATP-gated ion channel P2X7 as a CNS drug target. Glia. 2016;64:1772–1787. doi: 10.1002/glia.23001. [DOI] [PubMed] [Google Scholar]
- 8.Blennow K, Brody DL, Kochanek PM, Levin H, McKee A, Ribbers GM, Yaffe K, Zetterberg H. Traumatic brain injuries. Nat Rev Dis Primers. 2016;2:16084. doi: 10.1038/nrdp.2016.84. [DOI] [PubMed] [Google Scholar]
- 9.Bruttger J, Karram K, Wörtge S, Regen T, Marini F, Hoppmann N, Klein M, Blank T, Yona S, Wolf Y, Mack M, Pinteaux E, Müller W, Zipp F, Binder H, Bopp T, Prinz M, Jung S, Waisman A. Genetic cell ablation reveals clusters of local self-renewing microglia in the mammalian central nervous system. Immunity. 2015;43:92–106. doi: 10.1016/j.immuni.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 10.Butowski N, Colman H, De Groot JF, Omuro AM, Nayak L, Wen PY, Cloughesy TF, Marimuthu A, Haidar S, Perry A, Huse J, Phillips J, West BL, Nolop KB, Hsu HH, Ligon KL, Molinaro AM, Prados M. Orally administered colony stimulating factor 1 receptor inhibitor PLX3397 in recurrent glioblastoma: an Ivy Foundation Early Phase Clinical Trials Consortium phase II study. Neuro Oncol. 2016;18:557–564. doi: 10.1093/neuonc/nov245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cai Z, Ye T, Xu X, Gao M, Zhang Y, Wang D, Gu Y, Zhu H, Tong L, Lu J, Chen Z, Huang C. Antidepressive properties of microglial stimulation in a mouse model of depression induced by chronic unpredictable stress. Prog Neuropsychopharmacol Biol Psychiatry. 2020;101:109931. doi: 10.1016/j.pnpbp.2020.109931. [DOI] [PubMed] [Google Scholar]
- 12.Chung WS, Welsh CA, Barres BA, Stevens B. Do glia drive synaptic and cognitive impairment in disease. Nat Neurosci. 2015;18:1539–1545. doi: 10.1038/nn.4142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coleman LG Jr, Zou J, Crews FT. Microglial depletion and repopulation in brain slice culture normalizes sensitized proinflammatory signaling. J Neuroinflammation. 2020;17:27. doi: 10.1186/s12974-019-1678-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cowan M, Petri WA., Jr Microglia: immune regulators of neurodevelopment. Front Immunol. 2018;9:2576. doi: 10.3389/fimmu.2018.02576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crehan H, Hardy J, Pocock J. Microglia, Alzheimer’s disease, and complement. Int J Alzheimers Dis. 2012;2012:983640. doi: 10.1155/2012/983640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dagher NN, Najafi AR, Kayala KM, Elmore MR, White TE, Medeiros R, West BL, Green KN. Colony-stimulating factor 1 receptor inhibition prevents microglial plaque association and improves cognition in 3xTg-AD mice. J Neuroinflammation. 2015;12:139. doi: 10.1186/s12974-015-0366-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donat CK, Scott G, Gentleman SM, Sastre M. Microglial activation in traumatic brain injury. Front Aging Neurosci. 2017;9:208. doi: 10.3389/fnagi.2017.00208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elmore MR, Najafi AR, Koike MA, Dagher NN, Spangenberg EE, Rice RA, Kitazawa M, Matusow B, Nguyen H, West BL, Green KN. Colony-stimulating factor 1 receptor signaling is necessary for microglia viability unmasking a microglia progenitor cell in the adult brain. Neuron. 2014;82:380–397. doi: 10.1016/j.neuron.2014.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elmore MRP, Hohsfield LA, Kramár EA, Soreq L, Lee RJ, Pham ST, Najafi AR, Spangenberg EE, Wood MA, West BL, Green KN. Replacement of microglia in the aged brain reverses cognitive synaptic, and neuronal deficits in mice. Aging Cell. 2018;17:e12832. doi: 10.1111/acel.12832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erblich B, Zhu L, Etgen AM, Dobrenis K, Pollard JW. Absence of colony stimulation factor-1 receptor results in loss of microglia disrupted brain development and olfactory deficits. PLoS One. 2011;6:e26317. doi: 10.1371/journal.pone.0026317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feng L, Murugan M, Bosco DB, Liu Y, Peng J, Worrell GA, Wang HL, Ta LE, Richardson JR, Shen Y, Wu LJ. Microglial proliferation and monocyte infiltration contribute to microgliosis following status epilepticus. Glia. 2019;67:1434–1448. doi: 10.1002/glia.23616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forrester JV, McMenamin PG, Dando SJ. CNS infection and immune privilege. Nat Rev Neurosci. 2018;19:655–671. doi: 10.1038/s41583-018-0070-8. [DOI] [PubMed] [Google Scholar]
- 23.Frediani B, Bertoldi I. Clodronate: new directions of use. Clin Cases Miner Bone Metab. 2015;12:97–108. doi: 10.11138/ccmbm/2015.12.2.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fuhrmann M, Bittner T, Jung CK, Burgold S, Page RM, Mitteregger G, Haass C, LaFerla FM, Kretzschmar H, Herms J. Microglial Cx3cr1 knockout prevents neuron loss in a mouse model of Alzheimer’s disease. Nat Neurosci. 2010;13:411–413. doi: 10.1038/nn.2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gerber YN, Saint-Martin GP, Bringuier CM, Bartolami S, Goze-Bac C, Noristani HN, Perrin FE. CSF1R inhibition reduces microglia proliferation promotes tissue preservation and improves motor recovery after spinal cord injury. Front Cell Neurosci. 2018;12:368. doi: 10.3389/fncel.2018.00368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldmann T, Wieghofer P, Müller PF, Wolf Y, Varol D, Yona S, Brendecke SM, Kierdorf K, Staszewski O, Datta M, Luedde T, Heikenwalder M, Jung S, Prinz M. A new type of microglia gene targeting shows TAK1 to be pivotal in CNS autoimmune inflammation. Nat Neurosci. 2013;16:1618–1626. doi: 10.1038/nn.3531. [DOI] [PubMed] [Google Scholar]
- 27.Gonzalez NC, Allen J, Blanco VG, Schmidt EJ, van Rooijen N, Wood JG. Alveolar macrophages are necessary for the systemic inflammation of acute alveolar hypoxia. J Appl Physiol (1985) 2007;103:1386–1394. doi: 10.1152/japplphysiol.00312.2007. [DOI] [PubMed] [Google Scholar]
- 28.Graykowski DR, Wang YZ, Upadhyay A, Savas JN. The Dichotomous role of extracellular vesicles in the central nervous system. iScience. 2020;23:101456. doi: 10.1016/j.isci.2020.101456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Green KN, Crapser JD, Hohsfield LA. To kill a microglia: a case for CSF1R inhibitors. Trends Immunol. 2020;41:771–784. doi: 10.1016/j.it.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guglielmetti C, Chou A, Krukowski K, Najac C, Feng X, Riparip LK, Rosi S, Chaumeil MM. In vivo metabolic imaging of traumatic brain injury. Sci Rep. 2017;7:17525. doi: 10.1038/s41598-017-17758-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han X, Li Q, Lan X, El-Mufti L, Ren H, Wang J. Microglial depletion with clodronate liposomes increases proinflammatory cytokine levels, induces astrocyte activation, and damages blood vessel integrity. Mol Neurobiol. 2019a;56:6184–6196. doi: 10.1007/s12035-019-1502-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Han X, Li Q, Lan X, El-Mufti L, Ren H, Wang J. Microglial depletion with clodronate liposomes increases proinflammatory cytokine levels, induces astrocyte activation, and damages blood vessel integrity. Mol Neurobiol. 2019b;56:6184–6196. doi: 10.1007/s12035-019-1502-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hanlon LA, Raghupathi R, Huh JW. Depletion of microglia immediately following traumatic brain injury in the pediatric rat: Implications for cellular and behavioral pathology. Exp Neurol. 2019;316:39–51. doi: 10.1016/j.expneurol.2019.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Henry RJ, Ritzel RM, Barrett JP, Doran SJ, Jiao Y, Leach JB, Szeto GL, Wu J, Stoica BA, Faden AI, Loane DJ. Microglial depletion with CSF1R inhibitor during chronic phase of experimental traumatic brain injury reduces neurodegeneration and neurological deficits. J Neurosci. 40:2960–2974. doi: 10.1523/JNEUROSCI.2402-19.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heppner FL, Greter M, Marino D, Falsig J, Raivich G, Hövelmeyer N, Waisman A, Rülicke T, Prinz M, Priller J, Becher B, Aguzzi A. Experimental autoimmune encephalomyelitis repressed by microglial paralysis. Nat Med. 2005;11:146–152. doi: 10.1038/nm1177. [DOI] [PubMed] [Google Scholar]
- 36.Hillmer AT, Holden D, Fowles K, Nabulsi N, West BL, Carson RE, Cosgrove KP. Microglial depletion and activation: A [11C]PBR28 PET study in nonhuman primates. EJNMMI Res. 2017;7:59. doi: 10.1186/s13550-017-0305-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krauthausen M, Kummer MP, Zimmermann J, Reyes-Irisarri E, Terwel D, Bulic B, Heneka MT, Müller M. CXCR3 promotes plaque formation and behavioral deficits in an Alzheimer’s disease model. J Clin Invest. 2015;125:365–378. doi: 10.1172/JCI66771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kruse J, von Bernstorff W, Evert K, Albers N, Hadlich S, Hagemann S, Günther C, van Rooijen N, Heidecke CD, Partecke LI. Macrophages promote tumour growth and liver metastasis in an orthotopic syngeneic mouse model of colon cancer. Int J Colorectal Dis. 2013;28:1337–1349. doi: 10.1007/s00384-013-1703-z. [DOI] [PubMed] [Google Scholar]
- 39.Kumamaru H, Saiwai H, Kobayakawa K, Kubota K, van Rooijen N, Inoue K, Iwamoto Y, Okada S. Liposomal clodronate selectively eliminates microglia from primary astrocyte cultures. J Neuroinflammation. 2012;9:116. doi: 10.1186/1742-2094-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee JC, Seong J, Kim SH, Lee SJ, Cho YJ, An J, Nam DH, Joo KM, Cha CI. Replacement of microglial cells using Clodronate liposome and bone marrow transplantation in the central nervous system of SOD1(G93A) transgenic mice as an in vivo model of amyotrophic lateral sclerosis. Biochem Biophys Res Commun. 2012;418:359–365. doi: 10.1016/j.bbrc.2012.01.026. [DOI] [PubMed] [Google Scholar]
- 41.Lei F, Cui N, Zhou C, Chodosh J, Vavvas DG, Paschalis EI. CSF1R inhibition by a small-molecule inhibitor is not microglia specific; affecting hematopoiesis and the function of macrophages. Proc Natl Acad Sci U S A. 2020;117:23336–23338. doi: 10.1073/pnas.1922788117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu M, Jiang L, Wen M, Ke Y, Tong X, Huang W, Chen R. Microglia depletion exacerbates acute seizures and hippocampal neuronal degeneration in mouse models of epilepsy. Am J Physiol Cell Physiol. 2020;319:C605–610. doi: 10.1152/ajpcell.00205.2020. [DOI] [PubMed] [Google Scholar]
- 43.Liu Y, Given KS, Dickson EL, Owens GP, Macklin WB, Bennett JL. Concentration-dependent effects of CSF1R inhibitors on oligodendrocyte progenitor cells ex vivo and in vivo. Exp Neurol. 2019;318:32–41. doi: 10.1016/j.expneurol.2019.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lloyd AF, Davies CL, Holloway RK, Labrak Y, Ireland G, Carradori D, Dillenburg A, Borger E, Soong D, Richardson JC, Kuhlmann T, Williams A, Pollard JW, des Rieux A, Priller J, Miron VE. Central nervous system regeneration is driven by microglia necroptosis and repopulation. Nat Neurosci. 2019;22:1046–1052. doi: 10.1038/s41593-019-0418-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lunnon K, Teeling JL, Tutt AL, Cragg MS, Glennie MJ, Perry VH. Systemic inflammation modulates Fc receptor expression on microglia during chronic neurodegeneration. J Immunol. 2011;186:7215–7224. doi: 10.4049/jimmunol.0903833. [DOI] [PubMed] [Google Scholar]
- 46.Mancuso R, Fryatt G, Cleal M, Obst J, Pipi E, Monzón-Sandoval J, Ribe E, Winchester L, Webber C, Nevado A, Jacobs T, Austin N, Theunis C, Grauwen K, Daniela Ruiz E, Mudher A, Vicente-Rodriguez M, Parker CA, Simmons C, Cash D, et al. CSF1R inhibitor JNJ-40346527 attenuates microglial proliferation and neurodegeneration in P301S mice. Brain. 2019;142:3243–3264. doi: 10.1093/brain/awz241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martínez-Muriana A, Mancuso R, Francos-Quijorna I, Olmos-Alonso A, Osta R, Perry VH, Navarro X, Gomez-Nicola D, López-Vales R. CSF1R blockade slows the progression of amyotrophic lateral sclerosis by reducing microgliosis and invasion of macrophages into peripheral nerves. Sci Rep. 2016;6:25663. doi: 10.1038/srep25663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Masters CL, Bateman R, Blennow K, Rowe CC, Sperling RA, Cummings JL. Alzheimer’s disease. Nat Rev Dis Primers. 2015;1:15056. doi: 10.1038/nrdp.2015.56. [DOI] [PubMed] [Google Scholar]
- 49.Mazaheri F, Snaidero N, Kleinberger G, Madore C, Daria A, Werner G, Krasemann S, Capell A, Trümbach D, Wurst W, Brunner B, Bultmann S, Tahirovic S, Kerschensteiner M, Misgeld T, Butovsky O, Haass C. TREM2 deficiency impairs chemotaxis and microglial responses to neuronal injury. EMBO Rep. 2017;18:1186–1198. doi: 10.15252/embr.201743922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Michels M, Ávila P, Pescador B, Vieira A, Abatti M, Cucker L, Borges H, Goulart AI, Junior CC, Barichello T, Quevedo J, Dal-Pizzol F. Microglial cells depletion increases inflammation and modifies microglial phenotypes in an animal model of severe sepsis. Mol Neurobiol. 2019;56:7296–7304. doi: 10.1007/s12035-019-1606-2. [DOI] [PubMed] [Google Scholar]
- 51.Mildner A, Mack M, Schmidt H, Brück W, Djukic M, Zabel MD, Hille A, Priller J, Prinz M. CCR2+Ly-6Chi monocytes are crucial for the effector phase of autoimmunity in the central nervous system. Brain. 2009;132:2487–2500. doi: 10.1093/brain/awp144. [DOI] [PubMed] [Google Scholar]
- 52.Najafi AR, Crapser J, Jiang S, Ng W, Mortazavi A, West BL, Green KN. A limited capacity for microglial repopulation in the adult brain. Glia. 2018;66:2385–2396. doi: 10.1002/glia.23477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nandi S, Gokhan S, Dai XM, Wei S, Enikolopov G, Lin H, Mehler MF, Stanley ER. The CSF-1 receptor ligands IL-34 and CSF-1 exhibit distinct developmental brain expression patterns and regulate neural progenitor cell maintenance and maturation. Dev Biol. 2012;367:100–113. doi: 10.1016/j.ydbio.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Neal ML, Fleming SM, Budge KM, Boyle AM, Kim C, Alam G, Beier EE, Wu LJ, Richardson JR. Pharmacological inhibition of CSF1R by GW2580 reduces microglial proliferation and is protective against neuroinflammation and dopaminergic neurodegeneration. FASEB J. 2020;34:1679–1694. doi: 10.1096/fj.201900567RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nguyen PT, Dorman LC, Pan S, Vainchtein ID, Han RT, Nakao-Inoue H, Taloma SE, Barron JJ, Molofsky AB, Kheirbek MA, Molofsky AV. Microglial remodeling of the extracellular matrix promotes synapse plasticity. Cell. 2020;182:388–403.e315. doi: 10.1016/j.cell.2020.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nimmerjahn A, Kirchhoff F, Helmchen F. Resting microglial cells are highly dynamic surveillants of brain parenchyma in vivo. Science. 2005;308:1314–1318. doi: 10.1126/science.1110647. [DOI] [PubMed] [Google Scholar]
- 57.Nissen JC, Thompson KK, West BL, Tsirka SE. Csf1R inhibition attenuates experimental autoimmune encephalomyelitis and promotes recovery. Exp Neurol. 2018;307:24–36. doi: 10.1016/j.expneurol.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oh SJ, Ahn H, Jung KH, Han SJ, Nam KR, Kang KJ, Park JA, Lee KC, Lee YJ, Choi JY. Evaluation of the neuroprotective effect of microglial depletion by CSF-1R inhibition in a Parkinson’s animal model. Mol Imaging Biol. 2020;22:1031–1042. doi: 10.1007/s11307-020-01485-w. [DOI] [PubMed] [Google Scholar]
- 59.Olmos-Alonso A, Schetters ST, Sri S, Askew K, Mancuso R, Vargas-Caballero M, Holscher C, Perry VH, Gomez-Nicola D. Pharmacological targeting of CSF1R inhibits microglial proliferation and prevents the progression of Alzheimer’s-like pathology. Brain. 2016;139:891–907. doi: 10.1093/brain/awv379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.O’Neil SM, Witcher KG, McKim DB, Godbout JP. Forced turnover of aged microglia induces an intermediate phenotype but does not rebalance CNS environmental cues driving priming to immune challenge. Acta Neuropathol Commun. 2018;6:129. doi: 10.1186/s40478-018-0636-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ortega-Martinez S, Palla N, Zhang X, Lipman E, Sisodia SS. Deficits in enrichment-dependent neurogenesis and enhanced anxiety behaviors mediated by expression of Alzheimer’s disease-linked Ps1 variants are rescued by microglial depletion. J Neurosci. 2019;39:6766–6780. doi: 10.1523/JNEUROSCI.0884-19.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Otxoa-de-Amezaga A, Miró-Mur F, Pedragosa J, Gallizioli M, Justicia C, Gaja-Capdevila N, Ruíz-Jaen F, Salas-Perdomo A, Bosch A, Calvo M, Márquez-Kisinousky L, Denes A, Gunzer M, Planas AM. Microglial cell loss after ischemic stroke favors brain neutrophil accumulation. Acta Neuropathol. 2019;137:321–341. doi: 10.1007/s00401-018-1954-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Parkhurst CN, Yang G, Ninan I, Savas JN, Yates JR, 3rd, Lafaille JJ, Hempstead BL, Littman DR, Gan WB. Microglia promote learning-dependent synapse formation through brain-derived neurotrophic factor. Cell. 2013;155:1596–609. doi: 10.1016/j.cell.2013.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Perea JR, Llorens-Martín M, Ávila J, Bolós M. The role of microglia in the spread of tau: relevance for tauopathies. Front Cell Neurosci. 2018;12:172. doi: 10.3389/fncel.2018.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pósfai B, Cserép C, Orsolits B, Dénes Á New insights into microglia-neuron interactions: a neuron’s perspective. Neuroscience. 2019;405:103–117. doi: 10.1016/j.neuroscience.2018.04.046. [DOI] [PubMed] [Google Scholar]
- 66.Ransohoff RM. A polarizing question: do M1 and M2 microglia exist. Nat Neurosci. 2016;19:987–991. doi: 10.1038/nn.4338. [DOI] [PubMed] [Google Scholar]
- 67.Reemst K, Noctor SC, Lucassen PJ, Hol EM. The indispensable roles of microglia and astrocytes during brain development. Front Hum Neurosci. 2016;10:566. doi: 10.3389/fnhum.2016.00566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rice RA, Pham J, Lee RJ, Najafi AR, West BL, Green KN. Microglial repopulation resolves inflammation and promotes brain recovery after injury. Glia. 2017;65:931–944. doi: 10.1002/glia.23135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schreiner B, Romanelli E, Liberski P, Ingold-Heppner B, Sobottka-Brillout B, Hartwig T, Chandrasekar V, Johannssen H, Zeilhofer HU, Aguzzi A, Heppner F, Kerschensteiner M, Becher B. Astrocyte depletion impairs redox homeostasis and triggers neuronal loss in the adult CNS. Cell Rep. 2015;12:1377–1384. doi: 10.1016/j.celrep.2015.07.051. [DOI] [PubMed] [Google Scholar]
- 70.Serrats J, Schiltz JC, García-Bueno B, van Rooijen N, Reyes TM, Sawchenko PE. Dual roles for perivascular macrophages in immune-to-brain signaling. Neuron. 2010;65:94–106. doi: 10.1016/j.neuron.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta Neuropathol. 2010;119:7–35. doi: 10.1007/s00401-009-0619-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sosna J, Philipp S, Albay R, 3rd, Reyes-Ruiz JM, Baglietto-Vargas D, LaFerla FM, Glabe CG. Early long-term administration of the CSF1R inhibitor PLX3397 ablates microglia and reduces accumulation of intraneuronal amyloid neuritic plaque deposition and pre-fibrillar oligomers in 5XFAD mouse model of Alzheimer’s disease. Mol Neurodegener. 2018;13:11. doi: 10.1186/s13024-018-0244-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Spangenberg E, Severson PL, Hohsfield LA, Crapser J, Zhang J, Burton EA, Zhang Y, Spevak W, Lin J, Phan NY, Habets G, Rymar A, Tsang G, Walters J, Nespi M, Singh P, Broome S, Ibrahim P, Zhang C, Bollag G, et al. Sustained microglial depletion with CSF1R inhibitor impairs parenchymal plaque development in an Alzheimer’s disease model. Nat Commun. 2019;10:3758. doi: 10.1038/s41467-019-11674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Spillantini MG, Goedert M. Tau pathology and neurodegeneration. Lancet Neurol. 2013;12:609–622. doi: 10.1016/S1474-4422(13)70090-5. [DOI] [PubMed] [Google Scholar]
- 75.Stopper L, Bălşeanu TA, Cătălin B, Rogoveanu OC, Mogoantă L, Scheller A. Microglia morphology in the physiological and diseased brain -from fixed tissue to in vivo conditions. Rom J Morphol Embryol. 2018;59:7–12. [PubMed] [Google Scholar]
- 76.Streit WJ, Mrak RE, Griffin WS. Microglia and neuroinflammation: a pathological perspective. J Neuroinflammation. 2004;1:14. doi: 10.1186/1742-2094-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Su F, Bai F, Zhou H, Zhang Z. Microglial toll-like receptors and Alzheimer’s disease. Brain Behav Immun. 2016;52:187–198. doi: 10.1016/j.bbi.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 78.Szalay G, Martinecz B, Lénárt N, Környei Z, Orsolits B, Judák L, Császár E, Fekete R, West BL, Katona G, Rózsa B, Dénes Á Microglia protect against brain injury and their selective elimination dysregulates neuronal network activity after stroke. Nat Commun. 2016;7:11499. doi: 10.1038/ncomms11499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tanabe S, Saitoh S, Miyajima H, Itokazu T, Yamashita T. Microglia suppress the secondary progression of autoimmune encephalomyelitis. Glia. 2019;67:1694–1704. doi: 10.1002/glia.23640. [DOI] [PubMed] [Google Scholar]
- 80.Torres L, Danver J, Ji K, Miyauchi JT, Chen D, Anderson ME, West BL, Robinson JK, Tsirka SE. Dynamic microglial modulation of spatial learning and social behavior. Brain Behav Immun. 2016;55:6–16. doi: 10.1016/j.bbi.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Van Rooijen N, Sanders A. Liposome mediated depletion of macrophages: mechanism of action preparation of liposomes and applications. J Immunol Methods. 1994;174:83–93. doi: 10.1016/0022-1759(94)90012-4. [DOI] [PubMed] [Google Scholar]
- 82.Vinet J, Weering HR, Heinrich A, Kälin RE, Wegner A, Brouwer N, Heppner FL, Rooijen Nv, Boddeke HW, Biber K. Neuroprotective function for ramified microglia in hippocampal excitotoxicity. J Neuroinflammation. 2012;9:27. doi: 10.1186/1742-2094-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang C, Yue H, Hu Z, Shen Y, Ma J, Li J, Wang XD, Wang L, Sun B, Shi P, Wang L, Gu Y. Microglia mediate forgetting via complement-dependent synaptic elimination. Science. 2020a;367:688–694. doi: 10.1126/science.aaz2288. [DOI] [PubMed] [Google Scholar]
- 84.Wang J, Lai S, Li G, Zhou T, Wang B, Cao F, Chen T, Zhang X, Chen Y. Microglial activation contributes to depressive-like behavior in dopamine D3 receptor knockout mice. Brain Behav Immun. 2020b;83:226–238. doi: 10.1016/j.bbi.2019.10.016. [DOI] [PubMed] [Google Scholar]
- 85.Wilkinson K, El Khoury J. Microglial scavenger receptors and their roles in the pathogenesis of Alzheimer’s disease. Int J Alzheimers Dis. 2012;2012:489456. doi: 10.1155/2012/489456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Willis EF, MacDonald KPA, Nguyen QH, Garrido AL, Gillespie ER, Harley SBR, Bartlett PF, Schroder WA, Yates AG, Anthony DC, Rose-John S, Ruitenberg MJ, Vukovic J. Repopulating microglia promote brain repair in an IL-6-dependent manner. Cell. 2020;180:833–846.e16. doi: 10.1016/j.cell.2020.02.013. [DOI] [PubMed] [Google Scholar]
- 87.Wu W, Li Y, Wei Y, Bosco DB, Xie M, Zhao MG, Richardson JR, Wu LJ. Microglial depletion aggravates the severity of acute and chronic seizures in mice. Brain Behav Immun. 2020;89:245–255. doi: 10.1016/j.bbi.2020.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yang X, Ren H, Wood K, Li M, Qiu S, Shi FD, Ma C, Liu Q. Depletion of microglia augments the dopaminergic neurotoxicity of MPTP. FASEB J. 2018;32:3336–3345. doi: 10.1096/fj.201700833RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yao Y, Echeverry S, Shi XQ, Yang M, Yang QZ, Wang GY, Chambon J, Wu YC, Fu KY, De Koninck Y, Zhang J. Dynamics of spinal microglia repopulation following an acute depletion. Sci Rep. 2016;6:22839. doi: 10.1038/srep22839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhan L, Krabbe G, Du F, Jones I, Reichert MC, Telpoukhovskaia M, Kodama L, Wang C, Cho SH, Sayed F, Li Y, Le D, Zhou Y, Shen Y, West B, Gan L. Proximal recolonization by self-renewing microglia re-establishes microglial homeostasis in the adult mouse brain. PLoS Biol. 2019;17:e3000134. doi: 10.1371/journal.pbio.3000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang K, Yang C, Chang L, Sakamoto A, Suzuki T, Fujita Y, Qu Y, Wang S, Pu Y, Tan Y, Wang X, Ishima T, Shirayama Y, Hatano M, Tanaka KF, Hashimoto K. Essential role of microglial transforming growth factor-β1 in antidepressant actions of (R)-ketamine and the novel antidepressant TGF-β1. Transl Psychiatry. 2020;10:32. doi: 10.1038/s41398-020-0733-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang Y, Zhao L, Wang X, Ma W, Lazere A, Qian HH, Zhang J, Abu-Asab M, Fariss RN, Roger JE, Wong WT. Repopulating retinal microglia restore endogenous organization and function under CX3CL1-CX3CR1 regulation. Sci Adv. 2018;4:eaap8492. doi: 10.1126/sciadv.aap8492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhao R, Hu W, Tsai J, Li W, Gan WB. Microglia limit the expansion of β-amyloid plaques in a mouse model of Alzheimer’s disease. Mol Neurodegener. 2017;12:47. doi: 10.1186/s13024-017-0188-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Life span and turnover of microglia


