Abstract
While the COVID-19 pandemic is still in progress, being under the fifth COVID-19 wave in Madrid, over more than one year, Spain experienced a four wave pattern. The transmission of SARS-CoV-2 pathogens in Madrid metropolitan region was investigated from an urban context associated with seasonal variability of climate and air pollution drivers. Based on descriptive statistics and regression methods of in-situ and geospatial daily time series data, this study provides a comparative analysis between COVID-19 waves incidence and mortality cases in Madrid under different air quality and climate conditions. During analyzed period 1 January 2020–1 July 2021, for each of the four COVID-19 waves in Madrid were recorded anomalous anticyclonic synoptic meteorological patterns in the mid-troposphere and favorable stability conditions for COVID-19 disease fast spreading. As airborne microbial temporal pattern is most affected by seasonal changes, this paper found: 1) a significant negative correlation of air temperature, Planetary Boundary Layer height, and surface solar irradiance with daily new COVID-19 incidence and deaths; 2) a similar mutual seasonality with climate variables of the first and the fourth COVID-waves from spring seasons of 2020 and 2021 years. Such information may help the health decision makers and public plan for the future.
Keywords: COVID-19 disease, Synoptic atmospheric circulation, Air pollutants, Climate variables, NASA, Reanalysis NCEP/NCAR PSD
1. Introduction
Over the last 18 months, novel coronavirus disease 2019 (COVID-19) has spread from China to the rest of the world. This viral infection pandemic disease, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its new variants, is responsible for a global crisis spreading the disease and collapsing the world economy to levels not seen since the 1918 influenza pandemic. Official records indicate total global cumulative confirmed at least 198, 561, 249 COVID-19 cases, at least 4,233,121 deaths, and at least recovered 179, 291, 571 cases globally in 222 countries, as of 1 August, 2021 (Johns Hopkins Coronavirus; Worldometer Info, 2021). The infectious degree of this pandemic disease is very high and, therefore, the consequences of the transmission have been very hard for the entire World (Yuki et al., 2020; Byun et al., 2021). Recently, more new transmissible variants of SARS-CoV-2 have been identified globally (WHO, 2021a; (WHO, 2021b). On March 3, 2020, the first case of COVID-19 death was registered in Madrid, and by 1 August, 2021, roughly 833,467 persons had been diagnosed with SARS-CoV-2 infection (representing 10.87 % of Spain total cases) and 24,419 had died in the Madrid region (representing 29.97 % of total Spain COVID-19 deaths) (Instituto Nacional de Estadística, 2021; CM, 2021). These cumulative numbers of cases refer to laboratory-confirmed positive cases, the true number of cases being underestimated during the earlier stages of the pandemic (Soriano et al., 2021a). Due to high population density and urban mobility, Madrid was the national epicenter with the greatest number of cases and deaths and one of the main foci of the COVID-19 in Europe (CM, 2021; Soriano et al., 2021b; Polan et al., 2020).
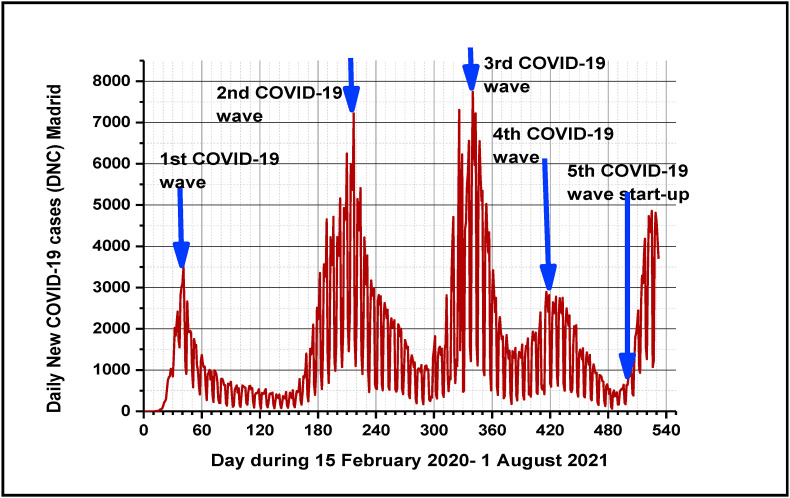
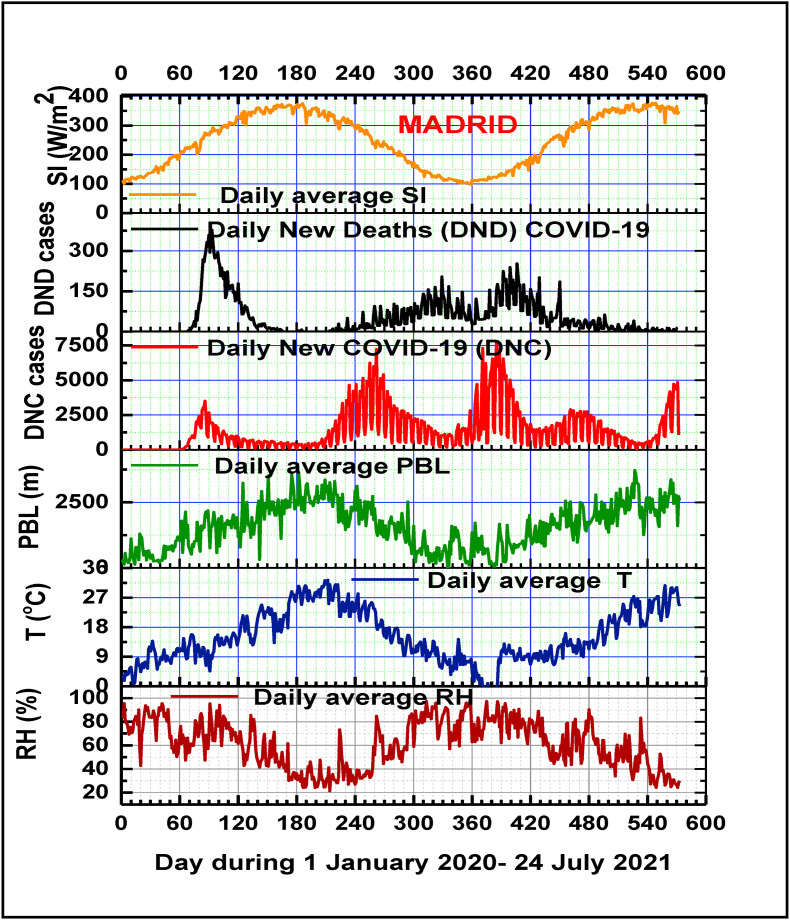
Since the first emergence of viral infection in February 2020, till the end of June 2021, together with the emergence of multiple variants of SARS-CoV-2, Spain has experienced the four successive waves of COVID-19 pandemic, and presently (at 1 August, 2021), Madrid in Spain is under the fivth wave, that started on 1 July, 2020. The first COVID-19 wave (15 February to 30 June, 2020) with a peak during March–April on 20 March, 2020 was a hard outbreak related to community transmission, and insufficient sanitary treatments. The second COVID-19 wave (10 August– 30 November, 2020) has a peak during September–October (on 28 October, 2020) started with increasing of social activities and tourism due to so called “new normality” by 21 June, 2020, with poor social distancing, being better mitigated by the rapid reinforcement of sanitary measures during the early stages. Compared to the second wave, the third COVID-19 wave (December 2020– end of February 2021), peaked on 15 January, 2021 was characterized by delayed social distancing reinforcement, winter holidays, longer duration and higher viral infections and fatalities rates. In spite of rigorous preventive and protective measures implemented in Spain during the first three waves, the fourth COVID-19 wave started on 1 March 2021, peaked in 20 April 2021 with a lower intensity than the second and especially the third wave (explained possible through vaccination campaign) and ended around 30 June 2021. COVID-19 disease transmission is under the ongoing fifth wave, that start-up on 1 July 2021 (Fig. 1 ). In fact, mounting evidence suggests that COVID-19 has the potential to become a seasonal disease like seasonal influenza (Lavine et al., 2021). This emphasizes the importance of understanding the transmission patterns of SARS-CoV-2 in environmental conditions, that is, whether it is a seasonal virus.
Fig. 1.
COVID-19 epidemiological multiwaves pattern in Madrid metropolitan region in Spain.
In order to minimize COVID-19 disease transmission, forecast its rate of outdoor and indoor dispersion and develop proper medical and intervention measures and vaccines, intense multidisciplinary, and interdisciplinary international scientific efforts are devoted to understand the basics of the pandemic, to propose solutions, and find strategies to increase population resilience (Anand et al., 2021; Soriano et al., 2021c). Is well recognized that environmental, demographic, clinical and social factors play an important role in exposure to SARS-CoV-2 pathogens transmission and COVID-19 disease severity, but host-specific genetic factors may also have a high contributions revealing biological mechanisms of specific therapeutic relevance and clarify causal relationships of environmental seasonality risk factors for SARS-CoV-2 infection and outcomes (Casado-Aranda et al., 2021; Iqbal et al., 2021; Bontempi, 2021).
Among these multifactors, environmental (climate and air quality) are mainly responsible of the dispersal, diffusion, and infectivity of the SARS-CoV-2 novel coronavirus and its new variants virions (Islam et al., 2021; Huang et al., 2020; Amin et al., 2020; Hassanzadeh et al., 2020). While a clear evidence for the effects of air pollution and climate factors on COVID-19 pandemic disease transmission and lethality remains controversial, it is crucial to understand the role of preventable environmental factors and mutual seasonality with SARS-CoV-2 pathogens, especially in large urban areas. This coronavirus is a new enveloped virus positive-sense, single-stranded RNA with roughly spherical or moderately pleomorphic virions of approximately 60–140 nm with an average to 0.1 μm in diameter (Mousavizadeh, Ghasemi, 2020; R. Lu et al., 2020; Shang et al., 2020; Bosch et al., 2003; Rivellese, Prediletto, 2020; Liu Y et al., 2020; Walls et al., 2020; Zowalaty and Järhult, 2020), that can be attached to atmospheric particulate matter. PM2.5 and PM10 may have inorganic and organic components, as well as biotic components (bacteria, fungi, viruses, and pollens), which are known as bioaerosols, constituting up to 25 % of the total atmospheric aerosols (Gao et al., 2015; Du et al., 2018).
Recent evidence and prior research studies from Spain, China, Italy, England, and the United States suggest that exposure to increased air pollutant concentrations (particulate matter PM2.5 and PM10, including Saharan dust intrusions, O3 and NO2) in big cities may play a significant role in COVID-19 incidence and mortality, being associated with to the worsening of multiple pathologies associated with human cardiorespiratory and immune systems (Domingo et al., 2020; Marquès et al., 2021; Lipsitt et al., 2021; Frontera et al., 2020; Salvador et al., 2019; Linares et al., 2017; Zoran et al., 2020a). Changes in the air pollution levels and climate variables affect urban environmental health, and frequently increasing risk/hazard viral infections probability.
The main important factors affecting air quality are natural and anthropogenic sources, and the rates of emissions, local and regional atmospheric circulation patterns, the physico-chemical composition of the atmosphere, air ventilation conditions inside the metropolitan region, as well as spatiotemporal variability of meso- and microclimatic parameters (Zhou et al., 2018; Molepo et al., 2019; Pfahl et al., 2015; Baldasano, 2020; Zoran et al., 2008; Yuan et al., 2021). Hot-spots urban air pollution episodes for several days (Pandolfi et al., 2014) can be correlated not only with local environmental conditions, but also with trans-border air pollution, as is the case of Saharan dust intrusions for Madrid region during investigated time period in this study (Linares et al., 2021). Due to their oxidative potential, ecotoxicity and genotoxicity, urban air pollutants have adverse health effects on airway inflammatory and cardiovascular diseases (Travaglio et al., 2021; Domingo et al., 2020a; Sugiyama et al., 2020; Chen et al., 2020; Seposo et al., 2020; Kelly, Fussell, 2011; Tager, 2005; Zoran et al., 2020b). Also, during stagnant anticyclonic air conditions that favour accumulation at the ground level of air pollutants, short-term or long-term exposure to high levels of particulate matter PM2.5 and PM10, and gaseous pollutants ozone (O3) and nitrogen dioxide (NO2) increase the susceptibility to morbidity and mortality from respiratory infections (Romano et al., 2020; Cohen and Kupferschmidt, 2020; Perrone et al., 2012; Perrone et al., 2014; Wang Y. et al., 2018; Wang Ye et al., 2020; Li, Y et al., 2004). Due to hydrophobic properties of COVID-19 spike protein, at the near-surface atmosphere, particulate matter can act as a viral vector, that can target the human immune system (Baron, 2021; Mousavizadeh, Ghasemi, 2020; Bowers et al., 2009; Bowers et al., 2013; Bosch et al., 2003; Cao C. et al., 2014; Cao Y. et al., 2020; Jones and Harrison et al., 2004; Khan et al., 2019; Kawasaki et al., 2019; WHO, 2020). The atmosphere can be a significant transport vector for airborne microbiome (bacterial, fungal, viral) communities, and their seasonal shift in both the concentration and biodiversity are strongly influenced by meteorological parameters seasonality and Planetary Boundary Layer heights (PBL) (Tignat-Perrier et al., 2020; Zoran et al., 2020b; Lepeule et al., 2014) and especially in urban areas (Mhuireach et al., 2019). Currently, the pathogenesis of COVID-19 deadly epidemics is not yet very clear (Nishiura et al., 2020; Luo et al., 2020; Walls et al., 2020), but its existence as viral bioaerosol indoors and outdoors explains its pathogenicity.
The main physical climate variables generally considered with a potential effect on SARS-CoV-2 virus persistence outdoors, include air temperature, relative humidity, wind speed intensity and direction, Planetary Boundary Layer height and the important contribution of sunlight radiation.
The solar UV region covers the wavelength range 100–400 nm, and is divided into three bands: UVA (315–400 nm), UVB (280–315 nm) and UVC (100–280 nm). While UV-C irradiation is highly efective in inactivating SARS-CoV-2 replication on contaminated surfaces (Biasin et al., 2021), UVB and UVA in sunlight are the primary virucidal agents in the environment (Herman et al., 2020; Giese, 1976; Lytle, Sagripanti, 2005; Santos et al., 2013; Coohill, Sagripanti, 2009; Heßling et al., 2020). Surface solar UV irradiance may affect the diffusion and the outcomes of the COVID-19 viral infection in patients in two pathways: 1) reduction of SARS-CoV-2 virions transmission through the virus inactivation during specific time periods of exposure (Sagripanti, Lytle, 2020; Schuit et al., 2020); and 2) synthesis of vitamin D in the body, that plays an essential role in the innate and adaptative immune systems defense increasing (Luo et al., 2021; Jayawardena et al., 2021; Calder et al., 2020; Ilie et al., 2020; Castillo et al., 2020).
The SARS-CoV-2 genome has the capability of suffering rapid mutations as the virus spreads (Luo et al., 2020; Mu et al., 2020).
Like its genetic and structural similarities and seasonality with previous pandemics reported from 1918 to 2015 (known as “Spanish flu”-produced by Influenza virus 1918 A/H1N1, SARS- CoV (2002–2003) and MERS-CoV (2012–2015), COVID-19 disease show also multiwaves pattern, future infection waves are likely to occur, with unpredictable height and breadth of the waves (Bakhshandeh et al., 2021; Rayan, 2021; He et. Al., 2020; Baay et al., 2020; Wong et al., 2020). The increased incidence and severity of new fast rapid mutations of SARS-CoV-2 genome, named variants of concern is associated with the increased risk to human health (Wang B. et al., 2020; Shang et al., 2020; Bakhshandeh et al., 2021; Wang Y.et al., 2020; Grubaugh et al., 2020). At 1 August 2021, the most contagious COVID-19 variants recognized by the WHO (World Health Organization) were: Alpha (B.1.1.7, B.1.1.7 + E484K), Beta (B.1.351), Gamma (P.1) and Delta (B.1.617.2), the last one being globally dominant. There is no doubt that the current vaccines are safe, anyway concerns arise about the effectiveness of vaccines with the emergence of new variants. Spain has known the severity of this first phase of COVID-19 in terms of cases and deaths. The second and the third COVID-19 waves were also hard tests for Madrid and Spain society, due to existence of socioeconomic differentials in COVID-19 disease exposure, and existing social inequalities and mobilities (Glodeanu et al., 2021).
More than one year into the global COVID-19 pandemic, the focus of attention has shifted to the seasonal mutual interaction between emergence and spread of SARS-CoV-2 and its new variants and environmental multifactors. Most respiratory viruses show pronounced seasonality (Liu et al., 2021; Rayan, 2021; Du et al., 2018; Stewart, 2016) but for SARS-CoV-2, this still needs to be scientific documented. Is an urgent need to confirm the important role of the climate and environmental factors in SARS-CoV-2 airborne diffusion route, from a reservoir to a susceptible host in densely populated urban areas.
The paper explores the two hypotheses: a) COVID-19 viral infection is associated with air pollution, and climate factors, that may act as determinants of COVID-19 disease spreading; b) seasonality of environmental factors has impacts on COVID-19 disease seasonality. Using daily time series analyses we tested the association between daily changes in climate in air pollution and meteorological variables, and COVID-19 incidence and mortality in Madrid metropolitan region.
The aim of this study was to examine the association between SARS-CoV-2 viral infection fast transmission under local/regional air pollution conditions and climate variables, and different synoptic atmospheric circulation patterns, related to the four COVID-19 waves start-up and evolution in the Madrid metropolitan region in Spain. This region has a wide range of air pollution exposure levels and climate variability with which to investigate inter and intra-urban relationships with COVID-19. By using in-situ and geospatial daily time series data, statistical analysis, regression methods, this study aims to compare air pollution and climate factors variability, which can trigger the transmission of SARS-CoV-2 viral infection during the all four COVID-19 pandemic waves. Also, this study aims to provide significant information regarding the mutual relationship between seasonality of environmental factors and the COVID-19 incidence and lethality in Madrid region during several seasons and over more than one pandemic year investigated period (1 January 2020– 1 July 2021). Future optimized interventions during pandemics need accurate estimation and timely information of the local and regional seasonal environmental and epidemiological parameters variability for decision-making as well as to fight the post-pandemic era.
2. Materials and methods
2.1. Test site description
Madrid, the Spain's capital and largest metropolitan region with high population of 6.661 millions inhabitants, and a density of 829.62 inhabitants/km2, representing 14.2 % of country's population was the national COVID-19 epicenter, and one of Europe's region most affected by COVID-19 pandemic waves. This metropolis is composed of Madrid city (centred on latitude 40.40792° N, and longitude 3.69281° W), with more than 3.3 million inhabitants and 26 satellite towns (Fig. 2 ), with an area of 604.3 km2 is located in the center of the Iberian Peninsula, on the high Castilian Central Plateau. Total area of Madrid Community region is of 8030.1 km2. Madrid's high levels of air pollution and O3 precursors are attributed to industry and transport sectors (Gómez-Losada et al., 2019). Is well recognized by extreme climate events especially summer frequent heat waves under urban heat island and trans-border Saharan dust intrusions (Diaz et al., 2006, 2015, 2019; Linares et al., 2020). Road traffic-related air pollution (Monzón and Guerrero, 2004; Cuevas et al., 2014) represents 65 % of NOx, 67 % of CO, 87 % of PM10 and 85 % of PM2.5 and 14 % of total VOCs emissions per year, respectively (Salvador et al., 2004; Salvador et al., 2012; Montero and Fernández-Avilés, 2018; Valverde et al., 2016). Although during the last years NO2 and PM10 ambient air concentrations have recorded a clear decreasing trend due to the emission reduction, Madrid experienced an increase of 30–40 % of ambient air O3 levels (Saiz-López et al., 2017).
Fig. 2.
Investigated test site Madrid metropolitan region in Spain.
Regarding air quality, despite general downward trends in emissions over recent years, and due to COVID-19 lockdown total/partial restrictions during spring/fall 2020 and respectively winter/spring 2021, still presents exceedances of air quality legal limits according to the Directive 2008/50/EC. From a regional point of view, the mountain breeze circulation influences the wind intensity and direction patterns and drives the transport of the urban air pollution over the Madrid metropolitan basin (Salvador et al., 2004, 2012, 2021).
From a synoptic scale, there are several trans-boundary transports of air pollutants and long-range transport events of Northern Africa dust intrusions over the spring-summer periods, that occurs predominately over the Atlantic Ocean as a result of the powerful West-ward trade winds (Díaz et al., 2017), characterized by an intense seasonal cycle, which may be a an additional risk factor for daily mortality especially during pandemic COVID-19 incidence. It is well recognized that the atmospheric circulation and low pressure fields, amplified by local thermodynamically mechanisms including soil moisture deficit has a significant role in increasing temperature extremes in Madrid metropolitan area.
2.2. Data used
The time series analysis of climate and air pollution seasonality relationship with COVID-19 incidence and mortality seasonality in Madrid is based on a large global dataset built by collecting information from various freely available sources from January 2020 up to end of July 2021.
Coronavirus COVID-19 incidence data (Total cumulative, Daily New cases, Daily New Deaths and Total Deaths) cases recorded in Spain and Madrid have been provided by the following websites: https://www.worldometers.info, https://www.statista.com/, Johns Hopkins Coronavirus (Johns Hopkins Coronavirus Resource Center, 2021), and the National Center for Epidemiology at the Carlos III Health Institute. Accumulated COVID-19 and Daily New confirmed positive data for 15 February 2020–25 July 2021 period for Madrid metropolitan region were provided by https://www.comunidad.madrid/servicios/salud/coronavirus.
Time series data of daily average air pollutants concentrations PM2.5, PM10, O3 and NO2 for Madrid selected stations have been collected from http://www.mambiente.madrid.es/sica/scripts/index.php and https://www.copernicus.eu/en/copernicus-services/atmosphere . Time series of meteorological data, including daily average temperature (T), daily average relative humidity (RH), and daily average wind speed for Madrid metropolitan region were collected from the State Meteorological Agency (Agencia Estatal de Meteorología- AEMET), Weather Underground (https://www.wunderground.com/), and Copernicus climate data (climate.copernicus.eu). Daily average surface solar global irradiance time series data have been provided by http://www.soda-pro.com/web-services/radiation/cams-mcclear . Planetary Boundary Layer PBL height data were collected from the archived data of NOAA's Air Resources Laboratory (https://ready.arl.noaa.gov). In order to describe urban air quality of Madrid metropolitan area, in Spain this paper considered daily average Global Air Quality Index (AQI) according to classification of air quality (http://www.eurad.uni-koeln.de) and EU regulations, which is defined by formula:
| (1) |
where , , , , represent daily average values of respectively O3, PM10, NO2, sulphur dioxide and carbon monoxide present in the urban air. Based on the global criteria for main air pollutants (O3, PM10, NO2, SO2, CO) air quality index is classified in six classes from very good to very poor (respectively: < 10-very good; 10–20- good; 20–30- satisfactory; 30–50 – sufficiently; 50–80- poor; > 80- very poor).
In order to analyze lower atmospheric circulation conditions associated with people's exposure to air pollutants and COVID-19 disease fast diffusion in Madrid metropolitan region during 1 January 2020–1 July 2021, we extracted geopotential heights at 500 mb anomalies and Omega at 850 mb surface charts provided by NASA, Reanalysis Data Project NCEP/NCAR PSD, Boulder, Colorado, USA (http://www.esrl.noaa.gov/psd/).
According to content of meteorological information of daily anomalies of geopotential height 500 hPa (at about 5.5 km height above the ground), positive anomalies are associated with the anticyclonic stability conditions like as, blocking systems, and negative anomalies with cyclonic conditions. Also, in Omega surface charts, downwards airflows are associated with high stability conditions given by positive values of omega (in Pa/s), while upwards airflow are associated with instability conditions, and given by negative values of omega surface charts.
2.3. Descriptive statistical analysis
This multiwaves pattern of COVID-19 in Madrid metropolitan region makes possible the further analysis of climate drivers, with descriptive statistical analysis method for transient correlations that identifies similar variation in the daily time series climate and air quality (considered independent variables) data together daily COVID-19 incidence and mortality over localized windows of time, corresponding to the four CVID-19 waves. First, a descriptive analysis was done to provide an overview of COVID-19 incidence and air quality during the study period. Next, for time series of data we used a linear regression model to fit the dependent variables (COVID-19 incidence) for each independent variable: daily average ambient air pollutants (particulate matter PM2.5, PM10, ozone O3 and NO2) and daily average meteorological parameters (air temperature-, air relative humidity- RH, wind speed intensity –w, surface solar irradiation) and daily maximum Planetary Boundary Planetary Boundary Layer - PBL. The dependence between pairs of time series was quantified in this study by standard tools of statistical analysis, Spearman and rank-correlation non-parametric test coefficients. The normality of data was evaluated using Kolmogorov-Smirnov Tests of Normality for time-series data sets. As the data on daily new COVID-19 cases (DNC) and daily new COVID-19 deaths (DND) showed non-normal distribution, Spearman rank correlation was selected to investigate the association between COVID-19 incidence and mortality and climate and air quality data, using ORIGIN 10.0 software.
The main reason for using non-parametric statistical tests is that compared with parametric statistical tests, are thought to be more suitable for non- normally distributed data, which are involved in our time series air pollution and climate variables data. The values for levels of correlation are bound in the range [0, +1], with 0 for no association and +1 for complete positive association and [0, −1] with −1 as negative correlation. Associated parameter „p-value” tells us if the result of an experiment is statistically significant. P values of <0.01 and < 0.05 were considered statistically significant. Though correlation and p-value provides us with the relationship between variables, care should be taken to interpret them correctly.
3. Results and discussion
3.1. Influence of environmental factors on COVID-19 disease dynamics
Over the last decades, environmental factors have become an increasingly serious global public health concern. Rapid urbanization has increased the amount of air pollution (particulate matter PM2.5, PM10 and gaseous ozone –O3, nitrogen dioxide –NO2, carbon monoxide –CO, volatile organic compounds –VOCs) to dangerous levels. Also, various sources of air and water pollution have impacted the composition of the environment and weather conditions with direct and indirect effects on the physiology and psychology of human health. The epidemiological studies linked exposure to ambient air pollution with particulate matter and gaseous pollutants under different meteorological conditions and occurrence of numerous respiratory viral infectious diseases transmission during several seasons (Wilson, Suh, 1997; Baklanov et al., 2016; Qian et al., 2010).
Also was established, that in large urban areas air pollution and climate factors variability including extreme climate events (heat waves, cold waves, floods, storms) are associated with multiple adverse outcomes in humans, including acute and chronic respiratory infections, chronic obstructive pulmonary disease (COPD), asthma, coronary artery diseases, and lung cancer (Sundell et al., 2016; Jones and Harrison, 2004; Wilson,Suh, 1997). The scientific studies during ongoing worldwide COVID-19 pandemic period found also that air pollution and climate parameters may promote the transmission of SARS CoV-2 viral infection pathogens and increase the incidence and lethality of COVID-19 cases (Landguth et al., 2020; van Doremalen et al., 2020; Luo Wu et al., 2020; Li et al., 2020; Cui et al., 2003).
Currently, is considered that the main pathways of COVID-19 transmission in humans are: a) inhalation of respiratory droplets sprays of aerodynamic diameter particle size ϴ > 5 μm (Thompson et al., 2021; Vejerano, Marr, 2018; Harrison et al., 2005; Gralton et al., 2011; Karimzadeh et al., 2021); b) via airborne transmission, through inhalation of nano-droplets/dried nano-droplets nuclei/aerosol (PM) of virus-laden respiratory tract fluid with diameter particle size ϴ < 5 μm (Ram et al., 2021; Belosi et al., 2021; Nor et al., 2021). c) direct contact with infected persons; d) direct contact with contaminated surfaces with SARS-CoV-2; e) possible oral/fecal contamination through wastewater and sewage sludge produced by hospitals and houses with infected people (Collivignarelli et al., 2020b; Carraturo et al., 2020; Wurtzer et al., 2020, 2021; Efstratiou and Tzoraki, 2021).
In hospitals were found two distinct size ranges of bioaerosols with SARS-CoV-2 pathogens, with aerodynamic dominant diameter ϴ, in the range 0.25 μm <ϴ < 1.0 μm (Baboli et al., 2021; Liu F. et al., 2020). Viral infectivity of SARS-CoV-2 pathogens is of fundamental importance for current and future COVID-19 waves adopting strategies.
3.1.1. Variability of air pollution impact on COVID-19 waves
In Madrid metropolis, industry and traffic related are the predominant emission sources of primary pollutants, PM2.5, PM10 and fossil-fuel combustion by-products, like as NO2, which are especially prevalent with a significant threat to human health (Linares et al., 2018; Borge et al., 2019). Table 1 summarizes descriptive statistics of the total Daily New of COVID-19 (DNC) incidence and mortality (DND) cases per periods and means of daily average concentrations of the main air pollutants (PM2.5, PM10, O3, and NO2) at the ground level, together air quality index and standard deviations recorded during 1 January 2020– 1 July2021 in Madrid metropolitan region. Data have been provided by Madrid air quality network stations over time during the four COVID-19 waves, through the six periods (winter 2020 COVID-19 pre-lockdown, COVID-19 beyond lockdown during the first wave, summer 2020 COVID-19 under heat wave, COVID-19 under second wave, COVID-19 under third and fourth waves). In addition, comparison with pre-lockdown period (Table 1) shows that during COVID-19 periods have been recorded reductions of air pollution levels (PM2.5 and PM10) across the Madrid metropolitan region as a result of the lockdown, with respectively (PM2.5: 26 % for the first and the third COVID-19 waves, with 22 % for the second COVID-19 wave, and 37 % for the fourth COVID-19 wave; PM10: with 28 % for the first COVID-19 wave, 20.7 % for the second COVID-19 wave with partial lockdown, with 23.2 % for the third COVID-19 wave, and 39 % for the fourth COVID-19 wave). The increased reduction of PM2.5 and PM10 concentrations during the fourth COVID-19 wave in spring 2021 can be associated to efficient interventions for daily mobility patterns in the metropolitan area of Madrid, (Glodeanu et al., 2021). Physicochemical reactivity and adherence properties of particulate matter in different size fractions (PM0.1 μm, PM2.5 μm and PM10 μm) to SARS-CoV-2 virions attachment depend on their surface morphology, composition, constituents both indoor and outdoor, virion loading being of great relevance for the development and severity of the COVID-19 disease (Duval et al., 2021; Tung et al., 2021). Another relevant parameter is the time of exposure to high ground concentrations levels of particulate matter, and gaseous toxic pollutants ozone (O3), nitrogen dioxide (NO2), carbon monoxide (CO), volatile organic compounds (VOCs), polyciclic aromatic hydrocarbons (PAHs), etc. frequently occurred in densely populated metropolitan areas (Penache, Zoran, 2019a; Cohen et al., 2017; Penache, Zoran, 2019b; Li Q., 2020; Wu C.F. et al., 2020; Zoran et al., 2019).
Table 1.
Descriptive statistics of the Total Daily New of COVID-19 incidence and mortality cases per periods and daily mean and standard deviations of the main air pollutants, and air quality index recorded during 1 January 2020– 1 July 2021 in Madrid metropolitan region.
| Time period | Daily New COVID-19 (DNC) | Daily New COVID-19 Deaths (DND) | Daily mean ± SD |
Daily mean ± SD |
Daily mean ± SD |
Daily mean ± SD |
Daily mean ± SD |
|---|---|---|---|---|---|---|---|
| PM2.5 (μg/m3) | PM10 (μg/m3) | O3 (μg/m3) | NO2 (μg/m3) | AQI | |||
| Pre-lockdown 1 January-29 February 2020 | 38 | 0 | 29.85 ± 12.23 | 69.16 ± 22.43 | 17.51 ± 7.62 | 28.72 ± 10.02 | 28.4 ± 10.26 |
| First COVID-19 wave 1 March 2020– 30 June 2020 | 92,602 | 11,134 | 19.43 ± 9.62 | 50.85 ± 17,36 | 34.50 ± 7.06 | 11.23 ± 8.54 | 31.58 ± 6.64 |
| Heat wave 1 July 2020–9 August 2020 | 21,783 | 27 | 27.9 ± 9.65 | 40 ± 14.32 | 46.63 ± 13.8 | 16.05 ± 6.34 | 33.4 ± 5.09 |
| Second COVID-19 wave 10 August 2020–30 November 2020 | 253,444 | 5933 | 23.14 ± 8.29 | 54.65 ± 15.6 | 29.64 ± 11.72 | 21.32 ± 8.48 | 27.25 ± 7.02 |
| Third COVID-19 wave 1 December 2020–28 February 2021 | 222,114 | 8795 | 21.92 ± 15.31 | 52.08 ± 29.00 | 22.41 ± 6.98 | 22.22 ± 13.44 | 25.69 ± 8.03 |
| Forth COVID-19 wave 1 March 2021– 30 June 2021 | 139,274 | 3516 | 17.46 ± 9.15 | 43.95 ± 14.56 | 35.81 ± 7.12 | 7.40 ± 6.23 | 32.31 ± 6.51 |
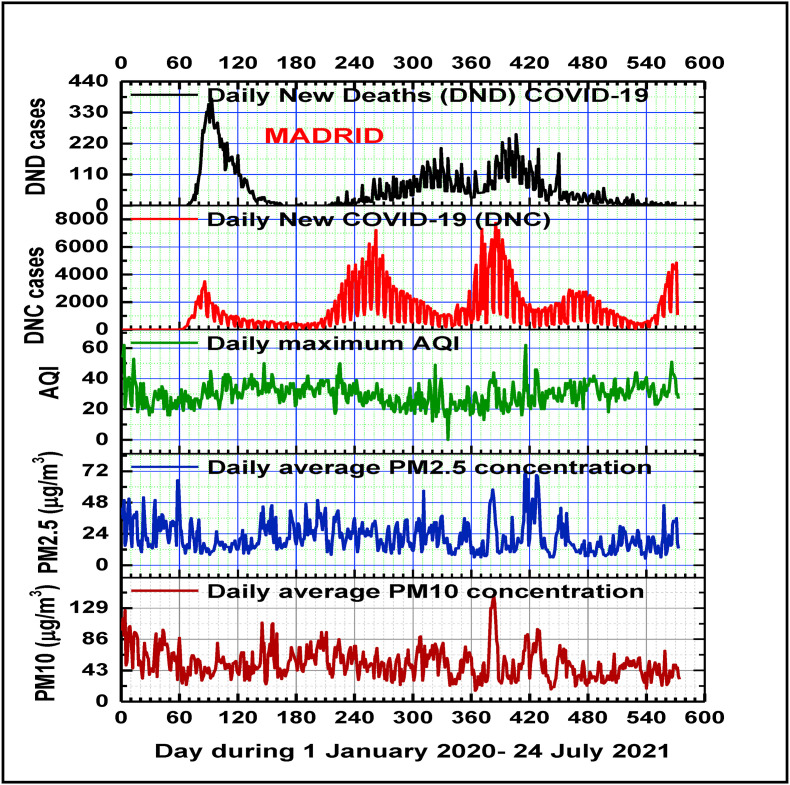
Fig. 3 Highlights that both particulate matter PM2.5 and PM10 concentrations as well as AQI follow a seasonal temporal variability pattern with higher values during winter and lower values during summer seasons being inversely correlated with Planetary Boundary Layer heights.
Fig. 3.
Temporal patterns of daily maximum AQI, and average ground levels of PM2.5, PM10, in relation with Daily New Confirmed COVID-19 cases and Daily New COVID-19 Deaths cases during the four COVID-19 pandemic waves in Madrid.
Daily mean of ground level average ozone concentrations follow also a seasonal pattern variation, but the concentrations during the four COVID-19 waves were increased in comparison with pre-lockdown period by the following factors: during lockdown and first wave period was an increase of 2.98 factor (explained by traffic and industrial related sources reduction and partially by spring seasonality), during heat wave period the increase of O3 was by a factor of 1.47 (attributed to summer seasonality and traffic-related sources), during second wave the increase of O3 was by a factor of 1.92, during the third wave the increase of O3 was by a factor of 1.44, and during the fourth wave the increase of O3 was by a factor of 2.20.
During the entire investigated period in this study, mean daily average NO2 ground level concentrations recorded decreased values as compared with the pre-lockdown period as follows: during first wave COVID-19 lockdown of 53 %, during heat waves period with 43 %, during the second COVID-19 wave with 24 %, during the third COVID-19 wave with 20 %, and during the fourth COVID-19 wave with 72 %, explained by traffic-related sources reduction, seasonal inversely variation pattern of NO2 with O3 during spring-summer seasons, when seasonal patterns of daily ground level NO2 concentrations record minimum values.
Our results support the hypothesis that through induced oxidative stress of the cardio-respiratory and immune systems, and altering the host resistance to viral and bacterial infections, urban air pollutants can increase susceptibility to morbidity and lethality from respiratory infections (Martelletti, Martelletti, 2020; Alghamdi et al., 2014; Asadi et al., 2020; Carugno et al., 2016; Romano et al., 2020; Cohen and Kupferschmidt, 2020). Recent studies considered epigenetic alteration of genes by combustion-related pollutants that can generate new viral mutations, which can favour the evolution of the COVID-19 pandemic (Bakadia et al., 2021). Clearly, urban air quality is associated with COVID-19 viral infections, and pathophysiologically, PM exposure could facilitate COVID-19 disease by increasing angiotensin-converting enzyme in the lung (Tung et al., 2021).
The anthropogenic emission sources, that were affected by the lockdown during the first COVID-19 wave and the implementation of other sanitary restrictions and partial lockdown during the second, and mainly the third COVID-19 waves, were mostly on-road mobile sources such as motor vehicles, and to a lesser extend the aircraft and industrial emissions. Like was expected, the main primary air pollutants from these combustion sources, nitrogen oxides (NOx), PM2.5, PM10, carbon monoxide (CO) and Volatile Organic Compounds (VOC) such as toluene, benzene, xylenes were decreased. But in case of ozone, a secondary pollutant, the effect can be complex and the level can increase or decrease depending on the location due to interaction of meteorology driving the dispersion of primary pollutants NOx, VOCs and the photochemical reactions forming the ozone levels across the Madrid region. Fig. 4 presents temporal patterns of daily average ground levels concentrations of ozone and nitrogen dioxide during 1 January 2020– 1 July 2021 showing the effect of total lockdown during the first COVID-19 wave, and partial lockdowns during the next COVID-19 waves in Madrid, as well as their impacts on daily new COVID-19 infections and daily new COVID-19 fatalities during the multiwaves COVID-19 pandemic.
Fig. 4.
Temporal patterns of daily average ground levels of O3, and NO2 in relation with Daily New Confirmed COVID-19 cases and Daily New COVID-19 Deaths cases during the four COVID-19 pandemic waves in Madrid.
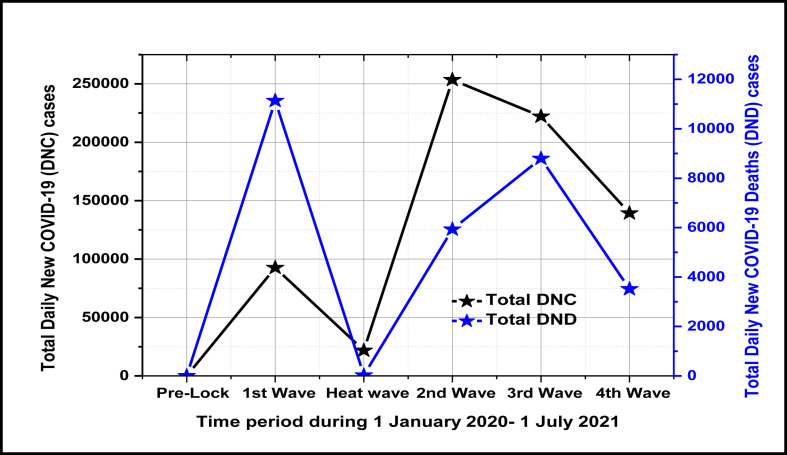
As can be seen in Table 1 and Fig. 5 during the second, the third, and the fourth COVID-19 waves, the total cumulative Daily New COVID-19 Deaths cases per waves were lower than for the first wave, because air quality was improved and also the clinical severity of the last variants of SARS-CoV-2 infections has declined significantly, most likely reflecting the impact of sanitary measures implementation (social distancing, wider face masking), improved medication treatments, or vaccination during the late third and fourth waves.
Fig. 5.
Total Daily New COVID-19 cases and Total Daily New COVID-19 Deaths per study periods (pre-lockdown, heat wave and during the each of the four COVID-19 waves).
Fig. 5 underlines that the total daily new COVID-19 confirmed positive (DNC) cases was higher for the second, the third, and the fourth waves, possible attributed to new SARS-CoV-2 variants increased virulence and increased human contacts, while the total daily new COVID-19 deaths (DND) cases was lower than for the first COVID-19 wave. During heat wave of summer 2020 the number of deaths and daily new COVID-19 cases were very low, confirming the inversely correlation with air temperatures.
Anyway, the epidemiological curve of the Daily New Confirmed COVID-19 in Madrid during the third wave was falling at 1 March 2021, but this third wave let significant damage: February 2021 was the month with the highest number of Daily New Covid-19 Deaths since the first wave of the pandemic last spring 2020.
Table 2 presents Spearman rank correlations between main air gaseous pollutants and climate variables with COVID-19 daily new cases (DNC) and COVID-19 daily new deaths (DND)in Madrid metropolitan region during each of the four COVID-19 waves recorded during entire studied period 1 March 2020–1 July 2021.
Table 2.
Spearman correlations between main air gaseous pollutants and climate variables with COVID-19 daily new cases (DNC) and COVID-19 daily new deaths (DND)in Madrid metropolitan region during the four COVID-19 waves.
| Factors | 1st COVID-19 wave |
COVID-19 Under Heat wave |
2nd COVID-19 wave |
3rd COVID-19 wave |
4th COVID-19 wave |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 March 2020–30 June 2020 |
1 July 2020–9 August 2020 |
10 August 2020–30 November 2020 |
1 December 2020–28 February 2021 |
1 March 2021–30 June 2021 |
||||||
| DNC | DND | DNC | DND | DNC | DND | DNC | DND | DNC | DND | |
| O3 (μg/m3) | r = -0.35 p < 0.01 | r = -0.25 p < 0.01 | −0.19 p > 0.05 | −0.04 p > 0.05 | r = 0.45 p < 0.01 | r = -0.59 p < 0.01 | r = -0.37 p < 0.01 | r = -0.16 p < 0.01 | r = -0.17 p < 0.01 | R = -0.35 p < 0.01 |
| NO2 (μg/m3) | r = 0.10 p > 0.05 | r = 0.40 p < 0.01 | 0.43 p < 0.01 | −0.28 p > 0.05 | r = 0.10 p > 0.05 | r = 0.55 p < 0.01 | r = 0.24 p < 0.05 | r = 0.12 p > 0.05 | r = 0.55 p < 0.01 | r = 0.49 p < 0.01 |
| T (oC) | r = -0.55 p < 0.01 | r = -0.58 p < 0.01 | 0.13 p > 0.05 | −0.32 p < 0.01 | r = 0.49 p < 0.01 | r = -0.70 p < 0.01 | r = -0.25 p < 0.05 | r = 0.46 p < 0.01 | r = -0.42 p < 0.01 | r = -0.65 p < 0.01 |
| RH (%) | r = 0.52 p < 0.01 | r = 0.65 p < 0.01 | 0.14 p > 0.05 | 0.16 p > 0.05 | r = -0.40 p < 0.01 | r = 0.69 p > 0.05 | r = 0.36 p < 0.01 | r = 0.25 p < 0.05 | r = 0.28 p < 0.01 | r = 0.32 p < 0.01 |
| w (km/h) | r = -0.45 p < 0.01 | r = -0.51 p < 0.01 | −0.28 p > 0.05 | 0.18 p > 0.05 | r = 0.18 p < 0.01 | r = -0.31 p < 0.01 | r = -0.21 p = 0.05 | r = 0.05 p > 0.05 | r = -0.26 p < 0.01 | r = -0.29 p < 0.01 |
| SI(W/m2) | r = -0.47 p < 0.01 | r = -0.45 p < 0.01 | −0.54 p < 0.01 | 0.05 p > 0.05 | r = 0.46 p < 0.01 | r = -0.80 p < 0.01 | r = 0.12 p = 0.2 > 0.05 | r = 0.53 p < 0.01 | r = -0.34 p < 0.01 | r = -0.69 p < 0.01 |
| PBL (m) | r = -0.39 p < 0.01 | r = -0.39 p < 0.01 | 0.26 p > 0.05 | −0.11 p > 0.05 | r = 0.49 p < 0.01 | r = -0.66 p < 0.01 | r = -0.32 p < 0.01 | r = -0.02 p > 0.05 | r = -0.35 p < 0.01 | r = -0.56 p < 0.01 |
Our analysis of all COVID-19 waves shows that daily average ground levels ozone concentrations are significant negative correlated with daily new deaths (DND) cases, and daily average ground levels of nitrogen dioxide are positive correlated with daily new deaths (DND) cases. Daily average ground levels of NO2 concentrations are positive correlated with COVID-19 daily new cases (DNC) for all four waves, while O3 concentrations are negative correlated with COVID-19 daily new cases (DNC) in case of the first, third and fourth COVID-19 waves and positive correlated in the case of the second wave.
The results demonstrate that urban ground surface level of air pollution with gaseous toxic especially NO2 may enhance COVID-19 incidence cases and fatality rates. Ozone is a potential oxidizer and pulmonary irritant causing an inflammatory response in the lungs as well as a cascade of subsequent responses (Arjomandi et al., 2018; Fuller et al., 2020; Ogen, 2020, Uetake et al., 2019; Zoran et al., 2013). As a highly reactive exogenous oxidant, NO2 can induce inflammation and enhance oxidative stress, which may eventually deteriorate the cardiovascular and immune systems, being a comorbidity factor in case of SARS-CoV-2 viral infections. The trends between O3 and NOx are strongly anti-correlated, showing that the O3 is strongly depressed by high NOx ( Gao W. et al., 2017). According with scientific studies in the field (Wang B. et al., 2020; Chen N. et al., 2020; Wang Y.. et al., 2020; Cohen, Kupferschmidt, 2020; Wang et al., 2021), the presence of existing comorbidities associated with patients' age, immunity system, sex, genetic and nutritional status, etc., might be essential factors for the etiology and severity of COVID-19 symptoms. The role of pre-existing immune disorders induced by long-term or short-term exposure to high ground levels of air pollutants (gaseous and PM) contributes to the impressive SARS-CoV-2 lethality in Madrid (Baldasano, 2020; Aleta, Moreno, 2020). As can be seen in Figs. 3 and 4, temporal patterns of Daily New Confirmed COVID-19 cases and Daily New COVID-19 Deaths in Madrid, this pandemic is ongoing and air pollution is a dominant environmental factor which must be considered in future COVID-19 waves decisions. Public health actions are needed to protect populations from COVID-19 disease in Madrid region with historically high NO2 and O3 exposure. Thus, air quality plays a complex role in the spreading of viral respiratory infection like novel coronavirus (Manoj et al., 2020; Cao et al., 2020). As Table 2 shows, like several recent studies investigating the relationship between COVID-19 incidence and air pollution of urban large areas, this study highlights that higher air pollution levels recorded in Madrid metropolitan region lead to greater mortality COVID-19 rates (Cole et al., 2020; Copat et al., 2020; López-Feldman et al., 2021; Pozzer et al., 2020; Travaglio et al., 2021).
3.1.2. Patterns of climate variables impact on COVID-19 waves
In order to describe the climate specific conditions over Madrid metropolitan region, which can be involved in the seasonal diffusion and severity of COVID-19 viral infection disease during different seasons over investigated time period (15 February 2020– 1 July 2021), have been analyzed the time series patterns of daily average climate parameters (air temperature, relative humidity, atmospheric pressure, precipitation rate, wind speed intensity, surface solar irradiance and Planetary Boundary Layer height).
As ambient air (Jin T., 2020) is contaminated by particulate matter, gases, bacteria, fungi and viruses, specific climate conditions can be top predictors of airborne novel coronavirus diffusion (Poole, 2020; Setti et al., 2020a, 2020b). Besides human behavior, environmental parameters are the main major factors contributing for the seasonal nature of respiratory viral infections with a high impact on respiratory SARS-CoV-2 virus stability and transmission rates (Moriyama et al., 2020).
Various diffusion patterns of COVID-19 disease transmissibility among humans, are influenced by the geographic location, season, and the local and regional climate conditions (wind speed intensity and direction, air relative humidity, air temperature and pressure, precipitation, Planetary Boundary Planetary Boundary Layer, and synoptic atmospheric circulation patterns) in which pathogen and host meet both outdoor as well as indoors (Collivignarelli et al., 2020; Poole, 2020; Conticini et al., 2020; Nuvolone et al., 2018; Shaw Stewart, 2016). The specific weather conditions and their seasonal variability in big cities (atmospheric thermal inversions, fog or haze, and extreme climate events) can have a high impact on local, regional and trans-border air pollutants and bioaerosols (viruses, bacteria and fungi) transport (Gong et al., 2020, Tobias and Querol, 2020; M. M. Sajadi et al., 2020; Zhao et al., 2021; Bontempi E., 2020; Bontempi, 2021). All types of seasonal viral human infections have been directly associated with the main climate parameters (ambient air temperature, relative air humidity, wind speed intensity, UV solar radiation, atmospheric pressure, precipitation rate) variability (Domingo et al., 2020; Domingo et al., 2020; Bashir et al., 2020; Ciencewicki and Jaspers, 2007; Barreca et al., 2012; Carugno et al., 2018; Coccia, 2020; Ballabio et al., 2013).
Table 2 presents also Spearman correlations between main climate variables (air temperature, air relative humidity, wind speed intensity, surface solar irradiance, and Planetary Boundary Layer height) with COVID-19 daily new cases (DNC) and COVID-19 daily new deaths (DND) in Madrid metropolitan region during the four COVID-19 waves. Table 3 presents a descriptive statistics of the daily mean main air climate parameters and ranges recorded during six analyzed periods for 1 January 2020– 1 July 2021 in Madrid metropolitan region.
Table 3.
Descriptive statistics of the daily mean main air climate parameters and ranges recorded during analyzed periods for 1 January 2020– 1 July 2021 in Madrid metropolitan region.
| Time period | Daily mean ± SDT (oC)Range | Daily mean ± SD RH (%) Range | Daily mean ± SD w (km/h) Range | Daily mean ± SD SI (W/m2) Range |
Daily mean ± SD PBL (m) Range |
|---|---|---|---|---|---|
| Pre-lockdown 1 January-29 February 2020 | 7.38 ± 3.12 (0.67–13.83) | 77.54 ± 12.69 (42.7–95.6) | 2.71 ± 1.98 (1.93–9.69) | 144.91 ± 28.66 (101.12–199.45) | 576.68 ± 317.66 (134–1301) |
| First COVID-19 wave 1 March 2020– 30 June 2020 | 16.60 ± 5.73 (4.61–30.56) | 60.44 ± 15.72 (30.2–95.3) | 4.98 ± 3.78 (1.49–22.37) | 309.28 ± 52.26 (202.45–372.72) | 1821.77 ± 663.39 (313–3651) |
| Heat wave 1 July –9 August 2020 | 28.74 ± 2.06 (24.83–32.39) | 31.65 ± 6.19 (21.4–47.7) | 8.82 ± 2.20 (4.18–14.00) | 342.98 ± 18.25 (302.96–375.58) | 2751.18 ± 312.31 (2108–3356) |
| Second COVID-19 wave 10 August 2020–30 November 2020 | 16.59 ± 6.24 (5.44–28.33) | 61.20 ± 1.18 (26.9–97.4) | 8.17 ± 5.13 (1.29–31.7) | 212.93 ± 66.88 (111.06–327.94) | 1414.57 ± 736.16 (415–3117) |
| Third COVID-19 wave 1 December 2020–28 February 2021 | 6.15 ± 4.77 (7.7–14.3) | 79.15 ± 10.20 (56.9–97.8) | 10.35 ± 7.42 (2.25–7.64) | 131.78 ± 26.85 (98.24–198.87) | 829.5 ± 463.74 (110–2012) |
| Forth COVID-19 wave 1 March 2021– 30 June 2021 | 15.98 ± 5.73 (14.3–27.39) | 56.81 ± 14.39 (27–53.65) | 9.01 ± 3.67 (2.74–19.96) | 311.44 ± 52.52 (173.08–376.58) | 2019.76 ± 571.05 (826–3717) |
As Table 2 shows, for each of the four COVID-19 waves, daily COVID-19 disease incidence (DND) was negative correlated with daily average air temperature and positive correlated with daily average air relative humidity, with an exception for the second COVID-19 wave. In good accordance with the existing literature in the field (Xiao et al., 2021; Tian et al., 2021; Luo et al., 2020) a linear relationships was found between all meteorological variables and COVID-19 incidence in Madrid. Table 4 shows that for entire analyzed pandemic period 15 February 2020– 1 July 2021, air temperature was negative correlated with daily new COVID-19 cases (DNC) (r = −0.15), daily new COVID-19 deaths (DND) (r = −0.64), Total COVID-19 deaths (r = −0.23), and positive correlated with Total COVID-19 incidence cases in Madrid (r = 0.11).
Table 4.
Spearman rank correlation coefficients and p values between COVID-19-incidence cases and daily average main air pollutants concentrations and climate variables for investigated metropolitan area Madrid region during entire analyzed pandemic period 15 February 2020– 1 July 2021.
| MADRID |
Air pollutant |
Climate parameter |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19 -incidence | PM2.5 (μg/m3) | PM10 (μg/m3) | O3 (μg/m3) | NO2 (μg/m3) | AQI | PBL (m) | T (oC) | RH (%) | w (Km/h) | SI (W/m2) |
| Total COVID-19 cases | 0.20* | 0.27* | 0.17* | −0.39* | 0.11* | −0.19* | 0.11* | −0.16* | 0.44* | −0.21* |
| Daily New cases (DNC) | 0.05*** | 0.14* | −0.11* | 0.22* | 0.10* | −0.16* | −0.15* | 0.15* | 0.05*** | −0.28* |
| Daily New Deaths (DND) | −0.09*** | −0.03*** | −0.50* | 0.23* | 0.22* | −0.60* | −0.64* | 0.68* | −0.28* | −0.61* |
| Total Deaths | −0.03*** | −0.04*** | −0.27* | 0.16* | 0.21* | −0.22* | −0.23* | 0.18* | 0.43* | −0.41* |
Note: PM2.5 (Particulate Matter of 2.5 μm size), PM10 (Particulate Matter of 10 μm size), O3 (ozone), NO2 (nitrogen dioxide), AQI (Global Air Quality Index), T (air temperature), RH (air relative humidity), SI (surface solar irradiance), w (wind speed intensity) and PBL (Planetary boundary Layer height), * and ** indicate p < 0.05 and p < 0.01 respectively and *** indicates p > 0.05.
From Table 5 , can be seen that for more than one year study period (1 January 2020– 1 July 2021) daily average temperature was inversely correlated with daily average relative humidity (Spearman correlation coefficient being r = −0.75, and p < 0.01).
Table 5.
Spearman correlations between main air pollutants and climate variables in Madrid metropolitan region during the entire study period (1 January 2020– 1 July 2021).
| Factors | PM2.5 (μg/m3) | PM10 (μg/m3) | O3 (μg/m3) | NO2 (μg/m3) | T (oC) | RH (%) | SI (W/m2) | w (Km/h) |
|---|---|---|---|---|---|---|---|---|
| PM10 (μg/m3) | 0.66** | |||||||
| O3 (μg/m3) | −0.15* | −0.19** | ||||||
| NO2 (μg/m3) | 0.56** | 0.49** | −0.49** | |||||
| T (oC) | 0.15* | 0.05 | 0.73** | −0.37** | ||||
| RH (%) | 0.03 | 0.09 | −0.77** | 0.30** | −0.75** | |||
| SI (W/m2) | −0.18** | −0.12* | 0.75** | −0.61** | 0.81** | −0.71** | ||
| w (Km/h) | −0.36** | −0.29** | 0.29** | −0.39** | 0.32** | −0.38** | 0.24** | |
| PBL (m) | −0.11* | −0.14* | 0.80** | −0.52** | 0.79** | −0.78** | 0.81** | 0.38** |
Note: T (air temperature), RH (air relative humidity), SI (surface solar irradiance), w (wind speed intensity) and PBL (Planetary boundary Layer height), * and ** indicate p < 0.05 and p < 0.01 respectively.
Air temperature is one of the major environmental factors that is related with seasonal and regional variation. Environmental temperature has strong and regulatory effect on the duration of survival and transmission of SARS-CoV-2 through droplet, aerosols and bioaerosols (Shi et al., 2020).
According to results of this study, cold weather is much more susceptible for the Daily New COVID viral infection transmission in Madrid than is case of good weather conditions. Hot summer 2020 conditions under heat waves events and heat island effect explained recorded reduced rates of the COVID-19 disease transmission during 30 June- August 10, 2020 in Madrid.
Our results are in good agreement with other studies, which demonstrated that air temperature and relative humidity parameters are involved in the transmission of the SARS-CoV-2 viral infection, playing an important role in COVID-19 mortality rate (Byun et al., 2021; Chen et al., 2020; Ma et al., 2020; Shi P. et al., 2020; Adams, 2020; Ahmadi et al., 2020; Poole, 2020). Although most studies indicated an inverse association of viral community spread with temperature (Jiang et al., 2020; Li H. et al., 2020; Li Q. et al., 2020; Benedetti et al., 2020; Bolaño- Ortiz et al., 2020; Sanchez-Lorenzo et al., 2021; Luo et al., 2020) some findings reported a positive relationship between temperature and the number of COVID19 cases (Bashir et al., 2020; Zoran et al., 2020b; Xie and Zhu, 2020; Pani et al., 2020) and few studied found no correlation (Briz- Redón, Serrano-Aroca, 2020).
Also, our findings are consistent with the hypothesis that higher air temperatures and summer sunlight can reduce the spread of SARS-CoV-2 and the prevalence of COVID-19, which was also suggested by most of the previous studies examining the same hypothesis with different data and approaches (Chen et al., 2021; Qi et al., 2020; P. Shi et al., 2020).
Daily average relative humidity is an essential meteorological variable of SARS-CoV-2 airborne diffusion, being involved in the formation and size of aerosol droplets, used as a medium to infect new hosts (Yang and Marr, 2012; Yang et al., 2012, 2020; Minhaz Ud-Dean, 2010). It seems that under high levels of air relative humidity large water droplets promote the growth by collision and coalescence, of suspended airborne COVID-19 and then accelerating its gravitational settling (Arias F.J., De Las Heras S., 2021). Some inconsistent findings in the relationship between air relative humidity and local transmission of SARS-CoV-2 were reported as follows: negative correlation (Jüni et al., 2020; Metelmann et al., 2020; Guo et al., 2020; Şahin, 2020; Mangla et al., 2020; Zoran et al., 2020b; Menebo, 2020) and positive correlations (Ozyigit, 2020; Oliveiros et al., 2020; Pani et al., 2020) and few studied found no correlation.
Seasonality of climate variables in the temperate regions are related with the COVID-19 pandemic disease spread. Several studies found that the changes of urban air pollution levels with aerosols and bioaerosols (fungi, bacteria and viruses) depend on multiple parameters among which anthropogenic and natural emission sources, the chemical composition of the atmosphere, local and regional meteorological conditions, relationship with Planetary Boundary Layer height (Zhao et al., 2019; Liu et al., 2020; Miao et al., 2015), synoptic atmospheric circulation patterns, micro- and meso-climatic features of the environment (Zhao et al., 2018) and geomorphology of the city.
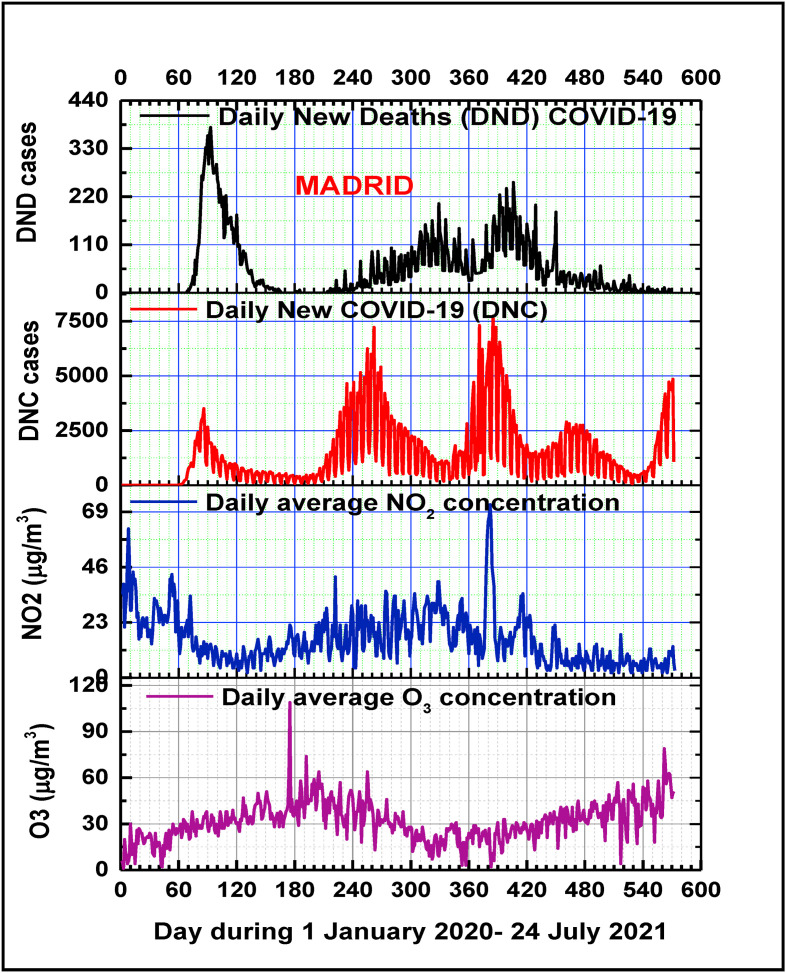
Among the climate variables, the mean of daily average wind speed intensity during 15 February 2020–1 July 2021 of recorded values (7.59 ± 5.20) km/h in the range of (0.87–31.7) km/h, had a weakly inverse relationship with the recorded Daily New COVID-19 Deaths (DND) (r = −0.28 with p < 0.01) and positive relationship with Total Confirmed COVID-19, Daily New Confirmed COVID-19 cases (r = 0.44, with p < 0.01) and Total COVID-19 Deaths cases (r = 0.18, with p < 0.01), as can be seen in Table 4. Temporal patterns of the daily average air temperature, relative humidity, wind speed intensity and Planetary Boundary Layer height in relation with dynamics of the coronavirus disease waves in Madrid are presented in Fig. 6 . Also, wind speed intensity is negatively correlated with ground level concentrations of air pollutants PM2.5(r= -0.36), PM10 (r= -0.29), NO2(r= -0.39) and relative humidity (r= -0.38), and positive correlated with O3 concentrations (r= 0.29) and surface solar irradiance (r= 0.24).
Fig. 6.
Temporal patterns of daily average air temperature, relative humidity, Planetary Boundary Layer height and solar surface irradiation in relation with Daily New COVID-19 positive cases and Daily New COVID-19 Deaths cases during the four COVID-19 pandemic waves in Madrid.
Mean surface solar global (direct and diffuse) irradiance registered in Madrid region during 1 January 2020– 1 July 2021 period of (249.79 ± 92.53) W/m2 in the range of (98.24 ± 377.09) W/m2 had an inversely relationship with all COVID-19 incidence cases (Table 3). During first COVID-19 wave in winter-spring 2020, due to lockdown measures in Spain, was recorded a reduction in anthropogenic pollution (less traffic and industrial activity led to reduction of NOx, CO2 and particulate matter PM2.5 and PM10 emissions) with direct consequence an increase in surface irradiance with respect to the 2010–2019 mean (van Heerwaarden et al., 2021). Earth's surface solar global (direct and diffuse) irradiance has seasonal variability, with altitude, geographical coordinates, stratospheric ozone, cloud cover, atmospheric density and air pollution (gases and aerosols). Our findings are in a good accordance with other studies (Metelmann et al., 2020) that evidenced a clear seasonality of COVID-19 within cities experiencing greater surface solar irradiance. Similarly with other viral infections diseases seasonal dynamics, COVID-19 disease incidence may decrease or even disappear when temperature and solar surface radiation increase in the summer (Baker et al., 2019; Obando-Pacheco et al., 2018; Santos et al., 2013). As Table 4 and Fig. 6 show, the results of this study highlight the mutual invers correlation of the daily average surface solar global irradiance with COVID-19 disease transmission in Madrid, during summer season being recorded lower daily COVID-19 incidence and mortality cases, and during winter season higher cases. Daily average precipitation rates contribution might be reflected in the daily average temperature and relative humidity and also in the atmospheric pressure.
Among the most important climate variable, the Planetary Boundary Layer height (PBL) is related to the vertical mixing, affecting the dilution of pollutants and bioaerosols (bacteria, fungi and viruses) near the ground. Also, PBL may be responsible of pandemic SARS-CoV-2 viral infection diffusion through airborne route. Lower levels of PBL heights may be associated with increased viral pathogens concentrations at the near surface, and higher transmission rates.
The mean value of daily maximum PBL height level during all investigated period in Madrid was of (1591.52 ± 846.12) m in the range of (132–3717) m.
As Table 3 shows, during each of COVID-19 pandemic wave the means of daily maximum PBL heights in Madrid recorded different values, namely: for the first COVID wave (1821.77 ± 663.39) m in the range of (313–3651) m; for the second COVID wave (1414.57 ± 736.16) m in the range of (415–3117) m; for the third COVID wave (829.5 ± 463.74) m in the range of (110–2012) m, and for the fourth COVID-19 wave (2019.76 ± 571.05) in the range of (826–3717) m.
The lower levels of PBL heights for the first and the third COVID wave may explain the highest Daily New COVID-19 confirmed positive cases and Daily New COVID-19 Deaths recorded in Madrid during that periods. From Table 4, Planetary Boundary Layer height was inversely correlated with all COVID-19 cases (with Daily New Deaths -DND cases r = −0.60, p < 0.01; Daily New cases –DNC, r = − 0.16; r = −0.19; with Total Deaths cases, r = −0.23) with Total Covid-19 cases. For each of the four COVID-19 pandemic waves (Table 2), is clear the same finding, with an exception for DNC of second COVID-wave.
Several studies revealed that urban air pollution depends on local or regional emission sources, photochemical reactions, and meteorological variables, including the thermodynamic structure of the Planetary Boundary Layer(PBL), which determines the vertical atmospheric mixing of air pollutants (Uetake et al., 2019). While in a cyclonic convective boundary layer, air quality is influenced by the dispersion/transport processes of air pollutants due to wind shears and convective turbulence, in an anticyclonic stable boundary layer, with potential temperature inversions, vertical mixing is weak, which leads to the accumulation of air pollutants (Miao, Liu, 2019; Tang et al., 2016; Li et al., 2017; Yadav et al., 2016). So, diurnal variation pattern of the PBL thermodynamic structure can affect surface concentrations of particulate matter (PM2.5 and PM10) and gaseous air pollutants (e.g. O3, NO2, CO2, SO2).
Because COVID-19 disease temporal variability is function of air pollution and meteorological seasonal variables (air temperature, relative humidity, Planetary Boundary Layer heights, solar surface irradiance, air pressure, local and regional winds and precipitation rates), like as other viral infections (human influenza virus, coronaviruses, etc.) is also seasonal sensitive. SARS-CoV-2 and its variants could exhibit seasonal patterns (Ye et al., 2020; Byun et al., 2021; Rahimi et al., 2021). Anyway seasonality of climate variables alone is not sufficient to curb the SARS-CoV-2 and its new variants transmission without intervention measures (Liu et al., 2021).
Even though the spreading of the COVID-19 pandemic is affected by several countermeasures and medical interventions, our results confirm that there is a close bidirectional seasonality of COVID-19 incidence and lethality with air pollutants and climate variables.
Spearman correlation coefficients for air pollutants and climate variable pairs for the study period are given in Table 5. Across the study period, PM2.5 concentrations were closely correlated with PM10 concentrations (Spearman rank correlation's coefficient r = 0.66), but less so of PM2.5 with NO2 (r = 0.56), and PM10 with NO2 (r = 0.49), and only weakly negative correlated of PM2.5 and respectively PM10 with O3 (r = −0.15 and r = −0.19). In addition, air temperature was highly positive correlated with O3 (r = 0.73), and negatively correlated with NO2 concentrations (r = −0.37). Air relative humidity was highly negatively correlated with ozone concentrations and air temperature, and no correlated with particulate matter PM2.5 and PM10. As is expected, surface solar irradiance is strongly positively correlated with ground level ozone concentrations (r = 0.75) and air temperature (r = 0.81), and negatively correlated with ground level nitrogen dioxide concentrations (r = −0.61), PM2.5 (r = −0.18) and PM10 (r = −0.12) and air relative humidity (r = −0.71).
As a very important climate variable in COVID-19 spatiotemporal spreading, Planetary Boundary Layer height (PBL) is inversely correlated with PM2.5 (r = −0.11), PM10 (r = −0.14), NO2 (r = −0.52) and air relative humidity (r = −0.78), and direct correlated with O3 (r = 0.80), air temperature (r = 0.79), surface solar irradiance (r = 0.81) and wind speed intensity (r = 0.38).
Is well known that climate warming and changes can play an important role in the dynamics of infectious diseases spreading (Altizer et al., 2013; Willox et al., 2015; Costello et al., 2009). Favorable environmental conditions are needed for survival, reproduction, and spread of viral infections pathogens, of their vectors and hosts (Facciola et al., 2021). Scientific literature documented significant correlations between climate parameters variability and the COVID-19 pandemic transmission (Araújo and Naimi, 2020; Aribi and Sghaier, 2020; Barcelo, 2020; Bashir et al., 2020).
3.2. Atmospheric pressure field and synoptic atmospheric circulations relation with COVID-19 waves
The epidemiological trend of the COVID-19 disease transmission in Madrid during the first 17 months of the pandemic can be uniquely categorized according to the four different waves and associated public health measures implemented in the metropolitan region and Spain:
-
1)
a first COVID-19 wave since last week of February 2020 till 30 June 2020 with an exponential increase of cases up to, 3510 DNC on 26 March 2020 and 379 DND cases on 2 April 2020, where the government implemented strict control measures during lockdown, that flattened the epidemiological curve and prolonged sporadic transmission;
-
2)
a second COVID-19 wave from late summer 2020 to end of November 2020 COVID-19 with a sharp increase of cases up to, 7225 DNC cases on 18 September 2020 and 204 DND cases on 24 November 2020, characterized by progressive easing of restrictions;
-
3)
a third COVID-19 wave from the beginning of December 2020 till the end of February 2021, that showed a progressive increase of the epidemiological curve with a maximum of 7745 DNC cases recorded on 19 January 2021 and 253 DND on 9 February 2021;
-
4)
a fourth COVID-19 wave from the beginning of March 2021 till the end of June 2021, that showed lower number of total confirmed positive cases, with a maximum of 2900 DNC on 4 March 2021 and a maximum of 379 DND on 2 April 2021. The above-mentioned pandemic waves were captured through the epidemiological surveillance system of severe symptomatic confirmed COVID-19 cases and might hide additional peculiar features of the pandemic in Madrid.
Madrid metropolitan area with Mediterranean transitions to a cold semi-arid climate, is characterized by blocking anticyclone atmospheric circulation systems and stagnant air conditions (high pressure/geopotential, low wind intensity favorable to accumulation of high levels of air pollutants due to urban traffic, industrial sources and long-distance transport of Saharan dust intrusions (Garrido-Perez et al., 2018; Borge et al., 2018; Russo et al., 2014; L'opez et al., 2019; Salvador et al., 2013; Salvador et al., 2014; Russo et al., 2020; Valverde et al., 2015; Linares et al., 2021).
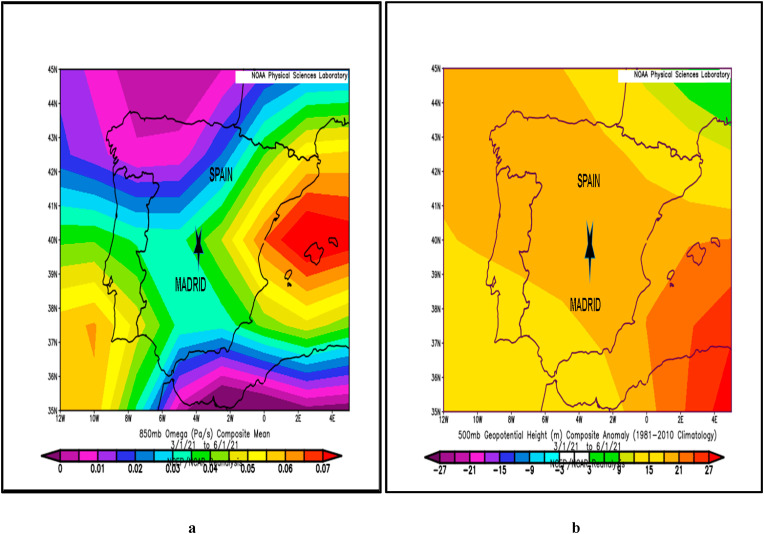
Before each of the four COVID-19 waves with at least one month, over Madrid in the mid-troposphere have been recorded anticyclonic stable atmospheric high pressure systems, frequently associated with urban high-pollution episodes and mostly related to SARS-CoV-2 virus transmission. Using NCEP/NCAR Reanalysis Intercomparison Tool provided by the NOAA/ESRL Physical Sciences Laboratory, Boulder Colorado, for each of the four COVID-19 waves, Omega surface charts composite mean (Pa/s) at 850 mb map and composite anomaly maps of 500 hPa geopotential heights over Madrid have evidenced anticyclonic stable atmospheric conditions for COVID-19 fast spreading.
-
1)
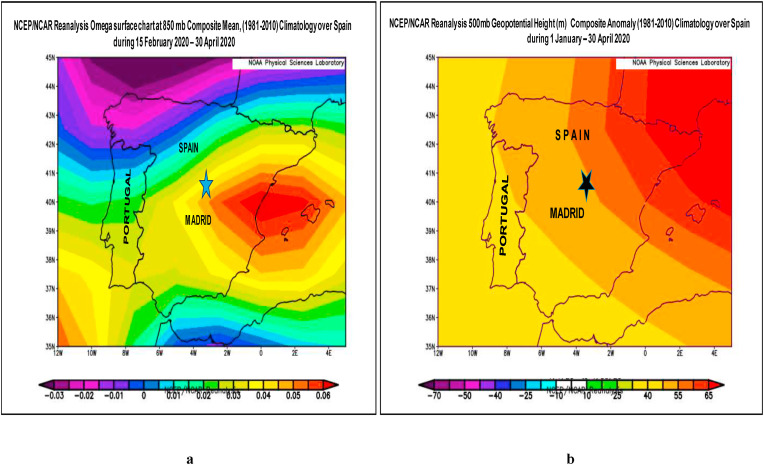
For the first COVID-19 wave, based on NCEP/NCAR Reanalysis Intercomparison Tool provided by the NOAA/ESRL Physical Sciences Laboratory, Boulder Colorado, Fig. 7a presents Omega surface chart composite mean (Pa/s) at 850 mb map over Madrid as compared to the climatology mean (1981–2010) period. This figure shows downwards airflows described by positive omega values, which characterize strong atmospheric inversion conditions. Fig. 7b presents satellite positive composite anomaly pattern in the upper troposphere of 500 mb geopotential height (m) map at 5.5 km height over Madrid during first COVID-19 wave start-up, that may have favored the SARS-CoV-2 viral infection transmission.
-
2)
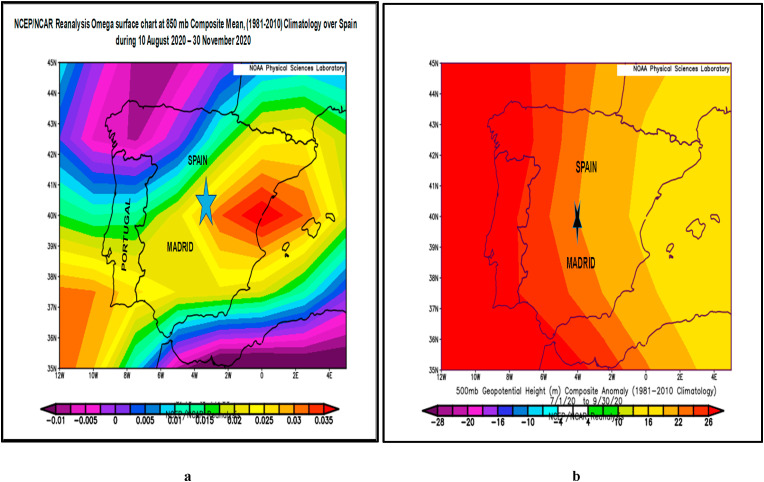
For the second COVID-19 wave, also NCEP/NCAR Reanalysis Intercomparison Tool provided useful information regarding the presence of anomalous synoptic anticyclonic circulations, with downwards airflows described by positive omega values and positive anomalies of isobaric surface heights of geopotential at 500 mb over Madrid as satellite maps present in Fig. 8 a and respectively in Fig. 8b. The comparative analysis of the first COVID-19 wave star-up in Madrid under similar anticyclone weather conditions, increase of ground level ozone and decreased air relative humidity may support the hypothesis that the strong atmospheric stability and associated dry conditions are main environmental factors related with the second COVID-19 wave start-up.
-
3)
In case of the third COVID-19 wave based on NCEP/NCAR Reanalysis Intercomparison Tool maps, before and during the third COVID-19 wave have been also recorded anomalous synoptic anticyclonic blocking atmospheric circulations with downwards airflows Omega surface satellite charts composite mean at 850 mb (Fig. 9 a) and with positive anomalies of isobaric surface heights of geopotential at 500 mb (Fig. 9b), associated with favorable stability conditions for the fast diffusion of the SARS-CoV-2. The related higher incidence and severity of COVID-19 disease in Madrid region during the third wave can be explained through existing stagnant atmospheric conditions favorable for the main air pollutants accumulation near the ground. However, clinically severe cases and lethality rates in Madrid were lower than in first COVID-19 wave (Soriano et al., 2021a, Soriano et al., 2021b, Soriano et al., 2021c).
-
3)
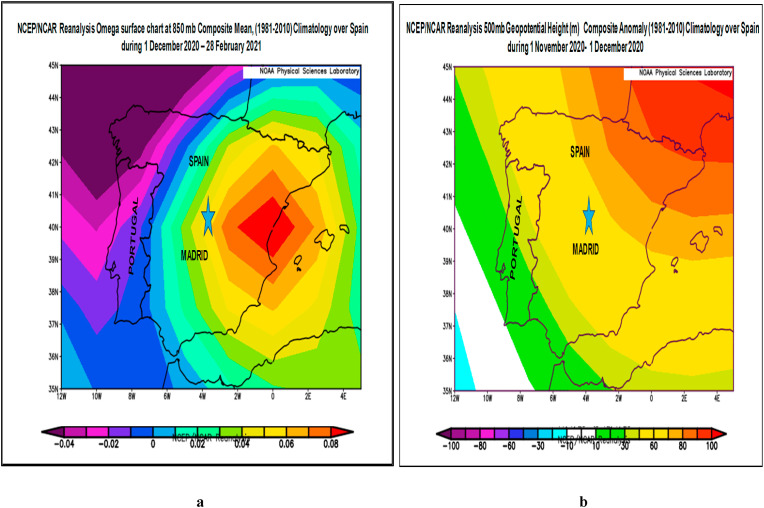
For the fourth COVID-19 wave developed in the same period of year like the first COVID-19 wave (1 March 2021–30 June 2021), NCEP/NCAR Reanalysis Intercomparison Tool charts show that before and during the viral infection wave have been registered also anomalous synoptic anticyclonic circulations, with downwards airflows described by positive omega values and positive anomalies of isobaric surface heights of geopotential at 500 mb over Madrid, as satellite maps present in Fig. 10 a and respectively in Fig. 10b. The comparative analysis of the first COVID-19 wave star-up in Madrid with the fourth COVID-19 wave under similar anticyclonic weather conditions, increase of ground level ozone and decreased air relative humidity may support the hypothesis that the strong atmospheric stability and associated climate factors seasonality are related with the fourth COVID-19 wave start-up and evolution.
Fig. 7.
a. Omega surface chart composite mean (Pa/s) at 850 mb map over Spain during the first COVID-19 wave in Madrid, b. Composite anomaly map of 500 mb geopotential height before and during the first COVID-19 wave in Madrid.
Fig. 8.
a. Omega surface chart composite mean (Pa/s) at 850 mb map over Spain during the second COVID-19 wave in Madrid. b. Composite anomaly map of 500 mb geopotential height before and during the second COVID-19 wave in Madrid.
Fig. 9.
a. Omega surface chart composite mean (Pa/s) at 850 mb map over Spain during the third COVID-19 wave in Madrid. b. Composite anomaly map of 500 mb geopotential height one month before the third COVID-19 wave in Madrid.
Fig. 10.
a. Omega surface chart composite mean (Pa/s) at 850 mb map over Spain during the fourth COVID-19 wave in Madrid. b. Composite anomaly map of 500 mb geopotential height during the fourth COVID-19 wave in Madrid.
The results of this study evidenced the significant role of meteorological conditions associated with the existing synoptic atmospheric circulations patterns before and during all COVID-19 waves in Spain, that provided optimal conditions for the SARS-CoV-2 and its new variants transmission in Madrid metropolitan region. In a good agreement with scientific literature in the field (Domingo and Rovira, 2020; Sanchez-Lorenzo et al., 2021; Liu X. et al., 2021), our analysis shows that seasonality of urban air pollution, climate and synoptic atmospheric circulations patterns may play an important role in the airborne seasonality transmission of the COVID-19 disease (Sajadi et al., 2020). However, climate variables seasonality alone is not sufficient to stop the coronavirus transmission during summer warm season. COVID-19 disease incidence analysis over time range of (15 February 2020– 1 July 2021) supports the possibility as SARS-CoV-2 viral infection transmission via airborne (Morawska and Cao, 2020) pathway to be highly dependent on independent climate variables, and regional atmospheric circulation patterns among which air temperature, relative humidity, wind speed intensity, atmospheric pressure, Planetary Boundary Layer height and surface solar global irradiance. The decrease in the fatalities rates during the second and third COVID-19 waves in comparison with the first infection wave may be attributed to the improvement in environmental conditions due to sanitary measures comparable with pre-lockdown period and adopting of different better preventive strategies and policies that reduce the health risks associated with COVID-19.
Based on results in Table 2, our study found a similar behavior of the mutual seasonality between climate variables and the first and the fourth COVID-waves in Madrid, developed in the same season of the years 2020 and respectively 2021 (1 March- 30 June).
The chemodynamics of SARS-CoV-2 virions and particulate matter interactions may be responsible for the COVID-19 pandemic transmission during several seasons, explaining reported correlations between urban high air pollution episodes registered during anticyclonic stagnant periods in densely urban/suburban regions, and new COVID-19 waves.
Other environmental factors like as waste waters, etc., can favour the growth, multiplication and spread of SARS-CoV-2 pathogens. Additional considered risk factors for fast spreading of COVID-19 disease among vulnerable population during the outbreak can be rapid urbanization, industrialization, globalization and migration of people. As other studies in the literature found, this paper suggests that the differences in the response to the COVID-19 pandemic waves periods can be attributed to different infectivity rates of new variants of SARS-CoV-2 as well as to adopted prevention and interventions strategies both at the regional and at the municipality level. Considering that timely and properly intervention polices, such as intensive contact tracing followed by quarantine and isolation, and intense vaccination procedure, can effectively reduce the spreading risk of the new more contagious SARS-CoV-2 variants (Cevik et al., 2021; Diao et al., 2021; Jin et al., 2021). In case of the fourth COVID-19 wave in Madrid metropolitan region, according to the epidemiological situation reported by World Health Organization (WHO, 2021b), and Community of Madrid (CM, 2021), at 1 August 2021 81.6 % of the total population received the first vaccine dose, and 66.8 % of the total population received the complete dose.
As a conclusion, seasonal variability of climate parameters and near the ground air pollutants concentrations may explain some important aspects in the COVID-19 disease transmission, but epidemiological measures of social distance and protection are essential. A seasonal effect of COVID-19 pandemic is potentially a significant contributor to the occurrence of multiwaves of outbreaks especially in the temperate Northern hemisphere. It is an imperative need to find the bidirectional relationship between environmental factors seasonality and COVID-19 pandemic disease ability to develop into a seasonal disease, and to provide scientific evidence for early public health strategies to reduce viral infections impacts.
3.3. Strengths and limitations
This study has added strength in having a longer observation time period over environmental factors related to COVID-19 epidemiology in Madrid metropolitan region, that spanned several seasons during 1 January 2020 till 1 July 2021, allowing us to examine a larger range of time series meteorological and air quality data over multiple months. Was also possible to make a comparison between the first and the fourth COVID-19 waves, that spanned during spring the same seasons belonging to respectively 2020 and 2021 years in Madrid. Furthermore, in an observational time series analysis of COVID-19 epidemiological data over more than one year period, we do not expect human individual risk factors to vary meaningfully over the study period. However, few studies have been focused on Madrid metropolitan region environmental factors seasonal mutual relationship with ongoing COVID-19 pandemic event.
This study has some limitations. Despite the use of official COVID-19 incidence and mortality data, under testing and underreporting throughout the course of the pandemic may have resulted in uncertainties of COVID-19 cases, limiting this study's capability to capture all COVID-19 cases. Also, due to COVID-19-related economic policies and sanitary restrictions, like lockdowns and stay-at-home measures, it is possible to be recorded lower air pollution at the ground levels, limiting this study's time correlation analysis results, with short term or long term exposure of air pollutants to individuals with pre-existing comorbidities. Despite the above limitations, our early analysis regarding the impact of environmental factors on COVID-19 transmission in Madrid could provide useful implications for policymakers in Spain and the public worldwide.
4. Conclusion
Nevertheless, being known that the airborne microbial temporal pattern is most affected by seasonal changes, we attempted to address the role of several environment parameters in driving the COVID-19 pandemic, and compare the four COVID-19 waves in Madrid. Our analysis was carried out at a metropolitan scale, to assess if the interactions between the seasonality of environmental factors could be captured and related with viral infection seasonality, being known that the airborne microbial temporal pattern is most affected by seasonal changes. Among the investigated climate variables, air temperature, relative humidity, solar surface global irradiance, Planetary Boundary Layer height, wind speed intensity and synoptic meteorological patterns are the most effective for controlling the novel coronavirus spread seasonality with higher incidence during winter-early spring and lower incidence during summer seasons. Time series analysis of Daily New COVID-19 incidence (DNC) and lethality (DND) cases in Madrid metropolitan region revealed a higher risk of mortality for the population consistently exposed to low levels of air quality and densely populated large cities. This paper demonstrates that climate factors seasonality and urban air quality are strongly implicated in the pathogenesis of COVID-19 infection and its sustained transmission. Moreover, the spatiotemporal atmospheric changes in air pollutants concentrations, and synoptic meteorological patterns may have encouraged COVID-19 multiwaves seasonality evolution to the more ubiquitous and possibly more contagious variants. This study considered also synergy effects of climate factors impacts and possible correlation among these variables with regional atmospheric circulation and COVID-19 waves start-up, synoptic meteorological patterns that may play a role in reducing or amplifying COVID-19 transmission. Also, this paper highlights a reciprocal relationship between the seasonality of COVID-19 pandemic waves and seasonality of local air pollution and climate factors, which are actively controlled by regional meteorological formation of extensive stationary anticyclone conditions with blocking effects over the region and higher COVID-19 incidence infection rates. In summary, our study found evidence that higher values of surface solar irradiances, air temperatures, Planetary Boundary Layer heights were associated with lower transmission of COVID-19. Comparison of the four COVID-19 waves found a similar behavior of the mutual seasonality between the first and the fourth COVID-waves in Madrid, developed in the same season of the years 2020 and respectively 2021 (1 March- 30 June). Even though the spreading of the COVID-19 pandemic is affected by several countermeasures and medical interventions, our results confirm that there is a close bidirectional seasonality of COVID-19 incidence and lethality with air pollutants and climate variables. This multiwaves pattern of COVID-19 in Madrid metropolitan region makes possible the further analysis of climate drivers, with descriptive statistical analysis and modelling methods for transient correlations, that identify similar variation in the time series data over localized windows of time. Meteorological conditions may play a role in reducing COVID-19 transmission, but in order to minimize the risk of resurgence, it is prudent to continue with safety practices, vaccination and implementation of prevention and control strategies of future viral pandemic infections.
Credit author statement
Maria Zoran: Conceptualization; Methodology, Supervision, Writing – review & editing. Roxana Savastru: Methodology, Validation, Review. Dan Savastru: Methodology, Validation, Review. Marina Tautan: Methodology, Validation. Laurentiu Baschir: Visualization; Software. Daniel Tenciu: Visualization; Data collection.
Consent for publication
All the co-authors consent the publication of this work.
Consent to participate
Not applicable.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This work was supported by Romanian Ministry of Research, Innovation and Digitalization Program NUCLEU Contract 18N/2021. We are thankful to NOAA/OAR/ESRL PSD, Boulder, Colorado, USA for providing useful climate data.
Abbreviation
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- COVID-19
Coronavirus Disease 2019
- SARS-CoV
Severe Acute Respiratory Syndrome Coronavirus
- MERS-CoV
Middle East respiratory syndrome coronavirus
- DNC
Daily New COVID-19 positive cases
- DND
Daily New COVID-19 Deaths
- PM
Particulate Matter: PM1(1 μm), PM2.5 (2.5 μm) and PM10(10.0 μm) diameter
- O3
Ozone
- NO2
Nitrogen dioxide
- PBL
Planetary Boundary Layer height
- T
Air temperature
- RH
Air relative humidity
- w
Wind speed intensity
- SI
Surface solar global irradiance
- NOAA
National Oceanic and Atmospheric Administration U.S.A.
References
- Adams M.D. Science of the Total Environment; 2020. Air Pollution in Ontario, Canada during the COVID-19 State of Emergency. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmadi M., Sharifi A., Dorosti S., et al. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleta A., Moreno Y. Evaluation of the potential incidence of COVID-19 and effectiveness of containment measures in Spain: a data-driven approach. BMC Med. 2020;18 doi: 10.1186/s12916-020-01619-5. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altizer S., Ostfeld R.S., Johnson P.T.J., Kutz S., Harvell C.D. Climate change and infectious diseases: from evidence to a predictive framework. Science. 2013;341:514–519. doi: 10.1126/science.1239401. [DOI] [PubMed] [Google Scholar]
- Amin M., Sorour M.K., Kasry A. Comparing the binding interactions in the receptor binding domains of SARS-CoV-2 and SARS-CoV. J. Phys. Chem. Lett. 2020;11:4897–4900. doi: 10.1021/acs.jpclett.0c01064. [DOI] [PubMed] [Google Scholar]
- Anand U., Cabreros C., Mal J., Ballesteros F., Jr., Sillanpa M., Tripathi V., Bontempi E. Novel coronavirus disease 2019 (COVID-19) pandemic: from transmission to control with an interdisciplinary vision. Environ. Res. 2021;197 doi: 10.1016/j.envres.2021.111126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araújo M.B., Naimi B. Spread of SARS-CoV-2 Coronavirus likely constrained by climate. 2020. medRxiv. [DOI]
- Arias F.J., De Las Heras S. The mechanical effect of moisturization on airborne COVID-19 transmission and its potential use as control technique. Environ. Res. 2021;197 doi: 10.1016/j.envres.2021.110940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aribi F., Sghaier M. Effect of climatic factors on the spread of COVID-19 pandemic: evidence from Tunisia. J. Sci Res. Rep. 2020;26(10):107–121. [Google Scholar]
- Arjomandi M., et al. Respiratory responses to ozone exposure. MOSES (the multicenter ozone 379 study in older subjects) Am. J. Respir. Crit. Care Med. 2018;197:1319–1327. doi: 10.1164/rccm.201708-1613OC. [DOI] [PubMed] [Google Scholar]
- Asadi S., Bouvier N., Wexler A.S., Ristenpart W.D. The coronavirus pandemic and aerosols: does COVID-19 transmit via expiratory particles? Aerosol. Sci. Technol. 2020;54(6):635–638. doi: 10.1080/02786826.2020.1749229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baay M., Lina B., Fontanet A., et al. SARS-CoV-2: virology, epidemiology, immunology and vaccine development. Biologicals. 2020;66:35–40. doi: 10.1016/j.biologicals.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baboli Z., Neisi N., Babaei A.A., Ahmadi M., Sorooshian A., Birgani Y.T., Goudarzi G. On the airborne transmission of SARS-CoV-2 and relationship with indoor conditions at a hospital. Atmos. Environ. 2021 doi: 10.1016/j.atmosenv.2021.118563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakadia B.M., Boni B.O.O., Ahmed A.A.Q., Yang G. The impact of oxidative stress damage induced by the environmental stressors on COVID-19. Life Sci. 2021;264 doi: 10.1016/j.lfs.2020.118653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker R.E., Mahmud A.S., Wagner C.E., Yang W., Pitzer V.E., Viboud C., Vecchi G.A., Metcalf C.J.E., Grenfell B.T. Epidemic dynamics of respiratory syncytial virus in current and future climates. Nat. Commun. 2019;10(1) doi: 10.1038/s41467-019-13562-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakhshandeh B., Sorboni S.G., Javanmard A.-R., et al. Variants in ACE2; potential influences on virus infection and COVID-19 severity. Infect. Genet. Evol. 2021;90 doi: 10.1016/j.meegid.2021.104773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baklanov A., Molina L.T., Gauss M. Megacities, air quality and climate. Atmos. Environ. 2016;126:235–249. doi: 10.1016/j.atmosenv.2015.11.059. [DOI] [Google Scholar]
- Baldasano J.M. COVID-19 lockdown effects on air quality by NO2 in the cities of Barcelona and Madrid (Spain) Sci. Total Environ. 2020;7411 doi: 10.1016/j.scitotenv.2020.140353. [DOI] [PubMed] [Google Scholar]
- Ballabio D., Bolzacchini E., Camatini M.C. Particle size, chemical composition, seasons of the year and urban, rural or remote site origins as determinants of biological effects of particulate matter on pulmonary cells. Environ. Pollut. 2013;176:215–227. doi: 10.1016/j.envpol.2013.01.012. [DOI] [PubMed] [Google Scholar]
- Barcelo D. An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J. Environ. Chem. Eng. 2020;84(4) doi: 10.1016/j.jece.2020.104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron Y.M. Could changes in the airborne pollutant particulate matter acting as a viral vector have exerted selective pressure to cause COVID-19 evolution? Med. Hypotheses. 2021;146 doi: 10.1016/j.mehy.2020.110401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreca A.I. Climate change, humidity, and mortality in the United States. J. Environ. Econ. Manag. 2012;63(1):19–34. doi: 10.1016/j.jeem.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., et al. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belosi F., Conte M., Gianelle V., Santachiara G., Contini D. On the concentration of SARS-CoV-2 in outdoor air and the interaction with pre-existing atmospheric particles. Environ. Res. 2021;193 doi: 10.1016/j.envres.2020.110603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedetti F., et al. Inverse correlation between average monthly high temperatures and COVID-19-related death rates in different geographical areas. J. Transl. Med. 2020;18:251. doi: 10.1186/s12967-020-02418-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biasin M., Bianco A., Pareschi G., Cavalleri A., et al. UV-C irradiation is highly efective in inactivating SARS-CoV-2 replication. Nat. Scientifc. Rep. 2021;(11) doi: 10.1038/s41598-021-85425-w. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolaño-Ortiz T.R., et al. Spread of SARS-CoV-2 through Latin America and the Caribbean region: a look from its economic conditions, climate and air pollution indicators. Environ. Res. 2020;191 doi: 10.1016/j.envres.2020.109938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. The europe second wave of COVID-19 infection and the Italy "strange" situation. Environ. Res. 2021;193 doi: 10.1016/j.envres.2020.110476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E., Vergalli S., Squazzoni F. Understanding COVID-19 diffusion requires an interdisciplinary, multi-dimensional approach. Environ. Res. 2020;188 doi: 10.1016/j.envres.2020.109814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borge R., Artínano B., Yagüe C., Gomez-Moreno F.J., Saiz-Lopez A., Sastre M., Narros A., García-Nieto D., Benavent N., Maqueda G., Barreiro M., de Andrés J.M., Cristóbal A. Application of a short term air quality action plan in Madrid (Spain) under a high-pollution episode - Part I: diagnostic and analysis from observations. Sci. Total Environ. 2018;635:1561–1573. doi: 10.1016/j.scitotenv.2018.03.149. [DOI] [PubMed] [Google Scholar]
- Borge R., Requia W.J., Yagüe C., Jhun I., Koutrakis P. Impact of weather changes on air quality and related mortality in Spain over a 25 year period [1993–2017] Environ. Int. 2019;133(B) doi: 10.1016/j.envint.2019.105272. [DOI] [PubMed] [Google Scholar]
- Bosch B.J., van der Zee R., de Haan C.A.M., Rottier P.J.M. The coronavirus spike protein is a class I virus fusion protein: structural and functional characterization of the fusion core complex. J. Virol. 2003 doi: 10.1128/jvi.77.16.8801-8811.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers R.M., Lauber C.L., Wiedinmyer C., Hamady M., Hallar A.G., Fall R., Knight R., Fierer N. Characterization of airborne microbial communities at a high-elevation site and their potential to act as atmospheric ice nuclei. Appl. Environ. Microbiol. 2009;75:5121–5130. doi: 10.1128/AEM.00447-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers R.M., Clements N., Emerson J.B., Wiedinmyer C., Hannigan M.P., Fierer N. Seasonal variability in bacterial and fungal diversity of the near-surface atmosphere. Environ. Sci. Technol. 2013;47:12097–12106. doi: 10.1021/es402970s. [DOI] [PubMed] [Google Scholar]
- Briz-Redón Á., Serrano-Aroca Á. A spatiotemporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byun W.S., Heo S.W., Jo G., Kim J.W., Kim S., Lee S., Park H.E., Baek J.-H. Is coronavirus disease (COVID-19) seasonal? A critical analysis of empirical and epidemiological studies at global and local scales. Environ. Res. 2021 doi: 10.1016/j.envres.2021.110972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calder P.C., Carr A.C., Gombart A.F., Eggersdorfer M. Optimal nutritional status for a well-functioning immune system an important factor to protect against viral infections. Nutrients. 2020;12:1–3. doi: 10.3390/nu12041181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao C., Jiang W., Wang B., Fang J., Lang J., Tian G., Jiang J., Zhu T. Inhalable microorganisms in Beijing's PM2.5 and PM10 pollutants during a severe smog event. Environ. Sci. Technol. 2014;48(3):1499–1507. doi: 10.1021/es4048472. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Y., Chen M., Dong D., Xie S., Liu M. Environmental pollutants damage airway epithelial cell cilia: implications for the prevention of obstructive lung diseases. Thorac. Cancer. 2020;11:505–510. doi: 10.1111/1759-7714.13323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carraturo F., Del Giudice C., Morelli M., Cerullo V., Libralato G., Galdiero E., Guida M. Persistence of SARS-CoV-2 in the environment and COVID-19 transmission risk from environmental matrices and surfaces. Environ. Pollut. 2020;265(B) doi: 10.1016/j.envpol.2020.115010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carugno M., Dentali F., Mathieu G., Fontanella A., Mariani J., Bordini L., Milani G.P., Consonni D., Bonzini M., Bollati V., Pesatori A.C. PM10 exposure is associated with increased hospitalizations for respiratory syncytial virus bronchiolitis among infants in Lombardy, Italy. Environ. Res. 2018;166:452–457. doi: 10.1016/j.envres.2018.06.016. [DOI] [PubMed] [Google Scholar]
- Casado-Aranda L.A., Sánchez-Fernández J., Viedma-del-Jesús M.I. Analysis of the scientific production of the effect of COVID-19 on the environment: a bibliometric study. Environ. Res. 2021;193 doi: 10.1016/j.envres.2020.110416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo M.E., Entrenas Costa L.M., Vaquero Barrios J.M., Alcalá Díaz J.F., Lopez Miranda J., Bouillon R., Quesada Gomez J.M. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 2020;203 doi: 10.1016/j.jsbmb.2020.105751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cevik M., et al. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. Lancet. 2021;2:e13–e22. doi: 10.1016/S2666-5247(20)30172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Zhang L., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/s0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Prettner K., Kuhn M., Geldsetzer P., et al. Climate and the spread of COVID-19. Sci. Rep. 2021;11 doi: 10.1038/s41598-021-87692-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciencewicki J., Jaspers I. Air pollution and respiratory viral infection. Inhal. Toxicol. 2007;19(14):1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- CM. 2021. www.comunidad.madrid/sites/default/files/doc/sanidad/210314_cam_covid 19.pdf
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J., Kupferschmidt K. Countries test tactics in “war” against COVID-19. Science. 2020;367(6484):1287–1288. doi: 10.1126/science.367.6484.1287. [DOI] [PubMed] [Google Scholar]
- Cole M.A., Elliott R.J.R., Liu B. The impact of the Wuhan COVID19 lockdown on air pollution and health: a machine learning and augmented synthetic control approach. Environ. Resour. Econ. 2020;76:553–580. doi: 10.1007/s10640-020-00483-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collivignarelli M.C., Abbà A., Bertanza G., Pedrazzani R., Ricciardi P., Miino M.C. Lockdown for CoViD-2019 in Milan: what are the effects on air quality? Sci. Total Environ. 2020;732 doi: 10.1016/j.scitotenv.2020.139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;114465 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coohill T.P., Sagripanti J.L. Bacterial inactivation by solar ultraviolet radiation compared with sensitivity to 254 nm radiation. Photochem. Photobiol. 2009;85:1043–1052. doi: 10.1111/j.1751-1097.2009.00586.x. [DOI] [PubMed] [Google Scholar]
- Copat C., Cristaldi A., Fiore M., Grasso A., et al. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ. Res. 2020;191 doi: 10.1016/j.envres.2020.110129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello A., Abbas M., Allen A., Ball S., Bell S., Bellamy R., Friel S., Groce N., Johnson A., Kett M., Lee M.C.L., Maslin M., McCoy D., McGuire B., Montgomery H., Napier D., Pagel C., Patel J., de Oliveira J.A.P., Redclift N., Rees H., Rogger D., Scott J., Stephenson J., Twigg J., Wolff J., Patterson C. Managing the health effects of climate change. Lancet. 2009;373:1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- Cuevas C.A., Notario A., Adame J.A., Hilboll A., Richter A., Burrows J.P., Saiz-López A. Evolution of NO2 levels in Spain from 1996 to 2012. Nat. Sci. Rep. 2014;4 doi: 10.1038/srep05887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Zhang Z., Froines J., Zhao J., Wang H., Yu S., et al. Air pollution and case fatality of SARS in the People's Republic of China: an ecologic study. Environ. Health. 2003;2(1):15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diao Y., Kodera S., Anzai D., et al. Influence of population density, temperature, and absolute humidity on spread and decay durations of COVID-19: a comparative study of scenarios in China, England, Germany, and Japan. One Health. 2021;12 doi: 10.1016/j.onehlt.2020.100203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz J., García-Herrera R., Trigo R.M., Linares C., Avendano A., Hernández E. The impact of summer 2003 heat wave in Iberia: how should we measure it? Int. J. Biometeorol. 2006;50:159–166. doi: 10.1007/s00484-005-0005-8. [DOI] [PubMed] [Google Scholar]
- Díaz J., Carmona R., Mirón I.J., Ortiz C., Linares C. Comparison of the effects of extreme temperatures on daily mortality in Madrid (Spain), by age group: the need for a cold wave prevention plan. Environ. Res. 2015;143:186–191. doi: 10.1016/j.envres.2015.10.018. [DOI] [PubMed] [Google Scholar]
- Díaz J., Linares C., Carmona R., Russo A., Ortiz C., Salvador P., Trigo R.M. Saharan dust intrusions in Spain: health impacts and associated synoptic conditions. Environ. Res. 2017;156:455–467. doi: 10.1016/j.envres.2017.03.047. [DOI] [PubMed] [Google Scholar]
- Díaz J., Sáez M., Carmona R., Mirón I.J., Barceló M.A., Luna M.Y., Linares C. Mortality attributable to high temperatures over the 2021–2050 and 2051–2100 time horizons in Spain: adaptation and economic estimate. Environ. Res. 2019;172:475–485. doi: 10.1016/j.envres.2019.02.041. [DOI] [PubMed] [Google Scholar]
- Domingo J., Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ. Res. 2020;187 doi: 10.1016/j.envres.2020.109650. https://doi.org/10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domingo J.L., Marqués M., Rovira J. Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A review. Environ. Res. 2020;188 doi: 10.1016/j.envres.2020.109861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du P., D R., Ren W., Lu Z., Fu P. Seasonal variation characteristic of inhalable microbial communities in PM2.5 in Beijing city, China. Science of the Total Environment 610–611. 2018:308–315. doi: 10.1016/j.scitotenv.2017.07.097. [DOI] [PubMed] [Google Scholar]
- Duval J.F.L., van Leeuwen H.P., Norde W., Town R.M. Chemodynamic features of nanoparticles: application to understanding the dynamic life cycle of SARS-CoV-2 in aerosols and aqueous biointerfacial zones. Adv. Colloid Interface Sci. 2021;290 doi: 10.1016/j.cis.2021.102400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efstratiou M.A., Tzoraki O. Coronavirus survival on beach sand: sun vs COVID-19. Mar. Pollut. Bull. 2021;167 doi: 10.1016/j.marpolbul.2021.112270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facciola A., Lagana P., Caruso G. The COVID-19 pandemic and its implications on the environment. Environ. Res. 2021;201 doi: 10.1016/j.envres.2021.111648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A., Cianfanelli L., Vlachos K., Landoni G., Cremona Severe air pollution links to higher mortality in COVID-19 patients: the "double-hit" hypothesis. J. Infect. 2020:163–4453. doi: 10.1016/j.jinf.2020.05.031. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller C.H., Jones J.W., Roblin D. Evaluating changes in ambient ozone and respiratory-related healthcare utilization in the Washington, DC metropolitan area. Environ. Res. 2020 doi: 10.1016/j.envres.2020.109603. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao M., Jia R., Qiu T., Han M., Song Y., Wang X. Seasonal size distribution of airborne culturable bacteria and fungi and preliminary estimation of their deposition in human lungs during non-haze and haze days. Atmos. Environ. 2015;118:203–210. [Google Scholar]
- Gao W., Tie X., Xu J., Huang R., Mao X., Zhou G., et al. Long-term trend of O3 in a mega City (Shanghai), China: characteristics, causes, and interactions with precursors. 2017. [DOI] [PubMed]
- Garrido-Perez J.M., Ordóñez C., García-Herrera R., Barriopedro D. Air stagnation in Europe: spatiotemporal variability and impact on air quality. Sci. Total Environ. 2018;645:1238–1252. doi: 10.1016/j.scitotenv.2018.07.238. [DOI] [PubMed] [Google Scholar]
- Giese A.C. Plenum Press; New York: 1976. Living with Our Sun's Ultraviolet Rays. (Chapter 3), 33–34. [Google Scholar]
- Glodeanu A., Gullon P., Bilal U. Social inequalities in mobility during and following the COVID-19 associated lockdown of the Madrid metropolitan area in Spain. Health Place. 2021;70 doi: 10.1016/j.healthplace.2021.102580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Losada A., Santos F.M., Gibert K., Pires J.C.M. A data science approach for spatiotemporal modelling of low and resident air pollution in Madrid (Spain): implications for epidemiological studies. Comput. Environ. Urban Syst. 2019;75:1–11. doi: 10.1016/j.compenvurbsys.2018.12.005. [DOI] [Google Scholar]
- Gong J., Qi J., Beibei E., Yin Y., Gao D. Concentration, viability and size distribution of bacteria in atmospheric bio aerosols under different types of pollution. Environ. Pollut. 2020;25 doi: 10.1016/j.envpol.2019.113485. [DOI] [PubMed] [Google Scholar]
- Gralton J., Tovey E., McLaws M.-L., Rawlinson W.D. The role of particle size in aerosolised pathogen transmission: a review. J. Infect. 2011;62:1–13. doi: 10.1016/j.jinf.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubaugh N., Hanage W., Rasmussen A. Making sense of mutation: what D614G means for the COVID-19 pandemic remains unclear. Cell. 2020;182(4):794–795. doi: 10.1016/j.cell.2020.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X.-J., et al. Transmissibility of COVID-19 and its association with temperature and humidity. PREPRINT (Version 1) Res. Square. 2020 doi: 10.21203/rs.3.rs-17715/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison R.M., Jones A.M., Biggins P.D.E., Pomeroy N., Cox C.S., Kidd S.P., et al. Climate factors influencing bacterial count in background air samples. Int. J. Biometeorol. 2005;49:167–178. doi: 10.1007/s00484-004-0225-3. [DOI] [PubMed] [Google Scholar]
- Hassanzadeh K., Pena H.P., Dragotto J., Buccarello L., Iorio F., Pieraccini S., et al. Considerations around the SARS-CoV-2 spike protein with particular attention to COVID19 brain infection and neurological symptoms. ACS Chem Nerosci. 2020;11:2361–2369. doi: 10.1021/acschemneuro.0c00373. [DOI] [PubMed] [Google Scholar]
- He D., Zhao S., Li Y., Cao P., et al. Comparing COVID-19 and the 1918–19 influenza pandemics in the United Kingdom. Int. J. Infect. Dis. 2020;98:67–70. doi: 10.1016/j.ijid.2020.06.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman J., Biegel B., Huang L. Inactivation times from 290 to 315 nm UVB in sunlight for SARS coronaviruses CoV and CoV-2 using OMI satellite data for the sunlit Earth. Air Qual. Atmos. Health. 2020 doi: 10.1007/s11869-020-00927-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heßling M., Hönes K., Vatter P., Lingenfelder C. Ultraviolet irradiation doses for coronavirus inactivation - review and analysis of coronavirus photoinactivation studies. GMS Hyg Infect Control. 2020;14 doi: 10.3205/dgkh000343. 15 Doc08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z., Huang J., Gu Q., Du P., Liang H., Dong Q. Optimal temperature zone for the dispersal of COVID-19. Sci. Total Environ. 2020;736 doi: 10.1016/j.scitotenv.2020.139487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilie P.C., Stefanescu S., Smith L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin. Exp. Res. 2020;32:1195–1198. doi: 10.1007/s40520-020-01570-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Nacional de Estadística (Spanish Statistical Office-SSO) Statistical information for the analysis of the impact of the COVID-19 crisis. 2021. https://www.ine.es/en/covid/covid_movilidad_en.htm#tablas_resultados Available online:
- Iqbal W., Tang Y.M., Chauc K.Y., Irfand M., Mohsin M. Nexus between air pollution and NCOV-2019 in China: application of negative binomial regression analysis. Process Saf. Environ. Protect. 2021;150:557–565. doi: 10.1016/j.psep.2021.04.039. [DOI] [Google Scholar]
- Islam N., Bukhari Q., Jameel Y., et al. COVID-19 and climatic factors: a global analysis. Environ. Res. 2021;193 doi: 10.1016/j.envres.2020.110355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayawardena R., Jeyakumar D.T., T V., Misra A. Impact of the vitamin D deficiency on COVID-19 infection and mortality in Asian countries. Diabetes, Metab. Syndrome: Clin. Res. Rev. 2021;15(3):757–764. doi: 10.1016/j.dsx.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Y., et al. Effect of ambient air pollutants and meteorological variables on COVID-19 incidence. Infect. Contr. Hosp. Epidemiol. 2020;41(9):1011–1015. doi: 10.1017/ice.2020.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin B., Ji J., Yang W., Yao Z., Huang D., Xu C. Process Safety and Environmental Protection; 2021. Analysis on the Spatio-Temporal Characteristics of COVID-19 in Mainland China. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins Coronavirus Resource Center COVID-19 dashboard by the center for systems science and engineering (CSSE) 2021. https://coronavirus.jhu.edu/map. Html Web.
- Jones A.M., Harrison R.M. The effects of meteorological factors on atmospheric bio aerosol concentrations - a review. Sci. Total Environ. 2004;326(1–3):151–180. doi: 10.1016/j.scitotenv.2003.11.021. [DOI] [PubMed] [Google Scholar]
- Jüni P., Rothenbühler M., Bobos P., et al. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. CMAJ May 25. 2020;192(21):E566–E573. doi: 10.1503/cmaj.200920. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karimzadeh S., Bhopal R., Nguyen Tien H. Review of infective dose, routes of transmission and outcome of COVID-19 caused by the SARS-COV-2: comparison with other respiratory viruses. Epidemiol. Infect. 2021;149(e96):1–8. doi: 10.1017/S0950268821000790. https://doi.org/10.1017/S0950268821000790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawasaki F., Wakamatsu M., Sugahara K. Trends in the prevalence of COPD in elderly individuals in an air-polluted city in Japan: a cross-sectional study. Int. J. Chronic Obstr. Pulm. Dis. 2019;14:791–798. doi: 10.2147/COPD.S189372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly F.J., Fussell J.C. Air pollution and airway disease. Clin. Exp. Allergy. 2011;41:1059–1071. doi: 10.1111/j.1365-2222.2011.03776.x. [DOI] [PubMed] [Google Scholar]
- Khan M.F., Hamid A.H., Bari M.A., Tajudin A.B., Latif M.T., et al. Airborne particles in the city center of Kuala Lumpur: origin, potential driving factors, and deposition flux in human respiratory airways. Sci. Total Environ. 2019;650(Part 1):1195–1206. doi: 10.1016/j.scitotenv.2018.09.072. [DOI] [PubMed] [Google Scholar]
- Landguth E., Holden Z., Graham J., Stark B., Mokhtari E., Kaleczyc E., et al. The delayed effect of wildfire season particulate matter on subsequent influenza season in a mountain west region of the USA. Environ. Int. 2020;139 doi: 10.1016/j.envint.2020.105668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavine J.S., et al. 2021. Immunological characteristics govern the transition of COVID-19 to endemicity, 10.1126/science.abe 6522 (2021 Science. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepeule J., Bind M.A.C., Baccarelli A.A., Koutrakis P., et al. Epigenetic influences on associations between air pollutants and lung function in elderly men: the normative aging study. Environ. Health Perspect. 2014;122:566–572. doi: 10.1289/ehp.1206458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Huang X., Yu I.T.S., Wong I.T.S., Qian H. Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air. 2004;15:83–95. doi: 10.1111/j.1600-0668.2004.00317.x. [DOI] [PubMed] [Google Scholar]
- Li X., Ma Y., Wang Y., Liu N., Hong Y. Temporal and spatial analyses of particulate matter (PM10 and PM2.5) and its relationship with meteorological parameters over an urban city in northeast China. Atmos. Res. 2017;198:185–193. doi: 10.1016/j.atmosres.2017.08.023. [DOI] [Google Scholar]
- Li H., Xu X.-L., Dai D.-W., Huang Z.Y., Ma Z., Guan Y.-J. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linares C., Carmona R., Russo A., Ortiz C., Salvador P., Trigo R.M. Saharan dust intrusions in Spain: health impacts and associated synoptic conditions Julio Díaza. Environ. Res. 2017;156:455–467. doi: 10.1016/j.envres.2017.03.047. [DOI] [PubMed] [Google Scholar]
- Linares C., Falcón I., Ortiz C., Díaz J. An approach estimating the short-term effect of NO2 on daily mortality in Spanish cities. Environ. Int. 2018;116:18–28. doi: 10.1016/j.envint.2018.04.002. [DOI] [PubMed] [Google Scholar]
- Linares C., Díaz J., Negev M., Martínez G.S., Debono R., Paz S. Impacts of climate change on the public health of the Mediterranean Basin population – current situation, projections, preparedness and adaptation. Environ. Res. 2020;182 doi: 10.1016/j.envres.2019.109107. [DOI] [PubMed] [Google Scholar]
- Linares C., Culqui D., Belda F., López-Bueno J.A., et al. Impact of environmental factors and Sahara dust intrusions on incidence and severity of COVID-19 disease in Spain. Effect in the first and second pandemic waves. Environ. Sci. Pollut. Control Ser. 2021 doi: 10.1007/s11356-021-14228-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitt J., Chan-Golston A.M., Liu J., Su J., Zhu Y., Jerrett M. Spatial analysis of COVID-19 and traffic-related air pollution in Los Angeles. Environ. Int. 2021;153 doi: 10.1016/j.envint.2021.106531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Zhou Q., Yang X., Li G., Zhang J., Zhou X., Jiang W. Cytotoxicity of the soluble and insoluble fractions of atmospheric fine particulate matter. J. Environ. Sci. 2020;91:105–116. doi: 10.1016/j.jes.2020.01.012. [DOI] [PubMed] [Google Scholar]
- Liu X., Huang J., Li C., et al. The role of seasonality in the spread of COVID-19 pandemic. Environ. Res. 2021;195 doi: 10.1016/j.envres.2021.110874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López V., Salvador P., Artínano B., Gomez-Moreno F.J., Fernández J., Molero F. Influence of the origin of the air mass on the background levels of atmospheric particulate matter and secondary inorganic compounds in the Madrid air basin. Environ. Sci. Pollut. Res. 2019;26(29):30426–30443. doi: 10.1007/s11356-019-06205-8. [DOI] [PubMed] [Google Scholar]
- López-Feldman A., Heres D., Marquez-Padilla F. Air pollution exposure and COVID-19: a look at mortality in Mexico City using individual-level data. Sci. Total Environ. 2021;756 doi: 10.1016/j.scitotenv.2020.143929. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C., Liu X., Jia Z. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo C., Yao L., Zhang L., Yao M., Chen X., Wang Q., et al. Possible transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in a public bath center in huai'an, Jiangsu Province, China. JAMA network open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo W., et al. The role of absolute humidity on transmission rates of the COVID-19 outbreak. Med Rxiv. 2020 2020. 02.12.20022467. [Google Scholar]
- Luo X., Liao Q., Shen Y., Li H., Cheng L. Vitamin D deficiency is associated with COVID-19 incidence and disease severity in Chinese people. J. Nutr. 2021;151:98–103. doi: 10.1093/jn/nxaa332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle C.D., Sagripanti J.-L. Predicted inactivation of viruses of relevance to biodefense by solar radiation. J. Virol. 2005;79:14244–14252. doi: 10.1128/JVI.79.22.14244-14252.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Zhou J., Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724(138226):1059–1071. doi: 10.1016/j.scitotenv.2020.138226. Allergy 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangla S., et al. Impact of environmental indicators on the COVID-19 pandemic in Delhi, India. PREPRINT (Version 1) Res. Square. 2020 doi: 10.21203/rs.3.rs-66969/v1. available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manoj M.G., Satheesh Kumar M.K., Valsaraj K.T., Sivan C., Vijayan S.K. Potential link between compromised air quality and transmission of the novel corona virus (SARS-CoV-2) in affected areas. Environ. Res. 2020;190 doi: 10.1016/j.envres.2020.110001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquès M., Rovira J., Nadal M., Domingo J.L. Effects of air pollution on the potential transmission and mortality of COVID-19: a preliminary case-study in Tarragona Province (Catalonia, Spain) Environ. Res. 2021;192 doi: 10.1016/j.envres.2020.110315. https://doi.org/10.1016/j.envres.2020.110315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martelletti L., Martelletti P. Air pollution and the novel Covid-19 disease: a Putative disease risk factor. SN Compr. Clin. Med. 2020;2:383–387. doi: 10.1007/s42399-020-00274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menebo M.M. Temperature and precipitation associate with Covid-19 new daily cases: a correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020;737 doi: 10.1016/j.scitotenv.2020.139659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metelmann S., et al. Impact of climatic, demographic and disease control factors on the transmission dynamics of COVID-19 in large cities worldwide. Med Rxiv. 2020 doi: 10.1101/2020.07.17.20155226. 2020.07.17.20155226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mhuireach G.A., Betancourt-Román C.M., Green L., Johnson B.R. Spatiotemporal controls on the urban aerobiome. Front. Ecol. Evol. 2019;7 [Google Scholar]
- Miao Y., Liu S. Linkages between aerosol pollution and planetary boundary layer structure in China. Sci. Total Environ. 2019;650:288–296. doi: 10.1016/j.scitotenv.2018.09.032. [DOI] [PubMed] [Google Scholar]
- Miao Y., Hu X.-M., Liu S., Qian T., Xue M., Zheng Y., Wang S. Seasonal variation of local atmospheric circulations and boundary layer structure in the Beijing-Tianjin-Hebei region and implications for air quality. J. Adv. Model. Earth Syst. 2015;7 doi: 10.1002/2015MS000522. [DOI] [Google Scholar]
- Minhaz Ud-Dean S.M. Structural explanation for the effect of humidity on persistence of airborne virus: seasonality of Influenza. J. Theor. Biol. 2010;264:822–829. doi: 10.1016/j.jtbi.2010.03.013. [DOI] [PubMed] [Google Scholar]
- Molepo K.M., Abiodun B.J., Magoba R.N. The transport of PM10 over Cape Town during high pollution episodes. Atmos. Environ. 2019;213:116–132. https://doi.org/10.1016/j.atmosenv.2019.05.041. [Google Scholar]
- Montero J.M., Fernández-Avilés G. Functional kriging prediction of atmospheric particulate matter concentrations in Madrid, Spain: is the new monitoring system masking potential public health problems? J. Clean. Prod. 2018;175:283–293. [Google Scholar]
- Monzón A., Guerrero M.J. Valuation of social and health effects of transport-related air pollution in Madrid (Spain) Sci. Total Environ. 2004;334–335:427–434. doi: 10.1016/j.scitotenv.2004.04.069. [DOI] [PubMed] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139 doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriyama M., Hugentobler W.J., Iwasak A. Seasonality of respiratory viral infections. Ann. Rev. Virol. 2020;7:83–101. doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- Mousavizadeh L., Ghasemi S. Genotype and phenotype of COVID-19: their roles in pathogenesis. J. Microbiol. Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.03.022. https://doi.org/10.1016/j.jmii.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mu F., Li Y., Lu R., Qi Y., Xie W., Bai W. Source identification of airborne bacteria in the mountainous area and the urban areas. Atmos. Res. 2020;231 [Google Scholar]
- Nishiura H., Lintona N.M., Akhmetzhanov A.R. Serial interval of novel coronavirus (COVID-19) infections. Int. J. Infect. Dis. 2020;93:284–286. doi: 10.1016/j.ijid.2020.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nor N.S.M., Wai Y.C., Ibrahim N., Rashid Z.Z., Mustafa N., Hamid H.H.A., et al. Particulate matter (PM2.5) as a potential SARS-CoV- 2 carrier. Sci. Rep. 2021;11(2508) doi: 10.1038/s41598-021-81935-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuvolone D., Petri D., Voller F. The effects of ozone on human health. Environ. Sci. Pollut. Res. 2018;25:8074–8088. doi: 10.1007/s11356-017-9239-3. [DOI] [PubMed] [Google Scholar]
- Obando-Pacheco P., Justicia-Grande A.J., Rivero-Calle I., Rodriguez-Tenreiro C., et al. Respiratory syncytial virus seasonality: a global overview. J. Infect. Dis. 2018;217(9):1356–1364. doi: 10.1093/infdis/jiy056. [DOI] [PubMed] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveiros B., et al. Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. Med Rxiv. 2020 03.05.20031872. https://doi.org/10.1101/2020.03.05.20031872. [Google Scholar]
- Ozyigit A. Understanding Covid-19 transmission: the effect of temperature and health behavior on transmission rates. Infect. Dis. Health. 2020;25(4):233–238. doi: 10.1016/j.idh.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandolfi M., Tobias A., Alastuey A., Sunyer J., Schwartz J., Lorente J., Pey J., Querol X. Effect of atmospheric mixing layer depth variations on urban air quality and daily mortality during Saharan dust outbreaks. Sci. Total Environ. 2014;494–49:283–289. doi: 10.1016/j.scitotenv.2014.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pani S.K., Lin N.-H., Babu S.R. Association of COVID-19 pandemic with meteorological parameters over Singapore. Sci. Total Environ. 2020;740 doi: 10.1016/j.scitotenv.2020.140112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penache M.C., Zoran M. Temporal patterns of surface ozone levels in relation with radon (222Rn) and air quality. AIP Conference Proceedings 2075. 2019 doi: 10.1063/1.5091279. [DOI] [Google Scholar]
- Penache M.C., Zoran M. Seasonal trends of surface carbon monoxide concentrations in relation with air quality. AIP Conference Proceedings 2075. 2019 doi: 10.1063/1.5091292. [DOI] [Google Scholar]
- Perrone M.G., Larsen B.R., Ferrero L., Sangiorgi G., De Gennaro G., Udisti R., Zangrando R., Gambaro A., Bolzacchini E. Sources of high PM2.5 concentrations in Milan, North- ern Italy: molecular marker data and CMB modelling. Sci. Total Environ. 2012;414:343–355. doi: 10.1016/j.scitotenv.2011.11.026. [DOI] [PubMed] [Google Scholar]
- Perrone M.G., Gualtieri M., Consonni V., Ferrero L., Sangiorgi G.M.L., Longhin E.M., Sandrini S., Fuzzi S., Piazzalunga A., Prati P., Bonasoni P., Cavalli F., Bove M.C., et al. Spatial and seasonal variability of carbonaceous aerosol across Italy. Atmos. Environ. 2014;99:587–598. doi: 10.1016/j.atmosenv.2014.10.032. [DOI] [Google Scholar]
- Pfahl S., Schwierz C., Croci-Maspoli M., Grams C.M., Wernli H. Importance of latent heat release in ascending air streams for atmospheric blocking. Nat. Geosci. 2015;8:610–614. doi: 10.1038/NGEO2487. [DOI] [Google Scholar]
- Pollán M., Pérez-Gómez B., Pastor-Barriuso R., Oteo J., Hernán M.A., Pérez-Olmeda M., et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396:535–544. doi: 10.1016/S0140-6736(20)31483-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole L. 2020. Seasonal influences on the spread of SARS-CoV-2 (COVID19), causality, and Forecastabililty (3-15-2020). Causality, and Forecastabililty 3-15–2020. (March 15, 2020) [Google Scholar]
- Pozzer A., Dominici F., Haines A., Witt C., Munzel T., Lelievel J. Regional and global contributions of air pollution to risk of death fromCOVID-19. Cardiovasc. Res. 2020;116:2247–2253. doi: 10.1093/cvr/cvaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., et al. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138778. https://doi. org/10.1016/j.scito tenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian Z., He Q., Lin H.M., et al. Part 2. Association of daily mortality with ambient air pollution, and effect modification by extremely high temperature in Wuhan, China. Res. Rep. Health Eff. Inst. 2010;154:91–217. [PubMed] [Google Scholar]
- Rahimi N.R., Fouladi-Fard R., Aali R., et al. Bidirectional association between COVID- 19 and the environment: a systematic review. Environ. Res. 2021;194 doi: 10.1016/j.envres.2020.110692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram K., Thakur R.C., Singh D.K., et al. Why airborne transmission hasn't been conclusive in case of COVID-19? An atmospheric science perspective. Sci. Total Environ. 2021 doi: 10.1016/j.scitotenv.2021.145525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayan R.A. Seasonal variation and COVID-19 infection pattern: a gap from evidence to reality. Curr Opin Environ Sci Health. 2021 doi: 10.1016/j.coesh.2021.100238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivellese F., Prediletto E. ACE2 at the centre of COVID-19 from paucisymptomatic infections to severe pneumonia. Autoimmun. Rev. 2020 doi: 10.1016/j.autrev.2020.102536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano S., Perrone M.R., Becagli S., Pietrogrande M.C., Russo M., Caricato R., Lionetto M.G. Ecotoxicity, genotoxicity, and oxidative potential tests of atmospheric PM10 particles. Atmos. Environ. 2020;221 [Google Scholar]
- Russo A., Trigo R.M., Martins H., Mendes M.T. NO2, PM10 and O3 urban concentrations and its association with circulation weather types in Portugal. Atmos. Environ. 2014;89:768–785. [Google Scholar]
- Russo A., Sousa P.M., Durẵo R.M., Ramos A.M., Salvador P., Linares C., Díaz J., Trigo R.M. Saharan dust intrusions in the Iberian Peninsula: predominant synoptic conditions. Sci. Total Environ. 2020;717 doi: 10.1016/j.scitotenv.2020.137041. [DOI] [PubMed] [Google Scholar]
- Sagripanti J.L., Lytle C.D. Estimated inactivation of coronaviruses by solar radiation with special reference to COVID-19. Photochem. Photobiol. 2020;96:731–737. doi: 10.1111/php.13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin M. Impact of weather on COVID-19 pandemic in Turkey. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saiz-López A., Borge R., Notario A., Adame J.A., de la Paz D., et al. Unexpected increase in the oxidation capacity of the urban atmosphere of Madrid, Spain. Nat. Sci. Rep. 2017;7 doi: 10.1038/srep45956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajadi M.M., et al. Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19) JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles-Wilhelm F., Amoroso A. 2020. Temperature and Latitude Analysis to Predict Potential Spread and Seasonality for COVID-19. (Available at: SSRN 3550308) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvador P., Artíñano B., Alonso D.G., Querol X., Alastuey A. Identification and characterisation of sources of PM10 in Madrid (Spain) by statistical methods. Atmos. Environ. 2004;38(3):435–447. [Google Scholar]
- Salvador P., Artíñano B., Viana M., Alastuey A., Querol X. Evaluation of the changes in the Madrid metropolitan área influencing air quality: analysis of 1999-2008 temporal trend of particulate matter. Atmos. Environ. 2012;57:175–185. [Google Scholar]
- Salvador P., Artínano B., Molero F., Viana M.M., Pey J., Alastuey A., Querol X. African dust contribution to ambient aerosol levels across central Spain: characterization of long-range transport episodes of desert dust. Atmos. Res. 2013;127:117–129. [Google Scholar]
- Salvador P., Molero F., Fernández A.J., Tobías A., Pandol M., et al. Synergistic effect of the occurrence of African dust outbreaks on atmospheric pollutant levels in the Madrid metropolitan area. Atmos. Res. 2019;226:208–218. [Google Scholar]
- Salvador P., Barreiro M., Gómez-Moreno F.-J., Alonso- Blanco E., Artínano B. Synoptic classification of meteorological patterns and their impact on air pollution episodes and new particle formation processes in a south European air basin. Atmos. Environ. 2021;245 2021. [Google Scholar]
- Sanchez-Lorenzo A., Vaquero-Martínez J., Calbó J., Wild M., Santurtún A., Lopez-Bustins J.A., Vaquero J.M., Folini D., Antón M. Anomalous atmospheric circulation favor the spread of COVID-19 in Europe? Environ. Res. 2021;194 doi: 10.1016/j.envres.2020.110626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos A.L., et al. Effects of UV radiation on the lipids and proteins of bacteria studied by mid-infrared spectroscopy. Environ. Sci. Technol. 2013;47 doi: 10.1021/es400660g. [DOI] [PubMed] [Google Scholar]
- Schuit, et al. Airborne SARS-CoV-2 is rapidly inactivated by simulated sunlight. J. Infect. Dis. 2020;222:564–571. doi: 10.1093/infdis/jiaa334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seposo X., Ueda K., Sugata S., Yoshino A., Takami A. Short-term effects of air pollution on daily single- and co-morbidity cardiorespiratory outpatient visits. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.138934. [DOI] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M., Palmisani J. Airborne transmission route of COVID-19: why 2 meters/6 feet of inter-personal distance could not Be enough. Int. J. Environ. Res. Publ. Health. 2020;17(8) doi: 10.3390/ijerph17082932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M., Palmisani J., et al. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: first evidence. Environ. Res. 2020;188 doi: 10.1016/j.envres.2020.109754. https://doi.org/10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang J., Ye G., Shi K., Wan Y., Luo C., Aihara H., et al. Structural basis of receptor recognition by SARS-CoV-2. Nature 1-8. 2020 doi: 10.1038/s41586-020-2179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw Stewart P.D. Seasonality and selective trends in viral acute respiratory tract infections. Med. Hypotheses. 2016;86:104–119. doi: 10.1016/j.mehy.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., et al. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138890. https://doi. org/10.1016/j.scito tenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., Dong Y., Yan H., et al. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano V., Ganado-Pinilla P., Sánchez-Santos M., Gómez-Gallego F., Barreiro P., de Mendoza C., et al. Main differences between the first and second waves of COVID-19 in Madrid, Spain. Int. J. Infect. Dis. 2021 doi: 10.1016/j.ijid.2021.02.115. http://dx.doi.org/10.1016/j.ijid.2021.02.115 S1201-9712(21)00201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano V., de Mendoza C., Gómez-Gallego F., Corral O., Barreiro P. Third wave of COVID-19 in Madrid, Spain. Int. J. Infect. Dis. 2021;107:212–214. doi: 10.1016/j.ijid.2021.04.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano V., Meiriño R., Corral O., Guallar M.P. Severe acute respiratory syndrome coronavirus 2 antibodies in adults in Madrid, Spain. Clin. Infect. Dis. 2021;72:1101–1102. doi: 10.1093/cid/ciaa769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart S. Seasonality and selective trends in viral acute respiratory tract Infections. Med. Hypotheses. 2016;86:104–119. doi: 10.1016/j.mehy.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiyama J.T., Ueda K., Seposo X.T., Nakashima A., Kinoshita M., Matsumoto H., et al. Health effects of PM2.5 sources on children's allergic and respiratory symptoms in Fukuoka. Sci. Total Environ. 2020;709 doi: 10.1016/j.scitotenv.2019.136023. https://doi.org/10.1016/j.scitotenv.2019.136023. [DOI] [PubMed] [Google Scholar]
- Sundell N., Andersson L.-M., Brittain-Long R., Lindh M., Westin J. A four year seasonal survey of the relationship between outdoor climate and epidemiology of viral respiratory tract infections in a temperate climate. J. Clin. Virol. 2016;84:59–63. doi: 10.1016/j.jcv.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tager I.B., et al. Chronic exposure to ambient ozone and lung function in young adults. Epidemiology. 2005;16:751–759. doi: 10.1097/01.ede.0000183166.68809.b0. [DOI] [PubMed] [Google Scholar]
- Tang G., Zhang J., Zhu X., Song T., Munkel C., Hu B., Schafer K., Liu Z., Zhang J., Wang L., Xin J., Suppan P., Wang Y. Mixing layer height and its implications for air pollution over Beijing, China. Atmos. Chem. Phys. 2016;16:2459–2475. doi: 10.5194/acp-16-2459-2016. [DOI] [Google Scholar]
- Thompson H., Mousa A., Dighe A., Fu H., Arnedo-Pena A., Barrett P., et al. SARS-CoV-2 setting-specific transmission rates: a systematic review and meta-analysis. Clin Infect Dis.ciab100. 2021 doi: 10.1093/cid/ciab100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F., Liu X., Chao Q., Qian Z.(M.), Zhang S., Qi L., Niu Y., Arnold L.D., Zhang S., Li H., Xu J., Lin H., Liu Q. Ambient air pollution and low temperature associated with case fatality of COVID-19: a nationwide retrospective cohort study in China. Innovation. 2021 doi: 10.1016/j.xinn.2021.100139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tignat-Perrier R., Dommergue A., Thollot A., Magand O., Amato P., Joly M., Sellegri K., Vogel T.M., Larose C. Seasonal shift in airborne microbial communities. Sci. Total Environ. 2020;716 doi: 10.1016/j.scitotenv.2020.137129. [DOI] [PubMed] [Google Scholar]
- Tobias A., Querol X., et al. Changes in air quality during the lockdown in Barcelona (Spain) one month into the SARS-CoV-2 epidemic. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M., Yu Y., Popovic R., Selley L., Leal N.S., Martins L.M. Links between air pollution and COVID-19 in England. Environ. Pollut. 2021;268 doi: 10.1016/j.envpol.2020.115859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung N.T., Cheng P.C., Chi K.H., Hsiao T.C., Jones T., BéruBé K., et al. Particulate matter and SARS-CoV-2: a possible model of COVID-19 transmission. Sci. Total Environ. 2021;750 doi: 10.1016/j.scitotenv.2020.141532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uetake J., Tobo Y., Uji Y., Hill T.C.J., DeMott P.J., Kreidenweis S., Misumi R. Seasonal changes of airborne bacterial communities over Tokyo and influence of local meteorology. Bio Rxiv. 2019 doi: 10.1101/542001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valverde V., Pay M.T., Baldasano J.M. Circulation-type classification derived on a climatic basis to study air quality dynamics over the Iberian Peninsula. Int. J. Climatol. 2015;35:2877–2897. [Google Scholar]
- Valverde V., Pay M.T., Baldasano J.M. Ozone attributed to Madrid and Barcelona on-road transport emissions: characterization of plume dynamics over the Iberian Peninsula. Sci. Total Environ. 2016;543:670–682. doi: 10.1016/j.scitotenv.2015.11.070. [DOI] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Heerwaarden C.C., Mol W.B., Veerman M.A., et al. Record high solar irradiance in Western Europe during first COVID-19 lockdown largely due to unusual weather. Commun. Earth Environ. 2021;2:37. [Google Scholar]
- Vejerano E.P., Marr L.C. Physico-chemical characteristics of evaporating respiratory fluid droplets. J. R. Soc. Interface. 2018;15 doi: 10.1098/rsif.2017.0939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls A.C., Park Y.-J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181(2):281–292. doi: 10.1016/j.cell.2020.02.058. e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Du H., Xu Y., Lu D., Wang X., Guo Z. Temporal and spatial variation relationship and influence factors on surface urban heat island and ozone pollution in the Yangtze River Delta, China. Sci. Total Environ. 2018;631–632:921–933. doi: 10.1016/j.scitotenv.2018.03.050. [DOI] [PubMed] [Google Scholar]
- Wang B., Li Y., Xie Z., Du S., Zeng X., Hou J., Ma T. Characteristics of microbial activity in atmospheric aerosols and its relationship to chemical composition of PM2.5 in Xi’an, China. J. Aerosol Sci. 2020;146 [Google Scholar]
- Wang R., Hozumi Y., Yin C., Wei G.-W. Mutations on COVID-19 diagnostic targets. Genomics. 2020;112(6):5204–5213. doi: 10.1016/j.ygeno.2020.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Chen Y., Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J. Med. Virol. 2020;92:568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T., Rovira J., Sierra J., Blanco J., Chen S.-J., Mai B.-X., Schuhmacher M., Domingo J.L. Characterization of airborne particles and cytotoxicity to a human lung cancer cell line in Guangzhou, China. Environ. Res. 2021;196 doi: 10.1016/j.envres.2021.110953. [DOI] [PubMed] [Google Scholar]
- WHO Science brief: SARS-CoV-2 and potential airborne transmission. 2020. https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html
- WHO COVID-19 weekly epidemiological update - 12 January 2021. 2021. https://www.who.int/docs/default-source/coronavir use/situation-reports/weekly_epidemiological_update_22.pdf [WWW Document] 1.13.21.
- WHO 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- Willox A.C., Stephenson E., Allen J., Bourque F., Drossos A., Elgarøy S., Kral M.J., Mauro I., Moses J., Pearce T. Examining relationships between climate change and mental health in the Circumpolar North. Reg. Environ. Change. 2015;15:169–182. doi: 10.1007/s10113-014-0630-z. [DOI] [Google Scholar]
- Wilson W.E., Suh H.H. Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J. Air Waste Manag. Assoc. 1997;47(12):1238–1249. doi: 10.1080/10473289.1997.10464074. [DOI] [PubMed] [Google Scholar]
- Wong K.W., Fung P.C.W., Chow W.K. COVID-19: a physical model. Open J. Biophys. 2020;10:88–95. doi: 10.4236/ojbiphy.2020.102008. [DOI] [Google Scholar]
- Worldometer Info, 2021. https://www.worldometers.info/.
- Wu C.F., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H., Zhang L., Zhou X., Du C., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurtzer S., Marechal V., Mouchel J.M., et al. Evaluation of lockdown impact on SARS-CoV-2 dynamics through viral genome 2 quantification in Paris wastewaters. 2020. medRxiv preprint. [DOI] [PMC free article] [PubMed]
- Wurtzer S., Waldman P., Ferrier-Rembert A., et al. Several forms of SARS-CoV-2 RNA can be detected in wastewaters: Implication for wastewater-based epidemiology and risk assessment. Water Res. 2021;198 doi: 10.1016/j.watres.2021.117183. https://doi.org/10.1016/j. watres.2021.117183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao S., Qi H., Ward M.P., Wang W., et al. Meteorological conditions are heterogeneous factors for COVID-19 risk in China. Environ. Res. 2021;198 doi: 10.1016/j.envres.2021.111182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav R., Sahu L.K., Beig G., Jaaffrey S.N.A. Role of long-range transport and local meteorology in seasonal variation of surface ozone and its precursors at an urban site in India. Atmos. Environ. 2016;176–177:96–107. [Google Scholar]
- Yang W., Marr L.C. Mechanisms by which ambient humidity may affect viruses in aerosols. Appl. Environ. Microbiol. 2012;78:6781–6788. doi: 10.1128/AEM.01658-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., Elankumaran S., Marr L.C. Relationship between humidity and influenza A viability in droplets and implications for Influenza's seasonality. PloS One. 2012;7 doi: 10.1371/journal.pone.0046789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Peng F., Wang R., Guana K., Jiang T., Xue G., Suna J., Chang C. The deadly coronaviruses: the 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J. Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye G., Pan Z., Pana Y., et al. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J. Infect. 2020;80(5):E14–E17. doi: 10.1016/j.jinf.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J., Wu Y., Jing W., Liu J., Du M., Wang Y., Liu M. Association between meteorological factors and daily new cases of COVID-19 in 188 countries: a time series analysis. Sci. Total Environ. 2021;780 doi: 10.1016/j.scitotenv.2021.146538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin. Immunol. 2020 doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao L., Oppenheimer M., Zhu Q., Baldwin J.W., Bou-Zeid E., Guan K., Liu X. Interactions between urban heat islands and heat waves. Environ. Res. Lett. 2018;1(3) [Google Scholar]
- Zhao Y., Richardson B., Takle E., Chai L., Schmitt D., Win H. Airborne transmission may have played a role in the spread of 2015 highly pathogenic avian influenza outbreaks in the United States. Sci. Rep. 2019;9 doi: 10.1038/s41598-019-47788-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao K., Luo H., Yuan Z., Xu D., Du Y., et al. Identification of close relationship between atmospheric oxidation and ozone formation regimes in a photochemically active region. J. Environ. Sci. 2021;102:373–383. doi: 10.1016/j.jes.2020.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou C., Wei G., Xiang J., Zhang K., Li C., Zhang J. Effects of synoptic circulation patterns on air quality in Nanjing and its surrounding areas during 2013–2015. Atmos. Pollut. Res. 2018;9:723–734. doi: 10.1016/j.apr.2018.01.015. [DOI] [Google Scholar]
- Zoran M., Savastru R., Savastru D., Miclos S., Mustata M.N., Baschir L. Urban landcover mapping using multiple endmember spectral mixture analysis. J. Optoelectron. Adv. Mater. 2008;10(3):701–706. [Google Scholar]
- Zoran M.A., Savastru R.S., Savastru D.M., Dida A.I., Ionescu O.M. Urban vegetation land covers change detection using multi-temporal MODIS Terra/Aqua data. Remote sensing for agriculture, ecosystems, and hydrology XV Book Series Proceedings of SPIE. 2013;8887 doi: 10.1117/12.2028710. Article Number 888720. [DOI] [Google Scholar]
- Zoran M., Savastru D., Tautan M.N., Baschir L. Use of satellite data for land surface radiative parameters retrieval of Bucharest metropolitan zone. J. Optoelectron. Adv. Mater. 2019;21(7–8):470–483. [Google Scholar]
- Zoran A.M., Savastru S.R., Savastru M.D., Tautan N.M. Assessing the relationship between ground-levels of ozone (O3) and nitrogen dioxide (NO2) with coronavirus (COVID-19) in Milan, Italy. Sci. Total Environ. 2020;740 doi: 10.1016/j.scitotenv.2020.140005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran A.M., Savastru S.R., Savastru M.D., Tautan N.M. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci. Total Environ. 2020;738 doi: 10.1016/j.scitotenv.2020.139825. https://doi.org/10.1016/j.scitotenv.2020.139825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zowalaty M.E., Järhult J. From SARS to COVID-19: a previously unknown SARS- related coronavirus (SARS-CoV-2) of pandemic potential infecting humans - call for a One Health approach. One Health. 2020;9 doi: 10.1016/j.onehlt.2020.100124. [DOI] [PMC free article] [PubMed] [Google Scholar]