Abstract
Background
Herpes simplex virus (HSV) encephalitis is a known cause of cognitive deterioration, neurological disturbances, and seizures though are rarely associated with sinus node dysfunction.
Case summary
We present a 54-year-old man admitted to the hospital with a 10-day history of fever, confusion, and fatigue, 1 week following a transient loss of consciousness. An initial workup suggested HSV encephalitis and the patient was started on intravenous Acyclovir. Due to his episode of syncope, a 24 h Holter electrocardiogram monitoring was performed. The Holter documented multiple episodes of sinus arrest, with a second episode of syncope noticed by the hospital staff concurrent with the last documented sinus arrest. Following antiviral treatment and resolution of the encephalitis we noticed complete resolution of sinus node dysfunction. We subsequently avoided permanent pacemaker implantation.
Discussion
Our case of proven HSV encephalitis complicated by sinus node arrest and syncope with complete resolution following antiviral treatment suggests no indication for permanent pacemaker implantation. This approach is consistent with data from previously reported cases.
Keywords: Case report, Syncope, Herpes simplex encephalitis, Sinus arrest
For the podcast associated with this article, please visit https://academic.oup.com/ehjcr/pages/podcast
Learning points
Sinus node dysfunction is a rare but important complication of herpes simplex encephalitis.
These patients may require closer cardiac monitoring and additional workup.
It is also a transient and reversible cause of sinus node arrest with treatment of the underlying encephalitis, and permanent pacing may not be required.
Introduction
Herpes simplex encephalitis (HSE) is a well-documented cause of cognitive impairment, focal neurologic deficits, and convulsions. It is also a rare and potentially reversible cause of sinus node dysfunction and arrest.1–3 While the mechanism underlying this phenomenon is not fully understood a few explanations have been suggested1,4,5 and this reversibility puts into questions the need for long-term pacing. We describe this association in a 54-year-old man with fever, confusion, and syncope.
This case also highlights the importance of initial syncope workup in identifying high-risk features,6 especially those associated potentially rapid clinical deterioration.
Timeline
| Event | |
|---|---|
| 10 days prior to admission | Onset of fever, confusion, and fatigue |
| 7 days prior to admission | Transient loss of consciousness |
| Day 0 | Patient presents to the emergency room with fever and fatigue. He is alert and haemodynamically stable. Twelve-lead electrocardiogram (ECG) and non-contrast head computed tomography (CT) are unremarkable |
| Day 1 |
Admission to internal ward Initial fever workup does not identify the source of patient's symptoms |
| Day 2 |
Patient is placed on 24 h Holter ECG Gradual cognitive impairment is noticed Head CT angiography demonstrated changes at the left hemispheric blood vessels and lumbar puncture confirms herpes simplex encephalitis Patient is started on parenteral Acyclovir |
| Day 3 |
Syncopal episode noticed by staff Holter documents five episodes of sinus arrest; prominent ones being 11 and 32 s Patient is transferred to intensive cardiac care unit |
| Day 5 | Cognition is fully restored, fever subsides |
| Day 7 | Patient is transferred back to internal ward, completes 14 days of parenteral Acyclovir treatment |
| Day 9 | Subsequent Holter ECG revealed normal heart rate without any evidence of bradycardia |
| Day 16 | Upon discharge an implanted loop recorder was considered but rejected by the patient |
| 5 months later | A follow-up Holter ECG documented normal heart rate and no evidence of bradycardia |
| 12 months follow-up | Patient is doing well and had no further episodes of syncope or documented bradycardia |
Case presentation
A 54-year-old man was admitted to the hospital with a 10-day history of fever, confusion, and fatigue. One week prior to admission he had a transient loss of consciousness (TLC). He reported standing up after a strained defecation, after which he lost consciousness. He woke up seconds later, lying down on his bathroom floor having no memory of the event. There was no report of incontinence; he had no early symptoms such as lightheadedness or palpitations, any chest pain, headache, or subsequent confusion.
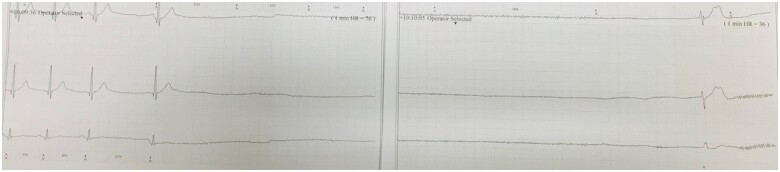
Upon admission, he was alert and haemodynamically stable, with a temperature of 39°C. Physical examination was otherwise normal and 12-lead electrocardiogram (ECG) was unremarkable (Figure 1). A head computed tomography (CT) excluded cerebral haemorrhage.
Figure 1.
Baseline electrocardiogram—normal sinus rhythm of 75 beats per minute. PR segment, QRS segment, and QT segment are within normal range, no conduction abnormalities.
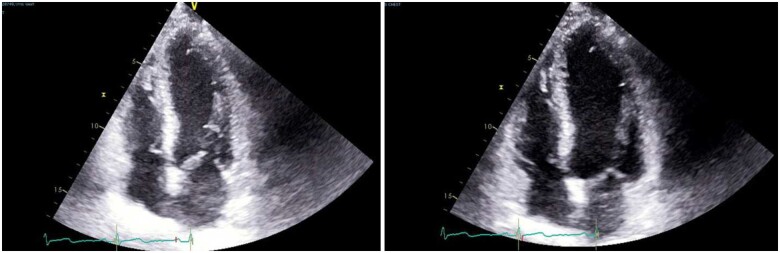
His medical history is notable for smoking and he was not taking any medications or illicit drugs. He was immunocompetent and there was no history of immunosuppressive or immunomodulatory treatment. He had no family history of cardiovascular disease or sudden cardiac death. One year prior to the present admission, he was hospitalized for chest pain and underwent coronary angiography with normal coronary anatomy. Transthoracic echocardiography was also performed and was normal (Figure 2).
Figure 3.
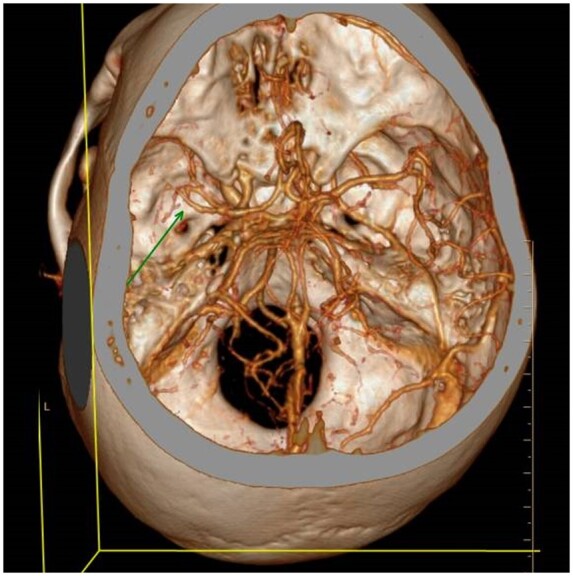
Reconstructed image from brain computed tomography angiography demonstrating changes in the left hemispheric blood vessels middle cerebral artery and anterior cerebral artery A1 segment correlating with cerebral vasculitis or angiitis. Arrowhead—narrow, irregular, and beading like appearance of middle cerebral artery M1, M2 segments.
An initial workup including chest radiography, urinalysis, complete blood count, routine blood chemistries, human immunodeficiency viruses immunoassay, and blood and urine cultures did not reveal the source of his fever. Thereafter, a gradual cognitive impairment, aphasia, and facial asymmetry were noticed, prompting further investigation by CT angiography (CTA) of the brain and neck, lumbar puncture, and empiric antiviral treatment with intravenous Acyclovir. Our differential diagnosis at this point mainly comprised of vasculitis/angiitis, meningoencephalitis, and stroke. CTA demonstrated changes at the left hemispheric blood vessels correlating with cerebral vasculitis or angiitis (Figure 3). Lumbar puncture showed mildly elevated protein level of 50 mg/dL (normal values 5–20 mg/dL), normal glucose level of 56 mg/dL, with blood glucose of 90 mg/dL, and marked pleocytosis with a lymphocytic predominance (86%). Polymerase chain reaction analysis from the cerebrospinal fluid confirmed the presence of herpes simplex virus (HSV). Magnetic resonance imaging (MRI) test was not performed due to its unavailability, although it may have shown potential cerebral lesions, which might have been missed by CT, and prompt the diagnosis of HSV encephalitis.
Figure 4.
Sinus pause of 32 s with return to junctional rhythm.
Due to his syncopal event, a 24 h Holter ECG monitoring was performed a day before the Lumbar Puncture (LP) test. The Holter documented five episodes of sinus arrest; prominent ones being 11 and 32 s at 06:13 and 10:09 o'clock accordingly (Figure 4). The average heart rhythm documented was sinus at 80 beats per minute (b.p.m.), with a minimal sinus rate of 65 b.p.m. and a maximal rate of 112 b.p.m. During this last sinus arrest, the patient had a TLC that was noticed by the staff. He was urgently transferred to the intensive cardiac care unit (ICCU) for further assessment and monitoring. During his stay in the ICCU, his cognitive impairment and focal deficits resolved and the fever subsided. He had no further episodes of syncope or documented bradycardia. Repeated echocardiography was also normal. Due to the potentially reversible underlying cause and complete recovery of his symptoms and heart rate, the decision was made not to implant a cardiac pacemaker.
Figure 2.
Representative images of the echocardiography (apical four-chamber view).
Our patient was subsequently transferred back to the internal ward and completed an unremarkable 14 days of treatment with intravenous Acyclovir. Subsequent Holter ECG revealed normal heart rate without any evidence of bradycardia.
Upon discharge, an implanted loop recorder was considered, but was rejected by the patient. At 1 year follow-up, he was stable and had no further episodes of syncope or documented bradycardia. Follow-up Holter ECG performed 5 months after discharge documented normal heart rate and no evidence of bradycardia.
Discussion
HSE is a known cause of cognitive deterioration, neurological disturbances, and seizures though are rarely associated with sinus node dysfunction.
Three cases of proven herpes encephalitis with syncope and sinus arrest have been described in the literature, one ended in death due to lack of antiviral treatment1 and two ended in resolution of symptoms after antiviral treatment without the need for a permanent pacemaker.2,3
The aetiology of sinus node dysfunction complicating HSE is not fully understood, but seems to result from lesions of the central nervous system and not from primary cardiac injury. Indeed, in the case presented by Pollock et al.,1 no structural abnormalities were found in the patient's necropsy, suggesting an ultra-structural source of damage induced by disruption of sympathetic and parasympathetic signalling.4 Involvement of insular cortex in seizures and stroke predisposes patients to ECG changes and cardiac arrhythmogenesis by increasing cardiac sympathetic tone4 and lesions of insular cortex or sub-insular white matter may result in impaired control of blood pressure, heart rate, and ultimately life-threatening cardiac arrhythmias.5 A proposed model of insular specialization entails the right insula as the centre for sympathetic autonomic control and the left insula as the centre for parasympathetic control,5 supporting the notion that right insular lesions decrease sympathetic tone resulting in parasympathetic over activity which can lead to bradyarrhythmia and ultimately asystole.5
The stimulation of regions within the central autonomic network triggering efferent parasympathetic pathways and favouring the development of bradyarrhythmia can also be the mechanism underlying the rare phenomenon of ictal asystole.6 In the context of HSE, it might be difficult to distinguish between ictal syncope and HSE induced sinus node arrest without a simultaneous recording of electroencephalogram (EEG) and ECG.
Clarifying the reason for the non-traumatic TLC in this unique case is worth addressing. In the Emergency Room (ER), the working assumption was reflex orthostatic syncope and not cardiac syncope. This is in view of the anamnesis suggesting a fall while the patient is standing, post-defecation, without palpitations or chest discomfort. The patient denied having any structural heart disease or family history of Sudden Cardiac Death (SCD), along with a normal physical examination and ECG.
The differential diagnosis of epileptic seizures causing TLC was rejected in the first stage due to the lack of description of myoclonic movements by eyewitnesses and a rapid return to full consciousness and awareness. The correct diagnosis turned out to be arrhythmic syncope due to herpes encephalitis.
Nevertheless, the fever from which the patient has suffered and the history of a change in state of consciousness in recent days, despite a normal neurological examination, are high-risk features suggesting a serious condition and justifying a broader neurological examination that may include LP and MRI examinations. Performing these tests in the early stages could have led to earlier diagnosis and treatment, which have a prognostic significance in herpes encephalitis. In retrospect, an EEG could be helpful in supporting the diagnosis of HSE, distinguishing encephalitis from seizures, and differentiate (with concomitant ECG) HSE sinus node dysfunction from ictal bradyarrhythmias.
Our case of proven HSE complicated by sinus node arrest and syncope with complete resolution following antiviral treatment suggests no indication for permanent pacemaker implantation. This approach is consistent with data from previously reported cases.
This case indicates, as highlighted in the ESC syncope guidelines, that the primary aim for an ED clinician is establishing an underlying diagnosis of syncope and identified high-risk features; especially those associated potentially rapid clinical deterioration.
Lead author biography

Dana Braiman is a 34-year-old internal ward specialist working in Soroka Hospital, Be'er Sheva, Israel. She recently completed her internship at Soroka medical centre and her field of interest is mainly intensive care medicine. While specializing in internal medicine she had a chance to experience ICCU and work extensively in the medical ICU, corona ICU, and E.R. She is currently a member of the Young Community of the European Society of Cardiology and vastly involved in the teaching of medicine and point-of-care US skills.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: The authors report no conflicts of interest related to the subject of this paper.
Funding: None declared.
Supplementary Material
References
- 1. Pollock S, Reid H, Klapper P, Metcalfe RA, Ahmed N.. Herpes simplex encephalitis presenting as the sick sinus syndrome. J Neurol Neurosurg Psychiatry 1986;9:331–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Smith BK, Cook MJ, Prior DL.. Sinus node arrest secondary to HSV encephalitis. J Clin Neurosci 2008;15:1053–1056. [DOI] [PubMed] [Google Scholar]
- 3. Nicol P-P, Talarmin J-P, Joseph T.. Herpes simplex encephalitis, an unusual cause of sinus node dysfunction: case report and literature review. Int J Clin Cardiol 2015;2: 1–4. [Google Scholar]
- 4. Oppenheimer SM, Wilson JX, Guiraudon C, Cechetto DF.. Insular cortex stimulation produces lethal cardiac arrhythmias: a mechanism of sudden death? Brain Res 1991;550:115–121. [DOI] [PubMed] [Google Scholar]
- 5. Sörös P, Hachinski V.. Cardiovascular and neurological causes of sudden death after ischaemic stroke. Lancet Neurol 2012;11:179–188. [DOI] [PubMed] [Google Scholar]
- 6. Benditt DG, Van Dijk G, Thijs RD.. Ictal asystole: life-threatening vagal storm or a benign seizure self-termination mechanism? Circ Arrhythm Electrophysiol 2015;8:11–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.