Researchers review exercise as an adjunctive treatment for women survivors of sexual violence and call for trauma-informed implementation efforts in future exercise interventions for this population.
Keywords: Physical activity, Health promotion, Trauma-informed care, Implementation, Gender
Abstract
Compared to their male counterparts, women experience alarmingly high rates of sexual violence (SV). Nearly 20% of women in the USA have been victims of SV, and prevalence of sexual assault among female service members is reported to be even higher, up to 50%. SV results in negative health outcomes like posttraumatic stress disorder, depression, obesity, poor body image, and pain-related disability. Exercise has been shown to positively impact both mental and physical health outcomes in populations experiencing posttraumatic symptoms, yet women survivors of SV are often excluded from exercise trials in trauma-affected populations. The purpose of this paper is to comment on the importance of incorporating women-specific trauma-informed principles in the content and delivery of exercise interventions in trauma-affected populations, particularly as it relates to SV. Researchers discuss the implications of female-specific and trauma-informed exercise considerations for SV survivors. This commentary highlights the need for trauma-informed implementation efforts and outcome measurements in exercise interventions involving women affected by SV. Researchers call for (a) increased qualitative work on trauma-specific implementation efforts across exercise intervention domains and (b) increased assessment of trauma-specific outcomes in exercise trials.
Implications.
Practice: To encourage participation of women survivors of SV in physical activity, exercise professionals need to consider trauma-informed principles when hiring exercise staff and maintaining exercise environment.
Policy: Policymakers need to promote enrollment of women in exercise and trauma trials in larger numbers.
Research: Future research should investigate trauma-informed implementation efforts to increase representation of trauma-affected women in exercise trials and assess all relevant psychosomatic symptoms SV survivors experience to include as outcomes in trials.
INTRODUCTION
Women are frequently exposed to traumatic events that can impact their health over a lifetime. Women are likely to experience sexual violence (SV), whereas traumatic events for men include higher rates of combat, accidents, natural disasters, and violence [1]. SV is defined as any sexual act or attempt to obtain a sexual act by violence or coercion by any person regardless of their relationship to the victim in any setting [2]. An estimated 18.3% of women in the USA have been victims of SV, with prevalence of sexual assault among female service members being reported at up to 52.5% [3, 4]. SV has been shown to predict the development of trauma-related symptoms (clinical and subclinical posttraumatic stress disorder, PTSD) more strongly than any other trauma [5, 6]. Women experience high rates of PTSD, with estimates ranging from 8.0% in civilian women to 13.4% in female veterans. This is nearly double the rate of men [1]. Another 3.6%–25.6% of all people experience significant trauma-related stress symptoms that do not meet full diagnostic criteria for PTSD [7].
Negative health outcomes like depression [3, 8], functional impairment [9], cardiovascular disease [10], and chronic pain [3, 11], as well as increased risk of metabolic disorders and inflammatory diseases (e.g., rheumatoid arthritis and fibromyalgia) [11,12], are prevalent among individuals with trauma-related psychological symptoms. Survivors of SV experience unique, additional health risks, including body image disorders, emotion dysregulation, disordered eating, pain-related disability, and overweight/obesity [5, 13–17]. This myriad of psychosomatic symptoms contributes to poor lifestyle behaviors, including low physical activity, increased sedentary behavior, and unhealthy diet [18]. Additionally, biases within the medical system, such as weight prejudice, stigmatization of SV, and misdiagnosis of pain contribute to women receiving inadequate care for these trauma-related health conditions [19–21]. All these considerations make nonpharmacological behavioral interventions (i.e., exercise) a valuable treatment option in this population. The purpose of this paper is to review exercise as a potential adjunctive treatment for women survivors of SV and advocate increased representation of women survivors in exercise trials. Researchers call for trauma-informed implementation efforts and outcome measures in future exercise interventions in this population.
Exercise as a potential adjunctive treatment
Women survivors can address SV-related posttraumatic symptoms (PTS) via several mental health treatment options. Gold standard psychotherapy treatments (prolonged exposure and cognitive processing therapy) for PTS are effective at improving symptoms but experience poor retention and substantial dropout [22, 23]. Residual symptoms, such as depression, anxiety, and poor quality of life often remain following clinical treatment for PTS [24]. These treatments and associated behavioral interventions, such as behavioral activation therapy and cognitive behavioral therapy (CBT), address mental health symptomatology without directly targeting associated chronic physical health conditions (i.e., cardiovascular and inflammatory diseases, metabolic disorders, and chronic pain). Physical activity represents an intervention with potential to lower the risk of chronic disease, decrease disease severity, and improve psychological symptoms. There is also evidence supporting exercise as a stepped care approach to PTS treatment [25, 26]. For instance, starting SV survivors with exercise and slowly moving toward a wellness model may make them more open to trauma-focused therapy [25, 26]. Exercise could, thus, be an effective adjuvant therapy before, after, or concurrently with mental health treatment.
Evidence on exercise in women survivors of SV is promising but limited. To our knowledge, there has been only four exercise studies targeting women survivors of SV, two using a walking intervention [27, 28] and two using yoga [29, 30]. The strongest evidence of a beneficial effect of exercise in women with a history of SV comes from a randomized controlled trial of yoga compared to health education for PTSD symptoms [29]. Another randomized trial found that acute meditation plus moderate intensity walking reduced posttraumatic cognitions and ruminative thoughts in women with a history of SV compared to a wait list control [28]. Other smaller, single-arm studies using yoga or CBT plus aerobic exercise also report improvements in PTSD symptoms and self-compassion [27, 30]. These few studies suffer methodological limitations. None of these studies offered a multicomponent exercise intervention that includes aerobic endurance and strengthening activities as recommended in public health guidelines [31, 32]; therefore, they may not be sufficient to effectively improve SV-related health conditions [33, 34]. There is a lack of information gathered on changes in clinical health indicators and physical function outcomes. Additionally, limiting exercise mode to exclusively yoga or walking excludes women who prefer exercise modalities such as weightlifting or interval training and misses an opportunity to understand how these activities may impact health-related outcomes.
In the absence of sufficient exercise trials in women survivors of SV, it is helpful to consider exercise research examining trauma more broadly. There is substantial and growing evidence showing that exercise improves PTSD symptoms, as well as related comorbid chronic physical and mental health conditions (i.e., anxiety, depression, quality of life, and physical functioning) [25, 29, 34–42]. Despite women’s high rates of PTSD (many of these PTSD cases stemming from SV), women are underrepresented in exercise and PTSD literature and trauma type is rarely assessed, making it unclear which results can be generalized to women survivors of SV [43]. Researchers examined all seven randomized controlled trials of exercise and PTS completed since 2014. All of these trials reported improvements in PTS symptoms and associated comorbid physical and mental health conditions following exercise [25, 29, 38–42]. Relative to gender makeup of these studies, two of the trials were female only, [29, 42] and five trials were mixed gendered [25, 29, 38–42]. The mixed-gendered randomized controlled trials enrolled a combined total of 213 study participants, of which 53 (25%) were women. Only one of these trials (sample was 82% female, 18 women and 4 men) reported trauma type, with half of the participants reporting sexual assault. Analyses by trauma type and/or gender were not performed, likely due to limitations of small sample size [38].
Preliminary exercise research in women survivors of SV, along with more established literature in exercise and PTSD, indicates that exercise has the potential to be an effective adjunctive treatment for women survivors of SV experiencing PTS symptoms. The paucity of published research on women survivors’ perceptions and response to exercise makes it challenging to develop and implement programs that take into consideration the distinct characteristics of this population. This evidence base could be enhanced by (a) increasing the number of women survivors of SV in mixed-gendered exercise and PTS trials; (b) enrolling sufficient numbers of women to allow analysis by gender and trauma type; and (c) increasing the development of targeted interventions specifically for women survivors of SV.
Trauma-informed implementation for exercise trials
Trauma-informed care (TIC) is broadly defined as incorporating trauma-informed approaches into program development and implementation (SAMHSA) [44]. Trauma-informed approaches include (a) realizing the widespread impact of trauma on individuals, (b) recognizing the signs and symptoms of trauma, (c) responding by fully integrating knowledge about trauma into policies, procedures, and practices, and (d) seeking to actively resist retraumatization [44]. These approaches adhere to key principles, including safety, trustworthiness and transparency, peer support, collaboration and mutuality, empowerment, choice, and responsiveness to cultural, historic, and gender issues [44]. TIC emphasizes resilience and positive adaptation to adversity over pathology [45]. In the context of SV, TIC broadly means that programs acknowledge the impact of SV on all aspects of women’s lives; it necessitates prioritizing survivors’ needs, perspectives, and choices.
Implementing TIC principles in behavioral interventions optimizes therapeutic outcomes and minimizes adverse effects on the study participants [45, 46]. TIC aims to avoid negative interactions with the health care system, which can exacerbate SV-related PTS symptoms and discourage survivors from seeking future care for trauma-related health conditions [46]. Examples of trauma-informed methods in psychotherapy interventions for women survivors of SV include: believing the survivor’s experience, psychoeducation on the impact of SV, focusing treatment on specific areas of concern for survivors of SV (i.e., guilt and risk of revictimization), and emphasizing self-esteem and empowerment [44–48]. Despite increased incorporation of TIC in health care services, TIC in health promotion and exercise programs remains largely unexplored. Survivors of SV have experienced an extreme violation of trust and loss of bodily autonomy and may be less likely to become involved in exercise research with unknown research staff members. Integrating trauma-informed principles and adapting them for exercise interventions represents an opportunity to more effectively engage this at-risk and underserved population.
To our knowledge, there has been only one study in women survivors of SV examining beliefs or attitudes toward physical activity [49]. This qualitative study revealed mixed feelings from participants concerning bodily awareness that accompanies exercise: some survivors feared it, other women welcomed the opportunity for bodily connection. Most survivors reported a preference for exercising individually and without the presence of men. The study indicated that competence, relatedness, and autonomy are needed for exercise motivation among women survivors of SV. Social-contextual factors of the exercise environment appeared critical. For instance, having the option of exercising in the presence of other women survivors seemed to promote a sense of relatedness that increased survivor’s motivation to exercise. In this study, the Rape Crisis Center (RCC) provided survivors with an environment they trusted and other participants to whom they could relate. Overall, survivors voiced a desire to exercise along with a view of exercise as being beneficial to their mental health.
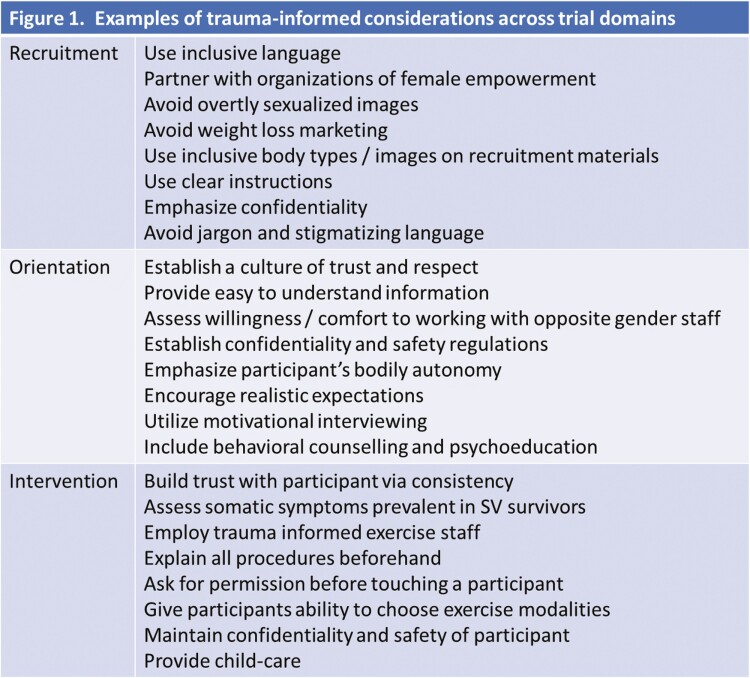
To effectively engage SV survivors in exercise interventions, researchers need to identify additional aspects of SV survivorship that may uniquely affect participation in physical activity trials (and/or contribute to sedentary behaviors) and consider these barriers/facilitators in trial development. Exercise professionals should adopt and study additional trauma-informed elements specific to exercise engagement. These approaches should be evidence based and must be considered across the full spectrum of intervention development: participant recruitment, patient education prior to initiating exercise, and the content and delivery method of the exercise prescription. In the absence of robust evidence on exercise-specific TIC, information from other behavioral intervention types can be used to improve exercise enjoyment and adherence in women survivors of SV. Figure 1 suggests a list of considerations across development and implementation stages further detailed below.
Fig 1.
Examples of trauma-informed considerations across trial domains.
Recruitment
Actively building relationships with community partners that empower women survivors of SV is a necessary part of engaging this population in trials. Partnering with community organizations, such as RCC and Young Women’s Christian Associations (YWCA), and legal aid offices are advisable to build trust within these communities and promote recruitment. Recruitment materials (e.g., flyers, brochures, and study description) are the first point of contact between researchers and participants. It is, therefore, essential that these materials consider strategies that most effectively engage this population. Inclusivity and diversity should be apparent on all recruitment materials [50]. Considering this population’s high prevalence of body image concerns, overt sexualization in advertisement images or verbiage focusing primarily on weight loss should be avoided [51]. It is important to include welcoming language (i.e., empowerment, survivor, solidarity, and strength) and avoid jargon or any stigmatizing verbiage (i.e., victim, blame, and shame), as well as emphasize confidentiality.
Orientation
Orientation sessions are often the first-time participants and research staff meets in person; they set the stage for the ongoing intervention. Exercise staff should make sure that they are easily identifiable and welcoming. Establishing a culture of trust and respect can be achieved from the start by acknowledging the prevalence of SV and associated PTS symptoms among women and explicitly verbalizing a commitment to providing trauma sensitive care. Providing participants with easy- to-understand information about research design and study rationale may improve participant trust in the research team [52, 53]. Using motivational interviewing techniques during the orientation session may help empower survivors to make positive behavioral changes and foster “buy-in” [52, 53]. Behavioral counseling and psychoeducation on the benefits of physical activity on psychological health is also an important part of orientation sessions in trauma-exposed populations [54]. Staff should assess the participant’s comfort working with the opposite gender staff, institute confidentiality and safety regulations, emphasize the participant’s bodily autonomy, and encourage realistic expectations [44, 55].
Exercise intervention
Establishing accessible and safe exercise locations associated with known community partners mentioned above (YWCA and RCC) would be advantageous for the comfort and safety of participants [44, 49]. Intervention teams must consistently reinforce a culture of trust, respect, and confidentiality [44]. Assessment of somatic symptoms prevalent in SV survivors is needed prior to initiating exercise and should inform the exercise prescription. Ongoing monitoring of these symptoms over the intervention period is also essential. The physical and social characteristics of the exercise environment is also a significant consideration in this population. Qualitative data from female trauma survivors suggest that participant comfort is maximized when the environment is primarily female [49, 56]. Additionally, principles from trauma-informed yoga practices emphasize limited or consensual touch [50]. Other examples of trauma-informed intervention strategies include explaining all procedures beforehand, giving exercise participants the ability to choose exercise routines (modality/intensity), using caution when placing mirrors in exercise locations, providing child care, and maintaining the confidentiality and safety of the participant [50, 54–57].
Exercise staff
Exercise staff trained in principles of TIC are essential to maintain a supportive exercise environment. Trauma sensitivity training for exercise staff is rare. Expansion of trauma-informed trainings for exercise physiologists and fitness professionals is needed. Trauma-informed yoga instructors avoid hands-on instruction and emphasize internal experience and bodily agency [55]. Knowledge of SV-specific health conditions discussed above (i.e., fibromyalgia, chronic pain, body image disorders, disordered eating, and emotion dysregulation) is essential for staff to develop safe and effective exercise prescriptions and to identify patient-centered goals. Exercise staff also need education and training on recognizing signs of abuse and screening for SV, as well as supporting women survivors in past or present abuse. Intervention teams should be prepared to refer survivors to appropriate legal and safety resources if necessary.
Outcome measurement
Trauma-informed assessments for women survivors of SV require that trials identify all relevant psychosomatic symptoms survivors experience and include them as outcomes. The small abovementioned available research in this area suggests that exercise may decrease PTSD symptoms, anxiety, and ruminative thoughts and increase sleep quality and self-compassion in women survivors of SV [27–30, 38, 42]. These outcomes exclude many trauma-specific health concerns for this population (i.e., body image, disordered eating, chronic pain, emotion dysregulation, physical functioning, and immune problems) [35, 58]. Although untested in this population, there is promising evidence that physical activity improves many of the unique health concerns women with SV experience. For instance, studies have shown that exercise improves body image [59], decreases chronic pain [60], and helps regulate disordered eating [61–63] among women. Future trials should also consider implementing the trauma-informed principle of resilience into outcomes by including measurements such as posttraumatic growth, resilience, quality of life, and hopefulness [45]. Increased studies in women survivors of SV may identify several mechanisms through which exercise may improve trauma-specific health concerns and uncover new opportunities for physical activity to operate as an effective adjunctive treatment.
CONCLUSION
Women survivors of SV experience trauma-related symptoms that negatively and cumulatively impact their health over a lifetime. Exercise is a low-cost and low-stigma health intervention that has been shown to be effective at improving trauma-related symptoms. TIC represents a growing area of health care that aims to address trauma-specific aspects of SV, and integration of these principles could greatly enhance health promotion efforts in this population. With the expansion of this line of research comes ample opportunity to move away from “one size fits all” exercise interventions toward trauma-informed health promotion strategies tailored to women survivors of SV. Researchers here call for (a) increased representation of women survivors of SV in exercise trials, (b) increased qualitative work on trauma-specific implementation efforts across exercise intervention domains, and (c) increased assessment of trauma-specific outcomes in exercise trials in this population.
Funding
This paper was supported by a grant from the Rehabilitation Research and Development Service (RX003120) to K.S.H.
Compliance with Ethical Standards
Conflicts of Interest: The authors have conflict of interests to report.
Authors’ Contributions Conceptualization, M.P.; Writing–original draft preparation, M.P.; Writing–review and editing, R.G. and K.H.; Resources, RG and KH; Supervision, R.G. and K.H.; Funding acquisition, K.H.
Ethical Approval This commentary is not an empirical paper and thus, did not require human subjects review.
References
- 1. Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran status. Am J Prev Med. 2018;54(1):e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. 2002. World report on violence and health, 6, 149. Available at https://www.who.int/violence_injury_prevention/violence/global_campaign/en/chap6.pdf. Accessibility verified October 18, 2019.
- 3. Center for Disease Control: National Center for Injury Prevention and Control. National intimate partner and sexual violence survey, 2010 summary report. Available at https://www.cdc.gov/violenceprevention/pdf/nisvs_report2010-a.pdf. Accessibility verified October 18, 2019.
- 4. Wilson LC. The prevalence of military sexual trauma: A meta-analysis. Trauma Violence Abuse. 2018;19(5):584–597. [DOI] [PubMed] [Google Scholar]
- 5. Jina R, Thomas LS. Health sonsequences of sexual violence against women. Best Pract Res Clin Obstet Gynaecol. 2013;27(1):15–26. doi: 10.1016/j.bpobgyn.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 6. Cortina LM, Kubiak SP. Gender and posttraumatic stress: Sexual violence as an explanation for women’s increased risk. J Abnorm Psychol. 2006;115(4):753–759. [DOI] [PubMed] [Google Scholar]
- 7. Fink DS, Gradus JL, Keyes KM, et al. Subthreshold PTSD and PTSD in a prospective-longitudinal cohort of military personnel: Potential targets for preventive interventions. Depress Anxiety. 2018;35(11):1048–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. [DOI] [PubMed] [Google Scholar]
- 9. Marshall RD, Olfson M, Hellman F, Blanco C, Guardino M, Struening EL. Comorbidity, impairment, and suicidality in subthreshold PTSD. Am J Psychiatry. 2001;158(9):1467–1473. [DOI] [PubMed] [Google Scholar]
- 10. Lutwak N, Dill C. Military sexual trauma increases risk of post-traumatic stress disorder and depression thereby amplifying the possibility of suicidal ideation and cardiovascular disease. Mil Med. 2013;178(4):359–361. doi: 10.7205/MILMED-D-12-0042. [DOI] [PubMed] [Google Scholar]
- 11. Lee YC, Agnew-Blais J, Malspeis S, et al. Post-traumatic stress disorder and risk for incident rheumatoid arthritis. Arthritis Care Res (Hoboken). 2016;68(3):292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Masodkar K, Johnson J, Peterson MJ. A review of posttrumatic stress disorder and obesity: exploring the link. Prim Care Companion CNS Disord. 2016;18(1). doi: 10.4088/PCC.15r01848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wong SP, Chang JC. Altered eating behaviors in female victims of intimate partner violence. J Interpers Violence. 2016;31(20):3490–3505. [DOI] [PubMed] [Google Scholar]
- 14. D’Aoust RF, Rossiter AG, Elliott A, Ji M, Lengacher C, Groer M. Women veterans, a population at risk for fibromyalgia: The associations between fibromyalgia, symptoms, and quality of life. Mil Med. 2017;182(7):e1828–e1835. [DOI] [PubMed] [Google Scholar]
- 15. Brewerton TD. Eating disorders, trauma, and comorbidity: Focus on PTSD. Eat Disord. 2007;15(4):285–304. [DOI] [PubMed] [Google Scholar]
- 16. Weaver TL, Griffin MG, Mitchell ER. Symptoms of posttraumatic stress, depression, and body image distress in female victims of physical and sexual assault: Exploring integrated responses. Health Care Women Int. 2014;35(4):458–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychol Bull. 2002;128(5):825–848. [DOI] [PubMed] [Google Scholar]
- 18. Santaularia J, Johnson M, Hart L, Haskett L, Welsh E, Faseru B. Relationships between sexual violence and chronic disease: A cross-sectional study. BMC Public Health. 2014;14:1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Driscoll M, Knobf M, Higgins D, Heapy A, Lee A, Haskell S. Patient experiences navigating chronic pain management in an integrated health care system: A qualitative investigation of women and men. Pain Med. 2018;19(1):S19–S29. doi: 10.1093/pm/pny139. [DOI] [PubMed] [Google Scholar]
- 20. Campaign to End Chronic Pain in Women. 2010. Chronic pain in women: Neglect, dismissal, and discrimination. Analysis and Policy Recommendations. Available at http://www.endwomenspain.org/. Accessibility verified October 18, 2019.
- 21. Darnall B, Li H. Hysterectomy and predictors for opioid prescription in a chronic pain clinic sample. Pain Med. 2011;12(2):196–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Najavits LM. The problem of dropout from “gold standard” PTSD therapies. F1000prime Rep. 2015;7:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gutner CA, Gallagher MW, Baker AS, Sloan DM, Resick PA. Time course of treatment dropout in cognitive–behavioral therapies for posttraumatic stress disorder. Psychol Trauma. 2016;8(1):115–121.doi: 10.1037/tra0000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Larsen SE, Bellmore A, Gobin RL, Holens P, Lawrence KA, Pacella-LaBarbara ML. An initial review of residual symptoms after empirically supported trauma-focused cognitive behavioral psychological treatment. J Anxiety Disord. 2019;63:26–35. [DOI] [PubMed] [Google Scholar]
- 25. Hall K, Morey M, Bosworth H, et al. Pilot randomized controlled trial of exercise training for older veterans with PTSD. J Behav Med. 2019. doi: 10.1007/s10865-019-00073-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cook JM, Simiola V, Hamblen JL, Bernardy N, Schnurr PP. The influence of patient readiness on implementation of evidence-based PTSD treatments in Veterans Affairs residential programs. Psychol Trauma. 2017;9(suppl 1):51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smith E, Rotunda RJ, Cosio-Lima L. Cognitive behavioral therapy and aerobic exercise for survivors of sexual violence with posttraumatic stress disorder: A feasibility study. J Trauma Stress Disord Treat. 2015;4(1). doi: 10.4172/2324-8947.1000136. [DOI] [Google Scholar]
- 28. Shors TJ, Chang HYM, Millon EM. MAP Training my brain: Meditation plus aerobic exercise lessens trauma of sexual violence more than either activity alone. Front Neurosci. 2018;12:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kolk BA, Stone L, West J, et al. Yoga as an adjunctive treatment for post-traumatic stress disorder: A randomized controlled trial. J Clin Psychiatry. 2014;75(6):e559–e565. doi: 10.4088/JCP.13m08561. [DOI] [PubMed] [Google Scholar]
- 30. Crews DA, Stolz-Newton M, Grant NS. The use of yoga to build self-compassion as a healing method for survivors of sexual violence. J Relig Spiritual Soc Work Soc Thought. 2016;35(3):139–156. doi: 10.1080/15426432.2015.1067583. [DOI] [Google Scholar]
- 31. Center for Disease Control. Physical activity guidelines for Americans. Executive summary. 2nd ed. 2018. Available at https://health.gov/sites/default/files/2019-10/PAG_ExecutiveSummary.pdf. Accessibility verified September 20, 2019. [Google Scholar]
- 32. King A, Powell KE, Kraus WE. The US physical activity guidelines advisory committee report—Introduction. Med Sci Sports Exerc. 2019;51(6):1203–1205. doi: 10.1249/MSS.0000000000001946. [DOI] [PubMed] [Google Scholar]
- 33. Vancampfort D, Rosenbaum S, Schuch F, et al. Cardiorespiratory fitness in severe mental illness: A systematic review and meta-analysis. Sports Med. 2017;47(2):343–352. [DOI] [PubMed] [Google Scholar]
- 34. Rosenbaum S, Vancampfort D, Steel Z, Newby J, Ward PB, Stubbs B. Physical activity in the treatment of post-traumatic stress disorder: A systematic review and meta-analysis. Psychiatry Res. 2015;230(2):130–136. [DOI] [PubMed] [Google Scholar]
- 35. Davidson CL, Babson KA, Bonn-Miller MO, Souter T, Vannoy S. The impact of exercise on suicide risk: Examining pathways through depression, PTSD, and sleep in an inpatient sample of veterans. Suicide Life Threat Behav. 2013;43(3):279–289. [DOI] [PubMed] [Google Scholar]
- 36. Hegberg NJ, Hayes JP, Hayes SM. Exercise intervention in PTSD: A narrative review and rationale for implementation. Front Psychiatry. 2019;10:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Whitworth JW, Craft LL, Dunsiger SI, Ciccolo JT. Direct and indirect effects of exercise on posttraumatic stress disorder symptoms: A longitudinal study. Gen Hosp Psychiatry. 2017;49:56–62. [DOI] [PubMed] [Google Scholar]
- 38. Whitworth JW, Nosrat S, SantaBarbara NJ, Ciccolo JT. High intensity resistance training improves sleep quality and anxiety in individuals who screen positive for posttraumatic stress disorder: A randomized controlled feasibility trial. Ment Health Phys Act. 2019;16:43–49. doi: 10.1016/j.mhpa.2019.04.001. [DOI] [Google Scholar]
- 39. Powers MB, Medina JL, Burns S, et al. Exercise augmentation of exposure therapy for PTSD: Rationale and pilot efficacy data. Cogn Behav Ther. 2015;44(4):314–327. doi: 10.1080/16506073.2015.1012740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: A randomized controlled trial. Acta Psychiatr Scand. 2015;131(5):350–359. [DOI] [PubMed] [Google Scholar]
- 41. Goldstein LA, Mehling WE, Metzler TJ, et al. Veterans group exercise: A randomized pilot trial of an Integrative Exercise program for veterans with posttraumatic stress. J Affect Disord. 2018;227:345–352. [DOI] [PubMed] [Google Scholar]
- 42. Mitchell KS, Dick AM, DiMartino DM, et al. A pilot study of a randomized controlled trial of yoga as an intervention for PTSD symptoms in women. J Trauma Stress. 2014;27(2):121–128. [DOI] [PubMed] [Google Scholar]
- 43. Pebole MM, Hall KS. Physical activity promotion in women with PTSD: What we need for progress. Psychol Sport Exerc. 2019;41:127–129. [PMC free article] [PubMed] [Google Scholar]
- 44. Substance Abuse and Mental Health Services Administration (SAMHSA). SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. HHS Publication No. (SMA) 14–4884. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- 45. Substance Abuse and Mental Health Services Administration. Trauma-Informed Care in Behavioral Health Services. Treatment Improvement Protocol (TIP) Series 57. HHS Publication No. (SMA) 13–4801. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [PubMed] [Google Scholar]
- 46. Ranjbar V, Speer SA. Revictimization and recovery from sexual assault: Implications for health professionals. Violence Vict. 2013;28(2):274–287. [DOI] [PubMed] [Google Scholar]
- 47. Elliott DE, Bjelajac P, Fallot RD, Markoff LS, Reed BG. Trauma-informed or trauma-denied: Principles and implementation of trauma-informed services for women. J Commun Psychol. 2005;33(4):461–477. doi: 10.1002/jcop.20063. [DOI] [Google Scholar]
- 48. Warshaw C, Sullivan CN, Rivera EA. 2013. A Systematic Review of Trauma-Focused Interventions for Domestic Violence Survivors. National Center on Domestic Violence, Trauma, and Mental Health. U.S. Department of Health and Human Services. Available at http://www.nationalcenterdvtraumamh.org/wp-content/uploads/2013/03/NCDVTMH_EBPLitReview2013.pdf. Accessibility verified October 29, 2019. [Google Scholar]
- 49. Smith-Marek EN, Baptist J, Lasley C, Cless JD. “I Don’t Like Being That Hyperaware of My Body”: Women survivors of sexual violence and their experience of exercise. Qual Health Res. 2018;28(11):1692–1707. [DOI] [PubMed] [Google Scholar]
- 50. Center for Disease Control and Prevention. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—National Intimate Partner and Sexual Violence Survey, United States, 2011. MMWR Surveill Summ. 2014;63(SS08):1–18. Available at https://www.cdc.gov/mmwr/pdf/ss/ss6308.pdf. Accessibility verified November 15, 2019. [PMC free article] [PubMed] [Google Scholar]
- 51. Castellini G, Ricca V. Sexual abuse and body image in eating and weight disorders. In: Cuzzolaro M, Fassino S, eds. Body Image, Eating, and Weight. Cham, Switzerland: Springer; 2018;273–280. doi: 10.1007/978-3-319-90817-5_20. [DOI] [Google Scholar]
- 52. Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ Res. 2005;20(4):439–447. [DOI] [PubMed] [Google Scholar]
- 53. Kiernan M, Oppezzo MA, Resnicow K, Alexander GL. Effects of a methodological infographic on research participants’ knowledge, transparency, and trust. Health Psychol. 2018;37(8):782–786. doi: 10.1037/hea0000631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pebole MM, Hall KS. Insights following implementation of an exercise intervention in older veterans with PTSD. Int J Environ Res Public Health. 2019;16:2630. doi: 10.3390/ijerph16142630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Center for Trauma and Embodiment at JRI. About us. 2019. Available at https://www.traumasensitiveyoga.com/about-us.html. Accessibility verified October 5, 2019.
- 56. Shivakumar G, Anderson EH, Surís AM, North CS. Exercise for PTSD in women veterans: A proof-of-concept study. Mil Med. 2017;182(11):e1809–e1814. [DOI] [PubMed] [Google Scholar]
- 57. Frayeh AL, Lewis BA. The effect of mirrors on women’s state body image responses to yoga. Psychol Sport Exerc. 2018;35:47–54. doi: 10.1016/j.psychsport.2017.11.002. [DOI] [Google Scholar]
- 58. Sack M, Boroske-Leiner K, Lahmann C. Association of nonsexual and sexual traumatizations with body image and psychosomatic symptoms in psychosomatic outpatients. Gen Hosp Psychiatry. 2010;32(3):315–320. [DOI] [PubMed] [Google Scholar]
- 59. Hausenblas HA, Fallon EA. Exercise and body image: A meta-analysis. Psychol Health. 2004;21(1):33–47. doi: 10.1080/14768320500105270. [DOI] [Google Scholar]
- 60. Busch AJ, Overend TJ, Schachter CL. Fibromyalgia treatment: the role of exercise and physical activity. Int J Clin Rheumatol. 2009;4(3):343–376. doi: 10.2217/IJR.09.23. [DOI] [Google Scholar]
- 61. Levine MP, Piran N. The role of body image in the prevention of eating disorders. Body Image. 2004;1(1):57–70. [DOI] [PubMed] [Google Scholar]
- 62. Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. J Psychosom Res. 2002;53(5):985–993. [DOI] [PubMed] [Google Scholar]
- 63. Cook BJ, Wonderlich SA, Mitchell JE, Thompson R, Sherman R, McCallum K. Exercise in eating disorders treatment: Systematic review and proposal of guidelines. Med Sci Sports Exerc. 2016;48(7):1408–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]