Abstract
Background:
Male sex workers (MSW) are disproportionately affected by HIV/AIDS, with an estimated HIV prevalence in the United States of 19.3%. Existing research suggests that MSW are also at risk of adverse psychosocial problems. Cross-sectional studies of MSW have suggested that co-occurring epidemics or a “syndemic” of psychosocial problems may increase vulnerability to HIV acquisition/transmission via elevated sexual risk. To our knowledge, there are no published studies examining this relationship longitudinally among MSW. This study examined how a syndemic of six psychosocial problems result in additive risk for condomless anal sex (CAS) with male clients among a multicity, longitudinal cohort of MSW.
Setting:
Community-based organization and health center in two Northeastern U.S. cities.
Methods:
Between 2015 and 2017, 100 MSW from Boston, MA and Providence, RI completed behavioral/psychosocial surveys at baseline, 6-, and 12-months. Generalized estimating equation modeling was used to examine the prospective relationship of additive psychosocial problems and subsequent CAS with male clients, adjusting for age, site, race/ethnicity, MSW-type, and HIV serostatus.
Results:
Mean age = 34.7 (SD = 11.8); 62% racial/ethnic minority; and 20% HIV+. The prevalence of six psychosocial syndemic problems was substantial at baseline and remained high at each time point (all within the past 6-months): 74% problematic depressive symptoms; 27% polydrug use (3+ drugs, not including stimulants); 57% stimulant (methamphetamine/cocaine/crack) use; 44% hazardous drinking; 15% experienced client-specific physical/sexual violence; and 57% childhood sexual abuse. Looking at the number of psychosocial problems experienced, 7% had zero, 27% had one, 24% had two, 27% had three, and 15% had four or more. We identified a statistically significant positive “dose-response” relationship between the number of psychosocial problems and CAS with male clients over time, with the greatest odds of engaging in CAS with a male client over follow-up among those with four or more psychosocial problems (aOR = 5.18, 95% CI: 1.61–16.62).
Conclusions:
Internet escorts and street-based MSW are likely to experience psychosocial problems and engaging in HIV sexual risk with male clients. The accumulation of psychosocial problems additively predicted CAS with male clients in a prospective cohort of MSW. The specification of psychosocial problems presents distinct treatment targets for HIV prevention among MSW in the United States.
Keywords: syndemic, male sex worker, HIV sexual risk behavior, mental health, substance use, physical abuse, sexual abuse, childhood sexual abuse
INTRODUCTION
Male sex workers (MSW) are disproportionately affected by HIV/AIDS. A recent meta-analysis estimated that the HIV prevalence among MSW globally and in the United States were 10.5% and 19.3%, respectively.1 Additionally, MSW-specific HIV prevalence estimates from 52 countries were reported to the United Nations General Assembly in 2012 and demonstrated the high burden of HIV among MSW, with four countries reporting HIV prevalence estimates of 25% or greater.2
MSW are currently understudied compared to other populations at high risk for HIV (e.g., men who have sex with men (MSM), people who inject drugs (PWID), female sex workers (FSW)),1,2 however, existing research suggests that they are also at risk of adverse psychosocial outcomes which may elevate their risk of acquiring HIV. A large proportion of MSW experience depression,3,4 anxiety,4 substance use,5,6 and intimate partner violence,7,8 all of which are known to elevate HIV sexual risk behavior.
The term “syndemic” was first developed to describe the co-occurring and mutually reinforcing epidemics of substance use, violence, and AIDS in poor urban communities and emphasizes how disadvantageous social conditions interact to adversely affect health outcomes within marginalized communities. The limited number of published studies specific to male sex workers that have examined syndemics in relation to sexual risk have relied on cross-sectional data.9–11 Despite this expanding evidence, research is needed to examine the syndemic production of HIV risk behavior longitudinally among this group.
To address this, in the present study, we drew from a large, multicity, prospective cohort of sexually active male sex workers in the United States to assess the interplay between multiple psychosocial problems and to determine the extent to which these psychosocial problems result in additive effects on sexual risk (i.e., condomless anal sex; CAS) over follow-up. Based on previous work (with other high-risk populations) supporting the centrality of syndemics in heightening HIV risk longitudinally, specifically among men who have sex with men (MSM),9,12–17 we hypothesized that psychosocial problems [i.e., clinically significant depressive symptoms; stimulant use; polydrug use (3 or more drugs used, excluding stimulants); hazardous drinking; history of childhood sexual abuse (CSA); intimate partner violence (IPV) from male clients (all the prior 6 months) would result in additive effects on sexual risk (i.e., a “dose response” relationship such that the additive effects of each psychosocial problem would increase the odds of engaging in CAS) over time among this cohort of male sex workers. The principal objective of this analysis is to improve and specify current HIV prevention intervention targets for this group.
METHODS
Participants and Procedures
This was a 12-month longitudinal cohort study which collected data between 2014 and 2016. Participants were 100 male sex workers recruited in greater Boston, MA and Providence, RI. Participants were recruited using multiple methods, including passive methods, such as flyering, paid online advertisements and referrals, as well as using active methods, including partnerships with community-based organizations who serve this population, phone calls, messages and emails to male sex workers found on IRB-approved websites.
Inclusion criteria included being 18 years of age or older, having a male sex assigned at birth, identifying as male, and having had anal sex (insertive or receptive) with 3 or more men in exchange for money in the month prior to enrollment. All procedures were approved by the Institutional Review Board at The Fenway Institute, Fenway Health in Boston, MA.
Study assessment visits occurred at baseline, 6- and 12-months. At each visit, participants were provided with the option to receive HIV counseling and testing, rectal and urethral chlamydia and gonorrhea screening, and syphilis testing. Moreover, participants completed a comprehensive quantitative assessment via audio computer-assisted self-interview (ACASI) for sensitive questions; non-sensitive questions were interviewer-administered.
Rapid HIV testing was conducted using the OraQuick® ADVANCE™ rapid HIV test. A blood sample was collected via finger-prick or blood draw (if the participant chooses to receive the optional syphilis testing). If the participant had a reactive test result, confirmatory testing was done immediately in coordination with the Bureau of Infectious Disease and Laboratory Sciences at the Massachusetts Department of Public Health. Pre-test and post-test counseling for HIV prevention followed standard of care, including information about HIV and STI transmission routes and prevention methods.
The quantitative assessment consisted of three sections: 1) completed by the participant alone, the assessment’s audio-computer assisted self-interview (ACASI) section included measures on potentially stigmatized and/or sensitive topics (e.g., sexual risk behavior, drug and alcohol use); 2) administered by the interviewer, the second section included less sensitive measures (e.g., demographics, healthcare access); and 3) completed with the interviewer, a network inventory assessed composition of participants’ social, sexual and drug use networks. Each study visit took approximately 1.5 hours to complete.
Measures
Sociodemographic characteristics.
Sociodemographic characteristics that may be independently associated with both syndemic psychosocial problems and condomless anal sex were examined. Age was assessed in years. Participants were coded according to study site: Boston, MA or Providence, RI. Participants were asked to indicate their primary race/ethnicity. Race/ethnicity was dichotomized as non-Hispanic/Latino white vs. person of color (black/ African American; Hispanic/Latino; Asian; American Indian/Alaskan Native; Native Hawaiian or other Pacific Islander; other another minority race/ethnicity). Participants were asked to report the highest level of education they had completed; responses were categorized as high school equivalent or less vs. some college or more. Participants were asked to report their total annual income and how many people their income supports (household income). Using Federal guidelines that account for annual income and number of dependents, participants were coded as living below the federal poverty line (yes, no). Participants were asked to indicate where they had met clients in the past 6 months (i.e., internet, sex club or bathhouse; bar, nightclub, or dance club; health club or gym; porn theater/video arcade; public bathroom; other public place, such as beach, park, woods, street, car, or van; some other place). For the sex worker type variable, participants who reported only meeting clients on the internet were coded as “internet only;” those who reported meeting clients on the internet and elsewhere where coded as “internet and street;” and those who reported only meeting clients on the street were coded as “street only.” Finally, HIV status was assessed at each time point via self-report and confirmed via rapid HIV testing (for those that agreed to testing). HIV status (i.e., negative vs. positive) is reported at baseline and for the full study period where positive status includes both prevalent cases at baseline and incident cases over follow up.
Syndemic psychosocial problems.
(1) Depression was assessed in the past seven days at each time point using 20-item Center of Epidemiologic Studies Depression Scale (CES-D). The items were summed and dichotomized based on a standard cutoff score of 16 or greater indicating problematic depressive symptoms in the past seven days.18,19 (2) Polydrug use in the past 6 months was defined as using ≥ 3 non-prescription drugs (marijuana, heroin, GHB, LSD/hallucinogens, pain medication, tranquilizers, amyl nitrite “poppers”) excluding stimulants.13,14 (3) Stimulant use was separated from the polydrug use variable due to its strong independent association with HIV risk behavior; this included any use of cocaine, crack, or crystal methamphetamine in the past 6 months.13,14 (4) Hazardous drinking in the past 6 months was assessed using the 10-item Alcohol Use Disorders Identification Test (AUDIT). Scale items were summed and dichotomized based on a standard cut off score of ≥8. A score of 8 or more is considered to indicate hazardous or harmful alcohol use. The AUDIT has been validated across genders and in a wide range of racial/ethnic groups and populations.20 (5) Childhood sexual abuse (CSA) was assessed at baseline using nine questions pertaining to experiences of unwanted or forced sexual touching or intercourse with a person when they were 17 years old or younger.21 CSA history was coded dichotomously such that participants responding yes to any of the eight questions were considered to have experienced one or more form of childhood sexual abuse. (6) Client violence in the past 6 months was assessed at each time point via a 23 -item scale assessing whether participants experienced any form of violence (e.g., sexual, physical, and emotional control) by a client (yes, no).22
The syndemic measure was calculated as a count score based on the number of psychosocial problems endorsed, resulting in scores ranging from 0–4 (note: category 4 includes those who reported experiencing 4 (n = 10) or 5 (n = 2) psychosocial problems).9,12–17
Condomless anal sex (CAS) with male client.
CAS was assessed as a count variable at each time point. Specifically, participants were asked, “in the past month, how many times have you had anal (receptive or insertive) sex without a condom with a male client.”23–25
Data Analysis
Statistical analyses were conducted in SAS 9.4. Means and frequencies were calculated to describe participant characteristics at baseline and syndemic psychosocial problems over time. We then conducted a series of generalized estimating equation (GEE) models with an unstructured covariance matrix and a negative binomial distribution based on the CAS count outcome.26 First, we conducted a test for trend to determine if the number of psychosocial problems increased (count) with the number of CAS acts with a male client over time. We then tested whether the number of psychosocial problems (referent = 0 psychosocial problems) increased the odds of CAS with a male client over time without adjusting for any covariates. Our final model tested whether the number of psychosocial problems increased the odds of CAS with a male client over time; we decided to adjust all models a priori for age, recruitment city, race/ethnicity, sex worker type, and HIV status, as these are the covariates typically adjusted for in the academic literature. Since the lifetime CSA measure was only assessed at baseline, the value for this measure was carried across all timepoints.
For this analysis, the sample was restricted to participants who had at least one follow up visit (n = 81). Note: Participants who had missing data at 6- and 12-months -- compared to those without missing data -- were not significantly different with respect to key socio-demographics. In addition, those with missing data at 6- and 12-months were also not significantly more likely to have a higher number of baseline psychosocial problems compared to those without missing data.
RESULTS
Sociodemographics (Table 1).
Table 1.
Characteristics of sample (N = 81).
| Street Only n=42 | Internet Only n=25 | Internet & Street n=14 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Range: 19–61 (full sample) | 34.7 | 11.8 | 36.5 | 11.9 | 32.0 | 10.4 | 34.5 | 13.37 | 0.33 |
| n | % | n | % | n | % | n | % | ||
| Study Site | |||||||||
| Boston | 39 | 48.8 | 12 | 28.6 | 23 | 92.0 | 4 | 28.6 | <0.001 |
| Providence | 42 | 51.3 | 30 | 71.4 | 2 | 8.0 | 10 | 71.4 | |
| Race/Ethnicity | |||||||||
| Non-Hispanic/Latino White | 31 | 38.3 | 13 | 31.0 | 13 | 52.0 | 5 | 35.7 | 0.22 |
| Person of Color | 50 | 61.7 | 29 | 69.0 | 12 | 48.0 | 9 | 64.3 | |
| Education | |||||||||
| High school/equivalent or less | 50 | 61.7 | 32 | 76.2 | 8 | 32.0 | 10 | 71.4 | 0.001 |
| Some college or more | 31 | 38.3 | 10 | 23.8 | 17 | 68.0 | 4 | 28.6 | |
| Income Below Federal Poverty Line (n=78) | |||||||||
| No | 39 | 50.0 | 13 | 31.7 | 20 | 80.0 | 6 | 50.0 | 0.01 |
| Yes | 39 | 50.0 | 28 | 68.3 | 5 | 20.0 | 6 | 50.0 | |
| Sex Worker Type | |||||||||
| Street-Based Only | 42 | 51.9 | 42 | 100.0 | 0 | 0.0 | 0 | 0.0 | n/a |
| Internet Only | 25 | 30.9 | 0 | 0.0 | 25 | 100.0 | 0 | 0.0 | |
| Internet & Street | 14 | 17.3 | 0 | 0.0 | 0 | 0.0 | 14 | 100.0 | |
| HIV Statusa | |||||||||
| Negative or unknown | 65 | 80.2 | 34 | 81.0 | 21 | 84.0 | 10 | 71.4 | 0.65 |
| Positive | 16 | 19.8 | 8 | 19.0 | 4 | 16.0 | 4 | 28.6 | |
| Prevalent (at baseline) | 14 | 17.3 | 8 | 19.0 | 4 | 16.0 | 2 | 14.3 | |
| Incident (over follow-up) | 2 | 2.5 | 0 | 0.0 | 0 | 0.0 | 2 | 14.3 | |
| Syndemic: psychosocial problemsb | |||||||||
| 0 | 6 | 7.4 | 3 | 7.1 | 1 | 4.0 | 2 | 14.3 | 0.79 |
| 1 | 22 | 27.2 | 10 | 23.8 | 8 | 32.0 | 4 | 28.6 | |
| 2 | 19 | 23.5 | 12 | 28.6 | 5 | 20.0 | 2 | 14.3 | |
| 3 | 22 | 27.2 | 12 | 28.6 | 8 | 32.0 | 2 | 14.3 | |
| Reported 4 or 5 | 12 | 14.8 | 5 | 11.9 | 3 | 12.0 | 4 | 28.6 | |
| 4 | 10 | 12.3 | 3 | 7.1 | 3 | 12.0 | 3 | 21.4 | |
| 5 | 2 | 2.5 | 2 | 4.8 | 0 | 0.0 | 0 | 0.0 | |
| Depression - Past 7 Days | |||||||||
| No | 21 | 25.9 | 8 | 19.0 | 8 | 32.0 | 5 | 35.7 | 0.33 |
| Yes | 60 | 74.1 | 34 | 81.0 | 17 | 68.0 | 9 | 64.3 | |
| Polydrug Use - Past 6 Months | |||||||||
| No | 59 | 72.8 | 33 | 78.6 | 16 | 64.0 | 10 | 71.4 | 0.42 |
| Yes | 22 | 27.2 | 9 | 21.4 | 9 | 36.0 | 4 | 28.6 | |
| Stimulant Use - Past 6 Months | |||||||||
| No | 35 | 43.2 | 15 | 35.7 | 14 | 56.0 | 6 | 42.9 | 0.27 |
| Yes | 46 | 56.8 | 27 | 64.3 | 11 | 44.0 | 8 | 57.1 | |
| Hazardous Drinking - Past 6 Months | |||||||||
| No | 45 | 55.6 | 25 | 59.5 | 12 | 48.0 | 8 | 57.1 | 0.65 |
| Yes | 36 | 44.4 | 17 | 40.5 | 13 | 52.0 | 6 | 42.9 | |
| Child Sexual Abuse - Lifetime | |||||||||
| No | 35 | 43.2 | 15 | 35.7 | 15 | 60.0 | 5 | 35.7 | 0.12 |
| Yes | 46 | 56.8 | 27 | 64.3 | 10 | 40.0 | 9 | 64.3 | |
| Client Violence - Past 6 Months | |||||||||
| No | 69 | 85.2 | 37 | 88.1 | 21 | 84.0 | 11 | 78.6 | 0.65 |
| Yes | 12 | 14.8 | 5 | 11.9 | 4 | 16.0 | 3 | 21.4 | |
| CAS with Male Client – Past 30 Days | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Range: 0–30 (full sample) | 2.3 | 4.9 | 1.4 | 1.8 | 1.1 | 2.3 | 7.5 | 10.1 | <0.0001 |
Note. CAS = Condomless Anal Sex. All variables are reported at baseline, except for incident HIV.
Prevalent = HIV infection at baseline; Incident = acquired HIV over follow-up.
4+ includes individuals with 4, 5, or 6 syndemic conditions. The variable was coded as 4 or more due to the low prevalence of individuals with 5 or 6 syndemics conditions at follow-up.
P-Value: Chi-Square or Fisher Exact for categorical variables; ANOVA for age and CAS acts.
Participants’ mean age was 34.7 years (SD: 11.8; range 19–61). Slightly more than half (51.3%) of participants were from Providence. The majority of the participants who engaged in any street-based sex work came from Providence (n = 40/56; 71.4%) and fewer came from Boston (n = 16/56; 28.6), compared to those who only did internet-based sex work who largely came from Boston (n = 23/25; 92%) and fewer from Providence (n = 2/25; 8%). The majority (61.7%) of participants were racial/ethnic minorities (37.0% black/African American; 16.0% Hispanic/Latino; 3.7% American Indian or Alaskan Native; 4.9% mixed race/other); 17.3% were HIV infected at baseline and 2 participants became infected with HIV over the 12-month follow-up period. The majority of participants (61.7%) reported up to a high school education, with internet escorts reporting greater educational attainment. Nearly half of participants (48.1%) had an income below the federal poverty line, with street-based sex workers reporting this most often.
Sexual behavior.
Participants reported engaging in an average of 2.3 (SD = 4.9) CAS acts with a male client in the past 30 days. Participants who engaged in both internet-based and street-based sex work had the highest number of CAS acts on average (mean = 7.5; SD = 10.1), followed by street-based alone (mean = 1.4; SD = 1.8), and internet-based alone (mean = 1.1; SD = 2.3), Substance use, mental health problems, and physical and sexual violence. Psychosocial problems prevalent at baseline were high: 74.1% reported clinically significant symptoms indicative of depression; 27.2% polydrug use in the past 6 months; 56.8% stimulant use in the past 6 months; 44.4% hazardous drinking in the past 6 months; 56.8% history of CSA; and 14.8% reported experiencing client violence in the past 6 months. Looking at the number of syndemic conditions experienced among the sample, 7.4% had zero psychosocial problems, 27.2% had 1, 23.5% had 2, 27.2% had 3, and 14.8% had 4 or more (4 = 12.3%; 5 = 2.5%).
Substance use, mental health problems, and physical and sexual violence.
Psychosocial problems prevalent at baseline were high: 74.1% reported clinically significant symptoms indicative of depression; 27.2% polydrug use in the past 6 months; 56.8% stimulant use in the past 6 months; 44.4% hazardous drinking in the past 6 months; 56.8% history of childhood sexual abuse; and 14.8% reported experiencing client violence in the past 6 months. Looking at the number of syndemic conditions experienced among the sample, 7.4% had zero psychosocial problems, 27.2% had one, 23.5% had two, 27.2% had three, and 14.8% had four or more (4 = 12.3%; 5 = 2.5%).
Changes in substance use, mental health problems, and physical and sexual violence over study follow-up.
There was a statistically significant change in the prevalence of the count of the syndemic measure at follow up (Table 2), with the largest reduction observed in the 4 or more group from baseline (14.8%) to 12 months (3.0%). When looking at individual syndemic conditions, there were significant reductions in polydrug use from baseline (27.2%) to 12 months (13.6%). There was also a significant reduction in client violence from baseline (14.8%) to 12 months (4.5%). These did not significantly differ by sex worker type. Correlations between all variables are shown in Table 3.
Table 2.
Descriptive analyses of syndemics conditions over time.
| Baseline | 6 Month | 12 Month | P-Value | ||||
|---|---|---|---|---|---|---|---|
| N=81 | N=69 | N=66 | |||||
| N | % | N | % | N | % | ||
| Syndemics | 0.02 | ||||||
| 0 | 6 | 7.4 | 8 | 11.6 | 9 | 13.6 | |
| 1 | 22 | 27.2 | 20 | 29.0 | 17 | 25.8 | |
| 2 | 19 | 23.5 | 22 | 31.9 | 19 | 28.8 | |
| 3 | 22 | 27.2 | 13 | 18.8 | 19 | 28.8 | |
| 4+ | 12 | 14.8 | 6 | 8.7 | 2 | 3.0 | |
| Depression - Past 7 Days | 0.67 | ||||||
| No | 21 | 25.9 | 21 | 30.4 | 15 | 22.7 | |
| Yes | 60 | 74.1 | 48 | 69.6 | 51 | 77.3 | |
| Polydrug Use - Past 6 Months | 0.04 | ||||||
| No | 59 | 72.8 | 54 | 78.3 | 57 | 86.4 | |
| Yes | 22 | 27.2 | 15 | 21.7 | 9 | 13.6 | |
| Stimulant Use - Past 6 Months | 0.04 | ||||||
| No | 35 | 43.2 | 33 | 47.8 | 34 | 51.5 | |
| Yes | 46 | 56.8 | 36 | 52.2 | 32 | 48.5 | |
| Hazardous Drinking - Past 6 Months | 0.38 | ||||||
| No | 45 | 55.6 | 46 | 66.7 | 41 | 62.1 | |
| Yes | 36 | 44.4 | 23 | 33.3 | 25 | 37.9 | |
| Child Sexual Abuse - Lifetime | 0.38 | ||||||
| No | 35 | 43.2 | 29 | 42.0 | 30 | 45.5 | |
| Yes | 46 | 56.8 | 40 | 58.0 | 36 | 54.5 | |
| Client Violence - Past 6 Months | 0.02 | ||||||
| No | 69 | 85.2 | 64 | 92.8 | 63 | 95.5 | |
| Yes | 12 | 14.8 | 5 | 7.2 | 3 | 4.5 | |
Note. P-Value represents the value for the regression analyses examining whether there was a significant change in the variable over time.
Table 3.
Correlations between syndemic variables (N = 81; all time points)
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Depression - Past 7 Days | --- | 0.11+ | 0.11+ | 0.15* | −0.04+ | 0.08+ |
| 2. Polydrug Use - Past 6 Months | --- | 0.29*** | 0.05+ | 0.11+ | 0.03+ | |
| 3. Stimulant Use - Past 6 Months | --- | 0.13+ | 0.18** | 0.01+ | ||
| 4. Hazardous Drinking - Past 6 Months | --- | −0.12+ | 0.17** | |||
| 5. Child Sexual Abuse - Lifetime | --- | −0.01+ | ||||
| 6. Client Violence - Past 6 Months | --- |
p<0.10;
p<0.05;
p<0.01;
p<0.001
Additive effect of substance use, mental health problems, and physical and sexual violence.
The odds of CAS were highest for those with more psychosocial problems over study follow up, with a trend toward a lower odds of engaging in CAS with a male client among those who reported fewer psychosocial problems (Table 4). Specifically, in both unadjusted and adjusted models, compared to those with no psychosocial problems (referent), those with four or more psychosocial problems had more than five times the odds of engaging in CAS with a male client over follow up (aOR = 5.18, 95% CI: 1.61–16.62); those with three psychosocial problems had more than three times the odds of engaging in CAS with a male client over follow up (aOR = 3.35, 95% CI: 1.07–10.48); and those with two psychosocial problems had three times the odds of engaging in CAS with a male client over follow up (aOR = 3.00, 95% CI: 1.01–8.91). The association between one psychosocial problem and CAS with a male client was in the expected direction, but did not reach statistical significance (aOR = 2.79, 95% CI: 0.86–9.03). All models adjusted for age, site, race/ethnicity, sex worker type, and HIV status. These did not significantly differ by sex worker type. A plot of adjusted odds ratios by total number of reported psychosocial problems can be found in Figure 1.
Table 4.
Bivariate and multivariable models examining the longitudinal association of syndemics and condomless anal sex with male clients (N = 81).
| CAS with Male Client | ||||||||
|---|---|---|---|---|---|---|---|---|
| Bivariate | Multivariable | |||||||
| OR | 95% CI | P-Value | aOR | 95% CI | P-Value | |||
| Syndemics | ||||||||
| 0 | 1.00 | --- | --- | --- | 1.00 | --- | --- | --- |
| 1 | 3.07 | 0.95 | 0.99 | 0.06 | 2.79 | 0.86 | 9.03 | 0.09 |
| 2 | 1.69 | 0.52 | 5.55 | 0.39 | 3.00 | 1.01 | 8.91 | 0.048 |
| 3 | 3.79 | 1.02 | 14.10 | 0.046 | 3.35 | 1.07 | 10.48 | 0.04 |
| 4 | 9.20 | 2.17 | 38.94 | 0.01 | 5.18 | 1.61 | 16.62 | 0.01 |
| COVARIATES | ||||||||
| Age | 1.04 | 1.01 | 1.07 | 0.02 | ||||
| Study Site | ||||||||
| Providence | 1.00 | --- | --- | --- | ||||
| Boston | 1.10 | 0.56 | 2.16 | 0.77 | ||||
| Race/Ethnicity | ||||||||
| Non-Hispanic/Latino White | 1.00 | --- | --- | --- | ||||
| Person of Color | 1.69 | 0.75 | 3.82 | 0.21 | ||||
| Sex Worker Type | ||||||||
| Street-Based Only | 1.00 | --- | --- | --- | ||||
| Internet Only | 0.91 | 0.29 | 2.88 | 0.87 | ||||
| Street and Internet | 3.64 | 1.80 | 7.38 | <0.001 | ||||
| HIV Positive | ||||||||
| No | 1.00 | --- | --- | --- | ||||
| Yes | 0.77 | 0.37 | 1.60 | 0.48 | ||||
Note. OR = odds ratio; aOR = adjusted odds ratio. HIV Positive = baseline status. The multivariable model adjusted for all covariates shown. Italicized p-values approached significance. Test for trend was also significant (aOR = 1.30; 95% CI = 1.09–1.55; p = 0.003)
Figure 1.
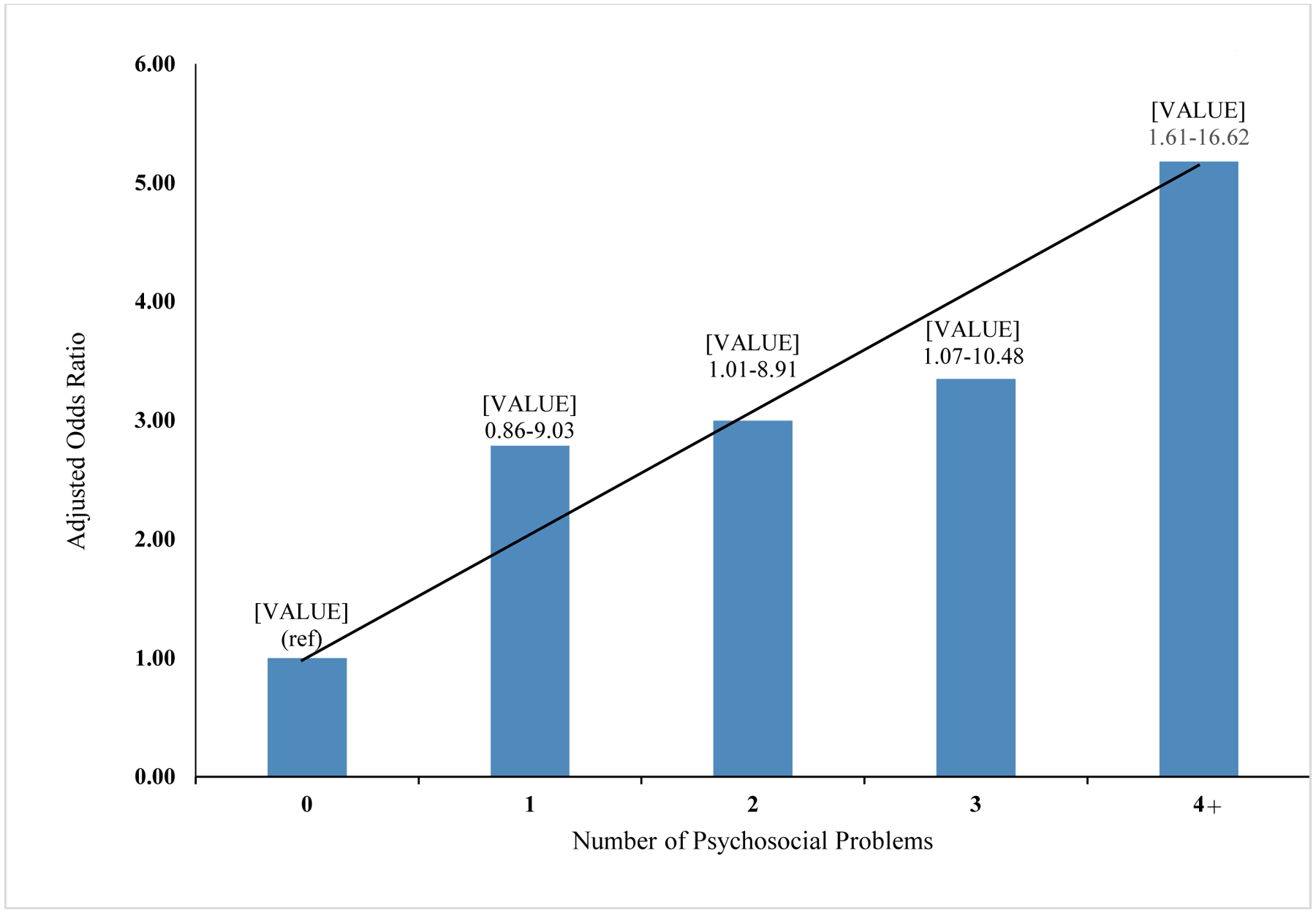
Plot of adjusted odds ratios by total number of reported psychosocial problems (N = 81).
DISCUSSION
This work demonstrates that MSW experience multiple, co-occurring psychosocial health conditions, and that greater burden of syndemic problems is prospectively associated with increased sexual risk behavior. Not only did we identify highly prevalent syndemic conditions (60% reported two or more, 32% reported three or more at 12-month follow-up), but the accumulation of overlapping psychosocial problems had an additive effect on CAS with their male clients. The odds of engaging in CAS with a client increased three-fold when men reported two or more psychosocial problems and fivefold when men reported four or more psychosocial problems, compared to men reporting none. This study builds on the existing literature elucidating the compounding effect of syndemic psychosocial problems on sexual risk and HIV seroconversion among men who have sex with men.14,27,28 While other research has examined multiple psychosocial conditions and their relation to sexual risk among MSW in cross-sectional studies,9 the present study uniquely assesses these relationships using longitudinal data.
Syndemic psychosocial problems have been linked to increased risk of HIV acquisition among MSM in the United States,17,27,29 and decreased adherence to HIV treatment once infected.30–32 For male sex workers, relations between poor mental health and sexual risk taking may be exacerbated by lower socioeconomic position/economic marginalization, unstable housing,33 lack of power in sexual relationships,2,34 and fewer resources to prioritize sexual risk reduction.11,35 Nearly half of participants (48.1%) in this sample had an income below the federal poverty line; these economic pressures often result in compromising safer sex practices for monetary incentives. Other contributory factors to HIV sexual risk may be tied to identity, regarding both sexual orientation and race. Almost two thirds of the sample identified as a racial/ethnic minority, and as such may experience heightened levels of minority stress (sexual identity and race/ethnicity related), which is associated with elevated sexual risk behavior.28,36
Interestingly, there was a statistically significant change in the prevalence of the count of the syndemic measure at follow up. Further, when examining each psychosocial problem separately, there were significant reductions in polydrug use from baseline 12 months, and in client violence from baseline to 12 months. This change may be due in part to the research team providing each participant with a list of referrals to local mental health and addictions treatment organizations, and other medical and social services available to them.
These results have implications for designing interventions to decrease sexual risk for HIV among this group. Consistent with syndemic theory, almost half of the sample reported dealing with negative early life events in addition to current stressors. Thus, HIV prevention efforts targeted for this population may need to include counseling to overcome depression and potential PTSD from negative early life experiences, as well as addictions treatment. For instance, interventions that integrate sexual risk reduction counseling with cognitive behavioral therapy or behavioral activation have shown greater success than counseling alone (e.g., supportive psychotherapy) and might be appropriate for this population.13,37 In addition, case management to assist with structural-level barriers that would impede safer sex practices could increase intervention effectiveness. Furthermore, partnering with community-based organizations that provide services to, and are trusted by, the MSW population may increase intervention efficacy.
While this study enhances our understanding of how syndemic psychosocial conditions affect a prospective cohort of MSW, this work is not without limitations. First, our syndemic indicators were based on self-report; thus, the extent of the impairment or distress associated with these measures is unknown. Recruitment for the cohort study occurred in urban centers in the Northeastern U.S., possibly preventing the generalizability of our findings to MSW in nonurban settings. Further, assessment of the higher-level structural variables highlighted in syndemic theory was also limited. And finally, the relatively low number of participants (n = 12) in the highest number of syndemics groups (for 4, 5, and 6 psychosocial problems reported) reduced our ability to examine these as distinct groups.
Internet escorts and street-based MSW are a vulnerable group for experiencing psychosocial problems and engaging in HIV sexual risk with male clients. Given the high prevalence of substance use, poor mental health, and traumatic life experiences/ victimization, MSW are a unique group requiring tailored HIV prevention approaches that concurrently address these co-occurring psychosocial problems.
Conflicts of Interest and Source of Funding:
All authors declare that they have no conflict of interest. Research reported in this article was supported by award R21DA035113-01A1 (MPIs: Drs. Mimiaga and Biello) from the National Institute on Drug Abuse of the National Institutes of Health.
Footnotes
Informed Consent and Protection of Human Subjects
All procedures performed involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all participants included in the study.
REFERENCES
- 1.Oldenburg CE, Perez-Brumer AG, Reisner SL, et al. Global burden of HIV among men who engage in transactional sex: a systematic review and meta-analysis. PLoS One. 2014;9(7):e103549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baral SD, Friedman MR, Geibel S, et al. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. Lancet. 2015;385(9964):260–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bar-Johnson M, Weiss P. Mental health and sexual identity in a sample of male sex workers in the Czech Republic. Med Sci Monit. 2014;20:1682–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldsamt LA, Clatts MC, Giang LM, Yu G. Prevalence and Behavioral Correlates of Depression and Anxiety Among Male Sex Workers in Vietnam. Int J Sex Health. 2015;27(2):145–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu G, Goldsamt LA, Clatts MC, Giang LM. Sexual Initiation and Complex Recent Polydrug Use Patterns Among Male Sex Workers in Vietnam: A Preliminary Epidemiological Trajectory. Arch Sex Behav. 2016;45(4):975–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu G, Clatts MC, Goldsamt LA, Giang le M. Substance use among male sex workers in Vietnam: prevalence, onset, and interactions with sexual risk. Int J Drug Policy. 2015;26(5):516–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunkle KL, Wong FY, Nehl EJ, et al. Male-on-male intimate partner violence and sexual risk behaviors among money boys and other men who have sex with men in Shanghai, China. Sex Transm Dis. 2013;40(5):362–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.George PE, Bayer AM, Garcia PJ, et al. Is Intimate Partner and Client Violence Associated with Condomless Anal Intercourse and HIV Among Male Sex Workers in Lima, Peru? AIDS Behav. 2016;20(9):2078–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biello KB, Colby D, Closson E, Mimiaga MJ. The syndemic condition of psychosocial problems and HIV risk among male sex workers in Ho Chi Minh City, Vietnam. AIDS Behav. 2014;18(7):1264–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvarado B, Mueses HF, Galindo J, Martinez-Cajas JL. Application of the “syndemics” theory to explain unprotected sex and transactional sex: A crosssectional study in men who have sex with men (MSM), transgender women, and non-MSM in Colombia. Biomedica. 2020;40(2):391–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedman MR, Kurtz SP, Buttram ME, Wei C, Silvestre AJ, Stall R. HIV risk among substance-using men who have sex with men and women (MSMW): findings from South Florida. AIDS Behav. 2014;18(1):111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogunbajo A, Oke T, Jin H, et al. A syndemic of psychosocial health problems is associated with increased HIV sexual risk among Nigerian gay, bisexual, and other men who have sex with men (GBMSM). AIDS Care. 2020;32(3):337–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mimiaga MJ, Hughto JMW, Biello KB, et al. Longitudinal Analysis of Syndemic Psychosocial Problems Predicting HIV Risk Behavior Among a Multicity Prospective Cohort of Sexually Active Young Transgender Women in the United States. J Acquir Immune Defic Syndr. 2019;81(2):184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mimiaga MJ, O’Cleirigh C, Biello KB, et al. The effect of psychosocial syndemic production on 4-year HIV incidence and risk behavior in a large cohort of sexually active men who have sex with men. J Acquir Immune Defic Syndr. 2015;68(3):329–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Safren SA, Blashill AJ, Lee JS, et al. Condom-use self-efficacy as a mediator between syndemics and condomless sex in men who have sex with men (MSM). Health Psychol. 2018;37(9):820–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Biello KB, Oldenburg CE, Safren SA, et al. Multiple syndemic psychosocial factors are associated with reduced engagement in HIV care among a multinational, online sample of HIV-infected MSM in Latin America. AIDS Care. 2016;28 Suppl 1:84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mimiaga MJ, Biello KB, Robertson AM, et al. High prevalence of multiple syndemic conditions associated with sexual risk behavior and HIV infection among a large sample of Spanish- and Portuguese-speaking men who have sex with men in Latin America. Arch Sex Behav. 2015;44(7):1869–1878. [DOI] [PubMed] [Google Scholar]
- 18.Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurements. 1977;1:385–401. [Google Scholar]
- 19.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12(2):277–287. [DOI] [PubMed] [Google Scholar]
- 20.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. [DOI] [PubMed] [Google Scholar]
- 21.Mimiaga MJ, Noonan E, Donnell D, et al. Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE Study. J Acquir Immune Defic Syndr. 2009;51(3):340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stephenson R, Finneran C. The IPV-GBM scale: a new scale to measure intimate partner violence among gay and bisexual men. PLoS One. 2013;8(6):e62592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mimiaga MJ, Reisner SL, Closson EF, et al. Self-perceived HIV risk and the use of risk reduction strategies among men who engage in transactional sex with other men in Ho Chi Minh City, Vietnam. AIDS Care. 2013;25(8):1039–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mimiaga MJ, Thomas B, Biello K, et al. A Pilot Randomized Controlled Trial of an Integrated In-person and Mobile Phone Delivered Counseling and Text Messaging Intervention to Reduce HIV Transmission Risk among Male Sex Workers in Chennai, India. AIDS Behav. 2017;21(11):3172–3181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landers S, Closson EF, Oldenburg CE, Holcomb R, Spurlock S, Mimiaga MJ. HIV prevention needs among street-based male sex workers in Providence, Rhode Island. Am J Public Health. 2014;104(11):e100–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Ming, “Generalized Estimating Equations in Longitudinal Data Analysis: A Review and Recent Developments”, Advances in Statistics, vol. 2014, Article ID 303728, 11 pages, 2014. [Google Scholar]
- 27.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dyer TP, Shoptaw S, Guadamuz TE, et al. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health. 2012;89(4):697–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blashill AJ, Bedoya CA, Mayer KH, et al. Psychosocial Syndemics are Additively Associated with Worse ART Adherence in HIV-Infected Individuals. AIDS Behav. 2015;19(6):981–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedman MR, Stall R, Silvestre AJ, et al. Effects of syndemics on HIV viral load and medication adherence in the multicentre AIDS cohort study. Aids. 2015;29(9):1087–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pantalone DW, Valentine SE, Woodward EN, O’Cleirigh C. Syndemic Indicators Predict Poor Medication Adherence and Increased Health Care Utilization for Urban HIV-Positive Men Who Have Sex with Men. J Gay Lesbian Ment Health. 2018;22(1):71–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Javanbakht M, Ragsdale A, Shoptaw S, Gorbach PM. Transactional Sex among Men Who Have Sex with Men: Differences by Substance Use and HIV Status. J Urban Health. 2019;96(3):429–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Katsulis Y, Durfee A. Prevalence and correlates of sexual risk among male and female sex workers in Tijuana, Mexico. Glob Public Health. 2012;7(4):367–383. [DOI] [PubMed] [Google Scholar]
- 35.Underhill K, Guthrie KM, Colleran C, Calabrese SK, Operario D, Mayer KH. Temporal Fluctuations in Behavior, Perceived HIV Risk, and Willingness to Use Pre-Exposure Prophylaxis (PrEP). Arch Sex Behav. 2018;47(7):2109–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hatzenbuehler ML, O’Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Ann Behav Med. 2011;42(2):227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tobin K, Davey-Rothwell MA, Nonyane BAS, Knowlton A, Wissow L, Latkin CA. RCT of an integrated CBT-HIV intervention on depressive symptoms and HIV risk. PLoS One. 2017;12(12):e0187180. [DOI] [PMC free article] [PubMed] [Google Scholar]


