Abstract
Introduction:
Alpha-gal Syndrome (AGS) is a unique allergy to non-primate mammalian meat (and derived-products) that is associated with tick bites and is due to a specific IgE antibody to the oligosaccharide galactose-α-1,3-galactose (alpha-gal). AGS has many novel features that broaden the paradigm of food allergy, including that reactions are delayed 3-6 hours after exposure and patients have frequently tolerated red meat for many years prior to the development of allergic reactions. Due to the ubiquitous inclusion of mammal-derived materials in foods, medications, personal products and stabilizing compounds, full avoidance is difficult to achieve.
Areas covered:
This review describes the author’s experience with diagnosis, management and design of appropriate avoidance for patients with AGS and provides clinicians with practical advice for care of these patients.
Expert opinion:
The number of patients with AGS is rising and may have exceeded awareness of the diagnosis amongst healthcare providers. In summarizing experience gained to thus far, we hope to create a resource for identifying and managing this unique allergic syndrome.
Keywords: Alpha gal allergy, food allergy, anaphylaxis, red meat, IgE, tick, galactose
1. Introduction
In 2009 Alpha-gal Syndrome (AGS) was described in 24 patients who reported delayed allergic reactions to mammalian meat [1]. This clinical observation was supported by prior identification of immunoglobulin E (IgE) specific for the oligosaccharide galactose-α-1,3-galactose (alpha-gal) that was associated with hypersensitivity reactions (HSRs) to cetuximab [2]. In >90% of cases the diagnosis of AGS can be made based on a history of delayed allergic reactions after eating non-primate mammalian meat * (e.g., “red meat” such as beef, pork, or lamb) and a positive blood test (>0.1 IU/mL) for IgE to alpha-gal [3]. The combination of both an appropriate clinical history and supporting blood test is necessary to establish an accurate AGS diagnosis [1]. Unlike more traditional food allergies where consumption of an allergen produces symptoms within minutes, AGS reactions typically occur 3-8 hours after eating [4]. Thus, many patients fail to consider food as a possible trigger and many healthcare providers do not routinely recognize the characteristic delay – both issues can prolong time to reach a diagnosis [5].
Following identification of AGS, patients with the same allergy in Australia, Europe, Scandinavia, Japan, and South Africa have been reported [6]. Owing to the geographical range and analysis of tick salivary factors, the lone star tick (Amblyomma americanum) appears to be the primary cause of AGS in the U.S.; however, no case-control study has confirmed this link. An association between AGS and tick bites has been reported throughout the world, despite the differences in tick species and populations [6-8]. Blood levels of alpha-gal IgE often decrease in patients who avoid recurrent tick bites but the rate of decline varies from patient to patient [7]. The titer of alpha-gal specific IgE does not predict reaction severity; rather dose (amount consumed) and presence of co-factors (alcohol, activity) affect the delay before reaction and resulting clinical manifestations [4]. In keeping with other food allergies, clinical experience suggests that the presence of co-factors appears to lower the eliciting dose required for reactivity but this requires further study in AGS [9]. Specific to AGS, recent tick bites appear to make patients more sensitive to prior tolerated exposures or even lower threshold for reactivity. Table 1 is a summary of clinical points accumulated over the last decade caring for patients with AGS.
Table 1 –
Clinical pearls for diagnosis and management of patients with AGS
| Consistently Inconsistent |
|
| Isolated Gastrointestinal |
|
| Co-factor Dependence |
|
| Bedtime Routines |
|
Allergen avoidance along with rescue medication(s) are the mainstays of management for AGS [10]. Although AGS is no different from other food allergies in this regard, avoidance of mammalian-derived products is more challenging due to a lack of adequate labeling and the inclusion of common components, such ‘natural’ flavorings, in numerous foods. For <10% of patients, the avoidance diet also includes removing dairy and derivatives as well as gelatin [11]. In addition, multiple medications are derived from mammals and specific mammalian tissues are used as medical devices. Products such as heart valves, gelatin-based plasma expanders, and pancreatic enzymes, are sources of alpha-gal exposure yet may trigger a reaction in more select patient groups [12,13]. In keeping with this, a minority of patients may benefit from avoiding a wide range of products that are prepared with mammalian-derived constituents [14]. Owing to the ubiquitous inclusion of mammal-derived products within both food and healthcare settings, allergen avoidance for patients with AGS can present unique challenges for management and we routinely include a dietician as part of our care team (or suggest referral) [11].
2. Diagnosis of AGS
The following characteristics occur in 85% of patients with AGS:
Onset in adult life after eating mammalian meat without problems for many years
Reactions range from pruritus, localized hives or angioedema to anaphylaxis
Patients can report strictly gastrointestinal symptoms (diarrhea, abdominal cramping, emesis) almost to the exclusion of cutaneous, cardiovascular or respiratory manifestations
Reactions start 3-8 hours after eating non-primate mammalian meat (or consumption of dairy, gelatin, or other mammalian-derived products)
Positive testing for alpha-gal IgE (>0.1 IU/mL)
Improvement of symptoms when adhering to an appropriate avoidance diet
Description of large local reactions to tick or other arthropod bites, often including report of an ‘index’ bite that behaved differently than prior bites
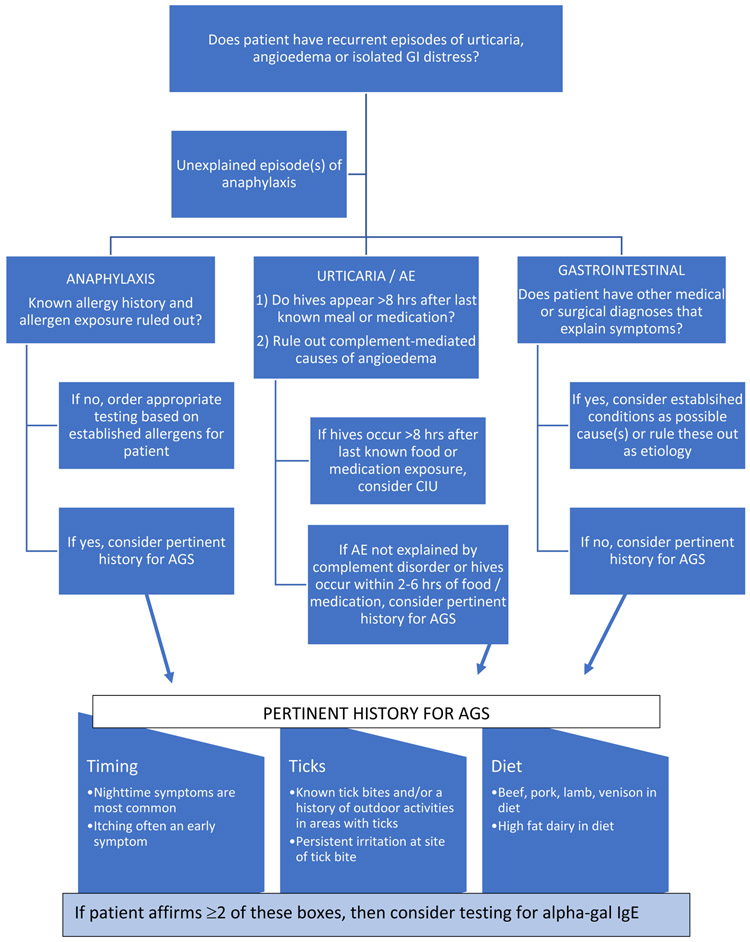
In many settings, the critical point is for the astute clinician to consider AGS as a possible cause of the patient’s symptoms and Figure 1 is included as a diagnostic algorithm. However, it is important to realize that some patients with AGS may not present with these characteristics. Despite point i) above, a significant number of pediatric cases of AGS has been reported [15] and children represent approximately 12% of subjects in one published cohort [16]. Although published data suggest that the condition in children has similar features to those of adult patients, it is not unusual for children with AGS to report a specific association with limited number of foods, predominance of GI symptoms and particular relevance of activity (e.g., sports practice). Moreover, a study of over 200 patients with AGS found that 16% reported subjective symptom onset in less than 2 hours after consuming mammalian meat [16]. History of a tick bite, larval tick bites (e.g., seed tick bites) or ‘chigger’ bites can be supportive of AGS as a diagnosis but the absence of such a history is not uncommon. Tick bites can be painless, and about half of the people who develop a tick-borne infection may not even remember being bitten by a tick. ‘Chiggers’ is a term often mentioned in the South that has become synonymous with ‘very itchy, small, red bites’ that can occur in isolation or in large numbers. We often inquire about ‘chigger’ bites with patients to gain a history of bug bites in general and less in direct questioning of their exposure to members of the Trombiculidae family of insects. Whether Trombiculidae bites can lead to the development of alpha-gal IgE is unclear but is a research question under our investigation.
Figure 1 –
Diagnostic algorithm for alpha-gal syndrome
Limited data do show that alpha-gal IgE rises following bee and wasp stings and begins to decline after 6-8 weeks. The amount of alpha-gal IgE increase appears to be driven by the number of stings: a greater rise was seen in a beekeeping-patient with 5 honeybee stings compared to the others with a single bee or wasp sting. Initial molecular analysis of stinging insect IgE component resolved diagnostics in these subjects showed that Api m 5 was the major allergen, frequently overshooting the Api m 1 value several fold. Api m 5 is a dipeptidyl peptidase and there is a similar, albeit distinct, enzyme in tick saliva that may explain the rise in alpha-gal IgE. It is not clear, however, whether stinging insect envenomation itself can drive the initial alpha-gal IgE response apart from tick bites. Equally, we do not have data directly addressing whether stings from hornets and/or yellow jackets are also associated with increases in alpha-gal IgE.
In terms of diagnosis, skin prick tests with extracts of mammalian meats (beef, pork, or lamb) were shown to be unreliable [1]. The majority of providers rely on commercially available blood testing for alpha-gal IgE that is widely available in the US (via Viracor-Eurofins) and Europe (via Phadia ThermoFisher). If skin testing is preferred, sensitization can be investigated using intradermal (ID) skin tests to the same diluted food extracts [1]; however, several reports suggest ID testing with gelatin may produce more consistent results [14,17-19]. One alternative is prick-prick skin testing using cooked meats – this approach has produced consistent, albeit small (5-7mm), wheals and should properly include a non-mammalian meat as well [1,19]. If beef is the only positive meat by prick-prick testing, a diagnosis of cow’s milk allergy must be ruled out since beef reactivity can occur in a minority of cow’s milk allergic patients [20]. Differentiating AGS from ‘traditional’ cow’s milk allergy can be accomplished efficiently with serum IgE testing for alpha-gal and cow’s milk components (e.g., casein, whey) [15]. There are no established criteria for the titer of alpha-gal IgE that confirms an AGS diagnosis and most clinical authorities report using the cut-off of >0.1 IU/mL as a positive test result, which has a reported specificity of 92.3% and sensitivity of 100% among patients with AGS [6,16,21]. Diagnosis is particularly challenging in patients with a history of reacting to mammalian products but whose blood test for alpha-gal IgE is negative. In our clinical experience, this occurs in approximately 2% of patients referred for AGS evaluation. Not uncommonly, we assess surrogate markers (beef, pork, lamb) by skin and serum IgE testing in these patients. When AGS diagnosis is in doubt due to negative IgE testing, it would be reasonable to test for IgE to cat serum albumin (Fel d 2) to identify patients who may have pork-cat syndrome. Similarly, clinicians could consider testing for IgE to gelatin – both porcine and bovine. As a referral center, we also perform skin testing to alpha-gal-containing biologics such as cetuximab and basophil activation testing. These approaches have led to diagnostic clarification in 41 of 52 (78%) patients with alpha-gal IgE seronegative testing who report compelling symptoms. For those remaining patients with uncertain diagnoses, we offer blinded food challenges using pork and emu sausages on two different occasions. Longitudinal data of patients with AGS suggest that alpha-gal IgE declines over time; additional tick bites, however, appear to lead to rises in alpha-gal IgE [7,16]. Thus, another possible reason for seronegative testing despite a history of symptoms is that a patient’s alpha-gal IgE has declined below the limit of test detection yet remains clinically relevant. Since IgE on the surface of mast cells may persist for months, it is conceivable that undetectable serum levels can occur in the setting of allergen-primed mast cells.
2.1. Food challenges.
We have performed over 150 food challenges, which includes those performed for research, for ‘diagnosis,’ and for assessment of clinical resolution. Due to the unpredictable nature of alpha-gal food challenges, risks and benefits should be discussed with patients [4]. This point should not be minimized: in our experience, 15-20% of food challenge reactions in patients with AGS require one or more doses of epinephrine and/or emergency medical transport. Three colleagues have independently contacted us about a severe alpha-gal food challenge reaction in their offices. As a result, we typically use an informed consent process for these challenges. We consider an alpha-gal food challenge clinically appropriate in several instances:
Patient with unclear etiology of possible allergic episode(s) and has positive alpha-gal IgE >0.1 IU/mL but reports ongoing, asymptomatic consumption of beef, pork, etc
Patient with known history of tick bites (or significant tick exposure) who tests positive for alpha-gal IgE >0.1 IU/mL and was told to avoid red meat due to the test result without supporting symptoms
Patient with alpha-gal IgE <2.0 IU/mL who fully tolerates high fat cow’s milk dairy ice cream, is able to consume a single slice of pepperoni (~12 g) without symptoms and reports no tick bites in the past 12 months
Patient with history of AGS, followed longitudinally, who now tests undetectable (e.g., <0.1 IU/mL) for alpha-gal IgE
Patient has a history suggestive of AGS but tests negative (<0.1 IU/mL) for alpha-gal IgE and diagnostic clarification testing discussed above has been unrevealing [food challenge has been positive in 7 of 11 patients in this scenario]
Our typical alpha-gal food challenge is at least two pork sausage patties (we use Jimmy Dean® original, fully cooked, approximately 70 grams) and preferably three patties for individuals >70 kg as well as those who are able to consume that amount. Complicating the topic is that approximately 10% of the challenges produce a false negative (subject does not react). Larger doses can then be used with great caution in settings where patients report that reactions have been inconsistent, require the presence of a co-factor, or prior challenges have been inconclusive. Depending upon specific patient history, consideration may be given to consumption of challenge dose prior to clinic arrival due to the delayed nature of these reactions. Since IgE-based diagnostics identify sensitization, we also perform alpha-gal food challenges for patients who are found to have alpha-gal IgE without a clear history of allergic reactions. In certain geographic areas and in populations with high tick exposure, the level of sensitization can be 15-35% but this does not represent clinical AGS, which appears to occur in 1-8% of sensitized individuals [2,7,22-25]. Again, larger doses of food challenge antigen may be indicated in these patients or, more recently described, an alpha-gal antigen basophil activation profile may differentiate between allergy and sensitization [26]. We have not found a correlation between alpha-gal sIgE and severity of the clinical syndrome but this may reflect the influence of tick bites on sIgE levels, timing of antigen exposure and incorporation of dairy in the diet [4,7,14,16]. Additional studies are needed in both groups to further characterize these patients and understand the limitations of current diagnostic testing for AGS, particularly as relates to the influence of sensitizing tick species.
2.2. Range of symptoms that can occur in relation to AGS.
Published work suggests that the most important group of ‘non-classical’ symptoms are those that involve the gastrointestinal (GI) tract [6]. While GI complaints are not uncommon as part of an allergic reaction, 3-20% of patients with AGS report abdominal pain, nausea, emesis, diarrhea, heartburn in isolation of cutaneous, cardiovascular or other signs/symptoms [16,27,28]. This pattern of signs and symptoms complicates the diagnosis as well as management of AGS because the possibility of food allergy is not obvious, but patients can be severely affected [27]. Indeed, examples of patients with AGS who have had exploratory surgery, removal of gallbladder or appendix, and partial pancreatectomy have been reported [11]. Notably, <1% of patients have reported isolated itching in the mouth or swelling of the tongue [16]. Other conditions that also arise less commonly, and may not be causally related to AGS, include joint pain and chronic pruritus [16,29]. Distinguishing AGS from chronic spontaneous urticaria (CSU) can be challenging, leading to misdiagnosis and, in some cases, the two entities may overlap [30] [29]. Analysis of other cohorts have found that AGS is not a cause of unrecognized CSU [31]. In keeping with both possibilities, we have seen patients develop AGS and achieve control of reactions through an appropriate avoidance diet yet within weeks or months they develop CSU (despite the continued mammalian avoidance diet). Approximately 3-5% of patients also appear to develop signs/symptoms consistent with a mast cell syndrome, which could be related to mast cell releasing factors present in tick saliva or the significant increase in total IgE leading to increased mast cell reactivity. Alternatively, emergence of a plasmablast-like, IgE-secreting B cell compartment with specific expansion of CCR6+ cells in subjects within 3 weeks of an attached A. americanum or I. scapularis tick bite may explain the new-onset urticaria and possible mast cell activation symptoms [32]. Establishing the role of these IgE-secreting plasmablasts that do not share typical characteristics of classical isotype-switched memory B cells that express high levels of CD27 is a major focus for our research program as this may be the target population for treatment of AGS.
3. Management of AGS
Firstly, all patients should be informed that further tick bites can maintain or lead to increases in the titer of alpha-gal IgE [6,7]. By contrast, most patients (89%) who successfully avoid tick bites will experience a decrease in their alpha-gal IgE level [33]. Although the rate of decline varies and it is not clear what degree of decrease is required to successfully regain tolerance, nearly 12% of patients in our registry followed for at least 5 years had negative titers (<0.1 IU/mL) and successfully re-introduced mammalian meat in their diet [11]. Published data provide strong evidence that eating mammalian meat alone is not sufficient to induce an IgE response to alpha-gal [34]. Equally, similar data also argue against a role for other mammalian exposures in developing AGS [34]; thus, we do not routinely ask patients to remove pets. To date, no studies have established whether eating mammalian meat or consuming dairy can influence the levels of alpha-gal IgE in patients with AGS. An additional point is that some patients with the syndrome may tolerate mammalian meat on occasion with few or no symptoms but have severe reactions on others. This intra-individual variability is often not explained by the amount of meat consumed and may reflect differences in the quantity or form of alpha-gal that is present in the meat or, more likely, reflects the importance of co-factors such as medications, activity, alcohol consumption or recent tick bites [27]. Regarding patients who test positive for alpha-gal IgE but do not report symptoms after eating mammalian meat, there are currently no published augmented food challenge studies or population-based follow-up studies. We suggest a food challenge and/or close monitoring without additional alpha-gal IgE surveillance except in the setting of symptoms as well as avoidance of tick bites.
3.1. Avoidance of mammalian meat
The primary advice for newly diagnosed patients with AGS is to completely avoid meat of mammals [11]. In most areas of the U.S. this means beef, pork, venison and lamb. Internal organs are equally or more able to induce reactions and these should be avoided as well, especially pork kidney [19]. Equally, fattier forms of meat are more consistently associated with symptoms and more severe reactions upon challenge [4,6,28]. Cooking does not appear to significantly denature the alpha-gal epitope but, in our experience, may reduce reaction severity likely through reduction in fat content [35]. Meat and products derived from other mammals such as bison, buffalo, rabbit, horse, and goat should equally be avoided [36]. Patients do report symptoms with exposure to fumes from mammalian meats/fats being cooked; however, no blinded challenges have been published to definitively document the airborne (droplet) route of exposure. Interestingly, experience suggests fumes may pose a more potent risk to reactive patients than moderate levels of pet dander exposure. As with other food allergies, we take an individualized approach to management of AGS [37]. This includes not only dietary avoidance advice (strict vs. isolated exposures vs. daily exposures) but also nutritional management, discussion of labeling issues and hidden exposures, awareness of individual eliciting threshold doses and the possible influence of tick bites, as well as use of masks for fume-sensitive patients, inhaled beta-agonists, prophylactic anti-histamines and even omalizumab.
3.2. Avoidance of dairy products
We do not routinely include avoidance of dairy products as part of primary avoidance, as 80-90% of patients with AGS do not react to milk or cheese [6,11,16]. However, published evidence and expert opinion articles indicate that full avoidance of dairy products perhaps should be recommended in patients already avoiding mammalian meat without adequate control of symptoms [11].
3.3. Avoidance beyond meat and dairy.
Mammal products can be introduced into food and other products that are not obviously mammalian during preparation or manufacturing processes [38]. Evidence for the presence of alpha-gal in these different food and medical products varies markedly, with some items clearly expressing alpha-gal (e.g., cetuximab) and other products avoided simply due to being derived from mammals (e.g., magnesium stearate, glycerin – see Table 2). Of note, alpha-gal has not been detected on bovine serum albumin (BSA) [39] – demonstrating that simply being mammal-derived does not equate to ‘contains alpha-gal.’ When patients continue to have reactions after removal of all obvious forms of alpha-gal from their diet, we turn to the ‘hidden’ forms of mammalian exposure despite little or even no evidence that such moieties actually contain alpha-gal (Table 2). In many cases, it is challenging to make informed assessment of risk based on the available data and we approach the avoidance diet on an individual patient basis. We know from experience with childhood food allergies that some patients can tolerate foods with ‘processed in’ or ‘may contain’ labels and this characteristic appears to hold consistent for AGS [4,17,40]. Equally, there may be some evidence that patients on a strict avoidance diet could experience anaphylaxis after ingestion of minimal amount of allergen and this has mirrored our overall clinical experience [17]. Thus, we focus particular attention to foods and items that are high in mammal fat content, especially when these exposures are paired with activity, alcohol, exercise, stress, lack of sleep, NSAIDs, illness, infection and menses.
Table 2 –
“Hidden” ingredients that may be non-human mammal-derived; alpha-gal content has not been established.
| Ingredient name | Notes |
|---|---|
| Arachidonic acid | Generally isolated from animal liver and found in pet food, skin creams, and lotions. |
| Arachidyl proprionate | Wax that can be made from animal fat |
| Biotin | Ubiquitous in every living cell but can be found in high amounts in milk |
| Carrageenan | Linear sulfated polysaccharides that are extracted from red edible seaweeds; contains alpha gal but amount and risk not clear |
| Castoreum | Used in some perfumes; derived from beaver’s castor sack |
| Glycerin | Often made from animal fat; can be plant or fish-derived |
| Lanolin | A product of the oil glands of sheep, extracted from their wool. Often applied as a lotion, in cosmetics or in medications. |
| Latex | May contain casein (see milk derivates) |
| Milk proteins | Labels may not indicate dairy but assess for these ingredients: biotin, casein, caseinate, sodium caseinate, whey |
| Myristic acid | Typically derived from nut oils (safe); occasionally of animal origin |
| Oleic acid | Usually obtained from inedible beef fat but can be vegetable-derived; verify with manufacturer. |
| Stearic acid | Also seen as magnesium stearate. When animal-derived, a fat from cows, pigs, sheep, etc. May also be of plant origin, including from cocoa butter and shea butter; verify with manufacturer. |
Potentially relevant food & cooking exposures to consider in the management of the patient with AGS:
Fat: High fat foods or those prepared with added fat are most consistently implicated in reactions and often are associated with more severe reactions. Lard (pork fat) is particularly important in Southern cooking and is frequently found in gravies and sauces. Importantly, lard may also be added to vegetables, mashed potatoes, or fry oil to enhance flavor. Tallow and suet are also mammalian fats commonly used in cooking, including desserts.
Sausages: Many varieties of sausages use casings derived from the pork gut. Patients have reported consuming chicken and turkey sausages, which they thought would be safe, that then led to allergic reactions.
Food additives: The two most relevant food additives that can contain alpha-gal epitopes are gelatin and carrageenan. Gelatin (a glycoprotein) typically comes from skin or hooves of hogs, horses, cows or other large mammals. In regards to food, gelatin is a main ingredient of gelatin desserts (e.g., Jello™), jellybeans, marshmallows, and puddings. Reactivity to gelatin is not uncommon among patients with AGS [17]; however, most patients tolerate the smaller exposures of everyday life [38]. It is likely that the amount of alpha-gal content and spatial arrangement of repeating alpha-gal epitopes is affected by processing and extraction of the raw material, which ultimately affects the risk for reactions. Carrageenan (a phycocolloid polysaccharide) is extracted from red edible seaweeds and is widely used in the food industry as a thickener and stabilizer. Although carrageenan is known to contain alpha-gal epitopes [41], clinical experience suggests the risk of reactions appears to be quite low and is likely pertinent to 1-2% of patients with AGS. One of the unfortunate issues we have found with carrageenan is that it can be included in plant-based foods (such as nut ‘milks’), which would otherwise be alpha-gal-free. Equally, exposure to carrageenan can occur in unsuspected manners: toothpaste, beer, personal lubricants, shampoos. Thus, in patients who report reactions despite an appropriate avoidance diet, careful analysis for carrageenan exposure might be indicated.
Stocks and bouillon cubes: these are often derived from mammalian sources and additional research is needed to understand the risks from these and other, ‘hidden’ exposures (Table 2).
3.4. Medical management of AGS
Given the myriad of exposures detailed above and those not even known or identified to date, we will implement adjunctive medical therapies for patients with AGS who either remain symptomatic or will have potential high risk for exposures (ex., travel to area where street-food is primary source of food – especially if not native language). A typical medication regimen may include:
Oral antihistamine (inverse agonist): we prefer long-acting oral antihistamines (OAH) such as fexofenadine or levocetirizine dosed twice daily. We have not had significant issues with stearate or lactose in either medication. For patients that do not tolerate these formulations, a similar long-acting OAH can be compounded. Another possible approach is to use short-acting OAH in on-demand dosing and in this scenario, many patients have successfully tolerated Unisom® SleepMelt™ tablets that contain 25 mg diphenhydramine without stearate or lactose. Additionally, an H2 antihistamine can be included in a setting of prophylaxis or for increased symptom management.
Oral cromolyn solution: we prefer this mast cell stabilizer medication for patients who report significant or persistent gastrointestinal symptoms despite an appropriate avoidance diet. Cromolyn solution (100 mg / 5 mL) can be dosed up to 4 times daily with a range from 100 mg – 200 mg per dose. We begin at 100 mg twice daily taken 20-30 minutes prior to meals and increase as tolerated to control symptoms.
Oral corticosteroid: used much as one might prescribe for a patient with asthma who is having an acute exacerbation, a 5-7-day short burst and taper has occasionally been quite helpful for AGS patients with acute, recurrent reactions especially in the setting of unknown exposures. Equally, we often provide a similar course to have available for our patients with AGS when traveling to areas where concern is high for cross-contamination and/or difficulty communicating with food preparation staff.
Omalizumab: we have successfully used omalizumab for control of continued reactivity, which could appear as CSU. In some instances, our patients on omalizumab have been able to add a small amount of red meat exposure back to their diets. For the patients who develop symptoms more consistent with a ‘mast cell activation’ phenotype with frequent need for acute care, omalizumab has also proven efficacious and can be advocated for due to reduction in healthcare utilization costs. We do not yet have sufficient data to assess whether omalizumab can prevent (or blunt) the rise in alpha-gal IgE following additional tick bites. It is worth mentioning that we have used compounded ketotifen with limited success in patients with mast cell activation symptoms who were unable to obtain omalizumab. Clearly, a true clinical trial with omalizumab (or other anti-IgE therapy) is needed for patients with AGS and other food allergies.
Metformin: six patients taking metformin in preparation for gastric bypass surgery have been able to resume dairy consumption and even return red meat to their diets. A similar observation in a murine model of food allergy has been reported by Dr. Fred Finkelman’s group and their suggestion is that metformin has effects on the unfolded protein response which can alter cytokine milieu and may lead to antigen re-programming [42,43].
3.5. Additional relevant medical exposures for patients with AGS
There are important medical uses of mammalian-sourced medications, treatments and devices that were not immediately apparent in the initial description of AGS as a delayed allergy to red meat. Table 3 summarizes the points above and below for clinicians and patients. Over the ensuing decade, we have developed significant experience relating to these, largely iatrogenic, exposures and subsequent reactions:
Table 3 –
Checklist for providers counseling patients with AGS
| Guidance for all patients at initial AGS diagnosis |
|---|
| FOOD |
| Avoid mammalian meats |
| Be cautious with high fat dairy & large amounts of butter |
| Educate regarding co-factors (esp., alcohol and activity) in setting of alpha-gal food exposure |
| Eating out can be challenging – inquire about fry oil, gravies, sauces and stocks. Some fast food restaurants add lard or suet to fryer (including French fries) |
| If tolerating dairy, full avoidance of this exposure may not be necessary |
| Equally, if dairy is tolerated then gelatin and carrageenan are often not issues |
| Cross-contamination during home cooking is typically ok (e.g., sharing spatulas) |
| Consider emu and duck as sources of meat to supplement chicken, turkey, seafood |
| Reminder about sausage casing as potential source of alpha-gal exposure |
| Consider referral to nutritionist if concern about safe and healthy forms of protein |
| ENVIRONMENT |
| Discuss tick bite prevention; refer to CDC website |
| Additional tick bites can increase sensitivity to various exposures (often transiently) |
| Having pets is fine but educate that pet dander can contain alpha-gal |
| Fumes from cooking mammalian meats are reported as an issue for some patients – consider educating in advance (although avoidance is not typically necessary) |
| Educate that bee, wasp, hornet stings may also lead to increased alpha-gal IgE |
| MEDICATIONS |
| Educate about heparin as possible iatrogenic exposure |
| Gelatin-based capsules are commonly not an issue |
| Lactose, microcrystalline cellulose and magnesium stearate may contain alpha-gal but are frequently not an issue |
| Should not receive vaccines with gelatin, if possible |
| Guidance for patients with continued reactivity despite avoidance diet |
| FOODS |
| Remove dairy in all forms, including butter |
| Remove gelatin and carrageenan |
| Read labels to avoid ‘natural’ flavoring as this often means pork or beef |
| ENVIRONMENT |
| Consider monthly washing of pets |
| Avoid fumes of mammalian meats being cooked |
| MEDICATION |
| Consider starting a daily oral anti-histamine |
| Switch to tablet formulations, consider opening capsules and taking with foods, if appropriate (e.g., medication is not time-release), or consider compounding pharmacy that will use plant-based gelatin capsule. |
| PERSONAL PRODUCTS |
| Switch to natural toothpaste |
| Avoid creams or lotions with lanolin |
Heparin: Heparin is derived from pig intestines. A small number of case reports have raised the possibility of heparin-induced allergic reactions in patients with AGS [11,12]. Importantly, we have not had issues with routine heparin prophylaxis for deep venous thrombosis (DVT) and our experience suggests this can be safely administered for the overwhelming majority of patients with AGS. There are, undoubtedly, exceptions that will require alternate forms of DVT prophylaxis. Heparin-based reactions that are much more common include those clinical scenarios where heparin is given at high doses for more complete anti-coagulation, such as during heart catheterization, valve procedures and extracorporeal membrane oxygenation (ECMO). In these instances, we favor a conversation with the surgical team to assess risk-benefit to the patient as opposed to strict avoidance of heparin. In fact, a standard pre-medication regimen using corticosteroid, antihistamine and even omalizumab has been successful at minimizing reactions to large doses of heparin in our experience. Out of an abundance of caution, we recommend use of sodium citrate as an alternative anti-coagulant for blocking ports or central lines in patients with AGS.
Engineered antibodies: Many monoclonal antibodies (mAbs) used clinically are produced in non-primate mammalian cell lines; however, the evidence for alpha-gal expression on most mAbs other than cetuximab is minimal. One exception is abatacept (Orencia), which is manufactured in a Chinese hamster ovary (CHO) cell line and also shown to contain the alpha-gal epitope [44]. Three of our patients reported reactions to abatacept and we know of a colleague, Dr. David Fitzhugh (Chpael Hill, NC), who has seen a patient with AGS that had ‘immediate and profound anaphylaxis’ to IV abatacept (personal communication). Another exception is infliximab, which has been shown to express low amounts of the alpha-gal and, despite wide usage, has been linked to only a small number of reactions in patients with AGS [45]. Despite an apparent risk with some CHO cell-produced mAbs, we have successfully administered omalizumab to numerous patients with AGS. Perhaps the route of delivery is critical to creating a risk for reaction; nevertheless, we proceed with caution (e.g., divided dose 10-90 plus extended observation time) on first dose of any mAb produced in a mammalian cell line.
Gelatin: The most severe reactions involving gelatin are anaphylaxis that has been well-documented when gelatin was administered IV as a plasma expander in some countries, particularly Australia and the U.K. [14,46]. Vaccines are also an important source of gelatin exposure, including Zostavax and MMR [13,47]. Cases of reactions to these vaccines in patients with alpha-gal IgE have been reported [47]. Gelatin capsules (“gel-caps”) are used for many medicines and may give rise to symptoms in a small proportion of patients. This exposure has been an infrequent (<5%) source of heartburn and/or nausea in patients, especially those whose medication regimen make contain multiple gelatin-based capsules [11].
Pancreatic enzymes: The enzymes used for replacement of pancreatic function (e.g., pancrealipase) are purified from the pancreas of large mammals. These proteins, and other mammalian-derived enzymes, have been shown to elicit positive skin tests yet have been administered successfully in several patients [47]. Alternatively, we have patients who were not diagnosed with AGS (due to their dietary choices) until beginning pancreatic enzymes, and this mammalian exposure produced symptoms (predominantly pruritus).
Thyroid hormones: Supplementation or replacement of endogenous thyroid hormone with ‘natural’ products (e.g., Armour thyroid) may be less ideal in patients with AGS since these products are derived from porcine thyroid glands. However, if patients feel strongly regarding this choice, we often supervise initial dosing in the clinic and only cease if symptoms develop (which we have seen happen both acutely as well as after several weeks of dosing). Of note, this issue – as well as that of pancreatic enzyme replacement and heart valves (see below) – may be solved by using alpha-gal deficient pigs as a source of material.
Bioprosthetic heart valves: Published reports have described patients who experienced hives or even anaphylaxis after transplantation of bovine or porcine heart valves [12]. As with heparin, the most important aspect to a successful valve replacement procedure in patients with AGS is communication with the surgical team. Through pre-medication, we have been successful in multiple cases with patients experiencing only minimal symptoms, which may have been related to heparin. More recently, mammalian valve degeneration in patients with alpha-gal IgE has been reported [48]. Although a collaboration is underway, no longitudinal study has been published that assesses whether developing alpha-gal IgE, a pro-inflammatory isotype, is associated with premature bioprosthetic valve destruction.
Anti-venom: Alpha-gal is present in anti-venom formulations because these purified fragments are derived from venom-immunized non-primate mammals. There has been at least one case report of an acute reaction to CroFab in a patient with AGS [49]. Despite this report, we advise administration of CroFab if clinically indicated even in patients with AGS as the risk of reaction to anti-venom has not been established in this scenario and may be quite low while, on the contrary, the therapeutic benefit of anti-venom is high.
4. Conclusion
It has now been ten years since the initial publications describing the oligosaccharide galactose-α-1,3-galactose as an IgE-binding epitope and a causal antigen in anaphylaxis to mammalian products. Alpha-gal Syndrome can involve immediate reactions to drugs which are delivered intravascularly, but characteristically manifests with a delay of 3-6 hours upon oral ingestion of mammalian products such as meat, organs and/or dairy. Although there are many ways that AGS could be considered to “break the rules,” investigation into this unusual allergen is likely to reveal novel insights into the causes and consequences of all allergic diseases. Based on the progress of understanding AGS in the initial decade, the next 10 years are likely to be an equally exciting and paradigm-shifting time.
5. Expert opinion
Increasing awareness of AGS among healthcare providers is a critical first step in addressing the unmet needs in the diagnosis and management of AGS. In geographic areas where tick bites are common, AGS is likely under-recognized and under-diagnosed. We suggest testing for alpha-gal IgE in tick-endemic areas as part of the evaluation for cases of idiopathic anaphylaxis, recurrent urticaria and/or angioedema, as well as recurrent, episodic gastrointestinal cramping of unestablished cause (Fig 1). Considerations to increase awareness of AGS could include making the diagnosis reportable, which could be accomplished in conjunction with the Centers for Disease Control and Prevention. Development of a repository of AGS-related information for patients and families, as well as providers is also an opportunity. In addition, published data related to the characteristics of alpha-gal IgE testing is lacking, including more basic parameters as sensitivity, specificity, as well as positive and negative predictive values. Larger population studies represent an important opportunity to define these diagnostic issues. As with management for any food allergy, AGS management is based on allergen avoidance. For patients with AGS, however, this tenet of self-protection is made difficult by the lack of adequate labeling for mammalian-derived sources in foods, medications, and vaccines. Approval of alpha-gal free porcine products would represent an effective way to develop ‘AGS-safe’ foods, medications, and implantable devices.
The prevalence of AGS cases is unknown, and it remains a challenge for widespread integration of AGS into healthcare training and awareness. In addition, the lack of a confirmed association between AGS and ticks as a vector for disease poses challenges for funding and for identification of at-risk individuals. We also need to better understand the risk of reactions to the wide variety of products that may include small amounts of material derived from mammals.
Article Highlights.
Alpha-gal Syndrome (AGS) is an IgE-mediated allergy affecting an increasing number of patients worldwide
AGS is characterized by delayed reactions after eating non-primate mammalian meat (e.g., beef, pork, lamb) or foods, medications and personal products that contain mammal-derived ingredients
AGS can be a challenging clinical diagnosis to make due to delayed reactions and guidance is provided for practicing clinicians to assist with recognizing and managing these patients
Unique among food allergies, AGS is due to a carbohydrate directed IgE response, can occur at any age, and appears to arise following a tick bite
Patients often present with nighttime urticaria, angioedema, anaphylaxis or even isolated gastrointestinal symptoms that are highly influenced by co-factors, including exercise & alcohol
Owing to numerous ‘hidden’ alpha-gal exposures beyond red meats and the need for individualized guidance, we recommend co-management with dietician colleagues
Funding
The author declares the following as sources of funding: U.S. Department of Health and Human Services; National Institutes of Health; National Institute of Allergy and Infectious Diseases; K08 AI085190; R01 AI135049
Footnotes
Declaration of interest
The author declares research grants from NIH and CDC; a member of Genentech speaker’s bureau; has received royalties from UpToDate
Reviewers Disclosure
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
Non-primate mammalian meat refers to meat derived from any mammal that is not a human or Great Ape. Commonly consumed examples are beef, pork, lamb, venison, rabbit, goat, squirrel, buffalo, etc. and include organ meats. For the purposes of this report, the term ‘mammalian meat’ and ‘mammalian-derived’ will be used to refer to non-primate mammalian meat and its animal sources as these are alpha-gal containing foods or products. Equally, note that references may state ‘mammalian meat’ or ‘red meat’ yet these also refer to non-primate mammalian meat, which is the primary source of alpha-gal.
References
Papers of special note have been highlighted as:
* of interest
** of considerable interest
- 1.Commins SP, Satinover SM, Hosen J, et al. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2009. February;123(2):426–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung CH, Mirakhur B, Chan E, et al. Cetuximab-induced anaphylaxis and IgE specific for galactose-alpha-1,3-galactose. N Engl J Med. 2008. March 13;358(11):1109–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Commins SP, Jerath MR, Cox K, et al. Delayed anaphylaxis to alpha-gal, an oligosaccharide in mammalian meat. Allergol Int. 2016. January;65(1):16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Commins SP, James HR, Stevens W, et al. Delayed clinical and ex vivo response to mammalian meat in patients with IgE to galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2014. July;134(1):108–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flaherty MG, Kaplan SJ, Jerath MR. Diagnosis of Life-Threatening Alpha-Gal Food Allergy Appears to Be Patient Driven. J Prim Care Community Health. 2017. October;8(4):345–348.*The authors interviewed patients with AGS and found that an average of 7 years passed between onset of symptoms and diagnosis of AGS.
- 6.Levin M, Apostolovic D, Biedermann T, et al. Galactose alpha-1,3-galactose phenotypes: Lessons from various patient populations. Ann Allergy Asthma Immunol. 2019. June;122(6):598–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Commins SP, James HR, Kelly LA, et al. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-α-1,3-galactose. J Allergy Clin Immunol. 2011. May;127(5):1286–93.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crispell G, Commins SP, Archer-Hartman SA, et al. Discovery of Alpha-Gal-Containing Antigens in North American Tick Species Believed to Induce Red Meat Allergy. Front Immunol. 2019;10:1056.**This report used mass spectroscopy to analyze tick salivary carbohydrate composition and reports the presence of alpha gal in tick saliva. Also noted that saliva from Ixodes scapularis appear to contain alpha-gal in addition to lone star ticks.
- 9.Brockow K, Kneissl D, Valentini L, et al. Using a gluten oral food challenge protocol to improve diagnosis of wheat-dependent exercise-induced anaphylaxis. J Allergy Clin Immunol. 2015. April;135(4):977–84 e4. [DOI] [PubMed] [Google Scholar]
- 10.Renz H, Allen KJ, Sicherer SH, et al. Food allergy. Nat Rev Dis Primers. 2018. January 4;4:17098. [DOI] [PubMed] [Google Scholar]
- 11.Commins SP. Invited Commentary: Alpha-Gal Allergy: Tip of the Iceberg to a Pivotal Immune Response. Curr Allergy Asthma Rep. 2016. September;16(9):61. [DOI] [PubMed] [Google Scholar]
- 12.Mozzicato SM, Tripathi A, Posthumus JB, et al. Porcine or bovine valve replacement in 3 patients with IgE antibodies to the mammalian oligosaccharide galactose-alpha-1,3-galactose. J Allergy Clin Immunol Pract. 2014 2014. Sep-Oct;2(5):637–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stone CA Jr., Hemler JA, Commins SP, et al. Anaphylaxis after zoster vaccine: Implicating alpha-gal allergy as a possible mechanism. J Allergy Clin Immunol. 2017. May;139(5):1710–1713 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mullins RJ, James H, Platts-Mills TA, et al. Relationship between red meat allergy and sensitization to gelatin and galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2012. May;129(5):1334–1342 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kennedy J, Stallings A, Platts-Mills T, et al. Galactose-alpha-1,3-galactose and Delayed Anaphylaxis, Angioedema, and Urticaria in Children. Pediatrics. 2013;131(5):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson JM, Schuyler AJ, Workman L, et al. Investigation into the alpha-Gal Syndrome: Characteristics of 261 Children and Adults Reporting Red Meat Allergy. J Allergy Clin Immunol Pract. 2019. Sep-Oct;7(7):2348–2358 e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caponetto P, Fischer J, Biedermann T. Gelatin-containing sweets can elicit anaphylaxis in a patient with sensitization to galactose-α-1,3-galactose. J Allergy Clin Immunol Pract. 2013 2013. May-Jun;1(3):302–3. [DOI] [PubMed] [Google Scholar]
- 18.Ebo DG, Faber M, Sabato V, et al. Sensitization to the mammalian oligosaccharide galactose-alpha-1,3-galactose (alpha-gal): experience in a Flemish case series. Acta Clin Belg. 2013 2013. May-Jun;68(3):206–9. [DOI] [PubMed] [Google Scholar]
- 19.Fischer J, Hebsaker J, Caponetto P, et al. Galactose-alpha-1,3-galactose sensitization is a prerequisite for pork-kidney allergy and cofactor-related mammalian meat anaphylaxis. J Allergy Clin Immunol. 2014. September;134(3):755–759.e1. [DOI] [PubMed] [Google Scholar]
- 20.Fiocchi A, Restani P, Riva E, et al. Heat treatment modifies the allergenicity of beef and bovine serum albumin. Allergy. 1998. August;53(8):798–802. [DOI] [PubMed] [Google Scholar]
- 21.Brestoff JR, Zaydman MA, Scott MG, et al. Diagnosis of red meat allergy with antigen-specific IgE tests in serum. J Allergy Clin Immunol. 2017. August;140(2):608–610 e5. [DOI] [PubMed] [Google Scholar]
- 22.Hamsten C, Tran TA, Starkhammar M, et al. Red meat allergy in Sweden: Association with tick sensitization and B-negative blood groups. J Allergy Clin Immunol. 2013. October. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burk CM, Beitia R, Lund PK, et al. High rate of galactose-alpha-1,3-galactose sensitization in both eosinophilic esophagitis and patients undergoing upper endoscopy. Dis Esophagus. 2016. August;29(6):558–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Villalta D, Pantarotto L, Da Re M, et al. High prevalence of sIgE to Galactose-alpha-1,3-galactose in rural pre-Alps area: a cross-sectional study. Clin Exp Allergy. 2016. February;46(2):377–80. [DOI] [PubMed] [Google Scholar]
- 25.Fischer J, Lupberger E, Hebsaker J, et al. Prevalence of type I sensitization to alpha-gal in forest service employees and hunters. Allergy. 2017. October;72(10):1540–1547. [DOI] [PubMed] [Google Scholar]
- 26.Mehlich J, Fischer J, Hilger C, et al. The basophil activation test differentiates between patients with alpha-gal syndrome and asymptomatic alpha-gal sensitization. J Allergy Clin Immunol. 2019. January;143(1):182–189. [DOI] [PubMed] [Google Scholar]
- 27.Iweala OI, Choudhary SK, Commins SP. Food Allergy. Curr Gastroenterol Rep. 2018. April 5;20(5):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mabelane T, Basera W, Botha M, et al. Predictive values of alpha-gal IgE levels and alpha-gal IgE: Total IgE ratio and oral food challenge-proven meat allergy in a population with a high prevalence of reported red meat allergy. Pediatr Allergy Immunol. 2018. December;29(8):841–849.*Large cohort of AGS subjects that had food challenges performed and demonstrated a striking number with solely GI issues.
- 29.Pollack K, Zlotoff BJ, Borish LC, et al. alpha-Gal Syndrome vs Chronic Urticaria. JAMA Dermatol. 2019. January 1;155(1):115–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ghahramani GK, Temprano J. Tick bite-related meat allergy as a cause of chronic urticaria, angioedema, and anaphylaxis in endemic areas. Int J Dermatol. 2015. February;54(2):e64–5. [DOI] [PubMed] [Google Scholar]
- 31.Maurer M, Church MK, Metz M, et al. Galactose-alpha-1,3-Galactose Allergy Is Not a Hitherto Unrecognized Cause of Chronic Spontaneous Urticaria. Int Arch Allergy Immunol. 2015;167(4):250–2. [DOI] [PubMed] [Google Scholar]
- 32.Cox KM, Commins SP, Capaldo BJ, et al. An integrated framework using high-dimensional mass cytometry and fluorescent flow cytometry identifies discrete B cell subsets in patients with red meat allergy. Clin Exp Allergy. 2019. May;49(5):615–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim MS, Straesser MD, Keshavarz B, et al. IgE to galactose-alpha-1,3-galactose wanes over time in patients who avoid tick bites. J Allergy Clin Immunol Pract. 2020. January;8(1):364–367 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Commins SP, Kelly LA, Rönmark E, et al. Galactose-α-1,3-galactose-specific IgE is associated with anaphylaxis but not asthma. Am J Respir Crit Care Med. 2012. April;185(7):723–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Apostolovic D, Tran TA, Hamsten C, et al. Immunoproteomics of processed beef proteins reveal novel galactose-alpha-1,3-galactose-containing allergens. Allergy. 2014. October;69(10):1308–15. [DOI] [PubMed] [Google Scholar]
- 36.Fischer J, Biedermann T. Delayed immediate-type hypersensitivity to red meat and innards: current insights into a novel disease entity. J Dtsch Dermatol Ges. 2016. January;14(1):38–44. [DOI] [PubMed] [Google Scholar]
- 37.D'Auria E, Abrahams M, Zuccotti GV, et al. Personalized Nutrition Approach in Food Allergy: Is It Prime Time Yet? Nutrients. 2019. February 9;11(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caponelto P, Fischer J, Biedermann T. Gelatin-containing sweets can elicit anaphylaxis in a patient with sensitization to galactose-alpha-1,3-galactose. J Allergy Clin Immunol: In Practice. 2013;1:302–303. [DOI] [PubMed] [Google Scholar]
- 39.Thall A, Galili U. Distribution of Gal alpha 1----3Gal beta 1----4GlcNAc residues on secreted mammalian glycoproteins (thyroglobulin, fibrinogen, and immunoglobulin G) as measured by a sensitive solid-phase radioimmunoassay. Biochemistry. 1990. April;29(16):3959–65. [DOI] [PubMed] [Google Scholar]
- 40.Wolver SE, Sun DR, Commins SP, et al. A peculiar cause of anaphylaxis: no more steak? The journey to discovery of a newly recognized allergy to galactose-alpha-1,3-galactose found in mammalian meat. J Gen Intern Med. 2013. February;28(2):322–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chauhan PS, Saxena A. Bacterial carrageenases: an overview of production and biotechnological applications. 3 Biotech. 2016. December;6(2):146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Samavedam UKS, Khodoun M, Wu D, et al. Saturated fatty acids promote allergic (Th2) cytokine responses by activation of unfolded protein response (UPR) and ER stress. The Journal of Immunology. 2016;196(1 Supplement):123.9–123.9. [Google Scholar]
- 43.Samavedam UKS, Morris SC, Khodoun M, et al. Saturated fat-induced food allergy: A paradigm for unfolded protein response (UPR)-mediated allergic inflammation. The Journal of Immunology. 2018;200(1 Supplement):104.14–104.14.*Interesting report of the UPR associated with Th2 cytokines and may suggest a new target for food allergy therapeutics.
- 44.Bosques CJ, Collins BE, Meador JW 3rd, et al. Chinese hamster ovary cells can produce galactose-alpha-1,3-galactose antigens on proteins. Nat Biotechnol. 2010. November;28(11):1153–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chitnavis M, Stein DJ, Commins S, et al. First-dose anaphylaxis to infliximab: a case of mammalian meat allergy. J Allergy Clin Immunol Pract. 2017. Sep-Oct;5(5):1425–1426. [DOI] [PubMed] [Google Scholar]
- 46.Uyttebroek A, Sabato V, Bridts CH, et al. Anaphylaxis to succinylated gelatin in a patient with a meat allergy: galactose-alpha(1, 3)-galactose (alpha-gal) as antigenic determinant. J Clin Anesth. 2014. November;26(7):574–6. [DOI] [PubMed] [Google Scholar]
- 47.Stone CA Jr., Commins SP, Choudhary S, et al. Anaphylaxis after vaccination in a pediatric patient: further implicating alpha-gal allergy. J Allergy Clin Immunol Pract. 2019. January;7(1):322–324 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hawkins RB, Frischtak HL, Kron IL, et al. Premature Bioprosthetic Aortic Valve Degeneration Associated with Allergy to Galactose-Alpha-1,3-Galactose. J Card Surg. 2016. July;31(7):446–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fischer J, Eberlein B, Hilger C, et al. Alpha-gal is a possible target of IgE-mediated reactivity to antivenom. Allergy. 2017. May;72(5):764–771. [DOI] [PubMed] [Google Scholar]