Abstract
Slip outcomes are categorized as either a backward loss of balance (LOB) or a no loss of balance (no-LOB) in which an individual does not take a backward step to regain their stability. LOB includes falls and nonfalls, while no-LOB includes skate overs and walkovers. Researchers are uncertain about which factors determine slip outcomes and at which critical instants they do so. The purpose of the study was to investigate factors affecting slip outcomes in proactive and early reactive phases by analyzing 136 slip trials from 68 participants (age: 72.2 [5.3] y, female: 22). Segment angles and average joint moments in the sagittal plane of the slipping limb were compared for different slip outcomes. The results showed that knee flexor, hip extensor, and plantar flexor moments were significantly larger for no-LOB than for LOB in the midproactive phase, leading to smaller shank-ground and foot-ground angles at the slip onset, based on forward dynamics. In the early reactive phase, the hip extensor and plantar flexor moments were larger for no-LOB than for LOB, and all segment angles were smaller for no-LOB. Our findings indicate that the shank angle and knee moment were the major determinants of slip outcomes in both proactive and reactive phases.
Keywords: proactive control, reactive control, fall, segment angle, joint moment
Falls can cause serious, devastating consequences for older adults,1,2 and slipping alone accounts for ~25% of falls among older people.3,4 Although ~30% of slip-related falls are injurious,5 not all slips lead to falls, and quite a few of them result in harmless transient postural disturbances.6 Consequently, the investigation of strategies that could prevent a potentially devastating outcome from a slip is important for slip-related fall prevention.
Evidence indicates that the central nervous system relies on reactive (feedback) control to recover from unexpected and unpredictable perturbations during movement.7,8 Specifically, for gait-slip perturbations, reactive control is effective for restoring one’s stability after a slip,9–11 and different reactive responses can lead to differences in slip performance,12 which can be broadly classified into backward loss of balance (LOB) and no loss of balance (no-LOB) classifications. Stability can be defined as the ability to maintain and regulate the projected center of mass (COM) state (ie, its position and velocity) within the limits of the base of support (BOS) during both static and dynamic tasks.13 Previous theoretical work has developed computation stability thresholds, which are postulated to be internal representations of stability. If an individual’s COM state locates within these thresholds, the person can be stable without the need of changing the BOS by stepping actions (ie, no-LOB).14 An LOB occurs when, upon a perturbation, the COM state is destabilized and traverses beyond the computational thresholds of backward balance loss in which a backward stepping action is required from the trailing limb.
The LOB classification could further be divided into fall and nonfall outcomes. A fall resulting from an external gait-slip perturbation can be custom defined as a sudden, uncontrolled, and irreversible hip descent resulting from the failure to reestablish stability or an inability to generate adequate vertical limb support (eg, via increase in net extensor torque),15 usually resulting in body contact with the lower-level ground. Alternatively, upon balance loss, restabilizing the COM state by taking an effective recovery step and/or providing sufficient vertical limb support to retard and/or reverse hip descent could turn a fall into a nonfall outcome.15 For both outcomes, the trailing limb lands behind the slipping limb (Figure 1A).
Figure 1 —
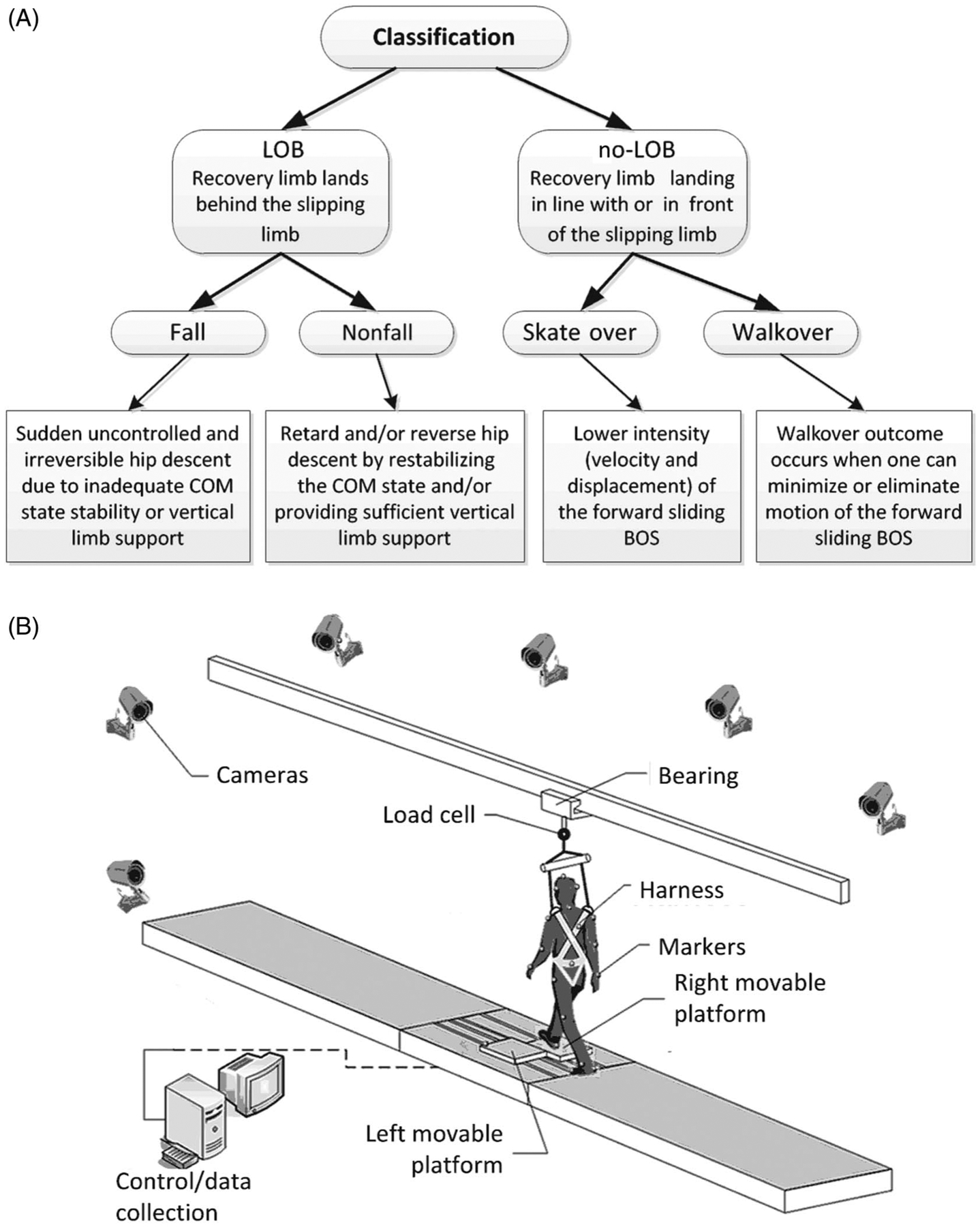
(A) The schematic diagram of slip outcomes, which can be broadly classified into backward LOB and no-LOB classifications. A LOB occurs when a backward stepping action is required from the trailing limb; otherwise, the outcome would be a non-LOB. The LOB classification could further be divided into fall and nonfall outcomes, and the no-LOB could also be further divided into walkover and skate over outcomes. (B) The 7-m walkway with embedded low-friction movable platforms for inducing overground slips and overground walking. The movable platforms were firmly locked during regular walking and unlocked electronic-mechanically without subjects’ awareness only in the slip trial at the instant of their right heel strike on the right platform. LOB indicates loss of balance; no-LOB, no loss of balance.
Similarly, upon a perturbation, if the body COM state can withstand the external destabilization and remain within the feasible stability region without the need for grasping or stepping actions, a balance loss can be prevented (ie, no-LOB). For example, after slip onset (SON), effective reactive responses, including increasing knee flexor and hip extensor moments in the slipping limb, can reduce the velocity of the forward sliding BOS11,16 and, hence, can reduce the likelihood of balance loss.10 For gait-slip perturbations, the no-LOB could also be further divided into skate over and walkover outcomes. A skate over outcome occurs when one can lower the intensity (velocity and displacement) of the forward sliding BOS but not eliminate it, whereas a walkover outcome occurs when one can minimize or eliminate the motion of the forward sliding BOS; nonetheless, both result in the trailing/recovery limb landing in line with or in front of the slipping limb, like regular gait (Figure 1A).
In addition to reactive adjustments, proactive adjustments (predominantly via feedforward control) of the slipping limb before SON also play a key role in affecting slip outcomes, especially when individuals realize they may experience a fall (ie, walking outside on a snowy or icy surface). Previous studies reported that the slipping limb critically determined slip outcomes before the recovery touchdown11; with a preslip flat foot landing, as well as increased knee-flexion angle of the slipping limb, individuals could reduce the slip intensity due to a reduction in the subsequent reactive braking impulse.17,18 Such changes subsequently affect the outcome of a slip to be a LOB, which could be either a fall or a nonfall as aforementioned.10,19,20 For example, Bhatt et al17 reported that, with receiving repeated slip perturbations, subjects adopted a more forward COM position relative to BOS before SON, which eliminated the need for a recovery stepping. Further proactive adjustments made in response to the awareness of a potential slip have also been known to enhance stability, reduce slip severity, and improve slip outcomes.21,22
Although it is known that kinematic and kinetic controls of the slipping limb were found to be related to the risk of slip-induced falls, relatively few studies have investigated whether there are specific movement control factors that can classify those who experience a LOB from a no-LOB. More importantly, it is unclear which of those factors contributes to further differentiating the slip responses into the possible 4 slip outcomes (LOB with and without fall, and no-LOB with skate over or walkover). Most previous studies have only examined the contribution of feet kinematics to slip outcomes,23,24 but the contribution of hip and knee kinematics and kinetics is still unclear. In addition, the mechanisms of lower limb control, such as joint moments and their relation to slip outcomes in the proactive phase, have been less studied for large-magnitude perturbations. Therefore, this study systematically investigated and compared the contribution of kinematic and kinetic factors to recovery in both the proactive and reactive phases. Understanding the mechanisms that contribute to recovery could provide insight for designing fall prevention interventions, such as targeting specific muscle group strengthening or retraining movement strategies.
Therefore, the purpose of the study was, first, to compare the kinematic and kinetic differences between 2 overall slip classifications (LOB vs no-LOB), and we hypothesized that there would be specific segment angle(s) and/or joint moment(s) that could differentiate a potential LOB outcome from the no-LOB. However, an event of LOB does not necessarily always result in falls, and the prime factors affecting the consequence of falls or nonfalls also need to be evaluated. Furthermore, in the event that a balance loss is prevented (no-LOB outcome), a walkover outcome was proposed to be a better recovery strategy compared to skate over due to having better reactive stability.17 Therefore, we further compared the kinematic and kinetic differences between the 4 slip outcomes (fall, nonfall, skate over, and walkover) and hypothesized that there would be specific biomechanical factor(s) that could differentiate fall and nonfall within the LOB class, as well as walkover and skate over within the no-LOB class.
Methods
Subjects
A total of 67 community-dwelling older adults were included in this study (age: 72.2 [5.3] y, height: 166.6 [15.1] cm, mass: 75.6 [12.7] kg, female: 22). All participants were screened via a questionnaire before the training session to exclude participants with self-reported neurological, musculoskeletal, cardiopulmonary, or other systemic disorders. Their history of falls 1-year prior to the test was recorded. All participants provided written informed consent, which was approved by the institutional review board at the University of Illinois at Chicago.
Experimental Setup and Study Design
All subjects received 24 slips provided in a “blocked-and-mixed” manner. This protocol contains around 10 regular walking trials, followed by 2 blocks of 8 repeated slip trials with 3 walking trails in between, and a final block of 15 mixed trials (8 slips and 7 walking trials).25 Slips were introduced by a pair of low-friction, moveable platforms (L: 0.65 × W: 0.30 m) embedded in a 7-m walkway during over-ground walking (Figure 1B). Without warning, the right slider would be released to freely slide in the anterior–posterior direction up to 90 cm, just as a slip does in real life. The participants took 5 to 10 unperturbed walking trials before receiving their novel slip. The instructions were consistent for all trials, with all participants being told “a slip may or may not occur”; hence, the participants would anticipate a slip in each trial, regardless of whether they experienced the slip or not.
The subjects were protected by a harness connected to a load cell (Transcell Technology Inc, Buffalo Grove, IL). The load cell consistently collected force data, which were later used to detect a fall.26 Four force plates (AMTI, Newton, MA) were installed beneath the walkway to record the ground reaction force. Kinematics from a full-body marker set (28 retroreflective markers) were recorded by an 8-camera motion capture system (Motion Analysis Corporation, Santa Rosa, CA). Kinematic data were sampled at 120 Hz and were synchronized with the force plate and load cell data, which were collected at 600 Hz.
A total of 134 slip trials, which combined the novel slip and the last slip from a mixed block, were analyzed. We have included a detailed analysis in Appendix to show that the combination of the novel slip and the last slip, although it slightly violated the independence of slip outcomes, did not affect the study results. For the novel slip, 100% of the participants lost their balance, while for the last slip, 94% of the participants adopted a full recovery, which together, allowed an investigation of all possible slip outcomes (Table 1).
Table 1.
Sample Size for Each Type of Slip Outcome for the First (Trial 1) and Last (Trial 24) Slip Trials
| LOB | no-LOB | |||
|---|---|---|---|---|
| Trial | Fall | Nonfall | Skate over | Walkover |
| Trial 1 | 31 | 36 | 0 | 0 |
| Trial 24 | 0 | 4 | 34 | 29 |
| Total | 31 | 40 | 34 | 29 |
Abbreviations: LOB, loss of balance; no-LOB, no loss of balance.
Definition of Slip Outcomes
Slip outcomes were first broadly classified as LOB or no-LOB. LOB was defined as the recovery limb landing posterior to the sliding heel17; otherwise, the slip outcome would be no-LOB. The LOB was further classified as a fall or nonfall. The trial was considered a fall if the peak load cell force during a slip exceeded 30% of the participant’s body weight, and the video recording was used to verify the result.27 No-LOB was further classified as a skate over, in which the sliding heel traveled >5 cm, or a walkover, in which the displacement of the sliding heel was smaller than 5 cm.17
Definition of Proactive and Reactive Phases
The proactive phase was taken from the slipping foot liftoff (LLO) before SON to SON. The instant of SON was determined to be when the sliding velocity exceeded 0.05 m·s−1, which was around 50 milliseconds after the right foot’s heel contact.15 The proactive phase covers the swing phase during the gait cycle, which contains the early, mid, and terminal swing phases. Hence, the proactive phase was divided, based on the swing phases, into 3 subphases: early proactive, mid proactive, and late proactive phases. Early proactive phase was defined as the duration between the onset of the early swing and the mid swing, mid proactive phase was defined as the duration between the onset of the mid swing and the terminal swing, and late proactive phase was defined as the duration between the onset of the terminal swing and SON. The reactive phase was divided into subphases, as an early reactive phase starting from SON to recovery foot LLO and a late reactive phase starting from LLO to recovery foot touchdown (Figure 2A). However, the latter phase has already been researched in our previous study28; therefore, it was not included in this study.
Figure 2 —
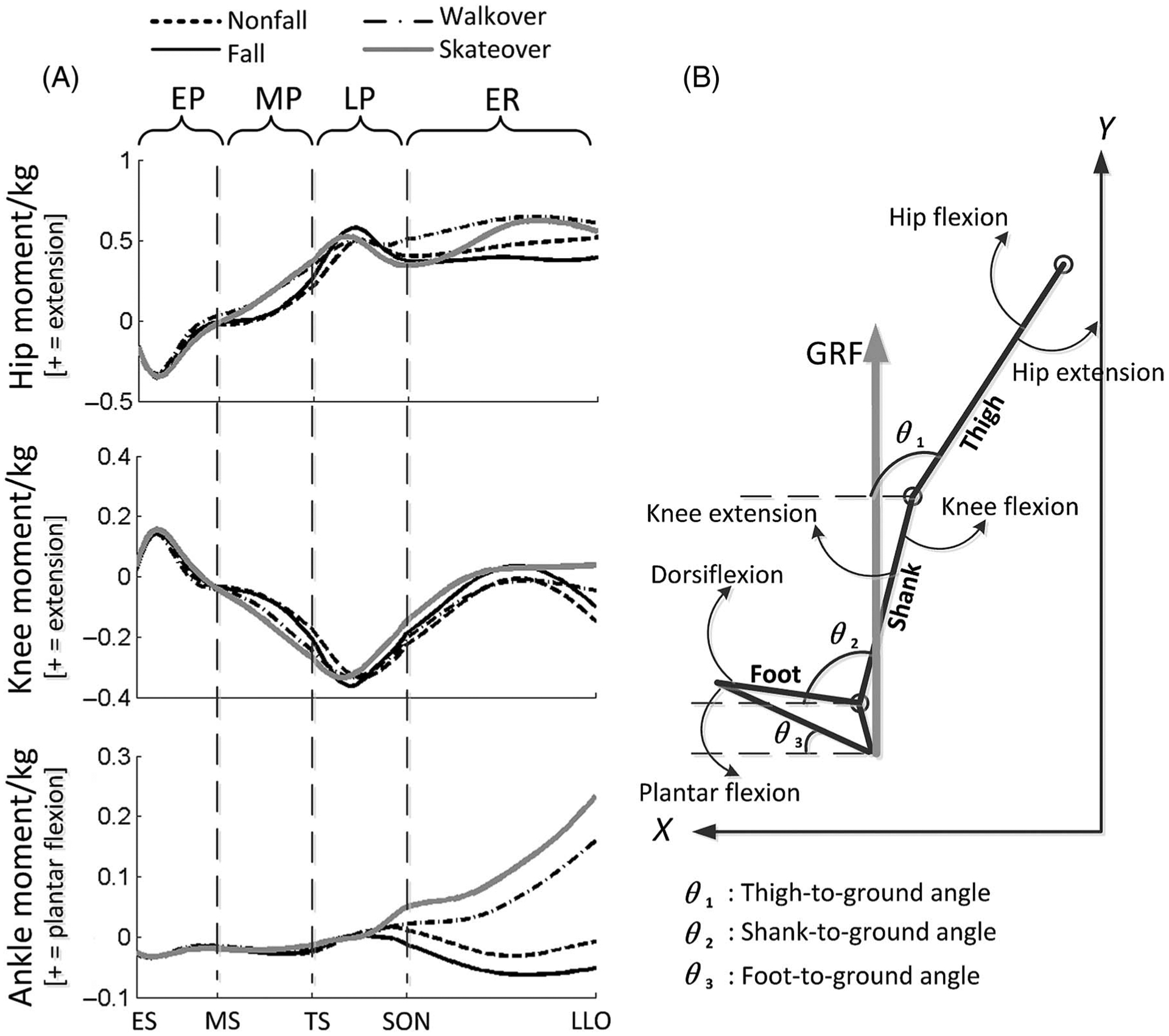
The right panel shows a schematic of the 3-link, sagittal-plane model of the lower limb. θ1, θ2, and θ3 represent the angles of the thigh, shank, and foot relative to the ground. The vertical gray arrow indicates the GRF applied on this limb. The positive x-axis is in the direction of forward progression and the positive y-axis is in upward direction. The left panel shows a typical profile of joint moments (N m·kg−1) in the sagittal plane from the ES instant to recovery foot LLO, with the MS, TS, and SON in between. This period could be divided into the EP, MP, LP, and ER. BOS indicates base of support; COM, center of mass; EP, early proactive phase; ER, early reactive phase; ES, early swing; GRF, ground reaction force; LOB, loss of balance; LLO, liftoff; LP, late proactive phase; MP, mid proactive phase; MS, mid swing; no-LOB, no loss of balance; SON, slip onset; TS, terminal swing.
Outcome Variables
To capture both the kinetic and the resulting kinematic controls that may influence slip outcomes, both joint moments and segment angles of the slipping limb, respectively, were analyzed in this study. While, from previous studies, it is known that recovery step length, which is predominantly affected by joint kinematics,29 can significantly determine slip outcomes,30,31 the underlying joint kinematic contributions to slip outcomes have not been examined. Hence, this study took a further step back by decoupling the step length into segment angles, which were chosen as outcome variables to examine kinematic control in this study. Only the slipping limb was studied, because the slipping limb critically determined slip outcomes before recovery touchdown,11 while the recovery limb mainly contributed in the late reactive phase to improve stability, which was not our focus in this study.15
Segment angles were defined as the angles between a segment and an anterior horizontal line in the sagittal plane (Figure 2B).11 Segment angles were taken at the instant of the completion of each phase. The joint moments were calculated using subject-specific musculoskeletal sagittal-plane models (7-link, 9-degree-of-freedom) in OpenSim32 with the inverse-dynamics formulation. Joint angle, angular velocity, ground reaction force, and center of pressure were inputted in this model. The individual models were scaled according to each subject’s anthropometric measurements.33 Average joint moments of both negative and positive values were calculated as the sum of the joint moments divided by the frames of each phase in each trial. The average moments were compared across different slip outcomes because segment angles in each phase were affected by their corresponding joint moments in that entire phase, instead of the joint moments at a specific instant.
Statistical Analysis
First, Fisher exact test was applied to examine any difference in the history of falls between different slip outcomes.
To test hypothesis 1, independent t tests were applied to examine any differences between LOB and no-LOB in terms of segment angles and average joint moments for each phase. Logistic regressions were then used to identify any segment angle(s) and/or joint moment(s) in each subphase that could differentiate LOB from no-LOB.
To test hypothesis 2, a 1-way analysis of variance was used to detect any differences among 4 slip outcomes (fall, nonfall, skate over, and walkover) in segment angles and average joint moments for each subphase. Four slip outcomes were treated as independent variables, while kinematic and kinetic outcomes were dependent variables. Follow-up comparisons were resolved using independent t tests between 2 groups. Benjamini and Yekutieli34 corrections were applied to reduce type II error (corrected α = .02). Logistic regressions were used to identify key factors in each subphase, resulting in fall, nonfall, walkover, and skate over. All statistical analyses were performed using SPSS (version 22; IBM Corp, Armonk, NY; α = .02 for post hoc tests and α = .05 for other tests).
Results
Out of 71 participants, 24 (33.8%) had a previous fall in the last year, and 11 (15.5%) had more than 1 fall. For the participants with a fall history, 9 of them had demonstrated a fall outcome in the laboratory test during the current study, and the other 15 participants with a fall history demonstrated a nonfall outcome. The Fisher exact test indicated that there is no significant difference in the history of falls between these slip outcomes (P > .05).
Independent t tests indicated that there was no significant difference between LOB and no-LOB in segment angles and average joint moments in the early proactive phase, and there was a significant difference in the studied variables in the mid proactive, late proactive, and early reactive phases (Table 2). At the end of the mid proactive phase, the shank angle was significantly larger (less vertical) for LOB in comparison with no-LOB (P = .01). Both the shank and foot angles were significantly larger (less flat for foot) for LOB than no-LOB at the end of the late proactive phase (P < .001 for both), and all lower limb segment angles at LLO were significantly larger for LOB than no-LOB (Table 2). Correspondingly, the average hip extensor and knee flexor moments in the mid proactive phase, as well as the plantar flexor moment in both the mid and late proactive phases, were all significantly higher for no-LOB than for LOB (P < .05 for all), and the average hip extensor and plantar flexor moments were significantly higher for no-LOB than for LOB (P = .03 and P < .001).
Table 2.
The Mean and SD Values for Final Segment Angles, Average Moments of the Slipping Limb in Each Phase, and Results of Independent t Tests for All Variables in Each Phase Between LOB and no-LOB
| Variables | Phase | Variable | LOB mean (SD) | no-LOB mean (SD) | P value |
|---|---|---|---|---|---|
| Angle, deg | Early proactive | Thigh | 113.4 (4.9) | 113.1 (4.9) | >.05 |
| Shank | 58.5 (4.5) | 59.7 (5.0) | >.05 | ||
| Foot | −28.3 (5.6) | −26.5 (6.7) | >.05 | ||
| Mid proactive | Thigh | 116.3 (4.7) | 116.1 (5.0) | >.05 | |
| Shank | 91.4 (0.9) | 91.0 (1.1) | .01 | ||
| Foot | 1.9 (4.0) | 1.7 (4.4) | >.05 | ||
| Late proactive | Thigh | 112.3 (4.5) | 112.8 (5.2) | >.05 | |
| Shank | 104.5 (5.0) | 97.1 (5.9) | <.001 | ||
| Foot | 8.7 (4.8) | 3.3 (4.3) | <.001 | ||
| Early reactive | Thigh | 107.4 (4.9) | 103.7 (4.9) | <.001 | |
| Shank | 100.0 (6.4) | 88.1 (5.2) | <.001 | ||
| Foot | 4.9 (4.5) | 0.5 (2.6) | <.001 | ||
| Moment, N m·kg−1 | Early proactive | Hip | −0.162 (0.103) | −0.155 (0.109) | >.05 |
| Knee | 0.045 (0.040) | 0.044 (0.051) | >.05 | ||
| Ankle | −0.024 (0.006) | −0.024 (0.007) | >.05 | ||
| Mid proactive | Hip | 0.079 (0.122) | 0.166 (0.131) | <.001 | |
| Knee | −0.092 (0.043) | −0.140 (0.056) | <.001 | ||
| Ankle | −0.024 (0.009) | −0.020 (0.009) | .01 | ||
| Late proactive | Hip | 0.429 (0.204) | 0.469 (0.231) | >.05 | |
| Knee | −0.289 (0.099) | −0.294 (0.102) | >.05 | ||
| Ankle | −0.001 (0.015) | 0.005 (0.021) | .04 | ||
| Early reactive | Hip | 0.434 (0.293) | 0.540 (0.271) | .03 | |
| Knee | −0.063 (0.186) | −0.037 (0.182) | >.05 | ||
| Ankle | −0.038 (0.102) | 0.093 (0.116) | <.001 |
Abbreviations: LOB, loss of balance; no-LOB, no loss of balance.
For LOB prediction, the shank angle at SON had the greatest prediction accuracy out of all variables in the proactive phase, providing a 74.6% accurate classification of outcomes (P < .001). In addition, the average knee moment and the initial shank angle for the mid proactive phase could accurately predict 71.6% of the outcomes (P < .001 and P = .04). The shank angle at LLO alone could accurately predict 85.1% of the outcomes with a threshold of 93° (P < .001). Moreover, the average knee moment in the early reactive phase and the shank angle at SON could accurately predict 77.6% of the outcomes (P ≤ .001 for both; Table 3).
Table 3.
Best Slip Outcome (LOB or Not) Prediction Models Using Logistic Regression for Proactive and Reactive Phases
| Phase | Model factors | P | OR | Sensitivity/specificity, % | Accuracy, % | |
|---|---|---|---|---|---|---|
| Proactive | 1 | Shank angle at SON | <.001 | 0.78 | 78.8/69.8 | 74.6 |
| 2 | Knee moment in MP | <.001 | 0.29 | 76.1/66.7 | 71.6 | |
| Shank angle at MS | .04 | 0.9 | ||||
| Reactive | 3 | Shank angle at LLOa | <.001 | 0.69 | 84.7/85.7 | 85.1 |
| 4b | Knee moment in ER | <.001 | 0.323 | 80.3/74.6 | 77.6 | |
| Shank angle at SON | .001 | 0.67 | ||||
Abbreviations: ER, early reactive phase; LLO, liftoff; LOB, loss of balance; MP, mid proactive phase; MS, mid swing; no-LOB, no loss of balance; OR, odds ratio; SON, slip onset. Note: MS is the initial instant of the mid proactive phase, and SON is the initial instant of the early reactive phase. Sensitivity indicated the predictive accuracy for LOB, and specificity indicated the predictive accuracy for no-LOB. For segment angles, it indicates the probability of having LOB decreases with a decrease of 1°, while for normalized joint moments, it indicates the probability of having LOB decreases with an increase of 1 SD in joint moments.
The threshold for distinguishing LOB and no-LOB is 93°, which was calculated using logistic regression.
The equation for model 4 could be represented as p(LOB) = 1/[1 + exp(39 − 0.39 × shank angle − 6.14 × knee moment)].
The 1-way analysis of variance showed that the shank angle in the mid proactive (F3,130 = 3.5, P < .001; Figure 3B2) and late proactive phases (F3,130 = 21.40, P < .001; Figure 3B3) significantly differed between the 4 slip outcomes. There was a main effect of slip outcome on foot angle in both the early proactive phase (F3,130 = 3.06, P = .03; Figure 3C1) and late proactive phase (F3,130 = 12.70, P < .001; Figure 3C3). In the early reactive phase, there was a main effect of slip outcome on all 3 segment angles (thigh: F3,130 = 5.83, shank: F3,130 = 57.03, and foot: F3,130 = 16.08; P < .001 for all; Figure 3A4, 3B4, and 3C4).
Figure 3 —
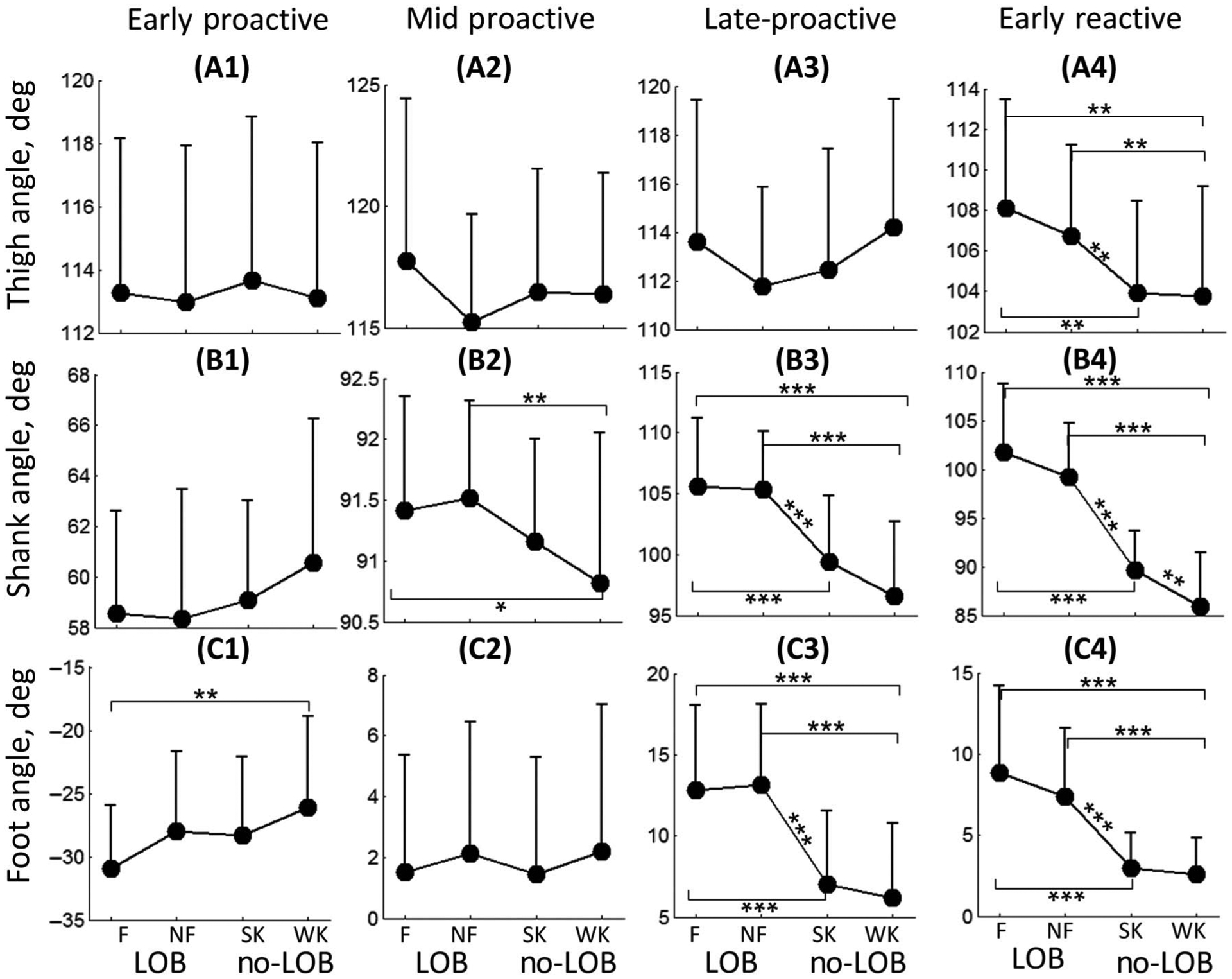
Segment angle comparison at mid proactive, slip onset, and left foot liftoff instants for each slip outcome. The error bar indicates the SD values. F indicates fall; LOB, loss of balance; NF, nonfall; no-LOB, no loss of balance; SK, skate over; WK, walkover. *P < .02. **P < .005. ***P < .001.
For average joint moments, the average hip extensor (F3,130 = 9.03, P < .001), knee flexor (F3,130 = 15.7, P < .001), and plantar flexor moments (F3,130 = 4.1, P = .004) for the mid proactive phase were significantly different between the slip outcomes (Figure 4A2, 4B2, and 4C2). Both the hip extensor (F3,130 = 3.87, P = .02; Figure 4A4) and plantar flexor moments (F3,130 = 14.75, P < .001; Figure 4C4) in the early reactive phase were significantly different between the slip outcomes.
Figure 4 —
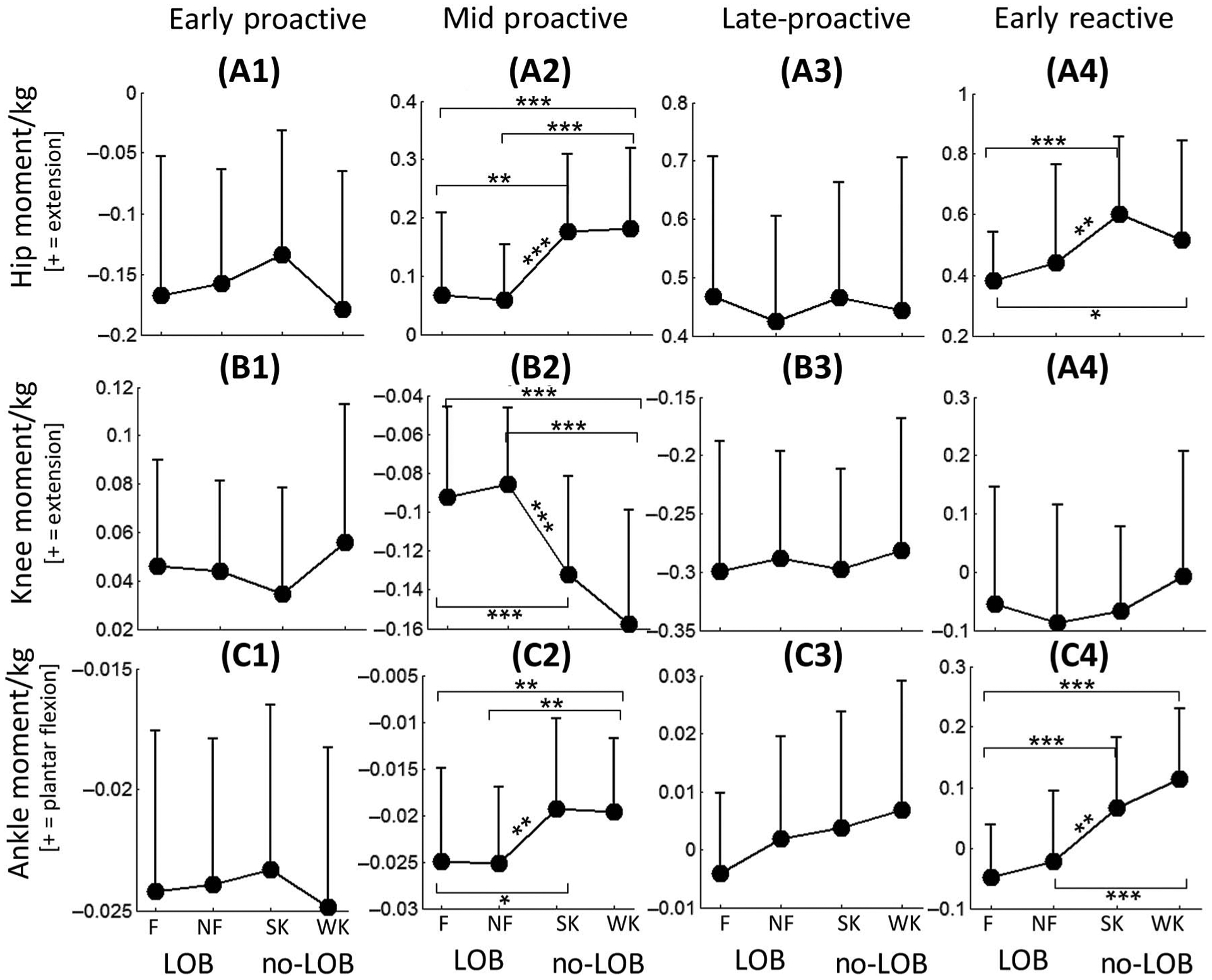
Average joint moment (N m·kg−1) comparison in proactive and reactive phases for each of the slip outcomes. The error bar indicates the SD values. F indicates fall; LOB, loss of balance; NF, nonfall; no-LOB, no loss of balance; SK, skate over; WK, walkover. *P < .02. **P < .005. ***P < .001.
Post hoc analysis further indicated that, between fall and nonfall, there were no significant differences in any of the segment angles and joint moments for all 3 phases (P > .02 for all), while between skate over and walkover, the shank angle at the end of the early reactive phase was significantly larger for skate over than walkover (P < .005). Moreover, between the 2 LOB outcomes (fall and nonfall) and 2 no-LOB outcomes (skate over and walkover), the results were highly consistent with the comparison between LOB and no-LOB, and for these comparisons, the shank angle in the late proactive and early reactive phases and the knee moment in the mid proactive phase showed significant differences (P < .02 for all).
Logistic regression revealed that there was no variable that could significantly differentiate fallers from nonfallers (P > .05; Table 4). However, skate over and walkover could be predicted with moderate accuracy (68.5%) using the shank angle at LLO.
Table 4.
Best Slip Outcome Prediction Models Using Logistic Regression to Distinguish Skate Over and Walkover, As Well As Fall and Nonfall
| Model | Factors | P | OR | Sensitivity/specificity, % | Accuracy, % |
|---|---|---|---|---|---|
| Skate over/walkover | Shank angle at LLO | .006 | 0.84 | 76.5/58.6 | 68.5 |
| Fall/nonfall | Shank angle at LLO | .13 | 0.94 | 82.5/32.3 | 60.6 |
Abbreviations: LLO, liftoff; OR, odds ratio. Note: OR indicates the probability of having skate over or fall decreases with a 1° decrease of shank angle.
Discussion
Our results indicated that the shank segment of the slipping limb plays a key role in preventing LOB in both the proactive and reactive phases. Specifically, a larger shank-to-ground angle increased predisposition to experience LOB. Thus, to prevent LOB, participants need to reduce their shank angle by increasing the knee flexor moment in the proactive and early reactive phases. Furthermore, there were significant differences across 4 slip outcomes, and the shank angle was also a key factor distinguishing walkover from skate over, while no significant difference in any studied variables was found between fall and nonfall.
Our results found that the shank angle of the slipping limb was associated with a forward displacement of BOS following a perturbation and was the most crucial determinant for preventing LOB. In both the proactive and early reactive phases, for a 1° increase in shank flexion, the odds of LOB would reduce to around 0.7 (0.78 for the proactive phase and 0.69 for the reactive phase; Table 3). This is because an external knee extensor moment would be applied on the shank segment due to gravity when the shank angle was >90° (the ankle was anterior to the knee in the sagittal plane; Figure 2). When stepping on a slippery surface, the foot would be propelled forward due to this external moment, which might induce LOB. On the contrary, if the shank angle was <90°, in which the ankle was posterior to the knee, the gravity would add an external knee flexor moment on the shank segment, which would decelerate the forward movement of the slipping foot, enabling no-LOB. This was consistent with our findings that, when the shank angle was >93° at LLO, the slip outcome was most likely an LOB; otherwise, the outcome was no-LOB (85.1% accuracy; Table 3). Besides the effect on ground reaction force, a larger shank flexion could also lead to a shorter step length. It has been reported that a shorter step length and a flexed knee angle could lower the risk of slip-induced falls for healthy older adults,23,30,35,36 which is consistent with our current finding.
An increased knee flexor moment in the mid proactive phase could lead to a decrease of the shank angle at SON according to forward dynamics,37 and hence, reduce the forward displacement of BOS, representing an effective adjustment for preventing LOB. The logistic regression model revealed that the decrease in the initial shank angle and the increment of the knee flexor moment in the mid proactive phase could reduce the likelihood of LOB (Table 3). Specifically, a 1° decrease in the initial shank angle in the mid proactive phase would reduce the odds of LOB to 0.9, while 1 SD increase in the knee flexor moment would reduce the odds to 0.29. However, the knee moment did not differ between no-LOB and LOB in the late proactive phase. This may be due to the occurrence of substantial shank adjustments in the shank-to-ground angle during the mid proactive phase, necessitating smaller adjustments in the late proactive phase. In addition, extensive increases in knee flexor moments in the swing phase could lead to a reduction in step length and gait speed.38 It can thus be postulated that, to prevent LOB without compromising the self-selected gait speed, the central nervous system may increase the hip extensor and knee flexor moments for the mid proactive phase but not for the late proactive phase.
None of the variables for fall or nonfall differed significantly in the proactive and early reactive phases (Figures 3 and 4). However, changes during the late reactive phase, in the form of a recovery step, have been established to successfully rebuild the relationship between COM and BOS to avoid a fall, especially when a slip perturbation results in a large displacement of BOS.15,39 Therefore, it is reasonable to postulate that whether LOB would result in a fall or not is determined predominantly in the late reactive phase, which was consistent with our previous study on the role of recovery foot stepping.28
However, proactive and early reactive controls were seen to contribute to preventing LOB. Slip classifications were predicted with 74.6% accuracy using the shank angle from the proactive phase, while classifications were predicted with 84.1% accuracy using only the shank angle from the early reactive phase (Table 3). Similarly, the shank angle in the proactive phase had a higher sensitivity (78.8% for LOB prediction) but lower specificity (69.8% for no-LOB prediction), which indicated that a larger shank angle at SON was likely to induce LOB, but a smaller shank angle could not guarantee no-LOB. This is because individuals also need to keep maintaining their shank angle, after SON, at near 90° in the early reactive phase to prevent LOB; otherwise, LOB could still occur, even though they performed well (smaller shank angle at SON) in the proactive phase. The equation for model 4—p(LOB) = 1/[1 + exp(39 − 0.39 × shank angle − 6.14 × knee moment)] (Table 3)—further supported this viewpoint that LOB or no-LOB was determined by both proactive adjustments (shank angle at SON) and reactive responses (knee moment in early reactive phase). A division line distinguishing LOB from no-LOB could be derived based on the beta coefficients (b = 0.39 for shank angle and b = 6.14 for knee moment) from the equation. As long as the sum of 0.39 × shank angle and 6.14 × knee moment is smaller than 39, a no-LOB will be likely (>50%) to occur, based on the aforementioned equation (Figure 5). In addition, the equation could reveal that, if sufficient proactive adjustments (smaller shank angle) were made, then less knee flexor moment (negative value) would be required in the following early reactive phase for LOB prevention. This finding was consistent with a previous proposal, that sufficient proactive adjustments could minimize dependence on reactive responses.17
Figure 5 —

Using logistic regression, all trials could be categorized into LOB and no-LOB based on the shank angle (in degrees) at SON and the following knee joint moment (N m·kg−1) in the ER, with an accuracy of 77.6% (model 4 in Table 3). The division line distinguishing LOB from no-LOB was derived based on the beta coefficients in the logistic regression model. The region below this division line was defined as the no-LOB region. ER indicates early reactive phase; LOB, loss of balance; no-LOB, no loss of balance; SON, slip onset.
Although only the shank angle at LLO was significantly different between skate over and walkover, the shank angle at SON was slightly larger for skate over (P = .06; Figure 3). This suggests that, for skate over, there is a slightly larger propelling force on the slipping foot due to gravity, leading to a longer forward slipping distance. In addition, there was a slightly larger knee flexor moment in the mid proactive phase for walkover than for skate over (P = .07; Figure 4). Such a large knee flexor moment would pull the foot posteriorly, resulting in a decreased initial slip velocity and a shorter forward slip distance.16
To achieve walkover, increased demand was placed on specific joint moments in the proactive and early reactive phases. With an insufficient knee flexor moment in the mid proactive phase, the slip intensity increased, leading to skate over. While both fall and nonfall can be attributed to insufficient adjustments in joint moments (ie, smaller plantar flexor, knee flexor, and hip extensor moment) during the mid proactive and early reactive phases, the difference between them may mostly have been that those with nonfall took a successful recovery step, while those with fall failed to do so in the late reactive phase.
The present study has several limitations. First, the current study only analyzed the characteristics of the slipping limb. Although previous studies found COM stability improvement was mostly due to the reactive actions of the slipping limb,11 the recovery limb’s actions could also affect slip outcomes. Second, the slipping side in this study was always the right side; thus, it is unclear whether the adaptation effects would be different (less robust and/or slower) if the perturbations were randomly applied to both limbs. However, previous studies have shown that adaptations to bilateral perturbations delivered in a random order could be achieved as rapidly as within 3 trials on each side, and the most improvement occurred after experiencing the first perturbation, regardless of the perturbation side.40 These results of fast adaption on either side indicated that providing the bilateral versus unilateral training (as currently used in the study) might not affect the results of improvements in kinematic and kinetic outcomes. Nonetheless, future studies incorporating bilateral training need to verify such postulation. Third, this study did not examine differences in neuromuscular activity across the different slip recovery strategies. Differences in neuromuscular activity among these strategies could provide further insight into fall prevention mechanisms and could be incorporated in future works. Finally, although our original assumption was based on taking slip outcomes as independent variables, 2 trials were analyzed for each participant due to the study design. Hence, pairwise comparisons for repeated trials were conducted to verify our results, and the results from the paired t tests were consistent with the current one (more details are shown in Appendix).
In summary, it was determined that a vertical shank angle and larger knee flexor moment of the slipping limb in both the proactive phase and reactive phase play key roles in preventing LOB and resulting in recovery outcomes of walkover or skate over. Although not every backward balance loss will result in a fall, reactively recovering from such a scenario by taking a rapid recovery step with the trailing limb while actively trying to reduce the slip intensity under the forwardly displacing slipping limb might increase the risk of musculoskeletal injuries, such as muscle sprains or strains, specifically in older adults. It is postulated that sufficient proactive adjustments can minimize a reliance on reactive responses; however, it remains to be definitively verified in future studies. These findings can provide a practical guide for clinicians and therapists on fall interventions in older adults with different physical conditions. For example, for older adults with a weakness in their hamstrings or an impaired activation in the hamstrings seen poststroke, reeducation of gait pattern with the shank in a more vertical position in a hazardous environment (ie, wet floor) is more effective than strengthening the hamstrings to reduce the risk of slip-induced falls in such a population.
Supplementary Material
Acknowledgments
This work was supported by the National Institutes of Health (NIH R01 AG050672-02 to T.B. and NIH R01-AG044364 to T.B. and Y.-C.P.). The authors would like to thank Ms Alison Schenone and Ms Shamali Dusane for their helpful edits. The authors have no conflicts of interest to disclose.
References
- 1.Englander F, Hodson TJ, Terregrossa RA. Economic dimensions of slip and fall injuries. J Forensic Sci. 1996;41(5):733–746. doi: 10.1520/JFS13991J [DOI] [PubMed] [Google Scholar]
- 2.Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Injury Prev. 2005; 11(2):115–119. doi: 10.1136/ip.2004.005835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holbrook TL, Grazier KL. The Frequency of Occurrence, Impact, and Cost of Selected Musculoskeletal Conditions in the United States. Chicago, IL: Amer Academy of Orthopaedic; 1984. [Google Scholar]
- 4.Tuunainen E, Rasku J, Jantti P, Pyykko I. Risk factors of falls in community dwelling active elderly. Auris Nasus Larynx. 2014;41(1):10–16. doi: 10.1016/j.anl.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 5.United States Department of Labor. Lost-Work-Time Injuries and Illnesses: Characteristics and Resulting Days Away From Work, 2001. Washington, DC: Bureau of Labor Statistics; 2003. [Google Scholar]
- 6.Redfern MS, Cham R, Gielo-Perczak K, et al. Biomechanics of slips. Ergonomics. 2001;44(13):1138–1166. doi: 10.1080/00140130110085547 [DOI] [PubMed] [Google Scholar]
- 7.Lam T, Anderschitz M, Dietz V. Contribution of feedback and feedforward strategies to locomotor adaptations. J Neurophysiol. 2006;95(2):766–773. doi: 10.1152/jn.00473.2005 [DOI] [PubMed] [Google Scholar]
- 8.Hay L, Redon C. Feedforward versus feedback control in children and adults subjected to a postural disturbance. Exp Brain Res. 1999; 125(2):153–162. doi: 10.1007/s002210050670 [DOI] [PubMed] [Google Scholar]
- 9.Tang PF, Woollacott MH, Chong RK. Control of reactive balance adjustments in perturbed human walking: roles of proximal and distal postural muscle activity. Exp Brain Res. 1998;119(2):141–152. doi: 10.1007/s002210050327 [DOI] [PubMed] [Google Scholar]
- 10.Pavol MJ, Runtz EF, Pai YC. Young and older adults exhibit proactive and reactive adaptations to repeated slip exposure. J Gerontol A Biol Sci Med Sci. 2004;59(5):494–502. doi: 10.1093/gerona/59.5.M494 [DOI] [PubMed] [Google Scholar]
- 11.Yang F, Pai YC. Role of individual lower limb joints in reactive stability control following a novel slip in gait. J Biomech. 2010; 43(3):397–404. doi: 10.1016/j.jbiomech.2009.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pavol MJ, Runtz EF, Edwards BJ, Pai YC. Age influences the outcome of a slipping perturbation during initial but not repeated exposures. J Gerontol A Biol Sci Med Sci. 2002;57(8):M496–M503. doi: 10.1093/gerona/57.8.M496 [DOI] [PubMed] [Google Scholar]
- 13.Pai YC. Movement termination and stability in standing. Exerc Sport Sci Rev. 2003;31(1):19–25. doi: 10.1097/00003677-200301000-00005 [DOI] [PubMed] [Google Scholar]
- 14.Mak MK, Yang F, Pai YC. Limb collapse, rather than instability, causes failure in sit-to-stand performance among patients with Parkinson disease. Phys Ther. 2011;91(3):381–391. doi: 10.2522/ptj.20100232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang F, Bhatt T, Pai YC. Role of stability and limb support in recovery against a fall following a novel slip induced in different daily activities. J Biomech. 2009;42(12):1903–1908. doi: 10.1016/j.jbiomech.2009.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cham R, Redfern MS. Lower extremity corrective reactions to slip events. J Biomech. 2001;34(11):1439–1445. doi: 10.1016/S0021-9290(01)00116-6 [DOI] [PubMed] [Google Scholar]
- 17.Bhatt T, Wening JD, Pai YC. Adaptive control of gait stability in reducing slip-related backward loss of balance. Exp Brain Res. 2006;170(1):61–73. doi: 10.1007/s00221-005-0189-5 [DOI] [PubMed] [Google Scholar]
- 18.Morris ME, Huxham F, McGinley J, Dodd K, Iansek R. The biomechanics and motor control of gait in Parkinson disease. Clin Biomech. 2001;16(6):459–470. doi: 10.1016/S0268-0033(01)00035-3 [DOI] [PubMed] [Google Scholar]
- 19.Mcilroy WE, Maki BE. Changes in early automatic postural responses associated with the prior-planning and execution of a compensatory step. Brain Res. 1993;631(2):203–211. doi: 10.1016/0006-8993(93)91536-2 [DOI] [PubMed] [Google Scholar]
- 20.Reynolds RF, Bronstein AM. The broken escalator phenomenon—aftereffect of walking onto a moving platform. Exp Brain Res. 2003;151(3):301–308. doi: 10.1007/s00221-003-1444-2 [DOI] [PubMed] [Google Scholar]
- 21.Bhatt T, Pai YC. Role of cognition and priming in interlimb generalization of adaptive control of gait stability. J Motor Behav. 2009; 41(6):479–493. doi: 10.3200/35-08-021 [DOI] [PubMed] [Google Scholar]
- 22.Siegmund GP, Heiden TL, Sanderson DJ, Inglis JT, Brault JR. The effect of subject awareness and prior slip experience on tribometer-based predictions of slip probability. Gait Posture. 2006;24(1):110–119. doi: 10.1016/j.gaitpost.2005.08.005 [DOI] [PubMed] [Google Scholar]
- 23.Allin LJ, Nussbaum MA, Madigan ML. Feet kinematics upon slipping discriminate between recoveries and three types of slip-induced falls. Ergonomics. 2018;61(6):866–876. doi: 10.1080/00140139.2017.1413212 [DOI] [PubMed] [Google Scholar]
- 24.Wang S, Liu X, Lee A, Pai YC. Can recovery foot placement affect older adults’ slip-fall severity? Ann Biomed Eng. 2017; 45(8):1941–1948. doi: 10.1007/s10439-017-1834-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhatt T, Yang F, Pai YC. Learning to resist gait-slip falls: long-term retention in community-dwelling older adults. Arch Phys Med Rehab. 2012;93(4):557–564. doi: 10.1016/j.apmr.2011.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pai YC, Yang F, Bhatt T, Wang E. Learning from laboratory-induced falling: long-term motor retention among older adults. Age. 2014; 36(3):1367–1376. doi: 10.1007/s11357-014-9640-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang F, Pai YC. Automatic recognition of falls in gait-slip training: harness load cell based criteria. J Biomech. 2011;44(12):2243–2249. doi: 10.1016/j.jbiomech.2011.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang S, Bhatt T, Liu X, Pai YC. The role of recovery lower limb segments in post-slip determination of falls due to instability or limb collapse. Ann Biomed Eng. 2020;48(1):192–202. doi: 10.1007/s10439-019-02327-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Begg RK, Sparrow WA. Ageing effects on knee and ankle joint angles at key events and phases of the gait cycle. J Med Eng Technol. 2006;30(6):382–389. doi: 10.1080/03091900500445353 [DOI] [PubMed] [Google Scholar]
- 30.Espy DD, Yang F, Bhatt T, Pai YC. Independent influence of gait speed and step length on stability and fall risk. Gait Posture. 2010;32(3):378–382. doi: 10.1016/j.gaitpost.2010.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lockhart TE, Woldstad JC, Smith JL. Effects of age-related gait changes on the biomechanics of slips and falls. Ergonomics. 2003;46(12):1136–1160. doi: 10.1080/0014013031000139491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Delp SL, Anderson FC, Arnold AS, et al. OpenSim: open-source software to create and analyze dynamic Simulations of movement. IEEE Trans Biomed Eng. 2007;54(11):1940–1950. doi: 10.1109/TBME.2007.901024 [DOI] [PubMed] [Google Scholar]
- 33.Gaffney BM, Harris MD, Davidson BS, Stevens-Lapsley JE, Christiansen CL, Shelburne KB. Multi-Joint compensatory effects of unilateral total knee arthroplasty during high-demand tasks. Ann Biomed Eng. 2016;44(8):2529–2541. doi: 10.1007/s10439-015-1524-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Stat. 2001;29(4):1165–1188. doi: 10.1214/aos/1013699998 [DOI] [Google Scholar]
- 35.Yang F, Su X, Wen PS, Lazarus J. Adaptation to repeated gait-slip perturbations among individuals with multiple sclerosis. Mult Scler Relat Disord. 2019;35:135–141. doi: 10.1016/j.msard.2019.07.019 [DOI] [PubMed] [Google Scholar]
- 36.Allin LJ, Nussbaum MA, Madigan ML. Two novel slip training methods improve the likelihood of recovering balance after a laboratory-induced slip. J Appl Biomech. 2018;35(1):1–31. [DOI] [PubMed] [Google Scholar]
- 37.Winter DA. Biomechanics and Motor Control of Human Movement. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]
- 38.Kerrigan DC, Lee LW, Collins JJ, Riley PO, Lipsitz LA. Reduced hip extension during walking: healthy elderly and fallers versus young adults. Arch Phys Med Rehabil. 2001;82(1):26–30. doi: 10.1053/apmr.2001.18584 [DOI] [PubMed] [Google Scholar]
- 39.Bhatt T, Wening JD, Pai YC. Influence of gait speed on stability: recovery from anterior slips and compensatory stepping. Gait Posture. 2005;21(2):146–156. doi: 10.1016/j.gaitpost.2004.01.008 [DOI] [PubMed] [Google Scholar]
- 40.van Hedel HJ, Biedermann A, Erni T, Dietz V. Obstacle avoidance during human walking: transfer of motor skill from one leg to the other. J Physiol. 2002;543(2):709–717. doi: 10.1113/jphysiol.2002.018473 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


