During the COVID-19 lockdown period, care of non-communicable diseases was limited due to difficulties in accessing services, population concerns about infectious risk in healthcare facilities, and relocation of healthcare resources to assist patients with COVID-19.1 Few studies so far have focused on the effect of the lockdown on medication prescriptions to treat non-COVID-19 conditions.
Direct oral anticoagulants (DOACs) are commonly used medications for stroke prevention in non-valvular atrial fibrillation (NVAF) and for the treatment and prevention of venous thromboembolism (VTE). We hypothesized that access to care for patients with these conditions might have been limited during the lockdown, leading to a reduction in new prescriptions of DOACs. Therefore, the aim of this retrospective, cross-sectional study was to assess new prescriptions of DOACs during the lockdown period (March–May 2020) and in the post-lockdown period (June–July 2020) and compare them with what is expected based on time series forecasts.
The Italian Medicines Agency (AIFA) monitors prescriptions of DOACs through a web-based monitoring registry.2 Prescription of DOACs in hospitalized patients are not monitored with this registry. New prescriptions observed from June 2013 to July 2020 were measured by analysing data from the registry. Estimates of new prescriptions during March–July 2020 were calculated based on time series forecasts, computed using seasonal Arima models estimated on historical data from June 2013 to February 2020 on monthly aggregated data. All statistical analyses were performed using R version 3.6.1 and figures were obtained using ggplot2.3 Time series analysis was performed using the Arima function of R base library and the forecast package for predictions.4
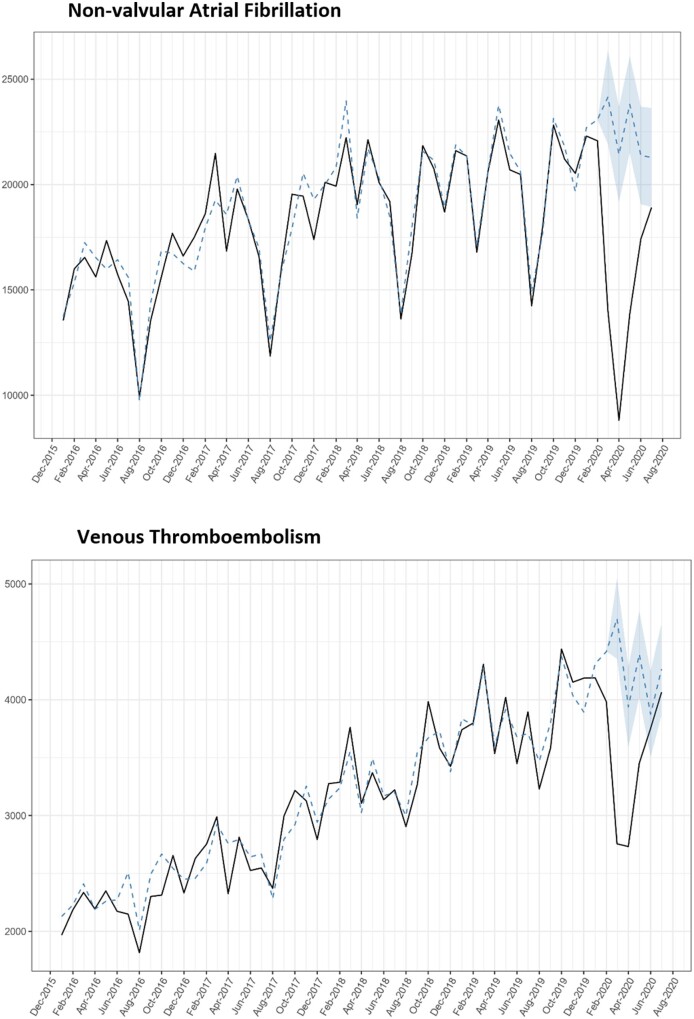
From June 2013 to July 2020, the registry collected data on 1 515 629 new DOACs prescriptions, including 1 312 214 (86.6%) new prescriptions for NVAF and 203 415 (13.4%) for VTE. Figure 1 presents observed and estimated numbers of new prescriptions of DOACs for NVAF and VTE from 2016 up to July 2020. New DOACs prescriptions progressively increased over time, with seasonal variations due to periodical reduction in the summer period. In the lockdown period, between March and May 2020, the number of new prescriptions declined substantially. After the lockdown period, in June and July 2020, this number increased for both conditions.
Figure 1.
Temporal trend in new prescriptions of non-vitamin K oral anticoagulants for treatment of non-valvular atrial fibrillation (upper panel) and venous thromboembolism (lower panel) from 2016 up to July 2020. Observed values are represented as a black coloured continuous line, while estimates are represented as a dashed light-blue line. Confidence intervals for March–July estimates are represented as a light-blue area.
The upper panel of Table 1 presents estimates based on time series forecasts and observed number of new DOACs prescriptions for NVAF by age group in the period between March and July 2020. Overall, the number of new prescriptions largely declined during the lockdown period as compared with what was forecasted (−34.8%), reaching a negative peak in April (−58.9%). In the post-lockdown period there was a less consistent decline in the number of new prescriptions (June −18.6% and July −11.2%). Large differences were observed across age groups, with the largest reduction in number of prescriptions in the March–July period observed in the population aged 65–74 years (−35.2%) and 75 years or older (−36.3%). The lower panel of Table 1 presents the estimated and observed number of new DOACs prescriptions for VTE by age group in the period between March and July 2020. A substantial decrease was observed in the number of new prescriptions as compared with what was forecasted (-20.8%), with a negative peak in March (−41.4%). Persons aged 75 years or older had the largest decrease in new prescriptions (−30.0%). The population aged <65 years had the lowest decrease (−9.0%) and the number of observed new prescriptions in this age group in the post-lockdown period (June and July) was very closed to the forecasted numbers.
Table 1.
Monthly estimated and observed new prescriptions of non-vitamin K oral anticoagulants for treatment of non-valvular atrial fibrillation and venous thromboembolism by age group
| Treatment of non-valvular atrial fibrillation |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall |
<65 years |
65–74 years |
75 years or older |
|||||||||
| Month | Estimated | Observed | Δ (95%CI) | Estimated | Observed | Δ | Estimated | Observed | Δ | Estimated | Observed | Δ |
| March | 24 151 | 14 024 | −41.9% | 2339 | 1531 | −34.5% | 5783 | 3368 | −41.8% | 16 085 | 9125 | −43.3% |
| April | 21 427 | 8811 | −58.9% | 1894 | 1052 | −44.5% | 5100 | 2147 | −57.9% | 14 417 | 5612 | −61.1% |
| May | 23 807 | 13 852 | −41.8% | 2073 | 1454 | −29.9% | 5586 | 3314 | −40.7% | 16 172 | 9084 | −43.8% |
| June | 21 382 | 17 414 | −18.6% | 1878 | 1787 | −4.8% | 5032 | 3994 | −20.6% | 14 514 | 11 633 | −19.9% |
| July | 21 288 | 18 914 | −11.2% | 1921 | 1918 | −0.2% | 5039 | 4363 | −13.4% | 14 331 | 12 633 | −11.8% |
| March–July | 112 055 | 73 015 | −34.8% | 10 105 | 7742 | −23.4% | 26 540 | 17 186 | −35.2% | 75 519 | 48 087 | −36.3% |
|
Treatment of venous thromboembolism
|
||||||||||||
|
Overall
|
<65 years
|
65–74 years
|
75 years or older
|
|||||||||
| Month | Estimated | Observed | Δ | Estimated | Observed | Δ | Estimated | Observed | Δ | Estimated | Observed | Δ |
| March | 4701 | 2756 | −41.4% | 1461 | 969 | −33.7% | 1124 | 676 | −39.9% | 2134 | 1111 | −47.9% |
| April | 3938 | 2732 | −30.6% | 1234 | 1163 | −5.8% | 964 | 684 | −29.1% | 1764 | 885 | −49.8% |
| May | 4394 | 3453 | −21.4% | 1426 | 1314 | −7.9% | 1062 | 791 | −25.5% | 1914 | 1348 | −29.6% |
| June | 3875 | 3753 | −3.1% | 1290 | 1298 | +0.6% | 938 | 920 | −1.9% | 1681 | 1535 | −8.7% |
| July | 4265 | 4065 | −4.7% | 1426 | 1479 | +3.7% | 1008 | 926 | −8.1% | 1843 | 1660 | −9.9% |
| March–July | 21 172 | 16 759 | −20.8% | 6838 | 6223 | −9.0% | 5096 | 3997 | −21.6% | 9336 | 6539 | −30.0% |
Rows identifying months characterized by the lockdown period are in grey.
The decline in use of DOACs shown by this study can be explained by different factors. First, the diagnosis of conditions requiring the use of DOACs might have declined during the COVID-19 lockdown period.5 Second, patients may have experienced difficulties in accessing healthcare services during the lockdown period or may have avoided contact with healthcare services due to increased risk and fear of contracting COVID-19.6 In addition, in the lockdown period healthcare resources were relocated to assist patients with COVID-19 and appointments or visits for conditions different from COVID-19 were often postponed.1
Older adults experienced a larger decline in use of DOACs as compared with younger adults. The presence of physical, psychological, and social problems in older adults and possible concerns about the severe consequences of COVID-19 may have increased difficulties in accessing healthcare services during the lockdown period.6,7
Study limitations relate to the fact that the registry only collects data on DOACs but information on other anticoagulants (i.e. warfarin) is not collected. Data from AIFA show that prescription of warfarin was not modified in March-April 2020 as compared with January–February 2020, suggesting that reduction in new DOACs prescription was not compensated by an increment in use of other anticoagulants.8 Data on prescriptions in hospitalized patients are not covered by the registry. Indeed, in patients with atrial fibrillation, hospitalization is associated with an increase in DOACs initiation, but hospitalizations due to this condition declined in the lockdown period as compared with 2019.9 In addition, new prescriptions of DOACs in hospitalized patients are tracked in the registry when the patient is discharged to the community. For these reasons, it is unlikely that the lack of data on inhospital prescriptions might have influenced our findings. Furthermore, an increase of VTE and cardiovascular events has been shown in COVID-19 hospitalized patients and this may have led to an overestimation of DOACs prescriptions for this specific condition during the lockdown period.10 In addition, occurrence of embolic events related to under-prescription of DOACs was not examined in this study. Finally, from July 2020, compilation of the web-based monitoring registry was no longer mandatory. Thus, the present analysis cannot be extended to the second half of 2020.
In conclusion, this study suggests that the COVID-19 epidemic might have caused relevant indirect health consequences due to the undertreatment of potentially life-threatening conditions, including NVAF and VTE. DOACs under-prescription seems more pronounced in older adults probably due to increased difficulties in accessing healthcare services during the lockdown period.
Acknowledgements
The views expressed in this work are personal and may not be understood or quoted as being made on behalf of or reflecting the position of the Italian Medicines Agency or of one of their committees or working parties. Present composition of the AIFA’s Monitoring Registries Group (in chronological order): Giorgia Bartoccioni, Daniele Ricagni, Susanna Valentini, Antonietta Colatrella, Valeria Angelini, Paola D'Antrassi, Laura Veo, Annalisa Guarcello, Luca Tomassini. Although the AIFA monitoring registries operate within a regulatory framework that provides for the mandatory collection of data from real clinical practice on specific treatments reimbursed by the Italian National Healthcare System (NHS), by all public health facilities, the authors are, however, grateful for the contribution of all the physicians and pharmacists who filled the DOACs registries.
Funding: G.A. has received personal fees as a consultant from Bayer AG and Boehringer Ingelheim, unrelated to this specific work.
Conflict of interest: none declared.
Data availability statement: The data underlying this article will be shared on reasonable request to the corresponding author.
Contributor Information
Graziano Onder, Department of Cardiovascular, Endocrine-metabolic Diseases and Aging, Istituto Superiore di Sanità, Rome, Italy.
Pier Paolo Olimpieri, Italian Medicines Agency, Rome, Italy.
Simone Celant, Italian Medicines Agency, Rome, Italy.
Andrea Di Lenarda, Cardiovascular Center, University Hospital and Health Services of Trieste, Trieste, Italy.
Giuseppe Ambrosio, Division of Cardiology and CERICLET-Centro Ricerca Clinica e Traslazionale, University of Perugia School of Medicine, Perugia, Italy.
Gianpaolo Reboldi, Department of Medicine and Surgery, University of Perugia, Perugia, Italy.
Gianfranco Gensini, Scientific Direction, IRCCS MultiMedica, Milan, Italy.
Antonietta Colatrella, Italian Medicines Agency, Rome, Italy.
Katie Palmer, Department of Geriatrics, Fondazione Policlinico A. Gemelli IRCCS, Rome, Italy.
Domenico Gabrielli, Division of Cardiology, Cardiovascular Department, San Camillo Hospital Rome, Italy.
Pierluigi Russo, Italian Medicines Agency, Rome, Italy.
References
- 1. Monsuez JJ. Cardiology practice in the COVID-19 era. Eur J Prev Cardiol 2020;27:1133–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Olimpieri PP, Di Lenarda A, Mammarella F, Gozzo L, Cirilli A, Cuomo M, Gulizia MM, Colivicchi F, Murri G, Gabrielli D, Trotta F.. Non-vitamin K antagonist oral anticoagulation agents in patients with atrial fibrillation: Insights from Italian monitoring registries. Int J Cardiol Heart Vasc 2020;26:100465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer-Verlag, 2016. ISBN 978-3-319-24277-4. [Google Scholar]
- 4. Hyndman R, Athanasopoulos G, Bergmeir C, Caceres G, Chhay L, O'Hara-Wild M, Petropoulos F, Razbash S, Wang E, Yasmeen F. forecast: Forecasting functions for time series and linear models. R package version 8.13, 2020.
- 5. Holt A, Gislason GH, Schou M, Zareini B, Biering-Sørensen T, Phelps M, Kragholm K, Andersson C, Fosbøl EL, Hansen ML, Gerds TA, Køber L, Torp-Pedersen C, Lamberts M.. New-onset atrial fibrillation: incidence, characteristics, and related events following a national COVID-19 lockdown of 5.6 million people. Eur Heart J 2020;41:3072–3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G.. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020;4:e10–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mantica G, Riccardi N, Terrone C, Gratarola A.. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health 2020;183:40–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. The Medicines Utilisation Monitoring Centre. Report on Medicines use during COVID‐19 epidemic Year 2020. Rome: Italian Medicines Agency, 2020. [Google Scholar]
- 9. D'Ascenzi F, Cameli M, Forni S, Gemmi F, Szasz C, Fabrizio VD, Mechi MT, Nocci M, Mondillo S, Valente S.. Reduction of emergency calls and hospitalizations for cardiac causes: effects of Covid-19 pandemic and lockdown in Tuscany Region. Front Cardiovasc Med 2021;8:625569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Agarwal MA, Ziaeian B, Lavie CJ, Fonarow GC.. Cardiovascular disease in hospitalized patients with a diagnosis of coronavirus from the pre-COVID-19 era in United States: National Analysis From 2016-2017. Mayo Clin Proc 2020;95:2674–2683. [DOI] [PMC free article] [PubMed] [Google Scholar]