The World Health Organization (WHO) reports that rehabilitation services are consistently amongst the health services most severely disrupted by the Coronavirus disease 2019 (COVID-19) crisis for all patients in need. It is suggested that lack of access to rehabilitation can compromise health outcomes, extend inpatient stays, and result in preventable hospital admissions due to health complications.1 The pandemic has increased the rehabilitation needs for the infected patients who are critically unwell with the disease, but also for non COVID-19 patient groups such as patients with cardiac disease requiring cardiovascular rehabilitation (CR).
However, although the pandemic has posed significant challenges to inpatient and outpatient CR that need to be addressed, it poses an opportunity to transform CR service delivery and accessibility. During the present ‘acute COVID-19 phase’, the impact on inpatient CR is associated with a transfer of healthcare staff from CR interventions to support COVID-19 patients. Furthermore, while a paradoxical reduction of hospitalization rates for patients with cardiovascular disease at high risk has been reported (possibly caused by patient reluctance to visit hospitals), unpublished observations from our group seem to agree with other reports suggesting that admissions of patients with cardiovascular disease are more complicated.2 Thus, patients who are finally hospitalized, especially the elderly and patients with co-morbidities, appear to be weaker and less functional compared to the pre pandemic era. Consequently, these patients need to stay longer in the hospital in order to improve both their overall health status and physical condition which is especially critical in the context of hospital bed shortages, increasing the requirements for inpatient CR. Furthermore, because of the pandemic restrictions, almost similarly to patients infected by COVID-19, these patients lack their family support and reassurance during the time-effort demanding process of rehabilitation. Patients are also scared of the infection risk while occasionally they express their agony of being neglected because they think that priority may be given to patients infected by the coronavirus. Thus, particular attention should be payed to patients’ individual status and feelings of stress, anxiety (worry, fear) or depression (low mood, sadness) that they may now deeply experience. Inpatient CR should focus on exercise education, self-management, behaviour modification, activity of daily living and psychosocial support, aiming for an early discharge and in reducing readmissions.
At the same time, outpatient CR is also challenged. Although exercise-based CR has been granted the highest class of recommendation and level of evidence (IA),3 improving exercise capacity and quality of life, but also hospitalizations and morbidity, most of the outpatient CR programs have ceased. Pandemic related constraints such as physical distancing, limited human resources, limited public transport, and infection risks suggest that tele-rehabilitation is now most likely to be required following discharge. Tele-rehabilitation is a cost-effective promising intervention improving exercise capacity and quality of life in patients with cardiovascular disease.4 However, this service has not been developed satisfactorily both in Europe and worldwide due to several reasons. For example, smartphones, internet capabilities and computers are not available for some individuals due to financial constraints and digital inequality.5 In addition, more studies are needed on the elderly population, on its long-term effects, on patients’ psychological profile, as well as, on morbidity and mortality. Nevertheless, in the era of COVID-19, it is of primary importance to ensure continuation of care and facilitate easy contact using structured tele-rehabilitation programmes when available, telephone calls, video use, e-mails, and postal services, between patients and rehabilitation professionals in order to provide individualized advice and remote exercise training when safe and appropriate to do so.1
COVID-19 is also expected to challenge rehabilitation services during a ‘post acute COVID-19 phase’. Many COVID-19 patients who continue to experience the long-term consequences of the illness, may need longer-term complex input such as pulmonary, cardiovascular, mental and neuromuscular rehabilitation interventions, with some countries already organizing COVID-19 rehab centres.6 In addition, it is possible that non COVID-19 patients with cardiovascular disease (or other pathologies, e.g. respiratory, neurological disease) who were unable to participate in any outpatient program during the pandemic to require increased attention. Although the nature of the problem is not known, most certainly, existing structures of rehabilitation will be unable to sustain this high demand. While tele-rehabilitation is expected to be developed and to play a significant role in the future, outpatient CR programmes will still be required especially for high risk patients who need to start exercise training in a supervised setting, at least an initial stage of CR, in order to be able to detect potential complications, modify medication and regain physical confidence.7 In addition, outpatient CR programs are known to encourage patient social interaction and motivation improving the psychological profile of the participants,8 which maybe of increased importance, especially during the ‘post acute COVID-19 phase’, in which feelings of isolation and depression have already been enhanced. Thus, unless there is a dramatic change in political and managerial-decision making with regard to rehabilitation services, a lot of patients may not receive expert rehabilitation at all.
Even before the pandemic and although CR is proved to be evidence-based and cost-effective, most patients with cardiovascular disease in Europe needing outpatient CR, were not receiving it.3,9,10 Main reasons include lack of resources, since CR programs are usually funded for only a short period of time or not funded at all in some countries resulting in an absence of sustained interest in the provision and commission of CR and in a low patient referral and adherence. For example, National Health Insurance in Greece does not cover outpatient CR. Thus, in our Institute, outpatient CR is mostly provided through CR research protocols. These protocols are based on the initiative and the professionalism of the scientific staff involved and sometimes supported by the Alexander S. Onassis Public Benefit Foundation. Lack of a unified implementation strategy of CR is another issue that may also need to be considered. Although steps have been made forward, CR services could possibly further improve if healthcare management was more aware that rehabilitation is framed in the context of a holistic biopsychosocial model of illness (introduced by Engel in 1977),11 rather than a biomedical model.6 This means that organization of CR services can become a complex task requiring the co-ordination and collaboration of different professionals such as medical doctors, physiotherapists, psychologists, dieticians, social workers, and nurses.6,11
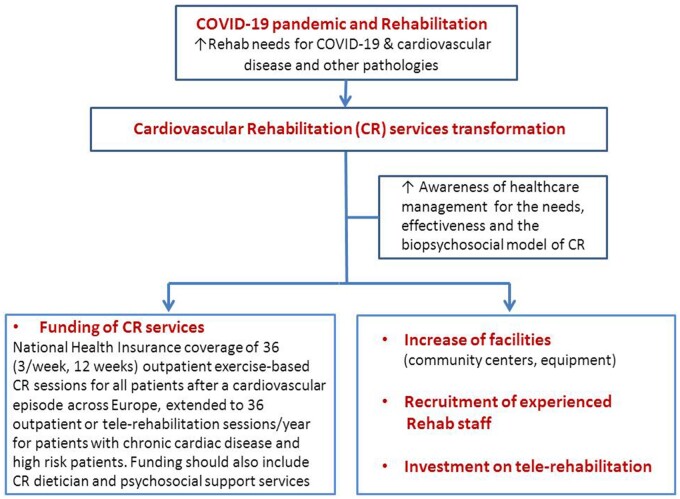
A ‘bell is ringing’ for the ‘acute’ and particularly for the ‘post acute COVID-19’ expected rise in rehabilitation needs. These needs should be associated with a unified European policy for funding and planning on the reconfiguration of CR and other rehabilitation services. Thus, considering that exercise training is the cornerstone of CR,3 it is suggested that all patients after an episode of cardiovascular disease (e.g., myocardial infarction, percutaneous coronary intervention, cardiac surgery, heart failure, device implantation) should be entitled to the prescription of 36 outpatient exercise-based CR sessions (3/week, 12 weeks) covered by all National Health Insurances across Europe. For patients with chronic cardiac disease or patients at high risk, coverage should be extended to 36 outpatient or tele-rehabilitation exercise-based CR sessions per year, according to individual needs. Funding should also include CR dietician and psychosocial support services. Furthermore, increasing facilities such as community centres and equipment, recruitment of experienced rehabilitation staff and investment on tele-rehabilitation programmes are all actions of high priority (Figure 1).
Figure 1.
COVID-19 pandemic and rehabilitation: time for transformation of cardiovascular rehabilitation services across Europe.
Thus, COVID-19 crisis should be looked not only as a disaster, but also as an opportunity to transform CR (and other rehabilitation) services, promoting change in order to increase the efficiency and effectiveness but also to fully integrate this intervention into healthcare services. In this way, healthcare systems will also become better prepared to face a future pandemic, if needed.
Conflict of interest: none declared.
Data Availability Statement
Data available upon reasonable request.
References
- 1. World Health Organization. Rehabilitation and COVID-19. https://www.who.int/teams/noncommunicable-diseases/covid-19/rehabilitation (accessed December 2020).
- 2. Tersalvi G, Winterton D, Cioffi GM, Ghidini S, Roberto M, Biasco L, Pedrazzini G, Dauw J, Ameri P, Vicenzi M.. Telemedicine inheart failure during COVID-19: a step into the future. Front Cardiovasc Med 2020;7:612818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ambrosetti M, Abreu A, Corrà U, Davos CH, Hansen D, Frederix I, Iliou MC, Pedretti RF, Schmid JP, Vigorito C, Voller H, Wilhelm M, Piepoli MF, Bjarnason-Wehrens B, Berger T, Cohen-Solal A, Cornelissen V, Dendale P, Doehner W, Gaita D, Gevaert AB, Kemps H, Kraenkel N, Laukkanen J, Mendes M, Niebauer J, Simonenko M, Zwisler AO.. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol 2020;doi:10.1177/2047487320913379. [DOI] [PubMed] [Google Scholar]
- 4. Scherrenberg M, Wilhelm M, Hansen D, Völler H, Cornelissen V, Frederix I, Kemps H, Dendale P.. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol 2020;doi:10.1177/2047487320939671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Deursen AJ. Digital inequality during a pandemic: quantitative study of differences in COVID-19-related internet uses and outcomes among the general population. J Med Internet Res 2020;22:e20073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wade DT. Rehabilitation after COVID-19: an evidence-based approach. Clin Med (Lond) 2020;20:359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schmid JP. Telehealth during COVID-19 pandemic: will the future last? Eur J Prev Cardiol 2020;doi:10.1093/eurjpc/zwaa016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alqahtani MM, Alanazi AMM, Yohannes AM, Smith CE, Goodfellow LT.. The effectiveness of cardiopulmonary rehabilitation programs on psychosocial factors in patients with pulmonary and cardiac disease. J Cardiopulm Rehabil Prev 2021;doi:10.1097/HCR.0000000000000599. [DOI] [PubMed] [Google Scholar]
- 9. Hinde S, Bojke L, Harrison A, Doherty P.. Improving cardiac rehabilitation uptake: potential health gains by socioeconomic status. Eur J Prev Cardiol 2019;26:1816–1823. [DOI] [PubMed] [Google Scholar]
- 10. Santiago de Araújo Pio C, Chaves G, Davies P, Taylor R, Grace SL.. Cochrane corner: increasing patient utilisation of cardiac rehabilitation. Heart 2020;106:248–250. [DOI] [PubMed] [Google Scholar]
- 11. Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129–136. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available upon reasonable request.