Abstract
Background:
Patients undergoing orthopedics surgery experience the most severe postoperative pain. The fasting time is a factor that affects this complication. The aim of this study was to investigate the impact of fasting time reduction by using oral carbohydrate on postoperative pain and analgesic consumption in orthopedic patients.
Materials and Methods:
This randomized control trial was conducted between November 2017 and December 2018. Sixty-four patients were randomly assigned into the intervention (which consumed 200 mL of the 12.50% carbohydrate, 2 h before the surgery) and the control group (which was fasted from midnight). Postoperative pain was measured by visual analog scale; the amount of the consumed analgesics was also recorded. The data were analyzed by using Chi-square and t-test.
Results:
The mean (SD) of the pain scores in the control group immediately and 2, 4, 6, 12 and 24 h after consciousness were 7.19 (2.64), 6.69 (2.17), 6.31 (2.05), 6.16 (2.08), 6.06 (2.24), and 5.38 (1.86), respectively. These scores for the intervention group were 7.44 (1.48), 6.31 (1.25), 5.72 (1.17), 5.59 (1.43), 5.25 (1.13), and 4.97 (1.57). The mean of the pain scores between two groups was not different (p > 0.05). The amount of the consumed morphine (t61= -2.10, p = 0.039), pethidine (t62= -2.25, p = 0.028), and diclofenac (t62= -2.51, p = 0.015) were significantly different between the two groups.
Conclusions:
The pain intensity in the patients with shortened fasting time was lower, but it was not statistically significant. Moreover, reducing fasting time by using carbohydrate significantly reduced the use of analgesics.
Keywords: Fasting, orthopedics, pain, postoperative, preoperative period
Introduction
Studies have shown that pain is the most prevalent postoperative complication.[1,2] Most of the pain-related complaints are made by patients having undergone orthopedic surgeries, so that 98.40% of these patients experience moderate postoperative pain.[3,4] Many factors including demographic characteristics, genetic differences, the patient's personality characteristics, the type, extent, and location of the surgery, and related diseases may influence the surgical pain.[5,6] Another influencing factor is the prolonged preoperative fasting time, which leads to more pain, anxiety, postoperative nausea and vomiting, insomnia, fatigue, impairment of the immunity system, and increased insulin resistance.[7,8,9]
In 1999, the American Society of Anesthesiologists (ASA) suggested that clear liquids should be used 2 h before surgery. In 2005, the Royal Nursing College of Britain referred to this issue in its guidelines.[9] However, many centers still utilize traditional methods and make patients fast from midnight.[10] According to some studies, preoperative reduction of fasting time leads to the reduction of postoperative pain. Yilmaz et al. showed that the patients who had consumed 12.50% carbohydrate solution 2 h before thyroidectomy experienced less postoperative pain compared with those who fasted from midnight.[11] The study of Singh et al. was similar to the previous study. They found that the patients who had fasted from midnight suffered from more postoperative pain compared with those patients who had consumed 12.50% carbohydrate 2 hbefore laparoscopic cholecystectomy.[12] Rizvanović et al. found that the consumption of oral carbohydrate solution 2 h before colorectal surgery did not diminish postoperative pain score compared with those who had fasted for 8 h.[13] Similar results have been shown in Xu et al. meta-analysis study.[14] However, some contradictory results have been obtained. Karlsson et al. found that the consumption of oral carbohydrate solution had no effect on postoperative pain in the patients who underwent laparoscopic gastric bypass.[15] Moreover, the systematic reviews of Smith et al. and Bilku et al. have obtained similar results that the reduction of fasting time by carbohydrate solution does not relieve postoperative pain.[16,17] Lauwick et al. found that reduction of fasting time up 2 before thyroidectomy by oral carbohydrate solution did not affect postoperative pain but reduced analgesic consumption.[18] Studies in this regard are very limited, and no other recent study has been found.
Although reduction of fasting time to 2 h before surgery by using clear liquids has been recommended, in some countries such as Iran, the traditional methods, Nil Per Os (NPO) from midnight, are still employed. As noted, there have been contradictory results about the effect of fasting time reduction, through the consumption of carbohydrate solution on postoperative pain. Additionally, almost all of these studies examined only the severity of pain and did not consider the use of analgesics. In addition, statistics and studies have reported the highest rate of postoperative pain in patients undergoing orthopedics surgery. However, a limited number of studies have been performed on these patients. Also, no similar study was found in Iran. Therefore, the present study was conducted in order to analyze the effect of fasting time reduction by using carbohydrate solution on postoperative pain and analgesic consumption in the patients undergoing orthopedic surgery who suffer from the most acute postoperative pain. In addition, in the present study, unlike previous studies, the effect of preoperative fasting time reduction on the use of postoperative analgesia was also analyzed.
Materials and Methods
This one-step randomized control trial is (IRCT20171216037895N1) on 24 Sep 2018. This study is as a part of a more comprehensive study on the postoperative complications of the orthopedic surgery, was conducted in Isfahan, Iran, between November 2017 and December 2018. The samples were selected by using a simple sampling method from the patients referred to a center for elective orthopedic surgeries. Given that the most important variable in this study is adjusting the fasting time of patients, so measures should be planned in such a way that the patient consumed the solution about 2 h before surgery. Therefore, considering cases such as workload and emergency surgery, a hospital with the maximum conditions was selected as a research environment. The sample size was determined with the help of statistical experts and similar studies.[11,12,19,20] The confidence coefficient, the test power, and the standard error were, respectively determined to be 95%, 80%, and 0.70 of standard deviation. Accordingly, the number of the samples was determined to be 64 patients. Sampling was continued until the size of the sample reached the predetermined size, and the exclusion of the samples was also was considered. The significance level was considered to be 0.05 in this study.
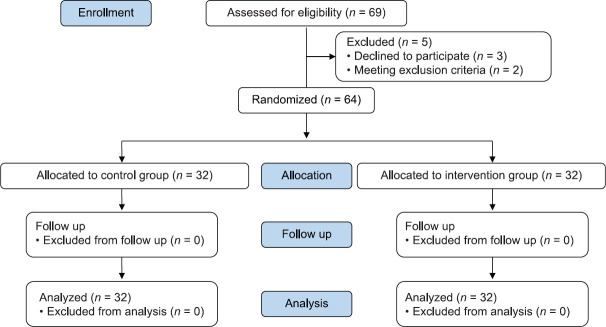
The patients meeting the inclusion criteria of willingness to participate in the study, being more than 18 years old, not having multiple traumas, having elective and nonemergency surgery, no suffering from diabetes mellitus, not being a candidate for spinal anesthesia, American Society of Anesthesiologists (ASA) status of 1 and 2, were randomly assigned into two groups of the intervention (who underwent fasting 2 h before the surgery) and the control. The random assignment of the samples was done using Excel software and RANDBETWEEN function in the range of 1 to 64. After selecting 64 patients, the first 32 patients, were assigned to the intervention group and the rest to the control group. The numbers listed by the software were then assigned to those patients attending the treatment. In case of any problem or disease (such as pregnancy, acute gastrointestinal ulcer, food poisoning, bowel obstruction, or multiple trauma) that required the use of medicines or other measures in the treatment process, or if it had an effect on the variable measured by the study, the patient was excluded from the study [Figure 1].
Figure 1.
Consort diagram
To the subjects of the intervention group 200 mL of 12.50% carbohydrate solution were given 2 h before the surgery.[14] The mentioned solution was prepared by one of the researchers. The control group subjects received the common training on the fasting time and fasted from midnight. The injection of intravenous fluids was started 8 h before the surgery. Before being taken to the operation room, the patients were injected with 1000 cc of serum dextrose 33.30% and sodium chloride 0.30% every 8 h. The same anesthesia technique was used for all of the patients. During the operation, the patients received 4 mL of the ringer serum kg/h. To measure the intensity scale of the postoperative pain, the Visual Analogue Scale (VAS) was employed.[21] The patients' pain was measured 6 times after the surgeries (immediately after consciousness, 2, 4, 6, 12, and 24 h later).[21,22] The intensity scale of the pain was recorded by the patients themselves. It should be noted that the type and dose of the used analgesics were determined according to the physician's order.
Blinding is not done in this study. But none of the health workers (including the surgeon, anesthesiologist, and nurses) and the analyzer were aware of the grouping of the patients. The data collected in the present study included demographic characteristics (such as age, sex, education level, and body mass index) and the surgical specifications (duration of unconsciousness period and the type of surgery) and the used medicines (types of analgesics, intravenous fluids, and other medicines). The data were analyzed using the Statistical Package for the Social Sciences (SPSS) software (version 16.0, SPSS Inc., Chicago, IL, USA) and the descriptive and inferential statistical methods. Chi-square and t-tests were employed for the analysis of the demographic and surgical characteristics. Independent t-test was also used in different time intervals in both the intervention and the control groups for the analysis and comparison of the pain intensity, the surgical specifications, and the dose of the used medicines.
Ethical considerations
This one-step randomized control trial is registered under the registration code IR.MUI.REC.1396.3.700 in the Ethics Committee of Isfahan University of Medical Sciences. The sampling was started after obtaining a written informed consent from the patients.
Results
In the present study, 64 patients participated. The results of the study showed that both groups were homogeneous in terms of demographic characteristics, surgical specifications, and the medicines (p < 0.05). The mean (SD) age of the samples participating in the study was 36.44 (13.60) and the mean age of the groups showed no significant differences (t62= -1.66, p = 0.102). In each group, 62.50% (n = 20) of the samples were male. The mean (SD) of Body Mass Index (BMI) was 26.29 (2.93) in the control group and 25.06 (4.36) in the intervention group and did not differ significantly between the two groups as one of the influential variables in the study (t62= -1.32, p = 0.192).
The mean (SD) fasting time of the intervention group was 130.31 (64.00) min and that of the control group was 641.25 (244.52) min. The mean (SD) duration of surgery was 123.12 (40.53) min in the intervention group and 123.59 (52.63) minutes in the control group that was not statistically significant (t62= -0.04, p = 0.968). As Table 1 shows, the type and location of surgeries in both groups were not different. Cefazolin was the only medicine used before the surgery for some of the patients, the mean use of which was not significantly different between the two groups (F63= 0.05, p = 0.817). Except for analgesics, other medications used in the patients after the surgery were not significantly different [Table 2].
Table 1.
Type and Location of surgeries in the intervention and control group
| Control group n=32 | Intervention Group n=32 | Chi square |
|||
|---|---|---|---|---|---|
| χ2 | df | p | |||
| Type of surgery | |||||
| Anterior Cruciate Ligament Reconstruction | 9 | 7 | 6.55 | 8.00 | 0.610 |
| Carpal Tunnel Syndrome | 5 | 2 | |||
| Fracture | 6 | 3 | |||
| High Tibial Osteotomy | 2 | 3 | |||
| Remove of plaque/pin | 3 | 5 | |||
| Tumor | 1 | 5 | |||
| Arthroscopy (meniscectomy) | 2 | 2 | |||
| Hand tendon repair | 3 | 3 | |||
| Other | 2 | 2 | |||
| Location of surgery | |||||
| Upper Limb | 16 | 10 | 2.33 | 1.00 | 0.130 |
| Lower Limb | 16 | 22 | |||
Table 2.
Medicines used after surgery in the intervention and control group
| Control group Mean (SD) | Intervention Group Mean (SD) | Independent t-test |
Confidence Interval |
||||
|---|---|---|---|---|---|---|---|
| t | df | p | Lower | Upper | |||
| Dextrose 33.3% and Sodium chloride 0.3% (mL*) | 1265.62 (567.74) | 1531.25 (564.40) | 2.10 | 62.00 | 0.053 | 13.98 | 579.76 |
| Ringer (mL*) | 1484.38 (641.12) | 1593.75 (787.37) | 0.96 | 62.00 | 0.506 | -186.93 | 530.68 |
| Cefazolin (mg**) | 547.00 (2.89) | 600.00 (2.64) | 0.77 | 62.00 | 0.446 | -0.85 | 1.91 |
| Gentamicin (mg**) | 150.40 (2.36) | 141.60 (2.36) | -0.16 | 62.00 | 0.875 | -1.27 | 1.08 |
| Enoxaparin (U***) | 4000.00 (4428.64) | 3000.00 (3801.52) | -0.97 | 62.00 | 0.336 | -3062.44 | 1062.44 |
| Morphine (mg**) | 7.19 (7.29) | 3.87 (4.95) | -2.11 | 61.00 | 0.039 | -6.46 | -0.16 |
| Pethidine (mg**) | 71.88 (85.13) | 34.06 (42.49) | -2.25 | 62.00 | 0.028 | -71.43 | -4.18 |
| Methadone (mg**) | 0.00 (0.00) | 0.31 (1.76) | 1.00 | 62.00 | 0.321 | -0.31 | 0.93 |
| Diclofenac suppository (mg**) | 56.31 (98.13) | 9.38 (39.01) | -2.51 | 62.00 | 0.015 | -84.25 | -9.62 |
| Paracetamol (mg**) | 1.97 (2.49) | 1.97 (2.30) | 0.00 | 62.00 | 1.00 | -1.20 | 1.20 |
| Acetaminophen Tablet (mg**) | 890.62 (1029.67) | 640.62 (1071.88) | -0.95 | 62.00 | 0.345 | -775.22 | 275.22 |
Milliliter*, milligram**, Unit***
The pain experienced by the patients was measured 6 times after the surgeries, immediately after the consciousness and then, 2, 4, 6, 12, and 24 h later. The greatest intensity of pain was recorded immediately after the consciousness and the least intensity of pain was recorded 24 h later. The greatest difference in pain intensity between the two groups was recorded 12 h after the consciousness. The mean (SD) pain intensity of the intervention group 7.44 (1.48) was higher than that of the control group 7.19 (2.64) only during the consciousness period (t62= 0.46, p = 0.642). But in other intervals, the mean pain intensity of the intervention group was lower than that of the control group [Table 3]. However, the total mean (SD) intensity of pain in the intervention group 5.88 (1.05) was lower than that of the control group 6.30 (1.92), but this difference was not statistically significant (t62= 1.07, p = 0.278)
Table 3.
Postoperative pain intensity in intervention and control group
| Control group Mean (SD) | Intervention group Mean (SD) | Independent t-test |
Confidence Interval |
||||
|---|---|---|---|---|---|---|---|
| t | df | p | Lower | Upper | |||
| Immediately after consciousness | 7.19 (2.64) | 7.44 (1.48) | 0.46 | 62.00 | 0.642 | -0.82 | 1.32 |
| 2 h after consciousness | 6.69 (2.17) | 6.31 (1.25) | -0.84 | 0.402 | -1.26 | 0.51 | |
| 4 h after consciousness | 6.31 (2.05) | 5.72 (1.17) | -1.42 | 0.161 | -1.42 | 0.24 | |
| 6 h after consciousness | 6.16 (2.08) | 5.59 (1.43) | -1.26 | 0.213 | -1.45 | 0.33 | |
| 12 after consciousness | 6.06 (2.24) | 5.25 (1.13) | -1.83 | 0.072 | -1.70 | 0.76 | |
| 24 h after consciousness | 5.38 (1.86) | 4.97 (1.57) | -0.94 | 0.350 | -1.26 | 0.45 | |
The amount of morphine (t62= -2.11, p = 0.039) and pethidine (t62= -2.25, p = 0.028) administered to the intervention group was significantly less than that of the control group. However, methadone administered to the two groups did not differ significantly (t62= 1.00, p = 0.321). Regarding nonopioid analgesics, the use of diclofenac suppository in the intervention group was significantly lower than its administration to the control group (t62= -2.51, p = 0.015). However, the amount of the paracetamol (t62= 0.00, p = 1.00) and acetaminophen (t62= -0.95, p = 0.345) tablets administered to each group was not different [Table 2].
Discussion
This study was planned and conducted with the aim of examining the impact of fasting time reduction by using oral carbohydrate on postoperative pain and analgesic consumption in orthopedic patients. In the present study, the mean fasting time of the control group was 641.25 (244.52) min. It was significant considering the duration of the surgery 123.59 (52.63) min for the control group), as well as the time each patient needs to reach the conditions of starting the postoperative diet. According to the previous research and reviews, if fasting takes a long time, it may have side effects such as hunger, thirst anxiety, postoperative nausea and vomiting, impairment of immunity and higher insulin resistance, longer hospitalization time, less comfort and satisfaction more postoperative Intensive Care Unit (ICU) admission, and even death on patients.[9,10,23,24] Regardless of the positive effects of fasting time reduction, this method is safe. The mentioned conclusion has been corroborated by some other similar studies.[15,25] The results of the systematic review conducted by Bilku et al. (2014) suggest that the consumption of carbohydrate solution, up to 90 min before the surgery, is completely safe and can improve postoperative recovery.[17]
Moreover, the results also show that the use of morphine, along with pethidine and diclofenac suppositories in the intervention group was significantly lower than that in the control group. These analgesic medicines were used in the post-anesthesia care unit (PACU) and surgical ward. Any reduction in the administration of analgesics, regardless of its effects on lowering the side effects of such medicines (such as cardiovascular, neurological, gastrointestinal, and respiratory disorders[26]), suggests a lessening of the pain in the patients. The results of the study by Lauwick et al., suggesting that the consumption of carbohydrates before the operation lowers the use of analgesics are consistent with those of the present study.[18] Similarly, the study of Jablameli et al. showed that the consumption of oral carbohydrate before elective surgeries reduced analgesics consumption compared with those received intravenous carbohydrate.[27] No study was found examining the mechanism of the effect of oral carbohydrate intake on analgesics consumption. It seems that more studies are needed in this regard.
Within the present study, the mean pain intensity of the intervention group clinically was lower than that of the control group in 2, 4, 6, 12, and 24 h intervals after the consciousness. It seems that lowering the administration of analgesics to the patients of the intervention group, compared with those of the control group, led to less pain in the former. However, the difference between the mean pain intensity of the two groups was not statistically significant which can be due to the subjectivity of the concept of pain and the lack of a more precise for measuring the pain.
The study of Karlsson et al., conducted on the patients undergoing gastric bypass surgery shows that if carbohydrates, proteins, and water are administered before surgery, the variables of pain, nausea, and headache will not change significantly.[15] Ljunggren and Hahn also conducted a study on the patients undergoing hip replacement surgery through spinal anesthesia, and found that the group to whom carbohydrates were administered before the surgery was not significantly different from the group that underwent fasting from midnight, and also from the group that drank water 2 h before the surgery in terms of the postoperative complications, such as pain.[28]
Unlike the present study and the research of Karlsson et al., the results of Yilmaz et al. show that the administration of oral carbohydrate 12.50% before thyroidectomy results in less oral dryness, fatigue, weakness, headache, vomiting, and postoperative pain.[11] In the study conducted by Cakar et al., 800 mL of the related solution was administered to the patients the night before the surgery and 400 mL of it was also administered 2 h before the surgery.[29] The study of Singh et al. also shows a similar result in this regard. This study was conducted on the patients undergoing cholecystectomy. The administration of 400 mL of carbohydrate solution 12.50% the night before surgery and 200 mL of it 2 h before the surgery lowered nausea and vomiting as well as postoperative pain in these patients.[12] Orthopedic surgeries are more major and invasive than thyroidectomy and laparoscopic cholecystectomy. Furthermore, according to studies, the severity of pain in these patients is higher than in other surgeries. On the other hand, several factors affect the amount of pain that was not discussed in these studies. Therefore, these are the reasons for the difference between the results of these studies and those of the present study.
In their study on the patients undergoing cholecystectomy, Tosun et al. found that the patients who undergo fasting for more than 12 h, compared with those who experienced preoperative fasting for less than 12 h, sustained more hunger, thirst, nausea, and more pain.[9] According to this study, a possible reason for the insignificance of the impact of shortening the patients' fasting time on the postoperative pain is the short mean of fasting time in the control group.
Some of the limitations of the study are as follows: A wide range of surgeries were considered in the study and there were no restrictions on the types of surgeries. Therefore, the severity of the pain caused by one of these surgeries was different. Because patients under general anesthesia were included in the study, major surgeries with more pain such as total knee replacement were excluded. Owing to the different types of studied surgeries, it was not possible to use the same postoperative analgesic regimen. Owing to the mental nature of the pain variable, several factors, including cultural differences, affect it, which cannot be measured. Various types of orthopedic surgeries have also been studied, which are considered minor surgeries. Therefore, the severity of pain was lower in these patients compared to those of the major surgeries. On the other hand, the analgesics used in these patients were of different types. If a specific type of analgesics was used in all patients, the results would be more specific.
Conclusion
Shortening the fasting time of the patients undergoing the elected orthopedic surgeries by the administration of 200 mL carbohydrate solution 12.50% 2 h before the surgery does not reduce pain intensity. However, the administration of this solution reduces the administration of analgesics, especially narcotic medicines.
Despite the positive results that some studies have shown for patients with reduced fasting time before surgery, no side effects have been reported so far, including an increased risk of aspiration. Therefore, it is not necessary to keep patients fasting for a long time. According to studies, one of the reasons for the noncompliance of medical staff with this method is the lack of awareness and fear of its complications. Although shortening the fasting time does not reduce pain intensity, it reduces the administration of analgesics. However, due to the limited number of similar studies, more extensive research is needed.
Financial support and sponsorship
Isfahan University of Medical
Conflicts of interest
Nothing to declare.
Acknowledgements
This study is part of a master's thesis and funded by Isfahan University of Medical Sciences (Funding ID is 396700). We appreciate all people who cooperated during the course of this study, especially all patients participating in the study and nurses.
References
- 1.Shaikh SI, Nagarekha D, Hegade G, Marutheesh M. Postoperative nausea and vomiting: A simple yet complex problem. Anesth Essays Res. 2016;10:388–96. doi: 10.4103/0259-1162.179310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zaslansky R, Meissner W, Chapman C. Pain after orthopaedic surgery: Differences in patient reported outcomes in the United States vs internationally. An observational study from the PAIN OUT dataset. Br J Anaesth. 2018;120:790–7. doi: 10.1016/j.bja.2017.11.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torabi Khah M, Yousefi H, Monazami Ansari A-H, Musarezaie A. Prevalence of postoperative nausea and vomiting and pain in patients undergoing elective orthopaedic surgery in Iran. J Perianesth Nurs. 2020;35:294–7. doi: 10.1016/j.jopan.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Polanco-Garcia M, Garcia-Lopez J, Fabregas N, Meissner W, Puig MM. Postoperative pain management in Spanish hospitals. A cohort study using the PAIN-OUT registry. J Pain. 2017;18:1237–52. doi: 10.1016/j.jpain.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Chapman CR, Vierck CJ. The Transition of acute postoperative pain to chronic pain: An integrative overview of research on mechanisms. J Pain. 2017;18:359.e1–38. doi: 10.1016/j.jpain.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Correll D. Chronic postoperative pain: Recent findings in understanding and management. F1000Res. 2017;6:1054. doi: 10.12688/f1000research.11101.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robleda G, Sillero-Sillero A, Puig T, Gich I, Banos JE. Influence of preoperative emotional state on postoperative pain following orthopedic and trauma surgery. Rev Lat Am Enfermagem. 2014;22:785–91. doi: 10.1590/0104-1169.0118.2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mousavi FS, Golmakani N, Saki A. The relationship between postoperative pain after cesarean section with pre and postoperative anxiety. Iran J Obstet Gynecol Infertil. 2016;19:1–10. [Google Scholar]
- 9.Tosun B, Yava A, Acikel C. Evaluating the effects of preoperative fasting and fluid limitation. Int J Nurs Pract. 2015;21:156–65. doi: 10.1111/ijn.12239. [DOI] [PubMed] [Google Scholar]
- 10.Pereira NC, Turrini RNT, Poveda VB. Perioperative fasting time among cancer patients submitted to gastrointestinal surgeries. Rev Escola Enfermagem U S P. 2017;51:e03228. doi: 10.1590/S1980-220X2016036203228. [DOI] [PubMed] [Google Scholar]
- 11.Yilmaz N, Çekmen N, Bilgin F, Erten E, Özhan MÖ, Coşar A. Preoperative carbohydrate nutrition reduces postoperative nausea and vomiting compared to preoperative fasting. J Res Med Sci. 2013;18:827–32. [PMC free article] [PubMed] [Google Scholar]
- 12.Singh BN, Dahiya D, Bagaria D, Saini V, Kaman L, Kaje V, et al. Effects of preoperative carbohydrates drinks on immediate postoperative outcome after day care laparoscopic cholecystectomy. Surg Endosc. 2015;29:3267–72. doi: 10.1007/s00464-015-4071-7. [DOI] [PubMed] [Google Scholar]
- 13.Rizvanović N, Nesek Adam V, Čaušević S, Dervišević S, Delibegović S. A randomised controlled study of preoperative oral carbohydrate loading versus fasting in patients undergoing colorectal surgery. Int J Colorectal Dis. 2019;34:1551–61. doi: 10.1007/s00384-019-03349-4. [DOI] [PubMed] [Google Scholar]
- 14.Xu D, Zhu X, Xu Y, Zhang L. Shortened preoperative fasting for prevention of complications associated with laparoscopic cholecystectomy: A meta-analysis. J Int Med Res. 2017;45:22–37. doi: 10.1177/0300060516676411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karlsson A, Wendel K, Polits S, Gislason H, Hedenbro JL. Preoperative nutrition and postoperative discomfort in an ERAS setting: A randomized study in gastric bypass surgery. Obes Surg. 2016;26:743–8. doi: 10.1007/s11695-015-1848-7. [DOI] [PubMed] [Google Scholar]
- 16.Smith MD, McCall J, Plank L, Herbison GP, Soop M, Nygren J. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst Rev. 2014:Cd009161. doi: 10.1002/14651858.CD009161.pub2. doi: 10.1002/14651858.CD009161.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bilku DK, Dennison AR, Hall TC, Metcalfe MS, Garcea G. Role of preoperative carbohydrate loading: A systematic review. Ann R Coll Surg Engl. 2014;96:15–22. doi: 10.1308/003588414X13824511650614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lauwick SM, Kaba A, Maweja S, Hamoir EE, Joris JL. Effects of oral preoperative carbohydrate on early postoperative outcome after thyroidectomy. Acta Anaesthesiol Belg. 2009;60:67–73. [PubMed] [Google Scholar]
- 19.Savluk OF, Kuscu MA, Guzelmeric F, Gurcu ME, Erkilinc A, Cevirme D, et al. Do preoperative oral carbohydrates improve postoperative outcomesin patients undergoing coronary artery bypass grafts? Turk J Med Sci. 2017;47:1681–6. doi: 10.3906/sag-1703-19. [DOI] [PubMed] [Google Scholar]
- 20.Onalan E, Andsoy II, Ersoy OF. The effect of preoperative oral carbohydrate administration on insulin resistance and comfort level in patients undergoing surgery. J Perianesth Nurs. 2019;34:539–50. doi: 10.1016/j.jopan.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Mohaghegh T, Yazdi B. Effect of intravenous anesthesia with propofol versus isoflurane inhalation anesthesia in postoperative pain of inguinal herniotomy: A randomized clinical trial. Med Gas Res. 2017;7:86–92. doi: 10.4103/2045-9912.208511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amiri HR, Mirzaei M, Beig Mohammadi MT, Tavakoli F. Multi-modal preemptive analgesia with pregabalin, acetaminophen, naproxen, and dextromethorphan in radical neck dissection surgery: A randomized clinical trial. Anesthesiol Pain Med. 2016;6:e33526. doi: 10.5812/aapm.33526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Imbelloni LE, Pombo IA, Morais Filho GB. Reduced fasting time improves comfort and satisfaction of elderly patients undergoing anesthesia for hip fracture. Rev Brasil Anestesiol. 2015;65:117–23. doi: 10.1016/j.bjan.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Pimenta GP, De Aguilar-Nascimento JE. Prolonged preoperative fasting in elective surgical patients: Why should we reduce it? Nutr Clin Pract. 2014;29:22–8. doi: 10.1177/0884533613514277. [DOI] [PubMed] [Google Scholar]
- 25.Shah JN, Maharjan S, Gurung R. Shortened preoperative fasting time to allow oral rehydration solution clear liquid up to two hours before elective major surgery in adults. J Coll Physicians Surg Pak. 2018;28:348–51. doi: 10.29271/jcpsp.2018.05.348. [DOI] [PubMed] [Google Scholar]
- 26.Carter GT, Duong V, Ho S, Ngo KC, Greer CL, Weeks DL. Side effects of commonly prescribed analgesic medications. Phys Med Rehabil Clin N Am. 2014;25:457–70. doi: 10.1016/j.pmr.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 27.Jablameli M, Nazemroaya B, Salehfard L. Effects of preoperative glucose (dextrose/carbohydrate) administration via intravenous versus oral route on recovery outcome in the post-anesthesia care unit. Arch Anesthesiol Crit Care. 2019;5:110–4. [Google Scholar]
- 28.Ljunggren S, Hahn RG. Oral nutrition or water loading before hip replacement surgery; A randomized clinical trial. Trials. 2012;13:97. doi: 10.1186/1745-6215-13-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Çakar E, Yilmaz E, Çakar E, Baydur H. The effect of preoperative oral carbohydrate solution intake on patient comfort: A randomized controlled study. J Perianesth Nurs. 2017;32:589–99. doi: 10.1016/j.jopan.2016.03.008. [DOI] [PubMed] [Google Scholar]