Abstract
Background
As COVID-19 continues to spread globally, it is important to understand psychological factors that may influence compliance with social distancing.
Purpose
The present study examined whether Theory of Planned Behavior (TPB) constructs were associated with social distancing, with a focus on exploring moderators of the intention–behavior relationship.
Methods
Using a longitudinal design, U.S. adults (N = 507) self-reported TPB constructs and social distancing behavior at baseline and 3 months later. Participants were from 48 U.S. States and the District of Columbia and were on average 50.39 years old (SD = 15.32, range = 18–80). The majority were Non-Hispanic White (71.6%), had a bachelor’s degree or higher (55.3%), and resided in suburban areas (55.8%).
Results
While positive attitudes toward social distancing increased over time (p = .002), subjective norms weakened (p < .001) and perceived behavioral control (PBC) remained stable (p = .22). Interestingly, despite an increase in intentions from baseline to follow-up (p < .001), there was a significant decrease in social distancing behavior over time (p < .001). Consistent with the TPB, baseline attitudes (p < .001), subjective norms (p < .001), and PBC (p < .001) for social distancing were all associated with baseline intentions to social distance. In turn, baseline intentions were significantly associated with social distancing behavior at follow-up (p < .001). Younger adults (p < .001) and non-White participants (p = .002) displayed a greater intention–behavior gap relative to older and White participants. In contrast, participants with more stable intentions over time displayed a stronger intention–behavior relationship (p < .001).
Conclusions
Targeting individuals’ attitudes, norms, and PBC may effectively promote protective behaviors intended to mitigate the spread of COVID-19 and similar viral outbreaks. Future research should examine effective strategies for translating social distancing intentions into actions.
Keywords: Theory of planned behavior, Social distancing, Intention–behavior, Prevention, COVID-19
Social distancing attitudes, norms, perceived behavioral control, and intentions were associated with social distancing behavior at 3-month follow-up. Racial minorities and younger adults displayed larger intention-behavior gaps.
Introduction
As rates of disease and death caused by the novel coronavirus (COVID-19) continue to rise globally, there is critical need to motivate protective behaviors to mitigate its spread. Due to the complex, unpredictable nature of pandemic viruses, considerable time is required to develop and implement safe, effective medical interventions. Furthermore, geographical containment of viral infections is becoming increasingly less feasible in a globally connected world. As such, pandemic response strategies from the World Health Organization (WHO) and United States Department of Health and Human Services (HHS) emphasize the critical role of nonpharmaceutical interventions (NPIs) to mitigate the scope and severity of viral disease outbreaks [1, 2]. One such NPI is social distancing, which refers to maintaining a safe space (i.e., at least 6 ft) between oneself and people from other households, as well as avoiding large crowds and crowded spaces. Despite strong evidence that maintaining physical distance from others effectively mitigates community-based spread of COVID-19 and other similarly transmitted viral infections (e.g., influenza A), compliance with social distancing measures varies among individuals and communities [3–5]. Thus, identifying the psychosocial factors associated with adherence to social distancing measures is essential for controlling the COVID-19 pandemic and informing strategies for responding to future pandemics.
As a voluntary, preventive health behavior, the Theory of Planned Behavior (TPB) may provide a useful framework for predicting compliance with social distancing [6]. Per the TPB, the likelihood of performing a behavior depends on intentions, as determined by subjective norms and attitudes about the behavior, and perceived behavioral control (PBC). PBC may sometimes directly influence behavior (i.e., when actual control is high) [6, 7]. There is strong empirical evidence supporting applications of the TPB for predicting health behavior generally [8–11] and for COVID-19 mitigation specifically [5, 12]. Notably, in a sample of UK adults, Norman, Wilding, and Conner [13] found that individuals’ intentions and confidence that they could engage in the behavior predicted later compliance with protective behaviors such as maintaining physical distance (6+ ft) and not visiting family or friends. Instrumental attitudes and experiential attitudes were associated with limiting leaving the home and maintaining physical distance when in stores, respectively. In addition, Hagger et al. [14] found that subjective norms, PBC, and intentions were positively associated with later social distancing behavior. However, both studies were conducted in April 2020 when most U.S. and UK residents were still under stay-at-home orders and the follow-up periods were very brief (i.e., 1 week). As such, it is unclear whether these findings generalize to later timeframes when States were in various phases of re-opening and COVID-19 restrictions lessened. Comprehensive, longitudinal tests of the TPB are needed to examine the utility of this theoretical framework over different contexts and longer periods of time.
Despite the utility of the TPB, meta-analytic work suggests that behavioral intentions only explain, on average, 28% of the variance in behavior [15]; the so-called intention–behavior gap [16]. To identify populations at risk of poor compliance with social distancing measures, it is critical to identify the characteristics of those who are least likely to translate their social-distancing intentions into actions. Few studies have examined moderators of the intention–behavior gap in the context of COVID-19. However, previous research has suggested that older age [17], higher socioeconomic status [18], stronger PBC [19], engaging in the behavior previously [19], and more stable intentions [19, 20] predict a stronger intention–behavior relationship.
The Present Study
This study examined the utility of the TPB for predicting social distancing behavior over time. As social distancing encompasses a range of behaviors intended to mitigate the spread of COVID-19, the present study assessed compliance with numerous behaviors including staying home as much as possible, not visiting family or friends, avoiding large crowds, and maintaining social distance (6 ft) when going out. It was hypothesized that baseline attitudes, subjective norms, and PBC would all be associated with baseline social distancing intentions, which would in turn be associated with social distancing behavior at 3-month follow-up. Exploratory analyses were conducted to determine the stability of these constructs over time, as well as identify moderators of the intention–behavior relationship.
Methods
Participants and Procedures
Baseline data collection occurred online from April 21 to April 23, 2020 and follow-up data collection occurred from July 27 to July 29, 2020. Baseline methods have been reported previously in Magnan, Gibson, and Bryan [21]. At the time of baseline data collection, most U.S. states were under stay-at-home orders [22] and over 2.4 million cases of COVID-19 had been confirmed globally [23]. At the time of follow-up, confirmed COVID-19 cases increased to over 16.5 million cases globally, and COVID-19 related deaths increased from 186,000 to 650,000 [23]. While an estimated 97.8% of participants (n = 496) were under stay-at-home orders at baseline, only six participants reported still being under stay-at-home orders at follow-up.
Participants were recruited from the online platform Prolific (www.prolific.co) and were eligible to participate if they were at least 18 years of age and a U.S. citizen. They were invited to complete an anonymous survey assessing their beliefs and behaviors related to the COVID-19 pandemic. Approximately 3 months later, 508 respondents who passed quality control checks (i.e., did not discontinue participation, answered at least two of the three attention check questions correctly) for the baseline survey were invited to complete a follow-up survey. One person did not correctly answer at least two of three attention check questions, resulting in a final follow-up sample of N = 507. Participants provided online informed consent before completing both surveys and were compensated for their time and effort during baseline ($2.00) and follow-up ($1.30). This study was deemed exempt by the University of Colorado Boulder IRB due to the low risk associated with participation.
Measures
TPB measures were adapted from Gardiner and Bryan [24] (full measures are presented in Electronic Supplementary Material 1). Prior to completing the TPB measures, participants read the following instructions: The following series of questions ask about what you think about social distancing. Social distancing refers to maintaining at least 6 feet (2 meters) between people you do not live with, and avoiding mass gatherings. Participants indicated their attitudes towards social distancing on 11, seven-point semantic differential scales (e.g., (1) “unhealthy” to (7) “healthy,” (1) “punishing” to (7) “rewarding”) (T1 α = .86; T2 α = .93). Participants rated the extent to which they agreed with eight items assessing subjective norms (e.g., “Most of my friends engage in social distancing,” “People who are important to me think that I should do social distancing”) on a 1 (strongly disagree) to 7 (strongly agree) scale (T1 α = .89; T2 α = .91). Participants indicated the extent to which they agreed with six items assessing their social distancing perceived behavioral control (e.g., “I feel confident that I could do social distancing even if I was lonely,” “I feel confident that I could do social distancing even if my friends/family did not”) on a 1 (strongly disagree) to 7 (strongly agree) scale (T1 α = .81; T2 α = .86). Participants were asked, “How likely is it that you will do social distancing regularly over the next [two weeks, month, six months, year] if necessary?.” These social distancing intentions were scored on a 1 (very unlikely) to 7 (very likely) scale (T1 α = .87; T2 α = .94). Engagement in social distancing behavior was assessed using a five-item measure: “In the past two weeks, how often did you engage in the following behaviors?” (e.g., “stayed home as much as possible,” “went to friends’/family’s houses” [reverse-coded]). Responses were scored on a 1 (never) to 7 (very often) scale (T1 α = .78; T2 α = .73).
Demographic and TPB-related moderators
Demographic information was assessed at baseline and included age, gender, race/ethnicity, and socioeconomic status (SES). SES was assessed using the MacArthur Scale of Subjective Social Status [25] which ranges from 1 to 10 with higher scores indicating higher SES. Intention stability was computed consistent with prior research [19, 20] (see Electronic Supplementary Material 2).
Planned Analyses
To examine change in the theoretical mediators and social distancing behavior over time, we conducted a series of dependent samples t-tests. Next, we estimated a path analytic model to test whether baseline TPB constructs were associated with social distancing at follow-up. Consistent with the TPB [6, 7], for PBC we estimated both the direct path to behavior and the indirect path through intentions to social distancing behavior at follow-up. Lastly, to examine moderators of the intention–behavior relationship, we conducted a series of linear regressions with social distancing behavior at follow-up as the dependent variable where baseline intentions, the moderator, and the baseline intentions × moderator interaction term served as predictors. Baseline social distancing behavior was included as a covariate. Moderators examined included age, gender, race (White vs. non-White), ethnicity (Hispanic vs. non-Hispanic), subjective SES, income, education, intention stability, PBC, and previous behavior. Continuous predictors were mean-centered prior to being entered into each model [26]. All analyses were conducted in R version 4.0.3 (www.R-project.org) and the path analytic model was estimated using the lavaan package in R [27].
Results
507 participants completed both the baseline and follow-up surveys (see Table 1). Bivariate associations between all TPB constructs, social distancing behavior, and moderators are provided in supplementary Table S2 (see Electronic Supplementary Material 3).
Table 1.
Baseline demographics and sample characteristics (N = 507)
| Variable | M (SD) or No. (%) |
|---|---|
| Age | 50.39 (15.32) |
| Gender (%) | |
| Male | 245 (48.3) |
| Female | 258 (50.9) |
| Non-binary | 4 (0.8) |
| Race (%) | |
| White | 395 (77.9) |
| White (Non-Hispanic) | 363 (71.6) |
| Black/African American | 65 (12.8) |
| Asian | 34 (6.7) |
| American Indian/Alaska native | 1 (0.2) |
| Native Hawaiian/Pacific Islander | 1 (0.2) |
| Two or more races | 7 (1.4) |
| Hispanic/Latinx - any race (%) | 32 (6.3) |
| Education (%) | |
| <High school | 3 (0.6) |
| High school or GED | 35 (6.9) |
| Some college | 133 (26.2) |
| Associate degree or technical certification | 56 (11.0) |
| Bachelor’s degree | 198 (39.1) |
| Master’s degree | 66 (13.0) |
| Doctoral or professional degree | 16 (3.2) |
| Annual household income (%) | |
| < $25,000 | 105 (20.7) |
| $25,000-$49,999 | 136 (26.8) |
| $50,000-$74,999 | 105 (20.7) |
| $75,000-$99,999 | 76 (15.0) |
| $100,000-$149,999 | 57 (11.2) |
| >$150,000 | 28 (5.5) |
| SES | 5.44 (1.75) |
| Location of residence (%) | |
| Rural | 106 (20.9) |
| Suburban | 283 (55.8) |
| Urban | 118 (23.3) |
Note: The sample included participants from 48 states and the District of Columbia.
Change in TPB Constructs Over Time
Means of each TPB construct at baseline and follow-up are presented in Table 2. Although positive attitudes toward social distancing increased over time (t(506) = 3.15, p = .002), subjective norms supporting social distancing weakened (t(506) = −8.57, p < .001) and PBC for social distancing remained stable (t(506) = 1.24, p = .217). Interestingly, despite an increase in intentions over time (t(506) = 4.47, p < .001), there was a significant decrease in social distancing behavior (t(506) = −10.38, p < .001).
Table 2.
Mean (SD) of TPB mediators and behavior at baseline and follow-up.
| Measure | Study time point | |
|---|---|---|
| Baseline | Follow-up | |
| Attitudes | 5.31 (0.94) | 5.43 (1.13) |
| Subjective norms | 5.91 (0.95) | 5.56 (1.09) |
| Perceived behavioral control | 6.14 (0.81) | 6.18 (0.90) |
| Intentions | 6.08 (1.07) | 6.26 (1.13) |
| Behavior | 6.61 (0.70) | 6.28 (0.92) |
Note: Measures that significantly changed (p < .05) from baseline to follow-up are bolded.
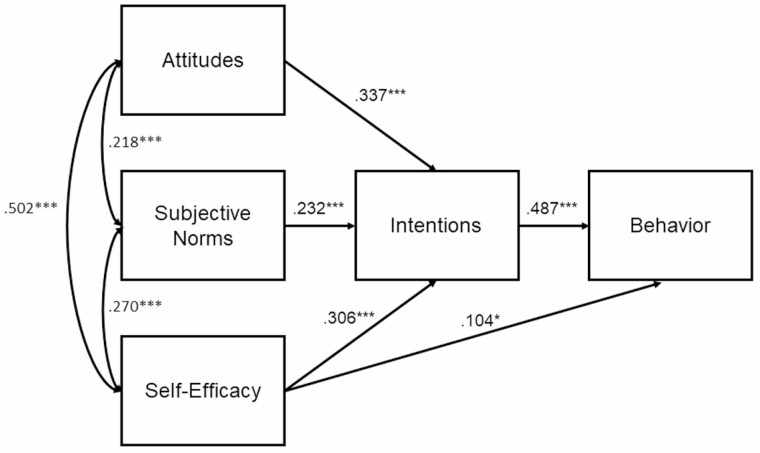
Model of Social Distancing Behavior at Follow-Up
The path model exhibited adequate fit to the data (χ2 = 16.07, p < .001, CFI = .973, RMSEA = .118, SRMR = .034) and accounted for 30.3% of the variance in social distancing behavior at follow-up (a large effect size for multivariate models in the social sciences; [28]). Standardized parameter estimates are presented in Fig. 1. Baseline attitudes, subjective norms, and PBC were significantly associated with intentions to social distance at baseline. In turn, baseline intentions were significantly associated with social distancing at follow-up. There was also a significant direct path from baseline PBC to social distancing behavior at follow-up. Note: Including demographic variables as exogenous predictors did not change the significance of the TPB pathways reported in the path analytic model.
Fig. 1.
Path analytic model. Note: all parameter values are standardized; *p < .05, **p < .01, ***p < .001.
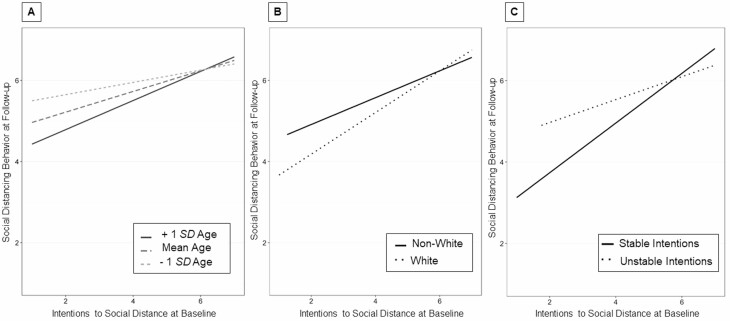
Moderators of the Intention–Behavior Relationship
Controlling for baseline social distancing, age (B = 0.18, t(503) = 3.09, p < .001) and race (B = 0.01, t(502) = 3.41, p = .002) significantly moderated the association between baseline intentions and behavior at follow-up, such that younger adults and non-White participants displayed a weaker intention–behavior relationship relative to older adults and White participants, respectively (see Fig. 2). In contrast, participants with more stable intentions over time displayed a stronger intention–behavior relationship (B = −0.10, t(502) = −4.65, p < .001) (see Fig. 2). Gender, ethnicity, subjective SES, income, education, and PBC, and previous behavior did not significantly moderate the association between social distancing intentions and behavior (ps > .060).
Fig. 2.
Significant moderators of the intention–behavior relationship. (A) Older participants exhibited a stronger intention–behavior relationship. (B) Non-White participants exhibited a weaker intention–behavior relationship relative to White participants. (C) Participants with stable intentions exhibited a stronger intention–behavior relationship compared to participants with unstable intentions.
Discussion
Despite uncontested biologic and epidemiologic support for social distancing, compliance with such measures during the COVID-19 pandemic is highly variable. Consistent with the TPB [6, 7], attitudes, subjective norms, and perceived behavioral control were associated with intentions to social distance at baseline, which were in turn associated with social distancing behavior 3 months later. Importantly, while the majority of participants were under stay-at-home orders at the time of baseline data collection, only six remained so at the time of follow-up. This suggests that the TPB is an effective framework for predicting adherence to NPIs in the context of a rapidly evolving health threat.
To our knowledge, this is the first study to examine demographic and TPB-related moderators of the intention–behavior relationship in the context of COVID-19. Consistent with previous intention–behavior gap work [17, 19], participants who were older and whose intentions were more stable were more likely to follow through with their intentions to social distance. We also found that race was a significant moderator of this relationship, with non-White participants displaying a greater intention–behavior gap than White participants. This finding may be driven, in part, by racial disparities in the ability to telework [29]. These findings suggest that interventions aimed at strengthening the connection between social distancing intentions and actions may be especially beneficial among those with larger intention–behavior gaps (i.e., younger, less stable intentions, and people of color), particularly if non-psychological barriers to social distancing can be addressed concurrently. Interestingly, the largest differences in intention–behavior strength emerged at low levels of intentions, suggesting that disparities in the intention–behavior relationship by age, race, and intention stability are greatest among those with weaker intentions.
Surprisingly, neither subjective SES, income, nor education moderated the intention–behavior relationship. Although previous studies have suggested that the intention–behavior gap is greater among those with fewer resources [18], other studies have found no such effect [30]. These inconsistencies may be due to differences in measurement; for instance, our study utilized a subjective measure of SES, while others have employed more objective measures (e.g., occupation status, area-level Townsend deprivation index) [18]. Previous behavior and PBC also did not moderate this relationship, possibly due to the small amount of variance in previous behavior and PBC at baseline [16]. Future studies should identify effective strategies for translating intentions to social distance into action. For instance, setting action plans reduced the social distancing intention–behavior gap in an Australian sample [14], which is in line with previous research which suggests that individuals are more likely to follow through with their intentions when they have a concrete plan for when, where, and how they will act on them [31]. Connecting a goal intention with a specific situational cue to action can increase individuals’ likelihood of goal attainment as exposure to these situational cues serve to elicit behavioral response automatically [31].
Although the present study was longitudinal in nature, the COVID-19 pandemic is a continuously evolving public health threat. Thus, COVID-19-related cognitions and protective behavior may vary as the pandemic evolves (e.g., the emergence of new strains; [32]). Consistent with this, participants’ attitudes, subjective norms, intentions, and behaviors all fluctuated from baseline to follow-up 3 months later. Interestingly, although intentions increased over time, social distancing behavior decreased. That engagement in social distancing was lower at follow-up is to be expected, given that most statewide stay-at-home orders had been lifted by this time, and is not necessarily indicative of a lack of adherence to social distancing guidelines. At the same time, the increase in social distancing intentions is likely a result of the public health community’s emphasis on the importance of these measures, as well as an increase in the number of people who had direct experience with COVID-19. Studies should continue to examine determinants of social distancing in the coming months, especially as vaccine distribution begins to ramp up [32].
As access to vaccine doses continues to increase in the USA, it is important to note that for many countries–in particular poorer, developing nations–this inoculation process will take time. In fact, research suggests that nearly a quarter of the global population will not have access to a vaccine until at least 2022 [33], which is particularly concerning given the emergence of several more contagious variants of COVID-19. As such, it is likely that NPIs such as social distancing will continue to serve a critical role in mitigating the spread of COVID-19 in the coming years and in future pandemics. Findings suggest that policymakers should consider health communications that target attitudes, subjective norms, and perceptions of control when developing public health campaigns aimed at increasing social distancing compliance. Additionally, our findings regarding moderators of the intention–behavior relationship suggest that it may be beneficial to tailor these communications to certain demographic groups who are least likely to translate their social distancing intentions into actions, including younger adults and racial minorities. Future studies should examine whether these demographic variables also moderate the intention–behavior relationship in the context of COVID-19 vaccinations. It will be important to help individuals within these communities not only establish intentions to get vaccinated (i.e., make the decision), but also to help them establish plans to minimize barriers. Furthermore, it may be of particular importance for health communications to target constructs that were shown to decrease over time, such as subjective norms about social distancing. For instance, public health campaigns that state that the majority of community members are complying with social distancing measures (or, alternatively, an increasing number when compliers are in the minority) may be effective at promoting positive subjective norms about social distancing [34].
Findings should be interpreted in light of several limitations. Although the study’s prospective design allows for temporal precedence, without experimentally manipulating these constructs we are unable to make causal inferences. It is also important to note that our intention measure assessed intentions to social distance over the next 2 weeks, 1 month, 6 months, and year, and thus lacks correspondence with the follow-up timeframe (i.e., 3 months). As such, it is possible that the strength of the relationship between social distancing intentions and behavior may be underestimated. In addition, our measure of intention stability was confounded with behavior, as the second measure of intention was collected at the same time follow-up behavior was assessed. Future studies examining the moderating effect of intention stability on the intention–behavior relationship in the context of COVID-19 protective behaviors should measure intentions at two time-points prior to measuring behavior.
Additionally, although the present study included a composite measure of social distancing, social distancing encompasses a wide variety of behaviors that may differ in likelihood of compliance (e.g., maintaining social distance when out in public vs. visiting family and friends). Although beyond the scope of the present paper, future studies could involve a more nuanced examination of psychological determinants of social distancing compliance, by examining each behavior separately. Notably, social distancing is not the only COVID-19 mitigation NPI. For instance, frequent hand washing and consistent mask wearing are also critical. Although our sample was diverse in terms of age, gender, SES, and region, the majority of participants were White and college-educated, limiting generalizability. Lastly, although the SRMR and CFI of the path analytic model indicated good model-data fit, the RMSEA was slightly above the recommended cutoff of 0.08. This may be due to the fact that our path analytic model had two degrees of freedom, and the RMSEA penalizes for model complexity. In fact, Kenny, Kaniskan, and McCoach [35] recommend against computing the RMSEA for low degree of freedom models, as these models can have artificially large RMSEA values.
Conclusion
This is not the first pandemic the world has faced, and public health experts warn that it is likely not the last [36, 37]. As effective therapeutics and vaccines are usually not readily available when contagious viruses do emerge, it is important to identify psychosocial determinants of adherence to NPIs in order to reduce strain on the healthcare system and prevent incidences of severe illness and death. Findings suggest that targeting individuals’ attitudes, norms, and PBC may promote protective behaviors (e.g., social distancing), and strategies to strengthen the intention-behavior gap targeted to critical groups need to be developed.
Funding This study was funded by University of Colorado Boulder Internal Funds.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards The authors declare that they have no conflict of interest.
Ethical Approval All procedures were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1. Qualls N, Levitt A, Kanade N, et al. Community mitigation guidelines to prevent pandemic influenza – United States. MMWR Recomm Rep. 2007;66:1–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza. Available at https://www.who.int/influenza/publications/public_health_measures/publication/en/. Accessibility verified January 19, 2021.
- 3. Ahmed F, Zviedrite N, Uzicanin A. Effectiveness of workplace social distancing measures in reducing influenza transmission: a systematic review. BMC Public Health. 2017;18:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coroiu A, Moran C, Campbell T, Geller AC. Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLoS One. 2020;15:e0239795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pedersen MJ, Favero N. Social distancing during the COVID-19 pandemic: who are the present and future noncompliers? Public Adm Rev. 2020;80:805–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 7. Madden TJ, Ellen PS, Ajzen I. A comparison of the theory of planned behavior and the theory of reasoned action. Pers Soc Psychol Bull. 1992;18:3–9. [Google Scholar]
- 8. Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40:471–499. [DOI] [PubMed] [Google Scholar]
- 9. Corace KM, Srigley JA, Hargadon DP, et al. Using behavior change frameworks to improve healthcare worker influenza vaccination rates: a systematic review. Vaccine. 2016;34:3235–3242. [DOI] [PubMed] [Google Scholar]
- 10. McEachan RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health-related behaviours with the Theory of Planned Behaviour: a meta-analysis. Health Psychol Rev. 2011;5:97–144. [Google Scholar]
- 11. Starfelt Sutton LC, White KM. Predicting sun-protective intentions and behaviours using the theory of planned behaviour: a systematic review and meta-analysis. Psychol Health. 2016;31:1272–1292. [DOI] [PubMed] [Google Scholar]
- 12. Godbersen H, Hofmann LA, Ruiz-Fernández S. How people evaluate anti-corona measures for their social spheres: attitude, subjective norm, and perceived behavioral control. Front Psychol. 2020;11:567405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Norman P, Wilding S, Conner M. Reasoned action approach and compliance with recommended behaviours to prevent the transmission of the SARS-CoV-2 virus in the UK. Br J Health Psychol. 2020;25:1006–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hagger MS, Smith SR, Keech JJ, Moyers SA, Hamilton K. Predicting social distancing intention and behavior during the COVID-19 pandemic: an integrated social cognition model. Ann Behav Med. 2020;54:713–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sheeran P. Intention-behavior relations: a conceptual and empirical review. Eur Rev Soc Psychol. 2002;12:1–36. [Google Scholar]
- 16. Sheeran P, Webb TL. The intention-behavior gap. Soc Personal Psychol Compass. 2016;10:503–518. [Google Scholar]
- 17. Reuter T, Ziegelmann JP, Wiedemann AU, Lippke S, Schuz B, Aiken LS. Planning bridges the intention-behaviour gap: age makes a difference and strategy use explains why. Psychol Health. 2010;25:873–887. [DOI] [PubMed] [Google Scholar]
- 18. Conner M, McEachan R, Jackson C, McMillan B, Woolridge M, Lawton R. Moderating effect of socioeconomic status on the relationship between health cognitions and behaviors. Ann Behav Med. 2013;46:19–30. [DOI] [PubMed] [Google Scholar]
- 19. Sheeran P, Abraham C. Mediator of moderators: temporal stability of intention and the intention-behavior relation. Pers Soc Psychol Bull. 2003;29:205–215. [DOI] [PubMed] [Google Scholar]
- 20. Conner M, Sheeran P, Norman P, Armitage CJ. Temporal stability as a moderator of relationships in the Theory of Planned Behaviour. Br J Soc Psychol. 2000;39 Pt 4:469–493. [DOI] [PubMed] [Google Scholar]
- 21. Magnan RE, Gibson LP, Bryan AD. Cognitive and affective risk beliefs and their association with protective health beh avior in response to the novel health threat of COVID-19. J Behav Med. 2021:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moreland A, Herlihy C, Tynan MA, et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement - United States, March 1-May 31, 2020. Mortal Wkly Rep. 2020;69:1198–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. World Health Organization. WHO timeline - COVID-19. Available at https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19. Accessibility verified January 19, 2021.
- 24. Gardiner CK, Bryan AD. Monetary incentive interventions can enhance psychological factors related to fruit and vegetable consumption. Ann Behav Med. 2017;51:599–609. [DOI] [PubMed] [Google Scholar]
- 25. Adler N, Stewart J. The MacArthur scale of subjective social status. Available at https://macses.ucsf.edu/research/psychosocial/subjective.php. Accessibility verified January 19, 2021.
- 26. Aiken LS, West SG, Reno RR.. Multiple Regression: Testing and Interpreting Interactions. New York: Sage; 1991. [Google Scholar]
- 27. Rosseel Y. Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA). J Stat Softw. 2012;48:1–36. [Google Scholar]
- 28. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 29. U.S. Bureau of Labor Statistics. Workers who could work at home, did work at home, and were paid for work at home, by selected characteristics, averages for the period 2017–2018. Available at https://www.bls.gov/news.release/flex2.t01.htm. Accessibility verified January 19, 2021.
- 30. Vasiljevic M, Ng YL, Griffin SJ, Sutton S, Marteau TM. Is the intention-behaviour gap greater amongst the more deprived? A meta-analysis of five studies on physical activity, diet, and medication adherence in smoking cessation. Br J Health Psychol. 2016;21:11–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: A meta‐analysis of effects and processes. Adv Exp Soc Psychol. 2006;38:69–119. [Google Scholar]
- 32. Mahase E. Covid-19: UK approves Oxford vaccine as cases of new variant surge. Available at https://www.bmj.com/content/371/bmj.m4968. Accessibility verified January 19, 2021. [DOI] [PubMed]
- 33. So AD, Woo J. Reserving coronavirus disease 2019 vaccines for global access: Cross sectional analysis. BMJ. 2020;371:m4750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Yoeli E, Hoffman M, Rand DG, Nowak MA. Powering up with indirect reciprocity in a large-scale field experiment. Proc Natl Acad Sci U S A. 2013;110 Suppl 2:10424–10429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kenny DA, Kaniskan B, McCoach DB. The performance of RMSEA in models with small degrees of freedom. Sociol Methods Res. 2017;44:486–507. [Google Scholar]
- 36. Global Preparedness Monitoring Board. A world at risk: Annual report on global preparedness for health emergencies; 2019. Available at https://apps.who.int/gpmb/assets/annual_report/GPMB_annualreport_2019.pdf. Accessibility verified January 19, 2021.
- 37. Mason DJ, Friese CR. Protecting health care workers against COVID-19 – and being prepared for future pandemics. Available at https://jamanetwork.com/channels/health-forum/fullarticle/2763478. Accessibility verified January 19, 2021. [DOI] [PubMed]