ABSTRACT
Introduction
Little evidence of outcome is available on critically ill Coronavirus Disease 2019 (COVID-19) patients hospitalized in a field hospital. Our purpose was to report outcomes of critically ill COVID-19 patients after hospitalization in a field intensive care unit (ICU), established under military tents in a civil–military collaboration.
Methods
All patients with COVID-19-related acute respiratory distress syndrome (ARDS) admitted to the Military Health Service Field Intensive Care Unit in Mulhouse (France) between March 24, 2020, and May 7, 2020, were included in the study. Medical history and clinical and laboratory data were collected prospectively. The institutional review board of the French Society Anesthesia and Intensive Care approved the study.
Results
Forty-seven patients were hospitalized (37 men, median age 62 [54-67] years, Sequential Organ Failure Assessment score 7 [6-10] points, and Simplified Acute Physiology Score II score 39 [28-50] points) during the 45-day deployment of the field ICU. Median length of stay was 11 [6-15] days and median length of ventilation was 13 [7.5-21] days. At the end of the deployment, 25 (53%) patients went back home, 17 (37%) were still hospitalized, and 4 (9%) died. At hospital discharge, 40 (85%) patients were alive.
Conclusion
In this study, a military field ICU joined a regional civil hospital to manage a large cluster of COVID-19-related ARDS patients in Mulhouse, France. This report illustrates how military teams can support civil authorities in the provision of advanced critical care. Outcomes of patient suggest that this field hospital deployment was an effective adaptation during pandemic conditions.
INTRODUCTION
In December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused a wave of pneumonia cases in Wuhan, China. This disease is now known as Coronavirus Disease 2019 (COVID-19), which sometimes leads to acute respiratory distress syndrome (ARDS).1 Two months later, the disease became an epidemic and spread in European intensive care units (ICUs).2 On March 16, 2020, the French President Emmanuel Macron ordered the deployment of a military field ICU in Eastern France, where hospitals and, in particular, ICUs were overwhelmed.3 Healthcare services were saturated at that time in the whole region, reaching a crisis level of surge capacity. All hospitals had previously extended their critical care capacity in fixed facilities and patient transfers had already been performed. Supply chains were overwhelmed, medical equipment and drugs were lacking, and the number of caregivers was insufficient. New means were needed to deliver even more critical care, such as temporary facilities. In an unprecedented initiative, the French Military Health Service designed a Military Health Service Field Intensive Care Unit (Élément Militaire de Réanimation du Service de Santé des Armées: EMRSSA), providing a full and integrated intensive care system.4 The EMRSSA field hospital joined up with and supported the Emile Muller Hospital, an 850-bed general hospital in Mulhouse, Eastern France, which was the initial epicenter of the COVID-19 epidemic in France.3 The Emile Muller Hospital has a usual capacity of 36 ICU beds, located in a medical ICU (20 beds) and a surgical ICU (16 beds). Before the EMRSSA field hospital deployment, the Emile Muller Hospital had increased the number of its ICU beds from 36 to 62. Twenty-six additional ICU beds were located in operating rooms (ORs). On March 24, 2020, every ICU bed was occupied in the Emile Muller Hospital. The mission of the EMRSSA field hospital was to achieve two main objectives under strenuous conditions: firstly, to treat critically ill patients with COVID-19-related ARDS according to the best standards of care5; and secondly, to protect caregivers.6 The conception and deployment of the EMRSSA field hospital are shortly described elsewhere previously,7 but outcomes of the critically ill COVID-19 patients managed in this field hospital were not available at the time of publication. The hypothesis of the present study was that the management of COVID-19-related ARDS patients in the EMRSSA field hospital was associated with favorable outcomes, comparable to those observed in conventional ICUs. The objective of this follow-up article was to describe the outcomes of COVID-19-related ARDS patients managed in the EMRSSA field hospital during the COVID-19 pandemic in spring 2020.
MATERIALS AND METHODS
Population and Setting
This single-center observational study was performed during the deployment of the EMRSSA field hospital, from March 24 to May 7, 2020, in the Emile Muller Hospital. All consecutive patients admitted to the EMRSSA field hospital were included. The EMRSSA field hospital was designed to treat up to 30 critically ill patients simultaneously with a high standard of care, according to international guidelines.8 The EMRSSA field hospital was located in a parking lot in close proximity to the emergency department, ICU, and helicopter drop zone at distances of 200, 100 and 50 meters, respectively. The deployment of 25 tents required 1,170 square meters. The Medical Regiment prepared and deployed a military field hospital comprising three wards, a hospital pharmacy, a medical staff room, a restroom, a dressing room, and a headquarters tent. Each ward could receive eight patients. One ward, designated as a post-critical care ward, was extended to receive three more patients. Figure 1 shows a general overview of the EMRSSA field hospital.
FIGURE 1.
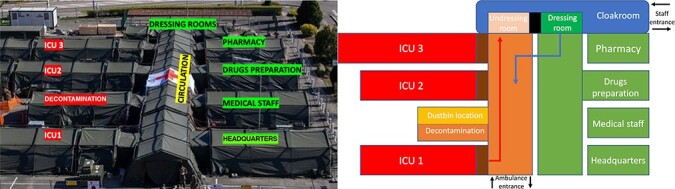
Left panel: aerial view of the EMRSSA field hospital; right panel: organization of the EMRSSA—protection zones.
Medical and paramedical staff comprised personnel from eight French military hospitals. Each ICU ward was staffed with one anesthesiologist/intensive care physician, three nurses (including one registered anesthesiology nurse), and three assistant nurses, following French guidelines on ICU structural and organizational requirements.9,10 The clinical staff was composed of 8 anesthesiologists/intensive care physicians, 34 nurses, and 18 assistant nurses. Two military pharmacists and three pharmacy dispensers were responsible for medical products supply. As the regional supply chain was also overwhelmed, the pharmacists were in permanent and direct contact with the French armed forces health products supply directorate, located in Orléans, which delivered all the durable and non-durable equipment requested, within 1 to 3 days. Medical support services included two medical imaging technicians with plain X-ray capability. A computed tomography scanner was available in the Emile Muller Hospital. A biomedical team (one biomedical engineer and two biomedical technicians) was in charge of the maintenance of biomedical equipment, including three high-capacity oxygen concentrators. Each concentrator could produce up to 125 L/min of oxygen. Two biological technicians coordinated biological tests (biochemistry, hematology, and microbiology) performed in the Emile Muller Hospital medical laboratory. Two physiotherapists performed chest physiotherapy and early mobilization in the EMRSSA field hospital. Finally, when appropriate, a head and neck surgeon (J.B.M.) supported by an OR nurse performed percutaneous tracheostomies.11 The EMRSSA medical director (P.P.) and the EMRSSA commander (J.E.), both experienced military anesthesiologists and intensivists, mentored the medical team and coordinated crisis management with the civilian medical staff of the Emile Muller Hospital.
The EMRSSA field hospital offered 30 supplementary beds in a fourth ICU integrated in the Emile Muller Hospital. A medical staff, composed of the head of every ICU (medical, surgical, OR, and EMRSSA) daily decided on the destination of all patients requiring intensive care. The EMRSSA field hospital offered no possibility for renal replacement therapy (RRT) or extra-corporal membranous oxygenation (ECMO). All patients admitted in the EMRSSA field hospital met the following conditions: intravenous sedation, tracheal intubation, and mechanical ventilation (MV). Respiratory support and sedation strategies followed current guidelines.12 If a patient admitted in the EMRSSA field hospital later needed ECMO or RRT, they were then transferred back to the conventional ICU. The medical staff discussed percutaneous tracheostomy for patients still requiring MV (more than two unsuccessful spontaneous breathing trials or one unsuccessful extubation), after improvement and stabilization of the respiratory condition (Pa/FiO2 > 150 and no need for neuromuscular blocking agent infusion or prone positioning for at least 96 hours). In case of indication for a tracheostomy, consent was obtained from the next of kin and the tracheostomy was performed at the bedside.
In agreement with the medical staff of the Emile Muller Hospital, a clinical pathway was designed to optimize utilization of ICU beds: emergency department (initial assessment and care); conventional ICU (beginning of ICU care); EMRSSA field hospital (until successful extubation or weaning from permanent MV in case of tracheostomy); post-ICU respiratory care (in case of tracheostomy, until decannulation); medical ward, until discharge to home or to long-term care facility. If the number of ICU beds was not sufficient in the Emile Muller Hospital, medical evacuation was organized by car, train, helicopter, or plane13 to available ICUs in the region, in France, or in neighboring countries (Germany, Luxembourg, and Switzerland).
Protection of the EMRSSA personnel was the second main objective of the mission. The field hospital was separated into three zones according to protection level: green zone on the right side comprising the right central corridor, the dressing room, pharmacy, drugs preparation, medical staff and headquarters (surgical mask); orange zone in the middle comprising the left central corridor, the undressing room and decontamination area (filtering facepiece 2 [FFP2] mask); and red zone on the left side comprising the 3 intensive care units (full personal protective equipment: FFP2 or FFP3 mask, gown, gloves, eye protection, and apron) (Fig. 1). As the EMRSSA was located under tents, it was not possible to generate and maintain a negative pressure. However, the available air conditioning devices included particulate filtration system. Surface decontamination was performed daily using a disinfectant detergent meeting NF14476 standards. The barrier between the red and orange zones consisted of two successive hermetic closures, present at the entrance of each ward to avoid contaminating the entire structure. A fence in the middle of the central corridor separated the green and orange zones. Circulation was permitted from the green to orange and red zones and between the orange and red zones, but it was forbidden from the orange to green zone without getting through the undressing room. A public health nurse was in charge of the definition and application of hygiene measures. Servicemen from the Medical Regiment systematically supervised donning and doffing.
Data Collection
Data were collected prospectively in an electronic medical record for daily medical reports. Data comprised the following
Demographic and clinical characteristics (age, gender, weight, height, body mass index, medical comorbidities, and usual severity scores)
Respiratory support assessment (Pa/FiO2, neuromuscular blocking agent infusion, prone positioning, nitric oxide inhalation, steroid injection, tracheostomy, and invasive MV time)
Other ICU-related treatments (intravenous sedation and vasopressor support) and specific treatments
Secondary infections (ventilator-associated pneumonia and line infection) and venous thromboembolism (deep venous thrombosis and pulmonary embolism)
Outcomes (length of stay, destination at EMRSSA discharge, and vital status at EMRSSA field hospital closure and at hospital discharge).
Statistical Analysis
Continuous variables are presented as median and interquartile range. Categorical variables are expressed as numbers and percentages. Analyses were performed with Microsoft Excel software.
Ethics and Consent
The institutional review board of the French Society Anesthesia and Intensive Care approved the study (Institutional review board number: 00010254-2020–115). Oral information was delivered to the patient’s next of kin, and an information sheet was given.
RESULTS
On March 24, 2020, the first patient was admitted in the EMRSSA field hospital. On March 29, 2020, 28 patients were present in the EMRSSA field hospital, while every ICU bed was occupied in the three other ICUs in the Emile Muller Hospital. From March 24 to May 7, 2020, a total of 47 patients were admitted to the EMRSSA field hospital, cumulating 603 ICU days. All patients were transferred from one of the three ICUs of the Emile Muller Hospital, after a median ICU stay of 3 (interquartile 1-4) days.
There were 37/47 (79%) male patients. At EMRSSA admission, their median (interquartile) age, and Sequential Organ Failure Assessment and Simplified Acute Physiology Score (SAPS) II scores were 62 (54-67) years, and 7 (6-10) and 39 (28-50), respectively.
Table I gives an overview of the patients respiratory status and the respiratory support treatment delivered. Table II shows other ICU-related treatments.
TABLE I.
Respiratory Support Assessment
| During the first 24 hours in EMRSSA | Available data, n | Median (IQR) |
|---|---|---|
| VT, mL/kg PBW | 42 | 6.4 (5.9-6.7) |
| Set PEEP, cm H2O | 47 | 12 (10-14) |
| Plateau pressure, cm H2O | 29 | 24 (22-28) |
| Driving pressure, cm H2O | 29 | 13 (10-14) |
| Static compliance, mL/cm H2O | 29 | 34 (28-45) |
| During entire EMRSSA stay | ||
| Lowest Pa/FiO2 ratio, median (IQR) | 47 | 128 (104-160) |
| NMBA infusion, n (%) | 47 | 32 (68) |
| Prone positioning, n (%) | 47 | 14 (30) |
| NO inhalation, n (%) | 47 | 1 (2) |
| Corticosteroid therapy, n (%) | 47 | 6 (13) |
| Length of MV, median (IQR), days | 47 | 9 (5-14) |
| Tracheostomy, n (%) | 47 | 18 (38) |
| Delay between tracheal intubation and tracheostomy, median (IQR), days | 18 | 12 (10-13) |
Abbreviations: EMRSSA, Élément Militaire de Réanimation du Service de Santé des Armées; IQR, interquartile range; MV, mechanical ventilation; NMBA, neuromuscular blocking agent; NO, nitric oxide; PBW, predicted body weight; PEEP, positive end-expiratory pressure; VT, tidal volume.
TABLE II.
Other ICU-Related and Specific Treatments
| Number of days with intravenous sedation | n (%) |
| Midazolam and/or propofol and/or sufentanil | 375 (62) |
| Clonidine alone | 88 (15) |
| None | 83 (14) |
| Missing data | 50 (8) |
| Vasopressor support | n (%) |
| Norepinephrine infusion on EMRSSA admission | 34 (72) |
| <0.1 mcg/kg/min | 10 (21) |
| >0.1 mcg/kg/min | 24 (51) |
| Length of infusion, median (IQR), days | 2 (1-5) |
| Specific treatments | n (%) |
| Hydroxychloroquine | 14 (30) |
| Lopinavir/Ritonavir | 3 (6) |
| Remdesivir | 1 (2) |
Abbreviations: EMRSSA, Élément Militaire de Réanimation du Service de Santé des Armées; ICU, intensive care unit; IQR, interquartile range.
Thirteen patients (28%) developed a ventilator-associated pneumonia and three a line infection (6%). Three patients (6%) presented a deep venous thrombosis and four a pulmonary embolism (9%).
Finally, the main outcomes for patients admitted to the EMRSSA field hospital are given in Table III.
TABLE III.
Outcomes
| Cumulative EMRSSA ICU stay, days | 603 |
| Length of stay in EMRSSA, median, days (IQR) | 11 (6-15) |
| Post-EMRSSA destination | n (%) |
| Post-respiratory ICU | 15 (32) |
| Emile Muller Hospital ICU | 6 (13) |
| Other ICU | 14 (30) |
| Medical ward | 11 (23) |
| Vital status and location on May 7, 2020 | n (%) |
| Alive, at home, or in long-term care facility | 26 (55) |
| Alive, medical ward, or post-ICU rehabilitation unit | 11 (24) |
| Alive, ICU | 6 (13) |
| Dead | 4 (9) |
| Vital status at hospital discharge | n (%) |
| Alive, at home, or in long-term care facility | 40 (85) |
| Dead | 7 (15) |
Abbreviations: EMRSSA, Élément Militaire de Réanimation du Service de Santé des Armées; ICU, intensive care unit; IQR, interquartile range.
DISCUSSION
This study is an original report detailing the unique experience of a field hospital dedicated exclusively to intensive care during the COVID-19 pandemic. This single-center prospective study reported 47 consecutive critically ill patients with COVID-19-related ARDS, managed in a 30-bed military field intensive care hospital. This report is an illustration of a civil–military collaboration providing advanced critical care.
By mid-March 2020, every hospital in Eastern France had all its ICU beds occupied, almost exclusively with COVID-19-related ARDS patients. All hospitals had already created new ICU beds, in particular transforming OR into ICU.14 Patient transfers were also performed, but became more and more challenging as the distance to a vacant ICU bed grew. In addition, to be performed safely, medical transfers of a critically ill patient require a stabilized clinical status and only moderate therapeutic needs.13 Therefore, both civilian and military health authorities decided to deploy a military intensive care field hospital in Mulhouse. Previous deployments of ICU beds in field hospitals have been reported, but were smaller with only 10 beds,15 were mainly deployed in war regions or post-earthquake areas,16 and concerned mostly trauma patients with shorter lengths of stay.17 To the best of our knowledge, this is the largest series in a field ICU during peacetime for a pandemic.
The clinical characteristics of the patients at their admission in the EMRSSA field hospital (median age 62; 79% men; median SAPS2 score 39) are comparable with other reports (median age 63; 60 to 82% men; SAPS2 score 37).2,18,19 The frequencies of hospital-acquired infections (ventilator-associated pneumonia 28% and line infection 6%) and thromboembolic complications (deep venous thrombosis 6% and pulmonary embolism 9%) observed in our cohort are consistent with other large critically ill COVID-19 patient cohorts. Grasselli et al. reported a ventilator-associated pneumonia frequency of 50% and a line infection of 10%.20 Schmidt et al. reported a deep venous thrombosis frequency of 8% and a pulmonary embolism frequency of 9%.19 On May 7, 2020, date of the EMRSSA field hospital closure, the overall 28-day mortality rate was 9%. In-hospital mortality rate was 15%, which is lower than mortality rates reported at the same time in conventional ICU in Europe (24 to 31%)18,19 or in ICU created in OR in the USA (41%).21 Patients admitted in the EMRSSA presented COVID-19-related ARDS with moderate needs for vasopressors. Patients with even more severe forms of COVID-19 such as those with an acute kidney injury requiring RRT or cardiogenic shock needing ECMO, stayed in the Emile Muller Hospital. These eligibility criteria for patient admission in the EMRSSA introduced a bias and could have contributed to the lower mortality rate observed in our cohort. The EMRSSA field hospital met several common points to other ICUs created in alternative care areas, such as ORs.21 Creating an ICU under a tent or in an OR implies architectural constraints, making it for example impossible to place patients in individual rooms. As Mittel et al., we chose to organize 12-hour shifts and to form specialized teams, such as a tracheostomy team, to secure this invasive intervention. As opposed to ICUs created in an OR, it was impossible to create a negative pressure atmosphere; therefore, a strict application of a rigorous hygiene protocol was performed. The mechanical ventilators were ICU-dedicated ventilators (Elisée 350, ResMed, Bella Vista, Australia) so that no adaptation had to be performed, contrary to anesthesia machines. The particular point concerning prone positioning in the EMRSSA field hospital was that the ICU beds did not include an electric motor and the bed height was not adjustable. Positioning a patient in the prone position required at least five caregivers. Every caregiver deployed in the EMRSSA was experienced in intensive care and therefore familiar with prone positioning. There was no dedicated team for prone positioning as seen elsewhere22 but the EMRSSA military caregivers were divided into fixed teams during the entire mission so that each member had an appropriate and fixed role.
The COVID-19-related ARDS patients are highly dependent and with huge therapeutic needs, in particular oxygen delivery and medications. Thus, an autonomous oxygen supply was provided by three high-capacity oxygen concentrators and an efficient on-site pharmacy service was organized. The EMRSSA field hospital pharmacy was located in the green zone (outside care units) and not placed directly in the care units.23 Medical prescriptions were electronic and sent on a printer situated in the drugs preparation tent, next to the pharmacy tent. A dedicated nurse was responsible of the preparation of the medications, which were then placed next to the entrances of the care units.
Confronted by a rapidly growing number of patients requiring MV, adaptive strategies were proposed to optimize the occupation of ICU beds.24 Physicians of the EMRSSA field hospital performed early tracheostomies to accelerate sedation and ventilation weaning.25 Recent guidelines concerning tracheostomies for COVID-19 patients support that it may be considered when prolonged MV is anticipated to improve ventilator-free days and shorter stay in the ICU.26 In order to limit the length of stay inside the EMRSSA field hospital, and more generally in the ICUs in Mulhouse’s hospitals, we decided to propose an early tracheostomy for patients with COVID-19. Although controversial, this strategy, also supported in other setting,27 allowed early transfers of patients to post-ICU stages for weaning from MV, including the use of home mechanical ventilators. Consequently, the Emile Muller Hospital organized a new 12-bed rehabilitation unit, with physicians and nurses trained in tracheostomy and ventilator weaning, where the patients were transferred as soon as MV was no longer needed.
The EMRSSA field hospital closed on May 7, 2020 for several reasons. First, the number of COVID-19 patients was decreasing at that time in Eastern France, due to increased government-lead infection control policies. The number of COVID-19-related ARDS patients was also decreasing, so there was no need for additive ICU beds in the region. On the contrary, other French regions faced increasing need for ICU beds due to a rising number of COVID-19-related ARDS patients. Just after the closure in Mulhouse, the EMRSSA field hospital was deployed in Mayotte, an island located in the Indian Ocean.28
Dealing with contagious patients and avoiding caregiver contamination in an austere environment was the second challenging point. The French Military Health Service had previous experience in preparing conventional ICU capacities to receive critically ill patients with a contagious disease such as Ebola virus.29 In the EMRSSA field hospital, a hygiene protocol had to be adapted, which was designed by a public health nurse, experienced in the treatment of Ebola virus under a military tent.30,31 The public health nurse also organized the training of the caregivers working in the EMRSSA field hospital. The training consisted in a one-hour instruction, given to every team before entering the ICUs. The instruction comprised a demonstration by the public health nurse of hand hygiene using alcohol-based hand sanitizer and the personal protection equipment (PPE) donning and doffing. Then, every caregiver was asked to repeat these hygiene skills, and then evaluated and corrected by the public health nurse. The PPE was composed of goggles, hood, coat, boots, gloves, and a FFP2 mask which is equivalent to an N95 respiratory. The PPEs were changed at least every 4 hours. The members of the EMRSSA field hospital underwent mandatory twice-daily checks on temperature and onset of clinical signs of acute respiratory infection. In case of suspicion, a nasopharyngeal sample was taken for reverse transcriptase-polymerase chain reaction in the Emile Muller Hospital. No COVID-19 contamination was diagnosed in the six caregivers who underwent reverse transcriptase-polymerase chain reaction testing for suspected COVID-19.
This study had several limitations. Firstly, it was a single-center study, and patients admitted to the EMRSSA field hospital were selected. All patients presented with COVID-19-related ARDS and received MV under intravenous sedation, but we were not able to perform RRT or ECMO due to the spartan conditions. Sharing this unique experience is of great interest in illustrating that it is possible to deal with 47 critically ill patients under military tents. This could be useful in future epidemic events. Secondly, the total number of patients may seem small, but all were critically ill, requiring intensive care under strenuous conditions. The fully integrated intensive care system proposed by the EMRSSA field hospital bears no comparison to other field hospitals that have been deployed during the COVID-19 outbreak, which dealt with patients presenting non-severe forms of COVID-19.32 Compared with other field hospitals such as Fangcang shelter hospitals32 or field hospitals implemented in convention centers,33 the EMRSSA field hospital does not need any construction and can be deployed rapidly nearly anywhere needed.
CONCLUSION
This study reported the sustained and resourceful activity of a military field ICU that integrated a regional civilian hospital to manage a large cluster of COVID-19-related ARDS patients in Mulhouse, Eastern France. Outcomes of COVID-19-related ARDS patients managed in the EMRSSA field hospital were favorable. This report illustrates how military teams can support civil authorities in the provision of advanced critical care. Further studies are ongoing to evaluate the efficacy of such medical organizations.
ACKNOWLEDGMENTS
The authors thank all the medical and technical teams from the French Military Health Service and the French Régiment Médical involved in the EMRSSA field hospital. The authors specially acknowledge Anne-FlorenceHoarau, Maelle Dussarat, Cloé Jacques-Sebastien, Erwan Mesdon, Pierre-Michel Baudouin, and Baptiste Legois who helped to collect the clinical data. Moreover, the authors pay a great tribute to the civilian ICU and medical teams from the Emile Muller Hospital: Dr Christian Meyer, Dr Odile Theissen, Dr Khaldoun Kuteifan, Dr Philippe Guiot, Dr Xavier Nazica, Dr Marc Noizet, and their collaborators.
Contributor Information
LTC Marc Danguy des Déserts, Intensive Care, Anesthesia, Emergency and Operating Theatre Department, Clermont Tonnerre Military Training Hospital, Brest 29240, France; EA3878 GETBO, University of Occidental Brittany, Brest 29238, France.
CPT Quentin Mathais, Intensive Care, Anesthesia, Burns and Operating Theatre Department, Sainte Anne Military Training Hospital, Toulon 83000, France.
LTC Jean Baptiste Morvan, Intensive Care, Anesthesia, Burns and Operating Theatre Department, Sainte Anne Military Training Hospital, Toulon 83000, France.
CPT Gwendoline Rager, Intensive Care, Anesthesia, Emergency and Operating Theatre Department, Robert Picqué Military Training Hospital, Villenave d’Ornon 33140, France.
MG Jacques Escarment, French Military Medical Academy, Paris 75005, France.
COL Pierre Pasquier, French Military Medical Academy, Paris 75005, France; Intensive Care, Anesthesia, Burns and Operating Theatre Department, Percy Military Training Hospital, Clamart 92140, France.
FUNDING
The authors received no financial support for the research, authorship, and/or publication of this article.
CONFLICT OF INTEREST STATEMENT
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
- 1. Guan W-J, Ni Z-Y, Hu Y, et al. : clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382(18): 1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grasselli G, Zangrillo A, Zanella A, et al. : Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 2020; 323(16): 1574–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kuteifan K, Pasquier P, Meyer C, Escarment J, Theissen O: The outbreak of COVID-19 in Mulhouse : hospital crisis management and deployment of military hospital during the outbreak of COVID-19 in Mulhouse, France. Ann Intensive Care 2020; 10(1): 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pasquier P, Luft A, Gillard J, et al. : How do we fight COVID-19? Military medical actions in the war against the COVID-19 pandemic in France. BMJ Mil Health 2020. 10.1136/bmjmilitary-2020-001569 [DOI] [PubMed] [Google Scholar]
- 5. Alhazzani W, Møller MH, Arabi YM, et al. : Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coro navirus disease 2019 (COVID-19). Intensive Care Med 2020; 46(5): 854–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Verbeek JH, Rajamaki B, Ijaz S, et al. : Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev 2020; 15(5): CD011621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Des Déserts MD, Mathais Q, Luft A, Escarment J, Pasquier P: Conception and deployment of a 30-bed field military intensive care hospital in Eastern France during the 2020 COVID-19 pandemic. Anaesth Crit Care Pain Med 2020; 39(3): 361–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sandrock CE: Care of the critically ill and injured during pandemics and disasters: groundbreaking results from the Task Force on Mass Critical Care. Chest 2014; 146(4): 881–3. [DOI] [PubMed] [Google Scholar]
- 9. Fourrier F, Boiteau R, Charbonneau P, et al. : 300 recommendations and guidelines on structural and organizational requirements for intensive care units. Réanimation 2012; 21(3): 523–39. [Google Scholar]
- 10. Valentin A, Ferdinande P, ESICM Working Group on Quality Improvement : Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Med 2011; 37(10): 1575. [DOI] [PubMed] [Google Scholar]
- 11. Schultz P, Morvan J-B, Fakhry N, et al. : French consensus regarding precautions during tracheostomy and post-tracheostomy care in the context of COVID-19 pandemic. Eur Ann Otorhinolaryngol Head Neck Dis 2020; 137(3): 167–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Marini JJ, Gattinoni L: Management of COVID-19 respiratory distress. JAMA 2020; 323(22): 2329–30. [DOI] [PubMed] [Google Scholar]
- 13. Beaussac M, Boutonnet M, Koch L, et al. : Oxygen management during collective aeromedical evacuation of 36 COVID-19 patients with ARDS. Mil Med 2020. milmed-2020.10.1093/milmed/usaa512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lefrant J-Y, Fischer M-O, Potier H, et al. : A national healthcare response to intensive care bed requirements during the COVID-19 outbreak in France. Anaesth Crit Care Pain Med 2020; 39(6): 709–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lockey DJ, Nordmann GR, Field JM, Clough D, Henning JDR: The deployment of an intensive care facility with a military field hospital to the 2003 conflict in Iraq. Resuscitation 2004; 62(3): 261–5. [DOI] [PubMed] [Google Scholar]
- 16. Halpern P, Rosen B, Carasso S, et al. : Intensive care in a field hospital in an urban disaster area: lessons from the August 1999 earthquake in Turkey. Crit Care Med 2003; 31(5): 1410–4. [DOI] [PubMed] [Google Scholar]
- 17. Roberts MJ, Fox MA, Hamilton-Davies C, Dowson S: The experience of the intensive care unit in a British Army field hospital during the 2003 Gulf conflict. J R Army Med Corps 2003; 149(4): 284–90. [DOI] [PubMed] [Google Scholar]
- 18. Thomson RJ, Hunter J, Dutton J, et al. : Clinical characteristics and outcomes of critically ill patients with COVID-19 admitted to an intensive care unit in London: a prospective observational cohort study. PLoS One 2020; 15(12): e0243710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schmidt M, Hajage D, Demoule A, et al. : Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med 2021; 47(1): 60–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Grasselli G, Scaravilli V, Mangioni D, et al. : Hospital-acquired infections in critically ill patients with COVID-19. Chest 2021. 10.1016/j.chest.2021.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mittel AM, Panzer O, Wang DS, et al. : Logistical considerations and clinical outcomes associated with converting operating rooms into an intensive care unit during the coronavirus disease 2019 pandemic in a New York City Hospital. Anesth Analg 2021; 132(5): 1182–90. [DOI] [PubMed] [Google Scholar]
- 22. Shelhamer MC, Wesson PD, Solari IL, et al. : Prone positioning in moderate to severe acute respiratory distress syndrome due to COVID-19: a cohort study and analysis of physiology. J Intensive Care Med 2021; 36(2): 241–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wallis N, Gust C, Porter E, Gilchrist N, Amaral A: Implementation of field hospital pharmacy services during the COVID-19 pandemic. Am J Health Syst Pharm 2020; 77(19): 1547–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vincent J-L, Creteur J: Ethical aspects of the COVID-19 crisis: how to deal with an overwhelming shortage of acute beds. Eur Heart J Acute Cardiovasc Care 2020; 9(3): 248–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rovira A, Dawson D, Walker A, et al. : Tracheostomy care and decannulation during the COVID-19 pandemic. A multidisciplinary clinical practice guideline. Eur Arch Otorhinolaryngol 2021; 278(2): 313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lamb CR, Desai NR, Angel L, et al. : Use of tracheostomy during the COVID-19 pandemic. Chest 2020; 158(4): 1499–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kwak PE, Connors JR, Benedict PA, et al. : Early outcomes from early tracheostomy for patients with COVID-19. JAMA Otolaryngol Head Neck Surg 2021; 147(3): 239–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Marolleau B, Rias M, Delahaye A, Aillet L, Weibel M, Romanat P: The military intensive care field hospital, a unique experience in the fight against covid-19. Soins Rev Ref Infirm 2020; 65(849): 22–7. [DOI] [PubMed] [Google Scholar]
- 29. Dubost C, Pasquier P, Kearns K, et al. : Preparation of an intensive care unit in France for the reception of a confirmed case of Ebola virus infection. Anaesth Crit Care Pain Med 2015; 34(6): 349–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bordes J, Gagnon N, Cotte J, et al. : Caring for critically ill patients infected with the Ebola virus: logistic and human challenges. Chest 2015; 148(2): e64–5. [DOI] [PubMed] [Google Scholar]
- 31. Levin AB, Ball CM, Featherstone PJ: From cholera to COVID-19: how pandemics have shaped the development of anaesthesia and intensive care medicine. Anaesth Intensive Care 2020; 48(3_Suppl): 28–38. [DOI] [PubMed] [Google Scholar]
- 32. Chen S, Zhang Z, Yang J, et al. : Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet 2020; 395(10232): 1305–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Brown DR, Hennecke P, Nottebrock D, Dhillon P: Vancouver Convention Health Centre (COVID-19 response): planning, implementation, and four lessons learned. Am J Disaster Med 2020; 15(2): 143–8. [DOI] [PubMed] [Google Scholar]


