Abstract
Given the global impact of coronavirus disease 2019 (COVID-19) on mental and physical health, we examined young adults’ changes in mental health, intimate relationship quality, alcohol use and weight-related behaviors during COVID-19 and their correlates (depressive symptoms, resilience, social context and COVID-19-related factors). We analyzed data from a longitudinal study of 1082 young adults across six metropolitan areas (Mage = 24.76 ± 4.70; 51.8% female; 73.6% White and 12.5% Hispanic), using multivariate linear regressions for continuous outcomes (magnitude of mental health impact) and logistic regressions for categorical outcomes (decreased relationship quality, physical activity and nutrition and increased alcohol use and sedentary behavior). Of five negative mental health impacts assessed, participants reported experiencing an average of 3.54 (SD = 5.46), experiencing more correlated with increased childcare responsibilities and lower resilience. Additionally, 23.6% of those in relationships experienced negative relationship impact, 41.3% increased alcohol use, 47.2% decreased physical activity, 74.0% were more sedentary and 34.7% experienced poorer nutrition, all of which was predicted by greater depressive symptoms. Additionally, lower resilience predicted negative relationship impact and poorer nutrition and social context/roles correlated with various outcomes (e.g. relationships and alcohol use). Interventions to reduce negative health behaviors given societal stressors should address key psychosocial and situational factors, including depressive symptoms and resilience.
Introduction
In early 2020, coronavirus disease 2019 (COVID-19) spread rapidly across the United States and by the end of March 2020, more than half of US states mandated stay-at-home orders to stop the spread of the virus [1]. Public health efforts to mitigate the spread of the disease (e.g. social distancing) led to societal stressors (e.g. social isolation, job loss and economic devastation), potentially related to poorer mental health outcomes, strained social relationships and decreases in healthy behaviors (e.g. physical activity and healthy eating) [2–4].
The uncertainty of the pandemic along with exposure to increased pandemic-related information and greater social isolation can adversely affect individuals’ mental health [4]. Indeed, individuals have reported increases in symptoms of anxiety, depression, fear and stress during COVID-19 [4, 5]. Despite the lower rates of mortality and illness severity among young people infected with COVID-19, younger individuals have reported more adverse psychological consequences (e.g. psychological distress, anxiety and depression) as a result of COVID-19 [6, 7].
Unfortunately, this psychological distress has been associated with a range of negative outcomes, including decreased intimate partner relationship quality [8, 9]. A high-quality romantic relationship may be a resource when coping with COVID-19-related stress [10]; however, maintaining a high-quality relationship during COVID-19 may be challenging, as individuals report greater negative evaluations of their relationship and more negative communication patterns with their partner during times of high-level stress [11, 12]. Compared to older adults, young adults are at particular risk for experiencing poorer romantic relationship quality during times of stress [13].
In addition, psychological distress is related to greater engagement in negative health behaviors. Stress—and poor mental health more globally—is a well-documented predictor of alcohol consumption [14], potentially to self-medicate [15]. In addition, individuals with greater psychological distress typically report lower levels of physical activities [16], as stress impairs efforts to be physically active [16, 17]. Experiencing stress has also been linked to poorer nutrition via various mechanisms [18, 19], for example, overeating foods rich in sugar may result in short-term increases in positive mood [20]. Engaging in negative health behaviors is particularly concerning given their potential impact on COVID-19-related risks and outcomes. Alcohol use, low physical activity and poorer nutrition weaken the immune system, increase inflammation and place individuals at greater risk of heart disease, diabetes and lung disease, which are risk factors for contracting COVID-19 and experiencing worsened outcomes [21–24].
Research is needed to document who is at greatest risk for increases in negative health behaviors during COVID-19. Prior research suggests that increases in anxiety and depression are associated with being female [4, 25, 26], younger in age [25], having a friend or relative diagnosed with COVID-19 [4], lower family income [27], less social support [27] and being unemployed [26]. Additionally, poorer romantic relationship quality has been associated with greater social isolation, financial strain and stress brought on by COVID-19 [28]. Additionally, increased alcohol use has been associated with greater COVID-related stress [29], greater decreases in physical activity and increases in sedentary behavior have been associated with being male and younger in age [30], and increased unhealthy eating has been associated with greater fear of COVID-19-related disease and death [31]. Given the recency of these circumstances, the research is currently limited, particularly regarding the broader range of risk and protective factors related to a range of negative health behaviors assessed in a single study.
Given the aforementioned literature and the need to expand our understanding of the impact of COVID-19 on individual risk for negative health behaviors, the current study draws from social cognitive theory (SCT) [32] to examine the risk and protective factors for changes in health behaviors during COVID-19. The SCT suggests that individuals vary in their risk for engaging in negative health behaviors as a result of dynamic intrapersonal (e.g. mental health) and interpersonal factors (e.g. social assets) [32]. In this study, we draw upon the literature that indicates that negative health behaviors are associated with sociodemographic characteristics [4, 25, 26, 30], one’s immediate social context (i.e. household composition and social roles [27], employment/financial factors [26–28]) and psychological factors (e.g. depression) [14, 16, 18, 19]. Thus, we examined (i) self-reported change in health behaviors (i.e. mental health impact, decreased relationship quality, increased alcohol use, decreased physical activity, increased sedentary behavior and decreased nutritional quality) during COVID-19 and (ii) sociodemographics, social context (i.e. household composition), employment/financial factors, resilience and depressive symptoms as risk factors for changes in health behaviors during COVID-19.
Methods
Study design
This study analyzed survey data among young adults (aged 18–34 years) participating in a 2-year, five-wave longitudinal cohort study, the Vape shop Advertising, Place characteristics and Effects Surveillance (VAPES) study. VAPES examines the vape retail environment and its impact on e-cigarette use, drawing participants from six metropolitan statistical areas (MSAs: Atlanta, Boston, Minneapolis, Oklahoma City, San Diego and Seattle) with varied tobacco and marijuana legislative contexts [33]. Bi-annual survey assessments began in Fall 2018. This study was approved by the Emory University Institutional Review Board.
Participants and recruitment
Potential participants were recruited via social media in Fall 2018 and were assessed biannually. Participant eligibility criteria were (i) 18–34 years old; (ii) residing in zip codes of the six aforementioned MSAs and (iii) English speaking. Purposive, quota-based sampling was also used to ensure sufficient proportions of the sample representing e-cigarette and cigarette users and to obtain roughly equal numbers of men and women and 40% racial/ethnic minority to explore use within subgroups. To obtain this sample, ads posted on Facebook and Reddit targeted individuals (i) using indicators reflecting those within the eligible age range and geographical locations (within 15 miles of their respective MSAs); (ii) by identifying work groups or activities of interest that appeal to young adults (e.g. sports/athletics, entertainment, arts, lifestyle and technology), as well as tobacco-related interests (e.g. Marlboro, Juul, Swisher Sweets) and (iii) by posting advertisements including images of young adults of diverse racial/ethnic backgrounds socializing in bars and/or outdoor spaces, young adult professionals in professional work settings, etc.
Once a potential participant clicked on an ad (e.g. ‘Help researchers learn more about what young adults in your city think about tobacco products!’), they were directed to a webpage with a study description and consent form. Once individuals consented, they were screened for eligibility. This screener also included questions regarding sex, race, ethnicity and past 30-day use of e-cigarettes and cigarettes, which were used to facilitate reaching recruitment targets of subgroups in each MSA (i.e. limiting participation among specific subgroups once their target enrollment was reached). Enrollment varied for each MSA, and thus subgroup enrollment was capped by MSA. Eligible individuals allowed to advance were then routed to complete the online baseline (Wave 1) survey (administered via SurveyGizmo). Upon the completion of the survey, participants were notified that, 7 days after completing the baseline survey, they would be asked to confirm their participation by clicking a ‘confirm’ button included in an email sent to them. The email reiterated study procedures and timeline. Once participants clicked ‘confirm,’ they were officially enrolled into the study and emailed their first incentive in the form of a $10 Amazon electronic gift card.
The participant flowchart is included in Fig. 1 and briefly described here. The duration of the recruitment period ranged from 87 to 104 days across the six MSAs. Of the 10 433 Facebook and Reddit users who clicked on ads, 9847 consented, of which 2751 (27.9%) were not allowed to advance because they were either (i) ineligible (n = 1427) and/or (ii) excluded in order to reach subgroup target enrollment (n = 1279). Of those allowed to advance to the survey, the proportion of completers versus partial completers was 48.8% (3460/7096) versus 51.2% (3635/7096). Partial completes were deemed ineligible for the remainder of the study; the majority of partial completers (n = 2469, 67.9%) completed only the initial sociodemographic section of the survey. Of the 3460 who completed the baseline survey, 3006 (86.9%) confirmed participation at the 7-day follow-up.
Fig. 1.
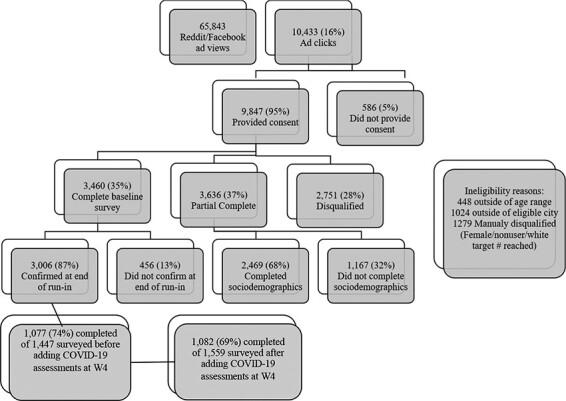
Participant recruitment flowchart.
This study uses data from Wave 3 (W3; Fall 2019) and Wave 4 (W4; Spring 2020). W4 data collection was launched in late January 2020; we interrupted data collection in mid-March to add questions specific to COVID-19. Thus, roughly half of participants (n = 1,559) were invited to complete the W4 assessment after these questions were added. The analytic sample was restricted to the 1082 participants (69.4% of the 1,559) with complete data related to COVID-19 at W4 and factors from W3. Of the 1082 participants in the analytic sample, 21.5% were current cigarette users and 26.6% were current e-cigarette users.
Measures
Outcomes
Outcomes in this study included mental health impact and relationship, alcohol use and weight-related behavior impacts. To assess ‘mental health impact’, participants completed five items assessing mental health, including ‘Compared to before COVID-19, are you doing more or less of the following: feeling down or depressed? (mental health impact item 1) feeling anxious or stressed out?’ (mental health impact item 2). Response options included: much more, somewhat more, no different, somewhat less, much less, not applicable (which was recoded as ‘no different’) and prefer not to answer. Participants were also asked, ‘To what extent do you agree or disagree with the following statements: The COVID-19 pandemic: (i) has been (or was) extremely stressful for me (mental health impact item 3); (ii) distracted me from doing other important things in my life (mental health impact item 4); and (iii) made me feel very lonely and distant from people’ (mental health impact item 5). Response options included strongly disagree, somewhat disagree, neutral/no opinion, somewhat agree and strongly agree. We created an overall number of mental health impact score by adding the total number of ‘more’ (much or somewhat) and ‘agree’ (strongly or somewhat); thus, individuals had scores ranging from 0 to 5 (Cronbach’s α = 0.72). (We examined this as an overall score of 0 = much less/strongly disagree to 4 = much more/strongly agree for each item and then totaled for a possible range of 0 to 20; however, associations were largely similar, and Cronbach’s α = 0.79 and correlation with number of mental health impacts was 0.90. Thus, for interpretability, we chose to use the number of mental health impacts.)
To assess ‘impact on quality of intimate relationship’, at W4, participants were asked, ‘How did/has COVID-19 impact[ed] your relationship with your partner (intimate relationship)?’ Response options included much worse, somewhat worse, no different, somewhat better, much better, not applicable or prefer not to answer. Responses were then recoded as 1 = negative outcome (i.e. somewhat/much worse) versus 0 (other responses). To assess ‘alcohol use and weight-related behavior impact’, participants were also asked, ‘Compared to before COVID-19, are you doing more or less of the following: drinking alcohol (including beer, wine, spirits)? engaging in physical activity (e.g. brisk walking, jogging, biking)? being sedentary (sitting/lying down when you are not sleeping)? eating a healthy, well-balanced diet?’ Response options included much more, somewhat more, no different, somewhat less, much less, not applicable (which was recoded as ‘no different’) and prefer not to answer. Responses were then recoded as 1 = negative outcomes (i.e. somewhat/much more for alcohol use and sedentary behavior; somewhat/much less for physical activity and healthy eating) versus 0 (other responses).
Independent variables
At W4, we assessed various ‘situational factors’. Participants were asked to report their current level of restrictions (no restrictions, shelter-in-place, quarantine/self-isolation and any positive COVID-19 tests in household). We also asked who else currently lived in the household (no one, roommates/friends, parents/guardians, siblings, spouse/romantic partner, children, extended family and other). To assess employment/financial factors/stressors, participants were asked to report whether they were currently a college student and their current work situation (enrolled as a college student; continued to work outside of the home; was working outside of the home/now working from home; laid off; was working at home/continues to and not working before COVID-19). We also assessed financial stressors since COVID-19 (i.e. personal loss of employment or income; loss of employment or income of a household member [or of a parent if still receiving support from parents]; more household financial problems). Participants were also asked if they took on more responsibility for caring for children since COVID-19.
Regarding ‘psychosocial factors’, ‘resilience’ was assessed at W3 using the 6-item Brief Resilience Scale, assessing individuals’ ability to cope with difficulties (1 = Strongly disagree to 5 = Strongly agree; score range 1–5; Cronbach’s alpha = 0.87) [34]. ‘Depressive symptoms’ were assessed at W3 and W4 with the Patient Health Questionnaire—2 item (PHQ-2), which assesses symptoms in the past 2 weeks (0 = not at all to 3 = nearly every day; score range 0–6; Cronbach’s alpha = 0.87) [35]. The PHQ-2 change scores were created by subtracting W3 scores from W4 scores.
Covariates
At baseline (W1), we assessed ‘sociodemographics’. Specifically, participants were asked to report their age, sex, sexual orientation, race and ethnicity.
Data analysis
Descriptive statistics were used to characterize the sample in terms of sociodemographics, situational factors, mental health impact, changes in relationship quality, alcohol use and weight-related behaviors. Then, multivariable regression models were examined for each outcome. We first examined models predicting mental health impact and PHQ-2 change, including the sociodemographic and situational factors, as well as resilience as the single psychosocial factor. Binary logistic regression was then conducted for each categorical variable including decreased relationship quality, increased alcohol use, decreased physical activity, increased sedentary behavior and decreased nutritional quality, to assess their correlates (i.e. sociodemographic and situational factors, as well as resilience and PHQ-2 change as psychosocial factors). We also conducted these models using multilevel modeling to account for the hierarchical structure of the data (i.e. clustering of young adults within each MSA); all intra-class correlations ranged from 0 to 0.01 for each outcome within MSA, and findings were not significantly different. Therefore, we reported the results based on the multivariate regression models. All analyses were conducted using SPSS version 26, with a significance level of P < 0.05.
Results
Participant characteristics
Among all participants included in these analyses (n = 1,082), participants were 24.77 years old on average (SD = 4.68), 45.7% male, 32.1% sexual minority, 4.0% Black, 12.4% Asian and 12.6% Hispanic (Table I). Additionally, 17.1% of participants reported being laid off from their job due to COVID-19.
Table I.
Participant characteristics and COVID-19 related factors
| Sociodemographics | n (%) or M (SD) |
|---|---|
| MSA, n (%) | |
| Atlanta | 72 (6.7) |
| Boston | 198 (18.3) |
| Minneapolis | 250 (23.1) |
| Oklahoma City | 128 (11.8) |
| San Diego | 208 (19.2) |
| Seattle | 226 (20.9) |
| Age, M (SD) | 24.77 (4.68) |
| Sex, n (%) | |
| Male | 494 (45.7) |
| Female | 556 (51.4) |
| Other | 32 (3.0) |
| Sexual minority, n (%) | 347 (32.1) |
| Race, n (%) | |
| White | 793 (73.3) |
| Black | 43 (4.0) |
| Asian | 134 (12.4) |
| Other | 112 (10.4) |
| Hispanic, n (%) | 136 (12.6) |
| Situational factors | |
| Household composition, n (%) | |
| Live alone | 161 (14.9) |
| Roommates/friends | 230 (21.2) |
| Parents/guardians | 294 (27.1) |
| Romantic partner | 457 (42.2) |
| Children | 150 (13.8) |
| Employment/financial factors, n (%) | |
| College student | 398 (36.8) |
| Continue work outside home | 202 (18.6) |
| Switched to work from home | 424 (39.1) |
| Laid off | 185 (17.1) |
| Continue work from home | 68 (6.3) |
| Not working before COVID-19 | 194 (17.9) |
| Any household financial strain | 617 (57.0) |
| Increased childcare responsibility | 109 (10.1) |
| Psychosocial factors, M (SD) | |
| Resilience | 3.36 (0.91) |
| W3 Patient Health Questionnaire −2 score | 1.71 (1.72) |
| W4 Patient Health Questionnaire −2 score | 2.10 (1.74) |
| Patient Health Questionnaire −2 change | 0.38 (1.80) |
| Mental health impact, n (%) | |
| Increased feeling down or depressed | 688 (63.9) |
| Increased feeling anxious or stressed out | 786 (73.0) |
| Increased COVID-related stress | 802 (74.1) |
| Increased distraction | 800 (73.9) |
| Increased feeling lonely/distant | 741 (68.4) |
| Overall sum of mental health impacts, M (SD) | 3.54 (5.46) |
| Negative impact on intimate partner relationship (N/A = 319), n (%) | 233 (23.6) |
| Increased alcohol use, n (%) | 446 (41.3) |
| Weight-related behavior impact, n (%) | |
| Decreased physical activity | 508 (47.2) |
| Increased sedentary behavior | 796 (74.0) |
| Decreased nutritional quality | 373 (34.7) |
Race categories represent individuals identifying as both Hispanic and non-Hispanic.
All participants except 1.3% (n = 14) reported living restrictions (e.g. shelter-in-place, quarantine), among six who reported that they were living with someone who tested positive; one had tested positive. Overall, 57.0% (n = 617) reported household financial strain (i.e. loss of employment and income), 10.1% (n = 109) reported taking on more responsibility for childcare and 41.8% (n = 452) reported increased food insecurity. The largest proportion of the sample reported living with a romantic partner (n = 457) that largely accounted for homes with children (n = 150), followed by living with parents (n = 294), which largely accounted for homes with siblings (n = 171) and/or extended family (n = 31), roommates/friends (n = 230) and alone (n = 161). At W3, average scores for resilience and PHQ-2 were 3.36 (SD = 0.91) and 1.71 (1.72), respectively. Average change in PHQ-2 was an increase of 0.38 (SD = 1.80). Exploratory analyses indicated that greater increases in PHQ-2 scores from W3 to W4 were predicted by being Asian (B = 0.38, P = 0.039), not living with parents/guardians (B = −0.045, P = 0.030), experiencing financial strain (B = 0.35, P = 0.007), and increased childcare responsibility (B = 0.23, P < 0.001; Adjusted R-square = 0.024).
Regarding outcome variables, 5.9% of participants reported 0 mental health impacts, 7.3% reported 1, 12.4% reported 2, 15.1% reported 3, 20.4% reported 4 and 38.9% reported 5. Participants reported between 3 and 4 adverse mental health impacts on average. Additionally, 23.6% reported experiencing decreases in intimate partner relationship quality, 41.3% of participants reported increasing their alcohol use, 47.2% reported decreased physical activity, 74.0% reported increased sedentary behavior and 34.7% reported decreased nutritional quality.
Multivariable regression results
With regard to changes in mental health, relationship quality and alcohol use (Table II), multivariable regression indicated that women, sexual minorities and Blacks (relative to Whites) and individuals with increased childcare responsibilities reported greater mental health impacts, whereas individuals with greater resilience reported fewer mental health impacts due to COVID-19. Non-Hispanics, individuals who do not live with their romantic partner, individuals with lower levels of resilience and those with greater increases in depressive symptoms were more likely to report decreased relationship quality since COVID-19. Whites (relative to Asians), individuals living with a romantic partner and without children, individuals with increases in childcare responsibility and those with greater increases in depressive symptoms were more likely to increase their alcohol use due to COVID-19.
Table II.
Regression analyses identifying correlates of mental health impact, increased alcohol use, and negative impact on intimate partner relationship
| Greater negative mental Health Impacta | Negative relationship impact (yes vs. no)a | Increased alcohol use (yes vs. no) | |||||||
| Sociodemographics | B | SE | P | OR | CI | P | OR | CI | P |
| Age | −0.02 | 1.01 | 0.148 | 1.01 | 0.96, 1.07 | 0.613 | 0.99 | 0.95, 1.02 | 0.485 |
| Male | −0.44 | 1.12 | <0.001 | 1.12 | 0.76, 1.63 | 0.579 | 0.99 | 0.75, 1.30 | 0.929 |
| Sexual minority | 0.30 | 0.82 | 0.005 | 0.82 | 0.55, 1.24 | 0.353 | 1.20 | 0.90, 1.61 | 0.216 |
| Race (ref: White) | |||||||||
| Black | −0.65 | 0.49 | 0.010 | 0.49 | 0.16, 1.49 | 0.207 | 0.66 | 0.32, 1.36 | 0.259 |
| Asian | 0.11 | 0.71 | 0.460 | 0.71 | 0.39, 1.27 | 0.247 | 0.61 | 0.39, 0.94 | 0.024 |
| Other | −0.08 | 1.19 | 0.610 | 1.19 | 0.64, 2.19 | 0.589 | 0.93 | 0.59, 1.46 | 0.740 |
| Hispanic | −0.21 | 0.52 | 0.168 | 0.52 | 0.29, 0.94 | 0.030 | 0.99 | 0.65, 1.51 | 0.954 |
| Household composition | |||||||||
| Live alone | −0.26 | 0.47 | 0.205 | 0.47 | 0.21, 1.04 | 0.062 | 1.03 | 0.59, 1.82 | 0.917 |
| Roommates/friends | −0.07 | 0.96 | 0.664 | 0.96 | 0.52, 1.78 | 0.897 | 1.28 | 0.81, 2.04 | 0.296 |
| Parents/guardians | −0.21 | 1.06 | 0.221 | 1.06 | 0.56, 2.03 | 0.859 | 0.65 | 0.40. 1.05 | 0.080 |
| Romantic partner | −0.01 | 0.23 | 0.977 | 0.23 | 0.12, 0.41 | <0.001 | 1.84 | 1.18, 2.89 | 0.008 |
| Children | −0.31 | 0.90 | 0.100 | 0.90 | 0.47, 1.74 | 0.756 | 0.41 | 0.24, 0.70 | 0.001 |
| Employment/financial factors | |||||||||
| College student | 0.11 | 1.07 | 0.331 | 1.07 | 0.70, 1.65 | 0.748 | 0.95 | 0.69, 1.31 | 0.751 |
| Continue work outside of home | −0.20 | 0.75 | 0.145 | 0.75 | 0.45, 1.26 | 0.278 | 0.75 | 0.51, 1.09 | 0.132 |
| Switched to work from home | 0.11 | 0.98 | 0.323 | 0.98 | 0.64, 1.49 | 0.907 | 1.12 | 0.81, 1.53 | 0.495 |
| Laid off | 0.27 | 0.68 | 0.066 | 0.68 | 0.39, 1.19 | 0.175 | 1.47 | 0.98, 2.20 | 0.063 |
| Any household financial strain | 0.10 | 1.31 | 0.353 | 1.31 | 0.88, 1.97 | 0.185 | 1.03 | 0.76, 1.39 | 0.845 |
| Increased childcare responsibility | 0.51 | 1.70 | 0.011 | 1.70 | 0.86, 3.36 | 0.129 | 2.12 | 1.22, 3.69 | 0.008 |
| Resilience | −0.30 | 0.67 | <0.001 | 0.67 | 0.54, 0.83 | <0.001 | 0.91 | 0.79, 1.06 | 0.233 |
| PHQ-2 change | – | 1.32 | – | 1.32 | 1.19, 1.46 | <0.001 | 1.13 | 1.05, 1.22 | 0.001 |
| R-square | 0.105 | 0.207 | 0.099 | ||||||
Adjusted R-square for mental health impact (per linear regression); Nagelkerke R-square for alcohol use and relationship quality (per binary logistic regression).
Note. All models are adjusted for the number of terms in the model.
Note. Significant P-values are noted in italics.
Regarding physical activity, sedentary behavior and nutritional quality (Table III), findings indicated that males, non-Hispanics and individuals with greater increases in depressive symptoms were more likely to decrease their physical activity, whereas younger adults, non-Hispanics, college students, individuals who switched to working from home and individuals with greater increases in depressive symptoms were more likely to increase their sedentary behavior. Finally, sexual minorities, individuals with lower levels of resilience and individuals with greater increases in depressive symptoms were more likely to report decreased nutritional quality since COVID-19.
Table III.
Binary logistic regression analyses identifying correlates of weight-related behavior impact
| Decreased physical activity (yes vs. no) | Increased sedentary behavior (yes vs. no) | Decreased nutritional quality (yes vs. no) | |||||||
| Sociodemographics | OR | CI | P | OR | CI | P | OR | CI | P |
| Age | 1.00 | 0.97, 1.04 | 0.857 | 0.95 | 0.91, 0.99 | 0.007 | 1.00 | 0.96, 1.04 | 0.908 |
| Male | 1.36 | 1.04, 1.78 | 0.026 | 1.01 | 0.73, 1.39 | 0.963 | 0.79 | 0.59, 1.06 | 0.119 |
| Sexual minority | 1.16 | 0.87, 1.55 | 0.300 | 1.30 | 0.91, 1.85 | 0.146 | 1.40 | 1.04, 1.88 | 0.029 |
| Race (ref: White) | |||||||||
| Black | 1.06 | 0.53, 2.09 | 0.875 | 1.20 | 0.54, 2.68 | 0.656 | 0.64 | 0.29, 1.43 | 0.277 |
| Asian | 0.86 | 0.57, 1.29 | 0.456 | 1.26 | 0.74, 2.14 | 0.392 | 0.94 | 0.61, 1.46 | 0.782 |
| Other | 1.34 | 0.86, 2.08 | 0.191 | 1.42 | 0.84, 2.40 | 0.193 | 1.26 | 0.80, 2.00 | 0.318 |
| Hispanic | 0.62 | 0.41, 0.95 | 0.027 | 0.52 | 0.33, 0.82 | 0.004 | 0.84 | 0.54, 1.32 | 0.454 |
| Household composition | |||||||||
| Live alone | 0.94 | 0.55, 1.63 | 0.836 | 1.15 | 0.59, 2.24 | 0.679 | 1.44 | 0.81, 2.59 | 0.217 |
| Roommates/friends | 1.11 | 0.71, 1.74 | 0.644 | 1.18 | 0.68, 2.04 | 0.565 | 1.34 | 0.83, 2.16 | 0.226 |
| Parents/guardians | 1.00 | 0.63, 1.59 | 0.998 | 0.76 | 0.44, 1.33 | 0.342 | 1.48 | 0.90, 2.41 | 0.121 |
| Romantic partner | 1.03 | 0.67, 1.59 | 0.897 | 1.14 | 0.67, 1.92 | 0.632 | 1.06 | 0.67, 1.68 | 0.805 |
| Children | 0.86 | 0.52, 1.42 | 0.555 | 0.58 | 0.37, 1.00 | 0.051 | 1.20 | 0.70, 2.06 | 0.511 |
| Employment/financial factors | |||||||||
| College student | 1.05 | 0.78, 1.43 | 0.740 | 1.63 | 1.11, 2.40 | 0.013 | 0.93 | 0.67, 1.29 | 0.652 |
| Continue work outside of home | 0.92 | 0.64, 1.32 | 0.654 | 0.73 | 0.49, 1.09 | 0.123 | 0.89 | 0.60, 1.32 | 0.559 |
| Switched to work from home | 1.18 | 0.87, 1.61 | 0.280 | 1.76 | 1.22, 2.55 | 0.003 | 1.09 | 0.79, 1.52 | 0.592 |
| Laid off | 1.06 | 0.72, 1.57 | 0.773 | 1.37 | 0.84, 2.23 | 0.210 | 1.05 | 0.70, 1.59 | 0.804 |
| Any household financial strain | 1.09 | 0.82, 1.46 | 0.558 | 1.13 | 0.80, 1.59 | 0.486 | 1.28 | 0.93, 1.74 | 0.126 |
| Increased childcare responsibility | 0.99 | 0.58, 1.70 | 0.980 | 1.19 | 0.66, 2.15 | 0.568 | 0.90 | 0.50, 1.60 | 0.708 |
| Resilience | 0.88 | 0.76, 1.20 | 0.094 | 0.86 | 0.72, 1.01 | 0.072 | 0.71 | 0.60, 0.83 | <0.001 |
| PHQ-2 change | 1.12 | 1.04, 1.20 | 0.003 | 1.30 | 1.18, 1.43 | <0.001 | 1.21 | 1.12, 1.31 | <0.001 |
| Nagelkerke R-square | 0.036 | 0.164 | 0.093 | ||||||
All models are adjusted for the number of terms in the model.
Note. Significant p-values are noted in italics.
Discussion
The current study leveraged the SCT to examine individual and interpersonal predictors of mental and physical health impact during COVID-19. On average, participants reported experiencing at least three of five negative mental health impacts, with more than half of participants reporting increases in each of the five mental health impacts (i.e. feeling down/depressed, feeling anxious/stressed out, experiencing COVID-related stress, feeling distracted and feeling lonely/distant). Findings suggest that on average, participants’ depressive symptoms increased from pre- to during COVID-19. However, only a quarter of those in relationships reported decreased intimate partner relationship quality. The most pervasive negative impacts documented were on physical activity (nearly half) and sedentary behavior (nearly 75%). Moreover, during COVID-19, about 4 out of 10 participants reported increased alcohol use, and one-third reported decreased nutritional quality. Greater increases in depressive symptoms and lower resilience were among the most prominent predictors of negative impacts.
Consistent with the SCT [32], findings regarding predictors of negative impacts of COVID-19 coincide with prior research that such predictors of negative reactions to stress include sociodemographic characteristics [4, 25, 26, 30], one’s immediate social context (i.e. household composition and social roles [27], employment/financial factors [26–28]) and psychological factors (e.g. depression) [14, 16, 18, 19]. Particularly salient predictors of negative impacts were greater increases in depressive symptoms, which were associated with all negative health behaviors, and resilience, which was associated with more mental health impacts and increased likelihood for experiencing decreases in romantic relationship quality and nutritional quality. These findings are consistent with research suggesting that individuals with greater depressive symptoms are more likely to engage in negative communication patterns leading to decreased relationship quality, use alcohol to self-medicate or cope with their internalizing symptoms, experience decreased motivation and energy to engage in physical activity and overeat comfort foods rich in sugar that have a temporary positive influence on mood [31, 36, 37]. Additionally, individuals with greater resilience are less impacted by the influence of stress and are more likely to engage in healthy coping-related behaviors during times of stress [38–41].
Associations among situational factors and changes in health behaviors during COVID-19 were more nuanced. With regard to mental health outcomes, individuals with increased childcare responsibilities reported more negative mental health impacts during COVID-19. Individuals with increased childcare responsibilities may be experiencing sudden changes to their daily schedules with less time to spend on their normal daily tasks (e.g. work), leading to more mental health impacts [42]. Increased childcare responsibilities were also associated with likelihood of increasing alcohol use, perhaps related to the possibility that childcare responsibilities may be associated with greater stress and depression, contributing to compensatory alcohol use [37]. Interestingly, not living with children was also associated with increases in alcohol use, suggesting that having increased childcare responsibilities, rather than having a child in the household alone, is associated with increased stress during the pandemic, contributing to increases in alcohol use. Additionally, living with a romantic partner predicted greater likelihood of increasing alcohol use. While overall alcohol rates are increasing during COVID-19 among young adults, individuals are less likely to engage in social drinking due to self-isolation policies [43]. However, young adults who live with their romantic partner may experience less social isolation and, thus, be more likely to increase their alcohol use.
Individuals who reported not living with their partner were at greater risk for experiencing decreased intimate partner relationship quality, which is consistent with research suggesting social isolation predicted lower relationship quality during COVID-19 [28]. Finally, being a college student and working from home were associated with greater risk of increasing sedentary behavior. College students and those who switched to working from home have experienced disruptions to their day-to-day lives due to COVID-19 and are less likely to leave home to travel to classes or work.
With regard to sociodemographics, our findings are consistent with previous research, indicating that females and sexual minorities were at risk for increased depression [44–46], Whites (relative to Asians) were at greater risk for increased alcohol use [47], males were at greater risk for decreased physical activity [48], younger individuals were at greater risk for sedentary activity [49] and sexual minorities were at greater risk for decreased nutritional quality [50]. Interestingly, Whites relative to Blacks were at greater risk for increases in mental health impacts, whereas non-Hispanics were at greater risk for decreased relationship quality, physical activity and increased sedentary activity, which is inconsistent with the literature suggesting that Blacks and Hispanics are at greater risk for COVID-related difficulties [51]. Future research should continue to investigate these associations and explore whether these differences may be due to other factors, such as socioeconomic status or COVID-related stress.
Current findings suggest that intervention efforts should be informed by characteristics of those at highest risk for experiencing more problematic health behaviors. While greater increases in depressive symptoms placed individuals at risk for all of the problematic health behaviors assessed, some risk factors were unique to the specific outcome (e.g. increased childcare responsibilities predicting increased mental health impacts and alcohol use and working from home predicting decreased sedentary behavior). Findings suggest that depressive symptoms and resilience may be an important target in intervention for a range of negative health behaviors. However, it is also important to intervene among the unique predictors of specific outcomes. Findings stress the importance for future researchers to continue to examine the differential associations among risk factors and a broad range of negative health behaviors, as current findings demonstrate unique associations among risk factors and changes in specific health behaviors.
Limitations
The study has some limitations, including limited generalizability to other young adults in the included MSAs or across the United States. Rates of negative health behaviors should not be interpreted as prevalence rates, as our sampling design aimed to achieve a sample with higher levels of substance use, including roughly a third being past 30-day e-cigarette and cigarette users, respectively. In this analytic sample, current cigarette and e-cigarette use prevalence was 21.5% and 26.6%, respectively. Tobacco users may be at increased risk for experiencing increases in negative health outcomes during COVID-19 and tobacco use may be associated with the psychosocial factors (e.g. resilience and depressive symptoms) examined in the current study, further reducing the generalizability of the findings. Over 30% of the current sample identified as a sexual minority, which is significantly larger than estimates of sexual minority individuals from national datasets in the United States (e.g. 4.5%) [52]. This may be due to the younger age range in the current sample, as 56% of sexual minority individuals are under the age of 35 years and to the higher prevalence of tobacco use among sexual minority adults relative to heterosexual adults (20.5% versus 15.3%, respectively) [53]. The current study also relied on participants’ self-reports of their changes in health behaviors during COVID-19 and does not account for participants’ level of negative health behaviors at W3. However, we examined a model predicting change in alcohol use that included W3 alcohol use, which did not influence our findings. Moreover, in our prior analyses related to tobacco and marijuana use, accounting for W3 levels did not significantly alter correlates of self-reported change.
Conclusion
As public health authorities strive to reduce negative health behaviors during COVID-19, it is crucial to understand the factors that influence individuals’ likelihood for increasing their engagement in negative health behaviors. Current findings indicate that a large portion of individuals reported increasing their engagement in a range of negative health behaviors, especially with regard to negative mental health impacts and sedentary behavior, and that changes in young adults’ negative health behaviors were uniquely predicted by a range of individual and interpersonal factors. Potentially important targets to identify individuals for intervention efforts include situational factors (i.e. household composition and employment factors), whereas depressive symptoms and resilience may be important targets of change to prevent increases in negative health behaviors during periods of societal stress.
Funding
This publication was supported by the US National Cancer Institute (R01CA215155-01A1; PI: Berg). Dr. Berg is also supported by other US National Cancer Institute funding (R01CA179422-01; PI: Berg; R01CA239178-01A1; MPIs: Berg, Levine), the US National Institutes of Health/Fogarty International Center (1R01TW010664-01; MPIs: Berg, Kegler), and the US National Institute of Environmental Health Sciences/Fogarty International Center (D43ES030927-01; MPIs: Berg, Marsit, Sturua).
Contributor Information
Katelyn F Romm, Department of Prevention and Community Health, Milken Institute School of Public Health, George Washington University Science & Engineering Hall, 800 22nd St NW, #7000C, Washington, DC 20052, USA; George Washington Cancer Center, George Washington University Science & Engineering Hall, 800 22nd St NW, #7000C, Washington, DC 20052, USA.
Brooke Patterson, Department of Global Health, Milken Institute School of Public Health, George Washington University Science & Engineering Hall, 800 22nd St NW, #7000C, Washington, DC 20052, USA.
Christina N Wysota, Department of Prevention and Community Health, Milken Institute School of Public Health, George Washington University Science & Engineering Hall, 800 22nd St NW, #7000C, Washington, DC 20052, USA.
Yan Wang, Department of Prevention and Community Health, Milken Institute School of Public Health, George Washington University Science & Engineering Hall, 800 22nd St NW, #7000C, Washington, DC 20052, USA.
Carla J Berg, Department of Prevention and Community Health, Milken Institute School of Public Health, George Washington University Science & Engineering Hall, 800 22nd St NW, #7000C, Washington, DC 20052, USA; George Washington Cancer Center, George Washington University Science & Engineering Hall, 800 22nd St NW, #7000C, Washington, DC 20052, USA.
Conflict of interest statement
None declared.
References
- 1.Kates J, Michaud J, Tolbert J. Stay-at-home orders to fight COVID-19 in the United States: the risks of a scattershot approach. https://www.kff.org/policy-watch/stay-at-home-orders-to-fight-covid19/. Published 2020. Accessed: 19 April 2021. [Google Scholar]
- 2.Mattioli AV, Sciomer S, Cocchi C et al. Quarantine during COVID-19 outbreak: changes in diet and physical activity increase the risk of cardiovascular disease. Nutr Metab Cardiovasc Dis 2020; 30: 1409–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmid L, Worn J, Hank K et al. Changes in employment and relationship satisfaction in times of the COVID-19 pandemic: evidence from the German family panel. European Societies 2020; 23: s743–58. [Google Scholar]
- 4.Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry 2020; 66: 504–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Torales J, O’Higgins M, Castaldelli-Maia JM et al. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry 2020; 66: 317–20. [DOI] [PubMed] [Google Scholar]
- 6.Conversano C, Marchi L, Miniati M. Psychological distress among healthcare professionals invovled in the COVID-19 emergency: vulnerability and resilience factors. Clin Neuropsy 2020; 17: 94–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qiu J, Shen B, Zhao M et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 2020; 33: e100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Broderick A, Brelsford GM, Wadsworth ME. Interparental relationships among low income, ethnically diverse, two-parent cohabiting families. J Child Fam Stud 2019; 28: 2259–71. [Google Scholar]
- 9.Conger RD, Conger KJ, Martin MJ. Socioeconomic status, family processes, and individual development. J Marriage Fam 2010; 72: 685–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pietromonaco PR, Beck LA. Adult attachment and physical health. Curr Opin Psychol 2019; 25: 115–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neff LA, Karney BR. How does context affect intimate relationships? Linking external stress and cognitive processes within marriage. Pers Soc Psychol Bull 2004; 30: 134–48. [DOI] [PubMed] [Google Scholar]
- 12.Williamson HC, Karney BR, Bradbury TN. Financial strain and stressful events predict newlyweds’ negative communication independent of relationship satisfaction. J Fam Psychol 2013; 27: 65–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hardie JH, Lucas A. Economic factors and relationship quality among young couples: comparing cohabitation and marriage. J Marriage Fam 2010; 72: 1141–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mota P. Avoiding a new epidemic during a pandemic: the importance of assessing the risk of substance use disorders in the COVID-19 era. Psychiatry Res 2020; 290: 113142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turner S, Mota N, Bolton J et al. Self-medication with alcohol or drugs for mood and anxiety disorders: a narrative review of the epidemiological literature. Depress Anxiety 2018; 35: 851–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med 2014; 44: 81–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bélair MA, Kohen DE, Kingsbury M et al. Relationship between leisure time physical activity, sedentary behaviour and symptoms of depression and anxiety: evidence from a population-based sample of Canadian adolescents. BMJ Open 2018; 8: e021119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Strien T. Causes of emotional eating and matched treatment of obesity. Curr Diab Rep 2018; 18: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evers C, Dingemans A, Junghans AF et al. Feeling bad or feeling good, does emotion affect your consumption of food? A meta-analysis of the experimental evidence. Neurosci Biobehav Rev 2018; 92: 195–208. [DOI] [PubMed] [Google Scholar]
- 20.Ma Y, Ratnasabapathy R, Gardiner J. Carbohydrate craving: not everything is sweet. Curr Opin Clin Nutr Metab Care 2017; 20: 261–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.García OP, Long KZ, Rosado JL. Impact of micronutrient deficiencies on obesity. Nutr Rev 2009; 67: 559–72. [DOI] [PubMed] [Google Scholar]
- 22.Childs CE, Calder PC, Miles EA. Diet and immune function. Nutrients 2019; 11: 1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO . Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Geneva: World Health Organization, 2018. [Google Scholar]
- 24.Sarkar D, Jung MK, Wang J. Alcohol and the immune system. Alcohol Res 2015; 37: 153–5. [Google Scholar]
- 25.Prout TA, Zilcha-Mano S, Aafjes-van Doorn K et al. Identifying predictors of psychological distress during COVID-19: a machine learning approach. Front Psychol 2020; 11: 586202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Solomou I, Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: age and sex matter. Int J Environ Res Public Health 2020; 17: 4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cao W, Fang Z, Hou G et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020; 287: 112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balzarini R, Muise A, Zoppolat G et al. Love in the time of COVID: perceived partner responsiveness buffers people from lower relationship quality associated with COVID-related stressors. 2020. [Google Scholar]
- 29.Stanton R, To QG, Khalesi S et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health 2020; 17: 4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alomari MA, Khabour OF, Alzoubi KH. Changes in physical activity and sedentary behavior amid confinement: the BKSQ-COVID-19 project. Risk Manag Healthc Policy 2020; 13: 1757–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Di Renzo L, Gualtieri P, Pivari F et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med 2020; 18: 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall, 1986. [Google Scholar]
- 33.Public Health Law Center . Commercial tobacco and marijuana. 2020.
- 34.Smith BW, Dalen J, Wiggins K et al. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008; 15: 194–200. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care 2003; 41: 1284–92. [DOI] [PubMed] [Google Scholar]
- 36.Vujeva HM, Furman W. Depressive symptoms and romantic relationship qualities from adolescence through emerging adulthood: a longitudinal examination of influences. J Clin Child Adolesc Psychol 2011; 40: 123–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcohol Clin Exp Res 2009; 33: 49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Collishaw S, Pickles A, Messer J et al. Resilience to adult psychopathology following childhood maltreatment: evidence from a community sample. Child Abuse Negl 2007; 31: 211–29. [DOI] [PubMed] [Google Scholar]
- 39.Masten AS. Ordinary magic. Resilience processes in development. Am Psychol 2001; 56: 227–38. [DOI] [PubMed] [Google Scholar]
- 40.Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol 2004; 59: 20–8. [DOI] [PubMed] [Google Scholar]
- 41.Wu Y, Sang ZQ, Zhang XC et al. The relationship between resilience and mental health in Chinese college students: a longitudinal cross-lagged analysis. Front Psychol 2020; 11: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Russell BS, Hutchison M, Tambling R et al. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent-child relationship. Child Psychiatry Hum Dev 2020; 51: 671–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bade R, Simpson BS, Ghetia M et al. Changes in alcohol consumption associated with social distancing and self-isolation policies triggered by COVID-19 in South Australia: a wastewater analysis study. Addiction 2020; 116: 1600–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suen YT, Chan RCH, Wong EMY. Effects of general and sexual minority-specific COVID-19-related stressors on the mental health of lesbian, gay, and bisexual people in Hong Kong. Psychiatry Res 2020; 292: 113365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhong BL, Luo W, Li HM et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci 2020; 16: 1745–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alexander JL, Dennerstein L, Kotz K et al. Women, anxiety and mood: a review of nomenclature, comorbidity and epidemiology. Expert Rev Neurother 2007; 7: S45–58. [DOI] [PubMed] [Google Scholar]
- 47.Vaeth PA, Wang-Schweig M, Caetano R. Drinking, alcohol use disorder, and treatment access and utilization among U.S. racial/ethnic groups. Alcohol Clin Exp Res 2017; 41: 6–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.García-Tascón M, Sahelices-Pinto C, Mendaña-Cuervo C et al. The impact of the COVID-19 confinement on the habits of PA practice according to gender (male/female): Spanish case. Int J Environ Res Public Health 2020; 17: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zheng C, Huang WY, Sheridan S et al. COVID-19 pandemic brings a sedentary lifestyle in young adults: a cross-sectional and longitudinal study. Int J Environ Res Public Health 2020; 17: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Calzo JP, Roberts AL, Corliss HL et al. Physical activity disparities in heterosexual and sexual minority youth ages 12–22 years old: roles of childhood gender nonconformity and athletic self-esteem. Ann Behav Med 2014; 47: 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Purtle J. COVID-19 and mental health equity in the United States. Soc Psychiatry Psychiatr Epidemiol 2020; 55: 969–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.UCLA Williams Institute School of Law . LGBT proportion of population: United States. Available at: https://williamsinstitute.law.ucla.edu/visualization/lgbt-stats/?topic=LGBT#density. Accessed: 14 April 2021.
- 53.Centers for Disease Control and Prevention . Lesbian, gay, bisexual, and transgender persons and tobacco use. Available at: https://www.cdc.gov/tobacco/disparities/lgbt/index.htm. Accessed: 14 April 2021.


