Abstract
We review some of the important discoveries and advances made in basic and translational cardiac research in 2020. For example, in the field of myocardial infarction (MI), new aspects of autophagy and the importance of eosinophils were described. Novel approaches, such as a glycocalyx mimetic, were used to improve cardiac recovery following MI. The strategy of 3D bio-printing was shown to allow the fabrication of a chambered cardiac organoid. The benefit of combining tissue engineering with paracrine therapy to heal injured myocardium is discussed. We highlight the importance of cell-to-cell communication, in particular, the relevance of extracellular vesicles, such as exosomes, which transport proteins, lipids, non-coding RNAs, and mRNAs and actively contribute to angiogenesis and myocardial regeneration. In this rapidly growing field, new strategies were developed to stimulate the release of reparative exosomes in ischaemic myocardium. Single-cell sequencing technology is causing a revolution in the study of transcriptional expression at cellular resolution, revealing unanticipated heterogeneity within cardiomyocytes, pericytes and fibroblasts, and revealing a unique subpopulation of cardiac fibroblasts. Several studies demonstrated that exosome- and non-coding RNA-mediated approaches can enhance human induced pluripotent stem cell (iPSC) viability and differentiation into mature cardiomyocytes. Important details of the mitochondrial Ca2+ uniporter and its relevance were elucidated. Novel aspects of cancer therapeutic-induced cardiotoxicity were described, such as the novel circular RNA circITCH, which may lead to novel treatments. Finally, we provide some insights into the effects of SARS-CoV-2 on the heart.
Keywords: Cardiac, Myocardial infarction, Myocardial injury, Heart failure, Non-coding RNA, Cardiomyocyte division, Induce pluripotent stem cells, Cardiotoxicity, Single-cell RNA sequencing s, COVID-19
Graphical Abstract

1. Introduction
The year 2020 was unique in modern history, temporarily affecting normal research activities worldwide, as well as affecting much of normal life. Nevertheless, cardiovascular research continued unabated, and output even increased. Incredibly, the number of publications in PubMed containing the keyword ‘cardiac’ actually increased by 14%, from 86 498 in 2019 to 98 683 in 2020. Here, we highlight some of the major advances that were made in basic and translational cardiac research—and mechanistic studies that we believe may have the greatest impact on the development of future therapeutics and bio-analytics for cardiovascular disease (Figure 1). It is, by its nature, a subjective selection, and some important advances may have been overlooked, but it represents a snapshot of some of what the authors believe were research highlights in 2020.
Figure 1.

The top cardiac-related phrases appearing in the titles of Cardiovascular Research articles published in 2020, with the size of the font indicating the phrase’s frequency.
2. Myocardial infarction, ischaemia/reperfusion injury, and heart failure, a trilogy
Ischemia and reperfusion (IR) injury is an unavoidable deleterious effect that determines the final infarct size after successful revascularization following myocardial infarction (MI). There is currently no effective therapy for reducing cardiac damage in the setting of MI. The year 2020 has brought relevant data to improve our understanding of the pathophysiological mechanisms behind IR and has identified new potential therapeutic targets to limit infarct size and the consequent adverse cardiac remodelling.
Gao et al.1 propose a novel signalling pathway, TXNIP (thioredoxin-interacting protein)/Redd that contributes to IR injury by promoting excessive autophagy during reperfusion. In particular, by combining studies in cardiac-restricted TXNIP-knock out mice with experiments in primary cultures of cardiomyocytes, the authors demonstrated that TXNIP (a pro-oxidative molecule) inhibits autophagosome clearance via a reactive oxygen species (ROS)-mediated mechanism; however, it upregulates autophagosome formation by upregulating Redd1 (mTOR inhibitor), leading to exacerbated autophagy after reperfusion and consequent cardiomyocyte death.1 The study by Liu et al.2 sheds new light on the role of eosinophils in acute MI. Through a series of mechanistic studies and transgenic mice, the authors provide evidence that eosinophils, by producing IL-4 and cationic protein mEar1, mitigate cardiomyocyte death, fibroblast activation, and neutrophil adhesion, ultimately improving cardiac function. The work establishes a cardioprotective role of eosinophils against post-IR injury supporting the hypothesis that an increase of circulating and cardiac eosinophils represents a compensatory mechanism to repair the ischemic heart.
Regarding novel approaches and opportunities for cardioprotection, the Panitch lab proposed a new therapeutic approach to limit IR injury by interfering with leukocyte recruitment and attachment at the site of injury.3 The authors designed a novel selectin-targeting glycocalyx mimetic (named DL-IkL) that targets a glycocalyx component of the damaged endothelium and reduces the availability of endothelial adhesion molecules (mainly selectins) interfering with neutrophil binding to the inflamed vessel wall. Administration of this new compound at reperfusion and 24 h thereafter to mice with a MI reduced neutrophil and macrophage accumulation, tissue fibrosis and cardiac damage, and improved cardiac function.3 Other novel therapeutic approaches to limit cardiac damage and lessen adverse cardiac remodelling have also been proposed. By means of cardiac magnetic imaging analyses in a pig model of MI, Mendieta et al.4 demonstrated that administration of intravenous atorvastatin during ischemia limits cardiac damage, improves the recovery of systolic function and mitigates adverse cardiac remodelling to a larger extent than when administered orally shortly after reperfusion. Furthermore, this intravenous approach also limits the systemic inflammatory response. This highly translational study supports the concept that statins can be repurposed and used intravenously as a feasible and safety cardioprotective approach on first medical contact in the setting of STEMI.4 Another study that deserves to be highlighted in the field of IR focused on the effect of circadian rhythm on acute MI, a subject of considerable scientific interest but with a wide knowledge gap with respect to the mechanism of the interaction. Zhang’s group demonstrated, in cardiomyocyte-specific Krüppel-like factor 15 (KLFL15) knockout mice, the key contribution of this oscillatory transcription factor to the susceptibility of IR injury in a time-of-day specific manner.5 Moreover, the effects of KLF15 were linked to the presence of NAD+, a key co-enzyme for the proper functioning of mitochondrial deacetylase sirtuin-3.5 The authors suggest that NAD+ supplementation during a critical time window may be particularly beneficial for patients with chronic heart diseases.
Over the past few years, long non-coding RNA (lncRNAs) have emerged as key regulators of the biological processes involved in the progression of heart failure.6 Viereck et al.7 focused on the potential of the highly conserved lncRNA H19, found to be downregulated in failing hearts. The authors demonstrated that cardiomyocyte-directed H19 gene therapy suppresses pressure-overload-induced left ventricular cardiac failure at both structural and functional level in mice. Mechanistically, the Thum lab identified a link between H19 and the suppression of pro-hypertrophic NFAT (nuclear factor of activated T cells) signalling.7 These findings open up new pathways for exploiting H19 as a potential therapeutic target in the management of heart failure patients.7
Lin et al.8 provided novel insights into the controversial approach of using proton pump inhibitors (PPIs) beyond their acid-suppressing action. In this work, the authors demonstrate that lansoprazole administration attenuates pressure overload-induced cardiac hypertrophy and improves heart failure in mice regardless of its H+/K+-ATPase inhibition. The protective benefits were associated with inhibition of the AKT/GSK-3β/β-catenin signalling pathway, upregulation of HO-1 (heme oxygenase-1) expression and reduction in ROS production, overall supporting the use of PPIs to alleviate cardiac adverse remodelling.8
One crucial outstanding question is why it has not yet been possible to translate cardioprotection to the clinic. This question was addressed in a position paper of the Working Group on Cellular Biology of the Heart, which provides important recommendations to improve translational research in sex-specific effects of comorbidities and risk factors in ischaemic heart disease.9 Furthermore, Schreckenberg et al. proposed that there may be a mix of responders and non-responders to cardioprotective interventions, and they identified the mitochondrial transcriptome as potentially involved.10
3. Rebooting cardiac regeneration by cardiomyocyte renewal and tissue engineering strategies
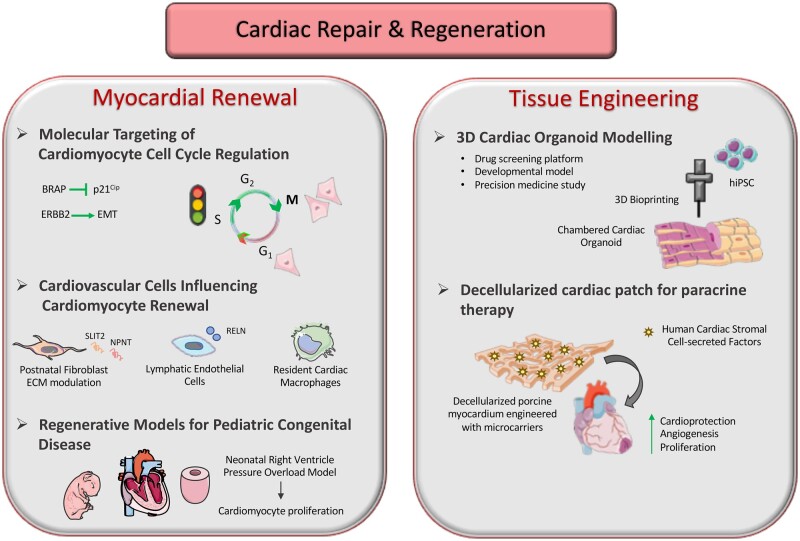
Since the first report in 2011, describing transient mammalian neonatal heart myocardial renewal by means of resident cardiomyocyte de-differentiation and proliferation,11 several independent studies have addressed the role of genetic, metabolic, immunologic, and stimulatory environmental factors to restore endogenous regenerative response in the heart. Therefore, the comprehensive analysis of regulatory mechanisms of cardiomyocyte cell-cycle control has become of increasing interest to basic and translational cardiac researchers (Figure 2).
Figure 2.
Schematic of the latest insights on myocardial renewal and tissue engineering strategies to enhance cardiac repair and to stimulate heart regeneration following injury. BRAP, BRCA1-associated protein; EMT, epithelial–mesenchymal transition; ECM, extra-cellular matrix; NPNT, nephronectin; RELN, Reelin; hiPSC, human induced pluripotent stem cell. Schematic has been produced using Smart—Servier Medical Art (available at https://smart.servier.com).
Several studies published in 2020 offered significant new insights into the mechanism of myocardial regeneration via reactivation of cardiomyocyte division. Volland et al.12 translated insights from cardiac development by demonstrating that BRCA1-associated protein (BRAP) is pivotal in blocking the cell-cycle inhibitor p21Cip, thus allowing DNA synthesis, cell-cycle progression, and proliferation in murine cardiomyocytes.12 In particular, the authors revealed a specific role for BRAP in regulating cardiac development and cardiomyocyte cell-cycle control; BRAP ablation resulted in attenuation of neonatal cardiomyocyte cell-cycle progression and evoked lethal heart failure in vivo at post-natal age; conversely, its overexpression enhanced the engagement into the DNA duplication phase and reduced p21Cip expression in neonatal cardiomyocytes. Therefore, BRAP signalling appears to be critical to regulate cardiomyocyte cell-cycle machinery, myocardial development, and adult myocardial performance, hence suggesting a fine mechanism with critical impact for future regenerative strategies.
The recapitulation of the embryonic developmental programme—such as activation of epithelial–mesenchymal transition (EMT) in cardiac stromal cells—has previously been shown to trigger reparative mechanisms within the heart.13,14 In 2020, Aharonov et al.15 showed that transient overexpression of activated ERBB2 in adult cardiomyocytes caused cardiac regeneration in a preclinical murine model of heart failure. Restoration of ERBB2 signalling in the injured myocardium triggered an EMT-like response within resident cardiomyocytes defined by cytoskeletal remodelling, junction dissolution, and extracellular matrix turnover, overall inducing their migration and replacement of scar tissue by means of myocardial renewal. This study suggests that reactivation in adult cardiomyocytes of developmental EMT-like behaviour and ERBB2–ERK–YAP mechano-transduction signalling may represent a relevant therapeutic target for cardiac restoration following injury.
Besides analytical investigation of signalling pathways regulating cardiomyocyte cell-cycle activity, increasing interest has been directed towards non-cardiomyocyte cell types, in driving myocardial renewal. Wu et al.16 recently addressed the role of post-natal cardiac fibroblasts and extra-cellular matrix (ECM) in influencing cardiomyocyte cell division by showing that fibroblast-induced ECM modulation can affect cardiomyocyte cytokinesis and induce their binucleation. SLIT2 and Nephronectin (NPNT) were identified as fibroblast-derived ECM reference components exerting proliferative effects, thus revealing two putative molecular candidates for further investigation on the mechanisms underlying bona fide cardiomyocyte cytokinesis from embryonic to adult stages.
Recent data have emphasized the role of lymphatic cells in improving cardiac function and inhibiting detrimental remodelling after injury.17–19 Liu et al.20 recently identified a function for lymphatic endothelial cells (LECs) in orchestrating cardiomyocyte proliferation and survival during heart development including the early post-natal regenerative stage. LECs were shown to release trophic lympho-angiocrine signals, among which the extracellular protein Reelin (RELN) emerged as promising therapeutic candidate, since it improved myocardial rescue in the adult mouse heart when administered via a bioengineered collagen patch.20 A growing body of evidence on the role of immune system cells during cardiac repair indicates that macrophages are prominent facilitators of neonatal mouse heart regeneration and cardiomyocyte mitochondrial homeostasis, e.g. by eliminating dysfunctional mitochondria ejected by cardiomyocytes.21–23 Notably, Li et al.24 confirmed that macrophage recruitment is critical to initiating endogenous myocardial regeneration, since genetic ablation of murine CD11b-positive macrophages inhibited neonatal heart restoration with worsening of cardiac function after apical resection. Moreover, the fundamental function of macrophages in myocardial renewal was validated by evidence of restoration of cardiomyocyte proliferation following transplantation of neonatal cardiac macrophages in the injured adult heart.24
At present, preclinical heart research in mammals focuses mainly on left ventricle myocardial infarction or cardiac ischaemic- or cardiotoxic injury models with the aim of modelling the adult clinical scenario. There is often limited correlation with congenital heart disease affecting paediatric patients. Of note, tetralogy of Fallot, pulmonary artery hypertension, and pulmonary stenosis in children are often caused by pressure overload in the right ventricle.25,26 Against this background, Ye et al.27 recently showed in the rat, that pulmonary artery banding at post-natal day 1 induces right ventricle pressure overload. This triggers myocardial renewal activation by over-proliferation of resident neonatal cardiomyocytes. Interestingly, such findings were further verified by histological analysis of human specimens of tetralogy of Fallot. The results suggest, for the first time, that right ventricular pressure overload model may represent an additional relevant model of heart regeneration and neonatal cardiomyocyte proliferation, with translational relevance for the pathogenesis of many paediatric congenital heart diseases.
New cardiac tissue engineering strategies were developed in 2020, in order to provide reliable tissue models for translational research (Figure 2). For example, Kupfer et al.28 optimized a 3D bio-printing strategy based on an ECM-derived bio-ink formulation, which supported human induced pluripotent stem cell (iPSC) viability, proliferation, and maturation into cardiomyocytes. This technique resulted in the fabrication of a geometrically complex, chambered cardiac organoid with robust electromechanical function, and provided remarkable advances in terms of in situ pluripotent stem cell differentiation at high density.28 Such engineered human cardiac structures could be exploited as drug screening platforms or for use in experimental medicine with in vitro developmental or injury/disease models. From a regenerative point of view, an acellular artificial cardiac patch has recently been described with cardioprotective, pro-angiogenic and proliferative potential in rodent and porcine models of acute myocardial infarction.29 De-cellularized porcine myocardium was engineered with biodegradable polylactic-co-glycolic acid (PLGA) microcarriers delivering human cardiac stromal cell-secreted factors.29 This combinatorial approach resulted in the optimization of a ready-to-use and cell-free graft, which maintained regenerative properties after cryopreservation, thus suggesting a feasible and clinically compliant therapeutic strategy.29 As such, this study offers an elegant proof-of-principle for the functional association of tissue engineering technique with paracrine therapy to heal the injured myocardium.
4. Looking beyond the cardiomyocytes—from phenotyping individual cell types to cell atlases of the heart
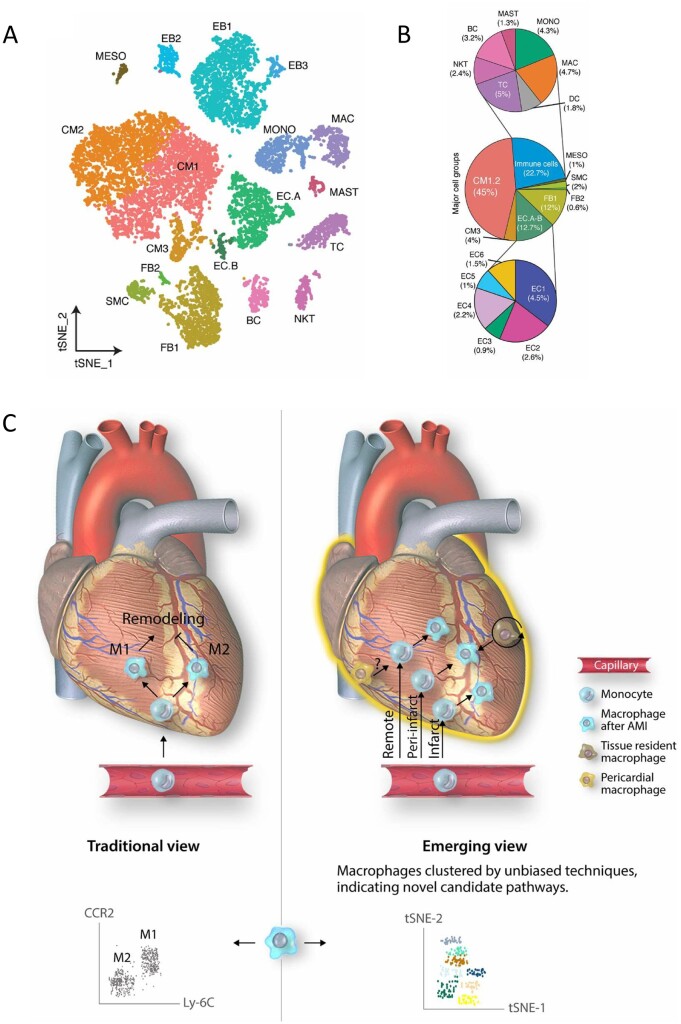
Microscopy entered a new era with the development of super-resolution techniques. Similarly, single-cell transcriptomics has kicked off a revolution in genetics, by providing a high-resolution view of gene transcription at the level of individual cells, rather than bulk tissue. Next-generation sequencing of mRNA expression in individual cells, combined with machine learning, can now provide unprecedented, granular detail of the individual cell types present within tissues.30 The trajectories of individual cell types can be followed as they undergo differentiation. In 2020, the technique’s enormous potential for the field of cardiovascular biology was revealed by a landmark study, published in Nature, which attempted to identify and categorize all the cell types of the adult human heart.31 After analysing approximately half a million single cells, this investigation revealed a surprising diversity of cell types in the heart, and unanticipated heterogeneity within cardiomyocytes, pericytes, and fibroblasts.31 Functional interactions between different cell types such as immune cells and fibroblasts could be deduced.31 By applying this same approach to mouse hearts, Ruiz-Villalba et al.32 were able to identify a unique subpopulation of cardiac fibroblasts expressing high levels of CTHRC1 (collagen triple helix repeat containing 1), that emerges following myocardial infarction and reduces the likelihood of death due to cardiac rupture. Suryawanshi et al.33 used single-cell transcriptomics to produce an equivalent map of all the cells within the foetal human heart. This showed an unanticipated diversity of cardiac cell types and allowed the separation of endothelial cells into previously uncharacterized sub-populations. A comparison with foetal human hearts affected by congenital heart block (CHB), a disease that results in significant mortality (17.5%), revealed a remarkable interferon response in many cell types of the diseased heart, which indicates a therapeutic target.33 By offering a new lens with which to view the heart, single-cell transcriptomics is sure to lead to many future insights into the secret life of cells of the heart.
A cell type of particular interest is macrophages, which are not only integral to the initial inflammatory response to injury, but also to subsequent wound healing. Consequently, maladaptive immune cell behaviour contributes to ventricular remodelling. A paradigm shift in macrophage biology occurred with the recognition that they can be divided into a population of pro-inflammatory, M1 macrophages and a population of reparative, M2 macrophages. Initial investigations of cardiac macrophage populations following acute MI suggested they aligned well to this model. However, as reviewed by Peet et al., 34 more recent data demonstrate remarkable heterogeneity and plasticity in macrophage development, phenotype, and function (Figure 3). These recent insights into macrophage biology may explain the failure of non-specific immunosuppressive strategies and are important to understand in the development of novel therapies targeting heart failure following acute MI.34
Figure 3.
(A) Identification of cell types in human foetal heart. Clustering for 12 461 cells from three healthy samples based on established lineage markers and visualized using t-SNE. (B) Averaged proportion of all cell types (except EBs) contributing to foetal human hearts. Middle panel indicates major cell groups with subgroups of immune cells (top panel) and endothelial cells (bottom panel) and number in parenthesis indicates percentage contribution to foetal heart cells. Figure taken from Suryawanshi et al.33 with permission. (C) Novel macrophage populations appear to play spatially restricted roles in remodelling of the myocardium following acute myocardial injury (AMI). Novel high throughput techniques allow unbiased resolution of cells into distinct populations, based on gene expression profile (scRNA-seq) or large panels of differentially expressed proteins (mass cytometry). Figure taken from Peet et al.34 with permission.
While a robust inflammatory response to tissue injury is a necessary part of the repair process, it can also result in the deposition of scar tissue. Bevan et al.35 used stable transgenic lines, whole organ imaging and genetic and pharmacological interventions to demonstrate that different subsets of macrophages promote scar deposition following cardiac injury and facilitate scar removal during regeneration.35 Osteopontin was identified as having both pro-fibrotic but also potentially pro-regenerative roles in the adult zebrafish heart, driving collagen deposition but also controlling inflammatory cell resolution.35
The use of stem cell therapy as a means to regenerate the heart has a long and chequered history. Despite the intuitive attractiveness of the approach, few still believe that it results in significant cardiac regeneration. While intracardiac stem cell injection appears to slightly improve cardiac function following MI, no clear mechanism had been established until Vagnozzi et al.36 showed it acts through an acute sterile immune response. This was characterized by the temporal and regional induction of CCR2(+) and CX3CR1(+) macrophages. Remarkably, the same response could be obtained by injecting either killed cells or a chemical inducer of the innate immune response. By modulating the macrophage response, these treatments initiated an acute, inflammation-based, wound-healing response that rejuvenates the infarct area of the heart. This important study likely represents a capstone on 30 years of research investigating the mechanism of stem cell-mediated regeneration of the injured heart.
In a further example of the importance of inter-cellular communication, Zhao et al.37 used an impressive variety of techniques ranging from bone marrow transplantation and parabiosis (conjoining of circulatory systems) to show that mir-210 can be delivered to the endothelium through the blood by a long-range endocrine mechanism. Significantly, it modulated expression of target genes in the endothelium and promoted pulmonary hypertension.
The cancer field has recently undergone a revolution with the discovery that cytotoxic T cells can be redirected to specifically recognize and eliminate cancer cells. Aghajanian et al.38 were able to ‘repurpose’ this technique, using T cells to recognize a novel cardiac fibroblast epitope they identified. By eliminating cardiac fibroblasts from injured mouse hearts it was possible to restore cardiac function. These results provide proof-of-principle for the development of immunotherapeutic drugs for the treatment of cardiac disease.
5. Cell-to-cell communication via exosomes and non-coding RNA
Cell-to-cell communication plays a pivotal role in cardiac remodelling and function, both under physiological conditions to maintain myocardial homeostasis, and under pathological conditions as an adaptive response to injury and stress. In 2020, different studies aimed at gaining a better understanding of how crosstalk between cells affects cardiac function, resulted in the identification of novel pathophysiological mechanisms of intercellular communication.
Moreira et al.39 identified a novel calcitonin-mediated paracrine mechanism between cardiomyocytes and fibroblasts in the human atrial myocardium that tightly regulates fibroblast function, preventing the accumulation of fibrous tissue and fibrogenesis. The authors used human right atrial tissue to demonstrate that isolated cardiomyocytes abundantly express the thyroid hormone calcitonin. Through specific receptor-binding on the membrane of atrial fibroblasts, cardiomyocyte-released calcitonin acts as a paracrine signal controlling cell proliferation and BMP1 (bone morphogenetic protein-type 1)-related collagen processing, as demonstrated by single-cell RNA sequencing and proteomic approaches. Supporting this finding, patients with persistent atrial fibrillation, a highly prevalent cardiac arrhythmia associated with considerable mortality and morbidity, had impaired production of myocardial calcitonin with loss of calcitonin receptor in the fibroblast membrane. Using several different mouse models, either with global disruption of calcitonin receptor expression or with atrial-specific knockdown of calcitonin, Moreira et al.39 demonstrated the relevance of the calcitonin–calcitonin receptor axis to control susceptibility to atrial fibrosis and fibrillation.
Evidence that has been accumulated over the past years relates the cardioprotective effects of mesenchymal stromal cells (MSC) to their paracrine activities, which result in anti-apoptotic, pro-angiogenic and immunomodulatory mechanisms rather than de novo cardiomyocyte regeneration through replication and differentiation. Using mouse models of MI and myocardial I/R, Yan et al.40 demonstrated that N-cadherin overexpression prolongs myocardial retention of implanted adipose-derived stem cells (ADSC) and enhances ADSC cardioprotective effects, mainly preserving capillary density and cardiomyocyte proliferation. Furthermore, the authors highlighted an increase in N-cadherin/β-catenin interaction and intracellular trafficking of β-catenin, with the subsequent expression of downstream molecules such as metalloproteinase (MMP)-10 and MMP-13 and hepatocyte growth factor (HGF), as responsible for the enhanced cardioprotective effects derived from N-cadherin overexpression in ADSC.
Exosomes are extracellular nanovesicles, released by a wide spectrum of cell types and carrying non-random subsets of bioactive molecules (proteins, lipids, non-coding RNAs and mRNAs) already present in their cells of origin. Together with soluble factors, exosomes are increasingly recognized as active intercellular messengers in paracrine signalling, but the mechanisms involved and their role as potential novel therapeutic candidates to improve heart function remain unclear. Gao et al.41 demonstrated, in a mouse model of MI that post-MI circulating exosomes from heart and kidney origin mediate the activation of pro-angiogenic signalling in adipose-derived MSCs (AD-MSCs). Through mechanistic studies in cultured AD-MSCs, the authors linked the effects of cardio-renal serum exosomes with activation of vascular endothelial growth factor (VEGF) signalling after delivering miR-1956 into the cells. Thus, miR-1956 acted as a functional exosome-messenger by downregulating Notch-1 expression, which was identified as a key mediator of exosome-miR1956-VEGF signalling in AD-MSCs. The benefits of exosome-induced paracrine signalling on cardiac regeneration were also evidenced in human iPSCs derived from cardiac fibroblasts (CF-iPSC).42 CF-iPSC exosomes were enriched in miRNA cluster miR-371-373, highly expressed in human embryonic stem cells, and significantly enhanced spontaneous differentiation of CF-iPSC into cardiomyocytes, evidenced by the increased number of contracting embryoid bodies.
There is consistent evidence that the molecular cargo of exosomes varies depending on environmental stimuli. Accordingly, there is increasing interest in identifying strategies to modulate endogenous exosome composition and thereby influence their biological effects. Lew et al.43 performed a study in diabetic db/db mice, in which the effectiveness of exercise for preventing or reversing cardiac and coronary dysfunction in diabetes was highlighted. Importantly, the study provided novel evidence implicating cardiovascular-related miRNAs and particularly miR-126 and its molecular targets (SPRED1/VEGF) as mechanistic effectors underlying the vascular protective ability and cardioprotective properties of exercise training. Of note, exercise-mediated changes in miRNA translation were related to the intensity and the time at which exercise was implemented during disease progression (i.e. early vs. late) in the diabetic mice.
Recent evidence also points to rare subtypes of non-coding RNAs, such as circular RNAs (circRNAs), as novel contributors to cardiovascular pathophysiology. However, their functional role in cardiac remodelling in different pathological settings still requires better delineation. Li et al.44 showed that circRNA_000203 was upregulated in the myocardium of Angiotensin-II (AngII)-infused mice to induce cardiac hypertrophy, and identified the potential mechanism involved. By means of dual luciferase and RNA-pull-down assays, authors demonstrated that circRNA_000203 acted as a sponge for miR-26b-5p and miR-140-3p in cardiomyocytes, which resulted in the increased expression of their common target gene, GATA4, thereby contributing to aggravated cardiac hypertrophy.
Beyond lipid-lowering, statins exert cardioprotective effects (see Mendieta et al.4). In this respect, Huang et al.45 demonstrated that exosomes released from atorvastatin-pretreated MSCs increased survival and promoted cell migration and tube-like structure formation when delivered into endothelial cells in vitro, under hypoxia and serum deprivation conditions. In addition, atorvastatin pre-treatment promoted the efficiency of MSC-derived exosomes to preserve cardiac function and enhance angiogenesis in animals presenting acute MI. Using different mechanistic approaches, the authors identified lncRNA H19 as a mediator of the pro-angiogenic effects induced by the atorvastatin-pretreated MSCs.
In recent years, increasing interest has been directed towards stimulating the specific release of reparative exosomes in the ischemic myocardium. Shock wave therapy (SWT) is frequently used as adjuvant therapy to improve wound healing, and a first-in-human study in patients with acute myocardial infarction was recently reported, 46 although mechanisms involved were not identified. The study by Gollmann-Tepeköylü et al.47 evidenced an increased release of miRNA-19a-3p enriched endothelial-exosomes in response to SWT, both in vitro and in vivo. Of note, exosomes derived from SWT-stimulated cells induced VEGF-mediated angiogenic signals and capillary formation. Using a mouse model of MI, the authors demonstrated the beneficial effects on cardiac contractility after treatment with the exosomes released from SWT-stimulated cells.
Strategies to enhance exosome effectiveness as a therapeutic tool also consider manipulating endogenous exosome biodistribution to increase their local concentration in response to need. In this regard, Liu et al.48 designed antibody-conjugated magnetic nanoparticles that can be used as a vesicle shuttle, due to their ability to simultaneously capture circulating exosomes (CD63-antigen binding) and target injured cardiomyocytes (myosin-light chain antigen) in the infarcted area, in addition to facilitating the local release of the captured exosomes on the injured cardiac tissue. The applicability of this novel vesicle-shuttle approach as a strategy for therapy was demonstrated in rat and rabbit models of MI. Thus, magnetic-guided accumulation of exosomes in infarcted tissue led to a reduction in the infarct size and enhanced angiogenesis four weeks after treatment, in addition to an improvement of the cardiac function, as assessed by echocardiography.
6. iPSC-CM (in vitro contraction, arrhythmia, in vivo cardiac repair)
As can be seen from the previous section, there is still a great deal that remains to be understood about how exosomes function. One resource that will be useful for investigating this is the atlas of exosomal microRNAs from human iPSC-derived cardiac cells, created by Chandy et al.49 To create this database, human iPSC were differentiated into cardiomyocytes (iPSC-CMs), endothelial cells (iPSC-ECs), or cardiac fibroblasts (iPSC-CFs). Small extracellular vesicles (sEVs) were then isolated from them using a microfluidic system, and their miRNA contents was sequenced and compared to the source cell. Interestingly, only a subset of total cellular miRNAs was found to be secreted in sEVs, but a common core of miRNAs was secreted by all three cardiac cell types. There was some cell specificity. For example, miR-1, which is critical for cardiac development and pathology, was only secreted by iPSC-CMs.
A practical way to study inherited arrhythmias in vitro without the need for cardiac biopsies is to differentiate patient-derived iPSCs into cardiomyocytes. Benzoni et al.50 took advantage of this technique to investigate the mechanism of inherited, untreatable persistent atrial fibrillation. Electrophysiological characterization of the patient-derived cardiomyocytes revealed functional alterations of If and ICaL currents leading to a cardiac substrate more prone to develop arrhythmias under stressful conditions.
One limitation of using iPSC-CM for electrophysiological or other studies, is that the iPSC-derived cells more closely resemble foetal cardiomyocytes, utilizing glycolysis for ATP generation, and expressing immature ion channels (e.g. high levels of the ‘sinoatrial’ (If) current, and low levels of IK1, which leads them to beat spontaneously).51 Therefore, Garbern et al.’s52 discovery that inhibition of mTOR signalling enhances maturation of cardiomyocytes derived from human iPSC, increasing their expression of sarcomere proteins and ion channels (including Kir2.1), was an important advance.
An alternative method that can be used to drive cardiomyocyte maturity is to culture them for several months on a nan-patterned surface, which results in human iPSC-CMs with adult-like dimensions and aligned myofibrils.53 Pioner et al.53 showed that if these cells are derived from a Duchenne muscular dystrophy (DMD) patient lacking full-length dystrophin, they have reduced myofibril contractile tension, slower relaxation kinetics, and to Ca2+ handling abnormalities, similar to DMD cells. This is very practical for in vitro investigations of cardiomyocyte-intrinsic genetic diseases.53
Despite initial enthusiasm in regenerative medicine for the approach of directly injecting cardiomyocytes derived from iPSC into the heart, this approach has been frustrated by poor survival and/or functional integration of implanted cells. However, Lou et al.54 showed that cell engraftment could be improved by overexpressing N-cadherin, a protein that mediates the adhesion between cardiac myocytes (CMs). This also improved their functional integration via paracrine activation of the extracellular signal-regulated kinase (ERK) signal transduction pathway, inducing neo-vasculogenesis and increasing survival of the implanted cells. Importantly, in mice that received these cells following MI, infarct size was also reduced and left ventricular (LV) ejection fraction was improved.54
Another interesting protein, very important in angiogenesis and cellular interactions, is angiopoietin-1. When Tao et al.55 overexpressed this protein in human atrial human iPSC-CMs, and seeded them into a fibrin/thrombin patch that was then implanted on the rat hearts following MI, the implanted cells secreted Ang-1 protein for up to 14 days, upregulated ERK signalling and inhibited pro-apoptotic Bax protein expression. They saw increased mitosis and arteriole formation, improved cell engraftment rate, and less LV dilation and improved LV global pump function.
Thus, while some studies suggest that iPSC-CM may be able to restore the damaged heart, other studies suggest that additional approaches such as those mediated through paracrine mechanisms may be required to provide meaningful benefit.
7. Powering the heart—mitochondria and metabolism
Transport of Ca2+ into mitochondria is mediated by the mitochondrial Ca2+ uniporter (MCU). This is important for metabolic adaption to work, but since it exposes the mitochondria to the risk of Ca2+ overload, MCU activity is modulated by other proteins. One such protein is the MCUB subunit. Using mice with cardiomyocyte-specific overexpression or deletion of MCUB, Huo et al.56 showed that MCUB is inducible and limits mitochondrial Ca2+ influx after IR, preventing mitochondrial permeability transition pore (mPTP) opening and protecting the myocardium. Interestingly, hindlimb remote ischemic preconditioning increased MCUB expression in the heart and decreased mitochondrial Ca2+ uptake.
Another regulator of MCU activity that plays an important role in regulating pathological Ca2+ overload in the heart is MICU3 (mitochondrial calcium uptake 3). Puente et al.57 eliminated MICU3 globally utilizing CRISPR-Cas9 and found that the mice were protected against IR injury and isoproterenol-induced cardiac dysfunction. Interestingly, it was originally found that global ablation of MCU is not cardioprotective,58 although this appears to have been due to compensatory modifications that desensitize the mPTP to Ca2+ leak.59
Lipid accumulation in diabetic and obese patients typically encompasses increased cardiac fatty acid (FA) uptake eventually surpassing the mitochondrial oxidative capacity. Nevertheless, decreased lipolysis via cardiac overexpression of Perilipin 5 (Plin5), a binding partner of Adipose triglyceride lipase (ATGL), is compatible with normal heart function and lifespan despite massive cardiac lipid accumulation. Kolleritsch et al.60 provide evidence that this can be explained by a reduction in dynamin-related protein 1 (Drp1)-mediated mitochondrial fission.
Doxorubicin is a chemotherapeutic drug widely used for treating a variety of cancers. However, it causes significant cardiotoxicity and heart failure. Dhingra et al.61 showed that doxorubicin de-represses nuclear factor-kB (NF-kB)-mediated suppression of Bnip3 expression. In other words, it causes increased Bnip3 expression, leading to mitochondrial injury, including calcium influx, mPTP opening, ROS production, and cell death. One interpretation is that maintaining NF-kB signalling may prove beneficial in reducing mitochondrial dysfunction and heart failure in cancer patients undergoing Doxorubicin chemotherapy.
Galan-Arriola et al.62 performed a study of anthracycline-induced cardiotoxicity in pigs and showed that cumulative exposure to doxorubicin significantly reduced LV ejection fraction and extensive mitochondrial fragmentation. Remote ischemic preconditioning (RIPC) applied before each doxorubicin cycle preserved cardiac contractility and LV ejection fraction in long-term cardiac MRI exams. RIPC prevented doxorubicin-induced irreversible mitochondrial fragmentation and dysregulated autophagy. They concluded that RIPC is an attractive strategy for treating anthracycline-induced cardiotoxicity in patients.
Ritterhoff et al.63 identified a role for metabolic remodelling in cardiac hypertrophy by using an in vitro model of phenylephrine-induced hypertrophy in primary adult rat cardiomyocytes, and an in vivo model of pressure overload-induced cardiac hypertrophy. They found that an increase in glucose consumption supports the aspartate synthesis that drives the increase of biomass during cardiac hypertrophy. Conversely, preservation of fatty acid oxidation prevents this metabolic shift, thus preventing cardiac hypertrophy.
8. Counteracting drug-induced cardiotoxicity: new insights for ad hoc cardioprotection
Myocardial dysfunction is often reported as a long-term complication of chemotherapy-based treatments in cancer survivors. For example, anthracycline formulations such as doxorubicin are widely used as effective oncological drugs against several tumours and cancers; yet, as major drawbacks, they also induce cumulative cardiotoxic effects leading to hypertension, arrhythmias, and congestive heart failure.64–66 Despite recent improvements in the field of cardio-oncology, no general consensus has yet been reached on the most effective strategy to maximally exploit oncological drug potential while minimizing cardiac injury. In 2020, a number of important studies were published describing novel therapeutic and diagnostic strategies and providing useful insights into the mechanisms underlying the detrimental effects of doxorubicin on cardiac tissue.
Milano et al.67 developed an original, preclinical rat model of chemotherapy-induced cardiotoxicity and chronic ventricular dysfunction, based on the dual administration of the monoclonal antibody Trastuzumab and doxorubicin, which simulates the current clinical protocol for HER2-positive breast cancer.67 Human cardiac stromal cell-derived exosomes were administered systemically and repeatedly in-between doxorubicin and Trastuzumab doses. Notably, this was able to counteract chemotherapy-induced cardiac fibrosis and LV dysfunction, while curbing inflammatory cell infiltration by means of the horizontal transfer of microRNA (miR-146a-5p).67
Another thought-provoking therapeutic approach has been recently proposed to prevent anthracycline-induced cardiomyopathy by means of gene therapy with pharmacological upregulation of telomerase in cardiomyocytes.68 The rationale of this approach was based on the significant pro-survival results obtained following AAV9 gene therapy for telomerase (Tert) cardiomyocyte overexpression after MI in the adult mouse,69 along with the TERT polymerase’s function in eliminating mitochondrial ROS in compromised arterioles of patients with coronary artery disease.70 By translating such findings in the anthracycline cardiotoxicity scenario, the authors provided new understandings on the ectopic expression of TERT targeting mitochondrial mechanisms, thus offering a possible therapeutic approach to promote cardiomyocyte preservation.
Although doxorubicin is well known for its pleiotropic detrimental effects on cardiomyocyte viability and metabolism—including DNA damage, generation of ROS, and mitochondria impairment—the details of the molecular mechanisms underlying its cardiotoxic effects remain unclear. Nevertheless, this understanding is needed to allow optimization of ad hoc cardioprotective approaches. Han et al.71 recently investigated the role of circular RNAs (circRNAs) in an in vitro system based on iPSC-derived cardiomyocytes exposed to doxorubicin. A circRNA generated from the ITCH gene (CircITCH) was found to significantly decrease cardiomyocyte sensitivity to doxorubicin, by antagonizing miR-330-5p and upregulating sirtuin 6, surviving, and SERCA2a expression.71 Interestingly, CircITCH was found to be downregulated in hearts from patients with doxorubicin -induced cardiomyopathy and in doxorubicin-treated iPS-cardiomyocytes. Conversely, AAV9-mediated overexpression of human CircITCH in murine hearts counteracted doxorubicin detrimental influence on cardiac function, thus raising its potential as a theragnostic candidate for early diagnosis of anthracycline-induced cardiotoxicity.
A recent genetic screen conducted in zebrafish shed new light on the role of endothelial cells in antagonizing doxorubicin damage; indeed, retinoid X receptor alpha a (i.e. the fish orthologue of the human Retinoid X receptor alpha) was shown to exert cardioprotective effects by rescuing the compromised endothelial barrier in anthracycline-induced cardiotoxicity. These findings advocate the relevance of considering cardiovascular cell lineages other than cardiomyocytes as therapeutic target against drug-related cardiotoxicity.72 In such a perspective, cardiac resident macrophages were also shown to operate as immune modulators in reducing adverse cardiac remodelling during doxorubicin-elicited cardiomyopathy, with their self-renewal potential tightly regulated by the cardioprotective scavenger receptor SR-A1.73
Last year also witnessed the implementation of 3D cell-based platforms to address the unmet need for comprehensive drug screening with the evaluation of cardiotoxicity effects. Indeed, a human cardiac organoid disease model with chronic adrenergic stimulation was optimized by combining iPS-cardiomyocyte biology with a tissue engineering approach.74 This organotypic construct recapitulated the major features of ischaemic infarcted myocardium including pathological metabolic shifts, fibrosis and impaired calcium handling.74 Nonetheless, it was also successfully validated to mimic hypoxia-enhanced doxorubicin detrimental effects, thus offering a useful tool to model drug-induced exacerbation of cardiotoxicity for oncological patients.74
Timely recognition of the early signs of cancer therapy-derived cardiotoxicity is of utmost importance to minimize the incidence of myocardial damage and heart failure in cancer survivors. However, reliable diagnostic markers to rapidly detect the early onset of doxorubicin-induced cardiomyopathy are currently missing. The impairment of cardiac energetics is a major aspect of doxorubicin-related heart failure. In this regard, various imaging techniques have been recently proposed to evaluate heart metabolic fluxes and assess cardiac mitochondrial metabolism. Timm et al.75 recently illustrated the application of hyperpolarized magnetic resonance imaging (MRI) in a rat preclinical model of doxorubicin-induced heart failure. This strategy revealed that a change in oxidative carbohydrate metabolism can be used as an advance warning of myocardial dysfunction due to cardiac mitochondria alterations.75 These data open up the possibility of early detection of doxorubicin-induced cardiac damage in the clinical setting.
Cardiotoxicity can be caused by drugs other than chemotherapeutic agents and is, in fact, often the cause for clinical failure or withdrawal of drugs from the market. An interesting approach has been developed to reveal the ‘hidden cardiotoxicity’ of drugs, which is defined as the cardiotoxicity of a drug that manifests in the diseased heart but not in the healthy heart, or as a drug-induced deterioration of cardiac stress adaptation. Brenner et al.76 revisited the COX-2 inhibitor rofecoxib, which was withdrawn from the market due to increased cardiovascular risk, and showed that it increased acute mortality in rats subject to ischaemia and reperfusion, due to its proarrhythmic effect.
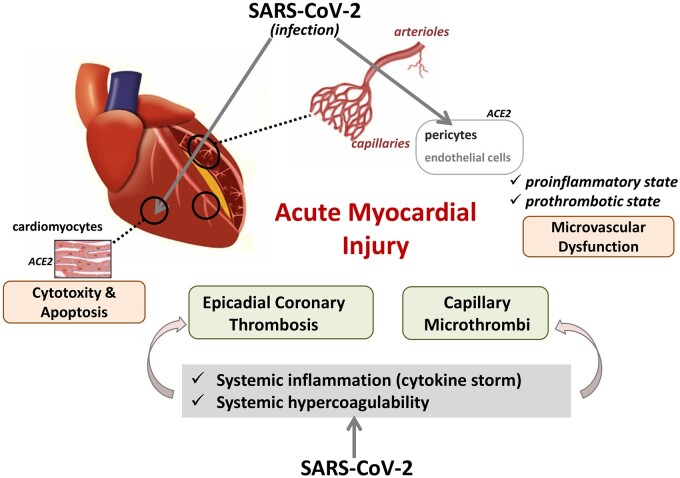
9. SARS-CoV-2—a new threat for the heart?
Coronavirus disease 2019 (COVID-19), caused by the virus SARS-CoV-2, predominantly affects the respiratory system. Nevertheless, since the pandemic onset there is accumulating evidence that SARS-CoV-2 infection frequently presents with cardiovascular complications and acute myocardial injury,77 as indicated by significantly elevated levels of troponin-T and NT-proBNP, associated with greater disease severity and worse outcomes.78 The underlying mechanisms for cardiac damage in COVID-19 remain uncertain. Studies performed during 2020 considered different possibilities ranging from primary viral infection of the cardiac tissue to myocardial microvascular dysfunction, microthrombosis and cardiac damage secondary to lung damage or systemic inflammation (massive inflammatory response/cytokine storm) and hypoxia—processes that occur during disease progression (Figure 4).
Figure 4.
Proposed mechanisms of acute myocardial injury (AMI) related to SARS-CoV-2 infection. AMI may result from primary viral infection of cardiac tissue inducing cytotoxicity and apoptosis of cardiomyocyte cells, or of pericytes and endothelial of the myocardial capillaries resulting in microvascular dysfunction. In addition, AMI may be secondary to systemic inflammation and hypercoagulability—processes that occur during the disease evolution and may derive towards the generation of capillary microthrombi in the heart or epicardial coronary thrombosis.
SARS-CoV-2 infects human cells via binding of its glycosylated envelope spike proteins to the angiotensin converting enzyme 2 (ACE2) receptor of host cells.79 The potential susceptibility of the human heart to SARS-CoV-2 infection was evidenced by Chen et al.,80 who showed a consistent presence of ACE2 in cardiac tissue, with expression levels even higher than those in the lung, by carrying out a comparative screen of ACE2 mRNA expression in different human organs based on the GTEx database. According to data obtained from single-cell RNA sequencing, cardiomyocytes and pericytes were identified as the cells with the highest expression of ACE2 in the heart, with ACE2 expression detected at a lower level in other major cells isolated from myocardial tissue, including endothelial cells, fibroblasts, and leucocytes.80,81 Of note, Nicin et al.81 identified cardiomyocytes as the cell type with the highest ACE2 expression, with ACE2 levels significantly elevated in the cardiomyocytes of patients with heart disease of different aetiology compared to healthy controls. On the contrary, the study by Chen and colleagues80 revealed the highest ACE2 expression specifically in mural pericytes. Thus, the authors concluded that pericytes might act as the target cardiac cell of SARS-CoV-2, subsequently disturbing the microvascular environment of the myocardium.
The hypothesis that SARS-CoV-2 can reside within the heart and, as a consequence, directly induce myocardial injury was evidenced by RT-PCR82 and electron microscopy83 in two independent studies, which demonstrated the presence of viral particles in cardiac biopsies from COVID-19 patients. In addition, two studies using human iPSC-CMs provided evidence that these cardiomyocytes are susceptible to SARS-CoV-2 infection in vitro via ACE2.84,85 Bojkova et al.84 further demonstrated the presence of intracellular double-stranded SARS-CoV-2 RNA and expression of the viral spike glycoprotein after incubating human iPSC-CMs with two different strains of the virus. In addition, they detected viral spike protein expression and viral particles in living human heart slices, derived from explanted hearts, after infection with the SARS-CoV-2 strains in vitro. SARS-CoV-2 infection-induced cytotoxicity and apoptotic effects associated with decreased α-sarcomeric actinin signal and inhibition of beating of cardiomyocytes in the in vitro studies.85 Furthermore, Bojkova et al. presented evidence that SARS-CoV-2 undergoes a full replication cycle when infecting cardiomyocytes and that cathepsins are likely involved, in addition to ACE2, in cardiomyocyte infection. Interestingly, transcriptional analysis of human iPSC-CMs showed that SARS-CoV-2 infection activates immune responses, while it inhibits the expression of genes involved in cellular metabolism and suppresses ACE2 expression.
It must be recognized that the relevance of these in vitro studies was in demonstrating the possibility for iPSC-derived cardiomyocyte infection by SARS-CoV-2, and they do not provide direct evidence of infection of cardiomyocytes in vivo. However, as proof-of-concept, the authors identified SARS-CoV-2 particles by electron microscopy in cardiomyocytes of an endocardial biopsy sample obtained from a young male COVID-19 patient with severe lung injury and reduced right and left ventricular ejection fraction.84 In contrast, however, a more recent study, focussed on post-mortem immunohistochemical, structural, and molecular evaluation of cardiac series of patients who died from active or cleared SARS-CoV-2 infection, did not find definitive evidence of direct myocardial injury by the virus.86 Instead, Bois et al. highlighted microthrombosis of the small myocardial vasculature in the heart as a relatively common finding in COVID-19 patients even in the absence of acute ischaemic injury. In this respect, among the various mechanisms underlying myocardial injury in COVID-19 patients that have been hypothesized since the origin of the disease in December 2019, the importance of microvascular damage is increasingly recognized, most likely due to endothelial cell dysfunction and formation of microscopic blood clots (summarized in Ostergaard (2021)87 and Roshdy et al. (2020)88). In addition, acute coronary syndrome due to coronary thrombotic events from atherosclerotic plaque rupture has been confirmed as a major cardiovascular clinical manifestation of COVID-19.89
Systemic hypercoagulability, with major elevation of D-dimer and fibrin/fibrinogen-degradation products, is considered a main cause of organ failure in severe COVID-19 cases. Thus, SARS-CoV-2- induced endothelial dysfunction may result in a procoagulant condition with relevant consequences, either on epicardial coronary thrombosis, or on generation of capillary microthrombi in the heart.
In line with the study by Bois et al.,86 a more recently published systematic pathologic analysis of hearts from patients dying of COVID-19 infection has reported 35% of cases with evidence of cardiac injury and identified microthrombi in myocardial capillaries, arterioles, and small muscular arteries as the leading cause of myocyte necrosis.90 It is noteworthy that neither transmission electronic microscopy (TEM) nor in situ-hybridization analysis evidence the presence of virus particles within endothelial cells in vessels with and without microthrombi in this study. Interestingly, by performing immunohistochemical analysis, Pellegrini et al.90 found that microthrombi were distinctly different in composition, with greater fibrin and c5-9 complement content, as compared to epicardial coronary thrombus aspirates from STEMI patients.
Supporting the effects of SARS-CoV-2 infection on the heart microvasculature, Maccio et al.91 provided evidence of SARS-CoV-2 specifically affecting capillaries, arterioles, and venules in a recent post-mortem study of cardiac tissue from COVID-19 patients. By immunohistochemical and histological evaluation of the entire coronary tree, the authors identified high endothelial ACE2 receptor expression specifically located in small epicardial vessels and lympho-monocytic inflammation increasing towards the small vessels, without involving the major coronary arteries. In addition, Fox et al.92 reported the presence of swollen endothelial cells in small arterioles, capillaries, and venules of hearts obtained from COVID-19 patients, who died of respiratory failure, without identifying large areas of myocyte necrosis, nor significant interstitial lymphocytic infiltrate.
Uncontrolled inflammation, associated with high levels of circulating cytokines, is thought to be a major cause of disease severity in COVID-19 and one of the suggested underlying mechanisms to induce cardiac damage in COVID-19 patients. In this regard, Basso et al.,93 by performing a systematic immunohistochemical analysis of cardiac tissue, obtained at autopsy from patients dying of COVID-19 due to respiratory failure, evidenced increased interstitial myocardial macrophage infiltration in the majority of patients (86%) and changes consistent with lymphocytic myocarditis in a small number of cases. The authors suggested that increased levels of myocardial macrophages in these COVID-19 patients resulted from high systemic levels of pro-inflammatory cytokines, since no causative relationship between SARS-CoV-2 and myocardial inflammation could be established. Consistent with this view, Del Valle et al.94 demonstrated that early cytokine measurements in COVID-19 patients are reliable predictors of disease course and outcome. The authors implemented a rapid multiplex cytokine assay and analysed blood samples on the day of hospital admission, in two independent cohorts of 1484 patients and 231 patients. Their results demonstrated that elevated levels of interleukin (IL)-6 and tumour necrosis factor (TNF)-α at hospitalization serve as strong predictors of disease severity and propose their use in stratification of patients with COVID-19.
10. Conclusion
As can be seen from the preceding sections, many exciting advances were made in cardiology in 2020. We wish to acknowledge the dedication and determination of the researchers worldwide who have produced the outstanding research we have discussed in this review, in addition to all the research we did not have space to include. From the junior postgraduate students travailing in the lab, to the most senior internationally renowned scientific leaders, it is interesting to look back and see what has been achieved in a difficult year. No doubt, there will be new challenges and changes to navigate—altered research funding priorities, changed working practises, greater reliance on web-based communication. But there will also be new opportunities. COVID-19 will surely remain an important topic of investigation, and studies of the potential long-term cardiovascular effects will require investigation. We look forward to seeing the progress that will be made in cardiovascular research in the following years.
Author contributions
T.P., S.B., D.D., P.E., I.H., G.V., and S.D. drafted the initial manuscript. T.G., J.Woj., C.W., J.Wal and all authors revised the manuscript.
Funding
This work was supported by the Hatter Cardiovascular Institute [to S.M.D.] and the British Heart Foundation [PG/18/44/33790 to S.M.D.; RG/19/10/34506 to P.C.E.]. T.P. is funded by the Spanish Ministry of Health-Institute of Health Carlos III [PI19/01687] and G.V. by the Spanish Ministry of Science and Innovation [PGC2018-094025-B-I00] and FEDER ‘Una Manera de Hacer Europa’. S.B. is funded by University of Genova, Genova, Italy, ‘Curiosity Driven’ grant. D.J.D. acknowledges support from the Netherlands CardioVascular Research Initiative financially supported by the Dutch Heart Foundation (CVON2014-RECONNECT and CVON2017-ARENA PRIME). T.J.G. is funded by European Research Council (CoG-2016-InflammaTENSION).
Conflict of interest: G.V. and T.P. are co-founders of the Spin-offs Glycardial Diagnostics SL. and IVESTATIN Therapeutics SL. J.Wal received honorarium from Daiichi-Sankyo and consultancy fees from Boehringer Ingelheim. T.J.G. received honoraria from Merck.
Data availability
No data included.
The first two authors contributed equally to the study.
References
- 1.Gao C, Wang R, Li B, Guo Y, Yin T, Xia Y, Zhang F, Lian K, Liu Y, Wang H, Zhang L, Gao E, Yan W, Tao L.. TXNIP/Redd1 signalling and excessive autophagy: a novel mechanism of myocardial ischaemia/reperfusion injury in mice. Cardiovasc Res 2020;116:645–657. [DOI] [PubMed] [Google Scholar]
- 2.Liu J, Yang C, Liu T, Deng Z, Fang W, Zhang X, Li J, Huang Q, Liu C, Wang Y, Yang D, Sukhova GK, Lindholt JS, Diederichsen A, Rasmussen LM, Li D, Newton G, Luscinskas FW, Liu L, Libby P, Wang J, Guo J, Shi GP.. Eosinophils improve cardiac function after myocardial infarction. Nat Commun 2020;11:6396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dehghani T, Thai PN, Sodhi H, Ren L, Sirish P, Nader CE, Timofeyev V, Overton JL, Li X, Lam KS, Chiamvimonvat N, Panitch A.. Selectin-targeting glycosaminoglycan-peptide conjugate limits neutrophil mediated cardiac reperfusion injury. Cardiovasc Res 2020;cvaa312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mendieta G, Ben-Aicha S, Gutiérrez M, Casani L, Aržanauskaitė M, Carreras F, Sabate M, Badimon L, Vilahur G.. Intravenous statin administration during myocardial infarction compared with oral post-infarct administration. J Am Coll Cardiol 2020;75:1386–1402. [DOI] [PubMed] [Google Scholar]
- 5.Li L, Li H, Tien CL, Jain MK, Zhang L.. Kruppel-like factor 15 regulates the circadian susceptibility to ischemia reperfusion injury in the heart. Circulation 2020;141:1427–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bar C, Chatterjee S, Falcao Pires I, Rodrigues P, Sluijter JPG, Boon RA, Nevado RM, Andres V, Sansonetti M, de Windt L, Ciccarelli M, Hamdani N, Heymans S, Figuinha Videira R, Tocchetti CG, Giacca M, Zacchigna S, Engelhardt S, Dimmeler S, Madonna R, Thum T.. Non-coding RNAs: update on mechanisms and therapeutic targets from the ESC Working Groups of Myocardial Function and Cellular Biology of the Heart. Cardiovasc Res 2020;116:1805–1819. [DOI] [PubMed] [Google Scholar]
- 7.Viereck J, Bührke A, Foinquinos A, Chatterjee S, Kleeberger JA, Xiao K, Janssen-Peters H, Batkai S, Ramanujam D, Kraft T, Cebotari S, Gueler F, Beyer AM, Schmitz J, Bräsen JH, Schmitto JD, Gyöngyösi M, Löser A, Hirt MN, Eschenhagen T, Engelhardt S, Bär C, Thum T.. Targeting muscle-enriched long non-coding RNA H19 reverses pathological cardiac hypertrophy. Eur Heart J 2020;41:3462–3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin H, Li Y, Zhu H, Wang Q, Chen Z, Chen L, Zhu Y, Zheng C, Wang Y, Liao W, Bin J, Kitakaze M, Liao Y.. Lansoprazole alleviates pressure overload-induced cardiac hypertrophy and heart failure in mice by blocking the activation of beta-catenin. Cardiovasc Res 2020;116:101–113. [DOI] [PubMed] [Google Scholar]
- 9.Perrino C, Ferdinandy P, Bøtker HE, Brundel BJJM, Collins P, Davidson SM, den Ruijter HM, Engel FB, Gerdts E, Girao H, Gyöngyösi M, Hausenloy DJ, Lecour S, Madonna R, Marber M, Murphy E, Pesce M, Regitz-Zagrosek V, Sluijter JPG, Steffens S, Gollmann-Tepeköylü C, Van Laake LW, Van Linthout S, Schulz R, Ytrehus K.. Improving translational research in sex-specific effects of comorbidities and risk factors in ischaemic heart disease and cardioprotection: position paper and recommendations of the ESC Working Group on Cellular Biology of the Heart. Cardiovasc Res 2021;117:367–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schreckenberg R, Klein J, Kutsche HS, Schulz R, Gomori K, Bencsik P, Benczik B, Agg B, Saghy E, Ferdinandy P, Schluter KD.. Ischaemic post-conditioning in rats: responder and non-responder differ in transcriptome of mitochondrial proteins. J Cell Mol Med 2020;24:5528–5541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Porrello ER, Mahmoud AI, Simpson E, Hill JA, Richardson JA, Olson EN, Sadek HA.. Transient regenerative potential of the neonatal mouse heart. Science 2011;331:1078–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volland C, Schott P, Didié M, Männer J, Unsöld B, Toischer K, Schmidt C, Urlaub H, Nickels K, Knöll R, Schmidt A, Guan K, Hasenfuß G, Seidler T.. Control of p21Cip by BRCA1-associated protein is critical for cardiomyocyte cell cycle progression and survival. Cardiovasc Res 2020;116:592–604. [DOI] [PubMed] [Google Scholar]
- 13.Blom JN, Feng Q.. Cardiac repair by epicardial EMT: current targets and a potential role for the primary cilium. Pharmacol Ther 2018;186:114–129. [DOI] [PubMed] [Google Scholar]
- 14.Smart N, Bollini S, Dube KN, Vieira JM, Zhou B, Davidson S, Yellon D, Riegler J, Price AN, Lythgoe MF, Pu WT, Riley PR.. De novo cardiomyocytes from within the activated adult heart after injury. Nature 2011;474:640–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aharonov A, Shakked A, Umansky KB, Savidor A, Genzelinakh A, Kain D, Lendengolts D, Revach OY, Morikawa Y, Dong J, Levin Y, Geiger B, Martin JF, Tzahor E.. ERBB2 drives YAP activation and EMT-like processes during cardiac regeneration. Nat Cell Biol 2020;22:1346–1356. [DOI] [PubMed] [Google Scholar]
- 16.Wu CC, Jeratsch S, Graumann J, Stainier DYR.. Modulation of mammalian cardiomyocyte cytokinesis by the extracellular matrix. Circ Res 2020;127:896–907. [DOI] [PubMed] [Google Scholar]
- 17.Henri O, Pouehe C, Houssari M, Galas L, Nicol L, Edwards-Levy F, Henry JP, Dumesnil A, Boukhalfa I, Banquet S, Schapman D, Thuillez C, Richard V, Mulder P, Brakenhielm E.. Selective stimulation of cardiac lymphangiogenesis reduces myocardial edema and fibrosis leading to improved cardiac function following myocardial infarction. Circulation 2016;133:1484–1497; discussion 1497. [DOI] [PubMed] [Google Scholar]
- 18.Klotz L, Norman S, Vieira JM, Masters M, Rohling M, Dube KN, Bollini S, Matsuzaki F, Carr CA, Riley PR.. Cardiac lymphatics are heterogeneous in origin and respond to injury. Nature 2015;522:62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vieira JM, Norman S, Villa Del Campo C, Cahill TJ, Barnette DN, Gunadasa-Rohling M, Johnson LA, Greaves DR, Carr CA, Jackson DG, Riley PR.. The cardiac lymphatic system stimulates resolution of inflammation following myocardial infarction. J Clin Invest 2018;128:3402–3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu X, De la Cruz E, Gu X, Balint L, Oxendine-Burns M, Terrones T, Ma W, Kuo HH, Lantz C, Bansal T, Thorp E, Burridge P, Jakus Z, Herz J, Cleaver O, Torres M, Oliver G.. Lymphoangiocrine signals promote cardiac growth and repair. Nature 2020;588:705–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aurora AB, Porrello ER, Tan W, Mahmoud AI, Hill JA, Bassel-Duby R, Sadek HA, Olson EN.. Macrophages are required for neonatal heart regeneration. J Clin Invest 2014;124:1382–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nicolás-Ávila JA, Lechuga-Vieco AV, Esteban-Martínez L, Sánchez-Díaz M, Díaz-García E, Santiago DJ, Rubio-Ponce A, Li JL, Balachander A, Quintana JA, Martínez-de-Mena R, Castejón-Vega B, Pun-García A, Través PG, Bonzón-Kulichenko E, García-Marqués F, Cussó L, A-González N, González-Guerra A, Roche-Molina M, Martin-Salamanca S, Crainiciuc G, Guzmán G, Larrazabal J, Herrero-Galán E, Alegre-Cebollada J, Lemke G, Rothlin CV, Jimenez-Borreguero LJ, Reyes G, Castrillo A, Desco M, Muñoz-Cánoves P, Ibáñez B, Torres M, Ng LG, Priori SG, Bueno H, Vázquez J, Cordero MD, Bernal JA, Enríquez JA, Hidalgo A.. A network of macrophages supports mitochondrial homeostasis in the heart. Cell 2020;183:94–109.e123. [DOI] [PubMed] [Google Scholar]
- 23.Bartelt A, Weber C.. Mitochondrial ejection for cardiac protection: the macrophage connection. Cell Metab 2020;32:512–513. [DOI] [PubMed] [Google Scholar]
- 24.Li Y, Li H, Pei J, Hu S, Nie Y.. Transplantation of murine neonatal cardiac macrophage improves adult cardiac repair. Cell Mol Immunol 2021;18:492–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Driessen MM, Hui W, Bijnens BH, Dragulescu A, Mertens L, Meijboom FJ, Friedberg MK.. Adverse ventricular-ventricular interactions in right ventricular pressure load: insights from pediatric pulmonary hypertension versus pulmonary stenosis. Physiol Rep 2016;4:e12833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vriz O, Pirisi M, Bossone E, Fadl ElMula FEM, Palatini P, Naeije R.. Right ventricular-pulmonary arterial uncoupling in mild-to-moderate systemic hypertension. J Hypertens 2020;38:274–281. [DOI] [PubMed] [Google Scholar]
- 27.Ye L, Wang S, Xiao Y, Jiang C, Huang Y, Chen H, Zhang H, Zhang H, Liu J, Xu Z, Hong H.. Pressure overload greatly promotes neonatal right ventricular cardiomyocyte proliferation: a new model for the study of heart regeneration. J Am Heart Assoc 2020;9:e015574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kupfer ME, Lin WH, Ravikumar V, Qiu K, Wang L, Gao L, Bhuiyan DB, Lenz M, Ai J, Mahutga RR, Townsend D, Zhang J, McAlpine MC, Tolkacheva EG, Ogle BM.. In situ expansion, differentiation, and electromechanical coupling of human cardiac muscle in a 3D bioprinted, chambered organoid. Circ Res 2020;127:207–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang K, Ozpinar EW, Su T, Tang J, Shen D, Qiao L, Hu S, Li Z, Liang H, Mathews K, Scharf V, Freytes DO, Cheng K.. An off-the-shelf artificial cardiac patch improves cardiac repair after myocardial infarction in rats and pigs. Sci Transl Med 2020;12:eaat9683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Han X, Zhou Z, Fei L, Sun H, Wang R, Chen Y, Chen H, Wang J, Tang H, Ge W, Zhou Y, Ye F, Jiang M, Wu J, Xiao Y, Jia X, Zhang T, Ma X, Zhang Q, Bai X, Lai S, Yu C, Zhu L, Lin R, Gao Y, Wang M, Wu Y, Zhang J, Zhan R, Zhu S, Hu H, Wang C, Chen M, Huang H, Liang T, Chen J, Wang W, Zhang D, Guo G.. Construction of a human cell landscape at single-cell level. Nature 2020;581:303–309. [DOI] [PubMed] [Google Scholar]
- 31.Litviňuková M, Talavera-López C, Maatz H, Reichart D, Worth CL, Lindberg EL, Kanda M, Polanski K, Heinig M, Lee M, Nadelmann ER, Roberts K, Tuck L, Fasouli ES, DeLaughter DM, McDonough B, Wakimoto H, Gorham JM, Samari S, Mahbubani KT, Saeb-Parsy K, Patone G, Boyle JJ, Zhang H, Zhang H, Viveiros A, Oudit GY, Bayraktar OA, Seidman JG, Seidman CE, Noseda M, Hubner N, Teichmann SA.. Cells of the adult human heart. Nature 2020;588:466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ruiz-Villalba A, Romero JP, Hernández SC, Vilas-Zornoza A, Fortelny N, Castro-Labrador L, San Martin-Uriz P, Lorenzo-Vivas E, García-Olloqui P, Palacio M, Gavira JJ, Bastarrika G, Janssens S, Wu M, Iglesias E, Abizanda G, de Morentin XM, Lasaga M, Planell N, Bock C, Alignani D, Medal G, Prudovsky I, Jin Y-R, Ryzhov S, Yin H, Pelacho B, Gomez-Cabrero D, Lindner V, Lara-Astiaso D, Prósper F.. Single-cell RNA sequencing analysis reveals a crucial role for CTHRC1 (collagen triple helix repeat containing 1) cardiac fibroblasts after myocardial infarction. Circulation 2020;142:1831–1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Suryawanshi H, Clancy R, Morozov P, Halushka MK, Buyon JP, Tuschl T.. Cell atlas of the foetal human heart and implications for autoimmune-mediated congenital heart block. Cardiovasc Res 2020;116:1446–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peet C, Ivetic A, Bromage DI, Shah AM.. Cardiac monocytes and macrophages after myocardial infarction. Cardiovasc Res 2020;116:1101–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bevan L, Lim ZW, Venkatesh B, Riley PR, Martin P, Richardson RJ.. Specific macrophage populations promote both cardiac scar deposition and subsequent resolution in adult zebrafish. Cardiovasc Res 2020;116:1357–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vagnozzi RJ, Maillet M, Sargent MA, Khalil H, Johansen AKZ, Schwanekamp JA, York AJ, Huang V, Nahrendorf M, Sadayappan S, Molkentin JD.. An acute immune response underlies the benefit of cardiac stem cell therapy. Nature 2020;577:405–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhao J, Florentin J, Tai YY, Torrino S, Ohayon L, Brzoska T, Tang Y, Yang J, Negi V, Woodcock CC, Risbano MG, Nouraie SM, Sundd P, Bertero T, Dutta P, Chan SY.. Long range endocrine delivery of circulating miR-210 to endothelium promotes pulmonary hypertension. Circ Res 2020;127:677–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aghajanian H, Kimura T, Rurik JG, Hancock AS, Leibowitz MS, Li L, Scholler J, Monslow J, Lo A, Han W, Wang T, Bedi K, Morley MP, Linares Saldana RA, Bolar NA, McDaid K, Assenmacher CA, Smith CL, Wirth D, June CH, Margulies KB, Jain R, Pure E, Albelda SM, Epstein JA.. Targeting cardiac fibrosis with engineered T cells. Nature 2019;573:430–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moreira LM, Takawale A, Hulsurkar M, Menassa DA, Antanaviciute A, Lahiri SK, Mehta N, Evans N, Psarros C, Robinson P, Sparrow AJ, Gillis MA, Ashley N, Naud P, Barallobre-Barreiro J, Theofilatos K, Lee A, Norris M, Clarke MV, Russell PK, Casadei B, Bhattacharya S, Zajac JD, Davey RA, Sirois M, Mead A, Simmons A, Mayr M, Sayeed R, Krasopoulos G, Redwood C, Channon KM, Tardif JC, Wehrens XHT, Nattel S, Reilly S.. Paracrine signalling by cardiac calcitonin controls atrial fibrogenesis and arrhythmia. Nature 2020;587:460–465. [DOI] [PubMed] [Google Scholar]
- 40.Yan W, Lin C, Guo Y, Chen Y, Du Y, Lau WB, Xia Y, Zhang F, Su R, Gao E, Wang Y, Li C, Liu R, Ma XL, Tao L.. N-cadherin overexpression mobilizes the protective effects of mesenchymal stromal cells against ischemic heart injury through a beta-catenin-dependent manner. Circ Res 2020;126:857–874. [DOI] [PubMed] [Google Scholar]
- 41.Gao L, Mei S, Zhang S, Qin Q, Li H, Liao Y, Fan H, Liu Z, Zhu H.. Cardio-renal exosomes in myocardial infarction serum regulate proangiogenic paracrine signaling in adipose mesenchymal stem cells. Theranostics 2020;10:1060–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kurtzwald-Josefson E, Zeevi-Levin N, Rubchevsky V, Bechar Erdman N, Schwartz Rohaker O, Nahum O, Hochhauser E, Ben-Avraham B, Itskovitz-Eldor J, Aravot D, Barac YD.. Cardiac fibroblast-induced pluripotent stem cell-derived exosomes as a potential therapeutic mean for heart failure. Int J Mol Sci 2020;21:7215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lew JK, Pearson JT, Saw E, Tsuchimochi H, Wei M, Ghosh N, Du CK, Zhan DY, Jin M, Umetani K, Shirai M, Katare R, Schwenke DO.. Exercise regulates microRNAs to preserve coronary and cardiac function in the diabetic heart. Circ Res 2020;127:1384–1400. [DOI] [PubMed] [Google Scholar]
- 44.Li H, Xu JD, Fang XH, Zhu JN, Yang J, Pan R, Yuan SJ, Zeng N, Yang ZZ, Yang H, Wang XP, Duan JZ, Wang S, Luo JF, Wu SL, Shan ZX.. Circular RNA circRNA_000203 aggravates cardiac hypertrophy via suppressing miR-26b-5p and miR-140-3p binding to Gata4. Cardiovasc Res 2020;116:1323–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang P, Wang L, Li Q, Tian X, Xu J, Xu J, Xiong Y, Chen G, Qian H, Jin C, Yu Y, Cheng K, Qian L, Yang Y.. Atorvastatin enhances the therapeutic efficacy of mesenchymal stem cells-derived exosomes in acute myocardial infarction via up-regulating long non-coding RNA H19. Cardiovasc Res 2020;116:353–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kagaya Y, Ito K, Takahashi J, Matsumoto Y, Shiroto T, Tsuburaya R, Kikuchi Y, Hao K, Nishimiya K, Shindo T, Ogata T, Kurosawa R, Eguchi K, Monma Y, Ichijo S, Hatanaka K, Miyata S, Shimokawa H.. Low-energy cardiac shockwave therapy to suppress left ventricular remodeling in patients with acute myocardial infarction: a first-in-human study. Coron Artery Dis 2018;29:294–300. [DOI] [PubMed] [Google Scholar]
- 47.Gollmann-Tepekoylu C, Polzl L, Graber M, Hirsch J, Nagele F, Lobenwein D, Hess MW, Blumer MJ, Kirchmair E, Zipperle J, Hromada C, Muhleder S, Hackl H, Hermann M, Al Khamisi H, Forster M, Lichtenauer M, Mittermayr R, Paulus P, Fritsch H, Bonaros N, Kirchmair R, Sluijter JPG, Davidson S, Grimm M, Holfeld J.. miR-19a-3p containing exosomes improve function of ischaemic myocardium upon shock wave therapy. Cardiovasc Res 2020;116:1226–1236. [DOI] [PubMed] [Google Scholar]
- 48.Liu S, Chen X, Bao L, Liu T, Yuan P, Yang X, Qiu X, Gooding JJ, Bai Y, Xiao J, Pu F, Jin Y.. Treatment of infarcted heart tissue via the capture and local delivery of circulating exosomes through antibody-conjugated magnetic nanoparticles. Nat Biomed Eng 2020;4:1063–1075. [DOI] [PubMed] [Google Scholar]
- 49.Chandy M, Rhee JW, Ozen MO, Williams DR, Pepic L, Liu C, Zhang H, Malisa J, Lau E, Demirci U, Wu JC.. Atlas of exosomal microRNAs secreted from human iPSC-derived cardiac cell types. Circulation 2020;142:1794–1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Benzoni P, Campostrini G, Landi S, Bertini V, Marchina E, Iascone M, Ahlberg G, Olesen MS, Crescini E, Mora C, Bisleri G, Muneretto C, Ronca R, Presta M, Poliani PL, Piovani G, Verardi R, Di Pasquale E, Consiglio A, Raya A, Torre E, Lodrini AM, Milanesi R, Rocchetti M, Baruscotti M, DiFrancesco D, Memo M, Barbuti A, Dell'Era P.. Human iPSC modelling of a familial form of atrial fibrillation reveals a gain of function of If and ICaL in patient-derived cardiomyocytes. Cardiovasc Res 2020;116:1147–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Goversen B, van der Heyden MAG, van Veen TAB, de Boer TP.. The immature electrophysiological phenotype of iPSC-CMs still hampers in vitro drug screening: special focus on IK1. Pharmacol Ther 2018;183:127–136. [DOI] [PubMed] [Google Scholar]
- 52.Garbern JC, Helman A, Sereda R, Sarikhani M, Ahmed A, Escalante GO, Ogurlu R, Kim SL, Zimmerman JF, Cho A, MacQueen L, Bezzerides VJ, Parker KK, Melton DA, Lee RT.. Inhibition of mTOR signaling enhances maturation of cardiomyocytes derived from human-induced pluripotent stem cells via p53-induced quiescence. Circulation 2020;141:285–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pioner JM, Guan X, Klaiman JM, Racca AW, Pabon L, Muskheli V, Macadangdang J, Ferrantini C, Hoopmann MR, Moritz RL, Kim DH, Tesi C, Poggesi C, Murry CE, Childers MK, Mack DL, Regnier M.. Absence of full-length dystrophin impairs normal maturation and contraction of cardiomyocytes derived from human-induced pluripotent stem cells. Cardiovasc Res 2020;116:368–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lou X, Zhao M, Fan C, Fast VG, Valarmathi MT, Zhu W, Zhang J.. N-cadherin overexpression enhances the reparative potency of human-induced pluripotent stem cell-derived cardiac myocytes in infarcted mouse hearts. Cardiovasc Res 2020;116:671–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tao Z, Loo S, Su L, Tan S, Tee G, Gan SU, Zhang J, Chen X, Ye L.. Angiopoietin-1 enhanced myocyte mitosis, engraftment, and the reparability of hiPSC-CMs for treatment of myocardial infarction. Cardiovasc Res 2021;117:1578–1591. [DOI] [PubMed] [Google Scholar]
- 56.Huo J, Lu S, Kwong JQ, Bround MJ, Grimes KM, Sargent MA, Brown ME, Davis ME, Bers DM, Molkentin JD.. MCUb induction protects the heart from postischemic remodeling. Circ Res 2020;127:379–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Puente BN, Sun J, Parks RJ, Fergusson MM, Liu C, Springer DA, Aponte AM, Liu JC, Murphy E.. MICU3 plays an important role in cardiovascular function. Circ Res 2020;127:1571–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pan X, Liu J, Nguyen T, Liu C, Sun J, Teng Y, Fergusson MM, Rovira II, Allen M, Springer DA, Aponte AM, Gucek M, Balaban RS, Murphy E, Finkel T.. The physiological role of mitochondrial calcium revealed by mice lacking the mitochondrial calcium uniporter. Nat Cell Biol 2013;15:1464–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Parks RJ, Menazza S, Holmstrom KM, Amanakis G, Fergusson M, Ma H, Aponte AM, Bernardi P, Finkel T, Murphy E.. Cyclophilin D-mediated regulation of the permeability transition pore is altered in mice lacking the mitochondrial calcium uniporter. Cardiovasc Res 2019;115:385–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kolleritsch S, Kien B, Schoiswohl G, Diwoky C, Schreiber R, Heier C, Maresch LK, Schweiger M, Eichmann TO, Stryeck S, Krenn P, Tomin T, Schittmayer M, Kolb D, Rulicke T, Hoefler G, Wolinski H, Madl T, Birner-Gruenberger R, Haemmerle G.. Low cardiac lipolysis reduces mitochondrial fission and prevents lipotoxic heart dysfunction in Perilipin 5 mutant mice. Cardiovasc Res 2020;116:339–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dhingra R, Guberman M, Rabinovich-Nikitin I, Gerstein J, Margulets V, Gang H, Madden N, Thliveris J, Kirshenbaum LA.. Impaired NF-kappaB signalling underlies cyclophilin D-mediated mitochondrial permeability transition pore opening in doxorubicin cardiomyopathy. Cardiovasc Res 2020;116:1161–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Galan-Arriola C, Villena-Gutierrez R, Higuero-Verdejo MI, Diaz-Rengifo IA, Pizarro G, Lopez GJ, de Molina-Iracheta A, Perez-Martinez C, Garcia RD, Gonzalez-Calle D, Lobo M, Sanchez PL, Oliver E, Cordoba R, Fuster V, Sanchez-Gonzalez J, Ibanez B.. Remote ischemic preconditioning ameliorates anthracycline-induced cardiotoxicity and preserves mitochondrial integrity. Cardiovasc Res 2021;117:1132–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ritterhoff J, Young S, Villet O, Shao D, Neto FC, Bettcher LF, Hsu YA, Kolwicz SC Jr., Raftery D, Tian R.. Metabolic remodeling promotes cardiac hypertrophy by directing glucose to aspartate biosynthesis. Circ Res 2020;126:182–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McGowan JV, Chung R, Maulik A, Piotrowska I, Walker JM, Yellon DM.. Anthracycline chemotherapy and cardiotoxicity. Cardiovasc Drugs Ther 2017;31:63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Galan-Arriola C, Vilchez-Tschischke JP, Lobo M, Lopez GJ, de Molina-Iracheta A, Perez-Martinez C, Villena-Gutierrez R, Macias A, Diaz-Rengifo IA, Oliver E, Fuster V, Sanchez-Gonzalez J, Ibanez B.. Coronary microcirculation damage in anthracycline cardiotoxicity. Cardiovasc Res 2021:cvab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Raber I, Asnani A.. Cardioprotection in cancer therapy: novel insights with anthracyclines. Cardiovasc Res 2019;115:915–921. [DOI] [PubMed] [Google Scholar]
- 67.Milano G, Biemmi V, Lazzarini E, Balbi C, Ciullo A, Bolis S, Ameri P, Di Silvestre D, Mauri P, Barile L, Vassalli G.. Intravenous administration of cardiac progenitor cell-derived exosomes protects against doxorubicin/trastuzumab-induced cardiac toxicity. Cardiovasc Res 2020;116:383–392. [DOI] [PubMed] [Google Scholar]
- 68.Chatterjee S, Hofer T, Costa A, Lu D, Batkai S, Gupta SK, Bolesani E, Zweigerdt R, Megias D, Streckfuss-Bomeke K, Brandenberger C, Thum T, Bar C.. Telomerase therapy attenuates cardiotoxic effects of doxorubicin. Mol Ther 2021;29:1395–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bar C, Bernardes de Jesus B, Serrano R, Tejera A, Ayuso E, Jimenez V, Formentini I, Bobadilla M, Mizrahi J, de Martino A, Gomez G, Pisano D, Mulero F, Wollert KC, Bosch F, Blasco MA.. Telomerase expression confers cardioprotection in the adult mouse heart after acute myocardial infarction. Nat Commun 2014;5:5863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Beyer AM, Freed JK, Durand MJ, Riedel M, Ait-Aissa K, Green P, Hockenberry JC, Morgan RG, Donato AJ, Peleg R, Gasparri M, Rokkas CK, Santos JH, Priel E, Gutterman DD.. Critical role for telomerase in the mechanism of flow-mediated dilation in the human microcirculation. Circ Res 2016;118:856–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Han D, Wang Y, Wang Y, Dai X, Zhou T, Chen J, Tao B, Zhang J, Cao F.. The tumor-suppressive human circular RNA CircITCH sponges miR-330-5p to ameliorate doxorubicin-induced cardiotoxicity through upregulating SIRT6, Survivin, and SERCA2a. Circ Res 2020;127:e108–e125. [DOI] [PubMed] [Google Scholar]
- 72.Ma X, Zhu P, Ding Y, Zhang H, Qiu Q, Dvornikov AV, Wang Z, Kim M, Wang Y, Lowerison M, Yu Y, Norton N, Herrmann J, Ekker SC, Hsiai TK, Lin X, Xu X.. Retinoid X receptor alpha is a spatiotemporally predominant therapeutic target for anthracycline-induced cardiotoxicity. Sci Adv 2020;6:eaay2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang R, Lohray R, Chow E, Gangupantula P, Smith L, Draper R.. Selective uptake of carboxylated multi-walled carbon nanotubes by class A type 1 scavenger receptors and impaired phagocytosis in alveolar macrophages. Nanomaterials (Basel) 2020;10:2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Richards DJ, Li Y, Kerr CM, Yao J, Beeson GC, Coyle RC, Chen X, Jia J, Damon B, Wilson R, Starr Hazard E, Hardiman G, Menick DR, Beeson CC, Yao H, Ye T, Mei Y.. Human cardiac organoids for the modelling of myocardial infarction and drug cardiotoxicity. Nat Biomed Eng 2020;4:446–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Timm KN, Perera C, Ball V, Henry JA, Miller JJ, Kerr M, West JA, Sharma E, Broxholme J, Logan A, Savic D, Dodd MS, Griffin JL, Murphy MP, Heather LC, Tyler DJ.. Early detection of doxorubicin-induced cardiotoxicity in rats by its cardiac metabolic signature assessed with hyperpolarized MRI. Commun Biol 2020;3:692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Brenner GB, Makkos A, Nagy CT, Onodi Z, Sayour NV, Gergely TG, Kiss B, Gorbe A, Saghy E, Zadori ZS, Lazar B, Baranyai T, Varga RS, Husti Z, Varro A, Tothfalusi L, Schulz R, Baczko I, Giricz Z, Ferdinandy P.. Hidden cardiotoxicity of rofecoxib can be revealed in experimental models of ischemia/reperfusion. Cells 2020;9:551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, Madhur MS, Tomaszewski M, Maffia P, D'Acquisto F, Nicklin SA, Marian AJ, Nosalski R, Murray EC, Guzik B, Berry C, Touyz RM, Kreutz R, Wang DW, Bhella D, Sagliocco O, Crea F, Thomson EC, McInnes IB.. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res 2020;116:1666–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, Danilov T, Kukar N, Shaban N, Kini A, Camaj A, Bienstock SW, Rashed ER, Rahman K, Oates CP, Buckley S, Elbaum LS, Arkonac D, Fiter R, Singh R, Li E, Razuk V, Robinson SE, Miller M, Bier B, Donghi V, Pisaniello M, Mantovani R, Pinto G, Rota I, Baggio S, Chiarito M, Fazzari F, Cusmano I, Curzi M, Ro R, Malick W, Kamran M, Kohli-Seth R, Bassily-Marcus AM, Neibart E, Serrao G, Perk G, Mancini D, Reddy VY, Pinney SP, Dangas G, Blasi F, Sharma SK, Mehran R, Condorelli G, Stone GW, Fuster V, Lerakis S, Goldman ME.. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol 2020;76:2043–2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q.. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 2020;367:1444–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen L, Li X, Chen M, Feng Y, Xiong C.. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res 2020;116:1097–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nicin L, Abplanalp WT, Mellentin H, Kattih B, Tombor L, John D, Schmitto JD, Heineke J, Emrich F, Arsalan M, Holubec T, Walther T, Zeiher AM, Dimmeler S.. Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts. Eur Heart J 2020;41:1804–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wenzel P, Kopp S, Gobel S, Jansen T, Geyer M, Hahn F, Kreitner KF, Escher F, Schultheiss HP, Munzel T.. Evidence of SARS-CoV-2 mRNA in endomyocardial biopsies of patients with clinically suspected myocarditis tested negative for COVID-19 in nasopharyngeal swab. Cardiovasc Res 2020;116:1661–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, Sepe PA, Resasco T, Camporotondo R, Bruno R, Baldanti F, Paolucci S, Pelenghi S, Iotti GA, Mojoli F, Arbustini E.. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail 2020;22:911–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bojkova D, Wagner JUG, Shumliakivska M, Aslan GS, Saleem U, Hansen A, Luxan G, Gunther S, Pham MD, Krishnan J, Harter PN, Ermel UH, Frangakis AS, Milting H, Zeiher AM, Klingel K, Cinatl J, Dendorfer A, Eschenhagen T, Tschope C, Ciesek S, Dimmeler S.. SARS-CoV-2 infects and induces cytotoxic effects in human cardiomyocytes. Cardiovasc Res 2020;116:2207–2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sharma A, Garcia G Jr, Wang Y, Plummer JT, Morizono K, Arumugaswami V, Svendsen CN.. Human iPSC-derived cardiomyocytes are susceptible to SARS-CoV-2 infection. Cell Rep Med 2020;1:100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bois MC, Boire NA, Layman AJ, Aubry MC, Alexander MP, Roden AC, Hagen CE, Quinton RA, Larsen C, Erben Y, Majumdar R, Jenkins SM, Kipp BR, Lin PT, Maleszewski JJ.. COVID-19-associated nonocclusive fibrin microthrombi in the heart. Circulation 2021;143:230–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ostergaard L.SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol Rep 2021;9:e14726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Roshdy A, Zaher S, Fayed H, Coghlan JG.. COVID-19 and the heart: a systematic review of cardiac autopsies. Front Cardiovasc Med 2020;7:626975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stefanini GG, Montorfano M, Trabattoni D, Andreini D, Ferrante G, Ancona M, Metra M, Curello S, Maffeo D, Pero G, Cacucci M, Assanelli E, Bellini B, Russo F, Ielasi A, Tespili M, Danzi GB, Vandoni P, Bollati M, Barbieri L, Oreglia J, Lettieri C, Cremonesi A, Carugo S, Reimers B, Condorelli G, Chieffo A.. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation 2020;141:2113–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pellegrini D, Kawakami R, Guagliumi G, Sakamoto A, Kawai K, Gianatti A, Nasr A, Kutys R, Guo L, Cornelissen A, Faggi L, Mori M, Sato Y, Pescetelli I, Brivio M, Romero M, Virmani R, Finn AV.. Microthrombi as a major cause of cardiac injury in COVID-19: a pathologic study. Circulation 2021;143:1031–1042. [DOI] [PubMed] [Google Scholar]
- 91.Maccio U, Zinkernagel AS, Shambat SM, Zeng X, Cathomas G, Ruschitzka F, Schuepbach RA, Moch H, Varga Z.. SARS-CoV-2 leads to a small vessel endotheliitis in the heart. EBioMedicine 2021;63:103182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fox SE, Li G, Akmatbekov A, Harbert JL, Lameira FS, Brown JQ, Vander Heide RS.. Unexpected features of cardiac pathology in COVID-19 infection. Circulation 2020;142:1123–1125. [DOI] [PubMed] [Google Scholar]
- 93.Basso C, Leone O, Rizzo S, De Gaspari M, van der Wal AC, Aubry MC, Bois MC, Lin PT, Maleszewski JJ, Stone JR.. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J 2020;41:3827–3835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Del Valle DM, Kim-Schulze S, Huang HH, Beckmann ND, Nirenberg S, Wang B, Lavin Y, Swartz TH, Madduri D, Stock A, Marron TU, Xie H, Patel M, Tuballes K, Van Oekelen O, Rahman A, Kovatch P, Aberg JA, Schadt E, Jagannath S, Mazumdar M, Charney AW, Firpo-Betancourt A, Mendu DR, Jhang J, Reich D, Sigel K, Cordon-Cardo C, Feldmann M, Parekh S, Merad M, Gnjatic S.. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med 2020;26:1636–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data included.