Introduction
In spring 2020, as the COVID-19 pandemic took hold in the United States, nursing home deaths accumulated rapidly, accounting for more than 40% of deaths nationally by June.1 Referred to as a “perfect storm” of risk factors2, nursing homes house, in close quarters, large numbers of older adults with underlying health conditions who need hours of hands-on care daily. The combination of these features with the virus’s asymptomatic spread presented a crisis to even the highest-quality nursing homes. Community spread of the virus was the biggest risk factor for nursing home cases and deaths, with apparently little that nursing homes could do to prevent outbreaks.3–5
Several months into the pandemic, best practices emerged: 1) test staff regularly, using rapid-results testing; 2) test residents regularly, especially once a case is detected; 3) separate COVID-positive from COVID-negative residents, ideally with dedicated staff for each group; 4) ensure staff use of personal protective equipment (PPE); and 5) employ standard sanitation procedures. Although the Centers for Disease Control (CDC) and the Centers for Medicare and Medicaid Services (CMS) issued guidelines consistent with these best practices, policymakers offered little assistance with securing supply chains for PPE and testing, technical assistance, or ensuring sufficient staffing. In summer 2020, in an implicit acknowledgement that nursing homes and states could not solve the supply chain issues on their own, CMS began shipping limited quantities of PPE and testing supplies to nursing homes.
Our objective in this study was to examine whether the most recent (September/October) surge in community spread was associated with a surge in nursing home cases and deaths; in other words, to assess whether nursing homes have become better equipped to avoid outbreaks.
Methods
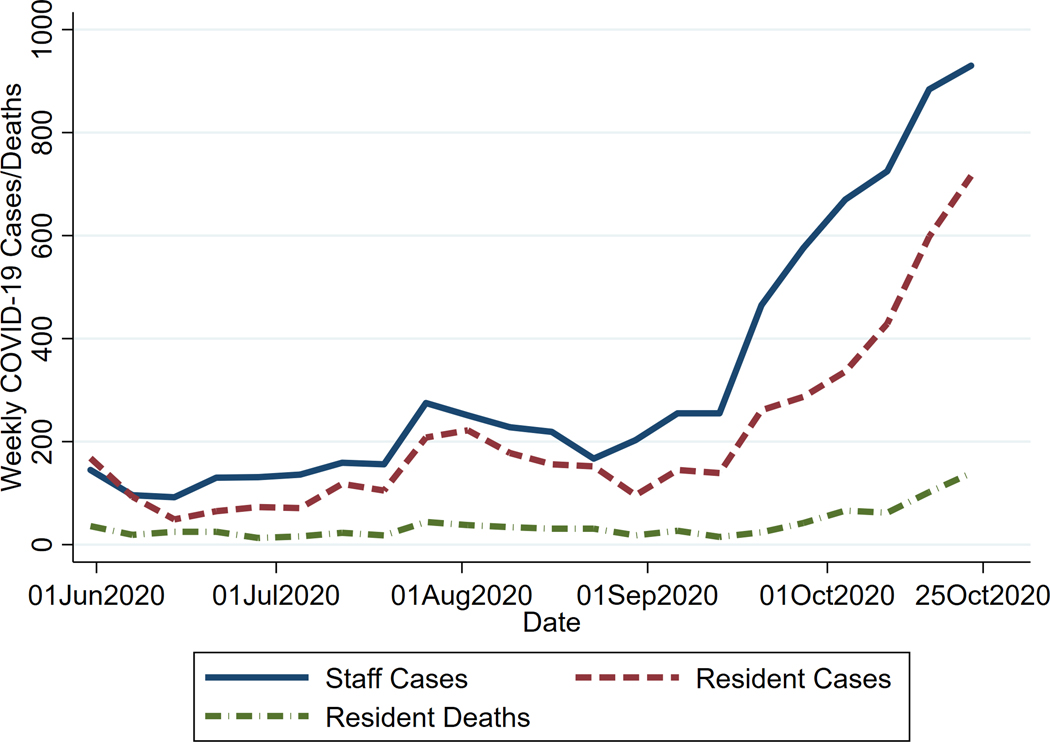
We used the COVID-19 Nursing Home Dataset6 including data from May 29 through October 25, 2020. This file contains weekly case and death counts among residents and staff reported by nursing facilities to CMS/CDC, plus responses to questions about testing, PPE, and staffing shortages. We included data from all facilities with reports meeting the CDC quality checks. We focused on six states experiencing the largest September/October surges in community spread, defined as ranked in the top five states for new cases per capita two or more of the latest five weeks: Idaho, Montana, North Dakota, South Dakota, Utah, and Wisconsin.6 Our study sample included 16,822 weekly reports from 778 facilities in those six states. We plotted the total number of confirmed COVID-19 cases among staff and both cases and deaths among residents. We also calculated the percent of nursing homes that reported shortages of nursing staff or PPE and whether they tested residents and staff during the prior week.
Results
Our plot of nursing home staff and resident cases (Figure 1) revealed a clear surge across the six states since early September, with weekly staff cases more than tripling to 930 in the week ending October 25 and weekly resident more than quadrupling to 716. By October, resident deaths also increased, with the four weeks in October showing the highest four consecutive weeks since reporting began.
Figure 1:
Nursing Home COVID-19 Cases and Deaths in States with Recent Surges in Community Spread
Source: Authors’ calculations of Centers for Disease Control / Centers for Medicare and Medicaid Services data. States include Idaho, Montana, North Dakota, South Dakota, Utah, and Wisconsin.
For the week ending October 25, one in five nursing homes reported shortages of PPE, unchanged since early June. Wisconsin reported the highest shortages (30%) of PPE. One in four nursing homes reported shortages of nursing staff. Although almost all facilities reported testing residents for COVID-19 during the week, 12% reported that they did not test staff during that time.
Discussion
In states experiencing a recent surge in community spread of COVID-19, nursing homes exhibit a substantial increase in staff and resident cases. Despite best practices having emerged, these practices are either not being fully implemented or are inadequate to control the virus. A lack of staff testing for 12% of facilities is especially concerning, given the role of staff in transmitting the virus.2 One likely explanation is that best practices require sufficient testing and PPE as well as sufficient staff to implement them, but substantial numbers of nursing homes continue to report shortages of these critical resources. Given that deaths lag cases, resident deaths are likely to continue to increase, but the rate at which they will increase is unclear, as improvements in treatment may have lowered case-fatality rates.7
Conclusion
Despite gains in knowledge about best practices in nursing homes, little has changed to mitigate the risk of COVID-19 to nursing home staff and residents in virus hotspots. Sporadic policy efforts to address resources gaps have been insufficient and/or ineffective to change the trajectory.
ACKNOWLEDGEMENTS
Funding:
Rebecca Gorges was supported by the National Institute on Aging under Grant Award Number T32 AG000243.
Footnotes
Conflict of Interest:
The authors have no conflicts.
Sponsor’s Role:
Not applicable.
Contributor Information
R. Tamara Konetzka, Department of Public Health Sciences | Department of Medicine, The University of Chicago Biological Sciences, 5841 S. Maryland Ave. | Room W255, MC2000 | Chicago, IL 60637.
Rebecca J. Gorges, Department of Public Health Sciences | Center for Health and the Social Sciences, The University of Chicago Biological Sciences, 5841 S. Maryland Ave. | Room W255, MC2000 | Chicago, IL 60637.
References
- 1.The New York TImes. 43% of U.S. Coronavirus Deaths Are Linked to Nursing Homes. 2020; https://www.nytimes.com/interactive/2020/us/coronavirus-nursing-homes.html. Accessed July 1, 2020.
- 2.Ouslander JG, Grabowski DC. COVID-19 in Nursing Homes: Calming the Perfect Storm. J Am Geriatr Soc. 2020. [DOI] [PubMed]
- 3.Abrams HR, Loomer L, Gandhi A, Grabowski DC. Characteristics of U.S. Nursing Homes with COVID-19 Cases. J Am Geriatr Soc. 2020. [DOI] [PMC free article] [PubMed]
- 4.Gorges RJ, Konetzka RT. Staffing Levels and COVID-19 Cases and Outbreaks in U.S. Nursing Homes. J Am Geriatr Soc. 2020. [DOI] [PMC free article] [PubMed]
- 5.White EM, Kosar CM, Feifer RA, et al. Variation in SARS-CoV-2 Prevalence in US Skilled Nursing Facilities. J Am Geriatr Soc. 2020. [DOI] [PMC free article] [PubMed]
- 6.US Coronavirus Cases and Deaths. 2020; USAFacts.org/visualizations/coronavirus-covid-19-spread-map. Accessed November 5, 2020.
- 7.Horwitz LI, Jones SA, Cerfolio RJ, et al. Trends in COVID-19 Risk-Adjusted Mortality Rates. J Hosp Med 2020. [DOI] [PubMed]