Abstract
Pediatric saliva specimen demonstrated high sensitivity (93%) and specificity (96.2%) compared to paired nasopharyngeal swabs (NPS) by Aptima SARS-CoV-2 Assay (Aptima). Viral loads were comparable in both specimen types. Saliva is a safe, noninvasive, and acceptable alternative specimen for SARS-CoV-2 detection in children.
Keywords: molecular assay, pediatric, saliva, SARS-CoV-2
Respiratory specimens such as nasopharyngeal swabs (NPS), mid-turbinate swabs, and nasal swabs are the currently accepted samples for nucleic acid-based amplification testing of SARS-CoV-2 and recommended by the US Centers for Disease Control and Prevention (CDC) and the Infectious Diseases Society of America (IDSA) [1]. Collecting these invasive samples is uncomfortable, and particularly challenging in children. Additionally, it poses a risk of virus transmission to the clinicians and requires the use of personal protective equipment (PPE) by health care workers, which may be in limited supply [2]. Adoption of an easy, safe, and noninvasive specimen collection method offers an optimal option for SARS-CoV-2 testing in children. Recent studies demonstrate saliva to be an acceptable specimen for SARS-CoV-2 detection, both in symptomatic and asymptomatic patients although with variable sensitivity compared with NPS [3–6]. However, saliva performance data from the pediatric population are comparatively limited. Our objective was to evaluate the diagnostic performance of saliva in comparison to paired NPS in children for SARS-CoV-2 virus by Aptima assay.
MATERIALS AND METHODS
A total of 336 paired samples were collected prospectively from 335 unique children (age range 5-18 years) who had standard of care (SOC) COVID-19 testing ordered by their health care provider. The Institutional Review Board approved study information sheet outlining the study objectives and instructions for saliva collection was sent to all patients electronically prior to their test date. Study participants were instructed to avoid eating or drinking anything 30 minutes prior to sample collection. Volunteer patients were given a saliva collection kit that included a 9.5″ plastic white individually wrapped straw (U.S. Foods, Lenexa, KS) and 10 ml conical tube without any transport media) during their visit at the drive-through test center and asked to fill their mouth with saliva and use the straw to fill the collection tube with 2 ml of saliva. Respiratory specimen was also collected with a flocked, nylon nasopharyngeal (NP) swab (Jiangsu Hanheng Medical Technology Co., Ltd, China) during the same visit, by the nurse and placed in viral transport media (BD Universal Viral Transport Medium, BD Diagnostics, CA) for SOC testing. Samples were transported to the laboratory by same-day courier (within 8 hours of sample collection) and stored at 4°C until testing was completed in the clinical laboratory within the next 2 days (except 4 specimens that were tested between 2 and 5 days from collection).
Paired NP swabs and saliva were obtained from 335 study participants. NP samples were tested first for SOC, and paired saliva samples were enrolled for testing to obtain roughly 50/50 of matched negative/positive specimen pairs. For performance comparison, saliva samples paired with the first 53 corresponding negative NPS (collected within the first 2 days of study initiation) and the first 57 corresponding positive NPS (collected over 3 weeks after study initiation) were tested by Aptima assay. One subject provided duplicate samples, 3 weeks apart, both of which were used for the study. A subset of positive NP swabs and paired saliva aliquots (n = 40) with sufficient residual volume were tested by Argene assay to obtain Ct values for viral load comparisons between paired specimens.
The Aptima SARS-CoV-2 assay is a sample-to-answer molecular assay performed on the Panther instrument (Hologic Inc., Marlborough, MA) that detects 2 unique regions of the ORF1ab gene of SARS-CoV-2 genome. Testing was done following the manufacturer’s instructions and results were interpreted as negative, positive, or invalid. Any invalid NP results were repeated without dilution; however, invalid saliva specimens were diluted 1:1 in 0.85% saline before repeat testing.
Argene SARS-COV-2 assay detects viral N and RdRp genes in the nucleic acid extracts from clinical samples. Nucleic acid was extracted by the NUCLISENS easyMAG system (BioMerieux, France) following the manufacturer’s instructions and amplification reaction was set up using specified assay protocol on the Applied Biosystems QuantStudio 5 Real-Time PCR System (Thermo Fisher Scientific, Waltham, MA). Sample was reported as positive if one or both targets (N and RdRp) were detected with Ct ≤40. Invalid saliva samples were diluted for repeat testing.
The study was reviewed and approved by the Institutional Review Board of Children’s Mercy Hospital (IRB# 00001538).
Data Analysis
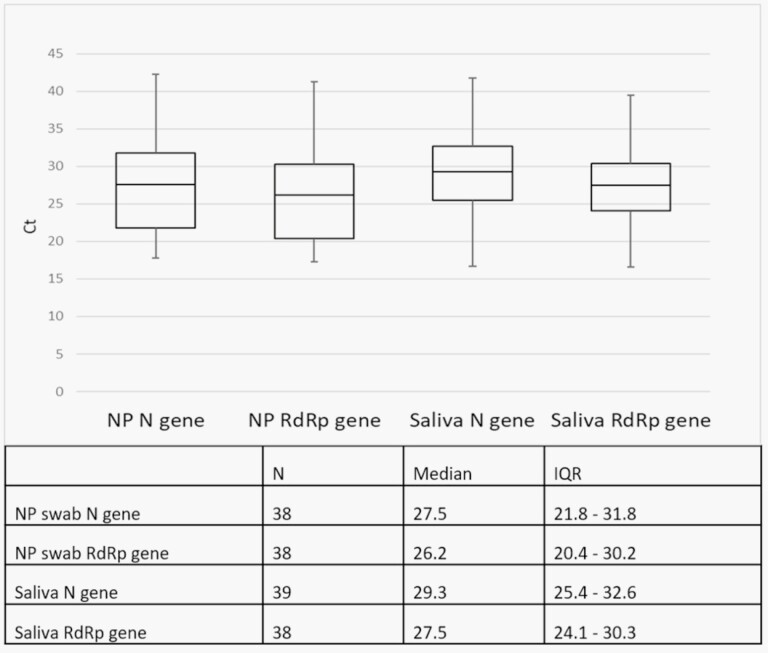
Sensitivity and specificity of saliva were compared to NPS by two-by-two table and presented as value ±95% confidence intervals (CI). A whisker box plot demonstrates the cycle threshold (Ct) values for the N and RdRp genes in each specimen type with the median and interquartile range (IQR). Statistical analyses comparing Ct values between each specimen type were calculated by a 2-tailed t test. Limited demographic information including age, gender, and clinical status (symptomatic vs asymptomatic) was also recorded for data analysis.
RESULTS
A total of 109 subjects participated in the study with the mean age of 10.8 years (age range 5-14 years) and similar gender distribution (50.5% males and 49.5% females). Of the total subjects, 100 (91.7%) were symptomatic at the time of sample collection; 9 subjects were asymptomatic with known COVID-19 exposure.
Sample Comparison
Among the 110 paired samples (NPS and saliva) tested, 53 pairs were positive for SARS-CoV2 in both NPS and saliva specimens. The overall agreement between performance of saliva and NPS was 94.5% (106/110). Sensitivity and specificity for saliva testing are shown in Table 1 with the proportion of symptomatic and asymptomatic individuals in each group. The 4 false-negative (FN) and 2 false-positive (FP) saliva specimens were from symptomatic and asymptomatic children, respectively. Argene assay reported positive results for 1/4 FN saliva samples (N gene Ct = 31.7 and RdRp gene Ct = 33.2) and both FP samples (N gene Cts = 39.3 and 38.6, respectively, RdRp was detected in one of the samples with Ct = 37.8). Viral load in concordant pair of samples is demonstrated by the Ct distribution for N gene and RdRp target for each specimen type in Figure 1. Paired t test showed significant difference between Ct of N and RdRp genes (P values <.001) with a lower Ct for RdRp detection in both specimen types. However, no significant difference was seen in Cts of N or RdRp detection between saliva and NPS. Initial invalid rate for saliva testing was 1.8% (2/110); however, both specimens demonstrated valid results on repeat testing.
Table 1.
Performance Comparison of Saliva and NPS for SARS-CoV-2 Detection by Aptima Assay
| Samples (n = 110) | Aptima NP | ||
|---|---|---|---|
| Positive | Negative | ||
| (Symp/Asymp) | (Symp/Asymp) | ||
| 50/7 | 50/3 | ||
| Aptima saliva | Positive | 53 | 2 |
| (Symp/Asymp) | |||
| 46/9 | |||
| Negative | 4 | 51 | |
| (Symp/Asymp) | |||
| 54/1 | |||
| Sensitivity 93% (95% CI 82.2-97.7) | |||
| Specificity 96.2% (95% CI 86-99.3) |
Symp/Asymp, symptomatic/asymptomatic exposure.
Figure 1.
Ct variation in NPS and saliva specimens for detection of N and RdRp genes with median and interquartile ranges (IQR).
Discussion
Data on the utility of saliva testing for SARS-CoV-2 detection in children are limited, primarily due to small sample size [3, 5, 7]. Earlier studies in both adults and children demonstrate saliva sensitivities ranging between 70% and 90% [8, 9] either in comparison to NPS or based on patient infected status (determined by a positive PCR result from a clinical specimen) [3]. We, however, report >93% sensitivity and specificity for SARS-CoV-2 detection by both methods of analyses which suggests the comparable performance of saliva to NPS. We also report comparable viral loads between both specimen types without any significant difference in Ct values. A negative NPS could, however, suggest poor sampling or specimen collection, especially in noncompliant children due to the uncomfortable and painful collection procedure.
Variable performance in saliva test results could be attributed to age of the patient, specimen collection technique, processing, and testing platforms used. We have used direct saliva for testing on Aptima assay in contrast to groups who have either used diluted saliva [10, 11] or used heated or lysed specimens prior to testing [12]. The differences in saliva performance may also be influenced by the method used for saliva collection such as oral swab, direct spitting in a cup, or use of straw and needs further investigation. Collection of saliva by straw is a safer and more hygienic alternative to spitting in a cup and causing droplet spray and possible contamination of cups, especially in younger children. Highly viscous saliva samples can interfere with testing which can be overcome by diluting specimens as shown in our study.
There are a few limitations to our study design, one of which included enrolling outpatients aged between 5 and 18 years alone. Any comparison with samples from hospitalized or younger children (<5 years), or any correlation with disease severity and viral load in specimen is unavailable. Additionally, a 1-time specimen collection excluded any determination of performance difference in the saliva specimens over the course of illness.
CONCLUSION
Our study demonstrates the utility of saliva as a reliable and easy specimen for COVID-19 testing in children, particularly in frail or immunocompromised patients who may need repeat COVID-19 tests prior to aerosol-generating procedures and may benefit from a less invasive sample collection method. Saliva sampling offers the convenience of self- or parent collection that negates the need for direct interaction with a health care worker and reduces the chance of viral transmission. Saliva collection in children provides a good option for pediatricians that are hesitant to collect NPS in private practice setting. Widespread implementation of saliva sampling could be extremely helpful for mass screening of asymptomatic children in schools and other public health efforts with validated test methods. Continued investigations are required to gather more relevant information and validate findings before implementing alternative testing strategies in the clinical setting.
NOTES
Acknowledgments. We thank the nursing staff in the urgent care center drive-through settings for facilitating the collection of saliva specimens and all the children and their families that volunteered for this study. The authors do not have an association that might pose a conflict of interest.
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
REFERENCES
- 1. Hanson KE, Caliendo AM, Arias CA, et al. . Infectious Diseases Society of America guidelines on the diagnosis of Coronavirus disease 2019 (COVID-19): serologic testing. Clin Infect Dis 2020; doi: 10.1093/cid/ciaa1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ranney ML, Griffeth V, Jha AK. Critical supply shortages—the need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med 2020; 382:e41. [DOI] [PubMed] [Google Scholar]
- 3. Yee R, Truong TT, Pannaraj PS, et al. . Saliva is a promising alternative specimen for the detection of SARS-CoV-2 in children and adults. J Clin Microbiol 2021; 59:e02686–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rao M, Rashid FA, Sabri FSAH, et al. . Comparing nasopharyngeal swab and early morning saliva for the identification of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Clin Infect Dis 2021; 72:e352–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wyllie AL, Fournier J, Casanovas-Massana A, et al. . Saliva or nasopharyngeal swab specimens for detection of SARS-CoV-2. N Engl J Med 2020; 383:1283–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCormick-Baw C, Morgan K, Gaffney D, et al. . Saliva as an alternate specimen source for detection of SARS-CoV-2 in symptomatic patients using Cepheid Xpert Xpress SARS-CoV-2. J Clin Microbiol 2020; 58:e01109-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Azzi L, Carcano G, Gianfagna F, et al. . Saliva is a reliable tool to detect SARS-CoV-2. J Infect 2020; 81:e45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pasomsub E, Watcharananan SP, Boonyawat K, et al. . Saliva sample as a non-invasive specimen for the diagnosis of coronavirus disease 2019: a cross-sectional study. Clin Microbiol Infect 2021; 27:285.e1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Williams E, Bond K, Zhang B, Putland M, Williamson DA. Saliva as a noninvasive specimen for detection of SARS-CoV-2. J Clin Microbiol 2020; 58:e00776-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Berenger BM, Conly JM, Fonseca K, et al. . Saliva collected in universal transport media is an effective, simple and high-volume amenable method to detect SARS-CoV-2. Clin Microbiol Infect 2021; 27:656-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jamal AJ, Mozafarihashjin M, Coomes E, et al. ; Toronto Invasive Bacterial Diseases Network COVID-19 Investigators . Sensitivity of nasopharyngeal swabs and saliva for the detection of severe acute respiratory syndrome Coronavirus 2. Clin Infect Dis 2021; 72:1064-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smyrlaki I, Ekman M, Lentini A, et al. . Massive and rapid COVID-19 testing is feasible by extraction-free SARS-CoV-2 RT-PCR. Nat Commun 2020; 11:4812. [DOI] [PMC free article] [PubMed] [Google Scholar]