Abstract
Background
The COVID-19 pandemic has focussed attention on models of healthcare that avoid face-to-face contacts between clinicians and patients, and teleconsultations have become the preferred mode of primary care delivery. However, the effectiveness of remote consultations in this setting remains unclear.
Objective
To evaluate the impact of telephone or video consultations compared to those conducted face-to-face on key patient-relevant outcomes and healthcare utilisation in primary care, mental health and allied health services, which have had a critical role in the management of the wider and longer-term consequences of COVID-19.
Methods
A systematic review of primary studies comparing telephone or video consultations versus face-to-face visits, following the PRISMA guidelines.
Results
Overall, consultations delivered by telephone and videoconference were as effective as face-to-face in-person visits to improve clinical outcomes in adults with mental health conditions and those attending primary care services. Patient satisfaction with telephone and video consultations and the therapeutic alliance was high across the studies. However, high discontinuation rates in patients receiving teleconsultations indicate this may not be a suitable modality of healthcare delivery for all patients. Teleconsultations offer significant patient time savings in primary care, but appropriate implementation, including training of healthcare professionals and management of technical issues, is essential to ensure effective and valuable clinical interventions.
Conclusions
Teleconsultations via telephone or videoconference are an effective alternative to face-to-face consultations for many patients attending primary care and mental health services. Teleconsultations have the potential to deliver time-efficient and lower-cost interventions at a distance while improving access to healthcare.
Keywords: Mental health, primary care, remote consultation, teleconsultation, telehealth, telemedicine
Key Messages.
Teleconsultations are an effective alternative to in-person primary care visits
Patient satisfaction with telephone and video consultations is high
Teleconsultations are time-efficient and potentially associated with lower costs
Teleconsultations are associated with high attrition rates
Teleconsultations may not be suitable for everyone
Background
The COVID-19 pandemic in 2020 focussed attention on models of healthcare that avoid face-to-face contacts between clinicians and patients (1). In many countries, primary care providers rapidly adopted telemedicine (i.e., video and telephone remote consultations) to manage patient flow through healthcare facilities, limit exposure and minimise the risk of infectious transmission (2).
In Europe, teleconsultations became the preferred mode of primary care delivery, where physicians were recommended to triage patients remotely, and face-to-face consultations were discouraged unless considered necessary by the attending doctor (3–5). In Italy, 20% of the teleconsultations carried out during the pandemic were telephone-based, 38% were conducted through web-based systems, 29% in specific platforms, and 13% via apps (6). By April 2020, telephone consultations in US outpatient centres accounted for 65.4% of primary care consultations and 71.6% of behavioural health visits (7).
Telephone consultations are a familiar and reliable technology in primary care, but video conferencing may be more appropriate for frail older patients or those with high levels of anxiety (8). Telephone or video consultations can potentially reduce access costs (9,10) and reduce transmission of infectious agents (1), but at the risk of compromising the quality of care if not implemented appropriately. There has been much speculation on whether the COVID-induced crises in healthcare will result in a more permanent shift in practice towards telemedicine. This will inevitably depend on the individual experience of clinicians and patients, and the evidence of the quality of care in particular groups of patients, and payment arrangements.
Past reviews of video consultations in patients with long-term conditions did not find sufficient high-quality evidence to be able to reach conclusions with confidence (11), but there was stronger evidence that telephone consultations can be of similar quality to face-to-face consultations in primary care (12). In contrast to earlier reviews, we also include mental health and allied health consultations as these are often provided in general practice. In the UK, it is estimated that 90% of mental health presentations are managed in primary care, and mental health accounts for approximately 40% of the workload in general practice. COVID-19 raised the prevalence of anxiety, depression and post-traumatic stress disorder (PTSD) in the general population, and mental health support through primary care has been identified as a top healthcare priority (13).
Objectives
This paper reviews the evidence on the impact of remote telephone or video consultations compared to those conducted face-to-face on key patient-relevant outcomes and healthcare utilisation in primary care, including mental health and allied health services.
Methods
This systematic review has followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (14).
Search methods for identification of studies
The Cochrane Library, Embase and PubMed were searched combining key terms for ‘telemedicine’ and ‘teleconsultation’ with ‘psychotherapy’, ‘counselling’, ‘primary care’ and ‘allied health’. The reference lists of included studies and relevant systematic reviews were also examined to identify potential studies. The search was limited to studies published from 2011 to the present to identify the most up-to-date studies.
Criteria for inclusion followed the PICOS format:
a) Population: adults (aged 18 years and older) receiving attending primary care, mental health or allied health services.
b) Intervention: telemedicine treatment delivered via telephone or videoconference that replaced the in-person consultation.
c) Comparator: the same therapy (as in intervention) delivered face-to-face.
d) Outcomes: key patient-relevant outcomes (e.g., clinical improvement, quality of life, patient satisfaction) and healthcare utilisation.
e) Study design: randomised controlled trial (RCT), non-randomised comparative studies of interventions
Studies were excluded if they were (a) not in English, (b) the telemedicine intervention included other telehealth modalities such as telemonitoring, telerehabilitation, mobile apps or interactive websites, (c) patients had to attend a healthcare centre to receive the telemedicine consultation, (d) the face-to-face intervention included a different therapeutic approach to that in the telemedicine group, (e) telemedicine triage services.
Data collection and analysis
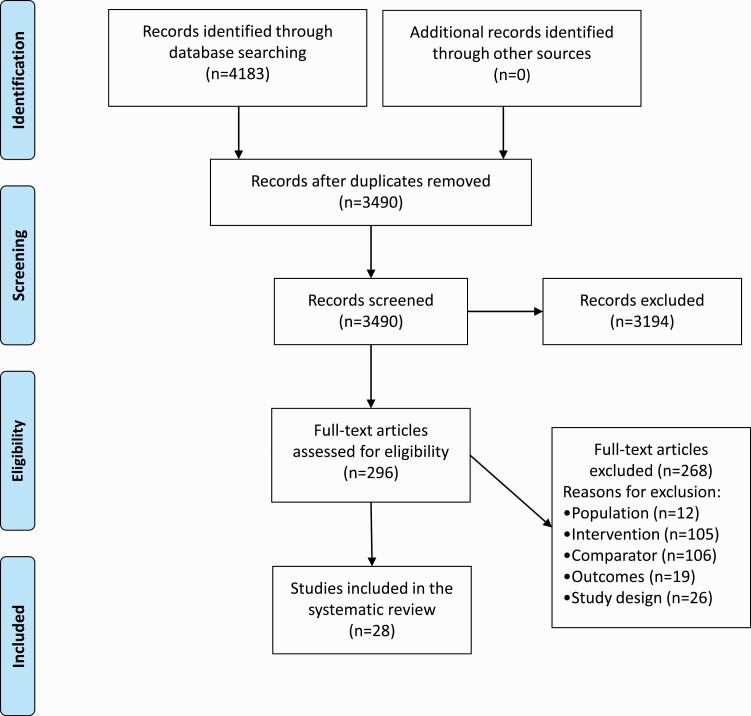
Following PRISMA guidelines (14), two authors (SCA and KLS) independently reviewed the retrieved citations in two stages; starting with a title and abstract screening against eligibility criteria and directly excluding studies that clearly failed to meet inclusion criteria, followed by a full-text screening of any potentially relevant publications. Further irrelevant articles were excluded at this second stage, with reasons for exclusion added to the study selection flow diagram (Figure 1).
Figure 1.
Flow diagram of the study selection process
The following data were extracted from the included studies: first author and date, country, design of the study, patient characteristics, main diagnosis, therapy type, telemedicine modality, session frequency and follow up, and key outcomes.
The quality of included studies was assessed using Version 2 of the Cochrane tool for assessing the risk of bias in randomised trials (RoB 2) (15) and the ROBINS-I tool (16) for assessing the risk of bias in non-randomised studies of interventions.
Due to the high level of heterogeneity among the studies, a narrative synthesis of the evidence was conducted. Effect estimates were presented for key outcomes where standardised measures were reported.
Studies were classified by the main setting: primary care, which also included allied health services and mental health. Some patients attending primary care also received mental health services, but these studies were included under ‘mental health’ as the key focus was the intervention received.
Results
The flow diagram (Figure 1) presents the details of the literature search and screening of studies. Following the removal of duplicate search’ records and screening titles and abstracts of studies, we appraised 296 relevant studies in full text. Of these, 265 articles did not meet our inclusion criteria and were removed. A total of 31 studies were included; 17 were classified within mental healthcare and 11 as primary care (including 5 in allied health).
Details on the risk of bias of included studies are provided in the supplementary materials (Supplementary Figures S1 and S2).
Primary care and allied health
Characteristics of included studies
Eleven studies (5 RCTs) were included comparing teleconsultations and face-to-face visits to primary care, including allied health services (Table 1). Two RCTs were designed to investigate teleconsultations versus face-to-face visits to primary care physicians (17,18) and three evaluated allied health services (19–21). Of the six non-randomised comparative studies, three were cross-sectional matched-control design using claims-based datasets (22–24) comparing the healthcare utilisation and quality of care of primary care visits.
Table 1.
Summary characteristics of included studies of teleconsultations in primary care and allied health
| Main Diagnosis | Study ID | Design | Risk of Bias | Country | Population | Therapy type | Sessions, Follow up |
Attrition | Key outcomes | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Video consultation | ||||||||||
| Cancer | Collins 2017 (26) | Non-randomised comparative study | High | Australia | Patients aged 32–77 with head and neck cancer; N = 30; TM = 15; F2F = 15; 67% male |
Model of care for reviews with speech pathology, nutrition and dietetics | Average 4.3 sessions/patient over 8 months | 6.7% (inappropriate technology) | Number and duration of appointments per person and total service cost | TM significantly reduced the number and duration of appointments required until discharge, and had significantly lower cost per patient. |
| Acute nonurgent conditions | Gordon 2017 (22) | Cross-sectional matched-control retrospective study | Some concerns | USA | Patients aged ≤ 65 with acute nonurgent conditions; N = 59 945a; TM = 4635; F2F = 13 881; 38% male |
Retail health clinics, urgent care centres, emergency departments, or primary care physicians | Index episodeb plus 3 weeks follow-up | NR | Healthcare utilisation during and following the index visit and cost of care | TM reduces health are utilisation (lab tests, imaging) and lower cost per episode including medical and pharmacy cost compared to F2F. |
| Disability | McCarthy 2020 (27) | Non-randomised comparative study | High | Australia | Caregivers aged ≥18 of deaf or hard hearing child (aged < 8); N = 141; TM = 41; F2F = 100; 11% male |
Family-Centred Early Intervention | Weekly/ fortnightly/ monthly sessions over >6 months | TM = 69% F2F = 71.5% |
Parental self- efficacy and session frequency | No significant difference on caregiver’s perception of self-efficacy and session frequency between TM and F2F. |
| Major diagnosis (ADGsc) | McGrail 2017 (23) | Cross-sectional matched-control retrospective study | High | Canada | Patients aged ≥18 with major ADGsc; N = 26617; TM = 5441; F2F = 21 176; 41% male |
Primary care visit | Index episode plus 3 years follow-up | NR | Cost of primary care visit | TM is significantly more likely to be used by younger patients and physicians. TM reduces primary care costs but benefit is significantly associated with seeing a known provider. |
| Smoking cessation | Nomura 2019 (17) | RCT | Some concerns | Japan | Adults with nicotine- dependence; N = 115; TM = 58; F2F = 57; 80% male |
Counselling (smoking cessation) | 5 sessions over 12 weeks 12 weeks follow-up |
2.6% (withdrew consent, lost to f/up) | continuous abstinence rate (CAR) | TM is non-inferior to F2F for CAR from weeks 9 to 12. No significant difference between TM and F2F in reduction of nicotine dependence and cravings. |
| Respiratory infection | Shi 2018 (24) | Cross-sectional matched-control retrospective study | Some concerns | USA | Patients aged 18–64 with acute respiratory infections; N = 981 452d; TM = 38 839; F2F = 942 613; 37% male |
Primary care visit | Index episode plus 21 days follow-up | NR | Quality of care | Compared to F2F, TM had significant but not clinically meaningful (small) improvement in some measures of quality of care (antibiotic use). On other quality measures F2F performed better. |
| Telephone consultation | ||||||||||
| Obesity | Harrigan 2016 (20) | RCT | High | USA | Breast cancer survivors with BMI≥25; N = 100; TM = 34; F2F = 33; 0% male |
Counselling (weight loss) | 11 sessions over 6 months 6 months follow-up |
TM = 53% F2F = 39% |
Body composition (height and weight) | No significant difference between TM and F2F for weight loss |
| Malnutrition | Lindegaard Pedersen 2017 (21) | RCT | Some concerns | Denmark | Patients aged 75–103 with malnourishment or risk of malnutrition; N = 208; TM = 68; F2F = 73; 17% male |
Counselling (nutrition) | 3 sessions over 4 weeks 8 weeks follow-up |
TM = 22 (32%) F2F = 20 (27%) |
Readmissions at 30 and 90 days after discharge | No significant difference between TM and F2F for readmissions |
| Smoking cessation | Ramon 2013(18) | RCT | Some concerns | Spain | Smokers aged ≥18 years; N = 600; TM = 201; F2F = 199; 51% male |
Counselling (smoking cessation) | 7 sessions over 52 weeks | TM = 70 (35%) F2F = 48 (24%) |
Continuous abstinence rate (CAR) | F2F had significantly higher CAR at 52 weeks compared to TM. |
| General | McKinstry 2011 (25) | Non-randomised comparative study | High | Scotland | Patients from 11 GPs; N = 175; TM = 50; F2F = 94; 31% male |
Primary care visit | Individual visit plus 9 days follow-up | 18% | Prospective- Retrospective Memory Questionnaire (PRM-Q) | TM and F2F were comparable in accuracy of recall (for single and multiple problem consultations). Significantly more repetition of advice in enhancing patient recall was given in F2F. |
| Post-partum | Seguranyes 2014 (19) | RCT | Some concerns | Spain | Post-partum patients; N = 1401; TMe = 683; F2F = 718; 0% male |
Post-natal care | Any over 6 weeks post-partum | TM = 228 (25%) F2F = 103 (12.5%)f |
Number and type of consults, health centre visits, infant feeding and maternal satisfaction with care | Significantly higher number of consults made by TM than F2F. TM group had significantly few visits to the health centre. TM and F2F comparable in prevalence of breast feeding and maternal satisfaction with care |
F2F, face-to-face; NR, not reported; RCT, randomised control trial; TM, telemedicine
aTotal sample included 52 751 adults, 7194 child ( < 18 years).
bIndex date defined as the date of the first outpatient or ED claim in a 3-week period for 11 of the most commonly diagnosed conditions.
c8 major aggregated diagnosis group using the Johns Hopkins’ adjusted clinical group, which included, mental disorders, diseases of respiratory system, diseases of musculoskeletal system, diseases of nervous system, metabolic diseases and immunity disorders, infections, diseases of circulatory system, disease of genitourinary system.
dnumber of health visits; number of patients not reported.
epatients could make videoconferencing or telephone consults.
fThe main reason for lost to follow-up in the TM group: failure to attend final visit, failure to register for skype and lack of internet access; and in the F2F group: failure to attend final visit. The study recruited 134 (TM = 113 and F2F = 21) to compensate for the subject lost.
The studies were conducted in seven different countries: Australia (n = 2), USA (n = 3), Spain (n = 2), Canada (n = 1), Denmark (n = 1), Japan (n = 1), and Scotland (n = 1). The health conditions and diseases addressed in the studies were broad ranging, including acute nonurgent conditions, major diagnoses (including mental disorders), respiratory infections, malnutrition, nicotine dependence, chronic conditions and post-partum care. All studies included adults (≥18 years), two studies enrolled caregivers of children and two studies focused on women’s health (breast cancer survivors and recent mothers).
Interventions
The included studies featured consultations delivered via in-home telephone or videoconferencing versus face-to-face consultations at an outpatient clinic with primary care physicians for acute conditions (22–25) or counselling for smoking cessation (17,18), as well as allied health services such as nutrition or weight-loss counselling (20,21), speech therapy (26), family-centred early intervention (27) and post-partum care (19). The number of health visits varied across the studies from an individual primary care consultation (25) to any number of visits over three years (23).
Effectiveness of teleconsultations vs. face-to-face consultations
The effectiveness of teleconsultations in the primary care population is summarised in Table 2. Four studies of teleconsultations in primary care reported that telemedicine was comparable to face-to-face in terms of quality of care and accuracy of patient’s recall. Teleconsultations were associated with a reduced cost and healthcare utilisation compared to face-to-face consultations. Shi et al.(24) reported that teleconsultations delivered by video conferencing had significant, although not clinically meaningful, improvements in some quality of care measures (e.g., antibiotic use and guideline-based antibiotic management), but face-to-face visits performed better on other quality measures (e.g., more appropriate testing and fewer follow-up visits). McGrail et al.(23) analysed the impact of videoconferencing on primary care utilisation and costs and reported that compared to in-person face-to-face primary care visits, teleconsultations significantly reduced primary care costs associated with seeing a known primary care physician (P < 0.001). Descriptive analyses of the patients and physicians using teleconsultations indicate that videoconferencing was significantly more likely to be used by younger patients and physicians (P < 0.001), with no differences by sex. There were no significant differences in teleconsultation use between rural and urban settings or by socioeconomic gradient, although older and sicker patients using teleconsultations were more likely to see a physician they had previously interacted within a traditional clinic setting. Gordon et al.(22) also reported video consultations reduced healthcare utilisation (e.g., lab tests, imaging) and cost per episode, including medical and pharmacy costs, compared to face-to-face.
Table 2.
Effectiveness of teleconsultations in primary care
| Outcome measures | N patients | TM, mean (SD or 95% CI) | F2F, mean (SD or 95% CI) | Treatment difference, mean (95% CI) | Follow upb | Study ID |
|---|---|---|---|---|---|---|
| Videoconsultation vs. F2F | ||||||
| Number of appointments per person | TM = 15 F2F = 15 |
3.4 (1.15) | 5.3 (2.10) | P = 0.003 | 8 months | Collins 2017 (26) |
| Duration (minutes) of appointments per person | 23 (6.0) | 27.5 (6.2) | P ≤ 0.01 | |||
| Total societal cost per person | $143 (46) | $317 (176) | $US 174, P = 0.002 | |||
| % outpatient visits after index visit | TM = 4635 F2F = 1388l1 |
28.1% | 28.1% | P = 0.99 | 3 weeks | Gordon 2017 (22) |
| % hospitalisation after index visit | 0.2% | 0.4% | P = 0.02 | |||
| Adjusteda mean cost of medical follow-up visit | $200 | $288 | P < 0.01 | |||
| SPICE parental self-efficacy subscales (PSEDU, PSESL, PIDU, PISL) | TM = 41 F2F = 100; |
5.56 (0.97), 6.03 (0.75), 5.68 (0.88), 5.83 (0.71) | 5.38 (1.07), 5.90 (0.99), 5.74 (0.93), 5.77 (0.83) | 0.18, 0.13, –0.06, 0.06 P > 0.05 |
>6 months | McCarthy 2020 (27) |
| % weekly session frequency | 68.3% | 67% | P < 0.05 | |||
| Cost of primary care (GP) visit | TM = 5441 F2F = 21176; |
– | – | –$CAN 3.79, P = 0.12 | 3 years | McGrail 2017 (23) |
| Cost of primary care visit with known known provider | –‘ | – | –$CAN 8.68, P < 0.001 | |||
| Continuous abstinence rate from weeks 9 to 12 | TM = 58 F2F = 57; |
81.0 (38.8) | 78.9 (40.8) | 2.1 (–12.8, 17.0) | 12 weeks | Nomura 2019 (17) |
| Continuous abstinence rate from weeks 9 to 24 | 74.1 (43.4) | 71.9 (45.3) | 2.2 (–14.0, 18.4) | 24 weeks | ||
| % Any antibiotic use | TM = 38,839c F2F = 942,613c |
52% | 53% | 1%, P < 0.01 | 21 d (3 weeks) | Shi 2018 (24) |
| % Guideline antibiotic management | 62% | 60% | 2%, P < 0.001 | |||
| Telephone consultation vs. F2F | ||||||
| Change in body weight (kg) | TM = 34 F2F = 33 |
–4.8 (–6.5, –3.1) | –5.6 (–7.1, –4.1) | P = 0.46 | 6 months | Harrigan 2016 (20) |
| –6.3 (–9.9, –2.6) | –5.6 (–8.0, –3.3) | P = 0.72 | 12 months | |||
| HR hospital readmission at 30 days | TM = 68 F2F = 73 |
0.6 (0.3–1.3) | 0.4 (0.2–0.9) | P < 0.05 | 30 days (1 months) | Lindegaard Pedersen 2017 (21) |
| HR hospital readmission at 90 days | 0.7 (0.4–1.3) | 0.4 (0.2–0.8) | P < 0.05 | 90 days (3 months) | ||
| Continuous abstinence rate from weeks 2 to 24 | TM = 201 F2F = 199 |
30.1 | 42.3 | P < 0.05 | 24 weeks | Ramon 2013 (18) |
| Continuous abstinence rate from weeks 2 to 52 | 20.1 | 27.9 | P < 0.05 | 52 weeks | ||
| % Accurate recall | TM = 50 F2F = 94 |
82% | 68% | 14% (–2%, 27%) | 13 days | McKinstry 2011 (25) |
| % Clinician approach (advice repetition) enhance recall | 28% | 47% | P = 0.04 | |||
| Number of post-partum consults | TMd = 683 F2F = 718 |
2.74 (1.47) | 1.22 (0.75) | P < 0.001 | 6 weeks | Seguranyes 2014 (19) |
| Number of health centre visits | 1.0 (0.85) | 1.17 (0.74) | P = 0.002 | |||
| Prevalence of breastfeeding | 64.5% | 65.4% | P > 0.05 | |||
| Satisfaction with midwifery care | 4.77 (0.49) | 4.76 (0.56) | p = 0.94 |
CLBP, Chronic low back pain; F2F, face-to-face; HR, hazard ratio; PIDU, Parental Involvement (Device Use); PISL, Parental Involvement (Speech and Language Development); PSEDU, Parental Self-Efficacy (Device Use); PSESL, Parental Self-Efficacy (Speech and Language Development); PD, Pulmonary disease; SPICE, Scale of Parental Involvement and Self-Efficacy; SPL, sound pressure level; TM, telemedicine; d, day; m, month; w, week
aCosts adjusted for age categories and baseline comorbidities.
bMean values with were measured at the specified follow-up times reported in the table
cnumber of health visits; number of patients not reported.
dpatients could make videoconferencing or telephone consults.
McKinstry et al.(25) showed similar accuracy of patient’s recall (for single and multiple problem consultations) between telephone and face-to-face GP consults, although significantly more repetition of advice was given in face-to-face consults.
Two studies of counselling on smoking cessation in primary care reported mixed results for continuous abstinence rate (CAR). In Nomura et al.(17) counselling delivered by video conferencing was non-inferior to face-to-face for CAR from weeks 9 to 12, whereas Ramon et al.(18) reported face-to-face counselling led to significantly higher CAR at 24 and 52 weeks compared to teleconsultations by telephone. Two further studies on counselling found no significant differences between telephone and face-to-face for counselling of weight loss (20) and nutrition (21) by a primary care physician or allied health practitioners.
For speech therapy, Collins et al.(26) showed video conferencing significantly reduced the number and duration of appointments with significantly lower service cost per patient.
In other studies, McCarthy et al.(27) found no significant differences between teleconsultations and face-to-face consultations for Family-Centred Early Interventions delivered to caregivers of children with a disability. Seguranyes et al.(19) reported a significantly higher number of teleconsultations for post-natal care in post-partum women using telephone compared to face-to-face visits.
Attrition
Treatment discontinuations were high across most of the included studies of allied health services, mainly due to loss to follow up, other personal reasons or technical issues. Ramon et al.(18) noted higher discontinuations for smoking cessation in the telephone group (35%) versus face-to-face (24%) and fewer session attended, which could be due to higher relapse rates. Similarly, Harrigan et al.(20) and Lindegaard Pedersen et al.(21) also noted lower adherence in the telephone group due to life events (e.g., hospital readmissions) or personal reasons (e.g., family caregiving needs, employment, ‘too much contact with healthcare professionals’, or ‘no specific reason’) and not randomisation to that group. Seguranyes et al.(19) had twice as many subjects discontinuing in the teleconsultation group (25%) than in the face-to-face group (12.5%), the main reason was the failure to attend final follow-up visit and technical issues (teleconsultation group only); however, the study recruited 14% and 3% additional subjects to the respective groups. McCarthy et al.(27) had an overall response rate of 29%, which was similar between groups, but the sample size was small.
Mental health
Characteristics of included studies
A total of 17 studies (13 RCTs) comparing mental health interventions delivered via teleconsultations or face-to-face (Table 3). Five of the RCTs (28–32) were designed to examine the non-inferiority of teleconsultations versus face-to-face consultations.
Table 3.
Summary characteristics of included studies of teleconsultations in patients with mental health conditions
| Main Diagnosis | Study ID | Design | Risk of Bias | Country | Population | Therapy type | Sessions, Follow up |
Attrition | Key outcomes | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Video consultation | ||||||||||
| Depression (HAMD≥15 |
Choi 2014 (41) | RCT | High | USA | Low income older adults (50–64 years) bN = 121 TM = 43 F2F = 42 Telephone support = 36 22.3% male |
Problem-solving therapy | 6 sessions 24 weeks follow-up |
a
TM = 5 (11.6%) F2F = 7 (16.6%)) |
Depression (HAMD) Treatment acceptance |
• Improvement in depression in both groups, no significant difference • Positive attitudes towards TM |
| Choi 2014b (42) | RCT | High | USA | Low income older adults (>50 years) bN = 158 TM = 56 F2F = 63 Telephone support = 39 21.5% male |
Problem-solving therapy | 6 sessions 36 weeks follow up |
a
TM = 7 (12.5%) F2F = 9 (14.3%) |
Depression (HAMD) and disability (WHODAS) | • Improvement in depression and disability in both groups • Significantly lower depression symptoms by Week 36 in TM vs. F2F • No significant difference in disability scores |
|
| Depression (DSM- IV criteria for major depressive disorder) (linked studies) |
Egede 2015 (28) | RCT (non-inferiority) | Low | USA | Military veterans (>58 years) N = 241 TM = 120 F2F = 121 97.5% male |
Behavioural activation | 8 sessions 12 month follow up |
TM = 20 (16.6%) F2F = 16 (13.2%) |
Depression (GDS, BDI) | • TM is non-inferior to F2F for the treatment of depression |
| Egede 2016 (29) | Low | Quality of life Satisfaction with treatment |
• No significant differences in SF-36 or satisfaction with treatment between TM and F2F at 12months | |||||||
| Egede 2018 (45) (subgroup analysis of Egede 2015/16) | RCT | Low | USA | Military veterans (>58 years) with type 2 diabetes N = 90 TM = 43 F2F = 47 97.8% male |
Behavioural activation | 8 sessions 12 month follow up |
NR | Type 2 diabetes control | • TM was superior to F2F treatment to lower HbA1C | |
| Depressive disorder (minor or major) | Luxton 2016 (30) | RCT (non-inferiority) | High | USA | Military members and veterans (18–65 years) N = 121 TM = 62 F2F = 59 81.8% male |
Behavioural activation | 8 sessions 3 month follow up |
TM = 22 (35.5%) F2F = 17 (28.9%) |
Depression | • Significant reductions in depression in both group • By the end of treatment (8w), the F2F group experienced a significantly greater reduction in depression symptoms vs. the TM group. However, this difference became non-significant in the 3m follow-up |
| PTSD | Acierno 2016 (31) | RCT (non-inferiority) | Some concerns | USA | Military veterans (mean age 45 years) N = 232 TM = 131 F2F = 134 94.4% male |
Behavioural Activation and Therapeutic Exposure | 8 sessions 12 month follow up |
48 did not complete at least 5 sessions TM = 18.0% F2F = 23.1% |
PTSD Depression |
• TM was non-inferior to F2F treatment to reduce PTSD and depression symptoms at all time points |
| PTSD | Acierno 2017 (32) | RCT (non-inferiority) | Some concerns | USA | Military veterans (mean age 42 years) N = 132 TM = 64 F2F = 68 96.2% male |
Prolonged exposure | 10 to 12 sessions 6 month follow up |
TM = 32.8% F2F = 19% (did not complete ≥6 sessions) |
PTSD Depression |
• TM was non-inferior to F2F treatment to reduce PTSD at all time points. • TM was non-inferior to F2F for depression at 6-month follow-up, but not earlier |
| PTSD | Maieritsch 2016 (33) | RCT | High | USA | Military veterans (mean age 31 years) N = 90 TM = 45 F2F = 45 93.3% male |
Cognitive processing therapy | 10 sessions 12 week follow up |
TM = 20 (44.4%) F2F = 19 (42.2%) |
PTSD Depression Therapeutic alliance |
• Significant decreases in depression and PTSD symptoms in both arms, but the difference between groups was not calculated due to high attrition |
| Medically unexplained pain | Chavooshi 2017 (34) | RCT | Some concerns | Iran | Adults aged 18–45 years with medically unexplained pain for ≥6 months N = 81 TM = 39 F2F = 42 64.2% male |
Intensive short- term dynamic psychotherapy | 16 sessions | TM = 9 (23%) F2F = 14 (33%) |
Pain intensity Depression Anxiety |
• F2F treatment led to significantly greater improvements in pain intensity, depression and anxiety compared to TM • Treatment satisfaction was similar in both groups |
| Opioid abuse | King 2014 (35) | RCT | High | USA | Outpatients attending addiction treatment services N = 59 TM = 24 F2F = 35 44.3% male |
Motivated Stepped Care Counseling | 12 weeks with number of sessions: TM = 5.4 (SD = 2.54) F2F = 6.1 (SD = 3.30” |
TM = 2 (8.3%) F2F = 1 (2.8%) (did not complete 3 follow-ups) |
Client satisfaction Therapeutic alliance |
• Treatment satisfaction and therapeutic alliance was high and similar in both groups |
| Telephone consultation | ||||||||||
| Depression | Alcantara 2016 (37) | RCT | High | USA & Puerto Rico | Low-income Latinos (≥18 years) in primary care N = 257 TM = 87 F2F = 84 Usual care = 86 18% male |
Engagement and Counselling for Latinos (ECLA); including psychoeducation, behavioural activation, cognitive reframing, and motivational interviewing | 6 to 8 sessions First 4 sessions were weekly; the 5th and 6th were biweekly unless more immediate care was needed. Continued up to 8 sessions. 2–4 months follow up |
TM = 17 (31.0%) F2F = 31 (46.9%) |
Worry reductions (PSWQ) | • Significantly larger worry reductions in TM vs. F2F |
| Depression (Major depression) | Fann 2015 (43) | RCT | High | USA | Patients with traumatic brain injury (mean age 45.8 years) bN = 100 TM = 40 F2F = 18 63% male |
Cognitive behavioural therapy | 12 sessions over 12 weeks 24 weeks follow up |
TM = 5 (12.5%) F2F = 2 (11.1%) |
Depression Therapeutic alliance |
• No significant differences between TM and F2F for depression severity or therapeutic alliance |
| Depression (linked studies) |
Kalapatapu 2014 (39) (subgroup analysis of Mohr 2012) |
RCT | Low | USA | Patients with problematic alcohol use in primary care (mean age 42–45 years) N = 103 TM = 50 F2F = 53 12.6% male |
Cognitive behavioural therapy | 18 sessions over 18 weeks 6 months follow-up |
TM = 26.0% F2F = 24.5% | Depression Alcohol use Treatment adherence |
• No significant difference between TM and F2F at any time point for depression outcomes |
| Mohr 2012 (38) | RCT (non-inferiority) | Low | USA | Patients in primary care (mean age 47 years) N = 325 TF = 163 F2F = 162 22.5% male |
Cognitive behavioural therapy | 18 sessions over 18 weeks 6 months follow-up |
TM = 34 (20.9%) F2F = 53 (32.7%) |
Depression Treatment adherence |
• TM improves adherence • Depression severity improved in both groups, but was significantly better in the F2F group by the 6-month follow-up |
|
| Stiles-Shields 2014 (40) | Low | Therapeutic alliance | • No significant differences in therapeutic alliance | |||||||
| Cancer | Watson 2017 (36) | RCT | High | UK | Cancer patients referred to psychological care (mean age 48–52 years) N = 118 TM = 60 F2F = 58 27.9% male |
Cognitive behavioural therapy | Up to 8 sessions over 12 weeks | TM = 17 (28.3%) F2F = 23 (39.6%) |
Depression Anxiety |
• No significant differences from baseline to Week 8 in depression and anxiety |
F2F, face-to-face, PTSD, post-traumatic stress disorder, RCT, randomised control trial, TM, telemedicine
aAttrition was due mostly to deteriorating health problems that resulted in hospitalization, nursing home placement, and death
bThird patient group was telephone support, but not included as the intervention given to this group differed from the others.
cThird patient group was usual care, including rehabilitation and primary care services (without cognitive behavioural therapy)
Most studies were conducted in the USA (n = 14). Videoconferencing was used in 11 studies, and telephone in six. The majority of studies (n = 11) included patients with a main diagnosis of depression, three studies assessed patients with post-traumatic stress disorder (PTSD) (31–33), one included patients receiving psychological treatment for medically unexplained pain (34), one study evaluated counselling for opioid abuse (35), and another study included mental health interventions given to patients with cancer (36).
All three studies in patients with PTSD included military veterans, who were mostly men (93.3%–96.2%). Patients with depression were mainly women (~80%), except for studies in military personnel. All studies included adults (≥18 years), and five studies focused on older adults (>50 years). Four studies in patients with depression were conducted in the primary care setting, all of them compared telephone to face-to-face consultations (37–40).
Interventions
All the included studies evaluated the effect of selected psychological interventions delivered via telephone or videoconferencing versus face-to-face consultations. The psychological interventions were varied, with the number of sessions ranging from 6 to 18 across the studies, and a follow-up period from 3 to 12 months. Cognitive behavioural therapy (CBT) was the most common therapy type in studies evaluating telephone consultations. The psychological interventions in studies of video consultations included among others problem-solving therapy, behavioural activation, therapeutic exposure, cognitive processing or short-term dynamic psychotherapy.
Effectiveness of teleconsultations vs. face-to-face consultations
A summary of effectiveness outcomes for videoconferencing and telephone versus face-to-face consultations can be found in Table 4. In patients with depression, most studies using videoconferencing (28,31,32,41,42) and telephone-delivered interventions (39,43,44) reported similar effectiveness for the two delivery options to reduce depression symptoms at various time points of follow up.
Table 4.
Effectiveness of teleconsultations in patients with mental health conditions
| Outcome measures | N patients | TM, mean (SD or 95% CI) | F2F, mean (SD or 95% CI) | Treatment difference; TM vs. F2F, mean (95% CI) | Follow upa | Study ID |
|---|---|---|---|---|---|---|
| Videoconsultation vs. F2F | ||||||
| HAMD, mean (SD) | TM = 43, F2F = 42 | 13.92 (1.18) | 14.44 (1.19) | t = −0.31, P = 0.755 | 12 weeks (~3 months) | Choi 2014 (41) |
| 13.37 (1.18) | 14.80 (1.12) | t = −0.90, P = 0.369 | 24 weeks (~6 months) | |||
| TM = 56, F2F = 63 | 13.68 (1.00) | 14.08 (0.94) | t = –0.06, P = 0.772 | 12 weeks (3 months) | Choi 2014b (42) | |
| 12.38 (0.85) | 14.12 (0.80) | t = –1.49, P = 0.809 | 24 weeks (6 months) | |||
| 11.08 (1.07) | 14.16 (0.99) | t = –2.11, P = 0.035 | 36 weeks (9 months) | |||
| BDI response, n (%), [95% CI] | TM = 120, F2F = 121 | 27 (22·54%), [15.40, 29.69] | 26 (21·49%), [14.72, 28.25] | 1·05% (–8·30, 10·41) | 12 months | Egede 2015 (28) |
| GDS response, n (%), [95% CI] | 25 (20·96%), [14.45, 27.47] | 23 (19·30%), [13.29, 25.31] | 1·66% (–7·20, 10·52) | 12 months | ||
| BHS, mean (SD) | TM = 45, F2F = 42 | 4.89 (4.64) | 4.43 (4.94) | 0.40 (0.12, 0.68)b,d | 8 weeks (~2 months) | Luxton 2016 (30) |
| TM = 42, F2F = 36 | 5.21 (5.10) | 5.53 (5.97) | 0.28 (–0.01, 0.58) b,d | 3 months | ||
| BDI-II, mean (SD) | TM = 45, F2F = 42 | 13.82 (12.02) | 11.74 (12.08) | 0.36 (0.06, 0.66) b,d | 8 weeks (~2 months) | |
| TM = 42, F2F = 36 | 14.76 (12.89) | 15.00 (12.61) | 0.16 (–0.16, 0.48) b,d | 3 months | ||
| BDI-II | TM = 131, F2F = 134 | NR | NR | 0.89 (NI)c,d | Post-treatment (~8–9 weeks) | Acierno 2016 (31) |
| 1.18 (NI) c,d | 3 months | |||||
| –0.29 (NI) c,d | 6 months | |||||
| BDI-II | TM = 64, F2F = 68 | NR | NR | –2.4 (–6.3, 1.5) | Post-treatment (~12 weeks) | Acierno 2017 (32) |
| –2.0 (–5.7, 1.6) | 3 months | |||||
| –0.3 (–4.1, 3.6) | 6 months | |||||
| BDI-II, mean (SE) | TM = 45, F2F = 45 | 19.26 (2.6) | 20.99 (2.7) | NRe | Post-treatment (~10 weeks) | Maieritsch 2016 (33) |
| 17.08 (2.2) | 17.29 (2.3) | NRe | 12 weeks | |||
| DASS depression, mean (SD) | TM = 39, F2F = 42 | 14.28 (3.9) | 7.5 (2.3) | < 0.001 | Post-treatment (16 weeks) | Chavooshi 2017 (34) |
| 13.31 (4.5) | 6.5 (3.5) | < 0.001 | 12 months | |||
| WHODAS, mean (SD)’ | TM = 56, F2F = 63 | 29.72 (1.25) | 30.13 (1.19) | t = 0.24, P = 0.809 | 12 weeks (3 months) | Choi 2014b (42) |
| 29.38 (1.12) | 30.60 (1.05) | t = –0.80, P = 0.426 | 24 weeks (6 months) | |||
| 29.04 (1.32) | 31.07 (1.24) | t = –1.12, P = 0.261 | 36 weeks (9 months) | |||
| PCL-M | TM = 131, F2F = 134 | NR | NR | –0.11 (NI) c,d | Post-treatment (~8–9 weeks) | Acierno 2016 (31) |
| –1.84 (NI) c,d | 3 months | |||||
| –0.66 (NI) c,d | 6 months | |||||
| PCL-M | TM = 64, F2F = 68 | NR | NR | −3.2 (−8.6, 2.1) | Post-treatment (~12 weeks) | Acierno 2017 (32) |
| −2.8 (−7.6 to 2.0) | 3 months | |||||
| 0.03 (−4.9 to 5.0) | 6 months | |||||
| PCL, mean (SE) | TM = 45, F2F = 45 | 48.07 (2.3) | 45.13 (2.5) | NRe | Post-treatment (~10 weeks) | Maieritsch 2016 (33) |
| 46.17 (2.2) | 45.94 (2.3) | NRe | 12 weeks | |||
| NPRS, mean (SD) | TM = 39, F2F = 42 | 6.15 (2.25) | 4.22 (1.65) | P < 0.001 | Post-treatment (16 weeks) | Chavooshi 2017 (34) |
| 6.36 (1.78) | 4.17 (1.14) | P < 0.001 | 12 m | |||
| DASS anxiety, mean (SD) | TM = 39, F2F = 42 | 15.9 (3.8) | 6.8 (3.4) | < 0.001 | Post-treatment (16 weeks) | |
| 15.3 (5.1) | 6.5 (5.3) | < 0.001 | 12 months | |||
| HbA1C, mean | TM = 43, F2F = 47 | 6.875 | 7.698 | –0.82 (–1.41, –0.24) | 12 months | Egede 2018 (45) |
| Telephone consultation vs. F2F | ||||||
| HAMD, mean (SD) | TM = 40, F2F = 18 | 13.3 (5.6) | 12.7 (7.2) | 0.60 (–3.15, 4.35) | 8 weeks (2 months) | Fann 2015 (43) |
| 11.5 (6.2) | 11.9 (6.1) | –0.40 (–3.81, 3.01) | 16 weeks (4 months) | |||
| 10.4 (6.4) | 12.1 (7.8) | –1.70 (–5.81, 2.41) | 24 weeks (6 months) | |||
| TM = 45 F2F = 47 | 12.8 (9.2) | 11.8 (7.2) | P = 0.93 | Post-treatment (18 weeks) | Kalapatapu 2014 (39) | |
| TM = 44 F2F = 47 | 13.4 (8.3) | 10.4 (6.0) | P = 0.12 | 3 months follow-up | ||
| TM = 42 F2F = 46 | 13.5 (8.7) | 10.4 (6.0) | P = 0.15 | 6 months | ||
| TM = 152 F2F = 141 | 13.58 (12.42 to 14.74)b | 12.51 (11.22 to 13.81) b | 1.07 (−0.63, 2.76), P = 0.22 | Post-treatment (18 weeks) | Mohr 2012 (38) | |
| TM = 146 F2F = 136 | 14.58 (13.45 to 15.71) b | 12.33 (11.01 to 13.64) b | 2.25 (0.52, 3.99), P = 0.01 | 3 months | ||
| TM = 134 F2F = 136 | 15.06 (13.84 to 16.27) b | 12.14 (10.84 to 13.45) b | 2.91 (1.20, 4.63) P < 0.001 | 6 months | ||
| HADS-depression, change from baseline (SD) | TM = 43 F2F = 35 | 1.86 (3.29) | 2.31 (4.40) | –0.45 (–2.19, 1.28) | 8 weeks (2 months) | Watson 2016 (36) |
| HADS-anxiety, change from baseline (SD) | TM = 43 F2F = 35 | 2.02 (3.54) | 2.11 (4.54) | –0.09 (–1.91, 1.73) | 8 weeks (2 months) | |
| PSWQ, mean change from baseline | TM = 87, F2F = 84 | –7.83 (11.45) | –6.73 (12.23) | P = 0.046 | 4 months | Alcantara 2016 (37) |
BDI, Beck depression inventory, BHS, Beck Hopelessness scale, DASS, Depression anxiety stress scale, GDS, Geriatric depression scale, HADS, Hospital anxiety and depression scale, HAMD, Hamilton rating scale for depression, NI, non-inferior, NPRS, Numeric pain rating scale, NR, not reported, PCL-M, Post-traumatic stress disorder checklist-military, PSWQ, Penn State Worry Questionnaire, WHODAS, World health organisation disability assessment schedule
aMean values with were measured at the specified follow-up times reported in the table
bStandardised difference using the baseline standard deviation; 90% Confidence interval used to evaluate non-inferiority
cCI not reported in the text, assessed as non-inferior (lower bound of CI < –8.8 for PCL-M and < –5.0 for BDI)
d90% Confidence interval used to evaluate non-inferiority
eTreatment difference not calculated in the study due to high levels of attrition
The three studies conducted in primary care that evaluated reductions in depression outcomes reached different conclusions: Mohr et al.(38) reported that telephone-delivered CBT in primary care patients with depression was inferior to face-to-face CBT by the 6-month follow-up, despite non-significant differences post-treatment; Kalapatapu et al.(39) found non-significant differences between the two CBT delivery methods at any time up to the 6-month follow-up in patients with depression and problematic alcohol use; and Alcantara et al.(37) showed that low-income Latinos receiving the intervention by telephone experienced greater worry reductions that those attending face-to-face consultations.
Three of the non-inferiority trials (28,31,32) considered video consultations were non-inferior to face-to-face treatment. Luxton et al.(30) found significant reductions in symptoms for both groups of patients with depression, but non-inferiority could not be firmly established.
Choi et al.(42) found both depression and disability improvements in their population of low-income older adults treated via video consultations were sustained longer than in those receiving the intervention face-to-face. Similarly, patients with depression and type 2 diabetes who received behavioural activation through video consultation experienced significant improvements in HbA1C levels compared to those treated face-to-face (45). In contrast, Chavooshi et al.(34) found that intensive short-term dynamic psychotherapy delivered face-to-face led to greater improvements in depression, anxiety and pain intensity in patients with medically unexplained pain. They also reported a lower understanding of content in patients treated via video consultation compared to face-to-face and suggested that the emotion-focused nature of their psychotherapy intervention may explain why patients in the face-to-face group had greater symptom improvements.
Among patients with depression, Choi et al.(41) reported high levels of treatment acceptance in both groups, but patients in the video consultation group had a more favourable attitude towards treatment. Egede et al.(29) showed non-significant differences in patient satisfaction and quality of life (SF-36 scores).
Therapeutic alliance was also similar between teleconsultations and face-to-face groups in a wide range of patient populations; patients with depression in primary care (40), PTSD (33), individuals undergoing counselling for substance abuse (35), patients with depression following traumatic brain injury (43), and patients with medically unexplained pain (34).
Attrition
Overall, treatment discontinuation was high and similar for both comparison groups in most studies. Maieritsch et al.(33) explained the higher than expected attrition rate led to a lack of sufficient statistical power that prevents them from conducting their original analyses. Luxton et al.(30) estimated their sample size assuming a 10% attrition rate, but their actual attrition was 32%.
Some studies showed higher discontinuation rates in the face-to-face group compared to teleconsultations (31,34,36–38), while other studies reported higher attrition in the teleconsultation group (30,32).
Mohr et al.(38) was the only study where the primary outcome was adherence to therapy. The authors found that attrition was significantly lower in primary care patients receiving CBT over the telephone compared to face-to-face (20.9% vs. 32.7%, P = 0.02). Lower discontinuation rates in the telephone group were also seen in other studies of low-income adults in primary care (37) and cancer patients (36).
Discussion
Overall, consultations via telephone and videoconference were as effective as face-to-face visits in improving clinical outcomes in primary care and mental health. This is not to say that teleconsultations are suited to all patients. A face-to-face consultation may be preferred in patients with high-risk conditions, who require a physical examination or who cannot communicate adequately by telephone or videoconference (46). In contrast, patients most likely to benefit from teleconsultations have been identified as those with chronic conditions, who require medical follow-ups, and patients with difficulties to travel to their health centre (either due to physical disability, or geographical dispersion, or work reasons) (47).
The majority of studies were conducted in high-income countries, interventions were heterogeneous and covered a range of therapeutic areas. Given country-specific variations in health systems, the reported effectiveness of teleconsultations may not be generalisable across clinical settings or treatments.
Studies in the primary care setting found the similar quality of care between the two modes of consultations, although patient experience appeared to be better in face-to-face consultations, with richer information provision and advice in face-to-face visits (48). The content and quality of clinician-patient interaction were found to be comparable via telephone and video consultation, although video consultations appeared to allow better rapport building (48). In contrast to face-to-face visits or videoconferencing, telephone consultations are restricted to verbal communication, the physician cannot observe ‘the whole picture’ such as the patient’s environment, their movement, body language and facial expressions, which may allow a more effective clinician-patient communication (21,47). In our review, patient satisfaction with teleconsultations and the therapeutic alliance was high across the studies that measured these outcomes (29,33–35,40,41,43). Telephone consultations may be more effective for patients with higher health literacy who are able to articulate their situation over the telephone, and health practitioners would need to take this into consideration. McKinstry et al.(25) found that patients using telephone consultations seemed to accurately recall the content of the consultation as well as patients in face-to-face visits; however, the general practitioners in the study regularly consulted over the telephone, and the study excluded patients unable to consent, with memory problems and those less literate (associated with poorer recall). Mohr et al.(38) found telephone consultations increased adherence to CBT treatment in primary care patients with depression, helping to overcome barriers and ambivalence toward treatment. However, it was suggested that teleconsultations may also help retain patients at greater risk for posttreatment deterioration, which might have influenced the poorer outcomes observed in patients given telephone consultations compared to those attending face-to-face visits. High attrition increased the risk of bias in many of the studies. The discontinuation rate of the included studies ranged from 0% up to 72%, which indicates that interventions delivered via the telephone or videoconference may not be acceptable to some groups of patients (49). Thus, teleconsultations may be as effective as face-to-face consultations, but only among participants who adhere to the interventions. Choi et al.(42) and Lindegaard-Pedersen et al.(21) reported that attrition was mainly due to deteriorating health problems leading to hospitalisation, nursing home placement and death in their population of older adults. Ramon et al.(18) noted higher discontinuations for smoking cessation in the telephone group, with fewer sessions possibly due to relapse.
Teleconsultations have the potential to improve equity and accessibility of care, particularly in regions where healthcare is less accessible. Results in studies of low-income adults (37,41,42) suggest that teleconsultations can be an effective way of treatment delivery in disadvantaged populations who may experience limited access to mental health services. McGrail et al.(23), however, reported no socioeconomic gradient in the overall use of teleconsultations.
While we did not specifically review economic evaluations comparing teleconsultations with face-to-face healthcare visits, some studies included cost analyses that showed teleconsultations offered significant time efficiencies compared to in-person primary care (12,26). On average teleconsultations were shorter (less than 10 minutes) compared to face-to-face visits at a health centre (average 15 to 30 minutes) (19). Patients using teleconsultations also attended fewer appointments, with significant cost-savings per person driven mainly by reduced travel and parking costs (26). Gordon et al.(22) found that teleconsultations reduced healthcare utilisation (e.g., lab tests, imaging), while the cost per episode in primary care and the proportion of follow-up visits within 3 weeks of the initial consultation were similar between teleconsultation and face-to-face visits. In contrast, Shi et al.(24) found that teleconsultations had less appropriate testing and more follow-up visits in patients with acute respiratory infections. In general, the evidence suggests that teleconsultations reduce the cost per episode of care, but may also increase the number treated (49,50).
Videoconferencing consultation has been found to be more likely to be used by younger patients and physicians who are technically informed (48). Implementing video conferencing technology in primary care has been previously highlighted as a challenge for patients and clinicians, with improvements in the infrastructure needed (48) as well as training for healthcare professionals (e.g., social-emotional and technical skills) (47). Technical problems with video conferencing systems were commonly reported in the studies reviewed (26,30,35). Half (50.3%) of the individuals in the video conferencing group of Luxton et al.(30) reported connectivity issues, and 35.7% of the treatment sessions required a phone call to resolve a technical issue. These kinds of issues may not prevent an adequate clinical assessment (49,51), and Choi et al.(41) recorded a low occurrence of technical problems related to the video consultations.
While developments in telehealth more broadly have the potential for better integration of patient information and communication, historically poorer continuity of care and empathetic communication with the patient on remote consultations have been highlighted as key areas of concern (52). Teleconsultations in general practice have often been restricted to those with an established doctor-patient relationship (53) on the grounds that an established therapeutic relationship contributes to better treatment continuity and clinical outcomes (46,47,50,53). Most patients in the included studies were seeing a new physician, although patients who were older and with more health problems were more likely to see a known physician with whom they previously interacted in a traditional face-to-face setting (23).
Limitations
This systematic review was limited to studies published from 2010 onwards. This was considered an appropriate time frame as technology has changed considerably since then, especially following the wider use of mobile phones in the general population.
Only studies published in English were included, and some studies from other cultural settings with different levels of acceptance for telemedicine interventions may have been missed. This review was also limited to adult patients, the effectiveness of teleconsultations in children and adolescents was not explored.
Patients receiving psychological care were part of specific subpopulations (e.g., military, low-income and older adults), and some had contributing conditions to their depression symptoms (e.g., unexplained medical pain, traumatic brain injury, or cancer). This may limit the generalisability of findings to wider patient populations requiring mental health services.
Only a few studies of mental health interventions were conducted in the primary care setting. Nevertheless, many of the mental health interventions included in this review could be potentially conducted in primary care, thus improving access to mental health support to a wider population.
Our results and conclusions were limited to the evidence in the included studies, which focused on comparative effectiveness and did not fully explore costs, cost-effectiveness, utilisation, or barriers to the implementation of telehealth modalities.
Conclusion
Patient care delivered by telephone and video consultation for suitable patients can be as effective as face-to-face clinic-based consultations for non-referred primary care services. Remote consultations may reduce workload in general practice and improve access to healthcare while maintaining the quality of care. However, appropriate implementation, including training of healthcare professionals, integration with practice information systems, service evaluation, and improved management of technical issues is essential to ensure effective and valuable clinical interventions. There remains considerable uncertainty about the impact of teleconsultations on healthcare utilisation and cost, particularly where there may be incentives in the funding system to increase low-value health service use. It is also important to consider which patients are most likely to benefit from face-to-face visits and design a funding model of teleconsultations that ensures reliable and effective clinical services that meet patient needs. Further research is needed to determine the best role for teleconsultations in terms of suitability for different patient groups and clinical conditions. As technologies rapidly evolve and healthcare needs change, good quality evidence is required to understand the effects of teleconsultations, either a standalone or as an integrated service, on health outcomes, patient and clinician satisfaction, and the overall cost of care.
Supplementary Material
Declaration
Ethical approval: This is a systematic review of published studies, no ethics approval needed.
Funding: No funding was received to conduct this study.
Conflict of interest: None declared.
Data availability: This is a systematic review of published studies, no primary data was used.
References
- 1. Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 2020; 20(1): 1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Car J, Koh GC, Foong PS, Wang CJ. Video consultations in primary and specialist care during the covid-19 pandemic and beyond. BMJ 2020; 371: m3945. [DOI] [PubMed] [Google Scholar]
- 3. Salud. SAd. El SAS impulsa la consulta telefónica para pacientes de Atención Primaria. www.sspa.juntadeandalucia.es/servicioandaluzdesalud/todas-noticia/el-sas-impulsa-la-consulta-telefonica-para-pacientes-de-atencion-primaria. Published 2020. Accessed 05/02/21.
- 4. NHS. General practice in the context of coronavirus (COVID-19). NHS England, 2020. [Google Scholar]
- 5. Ministero della Salute. Covid-19, al via triage telefonico da parte dei medici di famiglia. http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4084. Published 2020. Accessed 05/02/21.
- 6. ALTEMS. Analisi dei modelli organizzativi di risposta al Covid-19. ALTEMS (Alta Scuola di Economia e Management dei Sistemi Sanitari), 2020. [Google Scholar]
- 7. Uscher-Pines L, Sousa J, Jones Met al. Telehealth use among safety-net organizations in california during the COVID-19 pandemic. JAMA 2021; 325(11): 1106–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Greenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid-19. BMJ 2020; 368: m998. [DOI] [PubMed] [Google Scholar]
- 9. Bradford NK, Caffery LJ, Smith AC. Telehealth services in rural and remote Australia: a systematic review of models of care and factors influencing success and sustainability. Rural Remote Health 2016; 16(4): 4268. [PubMed] [Google Scholar]
- 10. Snoswell CL, Caffery LJ, Haydon HM, Thomas EE, Smith AC. Telehealth uptake in general practice as a result of the coronavirus (COVID-19) pandemic. Aust Health Rev 2020; 44(5): 737–40. [DOI] [PubMed] [Google Scholar]
- 11. Ignatowicz A, Atherton H, Bernstein CJet al. Internet videoconferencing for patient-clinician consultations in long-term conditions: a review of reviews and applications in line with guidelines and recommendations. Digit Health 2019; 5: 2055207619845831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Downes MJ, Mervin MC, Byrnes JM, Scuffham PA. Telephone consultations for general practice: a systematic review. Syst Rev 2017; 6(1): 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mughal F, Hossain MZ, Brady A, Samuel J, Chew-Graham CA. Mental health support through primary care during and after covid-19. BMJ 2021; 373: n1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sterne JAC, Savović J, Page MJet al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898. [DOI] [PubMed] [Google Scholar]
- 16. Sterne JA, Hernán MA, Reeves BCet al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355: i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nomura A, Tanigawa T, Muto Tet al. Clinical efficacy of telemedicine compared to face-to-face clinic visits for smoking cessation: multicenter open-label randomized controlled noninferiority trial. J Med Internet Res 2019; 21(4): e13520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ramon JM, Nerin I, Comino Aet al. A multicentre randomized trial of combined individual and telephone counselling for smoking cessation. Prev Med 2013; 57(3): 183–8. [DOI] [PubMed] [Google Scholar]
- 19. Seguranyes G, Costa D, Fuentelsaz-Gallego Cet al. ; Postpartum Telematics Research Group (Grupo de Grupo de Investigación Posparto Telemático (GIPT)GIPT). Efficacy of a videoconferencing intervention compared with standard postnatal care at primary care health centres in Catalonia. Midwifery 2014; 30(6): 764–71. [DOI] [PubMed] [Google Scholar]
- 20. Harrigan M, Cartmel B, Loftfield Eet al. Randomized trial comparing telephone versus in-person weight loss counseling on body composition and circulating biomarkers in women treated for breast cancer: the lifestyle, exercise, and nutrition (LEAN) study. J Clin Oncol 2016; 34(7): 669–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lindegaard Pedersen J, Pedersen PU, Damsgaard EM. Nutritional follow-up after discharge prevents readmission to hospital—a randomized clinical trial. J Nutr Health Aging 2017; 21(1): 75–82. [DOI] [PubMed] [Google Scholar]
- 22. Gordon AS, Adamson WC, DeVries AR. Virtual visits for acute, nonurgent care: a claims analysis of episode-level utilization. J Med Internet Res 2017; 19(2): e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McGrail KM, Ahuja MA, Leaver CA. Virtual visits and patient-centered care: results of a patient survey and observational study. J Med Internet Res 2017; 19(5): e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shi Z, Mehrotra A, Gidengil CA, Poon SJ, Uscher-Pines L, Ray KN. Quality of care for acute respiratory infections during direct-to-consumer telemedicine visits for adults. Health Aff (Millwood) 2018; 37(12): 2014–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McKinstry B, Watson P, Elton RAet al. Comparison of the accuracy of patients’ recall of the content of telephone and face-to-face consultations: an exploratory study. Postgrad Med J 2011; 87(1028): 394–9. [DOI] [PubMed] [Google Scholar]
- 26. Collins A, Burns CL, Ward ECet al. Home-based telehealth service for swallowing and nutrition management following head and neck cancer treatment. J Telemed Telecare 2017; 23(10): 866–72. [DOI] [PubMed] [Google Scholar]
- 27. McCarthy M, Leigh G, Arthur-Kelly M. Comparison of caregiver engagement in telepractice and in-person family-centered early intervention. J Deaf Stud Deaf Educ 2020; 25(1): 33–42. [DOI] [PubMed] [Google Scholar]
- 28. Egede LE, Acierno R, Knapp RGet al. Psychotherapy for depression in older veterans via telemedicine: a randomised, open-label, non-inferiority trial. Lancet Psychiatry 2015; 2(8): 693–701. [DOI] [PubMed] [Google Scholar]
- 29. Egede LE, Acierno R, Knapp RG, Walker RJ, Payne EH, Frueh BC. Psychotherapy for depression in older veterans via telemedicine: effect on quality of life, satisfaction, treatment credibility, and service delivery perception. J Clin Psychiatry 2016; 77(12): 1704–11. [DOI] [PubMed] [Google Scholar]
- 30. Luxton DD, Pruitt LD, Wagner A, Smolenski DJ, Jenkins-Guarnieri MA, Gahm G. Home-based telebehavioral health for U.S. military personnel and veterans with depression: a randomized controlled trial. J Consult Clin Psychol 2016; 84(11): 923–34. [DOI] [PubMed] [Google Scholar]
- 31. Acierno R, Gros DF, Ruggiero KJet al. Behavioral activation and therapeutic exposure for posttraumatic stress disorder: a noninferiority trial of treatment delivered in person versus home-based telehealth. Depress Anxiety 2016; 33(5): 415–23. [DOI] [PubMed] [Google Scholar]
- 32. Acierno R, Knapp R, Tuerk Pet al. A non-inferiority trial of prolonged exposure for posttraumatic stress disorder: in person versus home-based telehealth. Behav Res Ther 2017; 89: 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Maieritsch KP, Smith TL, Hessinger JD, Ahearn EP, Eickhoff JC, Zhao Q. Randomized controlled equivalence trial comparing videoconference and in person delivery of cognitive processing therapy for PTSD. J Telemed Telecare 2016; 22(4): 238–43. [DOI] [PubMed] [Google Scholar]
- 34. Chavooshi B, Mohammadkhani P, Dolatshahee B. Telemedicine vs. in-person delivery of intensive short-term dynamic psychotherapy for patients with medically unexplained pain: a 12-month randomized, controlled trial. J Telemed Telecare 2017; 23(1): 133–41. [DOI] [PubMed] [Google Scholar]
- 35. King VL, Brooner RK, Peirce JM, Kolodner K, Kidorf MS. A randomized trial of web-based videoconferencing for substance abuse counseling. J Subst Abuse Treat 2014; 46(1): 36–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Watson M, White C, Lynch A, Mohammed K. Telephone-delivered individual cognitive behavioural therapy for cancer patients: an equivalence randomised trial. Psychooncology 2017; 26(3): 301–8. [DOI] [PubMed] [Google Scholar]
- 37. Alcántara C, Li X, Wang Y, Canino G, Alegría M. Treatment moderators and effectiveness of engagement and counseling for Latinos intervention on worry reduction in a low-income primary care sample. J Consult Clin Psychol 2016; 84(11): 1016–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mohr DC,, Ho J,, Duffecy J,, Reifler D,, Sokol L,, Burns MN,, Jin L,, Siddique J. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: a randomized trial. JAMA 2012; 307(21):2278–85.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kalapatapu RK, Ho J, Cai X, Vinogradov S, Batki SL, Mohr DC. Cognitive-behavioral therapy in depressed primary care patients with co-occurring problematic alcohol use: effect of telephone-administered vs. face-to-face treatment-a secondary analysis. J Psychoactive Drugs 2014; 46(2): 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Stiles-Shields C, Kwasny MJ, Cai X, Mohr DC. Therapeutic alliance in face-to-face and telephone-administered cognitive behavioral therapy. J Consult Clin Psychol 2014; 82(2): 349–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Choi NG, Hegel MT, Marti N, Marinucci ML, Sirrianni L, Bruce ML. Telehealth problem-solving therapy for depressed low-income homebound older adults. Am J Geriatr Psychiatry 2014; 22(3): 263–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Choi NG, Marti CN, Bruce ML, Hegel MT, Wilson NL, Kunik ME. Six-month postintervention depression and disability outcomes of in-home telehealth problem-solving therapy for depressed, low-income homebound older adults. Depress Anxiety 2014; 31(8): 653–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fann JR, Bombardier CH, Vannoy Set al. Telephone and in-person cognitive behavioral therapy for major depression after traumatic brain injury: a randomized controlled trial. J Neurotrauma 2015; 32(1): 45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Watson HJ, McLagan N, Zerwas SC, et al. Cost-Effectiveness of internet-based cognitive-behavioral treatment for bulimia nervosa: results of a randomized controlled trial. J Clin Psychiatry. 2018; 79(1): 16m11314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Egede LE, Walker RJ, Payne EH, Knapp RG, Acierno R, Frueh BC. Effect of psychotherapy for depression via home telehealth on glycemic control in adults with type 2 diabetes: subgroup analysis of a randomized clinical trial. J Telemed Telecare 2018; 24(9): 596–602. [DOI] [PubMed] [Google Scholar]
- 46. RACGP. Guide to providing telephone and video consultations in general practice. The Royal Australian College of General Practitioners,2020. https://www.racgp.org.au/FSDEDEV/media/documents/Clinical%20Resources/Guidelines/Guide-to-providing-telephone-and-video-consultations.pdf. [Google Scholar]
- 47. Jiménez-Rodríguez D, Santillán García A, Montoro Robles J, Rodríguez Salvador MDM, Muñoz Ronda FJ, Arrogante O. Increase in video consultations during the covid-19 pandemic: healthcare professionals’ perceptions about their implementation and adequate management. Int J Environ Res Public Health. 2020; 17(14): 5112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hammersley V, Donaghy E, Parker Ret al. Comparing the content and quality of video, telephone, and face-to-face consultations: a non-randomised, quasi-experimental, exploratory study in UK primary care. Br J Gen Pract 2019; 69(686): e595–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. The Cochrane database of systematic reviews. 2015; 9: CD002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform 2010; 79(11): 736–71. [DOI] [PubMed] [Google Scholar]
- 51. Hammersley ML, Okely AD, Batterham MJ, Jones RA. An internet-based childhood obesity prevention program (time2bhealthy) for parents of preschool-aged children: randomized controlled trial. J Med Internet Res 2019; 21(2): e11964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Horton TJB. Three key quality considerations for remote consultations. https://www.health.org.uk/news-and-comment/blogs/three-key-quality-considerations-for-remote-consultations. Published 2020. Accessed 08/02/2021.
- 53. MBS. COVID-19 Temporary MBS Telehealth Services. http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Factsheet-TempBB. Published 2021. Accessed 21/05/2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.