Abstract
The impact of the coronavirus disease 2019 (COVID-19) pandemic on admission patterns and outcomes at a burn center is still largely unknown. The aim of this study was to determine how the COVID-19 pandemic affected the epidemiology of burn admissions at a major metropolitan burn center. This retrospective cohort study examined how the COVID-19 pandemic affected burn volumes and time to presentation. All burn admissions were included from January 20 to August 31 for the years 2020, 2019, and 2018. The COVID-19 pandemic group included admissions from January 20, 2020 to August 31, 2020 and was compared to the nonpandemic group comprised of admissions from January 20 to August 31 in 2018 and 2019. Subgroup analysis was performed according to meaningful dates during the COVID-19 pandemic including the first U.S. COVID-19 case, shelter-in-place, and state reopening orders. Admission volumes were 403 patients in the COVID-19 pandemic group compared to a mean of 429 patients in the nonpandemic group, which correlated to a 5.8% decrease in volume during the pandemic. The pandemic group showed an increase in time to presentation of 1 day (P < .0001). Subgroup analysis demonstrated stable admission volumes and an increase in time to presentation of 1 day (P < .0001) at each time point. During shelter-in-place orders, there were higher rates of second/third-degree burns and operative burns (94.7 vs 56.3% and 45.6 vs 27%, P < .0001, P = .013). During the pandemic, there were stable admission volumes, delayed time to admission, and an increase in operative burns during shelter-in-place orders. This reinforces the need to maintain appropriate burn center staffing and resources during the COVID-19 pandemic.
The coronavirus disease 2019 (COVID-19) has affected millions of people globally and was declared a pandemic by the World Health Organization on March 11, 2020.1 The impact of the COVID-19 pandemic on the U.S. healthcare system continues to evolve. There is evidence that since the beginning of March 2020, social distancing measures, shelter-in-place orders, school closures, cancelation of elective procedures, concerns over hospital capacity, and fears of contracting COVID-19 led to sharp declines in healthcare spending.2 Non-COVID-19-related hospital admissions fell precipitously in the United States at the start of the pandemic. Several hospitals reported declines in admissions for acute medical illness, including stroke and acute myocardial infarction.3–11 There is, however, minimal formally reported data from American burn centers regarding the impact of the COVID-19 pandemic on the epidemiology of burn patients.
Early studies showed a reduction in burn incidence, emergencies, and volume of admissions during the pandemic, due in part to the confinement of the population and the decrease in industrial activity.12, 13 As the impact of the COVID-19 pandemic continues to evolve, understanding its impact on a large metropolitan burn center can provide important information to help guide the management of a burn center moving forward. We hypothesized that the pandemic affected a patient’s decision to seek burn care as well as pediatric and work-related burn injuries. The purpose of this study was to retrospectively evaluate burn admissions to our burn center during the COVID-19 pandemic.
METHODS
This was a retrospective cohort study conducted with the approval of the Institutional Review Board and Research Oversight Committee at the university hospital and safety-net hospital, respectively. Primary study endpoints included the number of admissions and days from injury to burn center admission. Secondary endpoints included pediatric burn admissions, work-related injury, burn admissions requiring operative intervention, and length of stay. Patient data were collected for admissions to the burn center during the COVID-19 pandemic and compared to a historical cohort from years 2019 and 2018. These admissions were combined to help reduce confounding in the nonpandemic comparison group. Since the first U.S. case of COVID-19 was noted on January 20, 2020, the electronic medical record (EMR) was reviewed from January 20 to August 31 for the years 2020, 2019, and 2018.
The patient population included all thermal, chemical, and electrical burn adult and pediatric inpatient admissions over these time periods. Pediatric admissions were defined as age younger than 18 years old. Nonburn wound admissions and vulnerable (prisoners and pregnant women) patient populations were excluded.
The EMR was queried to obtain patient demographics, admission, hospital course, and discharge variables. Patient data were collected from admission to either discharge or death. Missing values were specified for each variable and were excluded from the analysis.
Subgroup analysis was performed according to meaningful dates during the course of the COVID-19 pandemic. Three separate subgroups were analyzed. Subgroup 1 included patients from January 20, 2020 to March 23, 2020, which corresponded to the first confirmed case of COVID-19 in the United States to the day before the local shelter-in-place order was implemented. Subgroup 2 consisted of burn admissions from March 24, 2020 to April 24, 2020, the time period that spanned the local shelter-in-place order to when the state reopened businesses. Lastly, subgroup 3 included all patients from April 25, 2020 to August 31, 2020, which captured the day after businesses reopened in the state to the end of the study’s data collection period.
SAS software (version 9.4; SAS Institute, Inc., Cary, NC) was used to analyze descriptive and inferential statistics for the study cohort. Continuous variables were reported as medians (interquartile range). Categorical variables were reported as frequency (percentage). Inferential statistics were calculated using Wilcoxon rank-sum tests for continuous variables, and chi-square test and Fisher’s exact test for categorical variables. All hypothesis testing was two-sided and conducted at a .05 level of significance.
RESULTS
The study sample population included a total of 1261 patients. In 2020 from January 20 to August 31, there were 403 inpatient burn admissions that comprised the COVID-19 pandemic exposure group compared to 436 and 420 in 2019 and 2018, respectively, which made up the nonpandemic comparison group. The COVID-19 pandemic group had a 5.8% decrease in admission volumes compared to the mean admission volume from the previous 2 years.
The second primary endpoint was the time between burn injury and burn center admission. During the pandemic, patients admitted to the burn center presented a median of 1 day later when compared to the nonpandemic group (P < .0001, Table 1). This outcome was then categorized as patients who were admitted the same day of their burn injury versus those who were admitted after the day of their burn injury. Sixty-eight percent of patients presented a day or more after their burn injury during the pandemic compared to 35.4% in the nonpandemic group (P < .0001, Table 1).
Table 1.
Burn demographic, admission, and hospital data during pandemic versus nonpandemic years
| Study Variables | COVID-19 Pandemic | Nonpandemic | Total | P |
|---|---|---|---|---|
| Admission volume | 403 | 858 (429) | 1261 | |
| Age, years | 38.0 (19.2–55.5) | 36.6 (20.1–53.8) | 37.1 (19.8–54.5) | .416* |
| Missing | 44 | 44 | ||
| Sex | ||||
| Male | 252 (62.5%) | 538 (65.9%) | 790 (64.8%) | .381† |
| Female | 151 (37.5%) | 277 (34.0%) | 428 (35.1%) | |
| Missing | 42 | 42 | ||
| Pediatric burn | 96 (23.8%) | 225 (26.2%) | 321 (25.5%) | .361† |
| Missing | 44 | 44 | ||
| Work injury | 33 (8.2%) | 75 (10.7%) | 108 (9.8%) | .744† |
| Missing | 2 | 158 | 160 | |
| Abuse | 9 (2.2%) | 7 (1.0%) | 16 (1.5%) | .043† |
| Missing | 2 | 158 | 160 | |
| TBSA | 5 (2–10%) | 4.5 (2–9%) | 5 (2–9%) | .289* |
| Missing | 43 | 234 | 277 | |
| Second/third-degree burn | ||||
| None | 42 (10.5%) | 227 (26.4%) | 269 (21.3%) | <.0001† |
| 1–10% | 283 (70.4%) | 496 (57.7%) | 779 (61.7%) | |
| 11–20% | 51 (12.7%) | 83 (9.7%) | 134 (10.6%) | |
| >20% | 26 (6.5%) | 54 (6.3%) | 80 (6.3%) | |
| Required OR | 150 (37.2%) | 312 (36.4%) | 462 (36.6%) | .768† |
| ICU admit | 60 (14.9%) | 185 (21.6%) | 245 (19.4%) | .005† |
| LOS (<20% TBSA) | 2 (1–5) | 3 (1–8) | 1.5 (1–3) | <.0001* |
| Missing | 48 | 97 | 84 | |
| Mortality | 2 (0.6%) | 21 (3.2%) | 23 (2.3%) | .008† |
| Missing | 59 | 210 | 269 | |
| Patient transfers | 132 (32.9%) | 286 (35.6%) | 418 (34.7%) | .354† |
| Missing | 2 | 55 | 58 | |
| Injury to admit | 1 (0–3) | 0 (0–1) | 0 (0–1) | <.0001* |
| >Same day | ||||
| Yes | 236 (68.0%) | 187 (35.4%) | 503 (43.7%) | <.001† |
| No | 111 (32.0%) | 341 (64.6%) | 647 (56.3%) | |
| Missing | 56 | 55 | 111 | |
| Transfer patients | ||||
| Injury to admit | ||||
| Same day | 76 (64.4%) | 169 (62.6%) | 245 (63.1%) | .284† |
| >Same day | 42 (35.6%) | 101 (37.4%) | 143 (36.9%) |
TBSA, total body surface area; OR, operation; ICU, intensive care unit; LOS, length of stay.
Categorical variables are presented as number (column frequency %), continuous variables are presented as median (interquartile range), and nonpandemic admission volumes are presented as number (2-year mean). COVID-19 pandemic group: (January 20, 2020–August 31, 2020) burn admissions; Nonpandemic group: (January 20, 2018–August 31, 2018 and January 20, 2019–August 31, 2019) burn admissions.
*Wilcoxon rank-sum two-sample test.
†Chi-square test.
When comparing the COVID-19 pandemic group versus the nonpandemic group, there were no significant differences with regard to pediatric burn admissions (23.8 vs 26.2%), work-related burn injuries (8.2 vs 10.7%), or number of transfer admissions (32.9 vs 35.6%). Patients requiring operative intervention were similar between groups (37.2 vs 36.4%) despite an increase in the proportion of second- and third-degree burns in the pandemic group (89.5 vs 73.6%, P < .0001). The COVID-19 pandemic group had a decreased median length of stay of 1 day for burns with less than 20% total body surface area (TBSA) compared to the nonpandemic group (Table 1).
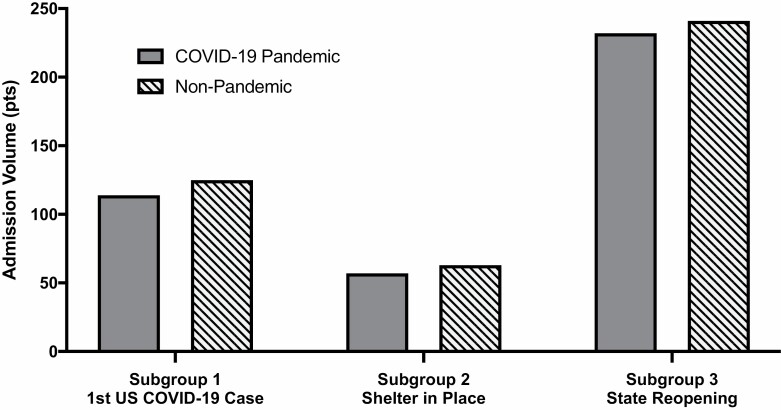
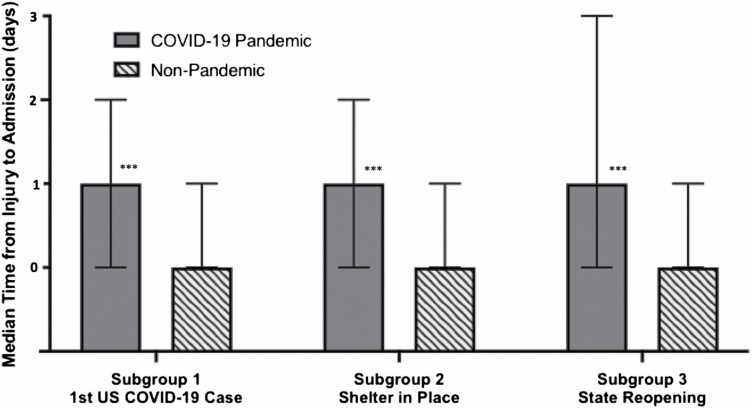
Subgroup analysis was performed, by stratifying admissions according to meaningful dates during the COVID-19 pandemic timeline: the first confirmed case of COVID-19 in the United States (subgroup 1), the local shelter-in-place order (subgroup 2), and the state reopening of businesses (subgroup 3). Burn center volumes during the COVID-19 pandemic decreased by 8.8% in subgroup 1, 9.5% in subgroup 2, and 3.7% in subgroup 3 compared to nonpandemic years. Within each subgroup, the COVID-19 pandemic group showed a statistically significant increase in time to presentation of 1 day (Tables 2–4, Figures 1 and 2).
Table 2.
Subgroup 1, burn demographic, admission, and hospital data after first U.S. case of COVID-19
| Study Variables | COVID-19 Pandemic | Nonpandemic | Total | P |
|---|---|---|---|---|
| Admission volume | 114 | 250 (125) | 364 | |
| Pediatric burn | 26 (22.8%) | 76 (30.4%) | 102 (28.0%) | .135* |
| Missing | 30 | 30 | ||
| Work injury | 13 (11.5%) | 25 (12.6%) | 38 (12.2%) | .685* |
| Missing | 1 | 52 | 53 | |
| Abuse | 3 (2.7%) | 1 (0.5%) | 4 (1.3%) | .111* |
| Missing | 1 | 52 | 53 | |
| TBSA | 5 (2.4–8.8) | 4 (2–7.8) | 4 (2–8) | .054† |
| Missing | 18 | 78 | 96 | |
| Second/third-degree burn | ||||
| None | 17 (15.0%) | 74 (29.5%) | 91 (25.0%) | |
| 1–10% | 79 (69.9%) | 144 (57.4%) | 223 (61.3%) | .032* |
| 11–20% | 11 (9.7%) | 20 (8.0%) | 31 (8.5%) | |
| >20% | 6 (5.3%) | 13 (5.2%) | 19 (5.2%) | |
| Required OR | 29 (25.4%) | 91 (36.4%) | 120 (33.0%) | .039* |
| LOS (<20% TBSA) | 2 (1–4) | 3 (1–7) | 3 (1–6) | .0001† |
| Missing | 15 | 37 | 52 | |
| Patient transfers | 36 (32.1%) | 94 (43.9%) | 130 (39.9%) | .039* |
| Missing | 2 | 36 | ||
| Injury to admit | 1 (0–2) | 0 (0–1) | 0 (0–1) | <.0001† |
| >Same day | ||||
| Yes | 56 (61.5%) | 65 (27.8%) | 121 (37.2%) | <.0001* |
| No | 35 (38.5%) | 169 (72.2%) | 204 (62.7%) | |
| Missing | 23 | 16 | 39 | |
| Transfer patients | ||||
| Injury to admit | ||||
| Same day | 20 (66.7%) | 62 (68.1%) | 82 (67.8%) | |
| >Same day | 10 (33.3%) | 29 (31.9%) | 39 (32.2%) | .369* |
TBSA, total body surface area; OR, operation; ICU, intensive care unit; LOS, length of stay.
Categorical variables are presented as number (column frequency %), continuous variables are presented as median (interquartile range), and nonpandemic admission volumes are presented as number (2-year mean). COVID-19 pandemic group: (January 20, 2020–March 23, 2020) burn admissions; Nonpandemic group: (January 20, 2018–March 23, 2018 and January 20, 2019–March 23, 2019) burn admissions.
*Chi-square test.
†Wilcoxon rank-sum two-sample test.
Table 3.
Subgroup 2, burn demographic, admission, and hospital data during shelter-in-place orders
| Study Variables | COVID-19 Pandemic | Nonpandemic | Total | P |
|---|---|---|---|---|
| Admission volume | 57 | 126 (63) | 183 | |
| Pediatric burn | 16 (28.1%) | 42 (33.3%) | 58 (31.7%) | .479* |
| Missing | 14 | 14 | ||
| Work injury | 2 (3.5%) | 6 (7.9%) | 8 (6.0%) | .701* |
| Missing | 50 | 125 | ||
| Abuse | 2 (3.5%) | 2 (2.6%) | 4 (3.0%) | .769* |
| Missing | 50 | 50 | ||
| TBSA | 5 (2–10) | 4.5 (2–8.5) | 5 (2–9.8) | .145† |
| Missing | 5 | 166 | 187 | |
| Second/third-degree burn | ||||
| None | 3 (5.3%) | 55 (43.7%) | 58 (31.7%) | |
| 1–10% | 38 (66.7%) | 59 (46.8%) | 97 (53.0%) | <.0001* |
| 11–20% | 10 (17.5%) | 9 (7.1%) | 19 (10.4%) | |
| >20% | 6 (10.5%) | 3 (2.4%) | 9 (4.9%) | |
| Required OR | 26 (45.6%) | 34 (27.0%) | 60 (32.8%) | .013* |
| LOS (<20% TBSA) | 2 (1–6) | 4 (1–9.5) | 3 (1–7) | .015† |
| Missing | 23 | 14 | 84 | |
| Patient transfers | 16 (28.1%) | 36 (32.4%) | 52 (31.0%) | .563* |
| Missing | 15 | 15 | ||
| Injury to admit | 1 (0–2) | 0 (0–1) | 0 (0–1) | .002† |
| >Same day | ||||
| Yes | 34 (69.4%) | 43 (37.7%) | 77 (47.2%) | .0002* |
| No | 15 (30.6%) | 71 (62.3%) | 86 (52.8%) | |
| Missing | 8 | 12 | 20 | |
| Transfer patients | ||||
| Injury to admit | ||||
| Same day | 9 (56.3%) | 19 (54.3%) | 28 (54.9%) | |
| >Same day | 7 (43.8%) | 16 (45.7%) | 23 (45.1%) | .218* |
TBSA, total body surface area; OR, operation; ICU, intensive care unit; LOS, length of stay.
Categorical variables are presented as number (column frequency %), continuous variables are presented as median (interquartile range), and nonpandemic admission volumes are presented as number (2-year mean). COVID-19 pandemic group: (March 24, 2020–April 24, 2020) burn admissions; Nonpandemic group: (March 23, 2018–April 24, 2018 and March 23, 2019–April 24, 2019) burn admissions.
*Chi-square test.
†Wilcoxon rank-sum two-sample test.
Table 4.
Subgroup 3, burn demographic, admission, and hospital data following state reopening
| Study Variables | COVID-19 Pandemic | Nonpandemic | Total | P |
|---|---|---|---|---|
| Admission volume | 232 | 482 (241) | 714 | |
| Pediatric burn | 54 (23.3%) | 107 (22.2%) | 161 (22.6%) | .747* |
| Work injury | 18 (7.8%) | 44 (10.3%) | 62 (9.4%) | .543* |
| Missing | 1 | 56 | 57 | |
| Abuse | 4 (1.7%) | 4 (1.0%) | 8 (1.2%) | .267* |
| Missing | 1 | 56 | 57 | |
| Required OR | 95 (41.0%) | 187 (38.8%) | 282 (39.5%) | .581* |
| Second/third-degree burn | ||||
| None | 22 (9.5%) | 98 (20.3%) | 120 (16.8%) | |
| 1–10% | 166 (71.6%) | 293 (60.7%) | 459 (64.2%) | .002* |
| 11–20% | 30 (12.9%) | 54 (11.2%) | 84 (11.8%) | |
| >20% | 14 (6.0%) | 38 (7.9%) | 52 (7.3%) | |
| LOS (<20% TBSA) | 2 (1–6) | 4 (1–8) | 3 (1–8) | .001† |
| Missing | 23 | 61 | 84 | |
| Patient transfers | 80 (34.5%) | 156 (32.6%) | 236 (33.2%) | .624* |
| Missing | 5 | |||
| Injury to admit | 1 (0–3) | 0 (0–1) | 0 (0–2) | <.0001† |
| >Same day | ||||
| Yes | 146 (70.5%) | 159 (35.0%) | 305 (46.1%) | <.0001* |
| No | 61 (29.5%) | 296 (65.1%) | 357 (53.9%) | |
| Missing | 25 | 27 | 52 | |
| Transfer patients | ||||
| Injury to admit | ||||
| Same day | 47 (65.3%) | 88 (61.1%) | 135 (62.5%) | |
| >Same day | 25 (34.7%) | 56 (38.9%) | 81 (37.5%) | .239* |
TBSA, total body surface area; OR, operation; LOS, length of stay.
Categorical variables are presented as number (column frequency %), continuous variables are presented as median (interquartile range), and nonpandemic admission volumes are presented as number (2-year mean). COVID-19 pandemic group: (April 25, 2020–August 31, 2020) burn admissions; Nonpandemic group: (April 25, 2018–August 31, 2018 and April 25, 2019–August 31, 2019) burn admissions.
*Chi-square test.
†Wilcoxon rank-sum two-sample test.
Figure 1.
Burn center admission volumes. COVID-19 pandemic: admissions during 2020 and nonpandemic: admissions during 2018 and 2019. x-axis: subgroup 1 (admissions from January 20 to March 23), subgroup 2 (admissions from March 24 to April 24), and subgroup 3 (admissions from April 25 to August 31); y-axis: admission volumes (%).
Figure 2.
Time to hospital presentation. COVID-19 pandemic: admissions during 2020 and nonpandemic: admissions during 2018 and 2019. x-axis: subgroup 1 (admissions from January 20 to March 23), subgroup 2 (admissions from March 24 to April 24), and subgroup 3 (admissions from April 25 to August 31); y-axis: median days from burn injury to admission (days). ***P < .0001.
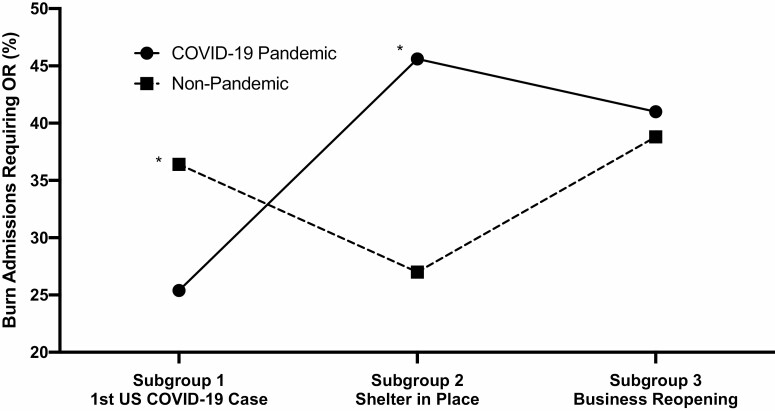
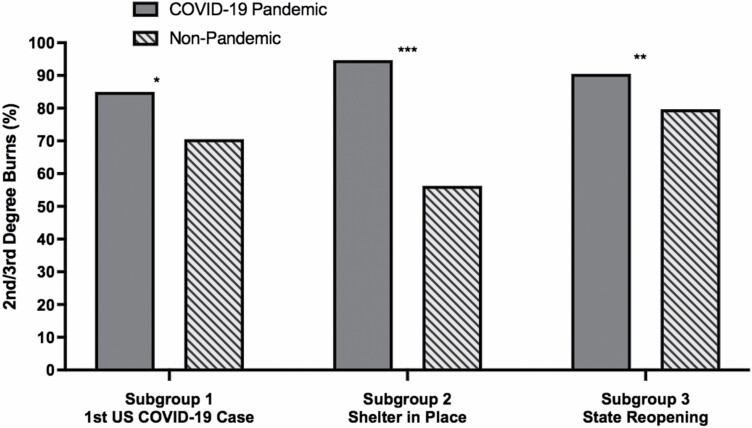
Furthermore, subgroup 2, which corresponded to the local shelter-in-place timeframe, showed an increase in burn admissions requiring operative intervention in the COVID-19 pandemic group compared to the nonpandemic group (45.6 vs 27%, P = .013) and also displayed an increased proportion of second- and third-degree burns (94.7 vs 56.3%, P < .0001; Table 3, Figures 3 and 4).
Figure 3.
Burn admissions requiring operations. COVID-19 pandemic: admissions during 2020 and nonpandemic: admissions during 2018 and 2019. x-axis: subgroup 1 (admissions from January 20 to March 23), subgroup 2 (admissions from March 24 to April 24), and subgroup 3 (admissions from April 25 to August 31); y-axis: burn admissions requiring operations (%). OR, operations; *P < .05.
Figure 4.
Percentage of patients with second/third-degree burns. COVID-19 pandemic: admissions during 2020 and nonpandemic: admissions during 2018 and 2019. x-axis: subgroup 1 (admissions from January 20 to March 23), subgroup 2 (admissions from March 24 to April 24), and subgroup 3 (admissions from April 25 to August 31); y-axis: second/third-degree burns (%). *P < .05, **P < .01, ***P < .0001.
DISCUSSION
This is one of the first descriptive studies of how the COVID-19 pandemic affected admissions and hospital course at a large metropolitan burn center, and future studies will be aimed at further understanding the impact of these study findings on patient outcomes.
Burn volumes remained relatively stable during the pandemic, with a slight decrease noted of 5.8%, in contrast to other studies that noted a decrease in total burn inpatient admissions ranging from 7 to 49% during the pandemic.13–17 Even as elective surgeries were canceled, burn volumes and burn admissions requiring surgery continued at stable rates. This potentially highlights the importance of maintaining appropriate staffing and resources for a burn center during the pandemic based on local epidemiology and patient needs.
Prior to this study, anecdotal observations suggested patients avoided presenting to the hospital early after burn injury due to fear of contracting COVID-19 at the hospital. Study data demonstrated a median delay of 1 day from burn injury to hospital admission during the pandemic compared to nonpandemic years. Further data collection and analysis are necessary to understand the factors leading to this finding and whether it affects patient outcomes. In this study, 68% of patients presented a day or more after injury in 2020. Of note, this was not explained by transfer admissions, as the percentage of transfers that were admitted after the day of injury was similar in each group. Delayed presentation to a burn center is associated with worse outcomes including increased rates of cellulitis and increased time to excision and grafting.18, 19 However, data on the incidence of burn wound infection are currently lacking and will need to be a focus of future studies.
Information regarding pediatric burn admissions during the pandemic is mixed. Some centers noted increased volumes, while others noted an overall decrease from previous years, but an increase in relative emergency room visits for pediatric burns compared to overall emergency room visits.13,17,20 Pediatric burn epidemiologic studies showed the majority of pediatric burns occur in the home.21 Despite hypothetical concern for increased pediatric admissions due to the shelter-in-place order, volumes of pediatric admissions did not differ from previous years in this study. Reasons for this are not entirely clear at this time.
Overall, there was a decreased length of stay for burns less than 20% TBSA, consistent with findings from other studies.22 A potential explanation for this may be an increased clinical and administrative emphasis on timely, medically appropriate patient discharges to limit patient hospital exposure and expand bed capacity for surge planning. These unprecedented hospital surges and limited bed capacity brought to the forefront the role of adequate social services support and ancillary support to facilitate effective discharges. This is especially important for burn care at a regional safety-net hospital with patients who have numerous comorbidities as well as social and financial needs in addition to their burn care.
Notably, during the shelter-in-place orders (subgroup 2), there was an increase in operative and second/third-degree burns during the COVID-19 pandemic compared to the previous years. This suggests that patients are presenting in a delayed fashion with deeper operative burns during the pandemic, in particular during the shelter-in-place orders. Most burns do occur in the home.23 The reasons for an increase in operative burns are not entirely understood at this time and will need to be investigated further.
Limitations include the retrospective nature of this study and dependence on EMR documentation. Using the COVID-19 pandemic as the main exposure is difficult to truly quantify. There is no data to determine whether patients altered their lifestyles secondary to the pandemic. This is a retrospective cohort study, so the control over known and unknown confounding factors in the data is limited. The results presented here are reflective of a single-institution experience at an urban burn center at one of the largest safety-net hospitals in the Southeast. Given the regionalism of burn epidemiology as well as the differing timeline of COVID-19 across the United States, extent of surge cases, and regional management thereof, the results may not be generalizable to other burn centers.
CONCLUSIONS
Understanding the impact of the COVID-19 pandemic on the epidemiology of burn patients is important. There are limited data on this subject, and this study is the largest descriptive review to date. This study shows stable admission volumes throughout the pandemic with an increase in delayed burn presentation as well as an increase in operative burns during shelter-in-place orders. Further research is needed to understand whether this delay increases complications. Given minimal changes in admissions, an increase in patients presenting delayed and operative volumes, this study reinforces the need to maintain appropriate burn center staffing and resources during a crisis such as the COVID-19 pandemic.
Funding: This study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Awards Number UL1TR002378, TL1TR002382. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement. None declared.
REFERENCES
- 1. Johns Hopkins University Coronavirus Resource Center. COVID-19 dash-board by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. 2020; https://coronavirus.jhu.edu/map.html; accessed 24 Jan. 2021.
- 2. Cox C, Kamal R, McDermott D.. How have healthcare utilization and spending changed so far during the coronavirus pandemic? Peterson-KFF Health System Tracker, 6 Aug. 2020; https://www.kff.org/coronavirus-covid-19/issue-brief/how-have-healthcare-utilization-and-spending-changed-so-far-during-the-coronavirus-pandemic/; accessed 24 Jan. 2021. [Google Scholar]
- 3. Cigna. Cigna Study finds reduced rates of acute non-elective hospitalizations during the COVID-19 pandemic. Bloomfield, CT: Cigna, Apr 2020; https://www.cigna.com/about-us/newsroom/studies-and-reports/deferring-care-during-covid-19. [Google Scholar]
- 4. Hartnett KP, Kite-Powell A, DeVies Jet al. ; National Syndromic Surveillance Program Community of Practice . Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian SV. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med 2016;168:16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. De Rosa S, Spaccarotella C, Basso Cet al. ; Società Italiana di Cardiologia and the CCU Academy Investigators Group . Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 2020;41:2083–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mahmud N, Hubbard RA, Kaplan DEet al. Declining cirrhosis hospitalizations in the wake of the COVID-19 pandemic: a national cohort study. Gastroenterology 2020;159:1134–6.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis 2020;29:104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Solomon MD, McNulty EJ, Rana JSet al. The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020;383:691–3. [DOI] [PubMed] [Google Scholar]
- 10. Trinkl J, Sizemore O.. Return to near average number of ED visits for acute MI and strokes 12 weeks post COVID-19 emergency declaration. Epic Health Research Network, 7 July 2020; accessed 24 Jan. 2021. [Google Scholar]
- 11. Nourazari S, Davis SR, Granovsky Ret al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med 2021;42:203–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barret J, Chong S, Depetris Net al. Burn center function during the COVID-19 pandemic: an international multi-center report of strategy and experience. Burns 2020;46:1021-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kruchevsky D, Arraf M, Levanon S, Capucha T, Ramon Y, Ullmann Y. Trends in burn injuries in Northern Israel during the COVID-19 lockdown. J Burn Care Res 2021;42:135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Varma P, Kazzazi D, Anwar MUet al. The impact of COVID-19 on adult burn management in the UK: a regional centre experience. J Burn Care Res 2021; 42:998–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kumar S, Kain R, More Aet al. Burns and COVID-19—initial experience and challenges. J Burn Care Res 2020. doi: 10.1093/jbcr/iraa217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rogers AD, Cartotto R. The impact of COVID-19 on burn care at a major regional burn center. J Burn Care Res 2021;42:110–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Williams FN, Chrisco L, Nizamani R, King BT. COVID-19 related admissions to a regional burn center: the impact of shelter-in-place mandate. Burns Open 2020;4:158–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Curch D, Elsayed S, Reid Oet al. Burn wound infections. Clin Microbiol Rev 2020;19:403-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Xiao-Wu W, Herndon DN, Spies M, Sanford AP, Wolf SE. Effects of delayed wound excision and grafting in severely burned children. Arch Surg 2002;137:1049–54. [DOI] [PubMed] [Google Scholar]
- 20. Sethuraman U, Stankovic C, Singer Aet al. Burn visits to a pediatric burn center during the COVID-19 pandemic and ‘Stay at home’ period. Burns 2021;47:491–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee CJ, Mahendraraj K, Houng Aet al. Pediatric burns: a single institution retrospective review of incidence, etiology, and outcomes in 2273 burn patients (1995–2013). J Burn Care Res 2016;37:e579–85. [DOI] [PubMed] [Google Scholar]
- 22. Farroha A. Reduction in length of stay of patients admitted to a regional burn centre during COVID-19 Pandemic. Burns 2020;46:1707–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Greenhalgh DG. Management of burns. N Engl J Med 2019;380:24. [DOI] [PubMed] [Google Scholar]