Abstract
The collection of patient reported outcomes (PROs) allows us to incorporate the patient’s voice into their care in a quantifiable, validated manner. Large-scale collection of PROs is facilitated by the electronic health record and its portal, though, historically, patients have eschewed the portal and completed patient-reported outcome measures in the clinic via tablet. Furthermore, access and use of the portal is associated with known racial inequities. Our institution oversees the largest clinical PRO program in the world, and has a long history of racially equitable PRO completion rates via tablet. However, when the COVID-19 pandemic forced us to remove tablets from clinics and rely exclusively on portal use for PRO completion, profound racial disparities resulted immediately. Our experience quantifiably demonstrates the magnitude of inequity that the portal, in its current configuration, generates and serves as a cautionary tale to other health care systems and electronic health records.
Keywords: patient-reported outcomes, portal, disparities, inequity
In 2014, Mass General Brigham built what would become the largest patient reported outcomes (PRO) program in the world, spanning 10 hospitals, 200 clinics, and more than 75 specialties.1 Arguably one of the best indices of quality and value in health care, PROs allow us to integrate the patient’s voice into their care, converting it to a quantitative measure to assess whether their condition is improving or worsening. In addition, routine collection and integration of PROs into clinical care has been widely associated with: improved patient outcomes, ranging from improved overall survival in patients with malignancy to better palliative care experiences; the ability to adequately describe postoperative outcomes and set expectations for patients undergoing arthroplasty; identifying and effectively triaging patients with occult depression and anxiety in routine primary care and obstetrics populations, and countless other fields as diverse as rheumatology, neurology, and surgery.2–11 Finally, PROs represent a powerful tool to promote health care equity by empowering patients to express their voice in health outcomes in a quantifiable, validated manner, reducing the chance that implicit bias could skew the provider understanding or assessment of the patient’s symptomatology .
In prior years, patient reported outcome measures (PROMs) were completed on paper, and the ability to aggregate large volumes of data was limited. Advances within the electronic health record (EHR) and the patient portal have changed this, enabling modern day PRO programs and the electronic dissemination and storage of millions of PROMs responses and the insights that they generate.12–14 The majority of current programs assign PROMs through the patient portal in the week prior to a clinic visit; on the day of the visit, tablets with PROMS are distributed to any patient who failed to complete them online.1,15–19 It is important to note, however, that historically the majority of patients have not chosen to use the portal to complete PROMs. As an example, prior to the COVID-19 pandemic only 17% of Mass General Brigham’s 10 million PROs were collected using our online patient portal. The balance were collected via tablet in clinic.1 Of note, within our health care system PRO completion rates are equitable (irrespective of race or ethnicity, which is self-identified and recorded within our EHR) when the PROMs are administered on tablets in clinic.
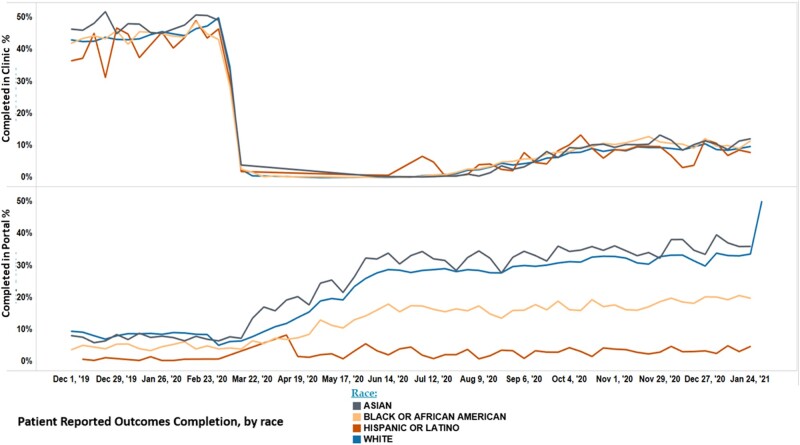
On March 13, 2020, all tablets used for PRO collection were removed from our clinics to both limit the spread of COVID-19 in clinics and to facilitate their use in our inpatient units at the height of the pandemic. This rapid transition prompted an overnight shift in the capture of PROs, from primarily in-clinic to the online portal; the shift to the portal introduced profound inequity in data collection (Figure 1) literally overnight. Suddenly, patients who self-identified as Black provided PROs at half the rate of white patients, and patients who identified as Hispanic almost stopped completing PROMs altogether.
Figure 1.
Patient-reported outcomes completion rate, by race and modality, over time. When it comes to hearing the patient’s voice and preferences, the portal leaves our Black and Latin(x) patients behind #medtwitter #inequity #telemedicine.
This development is unfortunately not surprising. Rather, it is a stark and troubling example of the uneven benefits and unfulfilled promises of the patient portal. As a result of policy and financial investments, more than 90% of providers offer patient portals; however, only about a third of patients use the portal.20 In addition, health care systems have long struggled with equitable implementation of patient portals. Even with the advent of mobile-enabled portals and the parity in the percentage of patients who identify as White, Black, and Hispanic with a smartphone (82%, 80%, 79%, respectively, based on the 2019 Pew Report), data clearly show that hospitals are less likely to offer Black and Hispanic patients portal access.2 Furthermore, even when offered access, Black and Hispanic patients are more likely to never log onto the portal.21 In their sentinel study utilizing Rogers diffusion of innovation model, Emani et al, showed that the primary predictor of using a portal is the perception that it will offer some sort of relative advantage. Together, this body of literature shows that EHR vendors and hospital systems have not made the portal available to or clearly communicated the benefits to patients of color. An even more fundamental underpinning of the problem is that due to systematic, structural racist housing, policy, and business practices, Black and Hispanic patients are markedly less likely than white patients to have the ability to connect to broadband internet in their homes.22 In fact, data shows that as a county’s African-American population rises, broadband availability begins to fall; the opposite relationship is seen when there is an increase in white residents.23 Our data showing pre-pandemic racial disparities in PRO completion when using the portal is also consistent with this body of literature and stands in stark contrast to the equity in completion rates seen when PROs are collected on tablet in clinic. (Figure 1, bottom panel).
Specifically at Mass General Brigham, in the first quarter of the year prior to the COVID 19 pandemic, we achieved equitable PRO completion rates across race/ethnicity when questionnaires were collected in the clinic using a tablet (Figure 1, top panel). At the onset of the pandemic when we shifted from primarily in-person tablet collection to exclusive use of the online portal for collection of PROs, disparities by patient race and ethnicity quickly emerged. We discovered this trend within a few months, and quickly leveraged a variety of outreach tools to increase online portal use including text messaging patients with links to complete PROs, embedding PROs in our electronic previsit check-in process, and including links to PROs in e-mail alerts to patients regarding upcoming appointments. Despite these efforts, the inequities in PRO collection rate persisted and were refractory to intervention (Figure 1, bottom panel). Now, rather than having PRO data reflective of our entire community, we have a cache of data where Black patients’ voices have been diminished by half, and we have almost completely lost the experience of Latin(x) patients.
What are we to do when faced with such data? First and foremost, it is critical that such a finding is viewed as unacceptable. The immediate decline in Black and Latin(x) PROs means that we have eliminated their voice from our care programs—making us less likely to incorporate these patients’ experiences and preferences into their care, preventing the same level of consideration and individualized medicine that our white patients receive. This type of systematic racism has far-reaching consequences. As a health care system, we aggregate our PROs and share with payers to define “high value performance,” which in turn influences payer decisions about reimbursement. Furthermore, PROs throughout our system inform a large volume of academic output, which is later used to define what is “normal” for any disease or condition.24–27 When we generate these “normal” expectations for patient experience, they now normalize an overwhelmingly white experience and effectively ignore the experience of Black and Latin(x) patients. Of course, there are many examples in health care where the voices of patients of color are ignored, leading to marked inequities in health outcomes. Our data illustrate the key issue that even when inequities do not exist, they can be created quite literally overnight, and we must be vigilant in monitoring for such changes. This finding is incredibly important, as failure to immediately rectify this problem allows for further creep of the structural racism that is already present in medicine and affects everything from our physiologic calculators to our willingness to refer Black women to cardiac catheterization at a rate that is comparable to white men.28,29
Awareness of this issue, however, allows for the opportunity to self-correct. We suggest 3 key steps to ensure that all patients are able to access online portals:
EHR vendors must develop their online portals in languages other than English: The Health Information Technology for Economic and Clinical Health Act (HITECH) provided over $30 billion dollars of federal funding to develop and promote “meaningful use” of the EHR and patient portals; vendors received a large swath of these funds. Despite this windfall, EHR vendors have been largely remiss in creating portals in languages other than English. When a patient presents for care in person, Title VI of the Civil Rights Act of 1964 requires recipients of federal financial assistance, including health care providers, to not discriminate on the basis of race, color or national origin; this has led to the widespread presence of interpreter services within the hospital. We must have the same expectation of EHR vendors, particularly as they bypass brick and mortar clinics and hospitals to interact with the patient directly in their home, thereby serving as a direct repository of patient reported data. The current solution of health care systems being forced to purchase software that can translate an English-only portal requires health care systems to inappropriately bear the cost of inequitable user interfaces, supplied by the EHR vendors, and would be cost-prohibitive for safety net systems.
Health care systems must create a universal access portal policy and establish anti-racist strategiesfor the communities they serve: Previous research shows that “opt-in” policies for portal use led to large socioeconomic disparities, and minority patients are offered access less often than white patients. In work by Ancker et al, establishing a “universal access policy” eliminated racial and ethnic disparities in portal registration in a safety net hospital within 4 years.30 However, while universal portal registration is critical, it is far downstream of key structural issues, like access to broadband within communities of color. Health care systems are powerful organizations within their local communities and wield significant hiring, policy, contracting, and political power that can be used to benefit historically disenfranchised patient populations. For example, in 2021 Mass General Brigham launched a multi-million dollar effort (United Against Racism) to examine and eliminate the barriers to equity that exist within our own organization.31 This sweeping initiative deeply engages with the community to tackle pertinent social determinants of health and implement innovative service lines in partnership with community stakeholders (eg, mobile health units, tablet loan programs with local hotspot connections) and leverages our weight as a purchaser and an employer to increase diverse hiring, support diverse contractor workforces, and create an external policy and contracting strategy. This strategy supports equity and anti-racism efforts, including equitable access to broadband, digital infrastructure, and financial investments in communities of color. If other health care systems throughout the country could leverage similar resources, it would be possible to begin to make real progress in reducing the structural barriers that patients of color face in trying to obtain health care.
Improve portal usability: Most research on improving portal use focuses on individual level interventions (ie, training a patient how to navigate through the portal). This represents a relatively weak intervention, as it affects only one patient at a time. A better approach would be to focus on portal usability and user-centered design. A study by Tieu et al showed that, on average, it took a patient with adequate health literacy almost 12 minutes to log into a portal and find lab results; limited health literacy patients required 22 minutes to complete the same task.32 EHR vendors and health care systems should focus on improving basic functionality, accessibility, and comprehension to a wide range of users rather than building advanced or esoteric functionality that is only applicable to a small cohort of patients.33
While the patient portal has the potential to dramatically improve the lives of our patients, the cautionary example of our PRO program shows that, in its current state, the online portal disproportionately benefits white patients. It is critical that health care systems, regulators, payers, and EHR vendors work together to ensure that a legacy of this technology is not worsening existing disparities, and even worse, creating those where they do not already exist.
FUNDING
This research received no specific grant from any funding agency in the public, commercial or not for profit sectors.
AUTHOR CONTRIBUTIONS
RS was responsible for the conception of the work, acquiring the data, drafting the work, revising the work and approving the work. As the corresponding author, she is responsible and accountable for the accuracy of the work.
JR was responsible for analyzing and interpreting data, drafting and revising the work, performing edits and final approvals, and is accountable for all accuracy of the work.
TS was responsible for the acquisition of the data, interpreting the data, revising and critically appraising the work, and participating in and incorporating edits.
DATA AVAILABILITY STATEMENT
The data underlying this article cannot be shared publicly due to the privacy of the patients involved. The data will be shared on reasonable request to the corresponding author.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1.Sisodia RC, Dankers CD, Orav J, et al. Factors associated with increased collection of patient reported outcomes within a large health care system. JAMA Netw Open 2020; 3 (4): e202764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gotay CC, Kawamoto CT, Bottomley A, Efficace F.. The prognostic significance of patient reported outcomes in cancer clinical trials. J Clin Oncol 2008; 26 (8): 1355–63. [DOI] [PubMed] [Google Scholar]
- 3.Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient reported outcomes for symptom monitoring during routine cancer treatment. JAMA 2017; 318 (2): 197–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sabah S, Alvand A, Knight R. et al. Patient reported function and quality of life after revision total knee arthroplasty: an analysis of 10,727 patients from the NHS PROMS Program [published online ahead of print Mar 19, 2021]. J Arthroplasty 2021. doi: 10.1016/j.arth.2021.03.037. [DOI] [PubMed] [Google Scholar]
- 5.Graham AK, Greene CJ, Kwasny MJ, et al. Coached mobile app platform for the treatment of depression and anxiety among primary care patients: a randomized clinical trial. JAMA Psychiatry 2020; 77 (9): 906–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maselko J, Sikander S, Turner EL, et al. Effectiveness of a peer delivered, psychosocial intervention on maternal depression and child development at 3 years postnatal: a cluster randomized trial. Lancet Psychiatry 2020; 7 (9): 775–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ziolokowski N, Behman R, Klassen A,et al. Determining the independent risk factors for worse SCAR-Q scores and future scar revision surgery. Plast Reconstr Surg 2021; 148 (1): 203–12. [DOI] [PubMed] [Google Scholar]
- 8.Estave P, Beeghly S, Anderson R.. Learning the full impact of migraine through patient voices: a qualitative study [published online ahead of print June 3, 2021]. Headache 2021. doi: 10.1111/head.14151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDermott MM, Tian L, Criqui MH.. Perceived versus objective change in walking ability in peripheral artery disease: results from 3 randomized clinical trials of exercise therapy. J Am Heart Assoc 2021; 10 (12): e017609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrold L, Bryson J, Lehman T.. Association between baseline anti-cyclic citrullinated peptide antibodies and 6 month clinical response following abatacept or TNF inhibitor treatment: A real world analysis of biologic experienced patients with RA [published online ahead of print June 2021]. Rheumatol Ther 2021; 8 (2): 937–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lordon RJ, Mikles SP, Kneale L, et al. How patient generated health data and patient reported outcomes affect patient clinician relationships: a systematic review. Health Informatics J 2020; 26 (4): 2689–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Willke RJ, Burke LB, Erickson P.. Measuring treatment impact: a review of patient reported outcomes and other efficacy endpoints in approved product labels. Control Clin Trials 2004; 25 (6): 535–52. [DOI] [PubMed] [Google Scholar]
- 13.Tarlov AR, Ware JE, Greenfield S.. The medical outcomes study: an application of methods of monitoring the results of medical care. JAMA 1989; 262 (7): 925–30. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine Committee on Quality of Health Care. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 15.Patt D, Wilfong L, Hudson K, et al. Implementation of electronic patient reported outcomes for symptom monitoring in a large multisite community oncology practice. JCO Clin Cancer Inform 2021; 5: 615–21. [DOI] [PubMed] [Google Scholar]
- 16.Basch E, Mody G, Dueck A.. Electronic patient reported outcomes as digital therapeutics to improve cancer outcomes. JCO Oncol Pract 2020. Sep; 16 (9): 541–2. [DOI] [PubMed] [Google Scholar]
- 17.Stehlik J, Rodriguez-Correa C, Spertus JA, et al. Implementation of real time assessment of patient reported outcomes in a heart failure clinic: a feasibility study. J Card Fail 2017; 23 (11): 813–6. [DOI] [PubMed] [Google Scholar]
- 18.Bernstein D, McIntyre AW, Baumhauer JF.. Effect of assessment administration method and timing on patient reported outcome measures competion and scores: overview and recommendations. Musculoskeletal Care 2020; 18 (4): 535–40. [DOI] [PubMed] [Google Scholar]
- 19.Mou D, Horn DM, Heng M.. Primary care physicians perceived value of patient reported outcomes (PROs) in clinical practice: a mixed methods study [published online ahead of print May 20, 2021]. BMJ Qual Saf 2021. doi: 10.1136/bmjqs-2020-012206. [DOI] [PubMed] [Google Scholar]
- 20.Anthony D, Campos Castillo C, Lim PS.. Who isn’t using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff (Millwood) 2018; 37 (12): 1948–54. [DOI] [PubMed] [Google Scholar]
- 21.Sarkar U, Karter A, Liu J, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011; 18 (3): 318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The Digital Divide: Percentage of households by Broadband Internet Subscription, computer type, race and Hispanic origin. The United States Census Bureau. 2015; https://www.census.gov/library/visualizations/2017/comm/internet.html. Accessed April 21, 2021.
- 23.The racial equality and economic opportunity case for expanding broadband. Third Way. 2019. https://www.thirdway.org/report/the-racial-equality-and-economic-opportunity-case-for-expanding-broadband. Accessed April 21, 2021.
- 24.Melnic CM, Paschalidis A, Katakam A, Bedair HS, Heng M; MGB Arthroplasty Patient Reported Outcomes Writing Committee. Patient reported mental health score influences physical function after primary total knee arthroplasty. J Arthroplasty 2021; 36 (4): 1277–83. [DOI] [PubMed] [Google Scholar]
- 25.Alimena S, Sullivan MW, Philp L, et al. Patient reported outcome measures among patients with vulvar cancer at various stages of treatment, recurrence and survivorship. Gynecol Oncol 2021; 160 (1): 252–9. [DOI] [PubMed] [Google Scholar]
- 26.Karhade AV, Sisodia RC, Bono CM, et al. Surgeon level variance in achieving clinical improvement after lumbar decompression: the importance of adequate risk adjustment. Spine J 2021; 21 (3): 405–10. [DOI] [PubMed] [Google Scholar]
- 27.De Marchi F, Berry JD, Chan J, et al. Patient reported outcome measures in amyotrophic lateral sclerosis. J Neurol 2020; 267 (6): 1754–9. [DOI] [PubMed] [Google Scholar]
- 28.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians recommendations for cardiac catheterization. N Engl J Med 1999; 340 (8): 618–26. [DOI] [PubMed] [Google Scholar]
- 29.Vyas D, Eisenstein L, Jones D. Hidden in Plain sight: reconsidering the use of race correction in clinical algorithms. N Engl J Med 2020; 383 (9): 874–82. [DOI] [PubMed]
- 30.Ancker JS, Nosal S, Hauser D, Hauser, et al. Access policy and digital divide in patient access to medical records. Health Policy Technol 2017; 6 (1): 3–11. [Google Scholar]
- 31.How Mass general Brigham Plans to Dismantle Racism in and Outside of Hospital Walls. https://www.wbur.org/commonhealth/2020/10/28/united-against-racism-boston-hospital-plan. Accessed April 21, 2021.
- 32.Tieu L, Schillinger D, Sarkar U, et al. Online patient websites for electronic health record access among vulnerable populations: portals to nowhere? J Am Med Inform Assoc 2017; 24 (e1): e47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peacock S, Reddy A, Leveille S, et al. Patient portals and personal health information online: perception, access and use by US adults. J Am Med Inform Assoc 2017; 24 (e1): e173–e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article cannot be shared publicly due to the privacy of the patients involved. The data will be shared on reasonable request to the corresponding author.