Abstract
Anxiety is associated with sleep disturbance and insomnia. Mindfulness-based interventions, such as Mindfulness-based Stress Reduction, have shown consistent anxiety reduction. Mindfulness training has been theorized to affect reinforcement learning, affecting habitual behaviors such as smoking and overeating, but a direct mechanistic link between the use of mindfulness training for anxiety reduction and improvement in sleep has not been studied. Moreover, the mechanisms by which mindfulness may affect worry and subsequent sleep disturbances have not been elucidated. This study protocol evaluates the impact an app-based mindfulness training program for anxiety has on decreasing worry, and improvement in sleep. A randomized controlled study will be conducted in approximately 80 adults with worry that interferes with their sleep. Subjects will be randomly allocated (1:1) to two groups: treatment as usual (TAU) or TAU + app-based mindfulness training (MT; Unwinding Anxiety app). The primary outcomes will be the nonreactivity subscale of the Five Facet Mindfulness Questionnaire and PROMIS sleep quality measures. Secondary outcomes will include the Penn State Worry Questionnaire, Generalized Anxiety Disorder-7, and Multidimensional Assessment of Interoceptive Awareness scale. This study is the first to test the mechanism of app-based mindfulness training on worry and sleep disturbance. Testing the mechanistic effects of mindfulness training using the Science of Behavior Change (SOBC) framework will help move the field forward both in further elucidation of potential mechanisms of mindfulness (e.g., targeting reinforcement learning), and determining whether such a platform may be a viable method for delivering high-fidelity treatment at scale and for a low cost.
Keywords: science of behavior change, mindfulness, sleep, worry, reinforcement learning, negative reinforcement, anxiety
Sleep disturbance affects approximately 20% of Americans (Garbarino, Lanteri, Durando, Magnavita, & Sannita, 2016). The Centers for Disease Control and Prevention report that insufficient sleep is associated with increased risk for obesity, diabetes, high blood pressure, coronary heart disease, stroke, mental distress, and all-cause mortality (Liu et al., 2016). Poor sleep also has negative effects on occupational functioning and quality of life, and fatigue-related performance failures may contribute to motor vehicle crashes and work injuries, among other problems (Garbarino et al., 2016; Simon & VonKorff, 1997).
Worry is common among people with insomnia (McGowan, Behar, & Luhmann, 2016); research has demonstrated that worrying in particular contributes to sleep disturbance (Bagley, Kelly, Buckhalt, & El-Sheikh, 2015; Yan et al., 2014). A study of adults with high worry levels found that worry on a particular day predicted increased sleep disturbance the same night (McGowan et al., 2016). A 24-hour monitoring study indicated that participants with high levels of worry in bed had lower sleep efficiency (expressed as a percentage of time in bed), increased nocturnal awakenings, and a higher heart rate than those who did not experience high levels of worry (Weise, Ong, Tesler, Kim, & Roth, 2013). Further, worry that is experimentally manipulated has been shown to have an effect on sleep; participants who were told they would have to give a speech immediately upon waking from a nap took longer to fall asleep than those without this directive, suggesting that worry about the speech interfered with sleep onset (Gross & Borkovec, 1982). Thus, further elucidation of pathways that reinforce worry may help identify specific treatments and mechanistic pathways that directly address the contributions of worry to sleep disturbances.
Worry is widely regarded as the central defining feature of generalized anxiety disorder, although it also occurs in other anxiety disorders (Association, 2013). A common working definition of worry is “a chain of thoughts and images, negatively affect-laden, and relatively uncontrollable,” representing an attempt to engage in mental problem solving on an issue with an uncertain outcome (T. D. Borkovec, Robinson, Pruzinsky, & DePree, 1983). In a model developed by Borkovec and colleagues, individuals engage in worry as a way to avoid unpleasant emotions, resulting in decreased distress and an increased sense of control—essentially an avoidance response (T. Borkovec, Ray, & Stober, 1998; T. D. Borkovec et al., 1983).
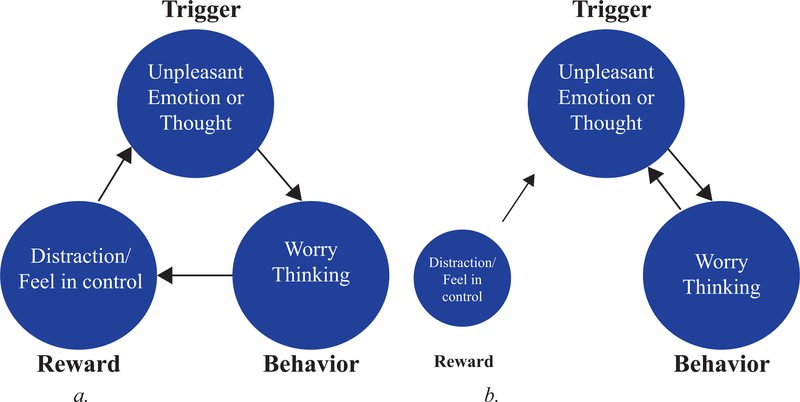
Current research shows that worry is also associated with a tendency to react to emotional experiences as if they are threatening in order to avoid those experiences (Roemer, Salters, Raffa, & Orsillo, 2005; Salters-Pedneault, Tull, & Roemer, 2004). In other words, worry is triggered as a mental response or mental behavior to unpleasant emotions. When worry is engaged as avoidance or a distraction for triggers such as negative thoughts and emotional states, the reduction in these feelings can lead to worry becoming “a negatively reinforced avoidant behavior” (Sibrava & Borkovec, 2008; B. F. Skinner, 1963) (see Figure 1a). Over time, worry as a mental behavior may be reinforced enough that it becomes habitual in nature, operating largely out of conscious control (Suhler & Churchland, 2009). This can be conceptualized as a habit loop that is formed in the same way as other conditioned behaviors, building on over 100 years of data supporting reinforcement learning as a basic learning process (B.F. Skinner, 1953; B. F. Skinner, 1963; Thorndike, 1898).
Figure 1.
Figure 1a. Development of a ‘habit loop’ via positive and negative reinforcement.
Figure 1b. Worry triggers itself when it feels less rewarding.
Importantly, worry as an avoidance strategy comes with two critical caveats: (1) worry is unpleasant, and (2) often worry thinking doesn’t consistently solve the problems that triggered it. When the negative affective qualities of worry are strong enough, the prefrontal cortex disengages, impeding higher-order prefrontal cortical function, such as problem solving (Arnsten, 2009, 2015). Additionally, when worry becomes habitual, the negative reinforcement pathway can spiral out of control; when the negative emotional experience of worry thinking increases to the level at which it is no longer rewarding, it becomes its own trigger for more worry thinking: it feeds itself (see Figure 1b). In accord, Tallis and Eysenck (1994) proposed that worry engages fight-or-flight states through alerting and (theoretically) preparing individuals for unresolved threatening situations. A prolonged fight-or-flight state may have far-reaching health consequences, ranging from myocardial infarction to insomnia (Brosschot, Gerin, & Thayer, 2006). Individuals who worry may be overly susceptible to reactive worry habit loops, as fatigue has also been shown to impede prefrontal cortical function (Casse-Perrot et al., 2016). These data suggest mechanistic avenues for treatment development; targeting worry may help individuals break these reactive cycles and treat the underlying cause of sleep disturbance in individuals with anxiety.
In conventional cognitive frameworks, anxiety is perceived as an overestimation of danger, and an underestimation of one’s ability to cope with it (Beck, Emery, & Greenberg, 1985). Cognitive therapies aim to interrupt the cycle of worry by replacing maladaptive cognitions with more constructive ones. Additionally, cognitive therapies that specifically target insomnia (e.g., cognitive behavioral therapy for insomnia [CBT-i]), have become first-line therapies for the treatment of insomnia due to their relative efficacy and clinically meaningful effect sizes (Trauer, Qian, Doyle, Rajaratnam, & Cunnington, 2015). By providing clear instructions for sleep hygiene, such as getting out of bed if one can’t fall asleep within a certain period of time, and not associating bed with television and screen time, CBT-i helps individuals learn to remove factors that become associated with being awake in bed. However, for individuals who cycle into anxious worry to a degree that impairs prefrontal cortical function, other strategies are needed. Next-generation behavioral treatments such as mindfulness training have shown promise both in efficacy and cost (treatment is largely delivered in group format), with effect sizes rivaling gold-standard treatments (Goyal et al., 2014; Hofmann, Sawyer, Witt, & Oh, 2010). Furthermore, a pilot intervention study found that providing participants with a combined MBSR and CBT-i curriculum reduced insomnia to non-clinically significant levels in most participants (Ong, Shapiro, & Manber, 2008). A second, 12 month follow-up study demonstrated that more than half of participants had no relapse of insomnia (Ong et al., 2008).
Mindfulness can be defined as the awareness that arises when paying attention in the present moment, on purpose and nonjudgmentally (Kabat-Zinn, 1990). In other words, when someone is being mindful, the attitudinal quality of not judging and allowing the experience to unfold with curiosity helps avoid being triggered by either positive or negative affective states, thus avoiding habitual behavior (Brewer & Pbert, 2015). Individuals learn to pay attention, pause, and “be with” their urges to habitually react, instead of acting on them. Importantly, this is fundamentally different than other cognitive techniques that encourage individuals to distract themselves or substitute another behavior when triggered. Instead of changing, suppressing, resisting, or avoiding triggers, mindfulness training helps people turn toward these thoughts, emotions, and body sensations. We have found that mindfulness training directly targets reinforcement habit loops by decoupling the urges to habitually react to triggers from subsequent actions. For example, in studies of cigarette smoking and emotional eating, mindfulness training was found to mechanistically decouple cigarette or food craving from smoking or eating, with a subsequent fivefold increase in smoking cessation rates, and a 40% reduction in craving-related eating, respectively (Brewer et al., 2011; Elwafi, Witkiewitz, Mallik, Thornhill-IV, & Brewer, 2013; Ashley E. Mason, Jhaveri, Cohn, & Brewer, 2017). People with insomnia tend to be outcome-driven and respond to external sleep cues (e.g. “I should be in bed by 10:30” or “It’s important to sleep because I have a presentation tomorrow”) instead of responding to their physiological states (Ong, Ulmer, & Manber, 2012). Mindfulness training, which helps participants increase awareness of their body, may help individuals respond more appropriately to sleep cues as they become more attuned to their physiological state.
Mindfulness training may be unique in its ability to tap into reinforcement learning. Reinforcement learning is dependent upon the rewards of one’s actions; however, if someone is habitually reacting to a trigger, he or she may not be aware of the present-moment reward value of the action. He or she is acting out a behavior whose value was determined in the past. Without updated information, the behavior’s value remains the same. A simple analogy is storing money in a mattress for 50 years, going to the store, and realizing that more money is needed to buy goods today than decades ago. By bringing awareness to the action, one experiences the actual value of the behavior, which gets updated in one’s memory. In the same way, when one pays attention when getting caught in a worry thought loop, the result of the behavior becomes clearer, leading to a natural neural depreciation of its reward value. For example, the individual sees more clearly that reactive worry is contributing to difficulties in falling asleep. Additionally, as one deepens a mindfulness practice, the rewards of curious awareness, even of unpleasant emotional states, become clearer, because curiosity feels better than anxiety or worry thinking. Thus, mindfulness training may act through reinforcement learning to dismantle anxiety habit loops, by updating old reward values of worry thinking, and revealing more rewarding rewards (Brewer, 2019). This may, in turn, help individuals break out of worry habit loops that contribute to poor sleep.
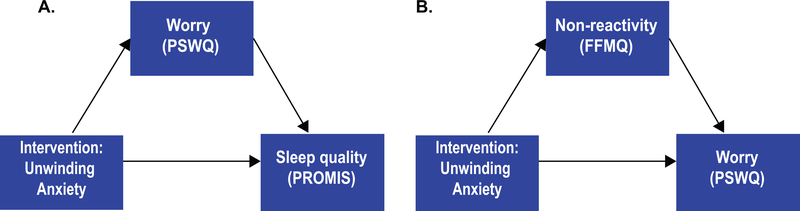
Guided by scientific evidence of core psychological mechanisms that perpetuate unhealthy behaviors, we developed an application (app)-based digital therapeutic program that delivers mindfulness training in a standardized, high-fidelity and accessible manner, to help individuals overcome anxiety (Unwinding Anxiety app). We designed it to mechanistically target the reinforcement learning process by training in mindfulness to help individuals 1) identify their habitual worry thinking patterns, and 2) learn to be with unpleasant emotions without reacting. The Unwinding Anxiety app bears similarity to the combined MBSR/CBT-i curriculum studied by Ong et al – and the principles, components, and activities overlap significantly. Both Unwinding Anxiety and MBSR/CBT-i include a focus on basic mindfulness tenets (e.g. present-focused awareness of body sensations) and activities (e.g. breathing meditations, body scans). Unwinding Anxiety has a specific focus on targeting anxious thoughts, and the content more specifically addresses the science of behavior change. Recently, the National Institutes of Health (NIH) articulated the Obesity-Related Behavioral Intervention Trials model for developing behavioral treatments for chronic diseases. This model provides a roadmap for iterative intervention development based on the identification of a clinical problem that can be addressed behaviorally, and clear goals and milestones of a stepwise process from behavioral mechanisms elucidation to Phase III efficacy trial initiation (Czajkowski et al., 2015). Additionally, the NIH encourages an experimental medicine approach to facilitate translational research: the Science of Behavior Change (SOBC) initiative (Riddle & Group, 2015). The SOBC approach involves testing whether an intervention engages an intended target, and whether target engagement leads to a desired behavior change outcome (Eisenberg et al., 2017). This framework is ideal for testing potential mechanisms of mindfulness as they relate to sleep. For example, changes in self-reported measures of mindfulness, such as the Five Facet Mindfulness Questionnaire (FFMQ) can be tracked and measured to determine if they moderate the effect of mindfulness training on sleep (see Figure 2).
Figure 2.
Hypothesized mediating effect of mindfulness on sleep quality and worry: (A) Mindfulness training (delivered by the Unwinding Anxiety application) decreases worry, as measured by the Penn State Worry Questionnaire, which, in turn, mediates the effect of the intervention on sleep quality. (B) Mindfulness training increases non-reactivity, as measured by the non-reactivity subscale of the Five Facet Mindfulness Questionnaire, which, in turn, mediates the effect of the intervention on worry.
The primary goal of this study is to test whether a mobile mindfulness training program for anxiety can help individuals decrease worry with concomitant improvements in sleep. We hypothesize that mindfulness training will increase nonreactivity, decrease worry, and improve sleep. The secondary goal is to explore our hypotheses that: 1) increases in mindfulness (FFMQ), will mediate the relationship between mobile mindfulness training and improvement in sleep quality 2) increases in mindfulness will mediate the relationship between reduction in worry and improvement in sleep.
Methods
Participants
Individuals who express an interest in using an app-based mindfulness training program to reduce worry and anxiety to improve their sleep will be recruited using Facebook advertisements, with the goal of enrolling 80 people. Participants will be eligible if they (1) have a score greater than 40 on the Penn State Worry Questionnaire, consistent with a moderate level of worry such as found in generalized anxiety disorder, (2) have a score of 40% or higher on the Worry Interfering with Sleep scale, demonstrating that worry interferes with their ability to sleep nearly half of the time, (3) own a smartphone, (4) endorse willingness to wear a sleep tracker and record sleep, and (5) are 18 years or older. Individuals will be excluded if they report (1) changing dose of any psychoactive medication in the previous 6 weeks, (2) as-needed use of benzodiazepines and/or hypnotic sleep aids, (3) a known sleep disorder, (4) a history of psychiatric conditions such as schizophrenia or bipolar disorder, (5) current post-traumatic stress disorder, (6) severe depression as determined by a score of 3 or higher on the Patient Health Questionnaire-2, (7) current shift employment that includes night shift work, (8) evening caffeine use, (9) a body mass index > 35 kg/m2 which makes undiagnosed obstructive sleep apnea more likely (10) pregnancy, (11) recently becoming new parents which is associated with inconsistent sleep patterns. Participants who use non-hypnotic and/or hypnotic sleep aids on a regular schedule will not be excluded from participating. Participants may be removed from the study at the discretion of the Principal Investigator.
Randomization
Eligible participants will receive a sequentially numbered, opaque, sealed envelope containing their random assignment: treatment as usual (TAU) or TAU + an app-based mindfulness training (TAU + MT). TAU was chosen as this is a pragmatic randomized controlled trial and it most closely mimics real-world conditions and what a patient would experience in a clinical setting had the intervention not been implemented (Löfholm, Brännström, Olsson, & Hansson, 2013; Staines, Mckendrick, Perlis, Sacks, & De Leon, 1999). Randomization will be on a 1:1 schedule in a parallel group design. Assignments will be generated by an independent statistician in random blocks of four and six to ensure approximately equal numbers of participants in the two study arms. The envelopes will be prepared, reviewed by two individuals independent of data acquisition, and will remain sealed before participants are enrolled and consented.
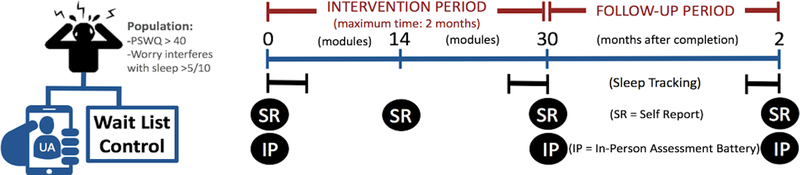
Participant Timeline
Eligible participants will attend an in-person visit at Brown University (Providence, RI) and the Project Coordinator will obtain informed consent. They will then complete an online questionnaire via Qualtrics Survey Tool (http://www.qualtrics.com) and a computer-based resistance to distraction task (Friedman & Miyake, 2004; Stahl et al., 2014). The Project Coordinator will help individuals assigned to the TAU + MT group install the app on their smartphones and provide brief instruction to ensure comprehension of its tools and features. Participants will then complete the first module of the program to demonstrate their ability to use the app and address any potential questions. They are instructed to use the app on a daily basis for 30 days. A follow-up online survey is sent to participants in the TAU group at 1 month and the TAU + MT group upon completion of module 14 or at 1 month (see Figure 3). Participants are asked to return to Brown University at either module 30 or 2 months (TAU + MT group) or 2 months (TAU group), where they will complete the same computer-based task and questionnaires completed at baseline. At this visit, the TAU group will be invited to download the app and an identical procedure to that done with the TAU + MT group will be followed to ensure comprehension. Both groups will be asked to return for a final assessment. The final assessment, where they will complete the same tasks as done previously, will be at either module 30 or 4-months post baseline (TAU group) and 4-months post baseline (TAU + MT group).
Figure 3.
Randomization and study flow overview. Self-report (SR) measures include the non-reactivity subscale from the Five Facet Mindfulness Questionnaire, Multidimensional Assessment of Interoceptive Awareness, Penn State Worry Questionnaire (PSWQ), Worry Interfering with Sleep Questionnaire, and the Patient-Reported Outcomes Measurement Information System sleep measures. In-person (IP) assessment includes the Shape Matching Task. UA = Unwinding Anxiety application.
Actigraphy
Fitbit Inspire devices will be used in addition to concomitant sleep diaries to track total sleep time. Fitbits will be initialized by a member of the study team in advance of the first patient visit to ensure the device is functional and the software up to date. The Project Coordinator will help the participant install the smartphone application and set-up the device. Participants will be instructed to wear the device at night on their non-dominant wrist for three, 7-day periods in addition to recording what time they go to sleep and wake up in a sleep diary. Data will be exported from the participant’s Fitbit dashboard and two independent members of the study team will review and score it. Total sleep time will be calculated by subtracting bedtime from rise time. In the event of incomplete or missing data, the sleep diaries will be used to provide additional clarity (Ancoli-Israel et al., 2015).
Retention Strategies
In order to improve participant retention, the Project Coordinator will emphasize the importance of follow-up and completion of study milestones. Additionally, participants will be compensated up to $100 in Amazon gift cards ($25 per assessment). They will also receive check-in calls on days 7, 14, and 45 from the time they initially download the app.
Study Blinding
Participants will be blinded to group assignment. The Principal Investigator, statistician, and Research Associate conducting data analysis will be blinded. The individual who is responsible for the randomization of participants and conducting the assessments will not be involved in data analysis. Each group will be labeled “Group 1” or “Group 2” to ensure that the principal investigator and members of the study team who conduct the statistical analyses are pseudo-blinded to group membership until all analyses are complete.
Monitoring
Prior to the enrollment of participants, approval will be obtained from Brown University’s Institutional Review Board (IRB) and any changes to the research protocol will be reviewed by the IRB before implementation. This study will be overseen by an independent Data Safety Monitor (DSM) who will receive regular reports regarding the status of the study. Adverse events and medication changes will be solicited at each participant’s final assessment for the study. Severe spontaneously reported adverse events will be reported immediately and all others will be recorded and reported quarterly. This study is not subject to audit by the NIH however internal quality assurance checks will be conducted monthly. All study data will be anonymized and stored on password protected servers while physical documents will be kept in locked filing cabinet.
Sample Size
To date there have not been previous studies of the intervention, therefore sample size calculations were informed by our previous work with MBSR for individuals with anxiety. This prior study found an increase of 3.5 points (SD = 4.85) in non-reactivity and a decrease of 2.6 points (SD = 3.6) in sleep disturbances based on the Pittsburgh Sleep Quality Index. A one sample t-test determined a sample size of 64 will have 80% and 83% power with two-sided type I error, to detect a statistically significant difference between groups in changes non-reactivity scores and sleep quality respectively. To account for 20% attrition, we plan to recruit 80 individuals.
Intervention
The app-based mindfulness training program (Unwinding Anxiety) aims to teach individuals (1) to learn how worry and anxiety develop and are perpetuated through reinforcement learning, (2) how to recognize “habit loops” related to anxiety, and (3) how to use mindfulness during times of stress and worry such that they can uncouple feelings of anxiety from reactive worry and productively work with habitual mind states that reinforce anxiety. This training is designed to help individuals extinguish worry at a basic mechanistic level. This experiential training is delivered through an app-based platform, which includes 30 core modules and 8 “theme weeks” (that reinforce core concepts) of brief didactic and experience-based mindfulness training (videos and animations, ~10 min/day; see Table 1), app-initiated check-ins, user-initiated guided meditations (5–15 min), and brief on-demand mindfulness exercises (30-sec) to help break worry cycles in the moment. The intervention content is based on a framework from previously developed in-person and app-based mindfulness trainings that share a core underlying mechanism (reinforcement learning) that have yielded clinically meaningful outcomes (e.g., cessation of smoking and overeating) (Brewer et al., 2011; Brewer, Ruf, Beccia, Essien, Finn, Lutterveld, et al., 2018; Brewer, Ruf, Beccia, Essien, Finn, van Lutterveld, et al., 2018; Garrison et al., 2018; A. E. Mason, Jhaveri, Cohn, & Brewer, 2018). Specific anxiety and worry-related content was developed from a combination of clinical experience with anxious individuals and several rounds of iterative pilot testing with the general public who self-described as anxious, after which the content and delivery of the modules and exercises were refined. Weekly telephone-based focus groups were used to gather feedback. After a Net Promoter Score (“How likely is it that you would recommend this to a friend or colleague?”) of 96 was achieved (70+ is rated as “world class”), videos, animations, and in-the-moment exercises were finalized and bundled into an app-based delivery platform that can be delivered via Android and iOS operating systems.
Table 1.
Overview of Unwinding Anxiety Themes and Content
| Modules 1–7: Goals; curiosity; reinforcement learning; body scan; self-monitoring |
| Sets goals and introduces how habits are formed around worry (e.g., reinforcement learning, distraction). Introduces curiosity to foster the nonjudgmental aspects of mindfulness and basic mindfulness practices including the body scan. Unpacks worry and fear both from a brain and behavior perspective. |
| Modules 8–14: Noting practice; RAIN; barriers to change; reinforce concepts |
| Introduces how to mindfully work with worry cues and affective states using RAIN (Recognize, Accept, Investigate and Note what emotions feel like as they arise and pass away). These also build on basic mindfulness using noting practice during everyday life, and introduce additional animations to reinforce mindfulness concepts that illustrate how we feed our anxiety by worry thinking and distraction. |
| Modules 15–21: Noting practice (cont’d); RAIN (cont’d); thinking vs. knowing; (un)resistance |
| Reinforces noting practice and continues to train and support self-kindness. Specifically addresses the difference between trying to think our way out of uncertainty (or anxiety), and resting in a kind, curious awareness of it. Modules also focus on not resisting experience, and not getting caught up in worry thinking. |
| Modules 22–30: Noting practice (cont’d); RAIN (cont’d); working with uncertainty and change |
| Helps individuals reflect on their own evidence base for working with worry to solidify their shift from reactivity to mindfully being with emotions as a new habit. |
| Modules 30+: Reinforcing concepts via theme weeks and individual customization via a personal week |
| Eight themed weeks and unlimited personalization of content by picking modules to develop a custom week for review. |
Measurements
Primary Outcomes
The primary clinical outcome is a change in the Patient-Reported Outcomes Measurement Information System (PROMIS) sleep quality items (Yu et al., 2012). The primary outcome is the nonreactivity subscale of the Five Facet Mindfulness questionnaire (Baer et al., 2008).
Secondary Outcomes
The secondary outcomes are changes in the Penn State Worry Questionnaire (PSWQ), Generalized Anxiety Disorder-7 Questionnaire (Spitzer, Kroenke, Williams, & Lowe, 2006), sleep actigraphy, Multidimensional Assessment of Interoceptive Awareness scale) (Mehling et al., 2012; Meyer, Miller, Metzger, & Borkovec, 1990), the Worry Interfering with Sleep scale, and the shape matching task, which assesses resistance to distraction (Friedman & Miyake, 2004).
Exploratory Outcomes
Theory-based potential mechanisms will be tested with a mediation analyses. The first will examine the relationship between the intervention, mindfulness (FFMQ), and effects on sleep, as measured by the PROMIS sleep quality items. The second will explore the relationship between changes in worry and sleep to see if it is mediated by mindfulness.
Expectancy Evaluation
Expectancy will be assessed at baseline using three questions. (1) At this point, how useful do you think the app will be in helping to reduce your worry to improve sleep? (2) How confident would you be in recommending this app to friends who want to reduce their worry? And (3) By the end of the study, how much improvement in worrying do you think will occur? The first two questions are assessed on a scale ranging from 1 (Not at all useful/Not at all confident) to 9 (Very useful/Very confident). The third question is measured from 0 to 100%. Post-treatment, participants are asked, “How likely are you to recommend the Unwinding Anxiety app to a friend?” and it is measured on a scale of 0 (Not at all) to 10 (Extremely likely).
Statistical Analysis
We will analyze both the intent-to-treat sample and the per-protocol sample (secondary). Changes from baseline to treatment completion for the primary and secondary outcomes will be assessed using a factorial repeated measures analysis of variance and using a random-effect generalized linear model estimated by the method of generalized estimating equations (Liang & Zeger, 1986). The TAU group will be evaluated at two, two-month time periods: baseline to assessment three (before receiving the intervention) and assessment three to four (after receiving the intervention). Using the random-effect model, we will also consider adjusting for covariates such as age, sex, and their interaction terms with the interventions, to quantify their main as well as their potential moderating effects. To overcome possible model overfitting, we will consider using the least absolute shrinkage and selection operator (LASSO) for the selection of important covariates in the model (Tibshirani, 1996). We will evaluate if changes in non-reactivity and/or worry mediate the direct effect of mindfulness on changes in sleep quality with mediation analyses at one and two-months post-baseline. These time points were chosen because they will allow for an evaluation of time ordered mediation and are prior to the TAU group receiving the intervention. We will consider the traditional Baron and Kenny approach in addition to robust mediation analyses (Baron & Kenny, 1986; Imai, Keele, Tingley, & Yamamoto, 2010). For the latter, we will utilize the ROBMED package in R which follows the same principles found in the Preacher & Hayes test (Preacher & Hayes, 2008) but employs a robust MM-regression estimator (Yohai, 1987) and a fast and robust bootstrap (Salibian-Barrera & Van Aelst, 2008) to compensate for deviations from model assumptions, for example, outliers (Alfons, Ates, & Groenen, 2018). Qualitative analysis will be carried out to evaluate expectancy, supplemented with basic summary statistics such as means with standard deviations or median with interquartile range. Interim statistical analyses will not be conducted.
Open Science approach
We will preregister the study on ClinicalTrials.gov. This was chosen in place of Open Science Framework (OSF) because the National Institute of Health requires its use per a 2016 policy update (Toelch & Ostwald, 2018). Raw data and analyses code will not be uploaded to data and/or code repositories but will be available to qualified researchers affiliated with other institutions by request. Additionally, results and study documents will be published on ClinicalTrials.gov and the manuscript submitted to a journal for publication.
Discussion
This study is one of the first to test the mechanistic effects of app-based mindfulness training for anxiety on worry and sleep disturbance. Although many meditation-related apps are available, very few have been tested with regard to clinical efficacy, fewer have been designed based on hypothesized theory to specifically target purported mechanisms related to the development and perpetuation of anxiety and worry, and even fewer have taken into account potential mediation effects that can link treatment to target to outcome.
Cognitive approaches to treat anxiety can be difficult to deliver at a population level due to the limited availability of highly trained individuals, time requirements of therapy, and associated costs; therefore, mindfulness-based approaches, which are delivered in a group format, may address some of these challenges. However, concerns remain around scalability and competency of in-person delivered MBI treatments (Crane et al., 2012). We aim to address this gap, by testing the effect of a specialized app-based mindfulness training. In addition, examining the mechanistic effects of app-delivered mindfulness training using the SOBC framework will move the field forward both in further elucidation of potential novel mechanisms of mindfulness (e.g., targeting reinforcement learning), and by determining whether such a platform is a viable method for delivering high-fidelity treatment at scale and low cost. This study will also further illuminate links between worry and sleep disturbance, which may reveal new avenues for treatment development.
Supplementary Material
Acknowledgments
This study was supported by the National Institutes of Health (NIH) Science of Behavior Change Common Fund Program through an award administered by the National Institute on Aging (R21DA046957).
Footnotes
Conflict of Interest Statement
Dr. Brewer is the founder of MindSciences, the company that developed the mindfulness app used in this study. He owns stock in, serves as a non-compensated scientist for the company and has previously served on the board of directors. This financial interest has been disclosed to, and is being managed by, Brown University, in accordance with its Conflict of Interest and Conflict of Commitment policies. All other authors report no biomedical financial interests or potential conflicts of interest.
References
- Alfons A, Ates N, & Groenen PJ (2018). A Robust Bootstrap Test for Mediation Analysis.
- Ancoli-Israel S, Martin JL, Blackwell T, Buenaver L, Liu L, Meltzer LJ, . . . Taylor DJ (2015). The SBSM guide to actigraphy monitoring: clinical and research applications. Behavioral sleep medicine, 13(sup1), S4–S38. [DOI] [PubMed] [Google Scholar]
- Arnsten AF (2009). Stress signalling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci, 10(6), 410–422. doi:nrn2648 [pii] 10.1038/nrn2648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnsten AF (2015). Stress weakens prefrontal networks: molecular insults to higher cognition. Nature Neuroscience, 18(10), 1376–1385. doi: 10.1038/nn.4087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association AP (2013). Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, . . . Williams JMG (2008). Construct Validity of the Five Facet Mindfulness Questionnaire in Meditating and Nonmeditating Samples. Assessment, 15(3), 329–342. doi: 10.1177/1073191107313003 [DOI] [PubMed] [Google Scholar]
- Bagley EJ, Kelly RJ, Buckhalt JA, & El-Sheikh M (2015). What keeps low-SES children from sleeping well: the role of presleep worries and sleep environment. Sleep Med, 16(4), 496–502. doi: 10.1016/j.sleep.2014.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- Beck A, Emery G, & Greenberg R (1985). Anxiety disorders and phobias: A cognitive approach. Basic, New York. [Google Scholar]
- Borkovec T, Ray WJ, & Stober J (1998). Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Cognitive Therapy and Research, 22(6), 561–576. [Google Scholar]
- Borkovec TD, Robinson E, Pruzinsky T, & DePree JA (1983). Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy, 21(1), 9–16. [DOI] [PubMed] [Google Scholar]
- Brewer JA (2019). Mindfulness training for addictions: has neuroscience revealed a brain hack by which awareness subverts the addictive process? Curr Opin Psychol, 28, 198–203. doi: 10.1016/j.copsyc.2019.01.014 [DOI] [PubMed] [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, . . . Rounsaville BJ (2011). Mindfulness training for smoking cessation: Results from a randomized controlled trial. Drug and Alcohol Dependence, 119(1–2), 72–80. doi: 10.1016/j.drugalcdep.2011.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, & Pbert L (2015). Mindfulness: An Emerging Treatment for Smoking and other Addictions? Journal of Family Medicine, 2(4). [Google Scholar]
- Brewer JA, Ruf A, Beccia AL, Essien GI, Finn LM, Lutterveld R. v., & Mason AE (2018). Can Mindfulness Address Maladaptive Eating Behaviors? Why Traditional Diet Plans Fail and How New Mechanistic Insights May Lead to Novel Interventions. Frontiers in Psychology, 9(1418). doi: 10.3389/fpsyg.2018.01418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Ruf A, Beccia AL, Essien GI, Finn LM, van Lutterveld R, & Mason AE (2018). Can Mindfulness Address Maladaptive Eating Behaviors? Why Traditional Diet Plans Fail and How New Mechanistic Insights May Lead to Novel Interventions. Frontiers in Psychology, 9, 1418–1418. doi: 10.3389/fpsyg.2018.01418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosschot JF, Gerin W, & Thayer JF (2006). The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research, 60(2), 113–124. [DOI] [PubMed] [Google Scholar]
- Casse-Perrot C, Lanteaume L, Deguil J, Bordet R, Auffret A, Otten L, . . . Micallef J (2016). Neurobehavioral and Cognitive Changes Induced by Sleep Deprivation in Healthy Volunteers. CNS Neurol Disord Drug Targets, 15(7), 777–801. [DOI] [PubMed] [Google Scholar]
- Crane RS, Kuyken W, Williams JMG, Hastings RP, Cooper L, & Fennell MJV (2012). Competence in Teaching Mindfulness-Based Courses: Concepts, Development and Assessment. Mindfulness, 3(1), 76–84. doi: 10.1007/s12671-011-0073-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czajkowski SM, Powell LH, Adler N, Naar-King S, Reynolds KD, Hunter CM, . . . Peterson JC (2015). From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychology, 34(10), 971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg I, Poldrack R, Bissett P, Enkavi AZ, Kim SJ, King JW, . . . Derby L (2017). SOBC (Marsch/Poldrack) Applying Novel Technologies and Methods to Inform the Ontology of Self-Regulation. Retrieved from https://osf.io/amxpv/ [DOI] [PMC free article] [PubMed]
- Elwafi HM, Witkiewitz K, Mallik S, Thornhill-IV TA, & Brewer JA (2013). Mindfulness training for smoking cessation: Moderation of the relationship between craving and cigarette use. Drug and Alcohol Dependence, 2013(1–3), 222–229. doi: 10.1016/j.drugalcdep.2012.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman NP, & Miyake A (2004). The relations among inhibition and interference control functions: a latent-variable analysis. Journal of Experimental Psychology: General, 133(1), 101. [DOI] [PubMed] [Google Scholar]
- Garbarino S, Lanteri P, Durando P, Magnavita N, & Sannita WG (2016). Co-Morbidity, Mortality, Quality of Life and the Healthcare/Welfare/Social Costs of Disordered Sleep: A Rapid Review. Int J Environ Res Public Health, 13(8). doi: 10.3390/ijerph13080831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrison KA, Pal P, O'Malley SS, Pittman BP, Gueorguieva R, & Brewer JA (2018). Craving to Quit: A randomized controlled trial of smartphone app-based mindfulness training for smoking cessation. Nicotine & Tobacco Research. [DOI] [PMC free article] [PubMed]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, . . . Shihab HM (2014). Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Internal Medicine, 174(3), 357–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross RT, & Borkovec T (1982). Effects of a cognitive intrusion manipulation on the sleep-onset latency of good sleepers. Behavior Therapy, 13(1), 112–116. [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, & Oh D (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. doi: 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai K, Keele L, Tingley D, & Yamamoto T (2010). Causal mediation analysis using R. In Advances in social science research using R (pp. 129–154): Springer. [Google Scholar]
- Kabat-Zinn J (1990). Full Catastropher Living: Using the Wisdom of Your Body and Mind to Face Stress. Pain and Illness, Delacorte, NY. [Google Scholar]
- Liang K-Y, & Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73(1), 13–22. [Google Scholar]
- Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, & Croft JB (2016). Prevalence of Healthy Sleep Duration among Adults--United States, 2014. MMWR. Morbidity and Mortality Weekly Report, 65(6), 137–141. doi: 10.15585/mmwr.mm6506a1 [DOI] [PubMed] [Google Scholar]
- Löfholm CA, Brännström L, Olsson M, & Hansson K (2013). Treatment-as-usual in effectiveness studies: What is it and does it matter? International journal of social Welfare, 22(1), 25–34. [Google Scholar]
- Mason AE, Jhaveri K, Cohn M, & Brewer JA (2017). Testing a mobile mindful eating intervention targeting craving-related eating: feasibility and proof of concept. Journal of Behavioral Medicine. doi: 10.1007/s10865-017-9884-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason AE, Jhaveri K, Cohn M, & Brewer JA (2018). Testing a mobile mindful eating intervention targeting craving-related eating: feasibility and proof of concept. Journal of Behavioral Medicine, 41(2), 160–173. doi: 10.1007/s10865-017-9884-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan SK, Behar E, & Luhmann M (2016). Examining the Relationship Between Worry and Sleep: A Daily Process Approach. Behav Ther, 47(4), 460–473. doi: 10.1016/j.beth.2015.12.003 [DOI] [PubMed] [Google Scholar]
- Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, & Stewart A (2012). The multidimensional assessment of interoceptive awareness (MAIA). PLoS ONE, 7(11), e48230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy, 28(6), 487–495. [DOI] [PubMed] [Google Scholar]
- Ong JC, Shapiro SL, & Manber R (2008). Combining mindfulness meditation with cognitive-behavior therapy for insomnia: a treatment-development study. Behavior Therapy, 39(2), 171–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong JC, Ulmer CS, & Manber R (2012). Improving sleep with mindfulness and acceptance: a metacognitive model of insomnia. Behaviour Research and Therapy, 50(11), 651–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Riddle M, & Group S. o. B. C. W. (2015). News from the NIH: using an experimental medicine approach to facilitate translational research. In: Oxford University Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Salters K, Raffa SD, & Orsillo SM (2005). Fear and avoidance of internal experiences in GAD: Preliminary tests of a conceptual model. Cognitive Therapy and Research, 29(1), 71–88. [Google Scholar]
- Salibian-Barrera M, & Van Aelst S (2008). Robust model selection using fast and robust bootstrap. Computational Statistics & Data Analysis, 52(12), 5121–5135. [Google Scholar]
- Salters-Pedneault K, Tull MT, & Roemer L (2004). The role of avoidance of emotional material in the anxiety disorders. Applied and Preventive Psychology, 11(2), 95–114. [Google Scholar]
- Sibrava NJ, & Borkovec TD (2008). The Cognitive Avoidance Theory of Worry. In Worry and its Psychological Disorders (pp. 239–256): John Wiley & Sons Ltd. [Google Scholar]
- Simon GE, & VonKorff M (1997). Prevalence, burden, and treatment of insomnia in primary care. American Journal of Psychiatry, 154(10), 1417–1423. doi: 10.1176/ajp.154.10.1417 [DOI] [PubMed] [Google Scholar]
- Skinner BF (1953). Science and human behavior: Free Press. [Google Scholar]
- Skinner BF (1963). Operant behavior. American Psychologist, 18(8), 503–515. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Lowe B (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Stahl C, Voss A, Schmitz F, Nuszbaum M, Tüscher O, Lieb K, & Klauer KC (2014). Behavioral components of impulsivity. Journal of Experimental Psychology: General, 143(2), 850. [DOI] [PubMed] [Google Scholar]
- Staines GL, Mckendrick K, Perlis T, Sacks S, & De Leon G (1999). Sequential assignment and treatment-as-usual: Alternatives to standard experimental designs in field studies of treatment efficacy. Evaluation Review, 23(1), 47–76. [DOI] [PubMed] [Google Scholar]
- Suhler CL, & Churchland PS (2009). Control: conscious and otherwise. Trends in Cognitive Sciences, 13(8), 341–347. doi: 10.1016/j.tics.2009.04.010 [DOI] [PubMed] [Google Scholar]
- Thorndike EL (1898). Animal intelligence: An experimental study of the associative processes in animals. Psychological Monographs: General and Applied, 2(4), 1–8. [Google Scholar]
- Tibshirani R (1996). Regression shrinkage and selection via the lasso. Journal of the Royal Statistical Society: Series B (Methodological), 58(1), 267–288. [Google Scholar]
- Toelch U, & Ostwald D (2018). Digital open science—Teaching digital tools for reproducible and transparent research. PLoS biology, 16(7), e2006022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, & Cunnington D (2015). Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Annals of Internal Medicine, 163(3), 191–204. [DOI] [PubMed] [Google Scholar]
- Weise S, Ong J, Tesler NA, Kim S, & Roth WT (2013). Worried sleep: 24-h monitoring in high and low worriers. Biological Psychology, 94(1), 61–70. doi: 10.1016/j.biopsycho.2013.04.009 [DOI] [PubMed] [Google Scholar]
- Yan Y, Lin R, Tang X, He F, Cai W, & Su Y (2014). The relationship between worry tendency and sleep quality in Chinese adolescents and young adults: the mediating role of state-trait anxiety. J Health Psychol, 19(6), 778–788. doi: 10.1177/1359105313479628 [DOI] [PubMed] [Google Scholar]
- Yohai VJ (1987). High breakdown-point and high efficiency robust estimates for regression. The Annals of Statistics, 15(2), 642–656. [Google Scholar]
- Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, . . . Pilkonis PA (2012). Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behavioral sleep medicine, 10(1), 6–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.