Abstract
Purpose:
Alongside the SARS-CoV-2 virus, the COVID-19 pandemic is associated with several secondary health effects. There is concern for increased substance use motivated by coping with stress, anxiety, depression, and boredom – all of which may be elevated during the pandemic. The current study examined intraindividual changes (from pre-COVID to during COVID) in young adults’ alcohol and marijuana use, perceptions of peers’ use (i.e., norms), and motives for use.
Methods:
A community sample of young adults (N=572; Mage=25.14; 60.8% women) was recruited in Washington State. Using a repeated-measures design, data were collected prior to the COVID-19 pandemic (January 2020) and again during the initial acute phase of the pandemic (April/May of 2020).
Results:
Young adults, on average, increased alcohol use frequency but decreased the amount consumed per drinking occasion. No changes in marijuana use were identified. Young adults (on average) perceived that peers had increased the frequency and total amount of alcohol use, and perceived that peers were engaging in heavier marijuana use than prior to COVID-19. For alcohol use motives, there was a significant increase in depression coping motives and significant decreases in social, enhancement, and conformity motives. Boredom motives for marijuana use significantly increased, while celebration motives decreased.
Conclusions:
Using a prospective design with a sample initially recruited in Washington State, these data indicate that (a) young adults’ patterns of alcohol use may have changed, (b) young adults tend to think that peers are engaging in heavier alcohol/marijuana use than before the pandemic, and (c) motives for using alcohol/marijuana may have changed during the pandemic.
Keywords: Substance Use, Drinking, Cannabis, SARS-CoV-2, Social Norms, Social Distancing
The COVID-19 pandemic may have myriad negative consequences to health and well-being that extend beyond the illness caused by the SARS-Cov-2 virus. Although “stay-at-home/shelter-in-place” orders and other physical distancing measures are critical for reducing the spread of COVID-19,1,2 studies indicate that many people are experiencing elevated levels of loneliness, stressors, anxiety, and depression during the course of the pandemic.3–7 Alongside psychological distress, there is emerging evidence that people may be coping in maladaptive ways, such as increasing their alcohol use.8 Thus, researchers face an urgent need to examine and understand pandemic-related changes in health-risk behaviors to inform immediate action and to enhance preparedness for future global crises.9
Early-stage evidence suggests that many Americans may be engaging in increased alcohol use during the COVID-19 pandemic.10 For example, hard alcohol sales in March of 2020 were 75% higher than March of 2019, while beer sales were up by 66% and wine sales were up by 42%.11 Although increased in-store sales may be offset by decreased drinking at bars and restaurants, these trends have prompted a call to action for research examining changes in alcohol and other substance use.12 Much of the focus has been on alcohol use, but there are also reports that marijuana use (or at least sales) may be increased during the pandemic.13 Little research has tied marijuana use to societal upheavals such as the pandemic, but increases in marijuana use were reported following Hurricane Katrina14 and among Manhattan residents following the tragic September 11th terrorists attacks.15
Prevalence of alcohol and marijuana use is particularly high for young adults,16,17 but the extent that use patterns among this population have changed during the COVID-19 pandemic is unclear. One recent study found that fewer Canadian adolescents (Mage=16.68 years) were using alcohol and marijuana, but those who were using these substances did so more frequently than before the pandemic.18 In another study of U.S. college students, only 10% self-reported that they had increased their alcohol use frequency compared to before the pandemic, while nearly half reported decreasing their alcohol use.19 This study also found that changes in alcohol use behaviors were associated with perceptions that peers’ alcohol use behaviors have changed (i.e., social norms). Given that young adults’ decisions to engage in health-risk behaviors are influenced by perceived social norms,20,21 it is important to examine how young adults’ perceptions of peers’ use have changed during the pandemic, and whether young adults hold overinflated misperceptions of peers’ alcohol and marijuana use. Such evidence would inform timely COVID-19-specific norms-based interventions such as personalized normative feedback that can reduce substance use by correcting normative misperceptions.22
It is also important to study changes in motives, or the reasons for engaging in substance use. Notably, young adults may have increased motives to engage in alcohol and marijuana use to relieve feelings of distress or boredom (i.e., self-medication hypothesis).23 Young adults often engage in substance use for social reasons such as wanting to fit-in,24 or as a form of celebration,25 and such motives may decrease during the pandemic due to social distancing. Understanding changes in young adults’ motives for substance use will help inform prevention efforts, many of which rely on motivational interviewing techniques that target salient motivations as leverage points for encouraging individuals to reduce or avoid substance use.26
Current Study
In response to the call-to-action for investigating changes in substance use behaviors during the COVID-19 pandemic,12 the current study aimed to estimate intraindividual changes in alcohol and marijuana use, norms, and motives. Intraindividual changes were estimated using a repeated-measures design, in which data were collected prior to COVID-19 (January 2020) and again during the initial phase of the pandemic and following the implementation of major physical/social distancing restrictions (April/May of 2020). We also explored whether changes in use, norms, and motives differed by theoretically important demographic characteristics. Specifically, we examined differences by (a) birth sex, as women may be more susceptible to pandemic-related distress and psychological consequences;3 (b) age and (c) college student status, as substance use is higher among younger adults and college students27 but there may be steeper decreases in use among these groups;28 and (d) race/ethnicity as there have been well-documented racial and ethnic disparities in pandemic-related health outcomes.29,30
Method
Procedure and sample
The participants for the present analyses were drawn from a longitudinal study on substance use and social role transitions among young adults.31 Between February 2015 and January 2016, the original project enrolled 778 young adults (Mage=20.6; 56.3% female) in the community to participate in ongoing monthly surveys (participants were enrolled on a rolling basis). Initial inclusion criteria entailed being between the ages of 18–23 at screening, drinking at least one alcoholic beverage in the past year, and living within 60 miles of the study office in Seattle, WA. In the original study, data were collected at baseline, monthly for 2 years, and at 30-month follow-up. To continue tracking these young adults as a secondary project unrelated to the COVID-19 pandemic, we invited the sample to complete a follow-up survey in January 2020. Then, to examine young adults’ health and well-being during the pandemic, we invited this sample to complete a survey in April/May 2020. The current study thus utilized data collected through an online survey platform in January (pre-COVID) and April/May of 2020 (during-COVID). A total of 572 young adults (Mage=25.14, SDage=1.84; 60.8% women) out of 767 invited from the original parent study completed at least one of the two surveys and comprises the analytic sample for the current study (n=560 in January; n=508 in April/May; n=459 completed both). Note that participants were originally recruited in Washington State, where recreational marijuana use is legalized, though 29.6% reported currently residing in a different state. Pertaining to race/ethnicity, 50.6% of the sample identified as White/Caucasian, 17.5% as Asian/Asian American, 23.8% as Other/Non-Hispanic1, and 8.2% identified as Hispanic. Pertaining to education, 72.1% had completed at least a bachelor’s level degree, and 16.3% were currently enrolled in two- or four-year college. The race/ethnicity of the sample approximately matches census data from the counties in Washington State from which participants were recruited. Participation was incentivized by a $15 gift card at each of the two timepoints. All procedures received Institutional Review Board approval and participants received information statements outlining study procedures and all elements of informed consent.
Measures
Instruments assessing substance use behaviors, norms, and motives were employed at both the pre-COVID and during-COVID timepoints. Alcohol use behaviors were assessed using the Daily Drinking Questionnaire (DDQ), in which participants reported the typical number of drinks they consumed on each day of the week in the past month.32 From this instrument, we calculated four discrete indices: (a) total number of drinks per week, (b) number of drinking days per week, (c) average number of drinks consumed during a drinking occasion, and (d) number of heavy episodic drinking occasions during a typical week (i.e., 4+ drinks for women/5+ drinks for men). Perceived same-sex drinking norms for these same indices of alcohol use were derived from the descriptive norms rating form (DNRF).33 The DNRF mirrors the DDQ, but instead asked participants to estimate how many drinks they thought same-sex and same-age peers typically consumed on each day of the week in the last month. Potentially spurious outliers were Winsorized for DDQ and DNRF at three standard deviations above the mean to reduce their influence on model estimates.34
Two indices of marijuana use—total hours high per week and number of days high per week—were calculated using the Daily Marijuana Questionnaire (DMQ)35 in which participants reported how many hours they were high on each day of a typical week in the past month. Perceived norms for peers’ marijuana use were assessed using a scale that mirrored the DMQ, which asked participants to estimate how many hours a typical person their age was high on each day of a typical week in the past month. Note that these norms are not gender-specific.
Among those participants who drank alcohol in the prior month, alcohol use motives were assessed using the 28-item Modified Drinking Motives Questionnaire,24 which comprises five subscales: anxiety coping motives, depression coping motives, social motives, enhancement motives, and conformity motives. On a five-point scale ranging from 1 = Almost never/Never to 5 = Almost always/Always, participants reported how often they drank for a variety of reasons (e.g., “to forget my worries” from the anxiety coping motives subscale). Internal consistency (α) of these subscales ranged from .71 to .94. Using similar stem wording and scoring, marijuana use motives among past-month marijuana users were assessed using the Marijuana Motives Questionnaire25 entailing the following subscales: enjoyment, conformity, coping, experimentation, boredom, alcohol-related, celebration, altered perceptions, perceived low-risk, sleep, and availability. The social anxiety subscale of this measure was not included. Internal consistency (α) was acceptable, ranging from .72 to .90, with the exception of conformity motives (α = .56 at time two) that should thus be interpreted cautiously.
Analytic Strategy
Sample mean values for all study variables were calculated at both pre- and during-COVID timepoints for participants completing both surveys. Examining within-person changes from pre- to during-COVID timepoints, we then calculated the percent of participants that decreased, increased, or were unchanged. To further estimate the extent that young adults’ alcohol and marijuana use behaviors, norms, and motives changed from pre- to during-COVID, we fit mixed effects models in which timepoint was entered as a covariate (pre-COVID = 0, during-COVID = 1). To account for third variables that are typically associated with substance use, we statistically controlled for birth sex, age, race/ethnicity, and college student status. Using maximum likelihood estimation, this approach uses all available data to estimate effects, including responses from participants who only completed one of the two surveys. Preliminary checks nevertheless indicated that data can be assumed to be missing at random given that missingness was not significantly associated with age (r = −.04, p=.397), sex (χ2 = 1.72, p=.189), weekly drinks (r = −.01, p=.765), or weekly hours high (r = −.02, p=.719).
To assess whether changes in behaviors, norms, and motives were moderated by sex, age, college status, and race/ethnicity, we tested interactions in separate models. To better understand these interactions, model-predicted estimates were plotted for statistically significant interactions. Models estimating changes in substance use motives estimated unstandardized beta coefficients (b) as these variables were measured on a continuous scale. Models estimating changes in use and perceived norms (i.e., count variables) were specified using a negative binomial distribution to estimate count ratios (CR). Mixed effect models with maximum likelihood estimation were conducted in R using the “nlme”36 and “glmmTMB”37 packages. Given the increased risk for type-1 error when conducting multiple tests, significance was determined following Benjamini-Hochberg adjustment of p-values calculated within each set of outcomes (e.g., alcohol use behaviors).38
Results
In a preliminary step, we explored whether participants who voluntarily participated in this supplemental follow-up study (n=572) differed systematically from those who did not respond (n=206). Examining data from the final wave of the original parent study, we found that women were more likely to participate in the supplemental study than men (χ2=14.12, p <.001), but there were no differences between respondents and non-respondents in age (t=1.35, p=.13), past month alcohol use (t=0.24, p=.35), or past month marijuana use (t=−1.15, p=.09). We also explored whether marijuana use differed between Washington State residents and non-residents, given the legality of recreational marijuana use in Washington State. Neither weekly hours high nor number of marijuana use days per week differed at either the pre-COVID or during-COVID timepoints: All t-values ≤0.78; all p-values ≥0.43.
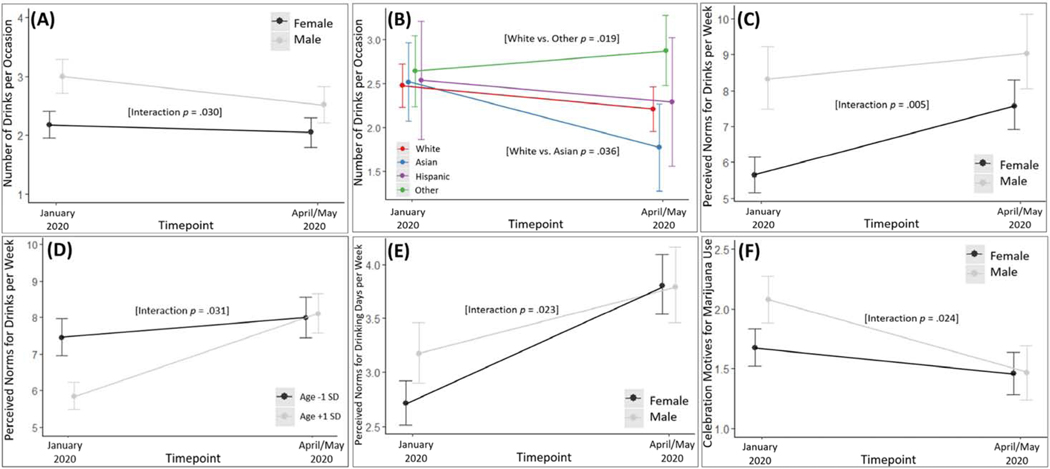
Changes in Self-Reported Alcohol and Marijuana Use
Means for alcohol and marijuana use and perceived norms at both timepoints are displayed in Table 1. On average, number of weekly drinks did not change significantly from pre- to during-COVID, with roughly equal percentages of participants reporting decreases, no change, and increases. There was a significant increase in the number of drinking days per week (+12%), but a significant decrease in the number of drinks consumed per occasion. There was a steeper decrease in number of drinks per occasion for men, relative to women (interaction p=.030; Figure 1A). There was also a steeper decrease in drinks per occasion for Asian/Asian American participants relative to White/Caucasian participants (interaction p=.036; Figure 1B), while drinks per occasion increased for participants grouped into the ‘Other’ race/ethnicity category (interaction compared to White/Caucasian p=.019; Figure 1B). Pertaining to changes in marijuana use, there were no significant changes in hours high per week or number of marijuana use days. Most young adults remained unchanged on these indices of marijuana use, but there was some heterogeneity. Over 20% of young adults increased in number of hours high per week, while 14.5% decreased. However, no significant interactions for changes in marijuana use were identified.
Table 1.
Pre- and during-COVID means for alcohol and marijuana use behaviors and perceived norms with regression models estimating change over time (N = 572).
| Variable | Pre-COVID Mean (SD) | During-COVID Mean (SD) | Effect of Time (CR) | p | BH adjusted p | 95% Confidence Interval | % that Decreased | % that was Unchanged | % that Increased |
|---|---|---|---|---|---|---|---|---|---|
| Participant Alcohol Use Behavior | |||||||||
| Typical # of Drinks in a Week1 | 4.67 (5.67) | 4.66 (6.74) | 0.92 | .108 | .144 | [0.83, 1.02] | 35.84% | 31.05% | 33.11% |
| Typical # of Drinking Days per Week | 1.83 (1.77) | 2.04 (2.20) | 1.12 | .014 | .028 | [1.02, 1.23] | 26.71% | 41.32% | 31.96% |
| Typical # of Drinks per Occasion on Average2 | 2.56 (1.88) | 2.28 (1.84) | 0.85 | .007 | .028 | [0.75, 0.96] | 46.84% | 24.54% | 28.62% |
| Typical HED Occasions per Week | 0.46 (1.09) | 0.40 (1.22) | 0.88 | .243 | .243 | [0.71, 1.09] | 14.39% | 78.53% | 7.08% |
| Perceived Alcohol Use Norms for | |||||||||
| Typical # of Drinks in a Week1 | 7.70 (5.81) | 9.14 (6.32) | 1.23 | <.001 | <.001 | [1.14, 1.33] | 34.17% | 13.76% | 52.06% |
| Typical # of Drinking Days per Week | 3.13 (2.05) | 4.04 (2.23) | 1.32 | <.001 | <.001 | [1.23, 1.41] | 21.10% | 32.57% | 46.33% |
| Typical # of Drinks per Occasion on Average | 2.59 (1.53) | 2.46 (1.38) | 0.91 | .063 | .084 | [0.83, 1.01] | 46.46% | 15.49% | 38.06% |
| Typical HED Occasions per Week | 0.67 (1.01) | 0.65 (1.20) | 0.99 | .859 | .859 | [0.84, 1.16] | 19.04% | 65.14% | 15.83% |
| Participant Marijuana Use Behavior | |||||||||
| Typical Hours High per Week | 4.98 (11.70) | 5.75 (13.40) | 1.13 | .177 | .177 | [0.95, 1.36] | 14.45% | 64.69% | 20.85% |
| Typical # of Marijuana Use Days per Week | 1.34 (2.41) | 1.46 (2.58) | 1.08 | .167 | . 177 | [0.97, 1.21] | 9.00% | 76.07% | 14.93% |
| Perceived Marijuana Use Norms | |||||||||
| Typical Hours High per Week | 6.91 (8.59) | 8.47 (9.14) | 1.30 | <.001 | <.001 | [1.19, 1.43] | 30.35% | 19.53% | 50.12% |
| Typical # of Marijuana Use Days per Week | 2.68 (2.35) | 3.31 (2.44) | 1.23 | <.001 | <.001 | [1.14, 1.32] | 20.71% | 37.41% | 41.88% |
Note: For count variables, a negative binomial distribution was specified to estimate Count Ratios (CRs) describing the proportional change from Time 1 (pre-COVID) to Time 2 (during-COVID). Because drinks per occasion variables only included non-zero values, truncated negative binomial models were specified. Covariates (not shown) included sex, age at Time 1, dummy codes for race/ethnicity, and college student status.
Typical number of weekly drinks and perceived norms for typical number of weekly drinks were Winsorized at 3 SD above the mean to reduce the influence of extreme values, though we ran these models with the raw un-Winsorized scores and the effect estimates and 95% confidence intervals were identical.
Participants who did not report any drinking (n = 111) were not included in models for number of drinks per occasion. BH = Benjamini-Hochberg adjustment for multiple comparisons. Significant effects are shown in bold.
Figure 1.
Significant interaction effects by sex, age, and race/ethnicity with simple-slopes and 95% confidence intervals.
Changes in Perceived Norms
Although young adults, on average, did not increase the number of total drinks consumed in a typical week, there was a large increase in perceived norms regarding peers’ weekly number of drinks (+23%), with over half of young adults reporting increased perceptions of how much they think others drink (Table 1). Women reported a steeper increase in perceptions of peers’ drinks per week relative to men (interaction p=.005; Figure 1C), as did younger participants relative to older (interaction p=.023; Figure 1D). Young adults also perceived a significant increase in peers’ number of drinking days per week (+32%), which aligns with the self-reported behaviors of young adults in our sample. Women perceived a steeper increase in perceived norms for drinking days per week, relative to men (interaction p=.023; Figure 1E).
In contrast to the finding that young adults in our sample had not, on average, significantly increased marijuana use, participants perceived an increase in peers’ marijuana use both in terms of hours high per week (+30%) and the number of marijuana use days per week (+23%). Indeed, over half of young adults reported increased perceptions of peers’ marijuana use during the COVID-19 pandemic relative to their perceptions reported prior to the pandemic. No interaction effects were identified for changes in marijuana use norms.
Changes in Alcohol and Marijuana Use Motives
Recall that alcohol and marijuana use motives were only assessed among those who reported using these respective substances (see Table 2). Compared to pre-COVID levels of drinking motives, anxiety coping motives did not change significantly among the sample as a whole, but there was substantial heterogeneity (44.62% decreased; 37.97% increased). There was a significant increase in depression coping motives (d=.16). On the other hand, there was a large decline in social motives from pre- to during-pandemic (d=−.99). Consistent with this, 86.6% of young adult drinkers reported decreased social motives. We also observed decreases in enhancement and conformity motives, but to a lesser degree (ds=−.14, −.13, respectively).
Table 2.
Pre- and during-COVID means for alcohol and marijuana use motives with regression models estimating change over time.
| Variable | Pre-COVID Mean (SD) | During-COVID Mean (SD) | Effect of Time (b) | p | BH adjusted p | 95% Confidence Interval | % that Decreased | % that was Unchanged | % that Increased |
|---|---|---|---|---|---|---|---|---|---|
| Alcohol Use Motives (n = 505) | |||||||||
| Anxiety Coping Motives | 2.08 (0.85) | 1.99 (0.79) | −0.06 | .163 | .163 | [−0.15, 0.02] | 44.62% | 17.41% | 37.97% |
| Depression Coping Motives | 1.38 (0.68) | 1.48 (0.76) | 0.11 | .001 | .002 | [0.04, 0.18] | 24.45% | 37.30% | 38.24% |
| Social Motives | 2.76 (0.95) | 1.77 (0.82) | −0.97 | <.001 | <.001 | [−1.07, −0.87] | 86.60% | 4.42% | 9.78% |
| Enhancement Motives | 2.66 (0.99) | 2.42 (1.08) | −0.21 | <.001 | <.001 | [−0.30, −0.11] | 56.47% | 11.04% | 32.49% |
| Conformity Motives | 1.22 (0.49) | 1.15 (0.46) | −0.08 | .003 | .004 | [−0.13, −0.03] | 22.88% | 68.65% | 8.46% |
| Marijuana Use Motives (n = 265) | |||||||||
| Enjoyment Motives | 3.60 (1.23) | 3.62 (1.18) | 0.05 | .578 | .795 | [−0.13, 0.23] | 42.44% | 25.18% | 32.37% |
| Conformity Motives | 1.10 (0.31) | 1.08 (0.32) | −0.03 | .325 | .715 | [−0.08, 0.02] | 10.79% | 79.14% | 10.07% |
| Coping Motives | 1.57 (0.92) | 1.56 (0.82) | 0.02 | .801 | .801 | [−0.11, 0.14] | 22.96% | 51.11% | 25.93% |
| Experimentation Motives | 1.20 (0.55) | 1.17 (0.52) | −0.05 | .238 | .655 | [−0.14, 0.03] | 13.87% | 76.64% | 9.49% |
| Boredom Motives | 2.07 (1.10) | 2.42 (1.18) | 0.36 | <.001 | <.001 | [0.19, 0.54] | 27.14% | 26.43% | 46.43% |
| Alcohol-Related Motives | 1.28 (0.68) | 1.18 (0.41) | −0.10 | .033 | .121 | [−0.20, −0.01] | 15.01% | 74.82% | 10.07% |
| Celebration Motives | 1.81 (1.00) | 1.46 (0.73) | −0.38 | <.001 | <.001 | [−0.54, −0.21] | 44.20% | 31.88% | 23.91% |
| Altered Perceptions Motives | 2.24 (1.35) | 2.24 (1.26) | 0.02 | .790 | .801 | [−0.16, 0.20] | 29.50% | 34.53% | 35.97% |
| Perceived Low Risk Motives | 2.07 (1.27) | 2.02 (1.19) | −0.03 | .710 | .801 | [−0.18, 0.12] | 27.14% | 45.00% | 27.86% |
| Sleep Motives | 1.87 (1.13) | 1.84 (0.99) | −0.05 | .437 | .740 | [−0.27, 0.08] | 30.22% | 42.44% | 27.34% |
| Availability Motives | 2.08 (1.08) | 2.03 (0.99) | −0.05 | .471 | .740 | [−0.20, 0.09] | 32.37% | 37.41% | 30.22% |
Note: Participants who did not drink alcohol at both timepoints (n = 67) were excluded from the regression models on alcohol use motives as these participants were not asked to report their motives for behaviors they did not engage in. The same applies to marijuana use motives (n = 307). Covariates (not shown) included sex, age at Time 1, dummy codes for race/ethnicity, and college student status. BH = Benjamini-Hochberg adjustment for multiple comparisons. Significant effects following adjustment are shown in bold.
Most marijuana use motives did not change significantly (i.e., among marijuana users), and the means for most motives were low, indicating infrequent endorsement. There was, however, a significant increase in boredom motives with nearly half of young adult marijuana users reporting increased boredom motives (d=.34). There were also significant decreases in celebration motives (d=−.35) and alcohol-related motives (d=−.18), but the change in alcohol-related motives was no longer significant after applying the Benjamini-Hochberg adjustment for multiple tests. Moreover, the change in celebration motives was steeper for men, relative women (interaction p=.024; Figure 1F). We also note that, despite non-significant changes for the sample as a whole, there was considerable heterogeneity in change patterns for many of the marijuana use motives.
Discussion
The COVID-19 pandemic has had major impacts on the lives of young adults, and early evidence suggests there may be important changes in substance use.7,19,39 In particular, it is important to understand alcohol and marijuana use among young adults because this age group is at high-risk in general and may be at-risk for elevated or increased use during the pandemic. In this sample of young adults, most living in Washington State during the pandemic, we found that total amount of alcohol consumed–on average–showed little change after the start of the COVID-19 pandemic, but there were notable changes in patterns of drinking. Compared to pre-COVID, young adults tended to drink on more days, but drank less per occasion. This pattern was generally reflected in perceptions young adults have of the drinking among their peers from before to during the pandemic, with young adults correctly thinking their peers increased drinking frequency but decreased amount of alcohol consumed per occasion. It is interesting to note, however, that similar to other studies of perceived drinking norms, young adults overestimated how much young adults were drinking compared to actual rates (e.g., during COVID-19 young adults reported on average 4 drinks per week while perceiving their peers were drinking on average over 9 drinks per week). Similarly, young adults tended to believe that peers had increased in marijuana use during the pandemic, when examination of actual rates showed that this may not be the case. Although marijuana use has remained relatively stable overall, the increases in perceptions of other’s use is alarming. While not consistent with actual rates, they are consistent with popular media references to increased alcohol and marijuana use/sales in legal states.11,13 As the pandemic continues to affect the lives of young adults, it is imperative to present an accurate portrayal of young adult alcohol and marijuana use, as potentially inaccurate information pertaining to major spikes in substance use may normalize this behavior by signaling to young adults that everyone else has increased use.
While the total amounts of alcohol and marijuana consumed may have changed little, the nature of use changed substantially. Prior research indicates that substance use motives are important theoretical antecedents to behavior.25,40 It is thus critical to understand not only what behaviors young adults are engaging in, but how their reasons for substance use may also be changing, as this holds important implications for prevention programs. With motivations to use alcohol increasing for depression coping motives and decreasing for social, enhancement, and conformity motives, there is indication that young adults’ motives for use during the pandemic may have shifted such that social/peer influences are less salient, while self-medication motives may have increased. Other emerging research has shown that rates of depression have been increasing during the pandemic, especially for young adults41; thus, the finding that drinking motives to cope with depression have increased is worrisome. Drinking to cope has been associated with negative consequences and problematic drinking, as well as solitary drinking.42 Interestingly, anxiety coping motives to drink did not increase in this sample, which aligns with recent findings that symptoms of anxiety did not increase in this sample (but depressive symptoms did).6
Unsurprisingly, social and conformity drinking motives decreased during the pandemic, as physical distancing restrictions likely reduced opportunities for social drinking. We similarly found that enhancement drinking motives decreased during the pandemic, which may be due to the common use of alcohol to enhance events and social scenarios that are no longer taking place (e.g., sport events, concerts). Taken together, drinking quantity (per occasion) decreased as did social peer-driven motives to drink, highlighting ways in which the pandemic-related social gathering restrictions may facilitate safer alcohol use patterns and less salient peer influences.
For the most part, marijuana use motives remained relatively similar among those who used marijuana. Consistent with the physical distancing restrictions in place, young adults indicated increased boredom motives and decreased celebratory motives. Interestingly, there was not an increase in coping motives for marijuana use during the pandemic, as was seen with alcohol depression coping motives. It may be, as documented in our prior research,43 that most young adults do not typically drink to cope with depression, but marijuana users do tend to use more frequently for coping reasons. Thus, during the pandemic, there were greater increases in depression motives for alcohol but not for marijuana, as many marijuana users may have already been using for those reasons.
The current study also explored whether intraindividual changes in alcohol and marijuana use, norms, and motives differed by sex, age, college status, and race/ethnicity. Men decreased more steeply in number of drinks per occasion and in celebration motives for marijuana use, while women increased more steeply in perceived norms for drinks per week and number of drinking days per week. Each significant interaction indicated convergence by sex whereby the two groups responded more similarly during the pandemic than they did prior to the pandemic. Given this convergence and the fact that few interactions were identified, it is possible that these interactions may be a result of regression to the mean. These findings are nevertheless hypothesis-generating as additional research is required to disentangle how pandemic-related changes in substance use may differ for men and women.
Testing time by age interactions revealed only one significant difference: Relative to younger participants, older participants reported steeper increases in perceived norms for peers’ drinks per week. Plotting this interaction showed that older participants (relative to younger) thought peers drank less at the pre-COVID timepoint, but the two groups converged at the during-COVID timepoint such that normative estimates were nearly identical for both older and younger adults. Pertaining to use and motives, no age differences were detected, nor were there differences between college students and non-students.
As it is critical to identify racial/ethnic health disparities during the COVID-19 pandemic, we explored time by race/ethnicity interactions, but interpret these results cautiously as our sample did not have enough racial/ethnic diversity to examine all specific minority groups. Whereas the sample, on average, decreased the number of drinks consumed per occasion, we found this may not be the case for some minority groups. Compared to White/Caucasian participants as the reference group, participants categorized as ‘Other’ slightly increased the number of drinks per occasion. However, this category was a heterogeneous combination of racial/ethnic groups that were underrepresented in our sample. Therefore, it is difficult to say which minority groups may be at risk of heavier alcohol use during the COVID-19 pandemic. Nevertheless, this finding highlights the need for in-depth research on minority health disparities related to substance use during the pandemic.
Several limitations warrant consideration. This study relied on self-report data, which are typically reliable for substance use behaviors44 but due to recall and social desirability biases may not be as accurate as objective measures (e.g., transdermal sensors). We also did not examine changes in simultaneous alcohol and marijuana (SAM) use, which is an important issue for future research given increasing SAM use prevalence45 and additional risks of SAM use beyond alcohol or marijuana alone.46 The sample was predominantly college graduates and included limited racial/ethnic diversity. The sample, therefore, may not be representative of young adults nationwide. Alongside the strength of estimating intraindividual changes in study variables from pre- to during-COVID, an inherent limitation to longitudinal research is that participants enrolling in multi-wave studies may alter their behavior in anticipation of forthcoming behavioral observations. In-depth research is needed to unpack racial/ethnic disparities in COVID-19 health outcomes. Although the race/ethnicity composition of this sample approximately matches census data from the counties it was collected in, we encourage researchers to oversample minority groups that may be disproportionately impacted by COVID-19. Finally, future studies may examine whether changes in marijuana use patterns during COVID-19 differed in states where marijuana is legalized.
As the pandemic continues and in preparation for similar future circumstances, it is important to identify risk-factors for increased substance use (i.e., mediators), beyond the moderators tested presently, and to design strategies to prevent risky spikes in use. Although additional studies are needed to understand the heterogeneity in intraindividual changes in substance use, these findings can help to prioritize and inform widespread intervention strategies such as social norms campaigns47 that leverage normative messages highlighting that young adults may not be engaging in extreme levels of substance use as is commonly portrayed in the media. Moreover, these results provide initial indication for how young adults’ motives for use have changed, which can facilitate more tailored strategies to target boredom and depression, for example. Given that alcohol use frequency increased, but the number of drinks consumed per occasion decreased, it remains unclear whether young adults are experiencing more or less negative consequences of use. Indeed, light drinking at-home may be far less risky than patterns of use typically exhibited by young adults (e.g., high-intensity drinking).48
The current study provides timely insight into intraindividual changes in young adults’ alcohol and marijuana use, perceived norms, and motives during the COVID-19 pandemic.9,12 The results have implications for creating pandemic-specific interventions, or tailoring existing evidence-based strategies to this unique time period. As the COVID-19 pandemic continues, we encourage additional research on young adult substance use to build upon these findings that, on average, young adults may (a) be drinking more frequently but in lower quantity, (b) overestimate peers’ alcohol/marijuana use during the COVID-19 pandemic, and (c) be less likely to use substances for social or peer-driven motives but more likely to use for coping and boredom motives.
Implications and Contributions.
Findings from this study provide timely evidence for how young adults’ alcohol and marijuana use, perceived norms, and motives for use may have changed during the COVID-19 pandemic.
Acknowledgements:
Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number R01AA022087, R01AA027496, and T32AA007455. Funds were also provided by the University of Washington Department of Psychiatry and Behavioral Sciences and the Arthur Elzey Research Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the University of Washington.
Footnotes
The combined ‘Other/Non-Hispanic’ group comprised participants who identified as ‘Other’ or as a group that was not large enough to be included as a covariate in the primary analyses as a separate group (i.e., 4% of total sample identified as Black/African American, 0.6% as American Indian/Native Alaskan, 0.5% as Native Hawaiian/Pacific Islander, 1.3% as Arab/Middle Eastern/North African).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mccloskey B, Heymann DL. SARS to novel coronavirus – old lessons and new lessons. Epidemiol Infect. 2020;148:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Implementation of mitigation strategies for communities with local COVID-19 transmission. Atlanta, GA US Dep Heal Hum Serv CDC. Published online 2020:https://www.cdc.gov/coronavirus/2019-ncov/communit. [Google Scholar]
- 3.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;6736(20). doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee CM, Graupensperger SA, Cadigan JM, Einberger C. Multi-faceted COVID-19 related concerns and stressors among young adults and the association with mental health, perceived health, and substance sse. Manuscr Submitt PEER Rev.
- 5.Luchetti M, Lee JH, Aschwanden D, et al. The trajectory of loneliness in response to COVID-19. Am Psychol. Published online 2020:Ahead of Print. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed]
- 6.Lee CM, Cadigan JM, Rhew IC. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J Adolesc Heal. Published online 2020:Ahead of Print. [DOI] [PMC free article] [PubMed]
- 7.Graupensperger S, Benson AJ, Kilmer JR, Evans MB. Social (un)distancing: Teammate interactions, athletic identity, and mental health of student-athletes during the COVID-19 pandemic. J Adolesc Heal. 2020;67:662–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez LM, Litt DM, Stewart SH. Drinking to cope with the pandemic: The unique associations of COVID-19- related perceived threat and psychological distress to drinking behaviors in American men and women. Addict Behav. 2020;110:106532. doi: 10.1016/j.addbeh.2020.106532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020;0366:1–14. doi: 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Satre DD, Hirschtritt ME, Silverberg MJ, Sterling SA. Addressing problems with alcohol and other substances among older adults during the COVID-19 pandemic. Am J Geriatr Psychiatry. Published online 2020:10–13. doi: 10.1016/j.jagp.2020.04.012 [DOI] [PMC free article] [PubMed]
- 11.Bremner J. U.S. alcohol sales increase 55 percent in one week amid coronavirus pandemic. Newsweek. Published online 2020.
- 12.Clay JM, Parker MO. Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? Lancet Public Heal. 2020;2667(20):30088. doi: 10.1016/S2468-2667(20)30088-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roig S. Amid COVID-19 cannabis sales soar. Bull. 2020;May 8.:https://www.bendbulletin.com/business/amid-covid-1.
- 14.Cepeda A, Valdez A, Kaplan C, Hill LE. Patterns of substance use among Hurricane Katrina evacuees in Houston, Texas. Disasters. 2010;34:426–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vlahov D, Galea S, Ahern J, Resnick H. Sustained increased consumption of cigarettes, alcohol, and marijuana among Manhattan residents after September 11, 2001. Am J Public Health. 2004;94:253–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, Patrick ME. Monitoring the Future National Survey Results on Drug Use, 1975–2016: Volume II, College Students and Adults Ages 19–55. Institute for Social Research, The University of Michigan.; 2017. [Google Scholar]
- 17.Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic SUrvey on Alcohol and Related Conditions III. JAMA Psychiatry. 2020;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dumas TM, Ph D, Ellis W, Ph D, Litt DM, Ph D. What does adolescent substance use look Llike during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Heal. 2020;67:354–361. doi: 10.1016/j.jadohealth.2020.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graupensperger S, Jaffe AE, Fleming CB, Kilmer JR, Lee CM, Larimer ME. Changes in college student alcohol use during the COVID-19 pandemic: Are perceived drinking norms still relevant? Emerg Adulthood. Published online 2021:Ahead of Print. [DOI] [PMC free article] [PubMed]
- 20.Napper LE, Kenney SR, Hummer JF, Fiorot S, LaBrie JW. Longitudinal relationships among perceived injunctive and descriptive norms and marijuana use. J Stud Alcohol Drugs. 2016;77:457–463. doi: 10.15288/jsad.2016.77.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee CM, Cadigan JM, Fairlie AM, Lewis MA. Transitions into young adulthood: Extent to which alcohol use, perceived drinking norms, and consequences vary by education and work statuses among 18–20 year olds. Addict Behav. 2018;79:107–112. doi: 10.1016/j.addbeh.2017.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Labrie JW, Lewis MA, Atkins DC, et al. RCT of web-based personalized normative feedback for college drinking prevention: Are typical student norms good enough? J Consult Clin Psychol. 2013;81:1074–1086. doi: 10.1037/a0034087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Acuff SF, Soltis KE, Dennhardt AA, et al. Temporal precedence of self-regulation over depression and alcohol problems: Support for a model of self-regulatory failure. Psychol Addict Behav. Published online 2020:Advance online doi: 10.1037/adb0000505. doi: 10.1037/adb0000505 [DOI] [PMC free article] [PubMed]
- 24.Grant V V, Stewart SH, Connor RMO, Blackwell E, Conrod PJ. Psychometric evaluation of the five-factor Modified Drinking Motives Questionnaire — Revised in undergraduates. Addict Behav. 2007;32:2611–2632. doi: 10.1016/j.addbeh.2007.07.004 [DOI] [PubMed] [Google Scholar]
- 25.Lee CM, Neighbors C, Hendershot CS, Grossbard J. Development and preliminary validation of a comprehensive marijuana motives questionnaire. J Stud Alcohol Drugs. 2009;70:279–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carey KB, Carey MP, Maisto SA, Henson JM. Brief motivational interventions for heavy college drinkers: A randomized controlled trial. J Consult Clin Psychol. 2006;74:943–954. doi: 10.1037/0022-006X.74.5.943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Evans-polce RJ, Maggs JL, Staff J, Lanza ST. The age-varying association of student status with excessive alcohol use: Ages 18 to 30 years. Alcohol Clin Exp Res. 2017;41:407–413. doi: 10.1111/acer.13294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White HR, Stevens AK, Hayes K, Jackson KM. Changes in alcohol consumption among college students due to COVID-19: Effects of campus closure and residential change. J Stud Alcohol Drugs. Published online 2020:Advance Ahead of Print. [DOI] [PMC free article] [PubMed]
- 29.Bambino D, Tai G, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Psychol TraumaTheory, Res Pract Policy. Published online 2020:s17–s21. doi: 10.1093/cid/ciaa815 [DOI]
- 30.Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America. Clin Infect Dis. 2020;12:17–21. [DOI] [PubMed] [Google Scholar]
- 31.Patrick ME, Rhew IC, Lewis MA, et al. Alcohol motivations and behaviors during months young adults experience social role transitions: Micro-transitions in early adulthood. Psychol Addict Behav. 2018;32:895–903. doi:doi: 10.1037/adb0000411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. J Consult Clin Psychol. 1985;53:189–200. [DOI] [PubMed] [Google Scholar]
- 33.Baer JS, Stacy A, Larimer M. Biases in the perception of drinking norms among college students. J Stud Alcohol. 1991;52:580–586. doi: 10.15288/jsa.1991.52.580 [DOI] [PubMed] [Google Scholar]
- 34.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 7th ed. Pearson; 2019. [Google Scholar]
- 35.Lee CM, Kilmer JR, Neighbors C, et al. Indicated prevention for college student marijuana use: A randomized controlled trial. 2013;81:702–709. doi: 10.1037/a0033285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pinheiro JC, Bates D, DebRoy S, Sarkar D. nlme: Linear and Nonlinear Mixed Effects Models. R Packag version 31–147, https//CRANR-project.org/package=nlme. Published online 2020.
- 37.Brooks ME, Kristensen K, van Benthem KJ, et al. Modeling zero-inflated count data with glmmTMB. bioRxiv. 2017;Preprint:doi: 10.1101/132753. The. doi: 10.1101/132753 [DOI]
- 38.Benjamini Y, Hochberg J. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J R Stat Soc. 1995;57:289–300. [Google Scholar]
- 39.Jacobson N, Lekkas D, Price G et al. Flattening the mental health curve: COVID-19 stay-at-home orders result in alterations in mental health search behavior in the United States. PsyArXiv. doi: 10.31234/osf.io/24v5b [DOI] [PMC free article] [PubMed]
- 40.Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychol Assess. 1994;6(2):117–128. doi: 10.1037//1040-3590.6.2.117 [DOI] [Google Scholar]
- 41.Liu CH, Zhang E, Tin G, Ba W, Hyun S, Chris H. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:Ahead of Print. doi: 10.1016/j.psychres.2020.113172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Skrzynski CJ, Creswell KG. Associations between solitary drinking and increased alcohol consumption, alcohol problems, and drinking to cope motives in adolescents and young adults : a systematic review and meta-analysis. Addiction. Published online 2020:Ahead of Print. doi: 10.1111/add.15055. doi: 10.1111/add.15055 [DOI] [PMC free article] [PubMed]
- 43.Patrick ME, Fleming CB, Fairlie AM, Lee CM. Cross-fading motives for simultaneous alcohol and marijuana use: Associations with young adults ‘ use and consequences across days. Drug Alcohol Depend. 2020;213:108077. doi: 10.1016/j.drugalcdep.2020.108077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simons JS, Wills TA, Emery NN, Marks RM. Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addict Behav. 2015;50:205–212. doi: 10.1016/j.addbeh.2015.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McCabe SE, Arterberry BJ, Dickinson K, et al. Assessment of changes in alcohol and marijuana abstinence, co-use, and use disorders among US young adults from 2002 to 2018. JAMA Pediatr. 2020;48109. doi: 10.1001/jamapediatrics.2020.3352 [DOI] [PMC free article] [PubMed]
- 46.Lee CM, Patrick ME, Fleming CB, et al. A daily study comparing alcohol‐related positive and negative consequences for days with only alcohol use versus days with simultaneous alcohol and marijuana use in a community sample of young adults. Alcohol Clin Exp Res. 2020;44:689–696. doi: 10.1111/acer.14279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mattern JL, Neighbors C. Social norms campaigns: Examining the relationship between changes in perceived norms and changes in drinking levels. Published online 2003:489493. [DOI] [PubMed]
- 48.Patrick ME, Cronce JM, Fairlie AM, Atkins DC, Lee CM. Day-to-day variations in high-intensity drinking, expectancies, and positive and negative alcohol-related consequences. Addict Behav. 2016;58:110–116. doi: 10.1016/j.addbeh.2016.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]